Abstract
Purpose
Breast cancer surgery may be associated with pain and physical symptoms in the upper limbs. Functional impairment and pain-related avoidance of movement may further increase disability level. This study aimed to investigate the potential effects of early postoperative virtual reality (VR) therapy on pain, range of motion (ROM), muscle strength, functionality, and fear of movement.
Methods
Forty women with breast cancer who had undergone unilateral mastectomy with axillary lymph node dissection and who were receiving adjuvant therapy were included in the study and randomly assigned to two groups: the Kinect-based rehabilitation group (KBRG) and the standardized physical therapy group (SPTG). The KBRG (n = 20) received VR therapy using Xbox Kinect-based games and the SPTG (n = 20) received standard physiotherapy. Study subjects were assessed at baseline and after the 6-week treatment. Outcome measures were pain (visual analogue scale), grip strength (dynamometer), functionality (disabilities of the arm shoulder and hand questionnaire), muscle strength (handheld dynamometer), ROM (digital goniometer), and fear of movement (Tampa kinesiophobia scale (TKS)).
Results
Both groups detected significant changes in pain, ROM, muscle strength, grip strength, functionality, and TKS scores after the treatment (p < 0.01). Fear of movement was significantly improved in the KBRG and the SPTG displayed more improvement in functionality (p < 0.05). There were no differences in ROM, muscle strength, grip strength, and pain between the groups after the treatment (p > 0.05).
Conclusion
Kinect-based VR therapy resulted in significant outcomes that were comparable to those obtained under standard physiotherapy in the early postoperative phase in patients who had undergone breast cancer surgery.
Trial registration
This study is registered at ClinicalTrials.gov (ClinicalTrials.gov identifier: NCT03618433).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most commonly diagnosed cancer among women worldwide and is the leading cause of cancer-related deaths. More than 1.3 million women are diagnosed with breast cancer every year [1]. While the incidence of breast cancer has gradually increased, the survival rate of breast cancer has increased dramatically [2]. Primary treatment approaches for breast cancer treatment may cause various side effects. Primary treatment of breast cancer includes surgery, adjuvant chemotherapy, radiation therapy, endocrine therapy, and targeted therapy [3]. Effective adjuvant therapies have the potential to reduce the risk of recurrence and mortality. However, these treatments are associated with significant adverse effects and a decrease in quality of life [4]. Neoadjuvant therapy or adjuvant therapy does not significantly contribute to complications associated with cancer therapy. Currently, axillary radiation therapy is known to be associated with an increased level of disability, an increased risk of lymphedema, impaired shoulder–arm mobility, and soft tissue thickening [5].
It has been reported that pain, fatigue, a decreased range of motion (ROM), and decreased muscle strength have developed during the early postsurgical period leading to limitation in daily living activities [6]. Passive mobilization, exercise, manual stretching, and conventional physiotherapy protocols consisting of a combination of these modalities have proven to be effective in the management of upper limb pain after surgery and in the restoration of functionality [7]. Arm morbidity might be reduced by a targeted physiotherapy program applied following surgery [8].
Conventional physiotherapy modalities focus on improving morbidity and functionality, while task-oriented programs focus on the adaptability of patients to various situations, to shorten adaptation processes and to gain rapid problem solving skills by overcoming the fear of movement. Task-oriented programs are superior to exercises involving repetitive multiple movement patterns in patients with musculoskeletal disorders. Task-oriented trainings also improve quality of life by improving personal functionality [9].
The use of technology in rehabilitation is rapidly increasing, while new technologies further motivate patients to participate in their own usual care and standard programs. Virtual reality (VR) therapy has shown as effective results as conventional therapy for upper extremity functional development and provides the capacity to conduct daily living activities [10]. Xbox 360 Kinect (Redmond, WA) produced by Microsoft, has advanced user technology that makes it easy to complete many clinical applications [11]. The main feature of Xbox 360 Kinect™, is its ability to interpret voice, image, and depth data flow and transfer this information to the interface through a microphone array and three dimensional depth sensors mounted on it. It perfectly perceives human body motions without physical contact and transfers relevant data to the computer system. As a product of rapidly developing video gaming technologies, Xbox 360 Kinect™ does not require a game controller and provides additional contributions to current rehabilitation programs [12, 13]. Kinect-based VR rehabilitation programs have been used to improve upper limb function in various groups of disease [14].
