Abstract
Right ventricular (RV) dysfunction harbingers adverse prognosis in pulmonary arterial hypertension (PAH). Although conventional two-dimensional echocardiography (2DE) is limited for RV systolic function quantitation, RV strain can be a useful tool. The diagnostic and prognostic impact of 2DE speckle-tracking RV longitudinal strain was evaluated, including other 2DE systolic indexes, in a group of PAH patients without severe impairment of functional capacity, chronic pulmonary thromboembolism or left ventricular dysfunction. Sixty-six group I PAH patients, 67 % NYHA functional class I or II (none in IV) were studied by 2DE to obtain: RV fractional area change, tricuspid annular plane systolic excursion, RV myocardial performance index, tissue Doppler tricuspid annulus systolic velocity. Global, free wall (RVFreeWSt) and septal RV longitudinal systolic strain were obtained. RV ejection fraction by cardiac magnetic resonance (CMR-RVEF) was also assessed. All patients were followed up to 3.9 years (mean 3.3 years). Combined endpoints were hospitalization for worsening PAH or cardiovascular death. Among all the 2DE indexes of RV systolic function, RVFreeWSt exhibited the best correlation with CMR-RVEF (r = 0.83; p < 0.005). Combined endpoints occurred in 15 (22.7 %) patients (6 hospitalizations and 9 deaths). Multivariate analysis identified RVFreeWSt ≤−14 % as the only 2DE independent variable associated with combined endpoints [HR 4.66 (1.25–17.37); p < 0.05]. We conclude that RVFreeWSt may be a suitable non-geometric 2DE surrogate of CMR-RVEF in PAH patients, constituting a powerful independent predictor of long-term outcome in this cohort with relatively preserved functional capacity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary arterial hypertension (PAH) comprises a special subset of patients with higher prevalence and degree of right ventricular (RV) dysfunction, resulting in more adverse prognosis with increased morbidity and mortality [1, 2]. Accurate non-invasive assessment of RV function is essential to proper clinical management of these patients.
The peculiar geometry and anatomic features of the RV systolic function jeopardizes its quantitative non-invasive evaluation. Its semilunar crescent shape does not allow the use of established formulas and algorithms by means of conventional two-dimensional Doppler echocardiography (2DE), requiring customized approaches to volumetric evaluation by several modalities of cardiac imaging [3].
Many 2DE indexes have been proposed to quantitatively evaluate RV systolic function, including RV fractional area change (RV-FAC), tricuspid annular plane systolic excursion (TAPSE), RV myocardial performance index (RV-MPI) and tissue Doppler-derived tricuspid lateral annular systolic velocity (RV-s’) [4, 5]. Lately, the RV longitudinal systolic strain, a novel approach to RV regional and global systolic function assessment based on RV deformation analysis utilizing 2DE speckle-tracking, has emerged with consistent results in characterizing RV dysfunction [6, 7].
Studies concerning the evaluation of echocardiographic indexes in PAH patients to assess RV dysfunction, including RV strain, have been previously published. Certain studies described significant correlation of RV longitudinal systolic strain with RV ejection fraction (RVEF) derived from cardiac magnetic resonance (CMR), including patients with chronic pulmonary thromboembolism [8–10]. Others pointed the relationship between RV dysfunction assessed by strain and functional capacity in predominantly class III–IV NYHA patients [11].
Several other studies reported the prognostic role of RV longitudinal systolic strain in patients with PAH, including significant proportion of advanced NYHA functional class (III/IV) individuals [11, 12], group IV PAH patients (chronic thromboembolism) [13–16] and low left ventricular (LV) ejection fraction [14], conditions that may affect long-term outcome. In another study, patients were followed for a relative short period of time [15].
