Abstract
Objective
The aim of this study was to investigate the inhibitory effect of geniposide on lipopolysaccharide (LPS)-induced interleukin-6 (IL-6) and interleukin-8 (IL-8) production in human umbilical vein endothelial cells (HUVECs).
Materials and methods
Primary HUVECs were used. The mRNA/protein levels of IL-6 and IL-8 was determined by reverse transcription-polymerase chain reaction (RT-PCR) and enzyme-linked immunosorbent assay (ELISA). LPS-induced HUVEC migration and adhesion of monocytes to HUVECs were studied by monolayer wound healing experiments and monocytic cell adhesion assay, respectively. Expression of nuclear factor κB (NF-κB), inhibitory factor κB-α (IκB-α), p38 mitogen-activated protein kinase (MAPK) and ERK1/2 were determined by Western blot analysis.
Results
Geniposide effectively inhibited LPS-induced expression of IL-6 and IL-8 in HUVECs at the transcription and translation levels. Additionally, geniposide suppressed LPS-induced HUVEC migration and U937 monocyte adhesion to HUVECs. Signal transduction studies indicate that geniposide blocked the activation of NF-κB, degradation of IκB-α, and phosphorylation of p38 MAPK and ERK1/2 in HUVECs challenged by LPS.
Conclusion
The results show that geniposide can inhibit LPS-induced IL-6 and IL-8 production in HUVECs by blocking p38 MAPK and ERK1/2 signaling pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endothelial cell injury and inflammation are shown to be the main mechanisms in the development of cardiovascular diseases [1]. When stimulated by pathogenic mediators, endothelial cells trigger critical inflammatory elements including increased permeability, intensified leukocyte recruitment and up-regulated production of inflammatory cytokines, to be involved in pathogenesis of vascular disorders [2].
Lipopolysaccharide (LPS), an integral part of the outer membrane of Gram-negative bacteria, is one of the important pathogenic stimuli. Circulating LPS in blood directly promotes vascular inflammation via the activation of resident cells such as endothelial cells and vascular smooth muscular cells [3]. It has been reported that human umbilical vein endothelial cells (HUVECs) after LPS challenge will initiate the over-production of interleukin-6 (IL-6), interleukin-8 (IL-8), vascular cell adhesion molecule-1 (VCAM-1) and E-selectin [4–6]. Among these inflammatory cytokines, IL-6 and IL-8 are of special importance for their potent pro-inflammatory and chemotactic activities in influencing the development of vascular inflammation [7]. Therefore, inhibiting the production of IL-6 and IL-8 in activated endothelial cells may be an effective strategy and target to prevent occurrence of cardiovascular diseases.
Gardenia, the fruit of Gardenia jasminoides Ellis (Rubiaceae), has been described as an anti-inflammatory agent. Geniposide is an iridoid glycoside isolated from Gardenia and widely used as a traditional Chinese medicine for its diverse pharmacological activities. In Asian countries, geniposide was commonly applied to ameliorating ligament injuries [8]. In addition, geniposide showed anti-oxidative [9, 10], anti-tumor [11, 12], anti-asthma and anti-diabetic activities [13, 14]. Recently, more studies have been focused on the therapeutic effect of geniposide on cardiovascular diseases. For instance, it has been shown that geniposide displayed an anti-thrombotic effect in vivo due to the suppression of platelet aggregation [15]. Koo et al. [16] have reported that geniposide possessed remarkable anti-angiogenic activity by chick embryo chorioallantoic membrane assay. Studies by Lee et al. [17] further proved that geniposide may be a therapeutic agent for ischemia in patients. However, no studies have provided direct evidence of geniposide-mediated inhibitory effect on LPS-induced over-production of IL-6 and IL-8 in endothelial cells, which may be important for further application of geniposide against cardiovascular diseases.
HUVECs, derived from human umbilical veins, are commonly accepted in vitro experimental models in vascular inflammation, angiogenesis, wound healing, atherosclerosis, etc. [18]. In the present study, we investigated the effect of geniposide on IL-6 and IL-8 production in LPS-induced HUVECs. We evaluated geniposide-mediated inhibition of IL-6 and IL-8 expression in HUVECs at the transcription and translation levels, as well as suppression of LPS-induced HUVEC migration and adhesion of U937 monocytes to HUVECs. To explore the underlying mechanism of suppressive effect of geniposide, the roles of nuclear factor κB (NF-κB) and mitogen-activated protein kinases (MAPKs) in HUVECs after LPS exposure were also determined.
Materials and methods
Chemicals and reagents
Geniposide was purchased from Chengdu Push Biotech Co., Ltd. (Chengdu, China). LPS (rough strains) from Escherichia Coli F583 (Rd mutant), 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), dimethylsulfoxide (DMSO) and endothelial cell growth supplements from bovine neural tissue were obtained from Sigma (St. Louis, MO, USA). ERK1/2 inhibitor (PD98059) and p38 MAPK inhibitor (SB203580) were purchased from Invitrogen Corporation (Carlsbad, CA, USA). Rabbit anti-nuclear factor κB (NF-κB) p65 polyclonal antibody and 2′,7′-bis-(2-carboxyethyl)-5-(and-d)-carboxyfluorescein, acetoxymethyl ester (BCECF AM) were obtained from the Beyotime Institute of Biotechnology (Jiangsu, China). Rabbit anti-inhibitory factor κB-α (IκB-α), anti-p38 MAPK, anti-phospho-p38 (p-p38) MAPK, anti-ERK1/2, anti-phospho-ERK1/2 (p-ERK1/2), anti-GAPDH polyclonal antibody and horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Enzyme-linked immunosorbent assay (ELISA) kits for measurement of IL-6 and IL-8 were obtained from R&D Systems, Inc (Minneapolis, USA). Dulbecco’s-modified Eagle’s medium F12 (DMEM-F12), RPMI-1640 medium and fetal bovine serum (FBS) were obtained from Gibco (Grand Island, NY, USA).
