Abstract
Dual left anterior descending artery (LAD) is not an uncommon coronary artery anomaly. Preoperative identification of this anomaly in patients with coronary artery disease is important to develop strategies to ensure complete revascularization of the LAD territory. From April 1996 through February 2022, more than 16,500 patients underwent isolated coronary artery bypass surgery (CABG) by our team. Retrospective review of the angiographic and operative records of these patients revealed 85 cases with stenosis of the dual LAD system. The incidence of dual LAD in patients undergoing CABG is 0.51%. Among the 85 patients, 59 (69.4%) had stenosis of both long and short LADs, whereas the remaining 26 (30.5%) had stenosis of either of the LADs. Among the 59 patients who had stenosis of both the LADs, 26 (44.1%) received a left internal thoracic artery (LITA) sequential graft to bypass both the LADs and two received a LITA-LITA baby-Y graft. And in 31 (52.5%) patients, the longer LAD was revascularized with LITA and the other LAD with saphenous vein graft.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In dual left anterior descending artery (LAD), two different arteries supply blood to the LAD territory. Waterston et al. reported the first case of dual LAD; i.e., the case of Sir James Mackenzie, a type IV dual LAD in the year 1939 [1], and Sajja et al. reported the first series of 4 cases of surgical revascularization of coronary artery disease (CAD) involving dual LAD [2]. The incidence of dual LAD ranges from 1 to 4.18% [3, 4]. Spindola-Franco proposed the original classification of the dual LAD system (types I, II, III, and IV) in 1983 [5]. Additional types and variants have also been described in the literature [6,7,8,9,10,11,12]. Jariwala et al. introduced another classification to include all types and variants of dual LAD [13].
Methods
From April 1996 through February 2022, more than 16,500 patients underwent isolated coronary artery bypass surgery (CABG) by our team. It is a retrospective observational study involving 85 patients with stenosis of the dual LAD system. The angiograms of these 85 patients were reviewed. CABG was performed by using either the on-pump and off-pump technique as reported earlier [14]. Institutional Ethics Committee approval is obtained and individual patient consent was waived off due to retrospective nature of the study.
Statistical analysis
Descriptive statistics have been used to describe numerical data as mean ± SD, and categorical data as frequencies and percentages. SPSS version 28 was used for the statistical analyses.
Results
The incidence of dual LAD in patients undergoing CABG in our practice is 0.51% (85/16500). The preoperative characteristics of this patient cohort are described in Table 1. Out of the 85 patients, 59 (69.4%) patients had stenosis of both long and short LADs, and the remaining 26 (30.5%) patients had stenosis of either short LAD or long LAD. Among the 59 patients who had stenosis in both the LADs, 26 (44.1%) patients received a left internal thoracic artery (LITA) sequential graft and 2 (3.3%) patients received a LITA-LITA baby-Y graft. In the other 31 (52.5%) patients with significant stenosis of both LADs, longer LAD was revascularized with LITA and other LAD was revascularized with saphenous vein graft (SVG). In instances, where short LAD was larger in diameter, the LITA graft was used to revascularize the short LAD, especially if revascularization of both the arteries was not feasible by using sequential artery grafting. In the 26 cases where only one LAD of the dual LAD system was stenosed, LITA graft was used to revascularize the stenosed artery. Intraoperative and postoperative characteristics are described in Table 2. The index of completeness of revascularization was 1.0 ± 0.08 and the number of grafts per patient was 3.94 ± 0.79.
Discussion
Dual LAD coronary anomaly assumes significance in patients with CAD undergoing CABG. The strategies for revascularization of dual LAD have not been reported except for individual case reports. The information about the morphology of this anomaly can be crucial in ensuring complete revascularization of the LAD territory to minimize residual ischemia and avoid postoperative major adverse cardiac events (MACE).
