Abstract
Objectives
The aim of this study was to investigate the involvement of the hemoxigenase-1 (HO-1) pathway in the anti-inflammatory action of a sulfated polysaccharide from the red seaweed Gracilaria birdiae (SP-Gb).
Methods
SP-Gb (5, 10 and 20 mg/kg) was administered to Wistar rats in a peritonitis model using carrageenan or a paw edema model using carrageenan or dextran. To analyze the involvement of HO-1 in the anti-inflammatory activity of SP-Gb, the animals were pretreated subcutaneously with a specific HO-1 inhibitor (ZnPP IX). To evaluate the systemic effects, SP-Gb (10 mg/kg) was administered to mice intraperitoneally before waiting for 48 h or for 14 days.
Results
SP-Gb (10 mg/kg) caused an anti-inflammatory effect that was evidenced by a decrease in leukocytes in the peritoneal cavity. SP-Gb also reduced the paw edema induced by carrageenan and inhibited the paw edema induced by dextran in the first half-hour. After being inhibited by ZnPP IX, the anti-inflammatory effect of SP-Gb on carrageenan-induced rat paw edema was not observed. SP-Gb did not cause mortality or significant changes in the biochemical, hematological and histopathological parameters.
Conclusion
SP-Gb may be used as a tool for further investigations into the inflammatory processes associated with the hemoxigenase-1 pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The primary response to infection or injury is inflammation, which functions to clear the injurious material or agent and to promote tissue repair. Inflammation is characterized by the sequential release of a battery of mediators, including bioactive amines, eicosanoids, cytokines, chemokines and growth factors that regulate increased vascular permeability and the recruitment of blood-borne leukocytes. Increased vascular permeability also results in the extravasation of plasma proteins that further amplify the inflammatory reaction. Inflammation is essentially a salutary response that normally resolves with the restoration of normal tissue structure and function; however, when inflammation persists (chronic inflammation), it can cause tissue damage and the loss of function [1].
Hemoxygenase (HO) catalyzes the first and rate-limiting enzymatic step of heme degradation and produces carbon monoxide (CO), iron and biliverdin (BVD) [2, 3], which is converted into bilirubin (BR) via biliverdin reductase [4]. Three genetically distinct HO isozymes are known: HO-1, HO-2 and HO-3. HO-1 is inducible, whereas HO-2 and HO-3 are constitutively expressed [5]. Generally, the induction of HO-1 has been considered to be an adaptive cellular response against the toxicity of oxidative stress [6]. More recently, HO-1 has also been recognized for exhibiting important immunomodulatory and anti-inflammatory functions [4].
According to previous studies, zinc protoporphyrin (ZnPP) IX has been used as a pharmacological reagent that selectively blocks HO action, resulting in the inhibition of carbon monoxide production [7]. Heme is also called ferrous protoporphyrin IX [8] and ZnPP IX acts as a competitive inhibitor, because it also presents a protoporphyrin IX group in its structure [9]. Therefore, ZnPP IX inhibits the production of products of heme (BVD, CO and iron), which protect against cell damage and oxidative stress.
The sulfated polysaccharides found in red seaweeds are mainly galactans [10]. The enantiomeric configuration of the α-galactose classifies the various galactans into two major groups, the carrageenans and the agars [11].
In a previous study, the chemical composition and covalent structure of galactan from the red seaweed Gracilaria birdiae was determined by infrared (FTIR) and nuclear magnetic resonance (NMR) spectroscopy to be an agar [12]. According to these authors, this structure is formed of repeating units of β-d-galactopyranose (50.3%); 3,6-anhydro-α-l-galactopyranose (40.5%) and α-l-galactopyranose-6 sulfate (9.2%).
Seaweeds exhibit diverse biological properties, including antioxidant [13], antitumor [14], immunostimulant [15], antinociceptive and pro-inflammatory activities [16, 17], and thus there is great interest in discovering from them new natural analgesic and anti-inflammatory compounds with few collateral effects [18].
The present study was aimed at investigating the unexplored anti-inflammatory activity of a sulfated polysaccharide isolated from the red seaweed Gracilaria birdiae (SP-Gb). We also investigated whether this anti-inflammatory effect depends on the integrity of the HO-1 pathway. A systemic evaluation of this polysaccharide was also performed.
Materials and methods
Animals
Male Swiss mice (20–25 g) and Wistar rats (180–240 g) from the Animal Care Unit of the Federal University of Ceará, Fortaleza, Brazil, were used throughout the experiments. They were housed in a temperature-controlled room with free access to water and food on a 12/12-h light/dark cycle. For each experiment, groups of six animals were segregated and handled separately. All procedures and animal treatments were carried out at a controlled ambient temperature (20–22°C), and special care was taken to avoid environmental disturbances that might influence animal responses. This study was conducted in accordance with the guidelines set forth by the U.S. Department of Health and Human Services and with the approval of the Ethics Committee of the Federal University of Ceará, Fortaleza, Brazil (CEPA No. 80/10).