Cell culture and drug treatment
HUVECs were isolated from normal human umbilical cords, digested with 0.05% trypsin containing 0.02% EDTA, and eluted with DMEM-F12. Cells were grown in DMEM-F12 supplemented with 10% FBS, 100 units/ml penicillin, 100 units/ml streptomycin, 30 μg/ml endothelial cell growth supplements and 5 units/ml heparin. Cells were maintained in a 37°C humidified incubator with a 5% CO2 and 95% air environment until desired confluency (80%) was reached. Passage 2–6 was used for experiments. The monocytic cell line U937, bought from the Wuhan Institute of Cell Biology (Wuhan, China), was cultured in RMPI-1640 medium containing 10% FBS and antibiotics.
For most experiments, HUVECs were pretreated with 1% FBS DMEM-F12 in the presence or absence of geniposide (25–100 μg/ml) for 24 h. Thereafter, cells were washed twice with phosphate-buffered saline (PBS, pH 7.4) and then exposed to 100 ng/ml of LPS diluted in culture medium with 1% FBS for different time intervals at 37°C until further assay.
Cell viability assay
Cell viability was assessed by the MTT conversion test. Briefly, HUVECs were seeded at a density of 5 × 103 cells/well in 96-well plates containing 150 μl of DMEM-F12 medium with 10% FBS and grown to sub-confluence. Next, cells received 150 μl of culture medium with 1% FBS plus different concentrations of geniposide (25, 50 and 100 μg/ml) and were incubated for 24 h. After incubation, cells were washed with PBS (pH 7.4) and then incubated with MTT (5 mg/ml) in culture medium for 3 h at 37°C. After that, the medium was discarded and formazan blue, which formed in the cells, was dissolved in 100 μl of DMSO. Optical density at 490 nm was determined with a Sunrise Remote Microplate Reader (Grodlg, Austria). Cell viability in each well was presented as percentage of the control level (treated with vehicle).
Reverse transcription-polymerase chain reaction (RT-PCR)
Total RNA was extracted using TRIZOL (Takara, Dalian, China) and RNA concentration was determined using a DNA/RNA Gene-Quant Calculator (Amersham Biosciences, USA). Reverse transcription was carried out in 10 μl of the reaction mixture containing 1 μg of total RNA, 25 pmol of oligo-dT primer, 10 nmol of dNTP mixture, 20 units of RNase inhibitor and 2.5 units of AMV reverse transcriptase (Bioer, Hangzhou, China) at 42°C for 1 h. PCR amplification was performed in 20 μl PCR reaction mixture containing 1 μl of cDNA reaction mixture, 10 nmol of dNTP mixture, 10 pmol of up- and down-stream primers and 2 units of BioReady rTaq polymerase (Bioer, Hangzhou, China). PCR amplification to detect differences among the samples was set as followed: 4 min at 94°C for initial denaturation; 30 cycles × 30 s at 94°C, 30 s at 60°C, and 30 s at 72°C for IL-8; 25 cycles × 1 min at 94°C, 45 s at 54°C, and 45 s at 72°C for IL-6; 30 cycles × 30 s at 94°C, 30 s at 54°C, and 30 s at 72°C for GAPDH. The following primer pairs were used: IL-6 (497 bp): sense 5′-TGA CAA ACA AAT TCG GTA CAT CC -3′; Antisense: 5′- ATC TGA GGT GCC CAT GCT AC-3′, IL-8 (292 bp): sense 5′-ATG ACT TCC AAG CTG GCC GTG GCT-3′; Antisense 5′- TCT CAG CCC TCT TCA AAA ACT TCT C-3′, GAPDH (230 bp): sense 5′-CTC TCT GCT CCT CCT GTT CGA CAG-3′; Antisense 5′-GTG GAA TCA TAT TGG AAC ATG T-3′. For the analysis of PCR products, 6 μl of each PCR reaction was electrophoresed on 1.5% agarose gel containing 1% GoldView™. Band intensity was analyzed with ImageJ system (NIH, USA) and the GAPDH was used as an internal control to evaluate relative expression of IL-8 and IL-6.
IL-6 and IL-8 production assay by ELISA
IL-6 and IL-8 concentrations in a culture medium of treated cells were measured using commercially available sandwich ELISA kits. All procedures were performed according to the manufacturer’s instructions. All samples were assayed in triplicate.
Monolayer wound healing experiments
To measure the migrating ability of induced HUVECs after treatment with geniposide or MAPK inhibitors, a wound healing assay was carried out [19]. In brief, cells were seeded at a density of 105 cells/well in 24-well plates in DMEM-F12 with 10% FBS and incubated for 24 h. The cells were then pretreated with geniposide for 24 h or with MAPK inhibitors for 1 h. After pretreatment, cell monolayer was interrupted using a 10 μl pipette tip, washed twice with PBS and induced with 100 ng/ml of LPS for 12 h. Cells were then fixed with paraform (4%) and submitted to Hematoxylin and Eosin Staining. Cell migration was photographed using a phase contrast microscope (Wetzlar, Germany). For evaluation of “wound closure” in different experimental conditions, the migrated cells were counted in the wounding zone by a pre-defined frame. The experiment was performed in triplicate.
