Abstract
The aim of this review was to describe the different ultrasonic modalities to non-invasively evaluate right cardiac chambers and pulmonary vascular bed function. M-Mode, 2-D, conventional pulsed doppler, tissue doppler imaging (TDI), strain rate imaging (SRI) and 3D echocardiography are illustrated in order to obtain both regional and global right heart and pulmonary function. The results have a good correlation with other invasive and non-invasive diagnostic techniques, as magnetic resonance imaging (MRI). All these echocardiograpic techniques can be employed to evaluate the morphologic and functional pictures of right heart and pulmonary circulation in presence of pulmonary hypertension (PH). The hemodynamic profile obtained consent to anatomically and functionally characterize PH. But, other experiences performed on more wide range of healthy and PH patients are necessary to confirm the described results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For long time, right heart chambers were judged such as cavities without any active function, placed between the venous systemic blood flow and the pulmonary vascular bed. But, recently both collected action and propulsive push of the right heart were remarked [1, 2]. Right ventricular cavity exhibits reduced walls’ thickness, as consequence of reduced loading in respect to the left ventricle (pulmonary resistances are about 1/6 towards these induced by systemic circulation). This cavity shows an inflow way (sinus) and an outflow tract (infundibulum), similarly to the left ventricle. Two ventricular parts are divided by the supraventricular crest and are connected respectively to the blood coming from the venous circulation (sinus) and the blood drawing to the pulmonary circulation (infundibulum). As consequence, in early systole the inflow tract contracts whereas its outflow tract expands and vice versa happens in late systole [3].
Microscopically, right ventricular walls predominantly consist of longitudinal fibers present in the epicardial zone, and radial fibers constituting the endocardial zone. This unlike orientation of myocardial fibers produces longitudinal motion (see in long-axis approach) and radial motion (see in short axis view) during systole [4]. The morphological (irregular shape and trabeculations) and functional complexity of right ventricle give rather difficult their volumes and EF% calculation. These parameters are usually evaluated by echocardiography. The normal echocardiographic values of main indexes of right structures (atrium and ventricle) are reported in Table 1 [5].
M-Mode echocardiography performed in parasternal long or short axis view, is used to measure RVEDD in mm. and walls’ thickness of RV in mm. The normal RV is approximately two thirds of the LV size. RVOT is evaluated by 2D echocardiography in parasternal short-axis view alone, by measuring the distance between the aortic root and the wall of the pulmonary truncus [6, 7]. Tricuspid annular plane systolic excursion (TAPSE) is a relatively new echocardiographic RV parameter, indicating the displacement of tricuspid annular plane in systole. It is obtained in long-axis view in M-Mode echocardiography, placing the sample-volume at level of lateral tricuspid annulus under B-Mode echocardiography’s guidance (Fig. 1a, b). TAPSE is related to RVEF% obtained with radionuclide methods. A value >15 mm indicates the normal systolic RV function, whereas a value <8 mm is connected with the significant RV dysfunction [8]. The degree of TAPSE approximately corresponds with RVEF%; 5 mm = 20% EF; 10 mm = 30% EF; 15 mm = 40% EF; 20 mm = 50% EF. The correspondence between TAPSE and RVEF% calculated from radionuclide angiography (judged as the standard method for assessing the right ventricular ejection fraction) depends of ability of the radionuclide method to evaluate the complex geometry of the right ventricle. In a recent study comparing TAPSE and radionuclide angiography, Ueti and colleagues confirm that this diagnostic technique can be considered the “gold standard” for assessing RVEF, because the obtained values not depend on the complex geometry of the right ventricle [9].
RA area is obtained in apical 2D-four chamber view, as the product between longitudinal and transverse side. Its normal value is equal to 13 ± 2 cm2, but it also depends for right atrial pressure, BMI, and age or sex.
Right atrial pressure is appraised from the inferior vena cava (IVC) diameter and its inspiratory collapse [10], detected by subcostal view. The diameters of IVC, % of inspiratory IVC collapse and the corresponding values of RA pressure are reported (Fig. 2).
From the matched values of IVC diameter and its inspiratory collapse, it is possible to estimate RA pressure. Right atrial pressure must be added to calculated value of tricuspid insufficiency (eventually present), for estimate systolic pulmonary pressure (PAPs).
