Abstract
Objective
Systemic inflammatory mediators, including the high mobility group box 1 (HMGB1) protein, play important roles in the development of various inflammatory conditions. Although anticoagulants, such as antithrombin III (AT III), inhibit inflammation resulting from various causes, their anti-inflammatory mechanism of action is not well understood. Nevertheless, as heat stroke is a severe inflammatory response disease, we hypothesized that AT III would inhibit inflammation and prevent heat stress-induced acute heat stroke.
Methods
Male Wistar rats received a bolus injection of saline or 250 U of AT III per kg of body weight into the tail vein, followed by heat stress (exposure to 42°C for 30 min). Levels of cytokines (interleukin-1 β, interleukin-6, and TNF-α), NOx, and HMGB1 were measured in serum and tissue at regular intervals for 6 h after the heat stress induction.
Results
Levels of cytokines, NOx, and HMGB1 in serum decreased over time in AT III-treated rats. AT III pretreatment also reduced NOx levels during heat stress-induced inflammation. As a result, AT III pretreatment improved survival in a rat model of heat stress-induced acute inflammation.
Conclusions
Our data suggest that AT III pretreatment inhibited the secretion of cytokines, NOx, and HMGB1, and prevented heat stress-induced acute inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heat stroke commonly occurs in the clinical setting. In particular, heat stroke is often experienced in emergency rooms and intensive care units during the summer season. Severe heat stroke can be fatal, and there has not been a substantial decrease in mortality from heat stroke (variably quoted as 10–50%) in the last 50 years [1]. Heat stroke in humans is characterized by body hyperthermia (>40°C) and multiple-organ dysfunction or failure with hemorrhage and necrosis [2]. Over the past several decades, various strategies to treat heat stroke-induced inflammation have been used clinically. However, the beneficial effects were limited by the particular interventions utilized [3]. Even in the new millennium, we are not much closer to understanding the mechanisms leading from heat stroke to multi-organ failure and death.
Systemic inflammation and hypercoagulable states occur during heat stroke in rats [4]. Given that clinical studies have shown that serum levels of cytokines and chemokines increase in heat stroke patients, these mediators might play an important role in the pathogenesis of heat stroke [5]. For example, levels of interleukin-6 (IL-6) are predictive of heat stroke severity [5, 6]. Nitric oxide (NO) has been implicated in diverse physiological processes, including immune regulation [7]. Because production of NO is increased in heat stroke patients, NO might be an important mediator and key player in pathophysiological processes resulting from heat stroke [8].
The high mobility group box 1 (HMGB1) protein is present in almost all eukaryotic cells. HMGB1, a nuclear protein, was originally identified as a nucleosome stabilizer and transcriptional regulator [9]. The biological importance of HMGB1 is underscored by its multifunctionality, as well as pathological conditions (e.g., trauma, shock, and ischemia–reperfusion injury) associated with its dysregulation [10–12]. Therefore, HMGB1 inhibitors might be beneficial in the treatment of various inflammatory diseases.
The role of clotting factors as inflammatory mediators has attracted recent attention. Antithrombin III (AT III) plays a central role in regulating hemostasis, is a potent anticoagulant with inhibitory effects on procoagulant processes [13], and influences the inflammatory process [14]. Actually, AT III has an inhibitory effect on proinflammatory and procoagulant processes [15, 16].
Based on these findings, we hypothesized that AT III would act as an inhibitor of inflammation and prevent heat stroke. To test this hypothesis, the impact of high-dose AT III pretreatment on serum levels of HMGB1, cytokines, and NO was investigated in a rat model of heat stress-induced acute heat stroke.
Materials and methods
Treatment protocol
All protocols conformed to National Institute of Health (NIH) guidelines, and animal care was performed in compliance with the Principles of Laboratory Animal Care. The study was approved by the Ethics Committee for Animal Research at the College of Medicine, Oita University, Oita, Japan. Rats had unlimited access to food and water before and after treatment.
