Abstract
Objective and design
During peritonitis, mesothelial cells assume macrophage characteristics, expressing macrophage markers, indicating that they might differentiate into macrophage-like cells.
Materials and subjects
Twenty-five male rats were used for in vivo experiments. For in vitro experiments, a primary mesentery culture model was developed. The mesothelial cell to macrophage-like cell transition was followed by studying ED1 expression.
Treatments
In vitro primary mesenteric culture was treated with granulocyte–macrophage colony-stimulating factor (GM-CSF, 1 ng/ml). Blocking internalization of receptor–ligand complex, Dynasore (80 µM) was used. Acute peritonitis was induced by Freund’s adjuvant’s (1 ml) intraperitoneal injection.
Results
Immunohistochemistry: GM-CSF in vitro treatment resulted in a prominent ED1 expression in transformed mesothelial cells. Blocking the internalization, ED1 expression could not be detected. GM-CSF receptor (both α and β) was expressed in mesothelial cells in vitro (even if the GM-CSF was not present) and in vivo. Inflammation resulted in an increasing GM-CSF and GM-CSF-receptor level in the lysate of mesothelial cells.
Conclusions
Mesothelial cells can differentiate into macrophage-like cells, and GM-CSF, produced by the mesothelial cells, has probably an autocrine regulatory role in this transition. Our results provide new data about the plasticity of mesothelial cell and support the idea that during inflammation macrophages can derive from non-hematopoietic sources as well.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mononuclear phagocyte system (MPS) [1] comprises monocytes, macrophages and dendritic cells, as well as their bone marrow-resident progenitors [2]. Monocytes and macrophages are the major differentiated mediators of immune responses and are widely distributed in many tissues and organs. Under normal (steady-state) conditions, a large number of these phagocytic cells reside in the peritoneal cavity [3]. These resident macrophages are self-sustaining by local proliferation in the “milky spots” of the mesentery [4]. A heterogeneous population of phagocytes appear in the peritoneal cavity as a result of inflammation [5]. The origin and plasticity of these chronic inflammatory macrophages are still poorly understood. Tissue-resident macrophages as well as infiltrating monocyte-derived macrophages play a distinct role in the progression of inflammation. It cannot be excluded, however, that cells originating from non-hematopoietic sources can also contribute to this subset of macrophages.
In a previous paper [6], we have shown that injection of Freund’s adjuvant into the peritoneal cavity of rats induces sterile peritonitis, leading to a large increase in the number of peritoneal macrophages. During this inflammation, the mesothelial cells undergo a biological process known as epithelial-to-mesenchymal transition (EMT) [7]: they detach from the mesentery, lose their intercellular junctions and assume a macrophage character expressing macrophage markers (ED1, OX43, CD63). The question arises whether these macrophage-like cells, in addition to emigrating blood monocytes and resident macrophages in “milky spots”, could form the third source of peritoneal macrophages during inflammation. To elucidate this problem, an in vitro experimental model was constructed in this study in which the mesentery was isolated and kept in culture medium for several days (“primary cultures”) without any access to blood supply. The transition of mesothelial cells into macrophage-like cells was initiated by granulocyte–macrophage colony-stimulating factor (GM-CSF) treatment.
GM-CSF is a member of the hematopoietic cytokine family and promotes the survival and activation of granulocytes, macrophages and dendritic cell differentiation in vivo, but it also stimulates proliferation of several non-hematopoietic cell types (osteoblasts, smooth muscle, endothelial and epithelial cells) [8]. GM-CSF is produced by activated, but not resting T-lymphocytes [9], monocytes, fibroblasts, endothelial cells and stimulated keratinocytes [10, 11]. The cytokine was described to signal through a heterodimeric receptor having an α and a signaling β subunit [12].
In the present study, the primary culture of the mesentery provides a suitable model that preserves its normal structure for several days. It could be stimulated by GM-CSF, leading to transformation of mesothelial cells to macrophage-like cells. Receptors of GM-CSF were present in mesothelial cells both in cultured and in situ mesenteries and showed an increased expression as a result of this treatment. In an in vivo experiment, GM-CSF was highly expressed both in the mesothelial cells and the peritoneal fluid during the inflammatory process, indicating the crucial role of this cytokine in the epithelial–mesenchymal transition and recruitment of additional macrophages.
