Abstract
Purpose
Younger women diagnosed with breast cancer have poorer prognoses and higher mortality compared to older women. Young black women have higher incidence rates of breast cancer and more aggressive subtypes than women of other races/ethnicities. In this study, we examined recent trends and variations in breast cancer incidence among young women in the United States.
Methods
Using 2004–2013 National Program of Cancer Registries and Surveillance, Epidemiology, and End Results Program data, we calculated breast cancer incidence rates and trends and examined variations in stage, grade, and tumor subtype by age and race/ethnicity among young women aged 20–49 years.
Results
The majority of breast cancer cases occurred in women aged 40–44 and 45–49 years (77.3%). Among women aged < 45 years, breast cancer incidence was highest among black women. Incidence trends increased from 2004 to 2013 for Asian or Pacific Islander (API) women and white women aged 20–34 years. Black, American Indian or Alaska Native, and Hispanic women had higher proportions of cases diagnosed at later stages than white and API women. Black women had a higher proportion of grade III–IV tumors than other racial/ethnic groups. Across all age groups, incidence rates for triple-negative breast cancer were significantly higher in black women than women of other races/ethnicities, and this disparity increased with age.
Conclusions
Breast cancer among young women is a highly heterogeneous disease. Differences in tumor characteristics by age and race/ethnicity suggest opportunities for further research into personal and cultural factors that may influence breast cancer risk among younger women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Breast cancers in young women aged < 40 years at diagnosis have poorer prognosis and higher mortality compared to breast cancers diagnosed in older women [1, 2]. Younger women tend to present at later stages and with more aggressive, larger tumors [3,4,5]. Although breast cancer is uncommon among younger women [6], it accounts for significant excess costs in medical treatment and lost productivity [7,8,9]. Incidence rates of breast cancer in younger women have remained stable in recent years [2, 6, 10]. However, an increasing incidence was reported in invasive breast cancer among young white women aged < 40 years from 1992 to 2004 [11] and in breast cancer with metastatic disease among women aged 25–39 from 1976 to 2009 [12].
Racial differences have been documented in breast cancer incidence at all ages and in breast cancer mortality in younger women [10, 13, 14]. Black women are more likely to be diagnosed at younger ages and with the more biologically aggressive triple-negative subtype [15, 16]. Young black women aged < 40 years have a higher breast cancer mortality rate compared to white women [10]. Racial differences in survival are possibly due to differences in tumor morphology, stage at the time of diagnosis, access to care, and quality of treatment [17, 18].
Recent trends and incidence rates for breast cancers in younger women have not been comprehensively described by race or ethnicity or age group. Using combined data from the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) and the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program (SEER) from 2004 to 2013, this study aims to report recent trends and describe variations in breast cancer incidence and stage, grade, and tumor subtype by age and race/ethnicity among women aged 20–49 years.
Methods
Data source
Population-based invasive breast cancer incidence data for women diagnosed from 2004 to 2013 were obtained from cancer registries funded by NPCR or SEER. Data were collected and reported using standard data items and uniform codes and procedures as promulgated by the North American Association of Central Cancer Registries [19]. Data were reported from 49 states and DC central cancer registries that met United States Cancer Statistics (USCS) publication standards [20]. The combined NPCR/SEER data covered 99.1% of the US population for this study [20]. The corresponding population data used for this analysis were obtained from the SEER program, which uses a slight modification of the annual population estimates from the Census Bureau [21].
Case definition
Site and histology for incident breast cancers were coded according to the International Classification of Diseases for Oncology third edition (ICD-O-3). Cases were defined as invasive, breast cancer (ICD-O-3 site code C50.0–C50.9) diagnosed in women aged 20–49 years. Cases reported to the cancer registry based on autopsy only or death certificate only were excluded (n = 601).
Population characteristics
Age at diagnosis was stratified into four groups (20–34, 35–39, 40–44, and 45–49 years). Race/ethnicity was combined and stratified into five mutually exclusive groups [Non-Hispanic (NH) White, NH Black, NH Asian or Pacific Islander (API), NH American Indian or Alaska Native (AIAN), Hispanic].
