Abstract
Introduction
Serum amyloid A (SAA), secreted group IIA phospholipase A2 (sPLA2-IIA), and C-reactive protein (CRP) are acute-phase proteins whose serum concentrations increase not only during inflammatory disorders, but also in the course of malignant diseases.
Materials and methods
In this study we analyzed serum levels of these inflammatory markers along with prostate-specific antigens (PSA) in patients with benign prostatic hyperplasia (BPH, n = 55), localized prostate cancers (PCa, n = 55), and metastatic prostate cancers (mPCa, n = 27) using immunological assays.
Results
We found that in comparison to healthy individuals (n = 55), patients with BPH, PCa and mPCa have elevated serum levels of SAA, sPLA2-IIA, and CRP, in addition to elevated levels of PSA. Significant differences with respect to inflammatory biomarkers were found between localized and metastatic PCa (p < 0.001), suggesting a prognostic value of these parameters. In addition, serum concentrations of SAA and sPLA2-IIA positively correlate with CRP in BPH patients (p < 0.05) and in patients with PCa and mPCa (p < 0.001), but not with PSA levels, Gleason score, or tumor stage, emphasizing a role of SAA and sPLA2-IIA as circulating biomarkers of inflammation rather than of neoplastic transformation. In contrast to PSA, which differed significantly between BPH and localized PCa patients (p < 0.01), such a difference was not found for SAA, sPLA2-IIA, and CRP. In order to elucidate whether the elevated levels of SAA and sPLA2-IIA can be caused by cancer cell-associated synthesis, in vitro studies were performed. These analyses demonstrated the expression of SAA and sPLA2-IIA in LNCaP and PC-3 prostate cell lines, which can be further upregulated by pro-inflammatory cytokines in a cell type-dependent manner. This might suggest that, in addition to the hepatic origin, SAA and sPLA2-IIA can also be synthesized and secreted by prostatic cancer tissue itself.
Conclusion
The results of the present study emphasize the utility of SAA, sPLA2-IIA, and CRP as circulating biomarkers of inflammation during BPH development and PCa progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) remains one of the most common forms of cancer affecting men today. In Europe, 382,000 new PCa cases were diagnosed and almost 90,000 patients died from the disease in 2008 [1]. Additionally, benign prostatic hyperplasia (BPH) is a frequent benign neoplasm affecting 50–80 % of the aged male population [2, 3]. To date, prostate-specific antigen (PSA) is the best serum marker of malignant prostatic disease that has a strong predictive value. However, there is a need for additional biomarkers because of the limited diagnostic specificity of PSA that can distinguish between BPH, prostatitis, and early stages of PCa [4–6].
Up-regulation of acute-phase proteins such as C-reactive protein (CRP), secreted group IIA phospholipase A2 (sPLA2-IIA) and serum amyloid A (SAA) is a hallmark of systemic inflammation [7–9]. A growing body of evidence suggests an important role of chronic inflammation caused by bacterial infections, urine reflux, dietary factors, hormones, and autoimmune response in the development and progression of benign and malignant prostatic disorders [3, 10–12]. As such, serum concentrations of CRP tend to be higher in patients with cancer than in healthy individuals [13–16]. The impact of CRP as an additional predictor of survival and post-treatment monitoring tool was shown in multiple myeloma, melanoma, lymphoma, ovarian, renal, pancreatic, prostatic and gastrointestinal tumors [14, 17, 18]. Furthermore, serum and intratumoral tissue levels of CRP were considered as a prognostic biomarker for androgen-independent and advanced PCa [12, 16, 18].
Serum levels of sPLA2-IIA were shown to be markedly elevated not only during inflammatory disorders, but also in malignant diseases [9, 19, 20]. However, the prognostic value of sPLA2-IIA is somewhat controversial. On the one hand, numerous studies reported that sPLA2-IIA is strongly upregulated in PCa specimens and PCa-derived cell lines [20–25]. On the other hand, a previous study revealed that serum levels of sPLA2-IIA are similarly elevated in BPH and PCa patients, suggesting that increased serum levels of sPLA2-IIA are not cancer-specific [26].
In comparison to CRP, SAA was found to be more sensitive for the diagnosis of advanced cancer and may be helpful for monitoring tumor progression [27–30]. In the phase of PCa progression, levels of SAA increased up to 500-fold with a decrease towards the normal range in the phase of remission [31].
