Abstract
Objectives
This study has been aimed at evaluating knowledge, attitudes and behaviour of university students regarding the usage of antibiotics focusing on differences between medical and nonmedical students.
Methods
This cross-sectional questionnaire-based study was performed on 800 students of the University of Novi Sad, Serbia.
Results
The identified predictors of adequate antibiotic knowledge were enrolled in medical program, higher grade average and appropriate use of antibiotics during last infection. Multivariate regression identified following predictors of self-medication: being medical student (B = 0.715; p < 0.001), more frequent (B = 0.628; p < 0.001) and irregular (B = 0.584; p = 0.001) antibiotic use, a family member engaged in medical profession (B = 0.789; p < 0.001), living in dormitory (B = 0.679; p = 0.007) or rented apartment (B = 0.621; p = 0.002), using antibiotics until symptoms resolved (B = 1.616; p < 0.001) or until the bottle was finished (B = 0.628; p < 0.001) during the last infection.
Conclusions
Although a high number of students showed adequate knowledge about antibiotics, numerous misconceptions were recorded, including self-medication. Further educational interventions are necessary to improve their understanding, perceptions as well as their behaviour towards antibiotic use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Serbia belongs to a group of European countries with the highest rates of resistance as well as with a high antibiotic consumption rate (WHO 2018a, b). Despite increasing concerns with antimicrobial resistance in Serbia, the implementation of physician education programs, promotion of rational use of antibiotics and hospital-based antimicrobial stewardship programs challenging have been impeded by limited resources (Kalaba et al. 2018). In addition, based on 2015 report by the WHO Europe Antimicrobial Medicines Consumption Network presenting data on 46 countries, overall consumption of antibiotics in these countries ranged from 7.66 to 38.18 DDD per 1000 inhabitants per day. Serbia with the consumption of 31.57 DDD per 1000 inhabitants per day was surpassed in total antibiotic consumption only by Greece and Turkey, while the lowest antibiotic consumption was reported in Netherlands, Germany and Austria.
Factors influencing overuse of antibiotics include doctors’ competence and experience, diagnostic uncertainties as well as patients’ wrong habits and their lack of knowledge (Eng et al. 2003; Gualano et al. 2015; Mc Nulty et al. 2007). In order to improve antibiotic use and restrain resistance through interventions such as educational campaigns, it is important to have an extensive understanding of the knowledge, behaviour and attitudes towards antibiotics within different population groups. So far, the only thorough study has been conducted on a representative sample of the general population in Serbia and some areas of misconceptions and improper behaviour have been identified: respondent’s uncertainty as to whether antibiotics are effective against viruses and high percentage of self-medication with antibiotics (Horvat et al. 2017).
An increasing number of research focused attention on university medical (as the future antibiotic providers) and nonmedical students, since their knowledge, attitudes and behaviour in relation to usage of antibiotics can greatly impact antibiotic-related issues in the future (Huangn et al. 2013; Jamshed et al. 2014; Scaioli et al. 2015).
Therefore, the objective of this study was to evaluate knowledge, attitudes and behaviour of university students regarding the usage of antibiotics in Serbia.
Methods
Data collection
The study was conducted at the University of Novi Sad (UNS), Serbia, between January and February of 2019. UNS, as the second largest university in Serbia, with more than 50,000 students in 2018 (4000 from medical and health science disciplines) is also one of the largest educational and research centres in Central Europe. The target study sample of 800 final year students was divided into two groups, medical (M) and nonmedical (NM). M group (n = 400) included students of health professions allowed to prescribe antibiotics in Serbia (Medicine, n = 200; Veterinary medicine, n = 100; Dentistry, n = 100). NM group (n = 400) included students randomly selected from other disciplines (Technical Sciences, Agriculture, Economic and Technology, 100 students from each program). The sample size calculated according to the estimate of 81.3% of M students and 92% of NM students practicing self-medication, with 10% relative precision and 95% confidence interval was 234 and 114, respectively (Klemenc-Ketis et al. 2010; Trninic et al. 2018). The sample size was deliberately exceeded to increase the power of the study and to provide for exclusions, dropouts, and the need to perform subgroup analysis.