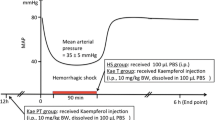
Male Wistar rats (Kyudou, Saga, Japan) weighing 250–300 g were anesthetized with 3% sevoflurane and randomly assigned to one of three groups [1]. In the sham-treated heat stroke group, rats received a bolus injection of a 0.9% NaCl solution (at 1.0 mL per kg) into the tail vein. Under 3% sevoflurane anesthesia, whole bodies of rats were warmed to 42°C for 30 min [2]. In the AT III-treated heat stroke group, rats received a bolus injection of 250 U of AT III (purchased from Mitsubishi Tanabe Pharma Co., Ltd., Osaka, Japan) per kg into the tail vein. Under 3% sevoflurane anesthesia, whole bodies of the rats were warmed to 42°C for 30 min [3]. In the negative control group, rats received a bolus injection of a 0.9% NaCl solution (at 1.0 mL per kg) into the tail vein. Under 3% sevoflurane (Maruishi Pharmaceutical Co., Ltd., Osaka, Japan) anesthesia, whole bodies of rats were warmed to 37°C for 30 min [4]. In the AT III-treated group, rats received a bolus injection of 250 U of AT III into the tail vein. Under 3% sevoflurane anesthesia, whole bodies of rats were warmed to 37°C for 30 min. Body warming was performed using a warm water blanket, and rectal temperature was continuously monitored. All rats were breathing spontaneously throughout the experimental protocol. Following treatment, rats were kept at room temperature.
Samples of venous blood were obtained from the left external jugular vein of rats at the following time points: 0 h (just prior to heat stress treatment), 1.5, 3, and 6 h following heat stress.
Histological examination
After heat stroke injury or exposure to mock warming, rats were anesthetized under 3% sevoflurane and sacrificed by cardiac puncture and exsanguination. Liver, small intestine, and lung tissue were harvested 6 h following heat stroke and fixed in 10% formalin and embedded into paraffin blocks. Sections (3 μm) were cut on a microtome, followed by staining with hematoxylin and eosin. A pathologist blind to treatment assignment evaluated the extent of lung injury according to Murakami’s technique [17]. Briefly, twenty-four areas of lung parenchyma were graded on a scale of 0–4 (0, absent and appears normal; 1, light; 2, moderate; 3, strong; 4, intense) for congestion, edema, inflammation, and hemorrhage. After scoring, we calculated the mean score for each parameter. A pathologist blind to treatment assignment evaluated the extent of liver injury according to Heijnen’s technique [18]. Briefly, liver injury score is reported as the sum of individual scores from 0 (no findings), 1 (mild), 2 (moderate), and 3 (severe) for each of the following six parameters: cytoplasmic color fading, vacuolization, nuclear condensation, nuclear fragmentation, nuclear fading, and erythrocyte stasis. Intestinal mucosa damage was evaluated by two different pathologists according to criteria of Chiu’s method [19]. The Chiu grading system consists of 5 subdivisions according to changes in the villus and glands of the intestinal mucosa: grade 0, normal mucosa; grade 1, development of subepithelial Gruenhagen’s space at the tip of the villus; grade 2, extension of the space with moderate epithelial lifting; grade 3, massive epithelial lifting with few denuded villi; grade 4, denuded villi with exposed capillaries; and grade 5, disintegration of the lamina propria, ulceration, and hemorrhage. A mean score for each of the parameters was then calculated.
Measurement of serum IL-1 β, TNF-α, IL-6, and HMGB1 levels
Serum (n = 8) was prepared from venous blood and stored at −70°C for later analysis. Serum levels of cytokines and HMGB1 were measured using commercial enzyme-linked immunosorbent assay (ELISA) kits for IL-1β, TNF-α, IL-6 (Invitrogen Corporation, Carlsbad, CA, USA), and HMGB1 (Shino-Test Corp., Tokyo, Japan). Assays were performed according to the manufacturers’ protocols. A450 values were obtained with an ELISA reader (Bio-Rad Laboratories, Hercules, CA, USA).