To the best of our knowledge, no studies investigating the potential effects of Kinect-based VR rehabilitation programs on upper limb dysfunction have been conducted in patients undergoing breast cancer surgery. Hence, this study aimed to investigate the potential effects of Kinect-based virtual rehabilitation programs on upper limb dysfunction in the early postoperative period in patients undergoing breast cancer surgery.
Materials and methods
Participants
All patients were recruited between August 2018 and July 2019 from the Department of Multidisciplinary Breast Surgery in collaboration with the Department of Radiation Oncology of Okmeydanı Training and Research Hospital (Istanbul). The patients were given written information before the study.
The inclusion criteria were as follows: (1) having undergone breast cancer surgery with axillary dissection; (2) in the second postoperative week; (3) female patient aged 30 to 60 years; (4) absence of any hearing, visual, or speech impairment. Exclusion criteria were (1) previous breast cancer surgery on the present or contralateral side; (2) active or metastatic cancer focus; (3) upper extremity ROM limitation before the surgery; (4) presence of pace-maker, infection, open wounds, or wound drains; and (5) mental disorders or cooperation issues [15, 16].
Study design and ethics
This study was designed as a prospective, randomized, controlled study and patients were randomly assigned into two groups: the Kinect-based rehabilitation group (KBRG) (n = 20), which received treatment with tissue massage, passive mobilization, and Xbox 360 Kinect™ video game program and the standardized physiotherapy group (SPTG) (n = 20), which received treatment with a standard upper extremity physiotherapy program including scar tissue massage and passive mobilization. The random allocation was performed using a computer-based system to generate random numbers to assign patients into the groups (Research Randomizer, https://www.randomizer.org/) [17]. Numbers were individually placed into opaque, sealed envelopes to conceal the allocation sequence. Both groups received the treatment for 45 min per session and two times a week for 6 weeks. All patients were given the same home exercise program except for the session days. The assessor was blind to the groups and used the same assessment procedure at baseline and after the last treatment session but not on the same day with the session. Patients received the same treatment protocol from the first day to the second week after the surgery before the initiation of study treatments (Table 1).
All study procedures were approved by the University Ethics Committee (Protocol ID:ATADEK-2018/9) and the study was conducted in accordance with the ethical rules of the Declaration of Helsinki.
This clinical trial was registered at www.clinicaltrials.gov (ClinicalTrials.govidentifier: NCT03618433). Written informed consent was obtained from the patients.
Interventions
Technical and fictional analysis of Xbox 360 Kinect games has been performed to detect movement patterns equivalent to those practiced in the standard physiotherapy group. Arman et al. described the transitions of Kinect video games from easiest to hardest in their study to improve upper extremity functionality and strength [16]. In line with the literature, we chose Kinect Sports I (darts, bowling, boxing) for the first 3 weeks of the 6-week treatment and in the last 3 weeks, Kinect Sports I (beach volleyball, table tennis) and Fruit Ninja were played for 30 min. Before starting each session, patients had a warm-up session for 5 min with Dance Central 3: Macarena. All the games required active upper extremity movements from the patients including shoulder flexion, abduction, extension, internal and external rotation, elbow flexion, extension, forearm supination, pronation, and wrist flexion and extension on the affected side. The treatment program consisted of playing Kinect video games for 35 min, scar tissue massage for 5 min, and passive shoulder joint mobilization for 5 min. The treatment program was performed by an experienced physiotherapist. Details of the treatment protocol are shown in Table. 1.
Outcomes measures
Primary outcomes
Primary outcome measurements included pain intensity and ROM.
Pain intensity
The visual analogue scale (VAS) was used to measure the intensity of pain. Patients were told to report their pain level in their neck, shoulder, axilla, arm, trunk side, and breast regions on the affected side during their daily living activities. The VAS is a simple and reliable method for measuring the intensity of pain [20]. Patients were asked to place a mark on a 10-cm scale to indicate the level of their pain with 0 representing no pain and 10 worst pain ever experienced [21].
Range of motion
Shoulder ROM was measured in degrees using a digital goniometer. Active flexion and abduction of the shoulder were assessed with the elbow extended in the supine position. External rotation was measured while the shoulder was adducted and in neutral position with the forearm in neutral supination and pronation while sitting on a chair. The angle between the longer axis of the forearm and sagittal plane of the body was defined as the rotational ROM. All measurements were repeated three times and the average of the three measurements was recorded [22, 23].