Materials and methods
Animal models
All rats were obtained from Charles River Research Models and Services, Germany, and maintained under specific pathogen-free conditions at room temperature (23 °C) and air humidity of 45 %. All rat experiments were carried out in accordance with the recommendations in the Guide for the use of Adjuvants in Research of the National Institutes of Health and approved by the Institutional Animal Care and Use Committee of the University of Massachusetts Amherst (ARAC Guidelines 2010) and Semmelweis University’s Institutional Animal Care and Use Committee. All efforts were made to minimize suffering.
In vivo experiments
To induce peritonitis, 1 ml complete Freund’s adjuvant (Sigma-Aldrich®, Saint Louis, MO, USA) was injected into the peritoneal cavity of 70- to 90-day-old male Sprague-Dawley rats (200–250 g). After 1, 3, 5, 8, and 11 days, the mesentery was isolated from the control and treated animals (n = 5, where n = number of the animals per group).
For in vitro experiments, a primary mesentery culture was developed: mesenteries were cut out from control animals and maintained in Dulbecco’s modified eagle medium (Nutrient Mixture F-12 (DMEM/F12, Life Technologies™, Paisley, UK) in humid condition at 37 °C with 5 % CO2. The tissue cultures were treated either with 1 ng/ml GM-CSF (Sigma-Aldrich®, Saint Louis, MO, USA) at 1, 2, 3, 6, 8 and 24 h. To block endocytosis, the primary mesenteric cultures were pre-treated with 80 µM Dynasore (Sigma-Aldrich®, Saint Louis, MO, USA) for 1 h, then the media were supplemented with GM-CSF and cultures were incubated for 6 and 8 h. An experiment was performed for two dishes per treatment and repeated five times.
Both in vivo and in vitro samples were fixed either in a mixture of 1 % glutaraldehyde (GA) and 1 % OsO4 in 0.1 M cacodylate buffer, pH 7.4 (1 h, on ice), or 4 % formaldehyde (FA) in 0.1 M phosphate buffer (PBS), pH 7.4 (1 h at room temperature). The GA and OsO4-fixed samples were subjected to electron microscopy (EM), while FA-fixed samples were used for immunohistochemistry.
Immunohistochemistry
The FA-fixed samples were stored in 1 % FA at 4 °C until further processing. For immunolabeling on frozen semithin sections, we applied a modified Tokuyashu technique [13]. The fixed samples were washed with 0.05 M glycine in PBS and infiltrated with 10 % gelatin at 37 °C for 30 min. The gelatin (containing the mesentery) was solidified on ice and cut into small blocks. For cryoprotection, blocks were infiltrated with 2.3 M sucrose at 4 °C, mounted onto aluminum pins and frozen in liquid nitrogen. The 0.6 µm-thick frozen sections were cut by Leica Ultracut S ultramicrotome (Vienna, Austria). The sections were mounted on microscope slides, washed with 0.02 M glycine in PBS three times for 10 min and blocked with 1 % BSA–PBS. To identify the macrophage character of the transformed cells, mouse monoclonal ED1 antibody (a generous gift from Prof. Dr. Christine Dijkstra; Dept. Molecular Cell Biology and Immunology, Vrije University, Amsterdam, The Netherlands) was applied in a dilution of 1:400, while for labeling mesothelial cells a polyclonal anti-mesothelin antibody (1:200) was used (Immuno-Biological Laboratories Co., Japan). Anti-mouse IgG Alexa Fluor 488 and anti-rabbit IgG Alexa Fluor 555 (1:200, Molecular Probes®, Leiden, The Netherlands) were applied as secondary antibodies. To detect GM-CSF receptor, a rabbit anti-GM-CSFRα antibody (1:500, GeneTex, Irvine, CA, USA) and GM-CSFRβ antibody (1:100, Bioss, Woburn, MA, USA) were used. Biotinylated anti-rabbit IgG (1:100; Vector Laboratories Inc., Burlingame, CA, USA) was applied as a secondary antibody and for immunofluorescence visualization Streptavidin-Alexa Fluor 488 (1:200, Molecular Probes®, Leiden, The Netherlands) was used. The nuclei were stained with DAPI (Vector Laboratories Inc., Burlingame, CA, USA). The visualization was performed with Zeiss LSM 780 confocal microscope. Images were performed by Adobe Photoshop 7.1.
Electron microscopy
The GA and OsO4-fixed samples were washed in 0.1 M cacodylate buffer, dehydrated with ethanol and stained with 1 % uranyl acetate in 70 % ethanol for 1 h (at room temperature) prior to araldite embedding. Semithin sections were stained with toluidine blue solution. Ultrathin sections were contrast-stained with uranyl acetate and lead citrate. The samples were analyzed in a Hitachi H-7600 (Tokyo, Japan) transmission electron microscope.
