Abstract
Background Irregular antibiotic use, including self-medication contributes to the development of antibiotic resistance. One method of accessing antibiotic use in the community is through obtaining an in house inventory of drugs. Objective The aim of this study was to investigate the extent of storage and self-medication with antibiotics agents in households in Novi Sad, Serbia. Setting Households in Novi Sad. Method The study was performed during a 4-month period (October 2015–January 2016) using a sample of 112 households in Novi Sad, Serbia. Two trained interviewers performed the survey by visiting each household. The study consisted of making an inventory of all drugs in household and a semi-structured interview about drug use practices and perceptions. Main outcome measure Number of antibiotics obtained without prescription. Results Out of 112 surveyed households, antibiotics were encountered in 55 (49.1%). Antibiotics constituted 11.98% (92/768) of total number of drug items in households. Out of all antibiotics in households, 41 (44.57%) were not in current use, and presented left-overs from previous treatment. Antibiotics were usually acquired with prescription (67, 67.7%), while about a quarter of packages were used for self-medication—purchased at pharmacy without prescription (19, 20.65%) or obtained through friends or family member (6, 6.52%).The most commonly used antibiotics for self-medication was amoxicillin (reported indications included common cold, cough, pharyngitis and tooth-ache). Conclusion Antibiotics were present in large share of households in Novi Sad. Self-medication with antibiotics and sale of antibiotics without prescription represent an important problem in Serbia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impacts on practice
-
Single most important source of antibiotics used for self-medication in Serbia are pharmacies.
-
Antibiotic sale restrictions still seem not to be completely implemented in Serbia, four years after the law was changed.
Introduction
Improper antibiotic use is recognized as a major factor for development of resistance which reaches alarmingly high rates in countries of South and South-East Europe [1–3]. Infections caused by resistant bacteria are an important cause of morbidity, mortality, healthcare costs and productivity losses in Europe [4, 5]. Antibiotics self-medication [6–8] not only contributes to the development of resistance, but also carries a risk of treatment failure and adverse effects potentially requiring additional therapy, burdening the health care system with subsequent financial costs [7, 9].
Recent studies indicate that Serbia is country with high antibiotic consumption [10]. One of the methods to effectively examine antibiotic use in general population is physical inspection of drugs in households [11, 12]. Antibiotics should be stored in households only if a household member is currently being treated, but due to non-compliance with prescribed therapy, storing the drugs for future use, unused packages of these drugs can be found in many households [6]. For this reason, data on antibiotic use based on either pharmacy or health care institutions reports may not be completely reliable, as they do not take patient compliance into account [13]. Relatively limited number of studies investigating antibiotics in households has been conducted worldwide [6, 7, 9, 14–17], but they demonstrated that antibiotics were commonly stocked and frequently used for self-medication [16, 17]. In Spain 42% and in Russia 83.6% of the surveyed households had antibiotics for systemic use in their home medicine cabinets [14, 16], while in Brazil antibiotics comprised 13%, and in Greece 17% of total medications found in households [15]. A study conducted in Serbia in 2012 showed that antibiotics stored in home-pharmacies represent a significant source of antibiotic misuse in the community [6]. Nearly half of the surveyed households stored antibiotics, and approximately one-third of these were used for self-medication. However, this earlier research was conducted shortly after the enforcement of laws restricting the purchase of antibiotics without medical prescription (November 2011), and because nationwide implementation of this regulation has faced some hurdles, the level of adherence to these regulations is uncertain. Therefore, it is of great importance to get a deeper insight into storage and patterns of antibiotic use in Serbian households 4 years after this enforcement occurred.
Aim of the study
The objectives of this study were to identify the presence, volume and structure of antibiotics in Novi Sad households. In addition, this study aimed evaluating the extent of self-medication with antibiotics.
Ethics approval
The study was approved by the Ethical Committee of the Faculty of Medicine in Novi Sad (approval number: 01-3384/1).