Secondary outcomes
Secondary outcomes included shoulder muscle strength and hand grip strength, upper extremity functionality, and fear of movement.
Arm strength
The affected upper extremity flexion, abduction, and external rotation muscle strength were measured during maximal voluntary isometric muscle contraction with the J Tech Commender Muscle Tester (Salt Lake City, Utah, USA) handheld dynamometer according to reported positions. Patients were asked to push their arm with the maximal strength which was recorded in kilograms. All measurements were repeated three times with a 30-s interval, and the average of three measurements was recorded [24, 25].
Hand grip strength
The Saehan hydraulic hand dynamometer was used to measure grip strength. The maximum grip strength on the affected side was measured in kilograms. Measurements were performed in the position defined by the American Society of Hand Therapists (in the sitting position while the shoulder is positioned at adduction with elbow in 90° flexion and the wrist in neutral position). The test was performed three times with 1-min intervals, and the average of three measurements was recorded [16, 26].
Upper extremity functionality
The disability of the arm, shoulder and hand (DASH) questionnaire was used to assess upper extremity functionality [27]. The DASH is a 30-item questionnaire. Each item is scored on a 1 (no difficulty) to 5 (unable) scale. The total score may range from 0 to 100 points. High scores indicate a high level of disability.
Fear of movement
This outcome measure was assessed with the Tampa kinesiophobia scale (TKS). TKS is a 4-point Likert-type scale (1 = strongly disagree, 4 = strongly agree) and total scores range from 17 to 68. High scores indicate an increased degree of kinesiophobia [28].
Sample size determination and statistical analyses
The sample size was determined based on our primary outcome (pain severity) from a study performed by Beurskens et al. [29]. Based on this study, a two-independent-samples t test was used to determine the sample size. At least 17 persons were found to be necessary for strength of 0.80 with an alpha level of 0.05. Considering a dropout rate of 10%, 20 subjects were included in each group.
The Shapiro–Wilk test was used to evaluate whether continuous variables were normally distributed. An independent t test was used for comparisons between the groups in terms of mean values. The paired t test was used for intragroup comparisons of pre-intervention and post-intervention mean values. General linear model repeated measures variance analysis (time × group interaction) was used to determine whether the differences between pre-intervention and post-intervention measurements varied by group. Cohen’s d was used to calculate the effect size. Fisher’s exact test was used for the analysis of categorical variables. A p value of 0.05 was considered to be significant in the analysis. An IBM SPSS 21 Statistics software package was used to analyze the study data.
Results
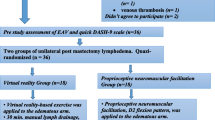
Figure 1 shows the flow diagram of patients. We evaluated 67 patients, 22 patients did not meet the inclusion criteria. Five patients refused participation. We included 40 patients in the study. All patients underwent pre-intervention assessment at baseline. Three patients from the SPTG and one patient from the KBRG were dropped out. Table 2 shows that no significant differences were found between the KBRG and SPTG in baseline characteristics except the affected side ratio (p = 0.049).
No significant intergroup differences were found in the primary and secondary assessments at baseline (p > 0.05). Within-group analysis revealed a significant decrease for all primary and secondary outcomes from baseline to post-intervention in both groups (p = 0.001) (Table 3). These results indicate that the effects of the Kinect-based VR rehabilitation program on changes from the baseline are more prominent than those of standard physical therapy approaches, with the exception of DASH scores and hand grip strength.
Statistically, significant intergroup differences were observed in the mean changes in DASH and TKS scores from the baseline to post-intervention. The mean TKS score change (12.89 points) (p = 0.001) was found to be significantly higher in the KBRG than in the SPTG, while the mean DASH score change was found to be significantly higher (36.53 points) (p = 0.025) in the SPTG than in the KBRG (Table 3). No significant intergroup differences were detected in other outcome parameters in terms of changes from the baseline. Cohen’s d values and confidence intervals for each group are shown in Table 4.
Discussion
We designed this study to investigate the effect of VR training using Xbox Kinect™ on upper extremity disability in the early phases after breast cancer surgery. In addition, we aimed to investigate the potential use of the Kinect video game program as an alternative treatment to a standard physiotherapy program. Considering the results of this study, both treatment approaches showed significant improvement in all clinical parameters. When the effect sizes of the treatment approaches were compared, the KBRG was superior to the SPTG in all parameters except DASH score and grip strength. However, this superiority was statistically significant only for the time-dependent changes in TKS scores. While the change in TKS scores for the KBRG was more significant, the change in DASH scores was more significant for the SPTG.