Tumor stage and grade
Stage was categorized (localized, regional, distant, unknown) according to the SEER Summary Staging 2000 [22]. Grade was classified into four groups (well differentiated [grade I], moderately differentiated [grade II], poorly differentiated and undifferentiated/anaplastic [grade III–IV], unknown). Given the small number of undifferentiated/anaplastic cases, poorly differentiated and undifferentiated/anaplastic grades were combined and analyzed together.
Tumor subtype
Tumor subtype was classified based on estrogen receptor (ER), progesterone receptor (PR), and human growth factor/neu receptor (HER2) status. ER and PR status were combined into one of three hormone receptor (HR) status categories: HR+ (cases with ER+ or PR+ or borderline ER or PR), HR−(ER− and PR− cases), and unknown HR status. Unknown HR status included ER− cases where PR test results were unknown or missing, PR− cases where ER test results were unknown or missing, and cases where both ER and PR test results were unknown or missing. HR and HER2 variables were combined into five categories as follows: HR+/HER2−, HR+/HER2+ , HR−/HER2+ , HR−/HER2− [triple-negative (TN)], and subtype unknown. Unknown subtype included cases with unknown HR status or cases where HER2 test results were borderline, unknown, or missing. Overall from 2011 to 2013, about 5% of cases were classified as unknown for ER and PR status and about 11% were classified as unknown for HER2 status.
Statistical analysis
SEER*Stat [23] was used to calculate incidence rates (per 100,000 women) and rate ratios. Corresponding 95% confidence intervals (CIs) were calculated. The annual percent change (APC) was calculated using the least squares method. We analyzed the relative proportion of age-specific incidence among racial and ethnic groups by stage and grade. All rates for the age groups 20–34 and 20–49 years were age adjusted to the US 2000 standard population.
For the HR/HER2 subtype analysis, we limited our analysis to 2011–2013 because a high percentage of data on ER, PR, and HER2 status was missing in prior years and HER2 data were unavailable prior to 2010. In the subtype analysis, the number of cases among AIAN women was too few to examine separately, but these cases were included in the results for all races/ethnicities combined. We examined the incidence of HR/HER2 subtypes among racial and ethnic groups by age and analyzed the relative proportion of rates of HR/HER2 subtype incidence among racial and ethnic groups by stage and grade.
Results
Incidence rates by race/ethnicity, age, and region
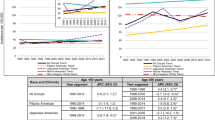
From 2004 to 2013, the vast majority of invasive breast cancer cases (77.3%) among young women occurred after age 40 years, and nearly half occurred among women aged 45–49 years (Table 1). Incidence rates increased with age within each racial and ethnic group and were more than 10 times higher for women aged 45–49 years compared to women aged < 35 years. Among women aged < 45 years, black women had significantly higher incidence rates than white women across all age groups. Among women aged 45–49 years, incidence rates in black women were significantly lower than those in white women. For all age groups combined, white women had significantly higher incidence rates than Hispanic, API, and AIAN women.
Incidence trends by race/ethnicity and age
From 2004 to 2013, breast cancer incidence trends remained stable across most age and racial/ethnic groups with a few exceptions (Table 1). API women aged 20-49 (APC = 0.9) and aged 45–49 (APC = 1.2) years experienced a significant increase over the 10-year period. Among women aged 20–34 years, there was a small but significant increase among white women (APC = 0.3). Hispanic women aged 35–39 had a significant decrease in incidence (APC = − 0.7) over this time period.