The students were approached and asked to complete the questionnaire during the last 15 min of their scheduled classes. Written informed consent was obtained prior to data collection. The study was approved by the Ethical Committee of the Faculty of Medicine in Novi Sad (Approval Number 01-39/240/1).
The questionnaire (S1 Questionnaire) used in this study is based on the questionnaire of Buke et al. (2003) and was previously used in a study conducted in general population in Serbia7. To enable correct answers, necessary modifications were made to questions and statements. The content, comprehension, readability and design of the questionnaire were pre-tested on 30 students at the University of Novi Sad. The questionnaire was divided into three sections. The first section consisted of eight questions referring to the respondents’ sociodemographic and academic characteristics. The second section was related to knowledge about antibiotics and consisted of 12 claims which were supposed to be categorized as “true” or “false”. The knowledge score was then determined by giving one point for each correct answer giving a maximum knowledge score of 12. The third section, which consisted of 15 yes/no questions and multiple-choice questions, was designed to determine the respondents’ attitudes and behaviour. The whole questionnaire is available as a supplementary file.
Data analysis
Descriptive and comparative statistical data analysis was performed with the IBM SPSS Statistics 22 (IBM Corporation, Armonk, NY, USA) software. Out of descriptive statistical methods, measures of central tendency (mean, median), measures of variability (standard deviation) and frequency were used. Two categorical variables were created—status of antibiotic knowledge (adequate/inadequate) and self-medication (yes/no). Knowledge categories were determined according to the median of knowledge score of total sample (10, interquartile range 2–12), and respondents were grouped into those with adequate (score ≥ 10) and those with inadequate knowledge (score ≤ 9). Self-medication was determined based on the answers to three questions in Part 3 of the questionnaire. This variable, “self-medication”, was generated by combining the answers for questions “Have you ever used antibiotics in order not to get ill” (“yes”), “Have you ever started antibiotics on your own when you got ill” (“yes”) and “How did you get antibiotics during your last infection?” (those who answered any of the following: “I used the antibiotic previously used or as advised by my friends; I used the antibiotic previously prescribed by my doctor; I asked the pharmacist and used the antibiotic recommended by them”).
The Chi-squared test was used to examine the association between categorical and sociodemographic variables. The Mann–Whitney U test was used for numeric data with non-normal distribution and ordinal data. Association of respondents’ characteristics with adequate antibiotic knowledge and self-medication was first evaluated using univariate logistic regression. Multivariate logistic regression included those predictors all variables with p < 0.05 in the univariate analysis. There was no multicolinearity between the predictors. The results were reported as odds ratio (ORs) with 95% confidence intervals (CIs). All p values less than 0.05 were considered significant.
Results
Sociodemographic and academic characteristics
Slightly less than two-third (63.9%) of the total 800 sample were females, and the mean age was 23.2 ± 1.6 years (Table 1). Several sociodemographic and academic characteristics were significantly different between M and NM students. For example, M students less frequently visited their general practitioner 5–10 (2.2%) or 10 times (0.5%) in the past year compared to the NM students (6.8% or 1.3%, respectively) (p < 0.001). Additionally, 33.5% of the M students had a relative working in health-related field versus 18% of the NM students (p < 0.001).
Knowledge on antibiotic use
The participants demonstrated a good knowledge on antibiotic use: percentage of respondents who provided correct answers was higher than 80% in 5 of 12 statements proposed (Table 2). The lowest percentage was recorded for the statements “Antibiotics can be used for common cold” and “An antibiotic is used until the bottle finishes”. Out of 800 students, 56.8% showed adequate knowledge, while 43.2% had inadequate knowledge. M students showed a significantly higher knowledge score compared to NM students (p < 0.001). The median knowledge score of M students was 11 (interquartile range 10–12), while the median knowledge score of NM students was 9 (interquartile range 7–10) (Fig. 1.). Out of M students, 77.8% showed adequate knowledge, compared with 35.8% of NM students.