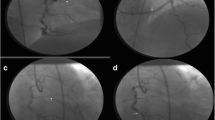
The LAD usually originates from the left main coronary artery and courses anterior to the interventricular septum (IVS) in the anterior interventricular groove or sulcus (AIVS) and runs until the apex of the heart. It gives off multiple diagonal branches to supply the anterior wall of left ventricle and other septal branches to the interventricular septum. The dual LAD system is characterized by a short LAD that terminates high in the AIVS giving off majority of the septal branches, and a long LAD that has a proximal course outside the AIVS and returns back into the AIVS distally giving rise to majority of the diagonal branches. Although the dual LAD system almost always comprises of short and long LAD, both the LADs can occasionally be of equal length. The angiographic images of different types of the Spindola-Franco classification are presented in Fig. 1. And the intraoperative appearance of different types of the Spindola-Franco classification of dual LAD is shown in Fig. 2.
Angiographic images of different types of Spindola classification of dual LAD system (yellow arrows, long LAD; orange arrows, short LAD; blue arrow, dip of the long LAD from surface to the intra-myocardial region). A Type 1, long LAD to the right of short LAD; B type 2, long LAD to the left of short LAD; C type 3, long LAD with an intra-myocardial portion; D type 4, long LAD arising from the right coronary sinus
Awareness and recognition of the pattern of involvement of dual LAD in CAD is important for several reasons [2]. Preoperative recognition of the dual LAD system improves precision in exposing the coronary artery intraoperatively, and correct placement of the arteriotomy [2, 15]. The identification of a short LAD is essential as the septal artery(s) arising from it supplies the basal part of IVS, and a missdiagnosis of a stenosed short LAD may compromise the revascularization of the IVS leading to postoperative residual ischemia with or without MACE. If both the short LAD and the long LAD are severely stenosed, vascular grafting of both the arteries is essential to avoid any residual ischemia.
Understanding the different variants of dual LAD also helps in planning the revascularization strategies in the preoperative phase. In the earlier days, surgical revascularization of patients with CAD involving both arteries of the dual LAD system was predominantly dealt with by using the LITA for the long LAD and the SVG for the short LAD (Fig. 3). This strategy is technically simpler compared to sequential LITA grafting, which was mostly in use in early practice of our coronary revascularization. With emerging literature showing the long-term benefits in survival of using LITA for revascularization and growing expertise in our practice, both the LADs were revascularized using the LITA graft in sequential grafting fashion. If both the LADs were lying close to and parallel to each other, a baby-Y anastomosis was fashioned, of a short segment of distal LITA interposed between the short LAD, and the in situ LITA running to the long LAD. The techniques employed were successful in establishing the revascularization of the myocardium of the dual LAD system as the index of completeness of revascularization (number of grafts performed/number of grafts intended) was 1.
Illustrations of various revascularization strategies employed. A The sequential LITA grafting using a single LITA to revascularize both LADs, B utilization of LITA to revascularize long LAD and the SVG for short LAD, C the LITA-LITA baby-Y grafting when both the LADs are in close proximity to each other. 1, sequential LITA grafting; 2, long LAD; 3, short LAD; 4, LITA graft; 5, SVG; 6, LITA-LITA baby-Y graft
While the location of the coronary ostia is one of the foremost anatomical factors for revascularization by the interventional cardiologist, surgical revascularization is primarily concerned with the relative course of both the arteries in the interventricular groove region for the appropriate placement of an arteriotomy. This contrasting approach to revascularization by surgical and interventional methods makes knowledge of a dual LAD much more critical for a surgeon. Hence, preoperative awareness of a dual LAD system and its spatial orientation in a patient undergoing CABG also helps in avoiding an incorrect placement of the arteriotomy [2, 15] at an intramyocardial location of both the LADs.
In a rare instance, a possibility of dual LAD should always be considered in patients with the angiography showing an unusually short LAD. In cases where the long LAD cannot be visualized intraoperatively, a high-frequency ultrasound can be employed for this purpose.