Determination of serum nitrite/nitrate levels
In biological fluids, NO is rapidly deactivated by oxidation to nitrite and nitrate. Blood samples (n = 8) were collected by cardiac puncture of anesthetized rats, and serum fractions were prepared. NO was detected via measurement of nitrite/nitrate levels. Concentration of nitrite/nitrate in serum was determined using a commercial kit (R&D Systems Inc, Minneapolis, MN, USA). The assay, which utilizes a modification of the Griess method [20], was performed according to the manufacturer’s protocol. Absorbance was measured at 540 nm. Nitrite/nitrate concentrations were calculated using a nitrite/nitrate standard curve and expressed as micromoles per liter.
Hematological markers
Blood samples (n = 6) were collected at 1.5 h after whole-body exposure to hyperthermia, anticoagulated with sodium citrate (to a final concentration of 3.13%), and centrifuged at 3,000 rpm for 10 min. Sera were harvested and stored at −70°C for later analysis. Serum concentrations of the hemostatic molecular markers, thrombin–antithrombin complex (TAT) and D-dimer, were measured quantitatively with separate commercial kits for each marker.
Statistical analysis
For descriptive purposes, all continuous data were presented as the mean ± standard deviation. Data were analyzed by one-way analysis of variance (ANOVA) for multiple comparisons followed by the t test with Bonferroni’s adjustment. Calculations were performed with StatView 5.0 (SAS Institute Inc., Cary, NC, USA). Survival curves were derived by the Kaplan–Meier method and compared by log-rank test. Survival rates were calculated with GraphPad 4.0 (GraphPad Software Inc., La Jolla, CA, USA). A P value <0.05 was considered statistically significant.
Results
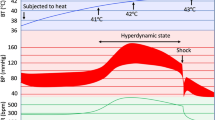
Mortality in rats
While 80% of rats died within 10 h after heat stress, 30% of rats pretreated with AT III (250 U/kg) died in the same time frame. We also examined survival in each group after heat stress and found that rats that did not survive died within 10 h after heat stress in all groups (Fig. 1). The increase in survival rate of AT III-treated rats was significant (P < 0.05). Moreover, all rats were alive in the negative control group after 24 h.
Survival of rats treated with high-dose antithrombin III prior to heat stress. Survival rates were compared between rats treated with a bolus injection of saline into the tail vein prior to heat stress (sham-treated heat stroke group, n = 10; represented by squares) and rats receiving a bolus injection of 250 U of antithrombin III (AT III) per kg of body weight prior to heat stress (AT III-treated heat stroke group, n = 10; represented by circles). Asterisk a significant difference in survival compared to the sham-treated heat stroke group (P < 0.05). Rats treated with high-dose AT III had significantly improved survival compared to rats in the sham-treated heat stroke group. All rats in the negative control group (n = 10) survived (data not shown)
Effect of AT III on lungs, small intestine, and liver after heat stress
Lung tissue specimens were obtained at 6 h after brief exposure to heat stress in rats treated with or without AT III. Although no histological alterations were observed in lung tissue from the negative control (sham-treated) group exposed to 37°C (Fig. 2a), marked interstitial edema and inflammatory cell infiltration were seen in the heat stroke group exposed to 42°C (Figs. 2b, 3a). Interstitial edema and inflammatory cell infiltration were markedly reduced in lung tissue from the AT III-treated heat stroke group (Figs. 2c, 3a) compared to the heat stroke group.