Usually, atrial filling happens from the point of minimal atrial volume until the onset of atrial systole. This phase starts at tricupid valve opening. On the contrary, atrial empying happens from maximal to minimal right atrial volume. Two phases of atrial emptying were described: passive emptying, occurring during ventricular diastole, and active emptying, occurring during atrial contraction. Emptying times progressively change with increasing age in healthy subjects. In fact right atrial passive emptying volume and passive emptying fraction decrease with age, whereas active empting volume and active right atrial ejection fraction increase with advancing age. This could indicate that with increasing age right ventricular diastolic function deceases [11].
These results are not without any impact in patients with pulmonary arterial hypertension (PH) and are important in the impact of age with some diseases, as chronic pulmonary diseases, pulmonary embolism, right ventricular infarction, chronic heart failure, atrial fibrillation, etc.
The main echocardiographic parameters evaluated in the pulmonary artery are:
Systolic pressure in pulmonary artery (PAPs), obtaining in presence of tricuspid valvular incompetence only, adding PARm to velocity of tricuspid insufficiency (corrected by Bernoulli formula):
in which: PAPs = systolic pressure in pulmonary artery; PARm = mean pressure in right atrium (estimated by IVC); 4V2 tricuspid max, i.e. velocity2 of tricuspid regurgitant jet × 4 (in accordance with modified Bernoulli equation). Doppler-derived PAPs critically depends upon age, body mass index and right atrial pressure. A value >30 mmHg indicates a condition of pulmonary hypertension (PH).
Diastolic arterial pressure (PAPd) can be calculated when the pulmonary valvular regurgitation is present, from the formula:
where PAPd = diastolic arterial pulmonary pressure; PR end diast. = end diastolic pulmonary regurgitant jet detected with continuous wave Doppler. It is obtained as the pulmonary regurgitant flow at end-diastole (Fig. 3).
Mean pulmonary artery pressure (PAPm), evaluated as:
where the values of PAPd and PAPs are previously reported.
A value of PAPs > 35 mmHg at rest, of PAPd > 15 mmHg and PAPm = 25 mmHg corresponds to PH.
Among the pulmonary pressures (systolic, diastolic, mean), PAPs is more frequently evaluated for its importance in to estimate maximal systolic pulmonary pressure. In a study investigating the relationship between PAPs and age, Ueda et al. [12] in healthy aged subjects found an increased value compared with that recorded in younger healthy subjects. This different behaviour seems to be reported to the changes of the senile lungs, characterized by a homogeneous enlargement of the alveolar airspaces without fibrosis or destructions of alveolar walls [13, 14]. Elevated PAPs in the elderly are also correlated with the thickness of the RV outflow tract wall. This is also attributed to an increase in pulmonary vascular resistance and decrease LV compliance. Usually, PAPs increases of 0.8 mmHg per decade in over 50 years of age controls. In connection to sex, McQuillan et al. indicated that PAPs is significantly higher in men than in women. BMI and obesity also induce an increase of PAPs in absence of any condition of pulmonary hypertension. Finally, a positive association between PAPs and posterior wall thickness was described [15].
Mean PAP (mPAP) > 25 mmHg at rest or >30 mmHg during exercise truly indicates pulmonary hypertension (PH). This condition corresponds to sPAP > 36 mmHg. Friedberg et al. [16] hypothesized that sPAP correlates with dPAP and mPAP. This correlation can be used to estimate diastolic and mean PAP from Doppler data (PAPs).
The previously reported mPAP formula:
implies that knowing the minimal and maximal values of the pressure signal allows a precise estimation of the mean pressure. In the formula: dPAP may reflect vascular tone, whereas sPAP depends on pulmonary artery compliance, and right ventricular ejection.
An invasive study also demonstrated that sPAP alone may estimate mPAP, without the need to include dPAP, for a linear relationship between mPAP and sPAP [17]. This implies that sPAP obtained by doppler flow (in presence of tricuspid regurgitation) may directly estimate mPAP and so a condition of PH.