Monocytic cell adhesion assay
To evaluate monocyte adhesion, HUVECs were seeded at 105 cells/well in 24-well plates and grown to sub-confluence. After pretreatment with geniposide (25–100 μg/ml) for 24 h, cells were induced by 100 ng/ml of LPS for 4 h. Then, the culture medium was removed, and U937 cells labeled with fluorescent dye BCECF-AM (10 μM) were added to culture plates (5 × 104 cells/well) and incubated for 1 h at 37°C. After the co-incubation, wells were gently washed to remove non-adherent U937 cells. Fluorescent images were obtained using a Leica DMRX microscope (Wetzlar, Germany) and fluorescent intensity of each sample was measured with Image-Pro Plus 6.0 software (Media Cybernetics, USA).
Western blot analysis
For isolation of total cell extracts, treated cells were washed twice in ice-cold PBS and lysed with RIPA lysis buffer (50 mM Tris with pH 7.4, 150 mM NaCl, 1% Triton X-100, 1% sodium deoxycholate, 0.1% SDS and 0.05 mM EDTA). Samples were centrifuged at 12,000g for 15 min at 4°C and the supernatant was collected as total cell lysate. Cytoplasmic and nuclear extracts were prepared using the Nuclear and Cytoplasmic Protein Extraction kit according to the manufacturer’s instructions (Beyotime Institute of Biotechnology, Jiangsu, China). Protein concentrations were determined using the Bicinchoninic Acid Protein Assay kit (Beyotime Institute of Biotechnology, Jiangsu, China).
Cell lysate samples were diluted with 5 × loading buffer (125 mM Tris–HCl, pH 6.8, 10% SDS, 8% dithiothreitol, 50% glycerol and 0.5% bromchlorphenol blue) and boiled for 10 min, and 50 μg of protein was loaded per lane on 8–12% SDS-polyacrylamide gels. Proteins were separated and transferred to 0.45 μm polyvinylidene fluoride membranes. Membranes were blocked with 5% skim milk in PBS with 0.1% Tween 20 (PBST) for 1 h. Primary antibodies against human NF-κB, IκB-α, p38, p-p38, ERK1/2, p-ERK1/2 and GAPDH in PBST were incubated with membranes overnight at 4°C. The membranes were then washed in PBST thrice and incubated with HRP-conjugated secondary antibodies for 1 h. After the final wash, protein bands were developed using enhanced chemiluminescence reagents and densitometric analysis was performed with the use of PDI Imageware System (Bio-Rad, Hercules, CA, USA).
Statistics
Statistical analyzes were performed by using the SPSS 10.0 package (SPSS Inc., Chicago, IL, USA). All values were expressed as mean ± S.D. Differences between multiple groups were analyzed using one-way ANOVA followed by a Bonferroni adjustment. Two groups were compared using the Student’s t test. Values of P < 0.05 were considered to be statistically significant.
Results
Geniposide inhibits LPS-induced IL-6 and IL-8 mRNA expression in HUVECs
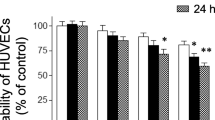
We first evaluated the effect of geniposide on HUVEC viability by MTT assay. Results show that geniposide alone at concentrations of 25, 50 and 100 μg/ml had no inhibitory effect on the viability of HUVECs (Fig. 1). Next, we assessed whether geniposide had inhibitory effect on the expression of inflammatory genes IL-6 and IL-8 in LPS-induced HUVECs by RT-PCR analysis. As shown in Fig. 2a, incubation of cells with 100 ng/ml of LPS for 4 h increased the mRNA expression of both IL-6 (4.1-fold of the vehicle-treated group, P < 0.01) and IL-8 (33.1-fold of the vehicle-treated group, P < 0.01). The increased IL-6 mRNA level was dose-dependently blunted in LPS-induced HUVECs that were pretreated with geniposide for 24 h (25 μg/ml, 57.5% of the LPS-treated group, P < 0.05; 50 μg/ml, 47.1% of the LPS-treated group, P < 0.01; 100 μg/ml, 37.5% of the LPS-treated group, P < 0.01). Geniposide at 25–50 μg/ml failed to show evidenced inhibition of LPS-induced IL-8 mRNA expression, whereas the effect of 100 μg/ml geniposide was statistically significant (37.6% of the LPS-treated group, P < 0.01).
Effect of Geniposide or LPS on cell viability of HUVECs. Cells were treated with Geniposide (25, 50 and 100 μg/ml) or LPS (100 ng/ml) alone for 24 h. After treatment, cell viability was determined by MTT analysis as described in “Materials and methods”. Data are expressed as means ± SD (n = 5)
Geniposide inhibits LPS-induced IL-6 and IL-8 expression in HUVECs at mRNA (a) and protein (b) levels. a Cells were pretreated with geniposide (25, 50 and 100 μg/ml) for 24 h and then exposed to LPS (100 ng/ml) for 4 h. After treatment, mRNA levels of IL-6 and IL-8 were determined by RT-PCR analysis as described in “Materials and methods”. Band density data are expressed as means ± SD (n = 3). b Cells were pretreated with geniposide (25, 50 and 100 μg/ml) for 24 h and then exposed to LPS (100 ng/ml) for 8 h. After treatment, the concentrations of IL-6 and IL-8 in culture medium were determined by ELISA analysis as described in “Materials and methods”. Data are expressed as means ± SD (n = 3). ## P < 0.01 compared to the vehicle-treated group; *P < 0.05, **P < 0.01 compared to the LPS-treated group
Geniposide decreases LPS-induced IL-6 and IL-8 protein secretion in HUVECs
To identify the inhibitory effect of Geniposide on LPS-induced IL-6 and IL-8 protein production in HUVECs, cells were pretreated with geniposide (25–100 μg/ml) for 24 h and then exposed to 100 ng/ml of LPS for 8 h. Thereafter, the cell-free supernatant was collected and subjected to ELISA analysis. Figure 2b shows that cells treated with LPS were found to have more IL-6 (5.7-fold of the vehicle-treated group, P < 0.01) and IL-8 (6.9-fold of the vehicle-treated group, P < 0.01) production. However, geniposide pretreatment remarkably ameliorated LPS-induced IL-6 and IL-8 secretion in HUVECs, with the maximum suppressive effect being observed at 100 μg/ml (for IL-6, 46.5% of the LPS-treated group, P < 0.01; for IL-8, 39.9% of the LPS-treated group, P < 0.01). These results were consistent with that in “Geniposide inhibits LPS-induced IL-6 and IL-8 mRNA expression in HUVECs”.