Due to the clinical relevance of RV dysfunction in PAH patients, further information is necessary regarding the relationship between echocardiographic indexes, functional capacity and the late prognosis of less impaired patients, without associated pulmonary thromboembolism or LV dysfunction. Therefore, the purpose hereof was to compare RV strain and others 2DE indexes of RV systolic function with RVEF derived from CMR and to evaluate the long-term prognostic role of RV systolic strain in a more homogenous group I PAH patients [17] with normal LV ejection fraction and relatively preserved functional capacity.
Materials and methods
Patients
Sixty-six patients of group I PAH (defined as mean pulmonary arterial pressure ≥25 mmHg and pulmonary capillary wedge pressure ≤15 mmHg during right heart catheterization) were selected, recruited from a tertiary center. The PAH diagnosis was made according to the current evidence-based guidelines [17]. Only patients ≥18 years old in the stable course of the disease were included, defined as functional class ≤III (NYHA), no physical signs or symptoms of overt RV failure, and ability to perform 6-min walk test. The following patients were excluded patients with cardiac rhythm other than sinus rhythm; previous pacemaker lead implant; pregnancy; LV systolic dysfunction (2DE LV ejection fraction ≤0.50); LV diastolic dysfunction ≥grade II; coronary heart disease; significant mitral or aortic valve disease; congenital heart disease; functional class IV (NYHA) at clinical selection; and patients with poor 2DE imaging.
Twenty-five healthy volunteers were studied, paired by gender, age and body surface area as control. The PAH and control groups underwent a comprehensive 2DE study with speckle tracking derived RV longitudinal systolic strain; 44 of such 66 patients were also evaluated by CMR. The PAH group performed a standard 6 min walk test.
All patients provided informed consent and the protocol study was approved by the institutional review board.
Echocardiography
All individuals were submitted to a comprehensive 2DE with a GE Vivid 7 echocardiography system with a 1.5–4.3 MHz phase array transducer under continuous electrocardiographic monitoring. Individuals were studied in the left lateral decubitus position and always by the same level 3 echocardiographer. Sector width, gain and gray scale were adjusted to ensure adequate imaging of cardiac chambers and endocardial borders, as well as appropriate frame rate to allow analysis of RV strain by speckle tracking. The quantification of the cardiac chambers was performed according to the American Society of Echocardiography guidelines [4, 5]. LV biplane ejection fraction was calculated according to a modified Simpson’s rule. RV systolic function was estimated by: RV-FAC calculated as (RV diastolic area − RV systolic area)/(RV diastolic area) × 100 %, from apical views; TAPSE obtained by M-mode sweep of the lateral tricuspid annulus; RV-s’ and RV-MPI were obtained from the lateral tricuspid annulus tissue Doppler spectral tracings [5].
Systolic pulmonary artery pressure (SPAP) was estimated by continuous Doppler assessment of maximal tricuspid regurgitant jet velocity and adding the estimated RA pressure inferred by inferior vena cava diameter and respiratory changes [18]. Pulmonary vascular resistance (PVR-echo) was estimated by the relationship of maximal tricuspid regurgitant jet velocity and pulmonary flow integral [19]. RV diastolic function was evaluated by pulsed Doppler analysis of early (E) and late (A) diastolic tricuspid flow velocities and by tissue Doppler recording of peak early (e′) tricuspid lateral annular velocity. Such data were used to calculate the tricuspid E/e′ ratio (Tr E/e′) as an estimation of RV filling pressures [20].
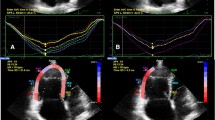
The RV strain was determined by 2DE speckle–tracking: four cycles RV oriented apical views were transferred to offline analysis (GE EchoPAC GE Healthcare); the necessary RV points of reference were signaled using a point and click technique with manual adjustments when deemed necessary to ensure proper software tracking and recognition of RV wall boundaries. The RV was divided in six segments (basal, mid and apical RV free wall and septal segments). Six curves of strain × time were obtained and the maximal RV free wall longitudinal systolic strain (RVFreeWSt), RV septum longitudinal systolic strain (RVSepSt) and RV global longitudinal systolic strain (RVGlSt) were obtained. A reference point was set at the onset of the QRS complex of the superimposed ECG [12] for all measurements.