Immunoblot analysis
The peritoneal cavity was washed with PBS to remove cells attached to the surface of the mesentery and then the isolated mesentery was incubated with 0.2 % collagenase, type II (Sigma-Aldrich®, Saint Louis, MO, USA) in DMEM/F12 for 1 h in humid condition at 37 °C. The solid remnants (adipose and connective tissue) were then removed and samples were washed three times in PBS by centrifugation at 1,000 rpm, for 10 min at 4 °C. The pellets were then placed in liquid nitrogen for 30 min and stored at −80 °C until use for biochemical investigation. The isolated mesothelial cells were dissolved in lysis buffer containing 50 mM Tris–HCl, pH 7.5, 150 mM NaCl, 2 mM EDTA, 200 mM Na3VO4, 1 mM NaF, 1 % Nonidet P-40 and protease inhibitor mixture (Complete Mini, Roche, Mannheim, Germany), kept for 1 h on ice, followed by centrifugation at 12,000 rpm for 20 min at 4 °C to remove insoluble material. The supernatants were collected and the protein contents were determined by Bradford [14] assay and diluted to a concentration of 1 mg/ml. Afterward, the samples were mixed with the same amount of reducing Tris–SDS buffer (0.5 M Tris pH 6.8, 10 % glycerol, 2 % SDS, 0.00125 % bromophenol blue, 0.5 % mercaptoethanol) and boiled at 100 °C for 4 min. Cell extracts were subjected to SDS-PAGE on 10 % gels. Proteins were transferred to nitrocellulose blotting membrane (Amersham Hybond ECL, Germany) and probed with antibodies to ED1 (1:1,000), GM-CSF (1:1,000; Sigma-Aldrich®, Saint Louis, MO, USA) and GM-CSF receptor alpha (1:500; GeneTex, Irvine, CA, USA). The signal was detected with species-specific peroxidase-conjugated secondary antibodies (Amersham, GE Healthcare Biosciences, Pittsburgh, USA). The same membranes also were probed to detect β-tubulin (1:1,000; Millipore, Temecula, CA, USA) as a loading control.
Statistical analysis
Relative optical densities were measured using the ImageJ software (U.S. National Institutional of Health, Bethesda, Maryland) and the results of three independent experiments were compared and statistically analyzed. The significance was tested by the ANOVA method and Turkey’s HSD test. All data were reported as the mean ± SD.
Results
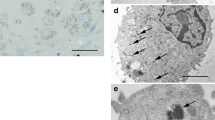
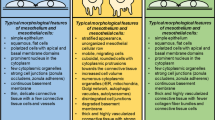
To study the effect of GM-CSF on mesothelial cells in vitro, isolated mesenteries were held in DMEM/F12 culture medium for 1, 2, 3 4, 5 and 7 days. Our light and electron microscopic studies showed that this culture medium without any supplements was sufficient to provide proper microenvironment for the mesentery in culture. Although our samples were in a good condition even on the fifth day of culturing, mesenteries kept in culture medium for 3 days were used for further experiments. The morphology of the 3-day cultured mesentery was very much similar to the non-treated in vivo samples: the mesothelial cells were flat, typical simple squamous cells, forming continuous layers completely covering both surfaces of the mesentery. The connective tissue contained only few cellular elements and collagen fibers (Fig. 1a). Cellular junctions were often seen, the basement membrane was continuous (Fig. 1b), and caveolae could be found on both the luminal (apical) and basal surfaces of the cell. Only few intracellular organelles (mitochondria, endoplasmic reticulum) and some multivesicular bodies and autophagic vacuoles were identified in the cytoplasm of these cells. When treating the primary mesenteric culture with 1 ng/ml GM-CSF (6 and 8 h), prominent changes could be detected: perinuclear areas of the mesothelial cells became more voluminous, and the amount of collagen fibers in the connective tissue significantly increased (Fig. 1c). Some of the cellular junctions had already disappeared; many cellular processes appeared on the basal surface of the cells indicating that the mesothelial cells had started to lose their polarity (Fig. 1d).