Attitudes and behaviour of respondents
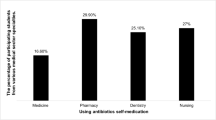
Larger share of NM students (37.3%) than M students (24.3%) started antibiotics by themselves when they were ill (p = 0.010) (Table 3). Irregular use of antibiotics prescribed by a doctor was reported by 27.5% of NM students and 36.0% of M students (p < 0.001). More than one-third of M and NM students visited their doctor and used the prescribed antibiotic (71.5% vs. 68.3%, respectively) (p = 0.343). Out of sociodemographic, academic characteristics and attitudes and behaviour regarding antibiotic use, nine variables (groups of medical/nonmedical students, number of visits to a general practitioner in the last 12 months, frequency of antibiotics use, average grade, use of antibiotic on their own, irregular use of antibiotic, duration of antibiotic use during the last infection, lack of effect of antibiotic therapy during treatment) showed a significant association with the students’ knowledge using univariate logistic regression. The model predicting knowledge about antibiotics’ use presented that M students were more than five times more likely to have adequate knowledge than NM students (OR = 5.; B = 1.683; p < 0.001) (Table 4); students with an average grade of 8 and higher have a 60% higher chance of adequate knowledge (OR = 1.6; B = 0.480; p = 0.013) and those who regularly take antibiotics prescribed by the doctor have a 50% higher chance of adequate knowledge (OR = 1.5; B = 0.381; p = 0.047); students who used antibiotics during the last infection until the bottle was finished 2.3 more likely to have adequate knowledge (OR = 2.3; B = 0.851; p = 0.005) or for the period advised by the doctor (OR = 5.5; B = 1.696; p < 0.001) were 5.5 times more likely to have adequate knowledge than those who reported cessation of antibiotic use after their symptoms resolved (as a reference category); students who chose the answer “other” (such as antibiotic has always worked, and I switch to natural remedies) when antibiotic therapy fails during the treatment were three times more likely to contribute to the prediction (OR = 3.1; B = 1.135; p = 0.001) than those who continued the use of antibiotics for the recommended period (as a reference category). Since three questions analysed the students’ propensity to self-medication, the results showed that in comparison with 319 students who reported self-medication (39.9% of total sample), self-medication was reported among 42.8% of respondents from the group of M and 37% of the NM students (p = 0.097).
The results of the logistic regression highpoint M having a two times higher likelihood of self-medication than NM students (OR = 2.0; B = 0.715; p < 0.001) (Table 5), also students with more frequent use of antibiotics (OR = 1.9; B = 0.628; p < 0.001) and students with irregular antibiotic use (OR = 1.8; B = 0.584; p = 0.001), as well as students who declared to have at least one relative working as health professional (OR = 2.2.; B = 0.789; p < 0.001), had all two times higher likelihood of self-medication. Students who lived in university dormitories (OR = 2.0; B = 0.679; p = 0.007) and in rented apartments (OR = 1.9; B = 0.621; p = 0.002) were more prone to self-medication than those who lived with their parents (as a reference category). Lastly, students who used antibiotics during the last infection until the bottle was finished (OR = 2.0; B = 0.716; p < 0.001) or until their symptoms resolved (OR = 5.0; B = 1.616; p < 0.001) had 2 and 3 times higher probability (respectively) of self-medication than those who took antibiotics for the period advised by the medical doctor (as a reference category).
Reasons for self-medication with antibiotics
Out of the total sample of 800 students, the most common reason for self-medication was sore throat. Medical students were most likely to list sore throat as a reason for self-medication, whereas nonmedical students were most prone to self-medication in case of common cold (25.8% and 29.8%, respectively) (Fig. 2).