In addition, increasing evidence from clinical studies emphasizes the importance of evaluating pulmonary artery flow and RV function during 2-D stress echocardiography. Stress echo can be performed with bicycle or treadmill test; hypoxia or pharmacologic tests can also be employed. In healthy individuals, the adaptation to exercise includes an increase in stroke volume, heart rate, and cardiac output, with minimal increase in PAPm and PVR. Values of doppler-derived systolic PAP have been reported to be <40–45 mmHg in healthy individuals [18]. Exercise echocardiography may uncover abnormal increases in pulmonary pressure and cardiac output. These parameters are further impaired in patients with resting pulmonary hypertension (PH), such as in scleroderma [19] and in thrombo-embolic pulmonary disease. It is also important in patients with right coronary artery disease, for evaluate right ventricular wall motion in ischemic patients. In these individuals, stress induces a decrease in RV function or RV asynergy [20, 21]. In detail, patients with inferoposterior MI have 50% RV involvement. In patients with acute RV infarction, severe hemodynamic compromise arises when both RV free wall and septum are involved. In turn, RV dysfunction leads to an elevated RV end-diastolic pressure, that shifts the septum toward the left in systole, thereby further limiting left-sided filling and compliance.
Right ventricular function
Unlike left ventricle, the anatomically complex right ventricle and its crescentic shape with both the infundibulum and some trabeculations is very difficult to assess in one manner its volumes and ejection fraction%. An additional condition rendering difficult to detect RV volumes is its variable shape with different loading conditions [22, 23]. A number of echocardiographic methods have used for evaluating RV volumes and %RVEF. Of these: two-dimensional echocardiography includes: the Simpson’s rule method and the biplane area-length method. Two dimensional echocardiography Simpson’s rule method requires computer calculations and was been used in a number of echocardiographic studies. The most frequently views utilized are: the apical four-chamber view or the subcostal approach [24–26]. RV volumes are recorded in diastole and in systole by subcostal approach, as reported in Fig. 4.
The area-length method, putted to subcostal outflow tract or to apical four-chamber view, is another 2-D echocardiographic method to evaluate RV volumes [27, 28].
RV myocardial performance index
Right ventricular myocardial performance index (MPI) has been demonstrated to be clinically useful to define RV function. The most frequently employed ultrasonic technique is pulsed doppler echocardiography (PDE). It is the result of (isovolumetric contraction time + isovolumetric relaxation time)/ejection time (Fig. 5). The RV mean reported value of MPI in healthy adults is = 0.25 ± 0.05 [29]. Its comparison with invasive measurements makes the index a sensitive indicator of RV function. This index, also named Tei index, is not influenced by heart rate, body weight, and aging and is correlated with %RVEF obtained by nuclear ventriculography [30]. Tei index can be also obtained using tissue doppler imaging (TDI) [31].
Calculation of myocardial performance index (MPI) of RV. The interval a was obtained in apical for chambers view at the tips tricuspid leaflets. The interval b was recorded from the parasternal short axis view, with doppler sampling site positioned just below the pulmonary valve, by pulsed doppler echocardiography. ICT Isovolumetric contraction time, IRT Isovolumetric relaxation time, ET Ejection time
MPI is prolonged in patients with primary pulmonary hypertension compared with normal subjects. In using this index to discriminate COPD patients with impaired diastolic function, El-Damarawy et al. [32] recently found the index had high efficacy, sensitivity and positive predicted values but low specificity and negative predicted values in to define RV dysfunction.
Tissue doppler imaging
Tissue doppler imaging (TDI) allows quantitative assessment of RV systolic and diastolic function by the measurement of myocardial velocities. Usually, sample volume is placed at level of lateral or septal tricuspid annulus (Fig. 6). Peak velocity <11.5 cm/s identifies RV dysfunction with a sensitivity and specificity of 90 and 85% respectively [33]. Using this technique, Lindqvist and coll demonstrated that RV isovolumic contraction velocity is a reproducible and an easily obtaining non-invasive parameter correlated with invasive measurements of RV referring to intrinsic contractility (dP/dt) and its filling pressures [34, 35]. Recently, Meluzin et al. [36] showed that the peak systolic velocity of RV myocardial free wall correlated to EF%. An advantage of using TDI to assess RV function is that measurement is independent of geometric assumptions and endocardial border tracing. Its main limitation is that it does not distinguish between active and passive wall motion both in animals and in humans [37, 38].