In order to evaluate the potential of the inflammatory biomarkers for diagnosis and discrimination between different types and stages of prostatic disease, the current study analyzed serum levels of SAA, CRP, sPLA2-IIA, and PSA in patients with BPH, localized (PCa), and metastatic PCa (mPCa). The levels of biomarkers were studied with respect to their diagnostic performances using receiver operating characteristic (ROC) analysis. To answer the question of whether acute phase proteins are also synthesized in addition to hepatocytes in cancer cells, in vitro studies were performed analyzing the expression of SAA in comparison to sPLA2-IIA in LNCaP, PC-3 and DU-145 prostate cancer cell lines.
Experimental section
Patients
A total of 117 serum samples originated from four study groups: healthy individuals (n = 30), patients with BPH (n = 30), localized PCa (n = 30) and metastasized PCa (n = 27). To increase the patient sample size for valid statistical analyses, values of PSA, sPLA2-IIA and CRP from 25 healthy individuals, 25 BPH patients and 25 PCa patients, which were measured and described previously [26], were additionally included in this study (Table 1). Among the 55 patients with localized PCa, 34 patients had organ-confined (pT2) tumors and 21 patients had non-organ confined (pT3/4) tumors. The study was approved by the Institutional Review Board.
Cell culture and incubations
The PCa cell lines LNCaP, PC-3, and DU-145 were purchased from the German Collection of Microorganisms and Cell Cultures (Braunschweig, Germany) and cultured as described previously [25]. For cytokine stimulation, PCa cells were seeded into a 24-well plate at a density of 2 × 104 cells per well. After reaching 80 % confluence, cells were used for cytokine treatment. Cells were cultured in medium in the presence or absence of IFN-γ, IL-1β, IL-6 or TNF-α at a final concentration of 25 ng/mL for 24 h. In the case of combined treatment with IL-1β and IL-6, both cytokines were used at a final concentration of 12.5 ng/mL.
CRP, SAA and PSA assays
Serum levels of CRP and PSA were measured using a turbidimetric method of agglutinated antigen–antibody complexes (Roche Diagnostics, Mannheim, Germany, and ARCHITECT total PSA, Abbott, Wiesbaden, Germany, respectively). SAA was measured using enhanced nephelometric latex SAA assay on Behring Nephelometer II analyzer (Dade Behring Diagnostics, NY, USA).
ELISA-based measurement of serum sPLA2-IIA
Serum concentrations of sPLA2-IIA were measured using an sPLA2-IIA-specific ELISA kit (Cayman Chemical, MI, USA) according to the manufacturer’s protocol. Prior to analysis, all serum samples were diluted 10-fold. Absorbance of reaction products was measured at 405 nm on a Victor3 1420 Multilabel Counter reader (Perkin-Elmer LAS GmbH, Germany). Concentrations of sPLA2-IIA were calculated using standards included in the ELISA kit and software supplied with Victor3.
RNA extraction and RT-quantitative PCR analysis
RNA was isolated after lysis of cells in TRI reagent (Sigma-Aldrich, Deisenhofen, Germany) according to the manufacturer’s instructions. Isolated RNA was converted to cDNA using the GeneAmp RNA-PCR kit (PerkinElmer LAS GmbH, Juegesheim, Germany). Portions of cDNA were then amplified using quantitative PCR on the Rotor-Gene Q in combination with QuantiTect SYBR Green RT-PCR kit (Qiagen, Hilden, Germany). The housekeeping gene products TATA box binding protein (TBP) and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) were used as internal controls for SAA and sPLA2-IIA measurements, respectively. Levels of mRNA were quantified using Rotor-Gene series software v1.7 (Qiagen) and values were expressed relative to the respective housekeeping gene. The used primer pairs were 5′-GTG ATC ATG ATC TTT GGC CTA CTG CA-3′ and 5′-TCT CCC TCG TGG GGA GCA ACG ACT-3′ for sPLA2-IIA, yielding PCR products with a length of 411 bp [25]; 5′-CGG GAC ATG TGG AGA GCC T-3′ and 5′-CGA GCA TGG AAG TAT TTG TCT G-3′ for SAA (SAA1 + SAA2) amplifying products with a length of 74 bp [32]; 5′-GAA TAT AAT CCC AAG CGG TTT G-3′ and 5′-ACT TCA CAT CAC AGC TCC CC-3′ for TBP amplifying products with a length of 226 bp [33]; and 5′-CGG AGT CAA CGG ATT TGG TCG TAT TG-3′ and 5′-GCA GGA GGC ATT GCT GAT GAT CTT G-3′ for GAPDH amplifying products with a length of 439 bp [25]. Primers were applied at a final concentration of 0.8 μM. Cycling conditions involved 3 min at 95 °C followed by 40 cycles of 1 min at 95 °C, 1 min at 55 °C and 2 min at 72 °C. Each RT-qPCR was performed at least twice.