Cardiac magnetic resonance imaging
Forty-four patients of the PAH group (PAH-CMR group) and 19 patients of the control group underwent CMR in a Magnetom Avanto 1.5 T equipment (Siemens Health Care, Erlangen Germany) within a period of 3 days to obtain an independent assessment of the RV systolic function. The imaging acquisition protocol consisted of thoracic orthogonal three-plane location followed by HASTE sequencing (Half Fourier Acquisition Single Shot Turbo Spin Echo) to obtain thoracic axial views and pulmonary artery diameter evaluation. Cine CMR with oblique views of the heart were obtained to evaluate LV long axis (4-chamber, 2-chamber and 3-chamber views) and RV long axis (4-chambers, 2-chambers and RV outflow views); short axis stacks to evaluate morphology as well as global and segmental biventricular function. Post-processing and global biventricular function analysis was achieved by volumetric Simpson method utilizing the software Cvi42, to obtain RV ejection fraction (CMR-RVEF).
Six-minute walk test all patients from the PAH group were submitted to a 6-min walk test in a 30-m long corridor, according to the American Thoracic Society Guidelines [21].
Clinical follow-up and endpoints the PAH Group patients were followed up to 3.9 years. The combined endpoint was hospitalization for worsening of PAH or cardiovascular death.
Statistical analysis
Statistical analysis was performed with SPSS 13.0 software (SPSS Inc.,Chicago, IL). Continuous data are presented as mean ± SD values and categorical data are reported as percentage. Chi square test was used to compare categorical variables. Non-paired “t” test was used to compare PAH and control groups. Pearson’s correlation coefficient was used to assess the level of association between 2DE variables and CMR-RVEF. Receiver operating characteristic curve analysis was used to establish cut-offs to indicate higher risk of morbidity-mortality. Clinical and 2DE RV systolic function variables which have been related to prognosis in PAH were included in a uni and multivariate model and the forward conditional method was used to define independent predictors of clinical endpoints (univariate and multivariate Cox proportional risk analysis). Survival curves were derived by the Kaplan–Meier method and groups were compared by log-rank test. A statistical significance of 0.05 was used for all tests.
Results
Clinical and hemodynamic data
The baseline clinical characteristics of PAH group and control are listed in Table 1. There were no significant differences between PAH and control groups in gender, age and body surface area. The patients of the PAH group were taking medications to manage PAH at the time of selection for the study on advise of the referring physician. Two-thirds (67 %) of the patients were in NYHA functional class I or II. None of the patients was in NYHA functional class IV.
Hemodynamic data as well as 6-min walk test results are displayed in Table 1.
Echocardiographic findings
All 2DE data from PAH and control groups are demonstrated in Table 2. The LV ejection fraction was normal in all individuals. The SPAP and pulmonary vascular resistance in the PAH group were significantly higher. Right chambers and inferior vena cava diameter were significantly larger in PAH group as compared to control. All the conventional 2DE RV systolic function variables (RV-FAC, TAPSE, RV-MPI, RV-s’) were significantly worse in the PAH group. The Tr E/e’ ratio was significantly higher in PAH patients.
The three RV longitudinal systolic strain values (global, free wall and septal) of the PAH group were also significantly lower than controls.
CMR findings
In the 44 patients of the PAH-CMR group, the CMR-RVEF was 39 ± 12 %, significantly lower than the CMR-RVEF in 19 individuals of the control group (63 ± 9 %; p < 0.005). Except for RV-s’, all echocardiographic variables of RV systolic function significantly correlated with RVEF assessed by CMR in the PAH-CMR group (Table 3). The best correlation was observed with RVFreeWst (Fig. 1). RVFreeWSt less negative than −18 % was associated with CMR-RVEF ≥ 0.45 (p < 0.05).