Discussion
To the best of our knowledge, this is the first study investigating these topics among students, and not general population in Serbia (Horvat et al. 2017). Our study showed that the interviewed students had good knowledge on antibiotics, although the percentage of students with adequate knowledge was slightly lower than among general population in Serbia (56.8% vs. 61.6%, respectively) (Horvat et al. 2017). Similar to other studies, the difference between M and NM students was especially obvious when the answers to the specialized question whether antibiotics can be used for the treatment of common cold were analysed (Huangn et al. 2013; Jairoun et al. 2019; Ghadeer et al. 2012). While 67% of the total sample of students believed that antibiotics should not be used for common cold, this percentage was significantly higher among M than NM students (79.3% and 52.8%, respectively). On the other hand, in the similar study conducted in Turkey 83.1% of the students both in M and NM group believed that antibiotics could be used against common cold (Buke et al. 2005).
Furthermore, this result of the present study is encouraging when compared to the Serbian general population. The 2015 WHO report on Antibiotic Resistance pointed out how only 28% of the Serbian subjects interviewed believed that antibiotics were not effective against cold and flu, while 4% did not know the answer to the question (WHO 2015). However, the results of the first detailed study performed on Serbian general population by Horvat et al. (2017) showed that 41.6% of the respondents stated that antibiotics were not useful for common cold. Similarly, in the first systematic review compiling 24 studies on the knowledge on antibiotic use, it was stated that about 50% of the respondents did not know that antibiotics were not effective against cold and flu (Gualano et al. 2015).
About one-third of all the students stated that antibiotics should be used until the bottle is finished or until symptoms disappear and the same percentage of respondents indicated that twice-daily antibiotic regimen entails taking medicine after waking up and before going to bed at night. These findings demonstrate clear misconception among our respondents regarding adherence to antibiotic regimens and are comparable with previously published data related to both M and NM students in India, Portugal, Italy and Turkey (Azevedo et al. 2009; Buke et al. 2005; Khan and Banu 2013; Scaioli et al. 2015). Our results are not in agreement with the results of the study performed in USA, where almost all the medical students interviewed were aware that inappropriate use of antibiotics could harm patients and increase prevalence of resistant strains of bacteria (Hawkings et al. 2008; Minen et al. 2010).
Despite the adequate level of knowledge, 11% of study population reported prophylactic antibiotic use (14.8% of NM and 7.3% of M students), which is almost twice as high as among general population in Serbia (6.0%), but significantly lower than among students in China (Horvat et al. 2017; Wang et al. 2017). Similarly, about 22% of NM and only 10% of M students used antibiotics only until their symptoms resolved in our study. This is similar to the results obtained in the study of M students in India (Khan and Banu 2013), whereas this behaviour was recorded among more than 70% of university students from Jordan (Suaifan et al. 2012), India (Limaye et al. 2018) and Portugal (Azevedo et al. 2009). This misconception in the antibiotic use may put the patients at risk of relapse with resistant pathogenic bacteria (Dyar et al. 2013; Sanya et al. 2013).
However, in addition to antibiotic prescribed by the doctor, 8.8% of our study sample students most frequently used leftover antibiotics previously prescribed by a physician. This is a considerably lower percentage than among Italian medical students (17.7%), Turkish students (25.9%) (Buke et al. 2005; Scaioli et al. 2015). In addition, it is also lower than the one reported for Serbian general population (17%) (Horvat et al. 2017). Similar to the latter study, our investigation highlights that leftovers are the most common source of self-medication in Serbia after enforcement of law restricting the purchase of antibiotics at the pharmacy without he medical prescription in 2011 (Horvat et al. 2017; Kusturica et al. 2015; Tomas et al. 2017). According to this result, Serbia is now more similar to southern, northern and western European countries where the major source of self-medication is leftover medications whereas in eastern countries purchase of antibiotics without prescription still occurs at high rate (Grigoryan et al. 2008).
Factors that were plausibly expected to have huge impact on knowledge about antibiotics among students, such as previous medical education level and higher average grade, showed a significant contribution to the prediction in our study. In the present study, medical students had more than 5 times greater odds for having adequate knowledge on antibiotic than nonmedical respondents. The same pattern was observed between medical and nonmedical students in the literature (Ghadeer et al. 2012; Huangn et al. 2013; Jairoun et al. 2019). These results are in accordance with other studies among general population and students, suggesting that higher education level represents a positive predictor for adequate knowledge (Dutt et al. 2018; Horvat et al. 2017; Minen et al. 2010; You et al. 2008).