Statistical analyses
The diagnostic performance of PSA, CRP, sPLA2-IIA, and SAA was assessed with ROC curves. ROC curves were constructed to analyze the performance of biomarkers to discriminate between different groups of patients. Areas under curves (AUC) as a measure of performance and other related characteristics were determined using SigmaPlot 11.2 (Systat Software GmbH, Erkrath, Germany).
The differences between two groups were analyzed with a Mann–Whitney rank sum test and among all studied groups with the Kruskal–Wallis one-way analysis of variance on ranks method. Correlations between different pairs of variables were studied with the Pearson correlation test. All statistical analyses were performed using the statistics module integrated into SigmaPlot 11.2 software.
Results
Levels of serum biomarkers in healthy individuals and in patients with prostatic diseases
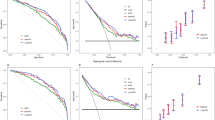
Serum concentrations of PSA, SAA, CRP, and sPLA2-IIA were significantly increased in PCa relative to healthy individuals, with the highest levels observed in the mPCa group (p < 0.001, Fig. 1). In contrast to PSA serum levels, which differed significantly between the patients with BPH and PCa (p < 0.001), such a difference was not detected in terms of SAA, sPLA2-IIA, and CRP serum levels. However, there were significant differences between the PCa and mPCa groups for all inflammatory biomarkers (p < 0.001, Fig. 1).
Box-plots of serum levels of SAA (a), sPLA2-IIA (b), CRP (c), and PSA (d) of healthy individuals (N), patients with BPH (B), and patients with localized (pT2 and pT3/4) and metastatic prostate cancers (M). Groups with tumor stages pT2 and pT3/4 are shown as T2 and 3/4. Boxes within the plots represent the 25–75th percentiles. Median values are depicted as solid lines. Circles indicate outlier values outside of the 10th and 90th percentiles. Statistical differences were calculated with the Mann–Whitney rank sum test
Furthermore, only PSA levels were able to discriminate between PCa patients with organ-confined (pT2, n = 34) and non-organ confined PCa (pT3/4, n = 21, p < 0.05), whereas SAA, sPLA2-IIA, and CRP levels were unable to differentiate between both groups (Fig. 2). In contrast, all analyzed biomarkers exhibited the highest levels in the mPCa group and differed significantly from those found in the pT3/4, pT2, and control groups (p < 0.001).
Receiver-operating characteristic (ROC) curves constructed from serum levels of PSA, sPLA2-IIA, CRP and SAA of healthy individuals and patients with BPH and PCa. N healthy controls, BPH patients with benign prostatic hyperplasia, PCa patients with localized prostate cancer, mPCa patients with metastasizing prostate cancer
Pearson correlation tests revealed significant correlations between SAA and CRP and between sPLA2-IIA and CRP in the groups of patients with BPH (p < 0.05), localized PCa (p < 0.001), and mPCa (p < 0.001), respectively (Table 2). Furthermore, a correlation was detectable between SAA and sPLA2-IIA in the case of mPCa (p < 0.05). No correlations were observed between the inflammatory biomarkers and PSA or Gleason score in the group of mPCa, as well as in other groups of prostate disease patients (Table 2).
Receiver operating characteristic (ROC) analysis of biomarker assays
In view of the identified correlations between PCa stages and serum levels of the inflammatory biomarkers, a parametric ROC analysis was performed. In this context, AUC values, 95 % confidence interval (95 % CI), sensitivity and specificity computed for optimum cut-off values were determined (Fig. 2). The performance of inflammatory biomarker assays was compared with the PSA tests as the ‘gold standard’ for the detection of PCa and discrimination between the different patient groups.
ROC analysis showed that AUC values for PSA were superior by comparison of the healthy control group vs. the groups of PCa and mPCa (AUC 0.99 and 1.00, respectively), BPH vs PCa (AUC 0.87), and PCa vs mPCa (AUC 0.99, Fig. 2; Table 3). Neither SAA nor sPLA2-IIA and CRP distinguished between groups of patients with BPH and PCa (Fig. 2; Table 3). ROC analyses revealed that in these cases the AUC values for SAA, sPLA2-IIA, and CRP were close to 0.5 with p values >0.05, indicating that inflammatory biomarkers are unable to discriminate between BPH and PCa groups (Table 3). However, the diagnostic accuracies of CRP (AUC 0.86) and SAA (AUC 0.84) were distinctly higher relative to PSA (AUC 0.81) for the discrimination between controls and patients with BPH by these inflammatory biomarkers. Moreover, a high accuracy was observed for the differentiation between controls and PCa patients in cases of SAA, sPLA2-IIA and CPP levels (AUC 0.84, 0.77 and 0.83, respectively), for the differentiation between controls and mPCa patients (AUC 0.98, 0.95 and 0.99, respectively) and between PCa and mPCa patients (AUC: 0.86, 0.86 and 0.93, respectively).