The effect of GM-CSF on primary mesenteric culture. a Light microscopic image of a 3-day-old (control) mesentery cultured in DMEM/F12 medium. The mesothelial cells are flat and show typical simple squamous epithelial morphology. They form continuous layers on both surfaces of the mesentery. Few cellular elements and collagen fibers are present in the connective tissue. b Electron microscopically, only few intracellular organelles (mitochondria, secretory granules, less developed endoplasmic reticulum, etc.) are found in the cytoplasm. The cells are connected with each other by cellular junctions (arrow); cellular processes are present only in the apical plasma membrane. c, d 6 h GM-CSF treatment resulted in remarkable changes. c The flat cells became more voluminous nd thick collagen fiber bundles are present in the connective tissue. d More mitochondria and other cellular organelles (endoplasmic reticulum, multilamellar body—MLB) appeared in the cytoplasm. Note that the cells develop many processes on their basal surface, suggesting that they lost their polarity. Bars a, c 18 µm, b 0.6 µm, d 0.9 µm
Expression of ED1 (in vitro)
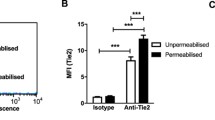
In 3-day-old mesentery cultures no ED1-positive mesothelial cells could be detected by immunohistochemistry (Fig. 2a). In contrast, 6 and 8-h GM-CSF treatment induced a well-observable expression of ED1 (a characteristic macrophage marker) in these cells (Fig. 2b, c). Alternatively, when the GM-CSF containing medium was completed with 5 nM transforming growth factor (TGF)β, a more prominent ED1 expression was found (Fig. 2d), indicating that TGFβ enhanced the effect of GM-CSF. To answer the question whether internalization has an essential role in the GM-CSF signaling driving the cell to express ED1, we used 80 µM Dynasore. Dynasore is known to block pinching off clathrin-coated vesicles, caveolae and some lipid rafts from the plasma membrane [15]. The presence of 80 µM Dynasore (before and during the whole experimental period) inhibited the ED1 expression in mesenteric mesothelial cells (Fig. 2e).
ED1 expression in mesothelial cells of primary mesenteric culture (in vitro). a No ED1 could be detected in the 3-day-old, non-treated mesothelial cells. b 6 and c 8 h GM-CSF treatment induced a significant expression of ED1. d The combined treatment with GM-CSF and TGFβ resulted in a more prominent ED1 expression, indicating that TGFβ enhanced the effect of GM-CSF. e When the culture was treated with Dynasore, GM-CSF had no effect on the ED1 expression. Bars a–e 15 µm (a red mesothelin, green ED1, blue DAPI. b–e green ED1, blue DAPI)
Expression of GM-CSF receptor α (in vitro)
To mediate the biological effect of GM-CSF, its receptor is supposed to be presented on the target’s cell membrane. Our immunohistochemical results show that the GM - CSF receptor is presented in the 3-day cultured mesenteric mesothelial cells (even if the GM-CSF was not present) (Fig. 3a). In mesenteries maintained in culture for 3 days and treated consecutively with GM-CSF for 8 h, we found a significantly increased receptor expression (Fig. 3b). A prominent labeling could be detected in the cytoplasm.
GM-CSF receptor expression on mesothelial cells of primary mesenteric culture (in vitro). a GM-CSF receptor is expressed on the plasma membrane of 3-day-old primary mesenteric mesothelial cells even if the GM-CSF was not present. b 8 h GM-CSF treatment increased the receptor expression and changed its distribution: more punctate-like structures could be seen in the cytoplasm. Bars a 20 µm, b 13 µm (green GM-CSF receptor, blue DAPI)
GM-CSF, GM-CSF-receptor and ED1 in in vivo mesentery
To detect whether mesothelial cells in vivo can produce and secrete GM - CSF into the peritoneal cavity, we used Western blot analyses in control and inflammation-induced animals. Studying the level of GM-CSF in the peritoneal wash, the maximum level of this cytokine was detected at the peak time of inflammation (5th and 8th day—Fig. 4a), indicating that mesothelial cells produce GM-CSF and contribute highly to the increased level of this cytokine. However, low levels of this hematopoietic factor were present even in healthy and regenerated conditions, suggesting that there is a steady-state level of GM-CSF in the peritoneal cavity. Checking the GM-CSF level in the mesothelial cell extract, we found that the control cells did not express GM-CSF, but the level of this cytokine considerably increased by the third and the fifth days of inflammation. As the regeneration of the mesentery had started (8th day), the amount of the GM-CSF was decreased to reach a level similar to that of the control after a few days (Fig. 4b).