Our research results showed that students who used antibiotics during the last infection until the bottle was finished or for the period advised by the doctor were more likely to have adequate knowledge than those who reported cessation of antibiotic use after their symptoms resolved. This was consistent with a study conducted in Korea, where adult respondents with adequate knowledge were 1.52 times more likely to demonstrate appropriate attitude (Kim et al. 2011). Interestingly, some promising results of Eurobarometer study (2018) demonstrate that people with low level of knowledge might actually benefit the most from the targeted media campaigns as they were more likely to change their habits.
Our study has shown that self-medication with antibiotics represents a common behaviour among students in Novi Sad (39.9%) and that the self-medication rate is slightly lower compared to the general population in Serbia (Horvat et al. 2017).
However, our study showed that M students had twice more likelihood for self-medication practice compared to NM students, which is comparable with the study performed in Italy, where it was shown that every year spent at university significantly decreased the chance of using antibiotics only when prescribed by the doctor (Scaioli et al. 2015). Similarly, the Chinese and Libyan studies documented a significantly higher rate of self-medication practice among medical students who had taken formal lectures about antibiotics (Ghaieth et al. 2015; Lv et al. 2014; Pan et al. 2012). Although it seems that students feel more confident with their knowledge regarding antibiotics use, as they attend medical related faculties, Iranian and Palestinian studies yielded the contrasting results and pointed that nonmedical students reported slightly higher rates of self-medication (Sarahroodi et al. 2010; Sawalha 2008).
In addition, our study showed that students who lived in university dormitories and in rented apartments were more prone to self-medication in comparison with those who lived with their parents. It seems that self-medication could be a good option for students who live either alone or without parents who take care of them, especially when they need to save time during the examination season. We also found that common cold, flu, sore throat and fever were the predominant health problems that provoked self-medication both in M and NM students, which is consistent with many previous studies (Buke et al. 2005; Kim et al. 2011; Sarahroodi et al. 2010; Sawalha 2008).
The strengths of the present study are that this is the first investigation on this topic among the university students in Serbia as well as that the size sample are higher than other studies on similar topic (Azevedo et al. 2009; Buke et al. 2005; Ghadeer et al. 2012; Minen et al. 2010).
Interpretation of the findings of this study should take into account certain potential limitations that might impact upon its conclusions. Because self-administered questionnaires are used instead of face-to-face interviews that are considered the gold standard method for survey administration, there is a possibility that participants may have over- or under-reported socially desirable behaviours. M students (medicine, dentistry and veterinary medicine) of the University of Novi Sad do not have specifically focused subject on antimicrobial use and resistance.
This topic is discussed in Pharmacology and Microbiology courses. Furthermore, the investigation was carried out in a single university centre in Novi Sad rather than opening up to different contexts, which could have given different results. Another limitation is that knowledge, attitudes and behaviour regarding antibiotic use as well as self-medication rates reported by this study were compared with the results obtained in the study performed among the general population of Serbia in 2017 (Horvat et al. 2017), and self-medication practices might have changed since. However, the results from this study can still provide important information about self-medication practice among the study population.
Conclusion
This study was the first in Serbia to assess university students’ knowledge, attitudes and behaviour related to antibiotics. The results indicate that although almost two-thirds of the students have shown adequate knowledge about antibiotics, numerous misconceptions that include their belief that antibiotics are appropriate in the treatment of common cold as well as that treatment lasts until the symptoms resolve have been recorded. Students with lower average grade, NM students, those who are prone to discontinue the therapy on the cessation of the symptoms and who follow the recommendation of the doctor even if they think that the prescribed antibiotics are not effective are strikingly in the need of improved knowledge about antibiotics.