Effects of pro-inflammatory cytokines on SAA and sPLA2-IIA expressions in prostate cancer cell lines
The basal expression of sPLA2-IIA was about 60-fold higher in LNCaP cells in comparison to that found in PC-3 cells (Fig. 3). In DU-145 cells no sPLA2-IIA transcripts were detectable using RT-qPCR under basal conditions and after incubation with the analyzed cytokines. Exposure of LNCaP cells to IL-1β or IL-6 alone and in combination with IL-1β increased the expression of sPLA2-IIA by 3.0-, 1.6- and 5.4-fold, respectively (Fig. 3). Incubation with TNF-α and IFN-γ led to 2.7- and 10.0-fold higher levels of sPLA2-IIA-specific transcripts in LNCaP and PC-3 cells, respectively.
Effects of pro-inflammatory cytokines on sPLA2-IIA expression in the PCa cell lines LNCaP and PC-3. Expression of sPLA2-IIA was determined using RT-qPCR. Cells were incubated with IFN-γ, IL-1β, IL-6, or TNF-α (all at a final concentration of 25 ng/mL) or with IL-1β and IL-6 (each at a final concentration of 12.5 ng/mL, respectively) for 24 h. Data bars represent the expression levels of sPLA2-IIA determined by comparative quantification relative to the housekeeping gene GAPDH. Results are presented as mean ± SD. Analyses were performed in triplicate and graphics are representative of two experiments with similar results
In contrast to sPLA2-IIA, the basal expression of SAA was comparable between all the analyzed PCa cell lines. IL-1β, IL-6, and TNF-α induced further SAA expression in a similar way as observed for sPLA2-IIA in LNCaP cells. However, the degree of SAA induction was remarkably higher with almost 100- and 1,000-fold induction of SAA by IL-1β alone and together with IL-6, respectively. In contrast to sPLA2-IIA expression, which was completely absent in DU-145 cells, the SAA expression was induced through IL-1β by 60-fold in this cell line. In PC-3 cells, treatment with TNF-α resulted in 54-fold higher SAA-mRNA levels (Fig. 4).
Effects of pro-inflammatory cytokines on serum amyloid A (SAA) expression in the PCa cell lines LNCaP, DU-145, and PC-3. Expression of SAA was determined using RT-qPCR. Cells were incubated with cytokines as described in Fig. 3. Data bars represent the expression levels of SAA determined by comparative quantification relative to the housekeeping gene TBP. Results are presented as mean ± SD. Analyses were performed in triplicate and graphics are representative of two experiments with similar results
Discussion
The present study shows that, in addition to elevated PSA levels, patients with prostatic diseases have increased serum concentrations of SAA, sPLA2-II, and CRP and significant differences were found between localized and metastatic PCa. This suggests a prognostic value of these inflammatory biomarkers for PCa progression. Furthermore, SAA, sPLA2-II, and CRP levels were significantly different between healthy individuals and BPH patients, indicating that inflammatory biomarkers can be informative concerning the early diagnosis of BPH development.
However, no discrimination between BPH and localized PCa was achieved with SAA, sPLA2-IIA, and CRP. Furthermore, serum concentrations of SAA and sPLA2-IIA positively correlated with CRP, but not with PSA levels, Gleason score, and tumor stage emphasizing a role of SAA and sPLA2-IIA as circulating biomarkers of inflammation rather than of neoplastic transformation. This conclusion is consistent with a previous study demonstrating a significant difference of serum sPLA2-IIA levels between healthy individuals and patients with BPH and PCa patients, but not between patients with BPH and PCa [26].
In contrast to BPH or localized PCa, patients with metastases had markedly higher concentrations of SAA, sPLA2-IIA, and CRP. According to ROC analyses of metastatic vs. localized PCa groups and metastatic PCa vs. healthy individual groups, the AUC scores were near 0.9 and 1.0, respectively, emphasizing a high discrimination capability of inflammatory biomarkers. Therefore, in addition to PSA, SAA, sPLA2-IIA, and CRP may be useful candidate biomarkers for the staging and prognosis of prostate cancers. This conclusion agrees with studies that considered these biomarkers separately [14, 31, 34, 35]. For instance, high plasma levels of sPLA2-IIA were reported to be significantly associated with high Gleason scores relative to intermediate Gleason score-PCa and advanced relative to indolent cancers with AUC values 0.73 and 0.74, respectively [34].