Limitations
This is a retrospective study and has all the limitations inherent to retrospective study. The data on dual LAD system were retrieved by reviewing the operative records that may have given a false-low incidence of dual LAD system. No comparisons have been drawn between the different revascularization strategies employed.
Conclusion
Dual LAD is not an uncommon anomaly. The options of revascularization for involvement of both the LADs include sequential grafting of LITA and LITA-LITA baby-Y grafting depending on the orientation of the LADs with each other.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Waterston O, Orr J, Cappell DF. Sir James Mackenzie’s Heart. Br Heart J. 1939;1:237–8.
Sajja LR, Farooqi A, Shaik MS, Yarlagadda RB, Baruah DK, Pothineni RB. Dual left anterior descending coronary artery: surgical revascularization in 4 patients. Tex Heart Inst J. 2000;27:292–6.
Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21:28–40.
Morettin LB. Coronary arteriography: uncommon observations. Radiol Clin North Am. 1976;14:189–208.
Spindola-Franco H, Grose R, Solomon N. Dual left anterior descending coronary artery: angiographic description of important variants and surgical implications. Am Heart J. 1983;105:445–55.
Bozlar U, Uğurel MS, Sarı S, Akgün V, Örs F, Tasar M. Prevalence of dual left anterior descending artery variations in CT angiography. Diagn Interv Radiol. 2015;21:34–41.
Manchanda A, Qureshi A, Brofferio A, Go D, Shirani J. Novel variant of dual left anterior descending coronary artery. J Cardiovasc Comput Tomogr. 2010;4:139–41.
Maroney J, Klein LW. Report of a new anomaly of the left anterior descending artery: Type VI dual LAD. Catheter Cardiovasc Interv. 2012;80:626–9.
Subban V, Murdoch D, Pincus M. Dual left anterior descending coronary artery with origin of short left anterior descending coronary artery from left main shaft - a rare coronary anomaly. J Invasive Cardiol. 2014;26:E59–60.
Celik T, Bozlar U, Ozturk C, et al. A new anomaly of the left anterior descending artery: Type X dual LAD. Indian Heart J. 2015;67:S14–7.
Bhargav A, Otaal PS, Singhal MK. Type X dual left anterior descending (LAD) artery masquerading as type 1 LAD — a case report. Egypt J Intern Med. 2021;33:22. https://doi.org/10.1186/s43162-021-00053-0
Lee Y, Lim Y-H, Shin J, Kim K-S.. A case report of type VI dual left anterior descending coronary artery anomaly presenting with non-ST-segment elevation myocardial infarction. BMC Cardiovasc Disord. 2012;12:101.
Jariwala P, Jadhav KP, Koduganti S. Dual left anterior descending artery: diagnostic criteria and novel classification. Indian J Thorac Cardiovasc Surg. 2021;37:285–94.
Sajja LR, Mannam G, Sompali S, et al. Does multi-vessel off-pump coronary artery bypass grafting reduce post-operative morbidity compared to on-pump CABG? Indian J Thorac Cardiovasc Surg. 2004;20:173–77.
Kim SY, Seo JB, Do K-H, et al. Coronary artery anomalies: classification and ECG-gated multi-detector row CT findings with angiographic correlation. Radiographics. 2006;26:317–34.
Acknowledgements
We thank Prashanthi Beri M.Sc. (Clinical Research), Clinical Coordinator, Sajja Heart Foundation, Hyderabad, India, for the help in preparing the manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval, Statement of human and animal rights and Informed consent
This study complies with the principles of the Declaration of Helsinki and was approved by the Institutional Ethics Committee dated 13/Aug/2022 with the reference number SH/RS/IEC/2021-2022/1003 and the need for informed consent from the patient was waived off due to the retrospective nature of this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sajja, L.R., Pusapati, V.R.R., Mannam, G. et al. Surgical revascularization strategies of CAD involving dual left anterior descending artery. Indian J Thorac Cardiovasc Surg 39, 145–149 (2023). https://doi.org/10.1007/s12055-022-01454-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-022-01454-8