Western blot analysis of GM-CSF following the time course of inflammation. a As the inflammation proceeded, the expression of this hematopoietic cytokine in the peritoneal wash showed a gradually increasing tendency with a maximum level at the fifth and eighth days. Note that there was a few amount of GM-CSF present in control (steady-state) circumstances. b We could detect an increasing level of GM-CSF expression in the mesothelial cell lysate as well, indicating that mesothelial cells produced GM-CSF during inflammation. The maximum GM-CSF expression could be detected at the peak time of inflammation (molecular weight: GM-CSF: 23 kDa, beta-tubulin: 50 kDa). Graphs relative levels of GM-CSF measured by densitometry. The asterisks show significant differences from the control group
Expression of GM-CSF receptor α and β (in vivo)
Time sequence of the GM - CSF receptor α expression was followed by Western blots of mesothelial lysates, which clearly indicated a relatively low level of GM-CSF receptor expression in control samples and a sharp rise by day 5 (maximum of inflammation) with a subsequent decrease during regeneration (Fig. 5). The receptors were localized with immunohistochemistry on frozen semithin sections. Although it is difficult to determine the precise localization of the GM-CSF receptor α and β in mesothelial cells of non-treated animals due to their highly flattened shape, our immunohistochemical confocal images suggest that both receptor subunits are presented mainly on the plasma membrane of the cells (Figs. 6a, 7a). By the third day of inflammation when the mesothelial cells become more voluminous, many small immunopositive punctate structures appeared in the cytoplasm of the mesothelial cells (Figs. 6b, 7b). At the fifth day of inflammation, the number of GM-CSF receptor-positive structures was lower in the cytoplasm, but they were increased in size (Fig. 6c).
GM-CSF receptor alpha expression (Western blot analysis). GM-CSF receptor expression significantly increased by the time of inflammation, with a maximum level at the fifth day (molecular weight: GM-CSF receptor alpha: 50 kDa, beta-tubulin: 50 kDa). Graph relative levels of GM-CSF receptor measured by densitometry. The asterisk shows significant differences from the control group
GM-CSF receptor α expression (in vivo). a GM-CSF receptor was found to be present on the plasma membrane of the control (healthy, non-inflamed) mesothelial cells. b On the third day of inflammation, when the mesothelial cells were rounded, GM-CSF receptor distribution changed: strong receptor labeling was found mainly in the cytoplasm (at this time of inflammation many cells—mainly granulocytes, mast cells, macrophages, lymphocytes, etc.—appear in the connective tissue. These cells also express the GM-CSF receptor). c On the fifth day of inflammation, large punctate-like immunopositive structures could be detected in the cytoplasm. Bars a–c 18 µm (green GM-CSF receptor α, blue DAPI)
GM-CSF receptor β expression (in vivo). a GM-CSF receptor β could be also detected on the plasma membrane of the control/non-inflamed mesothelial cells. b 3-day inflammation changed the cytoplasmic distribution of this subunit as well: similarly to the receptor α subunit, the β subunit appeared as immunopositive punctate-like structures in the cytoplasm. Bars a, b 15 µm (green GM-CSF receptor β, blue DAPI)
Expression of ED1 (in vitro)
ED1, a macrophage marker and indicator of mesothelial cell transformation, was followed by Western blots of mesothelial lysates (Fig. 8a) and with immunolocalization (Fig. 8b). While immunoblots from control animals gave a low signal for ED1, this was increased on day 3 after induction of inflammation and reached a maximal level on day 5, coinciding with the maximum of the inflammation reaction (Fig. 8a). Immunohistochemical localization of ED1on transformed mesothelial cells gave a strong signal primarily along the plasma membrane (Fig. 8b).
ED1 expression during inflammation (in vivo). a Western blot results: ED1 expression followed the time of inflammation, reached a maximum level at the fifth day (molecular weight: ED1: 90–100 kDa, beta-tubulin: 50 kDa). Graph relative levels of ED1 measured by densitometry. The asterisk shows significant differences from the control group. b Immunohistochemistry: ED1 could be detected on the mesothelial cell membrane on the third day of inflammation. Bar 14 µm (red mesothelin, green ED1, blue DAPI)
Discussion
Freund’s adjuvant injection induces acute peritonitis in rat. This inflammation results in a prominent, significant increase in the number of peritoneal macrophages. It is well known during inflammation that monocytes migrate out from the blood vessels, and macrophages resting in the “milky spots” of the peritoneum [3–5] become activated and play important role in the local defense. However, these two sources of newly appearing macrophages do not seem to explain the sharply increasing number of these cells from 105/ml in the resting peritoneal cavity to 107/ml in the inflammatory state [6]. We think a further source of this increased phagocytic cell population could be the mesenteric mesothelial cells, which were shown in our earlier work to be able to undergo EMT during inflammation. During this process, mesothelial cells can be detached from the underlying basement membrane and assume a macrophage character, both morphologically and by expressing macrophage markers [7, 16]. These results gave rise to the question whether mesenteric mesothelial cells can really differentiate into macrophage-like cells and contribute to the increase in the number of peritoneal phagocytic cells.