In addition, the current study underscores the crucial role of inflammation as a decisive force at different stages of tumor development, which agrees with previous reports (for review [36, 37]). In the case of prostatic diseases, inflammation was shown to be involved in the pathogenesis and progression of both BPH and PCa [11, 12]. The acute phase reactants analyzed here are thought to be derived mainly from the liver [7, 38]. A convincing case report of a patient with massive epithelioid hemangioendothelioma was described indicating a hepatic origin of serum sPLA2-IIA. After liver transplantation a dramatic fall of sPLA2-IIA levels from 830 to 33 μg/L on the first post-transplantation day was observed. Moreover, synthesis of sPLA2-IIA was detected in hepatocytes in non-neoplastic areas of the liver, but not in areas containing tumor cells [39].
Despite the hepatic origin, an extra-hepatic and tumor-associated expression of sPLA2-IIA was described in a number of different cancers such as those of the esophagus, pancreas, gallbladder, breast, colon, and prostate [20, 22, 23, 40–42]. The expression of sPLA2-IIA was elevated in primary gastric, colon, and early-stage PCa, but not in metastatic and late-stage tumors [43, 44]. In concordance with this observation, we previously showed a markedly upregulated expression of sPLA2-IIA in LNCaP cells [25]. In contrast, a completely absent expression of sPLA2-IIA due to epigenetic mechanisms was shown in DU-145 cells originating from a brain metastasis, and a low expression of sPLA2-IIA was shown in PC-3 cells originating from a bone metastasis. Both cell lines are androgen-independent in contrast to the androgen-dependent LNCaP cell line. A similar loss of sPLA2-IIA expression due to epigenetic silencing was demonstrated in gastric tumors [43].
In addition to sPLA2-IIA, an endogenous expression of SAA in all analyzed PCa cell lines was shown in this study, which can be further induced by pro-inflammatory cytokines such as IL-1β, IL-6 and TNF-α in a cell type-dependent manner. A strong synergistic effect was observed after simultaneous treatment with IL-1β and IL-6 in LNCaP cells, which resulted in a nearly 1,000-fold increase of SAA expression. Although a similar synergistic effect on sPLA2-IIA expression in LNCaP cells was seen with IL-1β and IL-6 treatment, the extent of induction was remarkably lower (about sixfold increase) when compared with the effect on SAA expression in the same cell line. The different degree of inducing effects of these cytokines on SAA and sPLA2-IIA expression may resemble the different magnitudes of SAA and sPLA2-IIA concentrations in serum samples of PCa patients. These data suggest that tumoral expression of SAA and sPLA2-IIA may be responsible, at least in part, for the elevated serum levels in PCa patients.
Functions and clinical significance of tumoral expression of acute phase reactants are still unclear. In the case of sPLA2-IIA, opposite effects on tumorigenesis were described. On the one hand, sPLA2-IIA may induce cellular senescence [45] and inhibit cancer cell invasion [43]. In this way, sPLA2-IIA could act rather as a tumor-suppressor and may explain the observation of decreased enzyme expression in metastatic and late-stage tumors [46]. On the other hand, studies demonstrated that sPLA2-IIA can exert pro-oncogenic effects mediated by eicosanoid production in cyclooxygenase- and lipoxygenase-dependent pathways and by anti-apoptotic signaling pathways including activation of ERK, PI3-kinase, protein kinase C, and NF-κB [47–51]. A knockdown or pharmacological inhibition of sPLA2-IIA suppressed lung cancer cell growth in vitro and in vivo through NF-κB activation [51, 52]. Similar local effects on cancer progression through NF-κB activation were described for CRP and SAA [18, 53].
In conclusion, this study demonstrated significantly increased serum levels of SAA, sPLA2-IIA, and CRP in patients with BPH, localized and metastasized PCa, in comparison to healthy individuals. In addition to PSA, inflammatory biomarkers may help to discriminate between healthy individuals and patients with BPH and may prove to have prognostic value, as these biomarkers significantly distinguished between PCa patients with and without metastases. On the basis of these data it will be interesting to elucidate whether serum levels of acute phase proteins are suitable for therapeutic monitoring of patients with prostatic diseases such as BPH and PCa.
Abbreviations
- AUC:
-
Area under curve
- BPH:
-
Benign prostatic hyperplasia
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- ELISA:
-
Enzyme-linked immunosorbent assay
- GAPDH:
-
Glyceraldehyde 3-phosphate dehydrogenase
- GS:
-
Gleason score
- PCa:
-
Localized prostate cancer
- mPCa:
-
Metastatic prostate cancer
- PSA:
-
Prostate-specific antigen
- pT2:
-
Organ-confined tumors
- pT3/4:
-
Non-organ confined tumors
- ROC:
-
Receiver operating characteristic
- SAA:
-
Serum amyloid A
- SEM:
-
Standard error of the mean
- sPLA2-IIA:
-
Secreted phospholipase A2 of group IIA
- TBP:
-
TATA box binding protein (TBP)
References
Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46:765–81.