Drugs and reagents
The following drugs and reagents were used: dextran sulfate, λ-carrageenan, cetylpyridinium chloride (CPC), 1-9 dimethyl-methylene blue (DMB), DEAE-cellulose, ο-dianisidine dihydrochloride, N-acetyl-N,N,N-trimethylammonium bromide, potassium phosphate monobasic, potassium phosphate dibasic, hexadecyltrimethylammonium bromide (HTAB), zinc protoporphyrin IX (ZnPP IX), cystein, papain and bovine serum albumin, which were purchased from Sigma Aldrich (St. Louis, MO, USA). Dexamethasone was purchased from Aché (Guarulhos, SP, Brazil). Gelatin was purchased from Oxoid Ltd. (Basingstoke, UK). Ethylenediaminetetraacetic acid (EDTA), formaldehyde, glacial acetic acid and chloral hydrate were purchased from Vetec Química Fina, Ltda (SP, Brazil). The drugs and the SP-Gb were solubilized in 0.9% sterile NaCl (saline). The enzymatic kits used for evaluation of the systemic toxicity of SP-Gb were from Labtest Diagnosis (Brazil). All other chemicals were of analytical grade.
Isolation of sulfated polysaccharides (SP)
G. birdiae was obtained from the Atlantic coast of Brazil (Flecheiras Beach, Trairí-Ceará). After collection, the specimens were taken to the Carbohydrates and Lectins Laboratory (CarboLec), Department of Biochemistry and Molecular Biology, Federal University of Ceará, and then cleaned of epiphytes, washed with distilled water and stored at −20°C until further use. A voucher specimen (No. 40781) was deposited in the Herbarium Prisco Bezerra in the Department of Biological Sciences, Federal University of Ceará, Brazil.
The dried tissue (5 g) was cut into small pieces and suspended in 250 ml of a 0.1 M sodium acetate buffer (pH 5.0) containing 510 mg of papain, 5 mM EDTA and 5 mM cysteine. It was then incubated at 60°C for 6 h as previously described [19], with some modifications. The total sulfated polysaccharides (TSP) obtained from G. birdiae, which is an agar formed by a complex chain of the alternating disaccharide repeating units (50 mg), was dissolved in 25 ml of a 50 mM sodium acetate buffer (pH 5.0) and applied to a DEAE-cellulose column (28 × 2.0 cm) equilibrated with the same solution. The column was developed by a step-wise gradient of 0 → 1.5 M NaCl in the same solution with intervals of 0.25 M between each concentration. The flow rate of the column was 2.5 ml/min. Fractions measuring 5 ml were collected and analyzed for sulfated polysaccharide content using the metachromatic assay (A525 nm) with DMB, as described [20], and for total sugar content according to the phenol–sulfuric acid method [21]. The biological protocols were performed with the fraction that showed the highest yield of sulfated polysaccharide (SP-Gb).
Chemical composition
The total sugar content was estimated by phenol–sulfuric acid analysis using d-galactose as the standard [21]. After acid hydrolysis of the soluble polysaccharides (1 M HCl, 110°C, 5 h), free sulfate was measured using Na2SO4, as is standard in the gelatin–barium method previously described [22]. The protein content was measured by binding Coomassie Brilliant Blue G-250 to protein using bovine serum albumin (BSA) as the standard [23].
Peritonitis model
Carrageenan (Cg) (700 μg/cav) or sterile saline (1 ml) were injected intraperitoneally (i.p.) in the rats. The animals were treated subcutaneously (s.c.) with SP-Gb (5, 10 or 20 mg/kg) 1 h before stimuli. Dexamethasone (1 mg/kg; s.c.), a synthetic glucocorticoid with potent anti-inflammatory and immunosuppressant properties, was administered 1 h before Cg as a reference compound [16]. Four hours later, the animals were killed, and the peritoneal cavity was washed with 10 ml of saline containing 5 IU/ml of heparin. The peritoneal fluid was recovered, and total and differential leukocyte counts were performed. Results are expressed as mean ± SEM of the number of cells × 103/ml of peritoneal fluid [24].
Carrageenan-induced rat paw edema
Carrageenan (500 μg/paw, 100 μl) was injected s.c. into the right paw of the rats. The animals were pretreated with SP-Gb s.c. at doses of 5, 10 or 20 mg/kg (0.1 ml/100 g body weight) 1 h before the stimuli. Dexamethasone (1 mg/kg, s.c.) was administered 1 h before carrageenan as a reference compound. Paw volume was measured immediately before (0 h) the stimulus and at selected time intervals (1, 2, 3 and 4 h) using a plethysmometer (Panlab, Spain). The results are expressed as the variation in paw volume (ml), calculated as the difference from the basal volume [25].