Effect of antithrombin III on organ injury in the heat stroke model. Photomicrographs of tissue sections stained with hematoxylin and eosin obtained 6 h after whole-body warming. A, B, and C are representative specimens (100× magnification) of lung tissue obtained from the a negative control, b sham-treated heat stroke, and c AT III-treated heat stroke groups. Representative specimens (100× magnification) of small intestine tissue obtained from the d negative control, e sham-treated heat stroke, and f AT III-treated heat stroke groups. Representative specimens (100× magnification) of liver tissue obtained from g negative control; h sham-treated heat stroke; and i AT III-treated heat stroke groups
Changes in lung, liver, and intestinal histology scores. a Histological changes included congestion, edema, inflammation, and hemorrhage 6 h after heat stroke. b Histological changes 6 h after heat stroke. c Histological changes included Chiu’s score taken 6 h after heat stroke. Black bars negative control group, white bars sham-treated heat stroke group, and hatched bars AT III-treated heat stroke group (n = 6 per group). Data are expressed as mean ± standard deviation. Asterisk denotes a significant difference relative to scores of rats in the sham-treated heat stroke group (P < 0.05)
Injury to the liver due to heat stroke was multifocal and disrupted the hepatocellular architecture (Figs. 2e, 3b). Pathological abnormalities included sinusoidal congestion, with intra-sinusoidal and central vein accumulation of erythrocytes and neutrophils. In contrast, pathological changes in liver tissue in rats pretreated with AT III were minimal (Figs. 2f, 3b).
Heat stroke-mediated injury to the small intestine was localized to the villi, with tissue loss, desquamation, and exposure of the lamina propria, which demonstrated edema, capillary dilatation, and congestion by erythrocytes (Figs. 2h, 3c). In contrast, minimal pathological changes were observed in the small intestine of rats pretreated with AT III (Figs. 2i, 3c).
Serum nitrite/nitrate levels
The ratio of serum nitrite/nitrate levels was measured at various times after heat stress. Serum nitrite/nitrate levels rose in rats exposed to heat stress (Fig. 4). However, nitrite/nitrate levels were significantly lower in the AT III-treated heat stroke group compared to the sham-treated heat stroke group (Fig. 4). Serum nitrite/nitrate levels in the negative control and AT III-treated groups did not change over the course of the experiment (data not shown).
Effect of antithrombin III on serum nitrite/nitrate levels in the heat stroke model. Serum nitrite/nitrate levels were measured at various times after heat stress. Squares data from the sham-treated heat stroke group, circles data from rats pretreated with 250 U of antithrombin III (AT III) prior to heat stress. All data are expressed as the mean ± standard deviation. Asterisk statistical significance (P < 0.05) compared to the sham-treated heat stroke group
Effects of AT III on serum TNF-α, IL-1 β, IL-6, and HMGB1 levels
Levels of secreted proteins in serum were measured after heat stroke. Serum levels of TNF-α were higher as early as 1.5 h following heat stress (Fig. 5). Injection of high-dose AT III prior to heat stress significantly decreased TNF-α levels (P < 0.05; Fig. 5).
Effect of antithrombin III on serum tumor necrosis factor α levels in the heat stroke model. Serum TNF-α levels were measured at various times after heat stress. Squares data from the sham-treated heat stroke group, circles data from rats pretreated with 250 U of antithrombin III (AT III) prior to heat stress. All data are expressed as the mean ± standard deviation. Asterisk denotes statistical significance (P < 0.05) compared to the sham-treated heat stroke group
Similarly, serum IL-1 β, IL-6, and HMGB1 levels increased following heat stress (Figs. 6, 7, and 8, respectively). The increases in IL-1 β, IL6, and HMGB1 levels in sera were significantly less prominent in the AT III-treated heat stroke group (Figs. 6, 7, and 8, respectively) compared to the sham-treated heat stroke group (P < 0.05; Figs. 6, 7, and 8, respectively). Serum TNF-α, IL-1 β, IL-6, and HMGB1 levels in the negative control and AT III-treated groups were undetectable (data not shown).