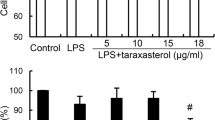
Geniposide suppresses LPS-induced HUVEC migration
Considering the crucial roles of IL-6 and IL-8 in cell chemotaxis and chemokinesis, we evaluated the suppressive effect of geniposide on LPS-induced HUVEC migration. As shown in Fig. 3, the stimulation of HUVECs with 100 ng/ml of LPS for 12 h after “injury” significantly increased cell migration into the “wounded” zone (4.1-fold of the vehicle-treated group, P < 0.01), whereas geniposide pretreatment for 24 h suppressed the migration of induced cells in a dose–dependent manner (25 μg/ml, 103.4% of the LPS-treated group, P > 0.05; 50 μg/ml, 68.9% of the LPS-treated group, P < 0.05; 100 μg/ml, 54.6% of the LPS-treated group, P < 0.01).
Geniposide suppresses LPS-induced HUVEC migration. a After wounding of the HUVEC monolayer, cells were stimulated with vehicle for 12 h. b After wounding of the HUVEC monolayer, cells were stimulated with 100 ng/ml of LPS for 12 h. c After pretreatment with geniposide (100 μg/ml) for 24 h, the HUVEC monolayer was wounded and then exposed to LPS (100 ng/ml) for 12 h. d HUVEC migration was presented as a percentage of the vehicle-treated group. Cells migrated into the denuded area were counted as described in “Materials and methods”. Data are expressed as means ± SD (n = 3). ## P < 0.01 compared to the vehicle-treated group; *P < 0.05, **P < 0.01 compared to the LPS-treated group
Geniposide inhibits U937 cell adhesion to LPS-induced HUVECs
Monocyte adhesion plays a critical role in vascular inflammation and can be induced by chemotactic cytokines. Therefore, we examined whether geniposide could inhibit U937 cell adhesion to LPS-induced HUVECs. We found that stimulation with 100 ng/ml of LPS for 4 h produced a 2.2-fold increase in adhesion of U937 cells to HUVEC monolayers compared with the vehicle-treated group (P < 0.01) (Fig. 4a, b). Pretreatment of HUVECs with geniposide at 25–50 μg/ml for 24 h showed no marked reduction of adherent cells to HUVECs. In contrast, the inhibitory effect of geniposide at 100 μg/ml was statistically significant (72.2% of the LPS-treated group, P < 0.05).
Geniposide inhibits U937 cell adhesion to LPS-induced HUVECs. a Adhesion of fluorescent-labeled U937 cells to vehicle-treated HUVECs for 4 h. b Adhesion of fluorescent-labeled U937 cells to LPS (100 ng/ml)-induced HUVECs for 4 h. c Adhesion of fluorescent-labeled U937 cells to HUVECs pretreated with geniposide (100 μg/ml) for 24 h before exposed to LPS (100 ng/ml) for 4 h. d Monocyte adhesion was presented as a percentage of total fluorescent intensity of the vehicle-treated group. Data are expressed as means ± SD (n = 3). ## P < 0.01 compared to the vehicle-treated group; *P < 0.05 compared to the LPS-treated group
Geniposide decreases nuclear translocation of NF-κB and inhibits degradation of IκB-α in LPS-induced HUVECs
Nuclear translocation of pro-inflammatory transcription factor NF-κB has been confirmed to be involved in the regulation of IL-6 and IL-8 promoters in endothelial cells [20]. Accordingly, we investigated whether geniposide affected LPS-induced NF-κB activation in HUVECs (Fig. 5a). After LPS (100 ng/ml) exposure for 4 h, NF-κB p65 protein showed pronounced decrease in the cytoplasm (54.3% of the vehicle-treated group, P < 0.01) and marked increase in the nucleus (3.1-fold of the vehicle-treated group, P < 0.01). By contrast, geniposide pretreatment for 24 h before LPS exposure led to remarkable up-regulation of cytoplasmic NF-κB p65 protein (25 μg/ml, 1.3-fold of the LPS-treated group, P > 0.05; 50 μg/ml, 1.6-fold of the LPS-treated group, P < 0.05; 100 μg/ml, 1.7-fold of the LPS-treated group, P < 0.05) and striking down-regulation of nuclear NF-κB p65 protein (25 μg/ml, 47.0% of the LPS-treated group, P < 0.01; 50 μg/ml, 50.7% of the LPS-treated group, P < 0.01; 100 μg/ml, 14.2% of the LPS-treated group, P < 0.01), suggesting that geniposide effectively inhibited LPS-induced NF-κB activation in HUVECs.