To our knowledge, there have been limited studies investigating the efficacy of VR in the treatment of patients with breast cancer that have focused on the effects of VR on pain, anxiety, cognitive function, and its role as a distraction from chemotherapy [30]. Kinect has been used to assess upper limb ROM and to monitor movement components [31]. Our study was the first randomized controlled study comparing Kinect-based VR rehabilitation program to standard physiotherapy in the early phases after breast cancer surgery.
Pain is one of the most prevalent symptoms associated with breast cancer treatment. Hidding et al. reported the rates of postoperative shoulder and chest pain following breast cancer surgery as 75% and 82%, respectively, and the risk of developing pain has been demonstrated with level of evidence 1 in patients undergoing axillary lymph node dissection (ALND), radiation therapy, and chemotherapy or receiving targeted medicines [32]. In our study, all patients had undergone ALND and were undergoing adjuvant therapy. At baseline, the mean pain score in both groups was calculated as 6.53. The minimal detectable change in VAS scores in breast cancer treatment was reported to be 9 to 11 mm [33]. Furthermore, pain reduction of 30.0 mm or greater decrease in the VAS score was necessary to ensure adequate control of acute severe pain [34]. In our study, the mean reduction in VAS scores was found to be 5.0 cm (0.29) for the KBRG and 3.97 cm (0.47) for the SPTG. Although the difference between the two treatment groups in the mean changes in VAS scores was not statistically significant, the mean change was higher in the KBRG. Zeng et al. reported more rapid and positive feedback for VR-based interventions for pain compared with conventional symptomatic management of cancer [30].
A systematic review suggested that Kinect-based VR might be preferred over other modalities to increase the shoulder ROM. Kinect-based VR approaches are generally used to treat neurodegenerative disorders [35]. Sin and Lee reported favorable effects of the addition of Kinect system to conventional therapy over conventional therapy alone in a group of patients with hemiplegia and this approach provided significant increases in upper limb ROM [36]. In a systematic review, an upper limb training program applied to patients receiving adjuvant treatment in their early postoperative period was found to provide an average increase of 12.92° for shoulder flexion and 9.72° for shoulder abduction [37]. Minimal clinically important change (MCIC) for shoulder ROM has been reported to be 15° in the general population [38]. In our study, the mean increases in shoulder flexion in the KBRG and SPTG were found to be 52.0° and 49.2°, respectively while the mean increases in shoulder abduction in the KBRG and SPTG were found to be 63.82° and 61.58°, respectively.
Upper limb muscle strength significantly improves in patients receiving exercise therapy compared to usual care who receive adjuvant treatment following breast cancer surgery. Early-term physiotherapy approaches are particularly well-known to improve quality of life by increasing muscle strength [39]. In our patients, both standard physiotherapy and the Kinect-based rehabilitation program provided significant improvements in shoulder flexion, abduction, external rotation, muscle strength, and hand grip strength. Resistance training has been reported to provide a mean increase of 1.49 kg in shoulder muscle strength [39]. In a study conducted in elderly patients, comparing the Xbox Kinect game with exercise and found that the effect sizes for hand grip strength were 0.40 in the Kinect group and 0.62 in the exercise group [40]. Our results were in line with those reported in the literature. Although Cohen’s d effect size was calculated as 0.5 and 0.4 for the SPTG and KBRG, respectively. In our study, no relevant standardized data have been found in the literature.
Harrington et al. recommend the use of the DASH scale to assess upper limb functionality in breast cancer survivors [27]. Prospective care of patients with breast cancer aims at improving joint mobility and muscle strength and reducing pain. A significant relationship was reported between arm and shoulder problems and functionality [41]. Although not validated for the DASH scale in breast cancer population, upper limb exercise training has been reported to result in a minimal detectable change of 15 points in DASH scores [39, 42]. In our study, changes in DASH scores from baseline were found to be higher than those reported in the literature in both groups. The mean change in DASH scores was 36.53 in the SPTG and 28.19 in the KBRG. The higher mean change in the SPTG than that in the KBRG might be associated with higher baseline values in the SPTG.