Effect of antithrombin III on serum interleukin-1 β levels in the heat stroke model. Serum interleukin-1 β levels were measured at various times after heat stress. Squares data from the sham-treated heat stroke group, circles represent data from rats pretreated with 250 U of antithrombin III (AT III) prior to heat stress. All data are expressed as the mean ± standard deviation. Asterisk denotes statistical significance (P < 0.05) compared to the sham-treated heat stroke group
Effect of antithrombin III on serum interleukin-6 levels in the heat stroke model. Serum interleukin-6 levels were measured at various times after heat stress. Squares data from the sham-treated heat stroke group, circles data from rats pretreated with 250 U of antithrombin III (AT III) prior to heat stress. All data are expressed as the mean ± standard deviation. Asterisk statistical significance (P < 0.05) compared to the sham-treated heat stroke group
Effect of antithrombin III on serum high mobility group box 1 protein levels in the heat stroke model. Serum high mobility group box 1 (HMGB1) levels were measured at various times after heat stress. Squares data from the sham-treated heat stroke group, circles represent data from rats pretreated with 250 U of antithrombin III (AT III) prior to heat stress. All data are expressed as the mean ± standard deviation. Asterisk statistical significance (P < 0.05) compared to the sham-treated heat stroke group
Effects of AT III on serum levels of TAT and D-dimer
Levels of serum TAT, which reflect the status of activating thrombin, showed an increasing trend after heat stroke. In the negative control group, TAT concentration at 1.5 h after a brief exposure to 37°C was 0.68 ± 0.39 ng/mL (Table 1). At 1.5 h after heat stress (exposure to 42°C) in the sham-treated heat stroke group, TAT concentration was 3.78 ± 0.964 ng/mL (Table 1). However, TAT concentration significantly rose to 21.83 ± 4.73 ng/mL (Table 1) in the AT III-treated group at 1.5 h after heat stress.
Plasma D-dimer levels in the negative control group were 0.016 ± 0.09 ng/mL (Table 1). At 1.5 h after heat stress in the sham-treated heat stroke group, plasma D-dimer levels increased to 0.143 ± 0.042 ng/mL. At 1.5 h after heat stress in the AT III-treated rats, plasma D-dimer levels significantly decreased to 0.033 ± 0.014 ng/mL compared to that in the sham-treated heat stroke group.
Discussion
The current study is the first report on improvement of inflammatory conditions by AT III administration in a rat model of heat stroke. We found that AT III treatment significantly attenuated damage to various organs and improved survival rates. Normally, heat stroke activates the inflammatory response, which can progress to multiple organ dysfunction/injury syndrome and death [2]. Therefore, AT III might attenuate the negative effects of heat stroke by attenuating systemic inflammation.
Heat stroke is characterized by systemic inflammation and multiple organ dysfunction. Many consequences of heat stroke result from excessive production of cytokine mediators, including IL-6 and TNF-α [5, 6]. Some studies have shown that HMGB1 is an important mediator of various inflammatory reactions [21, 22]. As such, cytokine and HMGB1 production might reflect this attenuation of systemic inflammation. The present study demonstrated that AT III decreased cytokine and HMGB1 secretion. AT III is a potent anticoagulant with anti-inflammatory properties [13]. Similarly, activated protein C has been shown to attenuate the effects of heat stroke through inhibition of systemic inflammation [23]. In a clinical study of patients with severe sepsis and high mortality risk, high doses of AT III improved sepsis and increased survival time [24]. These results suggest that anti-coagulant therapy not only prevents heat stroke-induced systemic inflammation, but can also be used to treat heat stroke and has potential therapeutic applications.
In this study, we demonstrated suppression of NO production by AT III treatment. NO contributes to the cytotoxicity of neutrophils and macrophages in the inflammatory response [25]. Moreover, under conditions of oxidative stress, the interaction of NO with superoxide radicals gives rise to peroxynitrite, which causes platelet aggregation, disseminated intravascular coagulation, and ubiquitous cell damage [26]. NO also induces HMGB1 secretion [27]. Under conditions of heat stroke, NO production may contribute to local vascular dysfunction [28]. These results suggest that NO is implicated in the organ dysfunction associated with heat stroke, and that inhibition of NO production by AT III treatment may be the mechanism by which AT III attenuates the negative effects of heat stroke.