Improper attitudes and behaviour regarding antibiotic use were also common in our study, whereas prophylactic and irregular use of antibiotics and discontinuation of treatment as soon as the symptoms subside were frequently recorded, particularly among nonmedical students. Additionally, our study demonstrated that dispensing whole packages of antibiotics leads to a higher number of students who are in the possession of leftover antibiotics, which is the most common source of self-medication nowadays in Serbia. Therefore, implementation of antibiotic regulation which will urge pharmacists to dispense antibiotics on unit-dose basis instead of selling a whole drug package should be taken into consideration.
This study has revealed a considerable rate with antibiotics among student’s community. Furthermore, medical students were the ones who pursued this practice more frequently, especially those who had a relative working as a health care professional and who lived in dormitories or rented apartments. Since the healthcare profession students will be a behavioural model for citizens and patients and 1 day prospective prescribers of these drugs, it is important to increase awareness on this topic during the study course.
Finally, this study has shown that there is a need for educational programs on antibiotics and their correct use targeting Serbian university students. It seems prudent to incorporate elective courses on antibiotic proper use among NM students and to re-evaluate the educational curricula of future antibiotic prescribers, specifically teaching of clinical pharmacology. Most importantly, there is a need to incorporate curriculum on abuse of antibiotics and the harm of such practice on short and long run.
Further research to investigate knowledge, attitudes and practice towards antibiotic in other settings will help to adopt and implement successful future educational campaigns in promotion of rational antibiotic use in Serbia where the problem of bacterial resistance is increasing at an alarming rate.
References
Azevedo MM, Pinheiro C, Yaphe J, Baltazar F (2009) Portuguese students’ knowledge of antibiotics: a cross-sectional study of secondary school and university students in Braga. BMC Public Health 9:359. https://doi.org/10.1186/1471-2458-9-359
Buke CA, Ermertcan S, Hosgor-Limoncu M, Ciceklioglu M, Eren S (2003) Rational antibiotic use and academic staff. Int J Antimicrob Agents 21:63–66. https://doi.org/10.1016/S0924-8579(02)00272-8
Buke C, Hosgor-Limoncu M, Ermertcan S, Ciceklioglu M, Tuncel M, Köse T, Eren S (2005) Irrational use of antibiotics among university students. J Infect 51(2):135–139. https://doi.org/10.1016/j.jinf.2004.12.001
Dutt HK, Sarkhil MZ, Hasseb AM, Singh G (2018) A comparative knowledge, attitude, and practice study of antimicrobial use, self-medication and antimicrobial resistance among final year students of MBBS, BDS, and BSc Nursing at a tertiary care hospital at Kannur. Natl J Physiol Pharm Pharmacol 8(9):1305–1311. https://doi.org/10.2147/IJGM.S200641
Dyar OJ, Howard P, Nathwani D, Pulcini C (2013) Knowledge, attitudes, and beliefs of French medical students about antibiotic prescribing and resistance. Méd Maladies Infect 43(10):423–430. https://doi.org/10.1016/j.medmal.2013.07.010
Eng JV, Marcus R, Hadler JL et al (2003) Consumer attitudes and use of antibiotics. Emerg Infect Dis 9:1128–1135. https://doi.org/10.3201/eid0909.020591
Ghadeer ARY, Suaifan Mayadah Shehadeh, Darwish Dana A, Al-Ijel Hebah, Yousef Al-Motassem M, Darwish Rula M (2012) A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. Afr J Pharm Pharmacol 6(10):763–770. https://doi.org/10.5897/AJPP12.080
Ghaieth MF, Elhag SR, Hussien ME, Konozy EH (2015) Antibiotics self-medication among medical and nonmedical students at two prominent Universities in Benghazi City, Libya. J Pharm Bioallied Sci 7(2):109–115. https://doi.org/10.4103/0975-7406.154432