To answer the question, we used an in vitro system, in which there were isolated mesenteries kept in the culture medium with no access to the blood circulation. We have chosen the GM-CSF to initiate mesothelial cell transformation in vitro. GM-CSF is a member of the hematopoietic cytokine family [8], which promotes the survival and activation of granulocytes, macrophages and dendritic cell differentiation in vivo, but it also stimulates proliferation of several non-hematopoietic cell types (osteoblasts, smooth muscle, endothelial and epithelial cells [8]) as well. GM-CSF is produced by a variety of cells. The major sources of GM-CSF include activated T and B lymphocytes, monocyte/macrophages, neutrophils, and eosinophil granulocytes [17, 18]. In addition, non-hematopoietic cells, like endothelial cells, fibroblasts, epithelial cells, Paneth cells, chondrocytes and tumor cells can also produce GM-CSF [19].
In this study, transformation of mesothelial cells in vitro was followed both with light and EM as well as with immunohistochemical detection of ED1, which is a widely used macrophage marker. As a result of GM-CSF treatment, mesothelial cells lost contact with each other and with the underlying basal lamina, basal cellular processes appeared, and the cells became more voluminous. While control cells did not express ED1, 6–8 h treatment with GM-CSF resulted in an increasing ED1 expression in mesothelial cells, as seen by immunolabeling. This indicates that a 6- to 8-h stimulation of mesothelial cells by GM-CSF was sufficient to induce mesothelial cells to macrophage-like cell transformation. That GM-CSF does indeed play a major role in the transformation of mesothelium could be observed in the Freund’s adjuvant induced peritonitis of rats in a parallel experiment in this study. Western blot analysis of isolated mesothelial cells’ lysates showed the GM-CSF expression followed a time course similar to the development of the inflammation, with a maximum on day 5 (peak of the inflammatory reaction). In the peritoneal wash, Western blots of GM-CSF showed similar results, with the only difference of a low level of GM-CSF in controls and after termination of the inflammation (steady-state level). It seems that GM-CSF is not only produced by the mesothelium, but is also released (secreted) into its environment. This is in good agreement with an earlier study [20] showing that during infection and inflammation, GM-CSF secretion is significantly increased.
The biological effects of GM-CSF are mediated through binding to its cell surface receptor that is composed of a cytokine-specific α-chain and a β-chain shared with receptors for IL-3 and IL-5 and involved in signal transduction. Association of α and β subunits result in receptor activation [21]. GM-CSF receptor widely appears on hematopoietic [22] and some non-hematopoietic cells such as endothelial cells [23, 24], colon epithelial cells [25, 26], human fallopian tube epithelial cells [27], and endometrial/glandular epithelial cells [28]. Although there are no data available about the GM-CSF receptor expression in mesothelial cells, it was obvious to suppose that the receptor is also expressed in our system. When using antibody against GM-CSF receptor, we could indeed detect GM-CSF receptors in mesothelial cells both in vivo and in vitro (even if the GM-CSF was not present). It is important to note there was a striking parallelism between the time courses of GM-CSF and GM-CSF receptor expressions as observed on immunoblots in our in vivo experiment. A further temporal parallelism was also observed in the expression of the macrophage marker ED1, showing a time course peaking also on day 5. All these point to a possible, similar or interconnected control mechanism during inflammation. Regulating factors of GM-CSF expression were already described for ovarian steroids in uterine endometrium [28, 29] for tumor necrosis factor (TNF)-α and TGF-β in several cell types, including macrophages, fibroblasts and endothelial cells [8]. Similarly, in our previous paper [30], estrogen, TNFα and TGFβ levels detected in the peritoneal wash were significantly increased during inflammation (Freund’s adjuvant induced peritonitis). GM-CSF, GM-CSF receptor, estrogen, TNFα and TGFβ all seem to play important roles during peritoneal inflammation and mesothelial transformation, possibly forming a regulatory network. Further studies are needed to clarify the details and hierarchy of these control mechanisms.