Method
This prospective study was performed on a sample of households in the municipality of Novi Sad over four-month period (01.10.2015–15.01.2016). Sample size was calculated based on the results of a study conducted in 2012 on 383 households in Novi Sad [8], where the percentage of antibiotics in total drug supplies was 7.3%. Based on this result, a sample size necessary to estimate the proportion of antibiotics bought without prescription with 95% confidence interval and 5% precision was 89 households. Novi Sad is divided into 28 administrative parts, and the biggest 14 were included in the study. The total number of households asked to participate was 121 (response rate 92.56%). The researchers employed a snowball recruitment methodology. The study was revealed to different acquaintances in order to recruit first participating household in every of the 14 administrative city parts. Afterwards, the respondents were asked to recommend the next household for possible inclusion in the study through their social contact, and this was done until 8 households in every city part agreed to participate. The respondent (family member >18 years) was informed on the details of the study over a telephone conversation. When families willing to cooperate were visited, respondents provided written consent prior to data collection. Two trained interviewers conducted review and analysis of all drugs in the household (trade name, pharmaceutical formulation, expiry date, presence of secondary packaging, presence of summary of product characteristics (SPC), the number of pills in a package. For every drug item the respondents answered the following questions—an indication for which the drug is/was used, method of obtaining the drug (voluntarily purchased in a pharmacy, obtained from friends and family or issued on prescription) and whether the drug was currently being used (current use was defined as use in 10 days prior to interview). For the drugs in current use the respondents were asked whether the drug was used correctly (dosage, dosing interval and treatment duration as prescribed by a doctor or as listed in the SPC). If irregular use was reported, the following reasons were offered
-
I did not finish full treatment course because my condition has improved; due to adverse effects; it did not improve my condition; forgetfulness; other (specify).
After the interviewer recorded all drugs in the household, respondents completed the questionnaire. The questionnaire was pre-tested on a small sample of households. The first part of the questionnaire (Electronic Supplementary Material 1) (three questions) was related to socio-demographic characteristics of the household, while the second part (three questions) referred to the opinions and knowledge of the respondent regarding antibiotics. Analysis of all drugs in the household by the interviewer and completion of the questionnaire (six questions) by the respondent took up to 20 min. After the data had been collected, drugs were classified according to the Anatomical Therapeutic Chemical (ATC) Classification System (http://www.whocc.no/atc/did/index database) [13, 18].
Statistical analysis was performed with SPSS software (SPSS 15.0 for Windows, SPSS Inc., Chicago, IL, USA). Results were presented as frequency, percent, median and range. Mann–Whitney U test was used for numeric data with non-normal distribution and ordinal data. Chi square test was used to test the differences between nominal data (frequencies). Spearman correlation coefficient was computed to assess the relationship between the amount of antibiotics in households and family size, total number of drugs in households, number of acutely and chronically ill members of the household. Logistic regression was used as the method for analyzing binary outcome and potential predictors. All p values <0.05 were considered significant.
Results
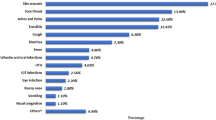
In this study we analyzed a total of 112 households, with a median of household size of 3 (range 1–7). Total number of drug items present in households was 768, 92 drugs belonged to J01 and D06 ATC group (antibiotics for systemic and for topical use) class, constituting 11.98% of the total stored medications. Median number of drugs per household was 6 (1–23). In households that had antibiotics, median number was 1 (1–6). Out of the surveyed households, 55 (49.1%) had at least one package of antibiotics stored at home (Fig. 1). Antibiotics were usually acquired with prescription (67, 72.8%). Around a quarter of antibiotics were used for self-medication—purchased at pharmacy without prescription (19, 20.65%) or obtained from friends or family (6, 6.52%). Out of all antibiotics in households, 41 (44.57%) were not in current use, and a majority of unused packages contained less than half a package and a quarter contained only 1–2 pills (Fig. 2), while 7 packages (7.61%) were expired. For the currently used antibiotics, most of the respondents reported regular use (40, 78.43%), but 8 (15.69%) reported not finishing the complete course of antibiotics because the symptoms had resolved (Fig. 3). Also, 3 (5.88%) admitted forgetting to take antibiotics during the treatment course. Secondary packaging and SPC were present in 65 (70.65%) packages. The most common dosage forms of stored antibiotics were oral solid dosage forms 78 (84.78%), followed by semisolids 10 (10.87%) and oral liquid dosage forms 4 (4.35%).
The most commonly stored antibiotics (Table 1) and the antibiotics most commonly used for self-medication (Table 2) were amoxicillin (reported indications included common cold, cough, pharyngitis and tooth-ache) and cephalexin (common cold, sore throat, cannot remember). When asked whether there were antibiotics in households, 11 of respondents (9.82%) answered incorrectly while 10 (8.92%) answered that they do not know what antibiotics were.