Grigoryan L, Burgerhof JG, Degener JE, Deschepper R, Lundborg CS et al (2008) Determinants of self-medication with antibiotics in Europe: the impact of beliefs, country wealth and the healthcare system. J Antimicrob Chemother 61:1172–1179. https://doi.org/10.1093/jac/dkn054
Gualano MR, Gili R, Scaioli G, Bert F, Siliquini R (2015) General population’s knowledge and attitudes about antibiotics: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf 24(1):2–10. https://doi.org/10.1002/pds.3716
Hawkings NJ, Butler CC, Wood F (2008) Antibiotics in the community: a typology of user behaviours. Patient Educ Couns 73(1):146–152. https://doi.org/10.1016/j.pec.2008.05.025
Horvat OJ, Tomas AD, Paut Kusturica MM, Savkov AV, Bukumirić DU, Tomić ZS, Sabo AJ (2017) Is the level of knowledge a predictor of rational antibiotic use in Serbia? PLoS ONE 7:e0180799. https://doi.org/10.1371/journal.pone.0180799
Huangn Y, Gu J, Zhang M, Ren Z, Yang W, Chen Y et al (2013) Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ 13:163. https://doi.org/10.1186/1472-6920-13-163
Jairoun A, Hassan N, Ali A, Jairoun O, Shahwan M (2019) Knowledge, attitude and practice of antibiotic use among university students: a cross sectional study in UAE. BMC Public Health 19(1):518. https://doi.org/10.1186/s12889-019-6878-y
Jamshed SQ, Elkalmi R, Rajiah K, Al-Shami AK, Shamsudin SH, Siddiqui MJ et al (2014) Understanding of antibiotic use and resistance among final-year pharmacy and medical students: a pilot study. J Infect Dev Ctries 8:780–785. https://doi.org/10.3855/jidc.3833
Kalaba M, Kosutic J, Godman B, Radonjic V, Vujic A, Jankovic S et al (2018) Experience with developing antibiotic stewardship programs in Serbia: potential model for other Balkan countries? J Comp Eff Res 7:247–258. https://doi.org/10.2217/cer-2017-0055
Khan AKA, Banu GKKR (2013) Antibiotic resistance and usage-a survey on the knowledge, attitude, perceptions and practices among the medical students of a Southern Indian Teaching Hospital. J Clin Diagn Res 8:1613–1616. https://doi.org/10.7860/JCDR/2013/6290.3230
Kim SS, Moon S, Kim EJ (2011) Public knowledge and attitudes regarding antibiotic use in South Korea. J Korean Acad Nurs 41(6):742–749. https://doi.org/10.4040/jkan.2011.41.6.742
Klemenc-Ketis Z, Hladnik Z, Kersnik J (2010) Self-medication among healthcare and non-healthcare students at university of Ljubljana, Slovenia. Med Princ Pract 19(5):395–401
Kusturica MP, Tomic Z, Bukumiric Z, Horvat O, Pavlovic N, Mikov M, Sabo A (2015) Antibiotics in Serbian households: a source of potential health and environmental threats? Cent Eur J Public Health 23(2):114–118. https://doi.org/10.21101/cejph.a4093
Limaye D, Naware S, Bare P, Dalvi S, Dhurve K, Sydymanov A, Limaye V, Pitani RS, Kanso Z, Fortwengel G (2018) Knowledge, attitude and practices of antibiotic usage among students from Mumbai University. Int J Res Med Sci 6(6):1908. https://doi.org/10.18203/2320-6012.ijrms20182270
Lv B, Zhou Z, Xu G et al (2014) Knowledge, attitudes and practices concerning self-medication with antibiotics among university students in western China. Trop Med Int Health 19:769–779. https://doi.org/10.1111/tmi.12322
Mc Nulty CAM, Boyle P, Nichols Clappison P, Davey P (2007) Don’t wear me out-The public’s knowledge of and attitudes to antibiotic use. J Antimicrob Chemother 59(4):727–738. https://doi.org/10.1093/jac/dkl558
Minen MT, Duquaine D, Marx MA, Weiss D (2010) A survey of knowledge, attitudes, and beliefs of medical students regarding antimicrobial use and resistance. Microb Drug Resist 16(4):285–289. https://doi.org/10.1089/mdr.2010.0009
Pan H, Cui B, Zhang D, Farrar J, Law F et al (2012) Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among university students in southern China. PLoS ONE 7:e41314. https://doi.org/10.1371/journal.pone.0041314