Geniposide decreases nuclear translocation of NF-κB (a) and inhibits degradation of IκB-α (b) in LPS-induced HUVECs. CE cytoplasmic extracts, NE nuclear extracts. a Cells were pretreated with geniposide (25, 50 and 100 μg/ml) for 24 h and then exposed to LPS (100 ng/ml) for 4 h. After treatment, nuclear and cytoplasmic fractions were analyzed for detection of NF-κB by Western blot analysis as described in “Materials and methods”. b Cells were pretreated with geniposide (25, 50 and 100 μg/ml) for 24 h and then exposed to LPS (100 ng/ml) for 1 h. After treatment, total cell extracts were analyzed for detection of the IκBα by Western blot analysis as described in “Materials and methods”. Data are representative of three experiments (mans ± SD). ## P < 0.01 compared to the vehicle-treated group; *P < 0.05, **P < 0.01 compared to the LPS-treated group
Having demonstrated that geniposide decreased LPS-induced nuclear translocation of NF-κB in HUVECs, we next determined the effect of geniposide on LPS-induced degradation of NF-κB inhibitory protein, I-κBα. Results in Fig. 5b show that LPS (100 ng/ml) exposure for 1 h caused a rapid decrease of cytoplasmic IκB-α (3.7% of the vehicle-treated group, P < 0.01). Pretreatment with geniposide for 24 h inhibited LPS-induced decrease of IκB-α (25 μg/ml, 2.0-fold of the LPS-treated group, P > 0.05; 50 μg/ml, 7.5-fold of the LPS-treated group, P < 0.05; 100 μg/ml, 17.7-fold of the LPS-treated group, P < 0.01). These data indicate that geniposide inhibited LPS-induced degradation of IκB-α in HUVECs.
Geniposide suppresses LPS-induced p38 MAPK and ERK1/2 phosphorylation in HUVECs
Since p38 MAPK and ERK1/2 act as upstream intermediates providing a link between extracellular stimuli and inflammatory cytokines in various cell lines [21, 22], we assessed the effect of geniposide on phosphorylation of both MAPKs by LPS challenge. HUVECs were induced with 100 ng/ml of LPS for 10 min for p38 detection and for 30 min for ERK1/2 detection (Fig. 6a, b). The results suggest that LPS alone markedly activated phosphorylation of p38 (15.1-fold of the LPS-treated group, P < 0.01) and ERK1/2 (1.8-fold of the LPS-treated group, P < 0.01). On the contrary, geniposide pretreatment for 24 h strikingly inhibited p38 MAPK phosphorylation (25 μg/ml, 57.6% of the LPS-treated group, P < 0.05; 50 μg/ml, 13.7% of the LPS-treated group, P < 0.01; 100 μg/ml, 1.1% of the LPS-treated group, P < 0.01), which was almost completely suppressed at 100 μg/ml. Also, geniposide displayed strong inhibition of phosphorylated ERK1/2 level (25 μg/ml, 61.4% of the LPS-treated group, P < 0.05; 50 μg/ml, 73.4% of the LPS-treated group, P < 0.05; 100 μg/ml, 32.6% of the LPS-treated group, P < 0.01).
Geniposide suppresses LPS-induced p38 MAPK and ERK1/2 phosphorylation in HUVECs. Cells were pretreated with geniposide (25, 50 and 100 μg/ml) for 24 h and then exposed to LPS (100 ng/ml) for 10 min for p38 detection and for 30 min for ERK1/2 detection. After treatment, cells were extracted and the protein levels of phosphorylated p38 (p-p38) MAPK, total p38 (t-p38) MAPK, phosphorylated ERK1/2 (p-ERK1/2) and total ERK1/2 (t-ERK1/2) were determined by Western blot analysis as described in “Materials and methods”. Data are representative of three experiments (mans ± SD). ## P < 0.01 compared to the vehicle-treated group; *P < 0.05, **P < 0.01 compared to the LPS-treated group
P38 MAPK and ERK1/2 inhibitors suppress LPS-induced HUVEC migration
Finally, we investigated whether p38 MAPK and ERK1/2 signaling pathways were involved in LPS-induced HUVEC migration. After the treatment as described in “Monolayer wound healing experiments”, both p38 inhibitor (SB203580, 25 μM) and ERK1/2 inhibitor (PD98059, 30 μM) effectively inhibited LPS-induced HUVEC migration (Fig. 7a–d), which was decreased to 43.2% (P < 0.01) and 34.0% (P < 0.01) of the LPS-treated group, respectively (Fig. 7e). These results imply potential roles of p38 MAPK and ERK1/2 pathways in LPS-induced HUVEC migration.
P38 MAPK and ERK1/2 inhibitors suppress LPS-induced HUVEC migration. a After wounding of the HUVECs monolayer, cells were stimulated with vehicle for 12 h. b After wounding of the HUVECs monolayer, cells were stimulated with LPS (100 ng/ml) for 12 h. c After pretreatment with p38 MAPK inhibitor (SB203580, 25 μM) for 1 h, the HUVECs monolayer was wounded and then exposed to LPS (100 ng/ml) for 12 h. d After pretreatment with ERK1/2 inhibitor (PD98059, 30 μM) for 1 h, the HUVECs monolayer was wounded and then exposed to LPS (100 ng/ml) for 12 h. e Cell migration was presented as a percentage of the vehicle-treated group. Cells migrated into the denuded area were counted as described in “Materials and methods”. Data are expressed as means ± SD (n = 3). ## P < 0.01 compared to the vehicle-treated group; **P < 0.01 compared to the LPS-treated group
Discussion
Vascular inflammatory responses seem to be the result of interaction between exogenous stimuli and endothelial cells. Among the strongest stimulators for endothelial cell injury in the body, LPS is proven to be a primary contributor responsible for tissue and organ damage during Gram-negative infection [23]. In pathophysiological situations blood vessels can be exposed to 0.1–100 μg/ml concentrations of LPS [24]. In vivo and in vitro studies also show that high-level LPS exposure can lead to the activation of endothelial cells, secretion of inflammatory cytokines and subsequently complicated immune responses, suggesting a link between endotoxin stress and endothelial cell injury [22]. Thus, how to abrogate the invasion of exogenous stimuli or inhibit the secretion of inflammatory mediators has come to be a pivotal step to prevent and/or delay the pathogenesis of vascular disorders. For the first time, we here demonstrated that geniposide could inhibit the production of IL-6 and IL-8 in LPS-induced HUVECs through the blockade of p38 MAPK and ERK1/2 pathways.