There was no difference in the household size [median 3, (1–7), p = 0.108] between the households that stored antibiotics and those that did not (Table 3). Antibiotics were present in the 63.1% of households with secondary education and 32.4% of households with college education, and this difference was statistically significant (p = 0.002). There was a statistically significant difference in the number of antibiotics in households with regard to the respondent education level (p = 0.002)—median number of antibiotics in households with elementary education was 0 (0–1), with secondary education 1 (0–6) and 0 (0–4) in households with college education. Households with the highest education (college education) stored less antibiotics compared to secondary school (p = 0.006) while there was no statistically significant difference compared to respondents with elementary school (p = 0.696). Presence of children younger than 12 years and health care professional in a household did not influence the amount of antibiotics stored. Presence of a family member with chronic condition negatively influenced the presence of antibiotics in a household (p = 0.02). Receiving information from a pharmacist and being familiar with the concept of antimicrobial resistance exhibited no statistically significant association with the presence of antibiotics in households. There was no statistically significant correlation between the number of antibiotics per household and household size (Rs = 0.117; p = 0.217), and number of household members with acute health condition (Rs = 0.071; p = 0.456). Overall, there was a weak, negative correlation between the number of household members with chronic health condition and the number of antibiotics in household (Rs = −0.227; p = 0.016).
Multivariate logistic regression analysis examining the predictors of storing antibiotic in the household included only predictors which were significant in a univariate logistic regression at a level of significance of 0.05. Multivariate logistic regression model included two predictors, as shown in Table 4, which were analyzed on 112 cases, 55 having the defined outcome (Table 4). The test of the full model was statistically significant (p < 0.001). There was no multi-collinearity between the predictors. Total number of drugs per household (B = 0.1180; p = 0.002) and presence of a household member with chronic condition (B = −1.122; p = 0.008) made a significant contribution to the prediction.
Discussion
Despite the efforts made to improve the control of antibiotic dispensing and use in Serbia, this still remains an important issue. Medicines and Medical Devices Agency of Serbia performs the classification of medicinal products, regulates the regime of their dispensing and publishes a list of around 300 drugs that are available OTC. Antibiotics are classified as prescription only medication which cannot be purchased without a physician’s prescription. However, there is a discrepancy between legislation and everyday practice. Despite existing legislation and stricter control starting November 2011, implementation of these regulations was not completely successful. Nowadays, although antibiotics are not easily available, it is still possible to purchase them without prescription in some local private pharmacies. A study from 2012 [6, 7] conducted in Novi Sad, revealed that 46.5% of households had at least one package of antibiotics stored at home. In the present study antibiotics were found in about 40% of households in Novi Sad which is comparable to the results of earlier research [6, 7], but the share of antibiotics in total drug inventory (10.04%) was higher than in the previous survey (7.3%) [6, 7]. The most commonly stored antibiotics in surveyed home pharmacies in Novi Sad were amoxicillin and cephalexin, similar to 2012 study [6, 7]. A study of antibiotic use in Eastern Europe also identified penicillins and first generation cephalosporins as the most commonly used antibiotics in Serbia [10].
Factors that were identified to influence the presence of antibiotics in households in the present study include the amount of total drugs stored and the chronic condition of family members. With every additional drug item in a household, chances of storing antibiotics in a household rises 20%. Households where a member has chronic condition have 70% lower chance of storing antibiotics, probably as these patients were less inclined to take antibiotics without consulting a doctor due to possible fear of interactions between antibiotics and drugs used in the treatment of chronic conditions [19]. Respondents’ education influenced the presence of antibiotics in households—fewer households with a respondent having a college degree stored antibiotics, and college education was linked to lower amount of antibiotics in households. This is in contrast to the research conducted in 2012 [7] where education did not influence the number of antibiotics in households. One of the factors reported in the literature affecting household drug storage includes the presence of health professional in the household [20]. In the present study, similar to the findings of the Croatian research [21], antibiotics were found with equal frequency in households with a healthcare professional and those without.
In Novi Sad households, half of antibiotics were not being used, suggesting that a large number of antibiotics present supplies for future use, or unused medications and leftovers from an earlier treatment [7, 22]. It is worrisome that 85% of unused antibiotic packages were opened, and 60% contained only 1–5 tablets, as this raises an issue of patient’s compliance. Studies have shown that patients often consider antibiotics as antipyretics and stop the treatment as soon as the symptoms resolve. In the present study, 39.02% of unused antibiotics contained about half a package and 12.2% were whole, unopened packages. Patients keep antibiotics as supplies for future use, leading to the problem of self-medication [7, 22, 23]. This occurrence has been confirmed by numerous studies conducted in the United States, where about 20–30% of the respondents used leftover antibiotics without consulting a doctor [21, 24].