Long-term follow-up results
The average follow-up period was 3.3 years with maximum duration of 3.9 years. The combined endpoint occurred in 15 patients (22.7 %): hospitalization for worsening PAH in 6 (9.1 %) and cardiovascular death in 9 (13.6 %) patients.
Univariate analysis showed significant relation of NYHA functional class, RVFreeWSt, RVGlSt, and RV-FAC with the combined endpoints, particularly with RVGlSt and RVFreeWSt (Table 4). A tendency was observed with the 6-min walk test. There was no relation between endpoints and the variables RV-MPI, RV-s’, SPAP and PVR-echo.
The multivariate analysis demonstrated that RVFreeWSt emerged as the only echocardiographic variable independently associated with the combined endpoint (Table 5). The NYHA class III was also independently related to the combined outcomes. The relatively small number of patients did not allow assessing the combined effect of both variables. The 6-min walk test was not independently related to the endpoints.
The RVFreeWSt cut-off value was −14 %. Only patients with RVFreeWst values less negative than −14 % had deterioration of clinical status, resulting in hospital admission or cardiovascular related death. Those with RVFreeWSt less negative than −14 % had a chance of 4.6 times more events than patients with more negative values of this index.
Kaplan-Meyer curve displayed in the Fig. 2 shows the effect of lower values of RVFreeWSt in the event-free medical evolution of PAH patients with relatively preserved functional capacity. Values of RVFreeWSt ≤−14 % were significantly associated with poor outcome.
Discussion
This study reports the long-term prognostic value of RVFreeWSt in predominantly oligo or asymptomatic patients (2/3 in NYHA functional class I or II), with significant PAH and variable degrees of RV function impairment as assessed by 2DE and CMR-RVEF. Additionally, our results also confirm previous data about the high correlation between RVFreeWSt and RVEF derived from CMR and reinforce the diagnostic value of this non-geometric index for RV systolic function.
Only patients with PAH characterized by elevated pulmonary vascular resistance secondary to precapillary forms of PAH (group I) were studied; patients with pulmonary venous hypertension, chronic respiratory disease and chronic thromboembolic disease were excluded, which may have different prognostic implications.
The RV dysfunction associated with heart failure in patients with PAH is the single most important factor leading to increased morbidity, mortality and adverse prognosis [22]. For those with relatively preserved functional capacity and less severe impairment of RV systolic function, it would be useful and clinically relevant to have a RV systolic echocardiographic index with prognostic capabilities, in order to improve early therapeutic procedures.
Comparison between CMR-RVEF and echocardiographic indexes of RV systolic function
The study revealed significant correlation between conventional (RV-FAC, TAPSE, RV-MPI), as well new indexes (RV strain) of RV systolic function and RVEF determined by CMR. Notwithstanding, RVGlSt and RVFreeWSt had the higher correlation indexes with the CMR-RVEF.
Conventional 2DE, despite its wide availability, still has limitations concerning RV systolic function evaluation, remaining uncertainties about the choice of the best 2DE parameter to be used on a daily practice. The American Society of Echocardiography guidelines recommend the use of multiple indexes to avoid misevaluation and improper overlooking of serious risk-prone patients [5]. The peculiar RV shape may limit accurate volumetric measurement and RVEF calculation. The LV twisting motion can compromise accuracy of the RV-FAC estimation due to possible differences in tomographic plane between systolic and diastolic RV frames [23]. Related problems are also encountered when TAPSE is measured, affected by transducer position and cardiac translation; also, TAPSE evaluates only the basal RV systolic function [23]. Tissue Doppler derived RV-s’ is also affected by Doppler transducer position (cursor alignment) and overall heart motion; as TAPSE, it only evaluates the basal RV function. RV-MPI is affected by elevated RA pressure, common place in PAH patients, that shortens right ventricular isovolumetric relaxation time producing falsely low values [24].