IL-6 has turned out to have various biological properties in a number of chronic endothelial dysfunctions such as modulation of hematopoiesis, proliferation and differentiation of lymphocytes, and induction of acute-phase reactions [25]. IL-8 has been generally recognized as a key intermediate regulator in acute inflammatory responses [26]. Both IL-6 and IL-8 can be over-expressed in endothelial cells challenged by inflammatory stimuli including tumor necrosis factor-α, IL-1α, phorbol myristate acetate and endotoxins [27, 28]. In keeping with these results, we found that LPS (100 ng/ml) induction resulted in an enhanced expression of IL-6 and IL-8 in HUVECs. Moreover, the over-expression of both cytokines was ameliorated by geniposide pretreatment (25–100 μg/ml) for 24 h. Other evidence in support of this view is from studies by Koo et al. [29] in which geniposide shows acute anti-inflammatory activities in rats. These findings indicate that geniposide can act as an inhibitor of IL-6 and IL-8 production.
Under different pathological conditions, endothelial cell migration displays double-faced functions. For instance, the ability of endothelial cells to migrate can be regarded as an important functional activity in wound healing [30]. On the other hand, this excessive migration toward inflammatory sites will aggravate inflammation responses because of the over-production of pro-inflammatory cytokines in endothelial cells. Also, endothelial cell migration is vital for tumor angiogenesis and thus promotes the occurrence and progression of tumors [31]. As early chemotactic signals in acute-phase inflammation reaction, IL-6 and IL-8 play crucial roles in recruiting immune cells to the site of inflammation. For example, IL-6 enhances neutrophil adhesion and recruitment [32], and IL-8 promotes granulocyte migration [27]. However, it remained to be determined about the roles of both pro-inflammatory cytokines in endothelial cell migration. In the present study, cell migration was induced in the LPS-treated HUVECs, implying that IL-6 and IL-8 might promote endothelial cell migration. Notably, the enhanced HUVEC migration was effectively blocked by geniposide (50 and 100 μg/ml) pretreatment. This result indicates that geniposide is an antagonist against endothelial cell migration. One of the integral parts of vascular inflammation is monocyte adhesion, which has been partly attributed to the chemotactic cytokine stimulation [19]. As we expected, geniposide pretreatment at 100 μg/ml significantly suppressed U937 monocyte adhesion to LPS-induced HUVECs. Based on these results, geniposide may lessen LPS-induced HUVEC migration and monocyte adhesion to HUVECs through the inhibition of IL-6 and IL-8 production. We cannot conclude whether there are some other mechanisms in participation of the above process. Hence, further experiments should be performed to support these conclusions.
NF-κB is the primary transcription factor mainly involved in regulating inflammatory and immune responses to extracellular stimulus. Upon activated, NF-κB (p65) dissociates from its inhibitory protein IκB-α and translocates from the cytosol into the nucleus [33], where NF-κB binds to related DNA elements and activates its target genes such as IL-6 and IL-8 [34]. To exploit the inhibitory mechanism of IL-6 and IL-8 production in HUVECs, we tested the effect of geniposide on NF-κB activation and IκB-α degradation. In fact, the levels of either cytoplasmic IκB-α or nuclear NF-κB p65 were markedly decreased in LPS-induced HUVECs as a result of geniposide pretreatment, suggesting that the inhibitory effect of geniposide on NF-κB is mediated through its impact on IκB-α degradation, thereby decreasing the nuclear translocation of NF-κB. A similar phenomenon was found in studies by Huang et al. [35] who reported that penta-acetyl geniposide exerted an inhibitory effect on NF-κB activation in glioma cells.
P38 MAPK and ERK1/2, the well-characterized members of MAPK family, elicit many cellular functions in physiology and human diseases [36]. Our studies showed that LPS (100 ng/ml) induced the phosphorylation of p38 MAPK and ERK1/2 in HUVECs, while geniposide pretreatment (25–100 μg/ml) strikingly suppressed the phosphorylated levels of both MAPKs. Previous studies have evidenced that p38 MAPK and ERK1/2 are upstream regulators of NF-κB protein in activated HUVECs and NF-κB activation is mediated, at least in part, by phosphorylation of the two MAPKs [37]. In our preliminary studies, the specific p38 MAPK inhibitor, SB203580, and ERK1/2 inhibitor, PD98059, could not only suppress NF-κB activation to a certain extent, but directly down-regulate over-expression of IL-6 and IL-8 in HUVECs [38], (to be published). Furthermore, in the present study, SB203580 and PD98059 pretreatment almost completely inhibited LPS-induced HUVEC migration. Collectively, the reduced expression of phosphorylated-p38 and ERK1/2 after geniposide pretreatment may have prevented NF-κB activation, decreased IL-6 and IL-8 production and consequent HUVEC migration.
The effective concentrations for geniposide (25–100 μg/ml) in this study seem relatively high. To our knowledge, there are no in vivo studies on the pharmacokinetics of geniposide, therefore we cannot conclude whether the effective concentrations are physiological relevant, and this should be investigated in future studies.