McDowell ME, Occhipinti S, Gardiner RA, Baade PD, Steginga SK. A review of prostate-specific antigen screening prevalence and risk perceptions for first-degree relatives of men with prostate cancer. Eur J Cancer Care (Engl). 2009;18:545–55.
Fibbi B, Penna G, Morelli A, Adorini L, Maggi M. Chronic inflammation in the pathogenesis of benign prostatic hyperplasia. Int J Androl. 2010;33:475–88.
Greene KL, Albertsen PC, Babaian RJ, Carter HB, Gann PH, Han M, Kuban DA, Sartor AO, Stanford JL, Zietman A, Carroll P. Prostate specific antigen best practice statement: 2009 update. J Urol. 2013;189(Suppl 1):S2–11.
Artibani W. Landmarks in prostate cancer diagnosis: the biomarkers. BJU Int. 2012;110(Suppl 1):8–13.
Schröder FH. Landmarks in prostate cancer screening. BJU Int. 2012;110(Suppl 1):3–7.
Bode JG, Albrecht U, Häussinger D, Heinrich PC, Schaper F. Hepatic acute phase proteins - Regulation by IL-6- and IL-1-type cytokines involving STAT3 and its crosstalk with NF-κB-dependent signaling. Eur J Cell Biol. 2012;91:496–505.
Kanoh Y, Ohtani H, Egawa S, Baba S, Akahoshi T. Levels of acute inflammatory biomarkers in advanced prostate cancer patients with α2-macroglobulin deficiency. Int J Oncol. 2011;39:1553–8.
Menschikowski M, Hagelgans A, Siegert G. Secretory phospholipase A2 of group IIA: is it an offensive or a defensive player during atherosclerosis and other inflammatory diseases? Prostaglandins Other Lipid Mediat. 2006;79:1–33.
De Marzo AM, Platz EA, Sutcliffe S, Xu J, Gronberg H, Drake CG, Nakai Y, Isaacs WB, Nelson WG. Inflammation in prostate carcinogenesis. Nat Rev Cancer. 2007;7:256–69.
De Nunzio C, Kramer G, Marberger M, Montironi R, Nelson W, Schröder F, Sciarra A, Tubaro A. The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur Urol. 2011;60:106–17.
Schenk JM, Kristal AR, Neuhouser ML, Tangen CM, White E, Lin DW, Kratz M, Thompson IM. Biomarkers of systemic inflammation and risk of incident, symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. Am J Epidemiol. 2010;171:571–82.
Heikkilä K, Ebrahim S, Lawlor DA. Systematic review of the association between circulating interleukin-6 (IL-6) and cancer. Eur J Cancer. 2008;44:937–45.
Lehrer S, Diamond EJ, Mamkine B, Droller MJ, Stone NN, Stock RG. C-reactive protein is significantly associated with prostate-specific antigen and metastatic disease in prostate cancer. BJU Inter. 2005;95:961–2.
Heikkilä K, Harris R, Lowe G, Rumley A, Yarnell J, Gallacher J, Ben-Shlomo Y, Ebrahim S, Lawlor DA. Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a metaanalysis. Cancer Causes Control. 2009;20:15–26.
Beer TM, Lalani AS, Lee S, Mori M, Eilers KM, Curd JG, Henner WD, Ryan CW, Venner P, Ruether JD, Chi KN. C-reactive protein as a prognostic marker for men with androgen-independent prostate cancer: results from the ASCENT trial. Cancer. 2008;112:2377–83.
Mahmoud FA, Rivera NI. The role of C-reactive protein as a prognostic indicator in advanced cancer. Curr Oncol Rep. 2002;4:250–5.
McCall P, Catlow J, McArdle PA, McMillan DC, Edwards J. Tumoral C-reactive protein and nuclear factor kappa-B expression are associated with clinical outcome in patients with prostate cancer. Cancer Biomark. 2011;10:91–9.
Triggiani M, Granata F, Giannattasio G, Marone G. Secretory phospholipases A2 in inflammatory and allergic diseases: not just enzymes. J Allergy Clin Immunol. 2005;116:1000–6.
Scott KF, Sajinovic M, Hein J, Nixdorf S, Galettis P, Liauw W, de Souza P, Dong Q, Graham GG, Russell PJ. Emerging roles for phospholipase A2 enzymes in cancer. Biochimie. 2010;92:601–10.