Non-volumetric assessment of RV systolic by 2DE speckle-tracking emerged as a useful tool with relatively low intra and interobserver variability [25], with high correlation with CMR-RVEF [10], as observed by us in PAH patients. The diagnostic superiority of longitudinal RV strain in RV function evaluation may be explained by the RV muscle fibers running in a longitudinal fashion, unlike in the LV, providing contraction in the longitudinal plane with the base of the RV moving toward the apex in systole [26]. The amount of RV free wall longitudinal deformation (strain) is an angle-independent sensitive measure of global and regional myocardial contractility, distinguishing true contractility of the wall from translational motion, a potential concern regarding M-mode and 2DE measurements of the longitudinal contraction [16]. Moreover, for PAH patients, the RV strain can potentially detect RV fibrosis confirmed by computed tomography [27] that may contribute to overt or silent impairment of RV systolic function with possible clinical and prognostic implications.
Prognostic value of RV longitudinal systolic strain in PAH patients with relatively preserved functional capacity
RVFreeWSt was the most powerful independent 2DE RV systolic function variable that identified high-risk PAH patients prone to unfavorable outcomes resulting in hospital admission or death in the PAH group of the study, with predominant mild to moderate impairment of functional capacity. Considering that the RV dysfunction has a great prognostic impact in PAH patients and that RVFreeWSt reflects the RVEF-CMR, it is not surprising that this index was shown to be the best independent predictor of adverse endpoints in the study.
The cut-off point of unfavorable clinical course was RVFreeWSt values less negatives than −14 %. There was no event of either PAH-related hospitalization or death in the group of patients with RVFreeWSt values more negative than −14 % during the follow-up.
Other authors studying larger series of PAH patients described similar results concerning the RV strain and prognosis, but with different cut-off value of RVFreeWSt (−19 %) to identify those with poor outcome, partially related to differences in patient selection [14]. The role of RVFreeWSt in predicting events in PAH patients was also noticed by other authors in heterogeneous groups, including pulmonary thromboembolism [13], or more severely impaired patients including functional class IV [11, 13, 14, 28], or shorter follow-up [15]. In turn, this study was able to demonstrate the long-term prognostic strength of RVFreeWSt in a more uniform cohort of group I PAH patients with relatively preserved functional capacity.
The prognostic value of RV strain in the study was highlighted by the fact that a quite large proportion of patients studied was in mild degrees of functional status impairment (67 % in NYHA class I or II, none in class IV) and scored reasonably well in the 6-min walk test (431 ± 92 m). This is remarkable because previous studies with more functionally compromised patients (most of them in NYHA class III and IV) revealed the need to investigate RV longitudinal strain in patients with more preserved functional capacity to assess its usefulness as an outcome predictor [11, 28]. This study has adequately evaluated such features.
Functional class III NYHA was independently related to the combined endpoints in the group of patients. However, the performance in the 6-min walk test distance of 330 m did not unmask a subgroup of poor prognosis, unlike previous reports [29]. This fact might be related to the relatively preserved functional capacity, small number of patients and to fewer occurrences of events observed.
Establishing prognosis based on sporadic functional capacity evaluation scores, such as the 6-min walk test, remains controversial. While previous studies reported prognostic value for a lower baseline cut-off of 332 m in PAH patients [29], other authors were unable to identify a specific threshold for prognosis [30]. They also noticed that improvement in the 6-min walk test did not affect survival, although worsening of the 6-min distance over time was strongly associated with poor prognosis [30].
Clinical implications
The use of RVFreeWSt by 2DE speckle-tracking in the routine echocardiographic study is feasible, cost-effective and available in most diagnostic centers and hospitals, with good correlation with CMR-RVEF. For clinical purposes in PAH patients, the RVFreeWSt could be used as a non-geometric echocardiographic surrogate of CMR-RVEF particularly when CMR is not available. Considering PAH patients with relatively preserved functional status and stable clinical course, in this clinical setting, the RVFreeWSt could help to select those with high risk of poor outcomes that should benefit from closer follow-up and monitoring of therapy.