Relative proportion of tumor stage and grade by race/ethnicity and age
Localized tumors represented the highest percentage of incident cases in older age groups (40–44 and 45–49 years), and the proportion of regional and distant stage tumors decreased with age (Fig. 1). Across all age groups, black women, and to a lesser extent AIAN and Hispanic women, had a higher proportion of cases diagnosed at regional and distant stages compared to white and API women. Among black, AIAN, and Hispanic women aged < 40 years, and white women aged < 35 years, more than half of cases were diagnosed at regional or distant stages. Across all ages, API women had the highest proportion of localized stage tumors than any other racial/ethnic group.
Across all races/ethnicities, grade III–IV tumors comprised more than half of incident cases among women aged 20–34 years, and this proportion decreased with age (Fig. 2). Conversely, the proportion of grade I and II tumors increased with age. Compared to other races/ethnicities, black women had the highest proportion of grade III–IV tumors, making up the majority of cases among black women, even in the oldest age group (45–49 years). White and API women had the lowest proportion of grade III–IV tumors across all age groups.
Incidence rates by HR/HER2 subtype, race/ethnicity, and age
Among women aged 20–49 years whose breast cancer was diagnosed from 2011 to 2013, invasive breast cancer incidence rates varied by HR/HER2 subtype and race/ethnicity (Table 2). HR+/HER2− was the most common breast cancer subtype, representing 58% of all cases and was the most common subtype for all races/ethnicities, with higher rates among white women compared to API, Black, and Hispanic women (p < 0.001, for all groups).
TN breast cancer was the second most common subtype overall, making up over 14% of all cases. TN was the second most common subtype for black and Hispanic women and the third most common for white and API women. Black women had the highest age-adjusted incidence of TN breast cancer compared to all other racial/ethnic groups (p < 0.001, for all groups). The TN incidence rate for black women was about two times higher than for white and Hispanic women and almost three times higher than for API women. Black women also had the highest proportional distribution of TN tumors (23%), followed by Hispanic (15%), white (13%), and API (10%) women.
HR+/HER2+ breast cancer was the third most common subtype, representing 13% of all cases. White women had significantly higher rates of HR+/HER2+ compared to black (p = 0.035), API (p = 0.018), or Hispanic (p < 0.001) women.
HR−/HER2+ breast cancer was the least common subtype for all races/ethnicities, accounting for only 5% of all cases. Black and API women had comparable rates of HR−/HER2+ , 4.1 and 3.9 per 100,000, respectively. Black and API women had significantly higher rates than white and Hispanic women. API, Hispanic, and black women had a slightly higher proportion of HR−/HER2+ tumors (6%) than white women (5%). Hispanic women had the highest percentage of unknown tumor subtypes (13%), followed by black (10%), API (9%), and white (8%) women.
Among all racial and ethnic groups, the incidence of HR +/HER2− tumors increased with age (Fig. 3). In women aged 20–34 years, black women had higher rates of HR+/HER2− than the other racial/ethnic groups (p < 0.001, for all groups) and white women had significantly higher rates than API (p = 0.04) and Hispanic (p < 0.01) women. In women aged 35–39 years, white, black, and API women all had comparable rates (32.3, 31.7, and 30.4 per 100,000, respectively). Among women aged ≥ 40 years, the incidence of HR+/HER2− tumors was significantly higher among white women than other races/ethnicities (p < 0.001, for all groups), with the second highest rates found in API women.
Incidence of TN tumors increased with age among all racial and ethnic groups (Fig. 4). In all age groups, TN incidence rates were significantly higher in black women compared to other racial and ethnic groups, and this difference increased with age (p < 0.01, for all groups). The proportion of all breast cancer that was TN was fairly consistent across age groups of black women, 24% in women aged < 45 years and 22% in 45–49 years (Fig. 5). In contrast, the proportion of TN breast cancer cases decreased with age for white, API, and Hispanic women.
Relative proportion of tumor stage and grade, by HR/HER2 subtype
Among HR+/HER2− tumors, white and API women have a higher proportion of localized tumors (61%) compared to black and Hispanic women (50 and 52%, respectively) (Fig. 6). White (58%) and API (61%) women have higher proportions of localized TN tumors than black (49%) or Hispanic women (53%). A greater proportion of HR+/HER2+ tumors were distant stage in black women (11%) than that in Hispanic, white, and API women (9, 7, and 6%, respectively). Among HR−/HER2+ tumors, black (15%) and Hispanic women (13%) had a higher proportion of distant stage tumors than white or API women (9 and 8%, respectively).