Taken together, the present study demonstrates that geniposide inhibited the expression of IL-6 and IL-8 in HUVECs induced by LPS at the transcription and translation levels. Moreover, geniposide suppressed LPS-induced HUVEC migration and U937 monocyte adhesion to HUVECs. Signal transduction studies suggest that geniposide blocked activation of NF-κB, degradation of IκB-α, and phosphorylation of p38 MAPK and ERk1/2 in HUVECs challenged by LPS. A further investigation shows that LPS-induced HUVEC migration was suppressed by pretreatment with specific p38 MAPK and ERK1/2 inhibitors. Our studies point towards a potential cellular role for geniposide in vascular inflammation and illustrate the novel signal transduction mechanisms of geniposide in regulating endothelial cell function.
References
Tuo QH, Wang C, Yan FX, Liao DF. MAPK pathway mediates the protective effects of onychin on oxidative stress-induced apoptosis in ECV304 endothelial cells. Life Sci. 2004;76:487–97.
Altman R, Motton DD, Kota RS, Rutledge JC. Inhibition of vascular inflammation by dehydroepiandrosterone sulfate in human aortic endothelial cells: roles of PPARalpha and NF-kappaB. Vascul Pharmacol. 2008;48:76–84.
Li HL, He Y, Zhang JJ, Sun SH, Sun BG. Lipopolysaccharide regulates toll-like receptor 4 expression in human aortic smooth muscle cells. Cell Biol Int. 2007;31:831–5.
Anand AR, Cucchiarini M, Terwilliger EF, Ganju RK. The tyrosine kinase Pyk2 mediates lipopolysaccharide-induced IL-8 expression in human endothelial cells. J Immunol. 2008;180:5636–44.
Weglarz L, Dzierzewicz Z, Skop B, Orchel A, Parfiniewicz B, Wiśniowska B, et al. Desulfovibrio desulfuricans lipopolysaccharides induce endothelial cell IL-6 and IL-8 secretion and E-selectin and VCAM-1 expression. Cell Mol Biol Lett. 2003;8:991–1003.
Hashimoto S, Gon Y, Matsumoto K, Maruoka S, Takeshita I, Hayashi S, et al. Selective inhibitor of p38 mitogen-activated protein kinase inhibits lipopolysaccharide-induced interleukin-8 expression in human pulmonary vascular endothelial cells. J Pharmacol Exp Ther. 2000;293:370–5.
Mantovani A, Bussolino F, Introna M. Cytokine regulation of endothelial cell function: from molecular level to the bedside. Immunol Today. 1997;18:231–40.
Chen QC, Zhang WY, Kim H, Lee IS, Ding Y, Youn UJ et al. Effects of gardeniae fructus extract and geniposide on promoting ligament cell proliferation and collagen synthesis. Phytother Res (in press) 2009. doi: 10.1002/ptr.2839.
Liu JH, Yin F, Guo LX, Deng XH, Hu YH. Neuroprotection of geniposide against hydrogen peroxide induced PC12 cells injury: involvement of PI3 kinase signal pathway. Acta Pharmacol Sin. 2009;30:159–65.
Liu J, Yin F, Zheng X, Jing J, Hu Y. Geniposide, a novel agonist for GLP-1 receptor, prevents PC12 cells from oxidative damage via MAP kinase pathway. Neurochem Int. 2007;51:361–9.
Wang SW, Lai CY, Wang CJ. Inhibitory effect of geniposide on aflatoxin B1-induced DNA repair synthesis in primary cultured rat hepatocytes. Cancer Lett. 1992;65:133–7.
Peng CH, Huang CN, Hsu SP, Wang CJ. Penta-acetyl geniposide-induced apoptosis involving transcription of NGF/p75 via MAPK-mediated AP-1 activation in C6 glioma cells. Toxicology. 2007;238:130–9.
Liaw J, Chao YC. Effect of in vitro and in vivo aerosolized treatment with geniposide on tracheal permeability in ovalbumin-induced guinea pigs. Eur J Pharmacol. 2001;433:115–21.
Wu SY, Wang GF, Liu ZQ, Rao JJ, Lü L, Xu W, et al. Effect of geniposide, a hypoglycemic glucoside, on hepatic regulating enzymes in diabetic mice induced by a high-fat diet and streptozotocin. Acta Pharmacol Sin. 2009;30:202–8.
Suzuki Y, Kondo K, Ikeda Y, Umemura K. Antithrombotic effect of geniposide and genipin in the mouse thrombosis model. Planta Med. 2001;67:807–10.
Koo HJ, Lee S, Shin KH, Kim BC, Lim CJ, Park EH. Geniposide, an anti-angiogenic compound from the fruits of Gardenia jasminoides. Planta Med. 2004;70:467–9.
Lee P, Lee J, Choi SY, Lee SE, Lee S, Son D. Geniposide from Gardenia jasminoides attenuates neuronal cell death in oxygen and glucose deprivation-exposed rat hippocampal slice culture. Biol Pharm Bull. 2006;29:174–6.
Unger RE, Krump-Konvalinkova V, Peters K, Kirkpatrick CJ. In vitro expression of the endothelial phenotype: comparative study of primary isolated cells and cell lines, including the novel cell line HPMEC-ST1.6R. Microvasc Res. 2002;64:384–97.
Shen J, DiCorleto PE. ADP stimulates human endothelial cell migration via P2Y1 nucleotide receptor-mediated mitogen-activated protein kinase pathways. Circ Res. 2008;102:448–56.