Limitations
A relatively small number of patients referred from a single institution were included in the study. All tests were run in a single echocardiographic machine (Vivid 7 GE). This still remains a limitation despite the fact that it was previously demonstrated reasonable correlation of strain values obtained offline from different vendor software [31]. As CMR-RVEF was not obtained in all 66 patients, this variable could not be included in the multivariate analysis. As a result, it is not possible to evaluate the role effectively played by this important index of RV systolic function in this clinical setting.
Conclusion
Right ventricular free wall strain analysis by 2DE speckle-tracking was the best non-geometric echocardiographic index reflecting CMR-derived RVEF in patients with group I PAH with variable degrees of RV impairment. Moreover, it has prognostic value in this patient population with relatively preserved functional capacity, and has emerged as the most powerful echocardiographic independent predictor of long-term outcome related to RV systolic function.
References
D’Alonzo GE, Barst RJ, Ayres SM et al (1991) Survival in patients with primary pulmonary hypertension. Results from a National Prospective Registry. Ann Intern Med 115:343–349
Rich S, Dantzker DR, Ayres SM et al (1987) Primary pulmonary hypertension. A national prospective study. Ann Intern Med 107:216–223
Cacciapuoti F (2009) Echocardiographic evaluation of right heart function and pulmonary vascular bed. Int J Cardiovasc Imaging 25:689–697
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Rudski LG, Lai WW, Afilalo J et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Puwanant S, Park M, Popovi´c ZB et al (2010) Ventricular geometry, strain, and rotational mechanics in pulmonary hypertension. Circulation 121:259–266
Meris A, Faletra F, Conca C et al (2010) Timing and magnitude of regional right ventricular function: a speckle tracking-derived strain study of normal subjects and patients with right ventricular dysfunction. J Am Soc Echocardiogr 23(8):823–831
Fukuda Y, Tanaka H, Sugiyama D et al (2011) Utility of right ventricular free wall speckle-tracking strain for evaluation of right ventricular performance in patients with pulmonary hypertension. J Am Soc Echocardiogr 24:1101–1108
Li Y, Xie M, Wang X, Lu Q, Fu M (2013) Right ventricular regional and global systolic function is diminished in patients with pulmonary arterial hypertension: a 2-dimensional ultrasound speckle tracking echocardiography study. Int J Cardiovasc Imaging 29:545–551
Freed BH, Tsang W, Bhave NM et al (2015) Right ventricular strain in pulmonary arterial hypertension: a 2D echocardiography and cardiac magnetic resonance study. Echocardiography 32:257–263
Sachdev A, Villarraga HR, Frantz RP et al (2011) Right ventricular strain for prediction of survival in patients with pulmonary arterial hypertension. Chest 139(6):1299–1309
Park JH, Kusunose K, Kwon DH et al (2015) Relationship between right ventricular longitudinal strain, invasive hemodynamics, and functional assessment in pulmonary arterial hypertension. Korean Circ J 45(5):398–407
Motoji Y, Tanaka H, Fukuda Y, Ryo K, Kawai H, Hirata K (2013) Efficacy of right ventricular free-wall longitudinal speckle-tracking strain for predicting long-term outcome in patients with pulmonary hypertension. Circ J 77:756–763
Haeck MLA, Scherptong RWC, Marsan NA et al (2012) Prognostic value of right ventricular longitudinal peak systolic strain in patients with pulmonary hypertension. Circ Cardiovasc Imaging 5:628–636
Fine NlM, Chen L, Bastiansen PM et al (2013) Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging 6:711–721
Giusca S, Dambrauskaite V, Scheurwegs C et al (2010) Deformation imaging describes right ventricular function better than longitudinal displacement of the tricuspid ring. Heart 96:281–288
Galie N, Humbert M, Vachiery J et al Guidelines for the diagnosis and treatment of pulmonary hypertension the task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) 2015, endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J. doi:10.1093/eurheartj/ehv317