Strain and strain rate imaging
The strain rate imaging (SRI) have made more assessment of global and regional systolic and diastolic RV function [39, 40]. But, while the assessment of longitudinal strain from apical view is feasible, the analysis of RV radial deformation from the parasternal window turned out to be difficult. In healthy individual, RV longitudinal velocities demonstrated a baso-apical gradient with higher velocities at the base; also RV velocities are higher as compared to the LV. Contrary to LV, the strain rate and the strain values of the RV are in homogeneously distributed. This pattern can be explained by the complex RV geometry. In a recent study RV strain demonstrated a good correlation between the peak systolic ε (this is the maximal deformation of the myocardium) recorded in the basal segment of the RV free wall and other prognostic markers of chronic heart failure, such as BNP concentration, peak VO2 or slope of the VE/VCO2 ratio. Some data recorded in patients with pulmonary hypertension suggested that in compensated patients, peak systolic strain rate correlated with peak systolic pulmonary artery pressure, with depression in the smooth inlet portion of RV [39].
Strain/strain rate values were reduced in all segments of RV free wall and interventricular septum in patients with PAPs > 35 mmHg compared with control group (<35 mmHg). A significant relationship was also found between peak systolic SR at basal free wall and radionuclide RVEF% [40]. Furthermore, in contrast to other ultrasound-based methods, SRI allows the quantification of longitudinally systolic and diastolic function for each segment of RV. The study demonstrates the utility of SRI for the evaluation of right ventricular function in chronic obstructive pulmonary disease patients and is correlated with severity of pulmonary disease.
But, strain measurements are angle dependent, therefore the strain interpretation should be performed with caution if tissue direction deviates more than 30° from the beam direction. On the contrary, speckle-tracking is a new, non-invasive method for the assessment of global and regional ventricular function for tracking every point on the 2D echocardiography [41]. With this method it is possible to detect myocardial coordinates in every frame, allowing a myocardial strain to be detect in any direction. In addition, RV function cannot easily appraisable because RV is a triangle-shaped chamber composed of the inlet portion, the outlet portion, and the apical portion with rough trabeculations having a complex architecture. For these reasons, RV global and regional function can be more entirely evaluated with speckle-tracking method [42].
Two works have been evaluated the behaviour of RV free wall and interventricular septum in healthy subjects and in patients with pulmonary hypertension. In the first, RV free wall longitudinal myocardium deformation, myocardial systolic peak strain, systolic peak strain rate (SRs), early diastolic peak strain rate (SRe), late diastolic peak strain rate (SRa), the ratio of SRe/SRa were measured in the basal, middle and apical segments of right ventricular free wall in healthy volunteers from the apical 4-chamber view. The results obtained shown that RV longitudinal strain and strain rate are highest in the basal and middle segments than in the apical of the free wall [43]. This study also shows that in normal subjects there was no difference between the contractile timing in the strain along the posterior wall and that of the pulmonary valvular annulus shortening. In another study, in patients with pulmonary hypertension, peak systolic myocardial velocities, strain rate, and strain resulted significantly impaired compared with controls and resulted most altered in patients with severe pulmonary arterial hypertension [44].
3-D echocardiography
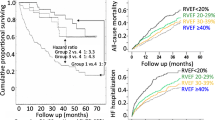
3-D echocardiography (3DE) has been proposed to evaluate RV function in spite of its complex geometry. Contrary to two-dimensional echocardiography, 3DE provides volumetric measurements without geometric assumptions and allows us to measure right ventricular volumes irrespective of the RV irregular shape [45]. The values of RV volumes and ejection fraction obtained with 3DE resulted closely correlated with magnetic resonance imaging (MRI) and radionuclide ventriculography (RNV) [46–48]. A close correlation was also found between radionuclide ventriculography and transesophageal 3DE. 3DE images of RV can be obtained from a modified apical window. Endocardial tracing and the calculation of volumes may be hindered by trabeculations and the presence of the moderator band. Contrary to 2D echocardiography that underestimates RV cavity, real-time 3D echocardiography (RT3D) slightly overestimated RV end-diastolic and end-systolic volumes, although this overestimation was not statistically significant [49]. In normals, the mean times for 3D acquisition are of few minutes and the imaging quality is good in 85% of cases. RVEF is negatively correlated with pulmonary arterial systolic pressure and positively correlated with TAPSE, peak systolic velocity, and fractional shortening area. In patients with pulmonary hypertension RV volumes were larger than in normals and RVEF appear lower than in these. In addition, data obtained by 3D evaluation are well correlated with those obtained by 2D and Doppler methods and can differentiate normal subjects and pulmonary hypertensive patients [50].