Nagy B, Szendroi A, Romics I. Overexpression of CD24, c-myc and phospholipase 2A in prostate cancer tissue samples obtained by needle biopsy. Pathol Oncol Res. 2009;15:279–83.
Kallajoki M, Alanen KA, Nevalainen M, Nevalainen TJ. Group II phospholipase A2 in human male reproductive organs and genital tumors. Prostate. 1998;35:263–72.
Graff JR, Konicek BW, Deddens JA, Chedid M, Hurst BM, Colligan B, Neubauer BL, Carter HW, Carter JH. Expression of group IIa secretory phospholipase A2 increases with prostate tumor grade. Clin Cancer Res. 2001;7:3857–61.
Kojima S, Mulholland DJ, Ettinger S, Fazli L, Nelson CC, Gleave ME. Differential regulation of IGFBP-3 by the androgen receptor in the lineage-related androgen-dependent LNCaP and androgen-independent C4-2 prostate cancer models. Prostate. 2006;66:971–86.
Menschikowski M, Hagelgans A, Gussakovsky E, Kostka H, Paley EL, Siegert G. Differential expression of secretory phospholipases A2 in normal and malignant prostate cell lines: regulation by cytokines, cell signaling pathways, and epigenetic mechanisms. Neoplasia. 2008;10:279–86.
Menschikowski M, Hagelgans A, Fuessel S, Mareninova OA, Neumeister V, Wirth MP, Siegert G. Serum levels of secreted group IIA phospholipase A2 in benign prostatic hyperplasia and prostate cancer: a biomarker for inflammation or neoplasia? Inflammation. 2012;35:1113–8.
Fischer K, Theil G, Hoda R, Fornara P. Serum amyloid a: a biomarker for renal cancer. Anticancer Res. 2012;32:1801–4.
Liu DH, Wang XM, Zhang LJ, Dai SW, Liu LY, Liu JF, Wu SS, Yang SY, Fu S, Xiao XY, He DC. Serum amyloid A protein: a potential biomarker correlated with clinical stage of lung cancer. Biomed Environ Sci. 2007;20:33–40.
Howard BA, Wang MZ, Campa MJ, Corro C, Fitzgerald MC, Patz EF Jr. Identification and validation of a potential lung cancer serum biomarker detected by matrix-assisted laser desorption/ionization-time of flight spectra analysis. Proteomics. 2003;3:1720–4.
Vlasova MA, Moshkovskii SA. Molecular interactions of acute phase serum amyloid A: possible involvement in carcinogenesis. Biochemistry (Mosc). 2006;71:1051–9.
Kaneti J, Winikoff Y, Zimlichman S, Shainkin-Kestenbaum R. Importance of serum amyloid A (SAA) level in monitoring disease activity and response to therapy in patients with prostate cancer. Urol Res. 1984;12:239–41.
Poitou C, Divoux A, Faty A, Tordjman J, Hugol D, Aissat A, Keophiphath M, Henegar C, Commans S, Clément K. Role of serum amyloid A in adipocyte-macrophage cross talk and adipocyte cholesterol efflux. J Clin Endocrinol Metab. 2009;94:1810–7.
Schmidt U, Fuessel S, Koch R, Baretton GB, Lohse A, Tomasetti S, Unversucht S, Froehner M, Wirth MP, Meye A. Quantitative multi-gene expression profiling of primary prostate cancer. Prostate. 2006;66:1521–34.
Oleksowicz L, Liu Y, Bracken RB, Gaitonde K, Burke B, Succop P, Levin L, Dong Z, Lu S. Secretory phospholipase A2-IIa is a target gene of the HER/HER2-elicited pathway and a potential plasma biomarker for poor prognosis of prostate cancer. Prostate. 2012;72:1140–9.
Dong Z, Liu Y, Scott KF, Levin L, Gaitonde K, Bracken RB, Burke B, Zhai QJ, Wang J, Oleksowicz L, Lu S. Secretory phospholipase A2-IIa is involved in prostate cancer progression and may potentially serve as a biomarker for prostate cancer. Carcinogenesis. 2010;31:1948–55.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–99.
Diamandis EP. Proteomic patterns in serum for early cancer diagnosis: drawing attention to potential problems. J Natl Cancer Inst (Bethesda). 2004;96:353–6.
Nevalainen TJ, Kallajoki M, Pesonen E, Andersson S, Kärkkäinen P, Höckerstedt K. Origin of circulating group II phospholipase A2 in hepatocytes in a patient with epithelioid hemangioendothelioma of the liver. Lab Invest. 1996;74:585–91.