Common sources of drugs used for self-medication include different social contacts, pharmacies and drugs stored in households [25]. In our study, self-medication with antibiotics was a direct result of the availability of antibiotics without a medical prescription in some pharmacies. Every fifth package of antibiotics was purchased without prescription in a pharmacy, while merely 5% were obtained through social contacts. Self-medication with antibiotics has declined from 32.2% in 2012 to 27.2% in the present study, but self-medication rates in Novi Sad are alarmingly high compared to neighboring countries—6% in Croatia, Slovakia and Slovenia, and only 2% in Hungary [22, 26, 27], as well as the countries of Northern and Western Europe with the frequency of self-medication with antibiotics at <3% [22, 27].
Some of the factors identified to contribute to the practice of self-medication with antibiotics in low-income countries include the cost of medical consultation, low satisfaction with medical practitioners and misconceptions regarding the efficacy of antibiotics [7, 28, 29]. Serbian healthcare system is managed by the National Health Insurance Fund, financed through compulsory contributions from the employees, which covers all citizens and permanent residents. However, despite this high coverage, in reality there are numerous obstacles in the functioning of Serbian healthcare. Certain population may not have access to treatment due to barriers such as high number of patients per one general practitioner (GP), long waiting hours necessary to reach the chosen GP who can exclusively prescribe reimbursed drugs, and low income with high cost of services in private health-care institutions [7, 29]. Thus, in current circumstances, self-medication and storage of surplus antibiotics in Serbian households could be expected, but this practice should not be encouraged as the misuse of antibiotics in the community contributes to the development of antibiotic resistance, already at alarmingly high rates in Serbia [4].
Amoxicillin and cephalexin, the most commonly prescribed antibiotics by Serbian physicians [30], were also the ones most commonly used for self-medication, therefore there is a possibility that the respondents were treated in the past with these drugs and may be using them for treating the conditions presenting with similar symptoms [31, 32]. Indications or illness for self-medication with antibiotics were typically associated with infections of the upper respiratory tract. In most cases, an indication for self-medication was adequate, but the respondents also reported using antibiotics for pain relief, cold or cough. Approximately 10% of the respondents answered incorrectly whether they have antibiotics in their households, while 10% admitted that they do not know what antibiotics were.
The study had a number of limitations. The information on patterns of use of drugs in households was self-reported, so a possibility of a recall bias cannot be ruled out. The use of non-probability sampling may have introduced a selection bias. It is important to note that conduction of the study during winter months may have influenced the results, as the seasonal variation of antibiotics consumption is well documented. The study was conducted in Novi Sad, second largest city in Serbia with high proportion of well-educated people and generalization to the population of Serbia should be done carefully. However, this approach of researching drug utilization provides the most accurate data and this study presents the most in-depth analysis of antibiotics in Serbian households up to date.
Conclusion
Results of this study clearly indicate that antibiotics are often present in households in Novi Sad and frequently used self-initially, without medical prescription. General population is considerably inclined toward self-medication with antibiotics, despite the absence of adequate knowledge about the importance of responsible antibiotic use, and the ability to select the proper indication for antibiotic use. In order to decrease self-medication practice, as well as the abuse of antibiotics to a greater extent, more stringent controls of the antibiotics dispensing are necessary.
References
De Kraker ME, Jarlier V, Monen JC, Heuer OE, Van De Sande N, Grundmann H. The changing epidemiology of bacteraemias in Europe: trends from the European Antimicrobial Resistance Surveillance System. Clin Microbiol Infect. 2013;19(9):860–8.
Goossens H, Ferech M, Vander Stichele R, Elseviers M, ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–873.
Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev. 2010;74(3):417–33.
European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe 2014. Annual report of the European Antimicrobial Resistance Surveillance Network [EARS-Net]. ECDC, Stockholm; 2015.
Bbosa GS, Mwebaza N. Global irrational antibiotics/antibacterial drugs use: a current and future health and environmental consequences. Microb Pathog Strateg Combat Them Sci Technol Educ. 2013;4(3):1645–55.
Paut Kusturica M, Tomić Z, Bukmirić Z, Horvat O, Pavlović N, Mikov M. Antibiotics in Serbian households: a source of potential health and enviromental threats. Cent Eur J Public Health. 2015;23(2):114–8.
Kusturica MP, Tomic Z, Bukumiric Z, Ninkovic L, Tomas A, Stilinovic N, et al. Home pharmacies in Serbia: an insight into self-medication practice. Int J Clin Pharm. 2015;37(2):373–8.
Cars O, Mölstad S, Melander A. Variation in antibiotic use in the European Union. Lancet. 2001;357:1851–3.
Grigoryan L, Monnet DL, Haaijer-Ruskamp FM, Bonten MJ, Lundborg S, Verheij TJ. Self-medication with antibiotics in Europe: a case for action. Curr Drug Saf. 2010;5(4):329–32.