Dextran-induced rat paw edema
Dextran (400 μg/paw, 100 μl), a classical osmotic agent [26], was injected s.c. into the right paw of the rats. One hour before stimuli, the animals were pretreated (0.1 ml/100 g body weight s.c.) with SP-Gb (5, 10 or 20 mg/kg). Paw volume was measured immediately before (0 h) the stimulus and at selected time intervals (0.5, 1, 2, 3 and 4 h).
Determination of myeloperoxidase activity
Myeloperoxidase (MPO) is an enzyme found primarily in the azurophilic granules of neutrophils and has therefore been used extensively as a biochemical marker of granulocyte infiltration into various tissues. The extent of neutrophil accumulation in the paw tissue was measured using an MPO activity assay, as previously described [27]. Briefly, 50–70 mg of paw tissue was homogenized in 1 ml of potassium phosphate buffer containing 0.5% HTAB for each 50 mg of tissue. Then, the homogenate was centrifuged at 4,000g for 12 min at 4°C. MPO activity was assayed by measuring the change in absorbance at 450 nm, taking two readings at 60 s intervals, using 1 mM o-dianisidine dihydrocloride and 0.0005% hydrogen peroxide in a microplate. A unit of MPO activity was defined as that which converted 1 μmol of hydrogen peroxide to water in 1 min at 22°C. The results are reported as MPO units/mg of tissue.
Analysis of HO-1 pathway involvement in the anti-inflammatory activity of SP-Gb
In order to analyze the involvement of HO-1 in the anti-inflammatory efficacy of SP-Gb, the animals were pre-treated (s.c.) with ZnPP IX (3 mg/kg), followed by injection (s.c.) of SP-Gb (10 mg/kg) 60 min later. After 1 h, carrageenan (500 μg/paw) was injected s.c. [28]. Paw volume was measured immediately before (0 h) the stimulus and at selected time intervals (1, 2, 3 and 4 h) using a plethysmometer (Panlab, Spain). The results are expressed as the variation in paw volume (ml), calculated as the difference from the basal volume (0 h).
Systemic evaluation of SP-Gb
Survival rate, hair erection, scratching or licking of paws, freezing reactions and general overall behavior were evaluated for 48 h after a single dose of SP-Gb (10 mg/kg, i.p.) or sterile saline.
In addition, body mass loss, organ weight alteration, and hematological and biochemical parameters were evaluated in the mice injected i.p. daily with a single dose of SP-Gb (10 mg/kg) or sterile saline for 14 consecutive days. Histopathological analyses were also performed.
Hematological and biochemical parameters
On the 15th day, all the animals were anesthetized with chloral hydrate, and blood samples were collected from the retro-orbital plexus for hematology and serum biochemistry. Hematology analysis was performed using an automated pocH 100iV DIFF hematology analyzer (Sysmex Europe GmbH, Hamburg, Germany). Blood samples (15 μl) were applied to the automatic analyzer to measure the following parameters: red blood cells count (RBC), hemoglobin concentration (HGB), hematocrit (HCT), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), platelet count (PLT), white blood cell count (WBC), and differential WBC (leukocytes, monocytes and neutrophils). For serum biochemistry analysis, the blood was centrifuged at 1,500g for 15 min after collection. The serum samples were stored at −80°C prior to analysis. The following serum biochemistry parameters were determined by enzymatic and colorimetric tests from Labtest: alkaline phosphatase (ALP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), creatinine and urea. After killing the animals, the liver, thymus, lymph nodes, spleen, kidney and heart were removed and weighed. Possible ulcerative lesions or hemorrhaging were quantified and macroscopically measured.
Histopathological analysis
The liver, thymus, lymph nodes, spleen, kidney and heart were fixed with formalin. The material was then dehydrated by increasing concentrations of 70% ethanol and processed for inclusion in paraffin. The resulting blocks were sliced in 5-μm-thick sections, stained with hematoxylin–eosin (H&E) and observed under a light microscope.
Statistical analysis
The data are presented as the mean ± standard error (SEM) for six animals per group. Analysis of variance (ANOVA) was performed using Bonferroni’s test and Student’s t test for unpaired values. Values of p < 0.05 were considered to be statistically significant.
Results
Isolation of sulfated polysaccharides
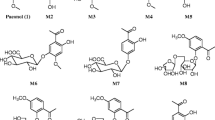
Enzymatic extraction of TSP from the seaweed Gracilaria birdiae, followed by the application of TSP on DEAE-cellulose chromatography, resulted in the determination of two fractions of TSP (FI and FII). Because FI provided a higher yield than FII, biological experiments were performed with FI (SP-Gb) (Fig. 1).