The expression of GM-CSF and GM-CSF receptor in rat mesenteric mesothelial cells suggests an autocrine/paracrine role of GM-CSF in the signaling process driving to macrophage-like cell differentiation. To study whether internalization of the receptor/ligand complex is necessary for the signaling, we used 80 µM Dynasore. Dynasore is a cell-permeable small molecule inhibiting the GTP-ase activity of dynamin1 and dynamin2, and blocks the dynamin-dependent endocytosis [31–33]. Applying Dynasore in our primary mesenteric culture could completely block the action of GM-CSF on ED1 expression, indicating that internalization is crucial in GM-CSF signaling.
In conclusion, our results provide evidences that mesenteric mesothelial cells (a) express GM-CSF receptor on their plasma membrane; (b) during inflammation they synthesize and secrete GM-CSF that can stimulate both the GM-CSF receptor expression and mesothelial cell to macrophage-like cell transformation; (c) in this transformation, GM-CSF (together with its receptor and other cytokines) has a major autocrine regulatory role; (d) the receptor–ligand internalization is essential for GM-CSF signaling; (e) during inflammation, peritoneal macrophages can derive from non-hematopoietic sources as well.
References
van Furth R, Cohn ZA, Hirsch JG, Humphry JH, Spector WG, Lange-Woort HL. Mononuclear phagocytic system: new classification of macrophages, monocytes and their cell line. Bull World Health Organ. 1972;47:651–8.
Geissmann F, Manz MG, Jung S, Siewehe MH, Merad M, Ley K. Development of monocytes, macrophages and dendritic cells. Science. 2010;327:656–61.
Ginsel LA, Rijfkogel LP, Daems WT. A dual origin of macrophages? Review and hypothesis. In: Reichard S, Kojima M, editors. Macrophage biology. New York: Alan R. Liss; 1985. p. 621–49.
De Bakker JM, de Wit AW, Woelders H, Ginsel LA, Deams WT. On the origin of peritoneal resident macrophages. II. Recovery of the resident macrophage population in the peritoneal cavity and milky spots after peritoneal cell depletion. J Submicrosc Cytol. 1985;7:141–51.
Papadimitriou JM, Ashman RB. Macrophages: current view on their differentiation, structure and function. Ultrastruct Pathol. 1989;13:343–72.
Kiss AL, Kittel A. Early endocytotic steps in elicited macrophages: omega-shaped plasma membrane vesicles at their cell surface. Cell Biol Int. 1995;19:527–38.
Katz S, Balogh P, Nagy N, Kiss AL. Epithelial-to-mesenchymal transition induced by Freund’s adjuvant treatment in rat mesothelial cells: a morphological and immunocytochemical study. Pathol Oncol Res. 2012;18:641–9.
Rasko JEJ, Grough MM. Granulocyte macrophage-colony stimulating factor. In: Thompson AW, editor. Cytokine handbook. 2 ed. New York: Academic Press; 1994. p. 342–69.
Gasson JC, Weisbart RH, Kaufman SE, Clark SC, Hewich RM, Wong GG, Golde DW. Purified human GM-colony stimulating factor: direct action on neutrophils. Science. 1984;226:1339–42.
Kupper TS, Lee F, Birchall N, Clark S, Dower S. Interleukin-1 binds to specific receptors on keratinocytes and induces granulocyte/macrophage colony stimulating factor mRNA and protein. A potential autocrine role for IL-1 in epidermis. J Clin Investig. 1988;82:1787–92.
Metcalf D, Begley CG, Johnson GR, Nicola NA, Vadas MA, Lopez AF, Williamson DJ, Wong GG, Clark SC, Wang EA. Biologic properties in vitro of a recombinant human granulocyte–macrophage colony-stimulating factor. Blood. 1986;67:37–45.
Martinez-Moczygemba M, Huston DP. Biology of common beta receptor-signaling cytokines: IL-3, IL-5 and GM-CSF. J Allergy Clin Immunol. 2003;112:653–65.
Liou W, Geuze HJ, Slot JW. Improving structural integrity of cryosections for immunogold labeling. Histochem Cell Biol. 1996;106:41–58.
Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein–dye binding. Anal Biochem. 1976;72:248–54.
Fletcher SJ, Poulter NS, Haining EJ, Rappoport JZ. Clathrin-mediated endocytosis regulates occluding, and not focal adhesion, distribution during epithelial wound healing. Biol Cell. 2012;104:238–56.