Black women with HR+/HER2− tumors had a lower proportion of grade I and II tumors (55%) compared to white, API, and Hispanic women (70, 68, and 65%, respectively) (Fig. 7). Across all racial/ethnic groups, TN tumors had the highest and HR−/HER2+ tumors have the second highest proportion of grade III–IV tumors compared to other subtypes.
Discussion
Our study provides updated data on breast cancer incidence among young women covering the entire country, and expands our understanding of differences in breast cancers among younger women by race and ethnicity in several areas. Breast cancers among young women are highly heterogeneous. Within the age range of 20–49 years, incidence increased markedly with age, and most cancers occurred among women aged 40–49 years. For all age groups < 45 years, incidence rates were highest among black women. Although breast cancer incidence trends were stable from 2004 to 2013 among all racial and ethnic groups combined, incidence increased over the 10-year study period among API women, driven by a significant increase among API women aged 45–49 years. An increasing trend in incidence was reported among API women in California aged < 50 years [24]. Our data also showed a smaller but significant increase in incidence among white women aged < 35 years.
White women aged 20–49 years had the highest rates of HR+/HER2− compared to women of other races/ethnicities, similar to the subtype distribution among women of all ages [25]. Among women aged < 40 years, other studies reported that API and white women had a similar incidence of HR+/HER2− [26, 27], but we found this similarity in incidence only among women aged 35–39 years. Among women aged < 35 years, white women had higher incidence rates of HR+/HER2− breast cancers than all other groups, including API women.
In our study results, the proportion of TN breast cancers decreased with age overall but was fairly consistent across age groups among black women, who also had the highest proportional distribution of TN tumors compared to other races/ethnicities. A study using registry data from California [26] had reported a decrease in the proportion of TN tumors with increased age in all women, but we are unaware of other studies that have reported on the proportion of TN breast cancer by race/ethnicity and age. A growing body of research points to multiple risk factors associated with the increased risk of TN breast cancer in black women, including parity, lack of breastfeeding initiation, and obesity [28,29,30,31,32].
Black, Hispanic, and AIAN women had a higher proportion of advanced stage tumors compared to white and API women at every age group. A difference in stage distribution between black and white younger women had been reported in earlier studies [33,34,35,36]. A study of women aged < 35 years diagnosed with breast cancer in the 1990s reported that Hispanic women presented with more advanced stage tumors compared to NH white women [33]. In contrast, a study in California examining data from 1988 to 2006 reported similar rates of advanced stage tumors among Hispanic and NH white women aged 40–49 years [35]. A study analyzing SEER registry data from 1973 to 2009 for women aged 18–39 years reported that black and Hispanic white women had higher proportions of advanced stage breast cancers compared to NH white and API women [36]. In a study of adult women aged 40–79 years from 2000 to 2006, black, Hispanic white, Pacific Islander, and AIAN women were more likely to present stage IV tumors than NH white women. However, only 23% of this study’s population was aged < 50 years and none were aged < 40 years [37]. Across all racial and ethnic groups, we found that HR+/HER2+ and HR−/HER2+ tumors were more likely to be distant stage than other subtypes. This finding is consistent with previous reports for women of all ages [38] and adolescent and young adult women of all races [26].
Among women aged < 40 years, black women had a higher proportion of high-grade tumors compared to other racial and ethnic groups, particularly white and API women, similar to previous reports [34, 36]. In contrast, a study among women aged < 35 years diagnosed with breast cancer from 1990 to 1998 reported that white women were as likely as black and Hispanic women to report high-grade tumors [33]. We also found that TN tumors were more likely to be high grade than other HR/HER2 subtypes, especially among younger black women. This association between TN subtype and high-grade tumors had been reported in studies of women of all ages [38, 39] and in a study of adolescents and young adults of all races [26].