Scheme of the isolation procedure of the total sulfated polysaccharide (TSP) from red seaweed Gracilaria birdiae. A TSP was obtained with papain digestion (60°C, 6 h) in a 0.1 M sodium acetate buffer (pH 5.0) containing 5 mM cysteine and 5 mM EDTA. B The freeze-dried TSP (50 mg) was submitted to a DEAE-cellulose column (28 × 2.0 cm) equilibrated with a 50 mM sodium acetate buffer (pH 5.0), separated into two SP fractions [F I (SP-Gb) and F II] eluted at concentrations of 0.5 and 0.75 M of NaCl, respectively
A yield of 4.66% TSP was obtained. The two fractions of TSP (FI and FII) were obtained using their metachromatic properties and their total sugar content (Fig. 2a). These fractions showed yields of 23.6 and 6.4%, respectively. The following values were obtained during the determination of soluble carbohydrates in the TSP and the fractions (FI and FII): 68.2% total carbohydrates for TSP, 37.4% soluble carbohydrates for FI and 30.8% soluble carbohydrates for FII. The following values were obtained during the determination of free sulfate in the hydrolysates of the TSP and the fractions (FI and FII): 8.38% of free sulfate in TSP, 14.81% of free sulfate for FI and 13.22% of free sulfate for FII. No content protein was detected in TSP or either fraction. The SP obtained was analyzed using 0.5% agarose gel electrophoresis and exhibited different charge densities. Each purified fraction showed a polydisperse band, whereas TSP exhibited a weak metachromasia on gel because it presented a lower sulfate level, according to the values obtained for the free sulfate content (Fig. 2b).
a Separation of SP-Gb by DEAE-cellulose. Fractions were collected and checked by metachromasia using 1,9-dimethymethylene blue (filled squares) and by total sugar content according to the phenol–sulfuric acid method (open squares). Down arrows represent the NaCl concentration. b Agarose gel electrophoresis of SP-Gb. Total sulfated polysaccharides (TSP) and fractions F I (0.5 M) and F II (0.75 M) on gel were stained with 0.1% toluidine blue
Anti-inflammatory activity
SP-Gb (10 mg/kg) injected s.c. caused a 52% reduction in total leukocyte migration when administered 1 h before Cg (Fig. 3a). This reduction was attributed to the inhibition of neutrophil and mononuclear cell influx (54.76 and 54.0%, respectively) (Fig. 3b, c). As a reference, dexamethasone decreased the Cg-induced neutrophil migration by 73.2%. Saline injection did not induce neutrophil migration or mononuclear cell influx (Fig. 3). In addition, Cg (500 μg/paw, s.c.) caused intense paw edema, which reached a maximum level at 3 h (0.47 ± 0.01 ml). Again, SP-Gb (10 mg/kg) significantly reduced the occurrence of edema after the stimulus, especially in the third hour, with a reduction of 44%. Pre-treatment of the animals with dexamethasone inhibited the edema by 66% (Fig. 4). These data were confirmed by MPO activity showing that 10 mg/kg SP-Gb and 20 mg/kg SP-Gb inhibited neutrophil accumulation in the paw by 59.3 and 36.92%, respectively. Dexamethasone also inhibited the MPO activity by 81.9% (Fig. 5).
The effect of SP-Gb on neutrophil migration induced by carrageenan in the rats. Before receiving an injection of carrageenan (700 μg/cav, s.c.), some groups of animals received SP-Gb (5, 10 or 20 mg/kg) and dexamethasone (1 mg/kg) s.c. Another group received only saline without Cg. Total leukocytes (a), neutrophils (b) and mononuclear cells (c) counts were performed. Data are expressed as mean ± SEM of six rats for each group. * Statistically significant difference (p < 0.05) from the carrageenan group
Activity of myeloperoxidase (MPO) in the supernatant of homogenates of the paw sections given carrageenan, SP-Gb (5, 10 or 20 mg/kg), dexamethasone or saline (s.c.), expressed as MPO units/mg of tissue. Data are expressed as mean ± SEM of six rats for each group. *Statistically significant difference (p < 0.05) from the carrageenan group (ANOVA; Bonferroni’s test)
The effect of SP-Gb on paw edema induced by carrageenan in the rats. Before receiving an injection of carrageenan (500 μg/paw, s.c.), some groups of animals received SP-Gb (5, 10 or 20 mg/kg) or dexamethasone (1 mg/kg) s.c. Another group received only saline without Cg. Data are expressed as mean ± SEM of six rats for each group. *Statistically significant difference (p < 0.05) from the carrageenan group (ANOVA; Bonferroni’s test)
Finally, dextran (400 μg/paw, s.c.) induced a significant increase in vascular permeability, with the maximum level being reached at 30 min (0.64 ± 0.04 ml) and then decreasing over the subsequent hours. SP-Gb (10 mg/kg) administered 1 h before dextran reduced the increase in vascular permeability by 48.4%, especially during the first 30 min, when compared to the non-treated group (Fig. 6).