Galley HF, Dhillon JK, Paterson RL, Webster NR. Effect of ciprofloxacin on the activation of the transcription factors nuclear factor kappaB, activator protein-1 and nuclear factor-interleukin-6, and interleukin-6 and interleukin-8 mRNA expression in a human endothelial cell line. Clin Sci (Lond). 2000;99:405–10.
Ozes ON, Mayo LD, Gustin JA, Pfeffer SR, Pfeffer LM, Donner DB. NF-kappaB activation by tumour necrosis factor requires the Akt serine–threonine kinase. Nature. 1999;401:82–5.
Hippenstiel S, Soeth S, Kellas B, Fuhrmann O, Seybold J, Krüll M, et al. Rho proteins and the p38-MAPK pathway are important mediators for LPS-induced interleukin-8 expression in human endothelial cells. Blood. 2000;95:3044–51.
Rietschel ET, Brade H. Bacterial endotoxins. Sci Am. 1992;267:54–61.
Endo S, Inada K, Inoue Y, Kuwata Y, Suzuki M, Yamashita H, et al. Two types of septic shock classified by the plasma levels of cytokines and endotoxin. Circ Shock. 1992;38:264–74.
Desai TR, Leeper NJ, Hynes KL, Gewertz BL. Interleukin-6 causes endothelial barrier dysfunction via the protein kinase C pathway. J Surg Res. 2002;104:118–23.
Noda A, Kinoshita K, Sakurai A, Matsumoto T, Mugishima H, Tanjoh K. Hyperglycemia and lipopolysaccharide decrease depression effect of interleukin 8 production by hypothermia: an experimental study with endothelial cells. Intensive Care Med. 2008;34:109–15.
Oh GS, Pae HO, Choi BM, Lee HS, Kim IK, Yun YG, et al. Penta-O-galloyl-beta-d-glucose inhibits phorbol myristate acetate-induced interleukin-8 [correction of intereukin-8] gene expression in human monocytic U937 cells through its inactivation of nuclear factor-kappaB. Int Immunopharmacol. 2004;4:377–86.
Kaplanski G, Teysseire N, Farnarier C, Kaplanski S, Lissitzky JC, Durand JM, et al. IL-6 and IL-8 production from cultured human endothelial cells stimulated by infection with Rickettsia conorii via a cell-associated IL-1 alpha-dependent pathway. J Clin Invest. 1995;96:2839–44.
Koo HJ, Lim KH, Jung HJ, Park EH. Anti-inflammatory evaluation of gardenia extract, geniposide and genipin. J Ethnopharmacol. 2006;103:496–500.
Malinda KM, Sidhu GS, Banaudha KK, Gaddipati JP, Maheshwari RK, Goldstein AL, et al. Thymosin alpha 1 stimulates endothelial cell migration, angiogenesis, and wound healing. J Immunol. 1998;160:1001–6.
Thevenard J, Ramont L, Devy J, Brassart B, Dupont-Deshorgue A, Floquet N et al. The YSNSG cyclopeptide derived from tumstatin inhibits tumor angiogenesis by down-regulating endothelial cell migration. Int J Cancer (in press) 2009. doi:10.1002/ijc.24688.
Liu J, Li X, Yue Y, Li J, He T, He Y. The inhibitory effect of quercetin on IL-6 production by LPS-stimulated neutrophils. Cell Mol Immunol. 2005;2:455–60.
Sun DI, Nizamutdinova IT, Kim YM, Cai XF, Lee JJ, Kang SS, et al. Bisacurone inhibits adhesion of inflammatory monocytes or cancer cells to endothelial cells through down-regulation of VCAM-1 expression. Int Immunopharmacol. 2008;8:1272–81.
Ponce C, Torres M, Galleguillos C, Sovino H, Boric MA, Fuentes A, et al. Nuclear factor kappaB pathway and interleukin-6 are affected in eutopic endometrium of women with endometriosis. Reproduction. 2009;137:727–37.
Huang HP, Shih YW, Wu CH, Lai PJ, Hung CN, Wang CJ. Inhibitory effect of penta-acetyl geniposide on C6 glioma cells metastasis by inhibiting matrix metalloproteinase-2 expression involved in both the PI3K and ERK signaling pathways. Chem Biol Interact. 2009;181:8–14.
Johnson GL, Lapadat R. Mitogen-activated protein kinase pathways mediated by ERK, JNK, and p38 protein kinases. Science. 2002;298:1911–2.
Nizamutdinova IT, Oh HM, Min YN, Park SH, Lee MJ, Kim JS, et al. Paeonol suppresses intercellular adhesion molecule-1 expression in tumor necrosis factor-α-stimulated human umbilical vein endothelial cells by blocking p38, ERK and nuclear factor-κB signaling pathways. Int Immunopharmacol. 2007;7:343–50.
Li XY, He JL, Liu HT, Li WM, Yu C. Tetramethylpyrazine suppresses interleukin-8 expression in LPS-stimulated human umbilical vein endothelial cell by blocking ERK, p38 and nulear factor-kappaB signaling pathways. J Ethnopharmacol. 2009;125:83–9.
Acknowledgments
This work was supported by the Natural Science Fund of Chongqing, China (KJ070304), and by the Science Fund of Chongqing Medical University (XBED200806).
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: M. Katori.
Rights and permissions
About this article
Cite this article
Liu, HT., He, JL., Li, WM. et al. Geniposide inhibits interleukin-6 and interleukin-8 production in lipopolysaccharide-induced human umbilical vein endothelial cells by blocking p38 and ERK1/2 signaling pathways. Inflamm. Res. 59, 451–461 (2010). https://doi.org/10.1007/s00011-009-0118-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-009-0118-3