Fear of movement further increases the risk of decline in upper limb function in breast cancer survivors. Upper limb dysfunction may be further aggravated by avoidance of movements that may induce pain [43]. There are no studies evaluating the effect of VR on fear of movement in breast cancer patients. Virtual gait effect integrated to a physiotherapy program might reduce fear of movement compared to physiotherapy alone in nonspecific low back pain [44]. The VR-based Wii Fit yoga program has also been demonstrated to reduce kinesiophobia [45]. In our study, the level of fear of movement significantly decreased in both groups. The mean change in the TKS scores favored the KBRG over the SPTG. Further studies are needed to explore the efficacy of Kinect-based VR rehabilitation programs in reducing the level of kinesiophobia.
No complications occurred during Xbox Kinect VR training performed early in the postoperative period after breast cancer surgery. The patients in the KBRG participated more motivationally and had less fear of movement during the entire program. Considering the significant clinical outcome measures of the KBRG, we think that Xbox Kinect VR training may be an alternative to standard physiotherapy or may display more improvement in clinical outcomes when applied in addition to standard physiotherapy.
Limitations and strengths
This study has certain limitations. The duration of the study was our limitation. Longer treatment duration may reflect the efficacy of VR therapy more precisely. Further studies should be designed with long-term follow-up. Another limitation might be the lack of an untreated control group.
The study also has strengths. First, baseline characteristics were similar between the groups, and the consequent homogeneity of the distribution of the study groups is one of the strengths of the study. Second, the estimated dropout rate was not exceeded, and only 4 dropouts (10%) occurred before the study was completed. Third, both groups received rehabilitation interventions and were treated by the same physiotherapist. Last, manual interventions (scar massage and glenohumeral joint mobilization) were used in both groups to avoid any intergroup differences resulting from such interventions.
Further research
No adverse effects were observed in patients receiving VR training using Xbox 360 Kinect™ after surgery. Future longitudinal studies may demonstrate whether functional improvements associated with the use of Xbox Kinect video games are long-lasting. Future studies are needed to compare the standard physiotherapy group with the Kinect-based VR training group without any scar tissue massage and passive glenohumeral joint mobilization. According to the results of these studies, Kinect-based VR may be used as an alternative to standard physiotherapy after breast cancer surgery.
Conclusions
This study has demonstrated that VR training using Xbox Kinect™ might be as effective as standard physiotherapy in the management of upper limb dysfunctions after breast cancer surgery. Xbox Kinect™ video games may provide more entertaining, low-cost, motivating programs. In clinic, Kinect-based VR rehabilitation programs may be added to standard physiotherapy or recommended instead of conventional physiotherapy for patients with high levels of fear of movement or particularly severe pain after breast cancer surgery.
References
Zhang X, Li Y, Liu D (2019) Effects of exercise on the quality of life in breast cancer patients: a systematic review of randomized controlled trials. Support Care Cancer 27(1):9–21
Loh SY, Musa AN (2015) Methods to improve rehabilitation of patients following breast cancer surgery: a review of systematic reviews. Breast Cancer: Targets and Therapy 7:81
Zaidi S, Hussain S, Verma S et al (2018) Efficacy of complementary therapies in the quality of life of breast cancer survivors. Front Oncol 7:32
Mijwel S, Backman M, Bolam KA, Olofsson E, Norrbom J, Bergh J, Sundberg CJ, Wengström Y, Rundqvist H (2018) Highly favorable physiological responses to concurrent resistance and high-intensity interval training during chemotherapy: the OptiTrain breast cancer trial. Breast Cancer Res Treat 169(1):93–103
Stubblefield MD, Keole N (2014) Upper body pain and functional disorders in patients with breast cancer. PM&R 6(2):170–118