The effect of SP-Gb on paw edema induced by dextran in the rats. Before receiving an injection of dextran (400 μg/paw, s.c.), some groups of animals received SP-Gb (5, 10 or 20 mg/kg). Another group received only saline without dextran. Data are expressed as mean ± SEM of six rats for each group. *Statistically significant difference (p < 0.05) from the dextran group (ANOVA; Bonferroni’s test)
To investigate the role of HO-1 activity in the anti-inflammatory effect of SP-Gb, the animals were pretreated (s.c.) with ZnPP IX (3 mg/kg), a specific HO-1 inhibitor. The anti-inflammatory effect of SP-Gb (10 mg/kg) on the Cg-induced rat paw edema test was not observed in the presence of ZnPP-IX (3 mg/kg) (Fig. 7).
HO-1 activity in paw edema induced by carrageenan in the rats. Before receiving an injection of carrageenan (500 μg/paw, s.c.), some groups of animals received SP-Gb (10 mg/kg) with or without ZnPP IX (3 mg/kg, s.c.). Another group received only saline without Cg. Data are expressed as mean ± SEM of six rats for each group. *Statistically significant difference (p < 0.05) from the carrageenan group (ANOVA; Bonferroni’s test)
Systemic effects of SP-Gb
SP-Gb injected in a single dose (10 mg/kg; i.p.) did not produce any signs of toxicity or mortality during the experimental period of 48 h.
After fourteen consecutive days of administration in mice, the animals’ body mass, and wet weights of the liver, kidney, thymus, lymph nodes and heart were considered normal. However, there was an increase in the weight of the spleen, but histopathological analyses of the organs removed from the animals treated with SP-Gb (10 mg/kg) did not reveal any damage to their tissues. The liver showed mild vacuolar panlobular degeneration of the hepatocytes, which might be a response to injury and is considered to be reversible. However, there were no significant lesions in the organs analyzed, and the above-mentioned mild histological change was taken to be reversible. Therefore, there were no consistent signs of systemic damage (data not shown).
In addition, no significant changes were noted in the blood parameters of the treated group. The slight decrease in platelet count is not thought to be of toxicological significance and is within the control range. The slight reduction in WBC and RBC counts were not associated with microscopic change in the associated hematopoietic tissues (Table 1). Although histopathological lesions were sporadically observed in the liver, there were no changes in the enzymatic activity of transaminases and alkaline phosphatase in the treated mice compared to the respective controls. Therefore, it is reasonable to conclude that they were of little toxicological significance. The treatment group also presented with normal kidney function, since SP-Gb did not induce any alteration in blood urea and creatinine levels (Table 2).
Discussion
Marine organisms are sources of structurally diverse bioactive compounds that contain substances with valuable pharmaceutical and biomedical potentials [29, 30]. The results reported here demonstrate that SP-Gb exerts an anti-inflammatory effect in two models of acute inflammation caused by different inductors, carrageenan and dextran.
SP-Gb was tested initially in carrageenan-induced peritonitis in the rats in order to investigate the possible alterations in leukocyte chemotaxy. Carrageenan induces neutrophil migration into the rat peritoneal cavity by an indirect mechanism, via activation of macrophages [31]. In this model, SP-Gb (10 mg/kg) significantly decreased the leukocyte count in the rat peritoneal cavities. The anti-inflammatory effect elicited by SP-Gb is in line with the literature that demonstrated that sulfated galactans of the red algae Pophyridium sp. also showed anti-inflammatory activity [32].
Due to the anti-inflammatory effect elicited by SP-Gb on the carrageenan-induced peritonitis, the anti-inflammatory effect of SP-Gb was tested in Cg- and dextran-induced rat paw edema. Carrageenan is classically used as a positive control in experimental models of inflammation because of its pro-inflammatory effects that involve cell migration and the participation of diverse mediators, such as histamine, serotonin, bradykinin, nitric oxide, and prostaglandins, and that are characterized by intense neutrophil infiltration [33, 34]. Conversely, dextran increases vascular permeability by releasing vasoactive amines, such as histamine and serotonin, causing an osmotic edema with low levels of protein and neutrophils [26]. SP-Gb (10 mg/kg) inhibited both Cg- and dextran-induced rat paw edema and neutrophil migration, as confirmed by myeloperoxidase activity. Myeloperoxidase tissue levels are a well-standardized marker of neutrophil infiltration into tissue and have been clearly shown to correlate with the disease severity [34]. These results suggest that the anti-edematogenic response of SP-Gb is complex and may be related to the inhibition of both neutrophil migration and the release of vasoactive amines. This is probably a result of the anti-histaminic effect that may be caused by the inhibition of mast cell degranulation [35, 36]. The results presented allowed us to characterize an inhibitory profile on cell migration. However, SP-Gb (5 or 20 mg/kg) did not show efficacy. These data are in accordance with the literature that reports both anti- and pro-inflammatory effects with sulfated polysaccharides from seaweeds [16, 17, 37–39]. It is believed that the presence of an effect with SP-Gb only at the intermediate dose is related to the “all or none” or quantal stimulus, in which the animal discriminates the presence or absence of the ideal dose and then emits a “yes or no” response [40].