The present study demonstrated activation of the coagulation pathway upon induction of heat stroke and found that the AT III-treated heat stroke group exhibited significantly reduced serum D-dimer levels. Acute inflammatory events, such as those that occur in response to heat stroke, lead to dysregulation of the coagulation cascade [29]. For instance, Bouchama et al. reported that coagulation and fibrinolysis are activated early and are sustained in heat stroke patients [30]. Increased intravascular coagulation can easily damage various organs. Furthermore, coagulation abnormalities that occur in acute heat stroke are related to the severity of organ damage [29]. Here, we found that levels of TAT and D-dimer increased significantly in the sham-treated heat stroke group, suggesting that these biomarkers are associated with the deterioration of various organ functioning in rats. In addition, AT III treatment reduced heat stroke-related coagulation abnormalities.
Several limitations of this study are worth noting. First, the number of animals evaluated in each treatment group was small. Second, the etiology and features of heat stroke and inflammation experienced by rats exposed to a brief period of heat stroke may be different from heat stroke and systemic inflammation experienced by patients in clinical settings. In addition, the effects of pretreatment of rats with AT III may not be equivalent to the effects of treatment of patients with AT III after diagnosis of heat stroke. Further studies are required to address these issues.
Using a rat heat stress-induced acute heat stroke model, we demonstrated that pretreatment with 250 U of AT III per kg can lower levels of several systemic inflammatory mediators and improve survival rate. These findings support the possibility that AT III can be used to reduce the severity of acute heat stroke. Our results also suggest that the beneficial effects of AT III can be attributed to modulation of levels of various inflammatory mediators. Given our findings, it is possible that AT III might have therapeutic benefit for patients with heat stroke. In line with this, AT III has low toxicity and has been approved for treatment of systemic inflammatory diseases.
References
Grogan H, Hopkins PM. Heat stroke: implications for critical care and anaesthesia. Br J Anaesth. 2002;88(5):700–7.
Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–88.
Simon HB. Hyperthermia. N Engl J Med. 1993;329:483–7.
Lee JJ, Lin MT, Wang NL, Lin CL, Chang CK. Platonin, a cyanine photosensitizing dye, causes attenuation of circulatory shock, hypercoagulable state, and tissue ischemia during heat stroke. Shock. 2005;24:577–82.
Lu KC, Wang JY, Lin SH, Chu P, Lin YF. Role of circulating cytokines and chemokines in exertional heatstroke. Crit Care Med. 2004;32:399–403.
Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–88.
Moncada S, Randomashi NW, Palmer RMJ. Endothelium-derived relaxing factor: identification as nitric oxide and role in control of vascular tone and platelet function. Biochem Pharmacol. 1988;37:2495–501.
Alzeer AH, Al-Arifi A, Warsy AS, Ansari Z, Zhang H, Vincent JL. Nitric oxide production is enhanced in patients with heat stroke. Intensive Care Med. 1999;25:58–62.
Bustin M. Regulation of DNA-dependent activities by the functional motifs of the high-mobility-group chromosomal proteins. Mol Cell Biol. 1999;19:5237–46.
Wang H, Bloom O, Zhang M, Vishnubhakat JM, Ombrellino M, Che J, et al. HMG-1 as a late mediator of endotoxin lethality in mice. Science. 1999;285:248–51.
Levy RM, Mollen KP, Prince JM, Kaczorowski DJ, Vallabhaneni R, Liu S, et al. Systemic inflammation and remote organ injury following trauma require HMGB1. Am J Physiol Regul Integr Comp Physiol. 2007;293:R1538–44.
Tsung A, Hoffman RA, Izuishi K, Critchlow ND, Nakao A, Chan MH, et al. Hepatic ischemia/reperfusion injury involves functional TLR4 signaling in nonparenchymal cells. J Immunol. 2005;175:7661–8.
Opal SM, Kessler CM, Roemisch J, Knaub S. Antithrombin, heparin, and heparan sulfate. Crit Care Med. 2002;30:S325–31.
Taylor FB Jr, Emerson TE Jr, Jordan R, Chang AK, Blick KE. Antithrombin-III prevents the lethal effects of Escherichia coli infusion in baboons. Circ Shock. 1988;26:227–35.
Wiedermann CJ. Clinical review: molecular mechanisms underlying the role of antithrombin in sepsis. Crit Care. 2006;10:209.