Yock PG, Popp RL (1984) Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation 70(4), 657–662
Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ (2003) A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol 41:1021–1027
Sade LE, Gulmez O, Eroglu S, Sezgin A, Muderrisoglu H (2007) Noninvasive estimation of right ventricular filling pressure by ratio of early tricuspid inflow to annular diastolic velocity in patients with and without recent cardiac surgery. J Am Soc Echocardiogr 20(8):982–988
Crapo RO, Casaburi R, Coates AL et al (2002) American thoracic society ATS statement: guidelines for the 6-min walk test this official statement of the American Thoracic Society was approved by the ATS board of directors March 2002. Am J Respir Crit Care Med 166:111–117
McLaughlin VV, Presberg KW, Doyle RL et al (2004)Prognosis of pulmonary arterial hypertension accp evidence-based clinical practice guidelines. Chest 126:78S–92S
Badano LP, Ginghina C, Easaw J et al (2010) Right ventricle in pulmonary arterial hypertension: haemodynamics, structural changes, imaging, and proposal of a study protocol aimed to assess remodelling and treatment effects. Eur J Echocardiogr 11:27–37
Lindqvist P; Calcutteea A, Henein M (2008) Echocardiography in the assessment of right heart function Eur J Echocardiogr 9:225–234
Moaref A, Abtahi F, Aghasadeghi K, Shekarforoush S (2014) Right ventricular strain and strain rate in patients with systemic sclerosis without pulmonary hypertension. Arch Cardiovasc Imaging 2(3):e20735
Leather HA, Ama’ R, Missant C, Rex S, Rademakers FE, Wouters PF (2006) Longitudinal but not circumferential deformation reflects global contractile function in the right ventricle with open pericardium. Am J Physiol Heart Circ Physiol 290:H2369–H2375
Ozawa K, Funabashi N, Tanabe N et al (2014) Two-dimensional global longitudinal strain of right ventricle using transthoracic echocardiography can detect right ventricular fibrosis confirmed by 320 CT in pulmonary hypertension. Int J Cardiol 172:e320–e323
Hardegree EL, Sachdev A, Villarraga HR et al (2013) Role of serial quantitative assessment of right ventricular function by strain in pulmonary arterial hypertension. Am J Cardiol 111:143–148
Miyamoto S, Nagaya N, Satoh T et al (2000) Clinical correlates and prognostic significance of 6-min walk test in patients with primary pulmonary hypertension comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med 161:487–492
Farber HW, Miller DP, McGoon MD et al (2015) Predicting outcomes in pulmonary arterial hypertension based on the 6-min walk distance. J Heart Lung Transplant 34:362–368
Castel AL, Szymanski C, Delelis F et al (2014) Prospective comparison of speckle tracking longitudinal bidimensional strain between two vendors. Arch Cardiovasc Dis 107:96–104
Acknowledgements
The study was approved by the ethical review board of our institution, Escola Paulista de Medicina, Federal University of São Paulo—UNIFESP.
Author contributions
Augusto Alberto da Costa Junior, Jaquelina Sonoe Ota-Arakaki, Roberta Pulcheri Ramos, Marly Uellendahl, Frederico José Neves Mancuso, Manuel Adan Gil, Cláudio Henrique Fischer, Valdir Ambrosio Moises, Antonio Carlos de Camargo Carvalho, Orlando Campos takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the Authors has received research grants from any companies and all them declare that there were no conflicts of interests
Ethical approval
There were no animals involved in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
da Costa Junior, A.A., Ota-Arakaki, J.S., Ramos, R.P. et al. Diagnostic and prognostic value of right ventricular strain in patients with pulmonary arterial hypertension and relatively preserved functional capacity studied with echocardiography and magnetic resonance. Int J Cardiovasc Imaging 33, 39–46 (2017). https://doi.org/10.1007/s10554-016-0966-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0966-1