Numerous studies have demonstrated that the HO-1/BVD/CO pathway expression has anti-inflammatory consequences [4]. HO-1 is a stress-responsive protein induced by various oxidative agents, and its expression in response to the different inflammatory mediators may contribute to the resolution of inflammation and has protective effects against oxidative injury in several organs [41]. Some authors have demonstrated that a sulfated polysaccharide fraction from the brown algae Porphyra haitanesis shows antioxidant properties in vivo [42]. Also, the anti-inflammatory effects of HO-1 have been reported in rat models induced by carrageenan [43]. Considering these data, in this work we explored the involvement of HO/BVD/CO in the anti-inflammatory effect of SP-Gb.
In the present study, after pretreatment with ZnPP IX, an anti-inflammatory effect of SP-Gb on Cg-induced paw edema was not observed, suggesting that HO-1 activity is involved in the inhibitory effect of SP-Gb in this model. Our group has recently determined the bilirubin levels (product of BVD conversion by the BVD reductase enzyme) in peritoneal exudates, as indexes of the HO-1 activity, in the writhing test [44]. After an acetic acid challenge, increased levels of bilirubin were detected in the peritoneal exudate and ZnPP IX reduced bilirubin production [44]. Thus, our findings corroborate other data showing that the inhibition of the HO-1 pathway is associated with the inhibition of the inflammatory response [45, 46].
It has been demonstrated in toxicological studies that sulfated polysaccharides are well tolerated in experimental animals [17, 47]. According to the literature, sulfated polysaccharides isolated from C. feldmannii induced morphological changes in the organs of experimental animals; nevertheless, these effects were reversible [14]. Subchronic SP-Gb treatment in mice did not affect animal body mass or the wet weight of organs such as the liver, heart, kidney, thymus or lymph nodes. Though an increase in the relative weight of the spleen was observed, there were no histopathological lesions in this organ suggestive of an immunostimulant action. Considering this, some authors have demonstrated that a sulfated polysaccharide fraction extracted from the brown algae Porphyra haitanesis shows an antioxidant property in vivo, causing an increase in the spleen and thymus sizes [42]. Furthermore, neither renal nor hepatic function nor the number of circulating leukocytes was altered by the SP-Gb treatment. These data suggest that SP-Gb is safe and well tolerated in mice.
Conclusion
The present study described both the efficacy and safety of sulfated polysaccharides from the seaweed G. birdiae in models of inflammation and toxicity. It provides evidence, for the first time, that our knowledge of the anti-inflammatory effect of sulfated polysaccharides from the red seaweed G. birdiae is related to the integrity of the HO-1/BVD/CO pathway, giving a new insight into the mechanism of the action of this sulfated polysaccharide.
References
Rodriguez-Vita J, Lawrence T. The resolution of inflammation and cancer. Cytokine Growth Factor Rev. 2010;21:61–5.
Tenhunen R, Marver HS, Schmid R. The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc Natl Acad Sci USA. 1968;61:748–55.
Maines MD. The heme oxygenase system: a regulator of second messenger gases. Annu Rev Pharmacol Toxicol. 1997;37:517–54.
Paine A, Eiz-Vesper B, Blasczyk R, Immenschuh S. Signaling to heme oxygenase-1 and its anti-inflammatory therapeutic potential. Biochem Pharmacol. 2010;80:1895–903.
McCoubrey WK, Huang TJ, Maines MD. Isolation and characterization of a cDNA from the rat brain that encodes hemoprotein heme oxygenase-3. Eur J Biochem. 1997;247:725–32.
Gozzelino R, Jeney V, Soares MP. Mechanisms of cell protection by heme oxygenase-1. Annu Rev Pharmacol Toxicol. 2010;50:323–54.
Okada D. Zinc protoporphyrin IX suppresses nitric oxide production through a loss of l-arginine in rat cerebellar slices. Neurosci Res. 1996;25:353–8.
Grochot-Przeczek A, Dulak J, Jozkowicz A. Heme oxygenase-1 in neovascularisation: a diabetic perspective. Thromb Haemost. 2010;104:424–31.
Yang G, Nguyen X, Ou J, Prasad Rekulapelli P, Stevenson DK, Dennery PA. Unique effects of zinc protoporphyrin on HO-1 induction and apoptosis. Blood. 2001;97:1306–13.
Fonseca RJC, Oliveira SNMCG, Melo FR, Pereira MG, Benevides NMB, Mourão PAS. Slight differences in sulfation of algal galactans account for differences in their anticoagulant and venous antithrombotic activities. Thromb Haemost. 2008;99:539–45.
Stortz CA, Cerezo AS. Novel findings in carragenans, agaroids and “hybrid” red seaweed galactans. Curr Topics Phytochem. 2000;4:121–34.
Maciel JS, Chaves LS, Souza BWS, Teixeira DIA, Freitas ALP, Feitosa JPA, de Paula RCM. Structural characterization of cold extracted fraction of soluble sulfated polysaccharide from red seaweed Gracilaria birdiae. Carbohydr Polym. 2008;71:559–65.