Tantawy SA, Kamel DM (2016) The effect of kinesio taping with exercise compared with exercise alone on pain, range of motion, and disability of the shoulder in postmastectomy females: a randomized control trial. J Phys Ther Sci 28(12):3300–3305
De Groef A, Van Kampen M, Vervloesem N et al (2017) Myofascial techniques have no additional beneficial effects to a standard physical therapy programme for upper limb pain after breast cancer surgery: a randomized controlled trial. Clin Rehabil 31(12):1625–1635
Rafn BS, Hung S, Hoens AM, McNeely M, Singh CA, Kwan W, Dingee C, McKevitt E, Kuusk U, Pao J, van Laeken N, Goldsmith CH, Campbell KL (2018) Prospective surveillance and targeted physiotherapy for arm morbidity after breast cancer surgery: a pilot randomized controlled trial. Clin Rehabil 32(6):811–826
Arman N, Tarakci E, Tarakci D, Kasapcopur O (2019) Effects of video games–based task-oriented activity training (Xbox 360 Kinect) on activity performance and participation in patients with juvenile idiopathic arthritis: a randomized clinical trial. Am J Phys Med Rehabil 98(3):174–181
Yang Z, Rafiei MH, Hall A, Thomas C, Midtlien HA, Hasselbach A, Adeli H, Gauthier LV (2018) A novel methodology for extracting and evaluating therapeutic movements in game-based motion capture rehabilitation systems. J Med Syst 42(12):255
Da Gama A, Fallavollita P, Teichrieb V, Navab N (2015) Motor rehabilitation using Kinect: a systematic review. Games for Health Journal 4(2):123–135
Fager SK, Burnfield JM (2014) Patients’ experiences with technology during inpatient rehabilitation: opportunities to support independence and therapeutic engagement. Disab Rehab: Assistive Technology 9(2):121–127
Parry I, Carbullido C, Kawada J, Bagley A, Sen S, Greenhalgh D, Palmieri T (2014) Keeping up with video game technology: objective analysis of Xbox Kinect™ and PlayStation 3 Move™ for use in burn rehabilitation. Burns 40(5):852–859
Ding ZQ, Luo ZQ, Causo A, Chen IM, Yue KX, Yeo SH, Ling KV (2013) Inertia sensor-based guidance system for upperlimb posture correction. Med Eng Phys 35(2):269–276
Celletti C, Fara MA, Filippi GM et al (2017) Focal muscle vibration and physical exercise in postmastectomy recovery: an explorative study. BioMed Research International 2017
Zengin Alpozgen A, Razak Ozdincler A, Karanlik H, Yaman Agaoglu F, Narin AN (2017) Effectiveness of Pilates-based exercises on upper extremity disorders related with breast cancer treatment. Eur J Cancer Care 26(6):e12532
Liu L, Petrich S, McLaren B, Kelly L, Baxter GD (2018) An integrative Tai Chi program for patients with breast cancer undergoing cancer therapy: study protocol for a randomized controlled feasibility study. J Integr Med 16(2):99–105
Wilson DJ (2017) Exercise for the patient after breast cancer surgery. Semin Oncol Nurs 33(1):98–105
Harris SR, Schmitz KH, Campbell KL, McNeely ML (2012) Clinical practice guidelines for breast cancer rehabilitation: syntheses of guideline recommendations and qualitative appraisals. Cancer 118(S8):2312–2324
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8(12):1153–1157
Wang L, Guyatt GH, Kennedy SA, Romerosa B, Kwon HY, Kaushal A, Chang Y, Craigie S, de Almeida CPB, Couban RJ, Parascandalo SR, Izhar Z, Reid S, Khan JS, McGillion M, Busse JW (2016) Predictors of persistent pain after breast cancer surgery: a systematic review and meta-analysis of observational studies. Can Med Assoc J 188(14):E352–E361
Smoot B, Paul SM, Aouizerat BE et al (2016) Predictors of altered upper extremity function during the first year after breast cancer treatment. Am J Phys Med Rehab/Assoc Acad Physiatrists 95(9):639
Serra-Añó P, Inglés M, Bou-Catalá C, Iraola-Lliso A, Espí-López GV (2019) Effectiveness of myofascial release after breast cancer surgery in women undergoing conservative surgery and radiotherapy: a randomized controlled trial. Supportive Care in Cancer 1-9
Donatelli R, Ellenbecker TS, Ekedahl SR, Wilkes JS, Kocher K, Adam J (2000) Assessment of shoulder strength in professional baseball pitchers. J Orthop Sports Phys Ther 30(9):544–551
Belmonte R, Messaggi-Sartor M, Ferrer M, Pont A, Escalada F (2018) Prospective study of shoulder strength, shoulder range of motion, and lymphedema in breast cancer patients from pre-surgery to 5 years after ALND or SLNB. Support Care Cancer 26(9):3277–3287
Smith TM, Broomhall CN (2016) Physical and psychological effects of a 12-session cancer rehabilitation exercise program. Clin J Oncol Nurs 20(6):653