Sanya TE, Titilayo OF, Adisa R, Segun JS (2013) Use of antibiotics among non-medical students in a Nigerian University. Afri Health Sci 13(4):1149–1155. https://doi.org/10.4314/ahs.v13i4.41
Sarahroodi S, Arzi A, Sawalha AF, Ashtarinezhad A (2010) Antibiotic self-medication among south Iranian University students. Int J Pharmacol 6(1):48–52. https://doi.org/10.3923/ijp.2010.48.52
Sawalha AF (2008) A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Social Adm Pharm 4:164–172. https://doi.org/10.1016/j.sapharm.2007.04.004
Scaioli G, Gualano MR, Gili R, Masucci S, Bert F, Siliquini R (2015) Antibiotic use: a cross-sectional survey assessing the knowledge, attitudes and practices amongst students of a school of medicine in Italy. PLoS ONE 10:e0122476. https://doi.org/10.1371/journal.pone.0122476
Special Eurobarometer 478, Antimicrobial Resistance (in the EU) European commission (2018) Available: http://data.europa.eu/euodp/data/dataset/S2190_90_1_478_ENG
Suaifan GA, Shehadeh M, Darwish DA, Al-Ije H, Yousef AM, Darwish RM (2012) A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. Afr J Pharm Pharmacol 6(10):763–770. https://doi.org/10.5897/AJPP12.080
Tomas A, Kusturica MP, Tomic Z, Horvat O, Koprivica DD, Bukumiric D, Sabo A (2017) Self-medication with antibiotics in Serbian households: a case for action? Int J Clin Pharm 39(3):507–513. https://doi.org/10.1007/s11096-017-0461-3
Trninic B, Vlajic N, Tomas A, Pavlovic N (2018) Self-medication attitudes and behaviour among medicine and pharmacy students. In: Abstract book of the 59th Congress of students of biomedical sciences, Kopaonik, Serbia, p 399
Wang X, Peng D, Wang W, Xu Y, Zhou X, Hesketh T (2017) Massive misuse of antibiotics by university students in all regions of China: implications for national policy. Int J Antimicrob Agents 50(3):441–446. https://doi.org/10.1016/j.ijantimicag.2017.04.009
World Health Organization (2015) Antibiotic resistance: multi-country public awareness survey. WHO Available: https://apps.who.int/iris/handle/10665/194460
World Health Organization (2018a) Central Asian and Eastern European surveillance of antimicrobial resistance. Annual report WHO Available: http://www.euro.who.int/__data/assets/pdf_file/0007/386161/52238-WHO-CAESAR-AR2018_low_V11_web.pdf?ua=1
World Health Organization (2018b) WHO report on surveillance of antibiotic consumption: 2016–2018 Early Implementation. Available: https://www.who.int/medicines/areas/rational_use/who-amr-amc-report-20181109.pdf
You JHS, Yau B, Choi KC, Chau CTS, Huang OR, Lee SS (2008) Public knowledge, attitudes and on antibiotic use: a telephone survey in Hong Kong. Infection 36:153–157. https://doi.org/10.1007/s15010-007-7214-5
Acknowledgements
We would like to thank all the students involved in this research for giving up their time to take part in the study.
Funding
This work was supported by the Ministry of Science and Technological Development, Republic of Serbia [Grant Number 451-03-68/2020-14/200117]; and the Provincial Secretariat for Science and Technological Development, Autonomous Province of Vojvodina [Grant Number 142-451-2565/2019-02].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Ethical Committee of the Faculty of Medicine in Novi Sad (Approval Number 01-39/240/1).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue “Adolescent health in Central and Eastern Europe”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Horvat, O., Tomas, A., Paut Kusturica, M. et al. Serbian students’ knowledge, attitudes and behaviour towards antibiotic use: is there room for improvement?. Int J Public Health 65, 1257–1267 (2020). https://doi.org/10.1007/s00038-020-01448-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-020-01448-6