Hagiwara S, Iwasaka H, Matsumoto S, Noguchi T. High dose antithrombin III inhibits HMGB1 and improves endotoxin-induced acute lung injury in rats. Intensive Care Med. 2008;34:361–7.
Murakami K, McGuire R, Cox RA, Jodoin JM, Bjertnaes LJ, Katahira J, et al. Heparin nebulization attenuates acute lung injury in sepsis following smoke inhalation in sheep. Shock. 2002;18:236–41.
Heijnen BH, Straatsburg IH, Gouma DJ, Van Gulik TM. Decrease in core liver temperature with 10°C by in situ hypothermic perfusion under total hepatic vascular exclusion reduces liver ischemia and reperfusion injury during partial hepatectomy in pigs. Surgery. 2003;134:806–17.
Chiu CJ, McArdle AH, Brown R, Scott HJ, Gurd FN. Intestinal mucosal lesion in low-flow states: I, a morphological, hemodynamic, and metabolic reappraisal. Arch Surg. 1970;101:478–83.
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR. Analysis of nitrate, nitrite and [15 N] nitrate in biological fluids. Anal Biochem. 1982;126:131–8.
Voll RE, Urbonaviciute V, Herrmann M, Kalden JR. High mobility group box 1 in the pathogenesis of inflammatory and autoimmune diseases. Isr Med Assoc J. 2008;10:26–8.
Mantell LL, Parrish WR, Ulloa L. Hmgb-1 as a therapeutic target for infectious and inflammatory disorders. Shock. 2006;25:4–11.
Lin XJ, Li YL, Mei GP, Zou F, He DD, Liu XQ, Li YJ, Zhao TB, Lin MT. Activated protein c can be used as a prophylactic as well as a therapeutic agent for heat stroke in rodents. Shock. 2009 Mar 13.
Wiedermann CJ, Hoffmann JN, Juers M, Ostermann H, Kienast J, Briegel J, et al. High-dose antithrombin III in the treatment of severe sepsis in patients with a high risk of death: efficacy and safety. Crit Care Med. 2006;34:285–92.
Dabrowski A, Gabryelewicz A. Nitric oxide contributes to multiorgan oxidative stress in acute pancreatitis. Scand J Gastroenterol. 1994;29:943–8.
Viola G, al-Mufti RA, Sohail M, Williamson RC, Mathie RT. Nitric oxide induction in a rat model of selective pancreatic ischemia and reperfusion. Hepatogastroenterology. 2000;47:1250–5.
Jiang W, Pisetsky DS. The role of IFN-alpha and nitric oxide in the release of HMGB1 by RAW 264.7 cells stimulated with polyinosinic-polycytidylic acid or lipopolysaccharide. J Immunol. 2006;177:3337–43.
Hall DM, Buettner GR, Matthes RD, Gisolfi CV. Hyperthermia stimulates nitric oxide formation: electron paramagnetic resonance detection of NO-heme in blood. J Appl Physiol. 1994;77:548–53.
al-Mashhadani SA, Gader AG, al Harthi SS, Kangav D, Shaheen FA, Bogus F. The coagulopathy of heatstroke: alterations in coagulation and fibrinolysis in heatstroke patients during the pilgrimage (Haj) to Makkah. Blood Coagul Fibrinolysis. 1994;5:731–6.
Bouchama A, Bridey F, Hammami MM, Lacombe C, al-Shail E, al-Ohali Y, et al. Activation of coagulation and fibrinolysis in heatstroke. Thromb Haemost. 1996;76:909–15.
Acknowledgments
The authors wish to thank Hiroaki Kawazato and Aiko Yasuda for helpful advice on hematoxylin and eosin staining.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: L. Li.
Rights and permissions
About this article
Cite this article
Hagiwara, S., Iwasaka, H., Shingu, C. et al. High-dose antithrombin III prevents heat stroke by attenuating systemic inflammation in rats. Inflamm. Res. 59, 511–518 (2010). https://doi.org/10.1007/s00011-009-0155-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-009-0155-y