Laye JP, Gill JH. Phospholipase A2 expression in tumors: a target for therapeutic intervention? Drug Dis Today. 2003;8:710–6.
Yamashita S, Yamashita J, Sakamoto K, Inada K, Nakashima Y, Murata K, Saishoji T, Nomura K, Ogawa M. Increased expression of membrane-associated phospholipase A2 shows malignant potential of human breast cancer cells. Cancer. 1993;71:3058–64.
Asano T, Shoda J, Ueda T, Kawamoto T, Todoroki T, Shimonishi M, Tanabe T, Sugimoto Y, Ichikawa A, Mutoh M, Tanaka N, Miwa M. Expressions of cyclooxygenase-2 and prostaglandin E-receptors in carcinoma of the gallbladder: crucial role of arachidonate metabolism in tumor growth and progression. Clin Cancer Res. 2002;8:1157–67.
Ganesan K, Ivanova T, Wu Y, Rajasegaran V, Wu J, Lee MH, Yu K, Rha SY, Chung HC, Ylstra B, Meijer G, Lian KO, Grabsch H, Tan P. Inhibition of gastric cancer invasion and metastasis by PLA2G2A, a novel beta-catenin/TCF target gene. Cancer Res. 2008;68:4277–86.
Mirtti T, Laine VJ, Hiekkanen H, Hurme S, Rowe O, Nevalainen TJ, Kallajoki M, Alanen K. Group IIA phospholipase A as a prognostic marker in prostate cancer: relevance to clinicopathological variables and disease-specific mortality. APMIS. 2009;117:151–61.
Kim HJ, Kim KS, Kim SH, Baek SH, Kim HY, Lee C, Kim JR. Induction of cellular senescence by secretory phospholipase A2 in human dermal fibroblasts through an ROS-mediated p53 pathway. J Gerontol A Biol Sci Med Sci. 2009;64:351–62.
Xing XF, Li H, Zhong XY, Zhang LH, Wang XH, Liu YQ, Jia SQ, Shi T, Niu ZJ, Peng Y, Du H, Zhang GG, Hu Y, Lu AP, Li JY, Chen S, Ji JF. Phospholipase A2 group IIA expression correlates with prolonged survival in gastric cancer. Histopathology. 2011;59:198–206.
Kandouz M, Nie D, Pidgeon GP, Krishnamoorthy S, Maddipati KR, Honn KV. Platelet-type 12-lipoxygenase activates NF-κB in prostate cancer cells. Prostaglandins Other Lipid Mediat. 2003;71:189–204.
Hughes-Fulford M, Li CF, Boonyaratanakornkit J, Sayyah S. Arachidonic acid activates phosphatidylinositol 3-kinase signaling and induces gene expression in prostate cancer. Cancer Res. 2006;66:1427–33.
Sadaria MR, Yu JA, Meng X, Fullerton DA, Reece TB, Weyant MJ. Secretory phospholipase A2 mediates human esophageal adenocarcinoma cell growth and proliferation via ERK 1/2 pathway. Anticancer Res. 2013;33:1337–42.
Hernández M, Martín R, García-Cubillas MD, Maeso-Hernández P, Nieto ML. Secreted PLA2 induces proliferation in astrocytoma through the EGF receptor: another inflammation-cancer link. Neuro Oncol. 2010;12:1014–23.
Yu JA, Kalatardi S, Dohse J, Sadaria MR, Meng X, Fullerton DA, Weyant MJ. Group IIa sPLA2 inhibition attenuates NF-κB activity and promotes apoptosis of lung cancer cells. Anticancer Res. 2012;32:3601–7.
Yu JA, Mauchley D, Li H, Meng X, Nemenoff RA, Fullerton DA, Weyant MJ. Knockdown of secretory phospholipase A2 IIa reduces lung cancer growth in vitro and in vivo. J Thorac Cardiovasc Surg. 2012;144:1185–91.
Lee HY, Kim MK, Park KS, Bae YH, Yun J, Park JI, Kwak JY, Bae YS. Serum amyloid A stimulates matrix-metalloproteinase-9 upregulation via formyl peptide receptor like-1-mediated signaling in human monocytic cells. Biochem Biophys Res Commun. 2005;330:989–98.
Acknowledgments
The authors are grateful to Margot Vogel and Romy Adler for their expert technical assistance.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: Michael J. Parnham
Rights and permissions
About this article
Cite this article
Menschikowski, M., Hagelgans, A., Fuessel, S. et al. Serum amyloid A, phospholipase A2-IIA and C-reactive protein as inflammatory biomarkers for prostate diseases. Inflamm. Res. 62, 1063–1072 (2013). https://doi.org/10.1007/s00011-013-0665-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-013-0665-5