These data showed women aged 20–39 years had higher proportions of later stage and higher grade breast cancer diagnoses than women aged 40–49 years. Leading organizations do not recommend screening by mammography for average risk women prior to the age of 40 [40,41,42]. Guidelines for mammography use are inconsistent for women aged 40–49 years, though some organizations recommend annual mammography screening starting at age 40 or 45 [40, 43]. Mammography has lower sensitivity, higher false-positive rates, and a lower positive predictive value for younger women compared with older women and may cause harms including false-positives, over-diagnosis, and radiation exposure [44]. Despite these limitations, younger women are receiving screening mammograms [45]. Young women more often detect their own breast cancers [46], which may be diagnosed at a more advanced stage or higher grade than tumors detected among asymptomatic women through screening.
We did not have information on family history or genetic test results for women with breast cancer, which may contribute to some early breast cancers. Early onset breast cancers are more often associated with BRCA1 and BRCA2 mutations or other genetic predispositions compared to breast cancers diagnosed in older women [47,48,49]. Events related to prenatal and early life exposures, contraception, reproduction, pregnancy, and breastfeeding may influence tumor biology, as well as overall breast cancer risk among young women [47, 50,51,52]. Modifiable cancer risk factors in early adulthood, such as alcohol consumption, are prevalent, and also may contribute to breast cancer among young women [53, 54]. Younger age has been found to be an independent determinant of poor breast cancer prognosis, regardless of intensity of treatment, stage, or tumor characteristics [55]. The Center for Disease Control and Prevention’s Bring Your Brave campaign raises awareness about breast cancer risk factors and symptoms and provides resources for young women and their providers [56].
We note some limitations of this analysis. Registry data are subject to variations in data quality, incomplete geographic, or population reporting, and data are not available for estimating underlying populations at risk. However, all the participating registries met USCS high data quality criteria. Analyses based on race and ethnicity might be biased if race and ethnicity were misclassified in medical records, although efforts were made to ensure that this information was as accurate as possible [57]. Additionally, trends should be carefully interpreted, as changes in incidence may be occurring even if the trend is not statistically significant.
Conclusions
Our examination of breast cancer incidence among young women by HR/HER2 subtype demonstrated variation by race/ethnicity, age, stage, and grade, underscoring the need to differentiate breast cancers by tumor subtype. TN breast cancer is a more aggressive cancer, associated with poorer outcomes and disproportionately affects black women aged < 50 years. Younger black women have higher breast cancer incidence (aged < 45 years) with higher rates of TN breast cancers. Differences in tumor characteristics by age and race/ethnicity suggest opportunities for further research into individual, cultural, and structural factors that may influence breast cancer risk among younger women.