Conclusive remarks
All right heart and pulmonary indices are useful to non-invasively define the hemodynamic profile both of healthy subjects and patients with primary or secondary PH, such as those with COPD . This condition is favoured by some diseases provoking PH with consequent RV dysfunction [51, 52]. In turn, the functional RV derangement induces an elevation of PAP and PVR, as adaptive mechanism, leading to RV enlargement and hypertrophy. When the adaptive mechanisms of RV dilatation and hypertrophy cannot compensate for the hemodynamic burden, right heart failure associated with poor prognosis occurs.
The conventional echocardiographic methods are important to non-invasively define right ventricular function and estimate pulmonary pressures. The new echocardiographic techniques, as TDI, SRI or 3DE, appear more accurate and sensitive in to detect both regional and global RV function in healthy and in RV dysfunctioning patients. The results achieved with these same have a good correlation with radionuclide angiography (that is considered as “gold standard”) in to accurately define RV function in spite of the RV complex features, its myoarchiytecture, and coarse trabeculations of the apex. But, further researches on large of healthy and diseased populations are needed to definitely validate the echocardiographic results obtaining both with new and conventional techniques.
References
Konstam MA, Pandian N (1988) Assessment of right ventricular function. In: Konstam MA, Isner JM (eds) The right ventricle. Kluwer, Boston, pp 1–15
Furey SA, Zieske HA, Levy MN (1984) The essential function of the right ventricle. Am Heart J 107:404–410
Cosio FG, Anderson RH, Kuck KH et al (1999) Living anatomy of atrioventricular juntions. A guide to electrophysiologhic mapping. A consensus statement from the cardiac nomenclature study group, working group of arrhythmias. European society of cardiology, and the task force on cardiac nomenclature from NASPE. Circulation 100:E31–E37
Weideman F, Eyskens B, Jamal F et al (2002) Quantification of regional left and right ventricular radial and longitudinal function in heathy children using ultrasound-based strain and strain rate imaging. J Am Soc Echocardiogr 15:20–28
Linqvist P, Calcutteea A, Henein M (2008) Echocardiography in the assessment of right heart function. Eur J Echocardiogr 9(2):225–234
Feigenbaum H (1994) Echocardiography. Lea & Febiger, Philadelphia
Jiang L, Wiegers S, Weyman AE (1994) Right ventricle. In: Weyman AE (ed) Principles and pratice of echocardiography. Lea & Febiger, Philadelphia, pp 901–921
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107:526–531
Ueti OM, Camargo EE, de Ueti A, de Lima-Filho EC, Nogueira EA (2002) Assessment of right ventricular function with doppler echocardiographic indices derived from tricuspid annular motion: comparison with radionuclide angiography. Heart 88:244–248
Kircher BJ, Himelman RB, Schiller NB (1990) Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol 66:493–496
Willens HJ, Fertel DP, Qin J, Labrador E, Lowery MH (2008) Effects of age and pulmonary arterial hypertension on the different phases of right atrial function. Int J Cardiovasc Imaging. doi: 10.1007/s10554-008-9306-4
Ueda R, Yokouchi M, Andou H, Suzuki T, Yamaoka M, Otomo E, Takahashi A, Katagiri T (2004) Pulmonary artery systolic pressure is elevated in the elderly: relationships between echocardiographic and pathological findings. Int Med 43:374–378
Verbeken EK, Cauberrhs M, Mertens I, Clement J, Lauweryns JM, Van de Woesrijne KP (1992) The senile lung. Comparison with normal and emphysematous lungs. I. Structural aspects. Chest 101:793–799
Verbeken EK, Cauberhs M, Mertens I, Clement J, Lauweryns JM, Van de Woestijne KP (1992) The senile lung. Comparison with normal and emphysematous lungs. 2 Functional aspects. Chest 101:800–809
McQuillan BM, Picard MH, Leavitt M, Weyman A (2001) Clinical correlates and reference intervals or pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 104:2797–2802