Harrington S, Michener LA, Kendig T, Miale S, George SZ (2014) Patient-reported upper extremity outcome measures used in breast cancer survivors: a systematic review. Arch Phys Med Rehabil 95(1):153–162
Lundberg M, Styf J, Jansson B (2009) On what patients does the Tampa Scale for Kinesiophobia fit? Physiother Theor Pract 25(7):495–506
Beurskens CH, van Uden CJ, Strobbe LJ, Oostendorp RA, Wobbes T (2007) The efficacy of physiotherapy upon shoulder function following axillary dissection in breast cancer, a randomized controlled study. BMC Cancer 7(1):166
Zeng Y, Zhang JE, Cheng AS, Cheng H, Wefel JS (2019) Meta-analysis of the efficacy of virtual reality–based interventions in cancer-related symptom management. Integrative Cancer Ther 18:1534735419871108
Uhm KE, Lee S, Kurillo G, Han JJ, Yang JH, Yoo YB, Lee J (2019) Usefulness of Kinect sensor–based reachable workspace system for assessing upper extremity dysfunction in breast cancer patients. Supportive Care in Cancer 1-8
Hidding JT, Beurskens CH, van der Wees PJ, van Laarhoven HW, Nijhuis-van der Sanden MW (2014) Treatment related impairments in arm and shoulder in patients with breast cancer: a systematic review. PLoS One 9(5):e96748
Harrington S, Gilchrist L, Sander A (2014) Breast cancer EDGE task force outcomes: clinical measures of pain. Rehab Oncol 32(1):13
Lee JS, Hobden E, Stiell IG, Wells GA (2003) Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med 10(10):1128–1130
Aguilar-Lazcano CA, Rechy-Ramirez EJ, Hu H, Rios-Figueroa HV, Marin-Hernandez A (2019) Interaction modalities used on serious games for upper limb rehabilitation: a systematic review. Games Health J 8(5):313–325
Sin H, Lee G (2013) Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am J Phys Med Rehabil 92(10):871–880
McNeely ML, Campbell K, Ospina M et al (2010) Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev 6:CD005211
Muir SW, Corea CL, Beaupre L (2010) Evaluating change in clinical status: reliability and measures of agreement for the assessment of glenohumeral range of motion. North Am J Sports Phys Ther: NAJSPT 5(3):98–110
Galantino ML, Stout NL (2013) Exercise interventions for upper limb dysfunction due to breast cancer treatment. Phys Ther 93(10):1291–1297
Htut TZC, Hiengkaew V, Jalayondeja C, Vongsirinavarat M (2018) Effects of physical, virtual reality-based, and brain exercise on physical, cognition, and preference in older persons: a randomized controlled trial. Eur Rev Aging Phys Act 15(1):10
Nesvold IL, Reinertsen KV, Fosså SD, Dahl AA (2011) The relation between arm/shoulder problems and quality of life in breast cancer survivors: a cross-sectional and longitudinal study. J Cancer Surviv 5(1):62–72
Campbell KL, Pusic AL, Zucker DS, McNeely ML, Binkley JM, Cheville AL, Harwood KJ (2012) A prospective model of care for breast cancer rehabilitation: function. Cancer 118(S8):2300–2311
Karadibak D, Yavuzsen T, Saydam S (2008) Prospective trial of intensive decongestive physiotherapy for upper extremity lymphedema. J Surg Oncol 97(7):572–577
Yelvar GDY, Çırak Y, Dalkılınç M, Demir YP, Guner Z, Boydak A (2017) Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial. Eur Spine J 26(2):538–545
Kim SS, Min WK, Kim JH, Lee BH (2014) The effects of VR-based Wii fit yoga on physical function in middle-aged female LBP patients. J Phys Ther Sci 26(4):549–552
Acknowledgments
We are grateful to our patients for taking part in this study. Part of this study was presented at the 11th Congress of the European Pain Federation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All study procedures were conducted in line with the rules and principles of the Declaration of Helsinki of the World Medical Association. The study was approved by the Ethics Committee of Acibadem Mehmet Ali Aydinlar University (Protocol ID:ATADEK-2018/9). Written informed consent was obtained from every eligible patient before the initiation of the study procedures.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feyzioğlu, Ö., Dinçer, S., Akan, A. et al. Is Xbox 360 Kinect-based virtual reality training as effective as standard physiotherapy in patients undergoing breast cancer surgery?. Support Care Cancer 28, 4295–4303 (2020). https://doi.org/10.1007/s00520-019-05287-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05287-x