Abbreviations
- AIAN:
-
American Indian or Alaska Native
- APC:
-
Annual percent change
- API:
-
Asian or Pacific Islander
- CI:
-
Confidence interval
- ER:
-
Estrogen receptor
- HER2:
-
Human growth factor/neu receptor
- HR:
-
Hormone receptor
- ICD-O-3:
-
International Classification of Diseases for Oncology third edition
- NH:
-
Non-Hispanic
- NPCR:
-
National Program of Cancer Registries
- PR:
-
Progesterone receptor
- SEER:
-
Surveillance, epidemiology, and end results program
- TN:
-
Triple-negative
- USCS:
-
United States Cancer Statistics
References
Assi HA, Khoury KE, Dbouk H, Khalil LE, Mouhieddine TH, El Saghir NS (2013) Epidemiology and prognosis of breast cancer in young women. J Thorac Dis 5(Suppl 1):S2–S8
Narod SA (2012) Breast cancer in young women. Nat Rev Clin Oncol 9(8):460–470
Warner ET, Colditz GA, Palmer JR, Partridge AH, Rosner BA, Tamimi RM (2013) Reproductive factors and risk of premenopausal breast cancer by age at diagnosis: are there differences before and after age 40? Breast Cancer Res Treat 142(1):165–175
Chollet-Hinton L, Anders CK, Tse C-K, Bell MB, Yang YC, Carey LA, Olshan AF, Troester MA (2016) Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina Breast Cancer Study: a case-control study. Breast Cancer Res 18(79):5
Chen HL, Zhou MQ, Tian W, Meng KX, He HF (2016) Effect of age on breast cancer patient prognoses: a population-based study using the SEER 18 database. PLoS ONE 11(10):e0165409
1999–2013 Incidence, WONDER Online Database (2016) US Department of Health and Human Services. United States Cancer Statistics. http://wonder.cdc.gov/cancer-v2013.html. Accessed 24 Dec 2016
Ekwueme DU, Trogdon JG, Khavjou OA, Guy GP Jr (2016) Productivity costs associated with breast cancer among survivors aged 18–44 years. Am J Prev Med 50(2):286–294
Ekwueme DU, Allaire BT, Guy GP Jr, Arnold S, Trogdon JG (2016) Treatment costs of breast cancer among younger women aged 19–44 years enrolled in Medicaid. Am J Prev Med 50(2):278–285
Allaire BT, Ekwueme DU, Guy GP Jr, Li C, Tangka FK, Trivers KF, Sabatino SA, Rodriguez JL, Trogdon JG (2016) Medical care costs of breast cancer in privately insured women aged 18–44 years. Am J Prev Med 50(2):270–277
Richardson LC, Henley SJ, Miller JW, Massetti G, Thomas CC (2016) Patterns and trends in age-specific black-white differences in breast cancer incidence and mortality—United States, 1999–2014. MMWR Morb Mortal Wkly Rep 65(40):1093–1098
Brinton LA, Sherman ME, Carreon JD, Anderson WF (2008) Recent trends in breast cancer among younger women in the United States. J Natl Cancer Inst 100(22):1643–1648
Johnson RH, Chien FL, Bleyer A (2013) Incidence of breast cancer with distant involvement among women in the United States, 1976 to 2009. JAMA 309(8):800–805
DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A (2016) Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin 66(1):31–42
White MC, Espey DK, Swan J, Wiggins CL, Eheman C, Kaur JS (2014) Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health 104(Suppl 3):S377–S387
Newman LA (2014) Breast cancer disparities: high-risk breast cancer and African ancestry. Surg Oncol Clin N Am 23(3):579–592
Dunn BK, Agurs-Collins T, Browne D, Lubet R, Johnson KA (2010) Health disparities in breast cancer: biology meets socioeconomic status. Breast Cancer Res Treat 121(2):281–292
Williams DR, Mohammed SA, Shields AE (2016) Understanding and effectively addressing breast cancer in African American women: Unpacking the social context. Cancer 122(14):2138–2149
Miller JW, Lee Smith J, Ryerson BA, Tucker TC, Allemani C (2017) Disparities in breast cancer survival in the United States (2001–2009): findings from the CONCORD-2 study. Cancer 123(S24):5100–5118
Thornton ML (ed) (2014) Standards for cancer registries Volume II: data standards and data dictionary, record layout version 15, 19th ed., North American Association of Central Cancer Registries. Springfield, IL