Friedberg MK, Feinstein JA, Rosenthal DN (2006) A novel echocardiographic doppler method for estimation of pulmonary arterial pressures. J Am Soc Echocardiogr 19(5):559–562
Castelain V, Chela D, Humbert M et al (2002) Pulmonary artery pressure-flow relations after prostacyclin in primary pulmonary hypertension. Am J Respir Crit Care Med 165:338–340
Himelman R, Stulbarg M, Kircher B, Lee E, Kee L, Dean NC, Golden J, Wolfe CL, Schiller N (1989) Noninvasive evaluation of pulmonary artery during exercise by saline-enhanced doppler echocardiography in chronic pulmonary disease. Circulation 79:863–871
Alkotob ML, Soltani P, Sheatt MA, Katestos MC, Rothfield N, Hager WD, Foley RJ, Silverman DI (2006) Reduced exercise capacity and stress-induced pulmonary hypertension in patients with scleroderma. Chest 130:176–184
Brown KA, Okada RD, Boucher CA, Strauss HW, Pohost GM (1984) Right ventricular ejection fraction response to exercise in patients with coronary artery disease: influence of both right coronary artery disease and exercise-induced changes in right ventricular afterload. J Am Coll Cardiol 3:895–901
Chaudhry FA, Tauje JT, Alessandrini RS, Vardi G, Parker MA, Bonow RO (1999) Prognostic implications of myocadial contractile reserve in patients with coronary artery disease and left ventricular dysfunction. J Am Coll Cardiol 34:730–738
Weyman AE, Wann LS, Feigenbaum H et al (1976) Mechanism of abnormal septal motion in patients with right volume overload. Circulation 54:179–186
Feneley M, Garagham T (1986) Paradoxical and pseudoparadoxical interventricular septal motion in patients with right ventricular volume overload. Circulation 74:230–238
Saito A, Ueda K, Nakano H (1981) Right ventricular volume determinations by two-dimensional echocardiography. J Cardiogr 11:1159–1168
Wann LS, Stikels KR, Bamrah VS et al (1984) Distal processing of contrast echocardiograms: a new technique for measuring right ventricular ejection fraction. Am J Cardiol 53:1164–1168
Levine RA, Gibson TC, Aretz T et al (1984) Echocardiographic measurement of right ventricular volume. Circulation 69:497–505
Gibson TC, Miller SW, Aretz T et al (1985) Method for estimating right ventricular volume by planes applicable to cross-sectional echocardiography: correlation with a geographic formulas. Am J Cardiol 55:1584–1588
Jiang L, Levine RA, Weyman AE (1997) Echocardiographic assessment of right ventricular volume and function. Echocardiogrphy 14:189–205
Tei C, Ling LH, Hodge DO et al (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function. A study in normal and dilated cardiomyopathy. J Cardiol 26:357–366
Kamati PK, Mohammed E, Torosoff M, Fein S (2008) Myocardial performance index correlates with ventricular ejection fraction measured by nuclear ventriculography. Echocardiography 25:381–385
Acharya G, Pavlovic M, Ewing L, Nollmann D, Leshko J, Huhta JC (2008) Comparison between pulsed-wave Doppler- and tissue Doppler-derived Tei indices in fetuses with and without congenital heart disease. Ultrasound Obstet Gynecol 31(4):406–411
El-Damarawy M, Zeidan H, Suwailem S (2008) Myocardial performance index in patients with chronic obstructive pulmonary disease. Heart Mirror J 2(2):60–66
Garcia MJ, Rodriguez L, Ares M, Griffin BP, Klein AL, Stewart WJ (1996) Myocardial wall velocity assessment by pulsed doppler tissue imaging: characteristic findings in normal subjects. Am Heart J 132:648–656
Isaaz K, Munoz del Romeral L, Lee E, Schiller NB (1993) Quantitation of the motion of the cardiac base in normal subjects by doppler echocardiography. J Am Soc Echocardiogr 6:166–176
Linqvist P, Waldenstrom A, Wikstrom G, Kazzam E (2005) The use of isovolumic contraction velocity to determine right ventricular state of contractility and filling pressures. A pulsed doppler tissue imaging study. Eur J Echocardiogr 6:264–270
Meluzin J, Spinarova L, Bakala J, Toman J, Krejci J, Hude P (2001) Pulsed doppler tissue imaging of the velocity of tricuspid annular systolic motion; a new, rapid, and noninvasive method for evaluating right ventricular systolic function. Eur Heart J 22:340–348