Costa LS, Fidelis GP, Cordeiro SL, Oliveira RM, Sabry DA, Câmara RBG, Nobre LTDB, Costa MSSP, Almeida-Lima J, Farias EHC, Leite EL, Rocha HAO. Biological activities of sulfated polysaccharides from tropical seaweeds. Biomed Pharmacother. 2010;64:21–8.
Lins KOAL, Bezerra DP, Alves APNN, Alencar NMN, Lima MW, Torres WM, Farias WRL, Pessoa C, Moraes MO, Costa-Lotufo LV. Antitumor properties of a sulfated polysaccharide from the red seaweed Champia feldmannii (Diaz-Pifferer). J Appl Toxicol. 2009;29:20–6.
Hou WY, Chen JC. The immunostimulatory effect of hot-water extract of Gracilaria tenuistipitata on the white shrimp Litopenaeus vannamei and its resistance against Vibrio alginolyticus. Fish Shellfish Immunol. 2005;19:127–38.
Assreuy AMS, Gomes DM, Silva MSJ, Torres VM, Siqueira RCL, Pires AF, Criddle DN, Alencar NMN, Cavada BS, Sampaio AH, Farias WRL. Biological effects of a sulfated-polysaccharide isolated from the marine red algae Champia feldmannii. Biol Pharm Bull. 2008;31:691–5.
Araújo IWF, Vanderlei ESO, Rodrigues JAG, Coura CO, Quinderé ALG, Fontes BP, Queiroz INL, Jorge RJB, Bezerra MM, Silva AAR, Chaves HV, Monteiro HSA, de Paula RCM, Benevides NMB. Effects of a sulfated polysaccharide isolated from the red seaweed Solieria filiformis on models of nociception and inflammation. Carbohydr Polym. 2011;86:1207–15.
Vanderlei ESO, Patoilo KKNR, Lima NA, Lima APS, Rodrigues JAG, Silva LMCM, Lima MEP, Lima V, Benevides NMB. Antinociceptive and anti-inflammatory activities of lectin from the marine green alga Caulerpa cupressoides. Int Immunopharmacol. 2010;10:1113–8.
Farias WRL, Valente MS, Pereira MS, Mourão PAS. Structure and anticoagulant activity of sulfated galactans––isolation of a unique sulfated galactan from the red algae Botryocladia occidentalis and comparison of its anticoagulant action with that of sulfated galactans from invertebrates. J Biol Chem. 2000;275:29299–307.
Farndale RW, Buttle DJ, Barret AJ. Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue. Biochim Biophys Acta. 1986;883:173–7.
Dubois M, Gilles KA, Hamilton JK, Rebers PA, Smith F. Colorimetric method for determination of sugars and related substances. Analytical Chem. 1956;28:350–6.
Dodgson KS, Price RG. A note on the determination of the ester sulfate content of sulfated polysaccharides. Biochem J. 1962;84:106–10.
Bradford MM. A rapid and sensitive method for the quantification of microgram quantities of protein utilizing the principle of protein-dye binding. Analytical Biochem. 1976;72:248–54.
Souza GEP, Ferreira SH. Blockade by antimacrophage serum of the migration of PMN neutrophils into the inflamed peritoneal cavity. Agents Action. 1985;17:97–103.
Winter CA, Risley EA, Nuss GW. Carrageenin induced oedema in hind paw of rats as an assay for anti-inflammatory drugs. Proc Soc Exp Biol Med. 1962;111:544–7.
Lo TN, Almeida AP, Beaven MA. Dextran and carrageenin evoke different inflammatory response in rat with respect to composition of infiltrates and effect of indomethacin. J Pharmacol Exp Ther. 1982;221:261–7.
Bradley PP, Christensen RD, Rothstein G. Cellular and extracellular myeloperoxidase in pyogenic inflammation. Blood. 1982;60:618–22.
Freitas A, Alves-Filho JC, Secco DD, Neto AF, Ferreira SH, Barja-Fidalgo C, Cunha FQ. Heme oxygenase/carbon monoxide biliverdin pathway down regulates neutrophil rolling, adhesion and migration in acute inflammation. Br J Pharmacol. 2006;149:345–54.
Yasuhara-Bell J, Lu Y. Review. Marine compounds and their antiviral activities. Antiviral Res. 2010;86:231–40.
Jiang Z, Okimura T, Yokose T, Yamasaki Y, Yamaguchi K, Oda T. Effects of sulfated fucan, ascophyllan, from the brown alga Ascophyllum nodosum on various cell lines: a comparative study on ascophyllan and fucoidan. J Biosci Bioeng. 2010;110:113–7.
Souza GE, Cunha FQ, Mello R, Ferreira SH. Neutrophil migration induced by inflammatory stimuli is reduced by macrophage depletion. Agents Actions. 1988;24:377–80.
Matsui SM, Muizzudin N, Arad S, Marenus K. Sulfated polysaccharides from red microalgae have anti-inflammatory in vitro and in vivo. Appl Biochem Biotechnol. 2003;104:13–22.