National Program of Cancer Registries and Surveillance Epidemiology & End Results (2016) NPCR and SEER incidence—USCS 2001–2014 public use database data standards and data dictionary, vol. 2017
National Cancer Institute (2017) Surveillance Epidemiology and End Results (SEER) Program. Population estimates used in NCI’s SEER*Stat software. http://seer.cancer.gov/popdata/methods.html. Accessed 26 Oct 2017
Young JL Jr RS, Ries LAG, Fritz AG, Hurlbut AA (2001) SEER summary staging manual—2000: codes and coding instructions, National Cancer Institute. In: NIH Pub No 01-4969. Bethesda, MD
Surveillance Research Program National Cancer Institute: SEER*Stat software (seer.cancer.gov/seerstat) version 8.3.4
Gomez SL, Von Behren J, McKinley M, Clarke CA, Shariff-Marco S, Cheng I, Reynolds P, Glaser SL (2017) Breast cancer in Asian Americans in California, 1988–2013: increasing incidence trends and recent data on breast cancer subtypes. Breast Cancer Res Treat 164(1):139–147
Kohler BA, Sherman RL, Howlader N, Jemal A, Ryerson AB, Henry KA, Boscoe FP, Cronin KA, Lake A, Noone A-M et al (2015) Annual Report to the Nation on the Status of Cancer, 1975–2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst 107(6):djv048
Keegan THM, DeRouen MC, Press DJ, Kurian AW, Clarke CA (2013) Occurrence of breast cancer subtypes in adolescent and young adult women. Breast Cancer Res 15(5):R95
Horne HN, Beena Devi CR, Sung H, Tang TS, Rosenberg PS, Hewitt SM, Sherman ME, Anderson WF, Yang XR (2015) Greater absolute risk for all subtypes of breast cancer in the US than Malaysia. Breast Cancer Res Treat 149(1):285–291
Ambrosone CB, Zirpoli G, Ruszczyk M, Shankar J, Hong CC, McIlwain D, Roberts M, Yao S, McCann SE, Ciupak G et al (2014) Parity and breastfeeding among African-American women: differential effects on breast cancer risk by estrogen receptor status in the Women’s Circle of Health Study. Cancer Causes Control 25(2):259–265
Boyle P (2012) Triple-negative breast cancer: epidemiological considerations and recommendations. Ann Oncol 23(Suppl 6):vi7–vi12
Anstey EH, Shoemaker ML, Barrera CM, O’Neil ME, Verma AB, Holman DM (2017) Breastfeeding and breast cancer risk reduction. Implications for black mothers. Am J Prev Med 53(3s1):S40–S46
Trivers KF, Lund MJ, Porter PL, Liff JM, Flagg EW, Coates RJ, Eley JW (2009) The epidemiology of triple-negative breast cancer, including race. Cancer Causes Control 20(7):1071–1082
Brewster AM, Chavez-MacGregor M, Brown P (2014) Epidemiology, biology, and treatment of triple-negative breast cancer in women of African ancestry. Lancet Oncol 15(13):e625–e634
Shavers VL, Harlan LC, Stevens JL (2003) Racial/ethnic variation in clinical presentation, treatment, and survival among breast cancer patients under age 35. Cancer 97(1):134–147
Ademuyiwa FO, Gao F, Hao L, Morgensztern D, Aft RL, Ma CX, Ellis MJ (2015) US breast cancer mortality trends in young women according to race. Cancer 121(9):1469–1476
Amirikia KC, Mills P, Bush J, Newman LA (2011) Higher population-based incidence rates of triple-negative breast cancer among young African-American women: implications for breast cancer screening recommendations. Cancer 117(12):2747–2753
Liu P, Li X, Mittendorf EA, Li J, Du XL, He J, Ren Y, Yang J, Hunt KK, Yi M (2013) Comparison of clinicopathologic features and survival in young American women aged 18-39 years in different ethnic groups with breast cancer. Br J Cancer 109(5):1302–1309
Ooi SL, Martinez ME, Li CI (2011) Disparities in breast cancer characteristics and outcomes by race/ethnicity. Breast Cancer Res Treat 127(3):729–738
Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LAG, Cronin KA (2014) US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst 106(5):dju055
Parise CA, Bauer KR, Caggiano V (2010) Variation in breast cancer subtypes with age and race/ethnicity. Crit Rev Oncol Hematol 76(1):44–52