Katz S, Balogh P, Kiss AL. Mesothelial cells can detach from the mesentery and differentiate into macrophage-like cells. APMIS. 2011;119:782–93.
Hamilton LA. GM-CSF in inflammation and autoimmunity. Trends Immunol. 2002;23:403–8.
Fleetwood AJ, Cook AD, Hamilton JA. Functions of granulocyte–macrophage colony-stimulating factor. Crit Rev Immunol. 2005;25:405–28.
Fukuzawa H, Sawada M, Kayahara T, Morita-Fujisawa Y, Suzuki K, Seno H, Takaishi S, Chiba T. Identification of GM-CSF in Paneth cells using single-cell RT-PCR. Biochem Biophys Res Commun. 2003;312:897–902.
Hamilton JA. Colony-stimulating factors in inflammation and autoimmunity. Nat Rev Immunol. 2008;8:533–44.
Hayashida K, Kitamura T, Gorman DM, Arai K, Yokota T, Miyajima A. Molecular cloning of a second subunit of the receptor for human granulocyte–macrophage colony-stimulating factor (GM-CSF): reconstitution of a high-affinity GM-CSF receptor. Proc Natl Acad Sci. 1990;87:9655–9.
Park LS, Friend D, Gills S, Urdal DL. Characterization of the cell surface receptor for human granulocyte/macrophage colony-stimulating factor. J Exp Med. 1986;164:251–62.
Griffin JD, Cannistra SA, Sullivan R, Demetri GD, Ernst TJ, Kanakura Y. The biology of GM-CSF: regulation of production and interaction with its receptor. Int J Cell Cloning. 1990;8:35–44.
Bussolino F, Colotta F, Bocchietto E, Guglielmetti A, Mantovani A. Recent developments in the cell biology of granulocyte–macrophage colony-stimulating factor and granulocyte colony-stimulating factor: activities on endothelial cells. Int J Clin Lab Res. 1993;23:8–12.
Panja A, Goldberg S, Eckmann L, Krishen P, Mayer L. The regulation and functional consequence of proinflammatory cytokine binding on human intestinal epithelial cells. J Immunol. 1998;161:3675–84.
Egea L, Hirata Y, Kagnoff MF. GM-CSF: a role in immune and inflammatory reactions in intestine. Expert Rev Gastroenterol Hepatol. 2010;4:723–31.
Zhao Y, Chegini N. Human fallopian tube expresses granulocyte–macrophage colony stimulating factor (GM-CSF) and GM-CSF alpha and beta receptors and contain the immunoreactive GM-CSF protein. J Clin Endocrinol Metab. 1994;79:662–5.
Zhao Y, Chegini N. The expression of granulocyte macrophage-colony stimulating factor (GM-CSF) and receptors in human endometrium. Am J Reprod Immunol. 1999;42:303–11.
Robertson SA, Seamark RF, Guilbert LJ, Wegmann TG. The role of cytokines in gestation. Crit Rev Immunol. 1994;14:239–92.
Balogh P, Szabó A, Katz S, Likó I, Patócs A, Kiss AL. Estrogen receptor alpha is expressed in mesenteric mesothelial cells and is internalized in caveolae upon Freund’s adjuvant treatment. PLoS One. 2013;8. doi:10.1371/journal.pone.0079508.
Corda D, Hidalgo Carcedo C, Bonazzi M, Luini A, Spano S. Molecular aspects of membrane fission in the secretory pathway. Cell Mol Life Sci. 2002;59:1819–32.
Nichols B. Caveosomes and endocytosis of lipid rafts. J Cell Sci. 2003;116:4707–14.
Takei K, Yoshida Y, Yamada H. Regulatory mechanisms of dynamin-dependent endocytosis. J Biochem. 2005;137:243–7.
Acknowledgments
We would like to express our thankfulness to Professor Pál Röhlich for the precious comments and accurate language correction of the manuscript. Our special thanks go to Katalin Lőcsey for her valuable technical help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Responsible Editor: John Di Battista.
Rights and permissions
About this article
Cite this article
Katz, S., Zsiros, V., Dóczi, N. et al. GM-CSF and GM-CSF receptor have regulatory role in transforming rat mesenteric mesothelial cells into macrophage-like cells. Inflamm. Res. 65, 827–836 (2016). https://doi.org/10.1007/s00011-016-0967-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-016-0967-5