Jamal F, Bergerot C, Argaud L, Loufouat J, Ovize M (2003) Longitudinal strain quantitates regional right ventricular contractile function. Am J Physiol Heart Circ Physiol 285:H2842–H2847
Eysken B, Weidemann F, Kowalski M et al (2004) Regional right and left function after the senning operation: an ultrasonic study of strain rate and strain. Cardiol Young 14:255–264
Bleeker GB, Steendijk P, Holman ER, Yu CM, Breithardt OA, Kaandorp TAM, Schalij MJ, van der Wall EE, Nihoyannopoulos P, Bax JJ (2006) Assessing right ventricular function: the role of echocardiography and complementary technologies. Heart 92:i19–i26
Vitarelli A, Conde Y, Cimino E, Stellato S, D’Orazio S, D’Angeli I, Nguyen BL, Padella V, Caranci F, Petroianni A, D’Antoni L, Terzano C (2006) Assessment of right ventricular function by strain rate imaging in chronic obstructive pulmonary disease. Eur Respir J 27:268–275
Toyoda T, Baba H, Akasaka T, Akiyama M, Neishi T, Tomita J, Sukmawan R, Koyama Y, Watanabe N, Tamano S, Shinomura R, Komuro I, Yoshida K (2004) Assessment of regional myocardial strain by novel automated tracking system from digital image files. J Am Soc Echocardiogr 17:1234–1238
Matsui H, Satomi G, Yasukochi S, Kaneko S, Haseyama K (2008) Evaluation of right ventricular contraction by myocardial strain in children using two-dimensional tissue tracking method. Pediatr Cardiol 29:377–381
Tong C, Li C, Song J, Liu H, Deng Y (2008) Assessment of right ventricular free wall longitudinal myocardial deformation using speckle tracking imaging in normal subjects. J Huazhong Univ Sci Technol (Med Sci) 28(2):194–196
Pirat B, Culloch ML, Zoghbi W (2006) Evaluation of global and regional right ventricular systolic function in patients with pulmonary hypertension using a novel speckle tracking method. Am J Cardiol 98:699–704
Jenkins C, Chan J, Bricknell K, Strudwick M, Marwick TH (2007) Reproducibility of right ventricular volumes and ejection fraction using real-time three-dimensional echocardiography. Chest 131:1844–1851
Angeline ED, Homma S, Pearson G, Holmes JW, Laine AF (2005) Segmentation of real-time three-dimensional ultrasound for quantification of ventricular function: a clinical study on right and left ventricles. Ultrasound Med Biol 31:1143–1158
Joachim NH, Wolfgang T, Ayan P, Navroz MD, Bernhard M, Pandian N (2006) Quantitation of right ventricular volumes and ejection fraction by three-dimensional echocardiography in patients: comparison with magnetic resonance imaging and radionuclide ventriculography. Echocardiography 8:666–680
Papavassiliou DP, Parks WJ, Hopkins KL, Fyfe DA (1998) Three-dimensional echocardiographic measurement of right ventricular volume in children with congenital heart disease validated magnetic resonance imaging. J Am Soc Echocardiogr 11(8):770–777
Fujimoto S, Mizuno R, Nagakawa Y, Dohi K, Nakano H (1998) Estimation of the right ventricular volume and ejection fraction by trans-thoracic three-dimensional echocardiography.A validation study using magnetic resonance imaging. Int J Card Imaging 14(6):385–390
Tamborini G, Brusoni D, Torres Molina JE, Galli CA, Maltagliati A, Muratori M, Susini F, Colombo C, Maffessanti F, Pepi M (2008) Feasibility of a new generation three-dimensional echocardiography for right ventricular volumetric and functional measurements. Am J Cardiol 102:499–505
Schulman DS, Matthay RA (1992) The right ventricle in pulmonary disease. In: Smiley I, Rich S, Mc Laughlin VV (eds) Cardiology clinics: the right ventricle. WB Saunders, Philadelphia, pp 111–135
Dhainaut JFA, Doise JM, Brunet F (1996) Heart-lung interaction in chronic ostructive pulmonary disease. In: Derenne JP, Whitelaw WA, Smilowski T (eds) Acute respiratory failure in chronic obstructive pulmonary disease. New York, Marcel Dekker, pp 267–302
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cacciapuoti, F. Echocardiographic evaluation of right heart function and pulmonary vascular bed. Int J Cardiovasc Imaging 25, 689–697 (2009). https://doi.org/10.1007/s10554-009-9478-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-009-9478-6