DiRosa M, Giroud JP, Willoughby DA. Studies of the mediators of the acute inflammatory response induced in rats in different sites by carrageenan and turpentine. J Pathol. 1971;104:15–29.
Posadas I, Bucci M, Roviezzo F, Rossi A, Parente L, Sautebin L, Cirino G. Carrageenan-induced mouse paw oedema is biphasic, age-weight dependent and displays differential nitric oxide cyclooxygenase-2 expression. Br J Pharmacol. 2004;142:331–8.
Barbosa ALR, Pinheiro CA, Oliveira GJ, Moraes MO, Ribeiro RA, Vale ML, Souza MHLP. Tumor bearing decreases systemic acute inflammation in rats––role of mast cell degranulation. Inflamm Res. 2009;58:235–40.
Babu NP, Pandikumar P, Ignacimuthu S. Anti-inflammatory activity of Albizia lebbeck Benth., an ethnomedicinal plant, in acute and chronic animal models of inflammation. J Ethnopharmacol. 2009;125:356–60.
Campo VL, Kawano DF, Silva-Junior DB, Carvalho I. Carrageenans: biological properties, chemical modifications and structural analysis––A review. Carbohydr Polym. 2009;77:167–80.
Assreuy AMS, Ponte GC, Rodrigues NVFC, Gomes DM, Xavier PA, Araujo GS, Sampaio AH, Cavada BS, Pereira MG, RL Farias W. Vascular effects of a sulfated polysaccharide from the red marine alga Solieria filiformis. Nat Product Commun. 2010;5:1267–72.
Silva FRF, Dore CMPG, Marques CT, Nascimento MS, Benevides NMB, Rocha HAO, Chavante SF, Leite EL. Anticoagulant activity, paw edema and pleurisy induced carrageenan: action of major types of commercial carrageenans. Carbohydr Polym. 2010;79:26–33.
McMillan DE, Li M, Hardwick WC. Schedule control of quantal and graded dose-effect curves in a drug-drug-saline discrimination. Pharmacol Biochem Behav. 2001;68:395–402.
Naito Y, Takagi T, Uchiyama K, Yoshikawa T. Heme oxygenase-1: a novel therapeutic target for gastrointestinal diseases. J Clin Biochem Nutr. 2011;48:126–33.
Zhang Q, Li N, Zhou G, Lu X, Xu Z, Li Z. In vivo antioxidant activity of polysaccharide fraction from Porphyra haitanesis (Rhodophyta) in aging mice. Pharmacol Res. 2003;48:151–5.
Willis D, Moore AR, Frederick R, Willoughby DA. Heme oxygenase: a novel target for the modulation of the inflammatory response. Nat Med. 1996;2:87–90.
Grangeiro NMG, Aguiar JA, Chaves HV, Silva AAR, Lima V, Benevides NMB, Brito GAC, da Graça JRV, Bezerra MM. Heme oxygenase/carbon monoxide-biliverdin pathway may be involved in the antinociceptive activity of etoricoxib, a selective COX-2 inhibitor. Pharmacol Rep. 2011;63:112–9.
Hayashi S, Takamiya R, Yamaguchi T, Matsumoto K, Tojo SJ, Tamatani T. Induction of heme oxygenase-1 suppresses venular leukocyte adhesion elicited by oxidative stress: role of bilirubin generated by the enzyme. Circ Res. 1999;85:663–71.
Alcaraz MJ, Fernández P, Guillén MI. Anti-inflammatory actions of the heme oxygenase-1 pathway. Curr Pharm Des. 2003;9:2541–51.
Siqueira RCL, Silva MSJ, Alencar DB, Pires AF, Alencar NMN, Pereira MG, Cavada BS, Sampaio AH, Farias WRL, Assreuy AMS. In vivo anti-inflammatory effect of a sulfated polysaccharide isolated from the marine brown algae Lobophora variegata. Pharm Biol. 2011;49:167–74.
Acknowledgments
This work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundação Cearense de Apoio ao Desenvolvimento Científico e Tecnológico (FUNCAP) and Programa Rede Nordeste de Biotecnologia (RENORBIO). We thank Dr. Ana de Fátima Fontenele Urano Carvalho from the Department of Biology of the Federal University of Ceará for the use of the automated hematology analyzer, and Ângela Magalhães Vieira for technical assistance. N.M.B. Benevides is a senior investigator of CNPq Brazil.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: Michael Parnham.
Rights and permissions
About this article
Cite this article
de Sousa Oliveira Vanderlei, E., de Araújo, I.W.F., Quinderé, A.L.G. et al. The involvement of the HO-1 pathway in the anti-inflammatory action of a sulfated polysaccharide isolated from the red seaweed Gracilaria birdiae . Inflamm. Res. 60, 1121–1130 (2011). https://doi.org/10.1007/s00011-011-0376-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-011-0376-8