Oeffinger KC, Fontham EH, Etzioni R et al (2015) Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA 314(15):1599–1614
United States Preventive Services Task Force (2016) Final update summary: breast cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1. Accessed 26 Oct 2017
American College of Obstetricians and Gynecologists (2011) Practice bulletin no. 122: breast cancer screening. Obstet Gynecol 118(2 Pt 1):372–382
Hale PJ, Gilson deValpine M (2014) Screening mammography: revisiting assumptions about early detection. The Journal for Nurse Practitioners 10(3):183–188
International Agency for Research on Cancer (2015) IARC handbooks of cancer prevention, vol 15. Breast Cancer Screening, Lyon
Qin J, White MC, Sabatino SA, Febo-Vazquez I (2017) Mammography use among women aged 18–39 years in the United States. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-017-4625-6
Ruddy KJ, Gelber S, Tamimi RM, Schapira L, Come SE, Meyer ME, Winer EP, Partridge AH (2014) Breast cancer presentation and diagnostic delays in young women. Cancer 120(1):20–25
Azim HA, Partridge AH (2014) Biology of breast cancer in young women. Breast Cancer Res 16(4):427
Malone KE, Daling JR, Neal C, Suter NM, O’Brien C, Cushing-Haugen K, Jonasdottir TJ, Thompson JD, Ostrander EA (2000) Frequency of BRCA1/BRCA2 mutations in a population-based sample of young breast carcinoma cases. Cancer 88(6):1393–1402
Greenup R, Buchanan A, Lorizio W, Rhoads K, Chan S, Leedom T, King R, McLennan J, Crawford B, Kelly Marcom P et al (2013) Prevalence of BRCA mutations among women with triple-negative breast cancer (TNBC) in a genetic counseling cohort. Ann Surg Oncol 20(10):3254–3258
Anderson KN, Schwab RB, Martinez ME (2014) Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat 144(1):1–10
Interagency Breast Cancer and Environmental Research Coordinating Committee (2013) Breast cancer and the environment: prioritizing prevention. https://www.niehs.nih.gov/about/boards/ibcercc/index.cfm. Accessed 26 Oct 2017
Institute of Medicine (2012) Breast cancer and the environment: a life course approach. The National Academies Press, Washington, DC
Ekwueme DU, Allaire BT, Parish WJ, Thomas CC, Poehler D, Guy GP Jr, Aldridge AP, Lahoti SR, Fairley TL, Trogdon JG (2017) Estimation of breast cancer incident cases and medical care costs attributable to alcohol consumption among insured women aged < 45 years in the U.S. Am J Prev Med 53(3s1):S47–S54
White MC, Shoemaker ML, Park S, Neff LJ, Carlson SA, Brown DR, Kanny D (2017) Prevalence of modifiable cancer risk factors among U.S. adults aged 18–44 years. Am J Prev Med 53(3s1):S14–S20
Fredholm H, Eaker S, Frisell J, Holmberg L, Fredriksson I, Lindman H (2009) Breast cancer in young women: poor survival despite intensive treatment. PLoS ONE 4(11):e7695
Centers for Disease Control and Prevention (2017) Bring your brave compaign. https://www.cdc.gov/cancer/breast/young_women/bringyourbrave/. Accessed 26 Oct 2017
Centers for Disease Control and Prevention (2017) Interpreting Race and Ethnicity in Cancer Data. https://www.cdc.gov/cancer/npcr/uscs/technical_notes/interpreting/race.htm. Accessed 26 Oct 2017
Acknowledgements
This research was supported in part by an appointment (M.L. Shoemaker) to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and CDC.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interests.
Additional information
Availability of data
The dataset generated and analyzed during the current study is available in the U.S. Cancer Statistics repository, https://www.cdc.gov/cancer/npcr/public-use/index.htm.
Rights and permissions
About this article
Cite this article
Shoemaker, M.L., White, M.C., Wu, M. et al. Differences in breast cancer incidence among young women aged 20–49 years by stage and tumor characteristics, age, race, and ethnicity, 2004–2013. Breast Cancer Res Treat 169, 595–606 (2018). https://doi.org/10.1007/s10549-018-4699-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4699-9