Versporten A, Bolokhovets G, Ghazaryan L, Abilova V, Pyshnik G, Spasojevic T, et al. Antibiotic use in eastern Europe: a cross-national database study in coordination with the WHO Regional Office for Europe. Lancet. 2014;14(5):381–7.
Larson E, Lin XS, Gomez-Duarte C. Antibiotic use in hispanic households, New York City. Emerg Infect Dis. 2003;9(9):1096–102.
González J, Orero A, Prieto J. Storage of antibiotics in Spanish households. Rev Esp Quimioter. 2006;19(3):275–85.
WHO. Introduction to drug utilization research. Oslo: WHO; 2003.
Orero A, Gonzalez J, Prieto J. Antibióticos en los hogares españoles. Implicaciones médicas y socioeconómicas [Antibiotics in Spanish households. Medical and socioeconomic implications. URANO Study Group]. Med Clin (Barc) 1997;109:782–5. (in Spanish).
Ngokwey N. Home remedies and doctor’s remedies in Feira (Brasil). Soc Sci Med. 1995;40:1141–53.
Stratchounski LS, Andreeva IV, Ratchina SA, Galkin DV, Petrotchenkova NA, Demin AA, et al. The inventory of antibiotics in Russian home medicine cabinets. Clin Infect Dis. 2003;37(4):498–505.
Sawalha A. Extent of storage and wastage of antibacterial agents in Palestinian households. Pharm World Sci. 2010;32(4):530–5.
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2013. Oslo; 2012. https://www.whocc.no/filearchive/publications/1_2013guidelines.pdf. Accessed 14 Dec 2016.
De Bolle L, Mehuys E, Adriaens E, Remon JP, Van Bortel L, Christiaens T. Home medication cabinets and self-medication: a source of potential health threats? Ann Pharmacother. 2008;42(4):572–9.
Wondimu A, Molla F, Demeke B, Eticha T, Assen A, et al. Household storage of medicines and associated factors in Tigray Region, Northern Ethiopia. PLoS ONE. 2015;10(8):e0135650.
Aljinovic-Vucic V, Trkulja V, Lackovic Z. Content of home pharmacy and self-medication practices in households of pharmacy and medical students in Zagreb, Croatia: findings in 2001 with a reference to 1977. Croat Med J. 2005;46(1):74–80.
Grigoryan L, Haaijer-Rysjamp FM, Burgerhof JG, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12:452–9.
Ceaser S, Wurtz R. Leftover antibiotics in the medicine cabine. Ann Intern Med. 2000;133:74.
Richman P, Garra G, Eskin B, Nashed A, Cody R. Oral antibiotic use without consulting a physician: a survey of ED patient. Am J Emerg Med. 2001;19:57–60.
Bennadi D. Self-medication: a current challenge. J Basic Clin Pharm. 2014;5(1):19–23.
Väänänen MH, Pietilä K, Airaksinen M. Self-medication with antibiotics-does it really happen in Europe? Health Policy. 2006;77(2):166–71.
Matuz M, Benko R, Doro P, Hajdu E, Soos G. Non-prescription antibiotic use in Hungary. Pharm World Sci. 2007;29:695–8.
Saradamma RD, Higginbotham N, Nichter M. Social factors influencing the acquisition of antibiotics without prescription in Kerala State, south India. Soc Sci Med. 2000;50(6):891–903.
Jakovljevic M. Resource allocation strategies in Southeastern European health policy. Eur J Health Econ. 2013;14:153–9.
Vukmirovic S. Farmakoepidemiološki i farmakoterapijski aspekti upotrebe antibakterijskih lekova–usklađenost nacionalnih vodiča i lokalne rezistencije bakterija [Pharmacoepidemiological and pharmacotherapeutic aspects of antibacterial use—adherence to National guidelines and local resistance patterns] [dissertation]. Novi Sad (Serbia): Medical faculty of Novi Sad; 2013.
Morgan DJ, Okeke NI, Laxminarayan R, Perencevich NE, Weisenberg S. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis. 2011;11:692–701.
Grigoryan L, Burgerhof J, Haaijer-Ruskamp F, Degener J, Deschepper R, Monnet D, et al. Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrob Chemother. 2007;59(1):152–6.
Acknowledgements
We would like to thank all study participants involved in this research for giving up their time to take part in the study.
Funding
This work was supported by the Ministry of Science and Technological development, Republic of Serbia, Project No. 41012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors of this manuscript have no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tomas, A., Paut Kusturica, M., Tomić, Z. et al. Self-medication with antibiotics in Serbian households: a case for action?. Int J Clin Pharm 39, 507–513 (2017). https://doi.org/10.1007/s11096-017-0461-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-017-0461-3