Abstract
Purpose
Treatment for hallux valgus (HV) remains challenging. Third-generation percutaneous procedures try to reproduce chevron-type osteotomies to replicate their benefits, such as intrinsic stability and reproducibility. We report the first results using a percutaneous, intra-articular, chevron osteotomy (PeICO) technique that mimics the classic intra-articular open chevron procedure, associated with a percutaneous adductor tendon release (PATR) for the treatment of mild-to-moderate HV.
Methods
From May 2015 to October 2018, a total of consecutive 114 feet (74 patients) were included. Primary outcome measures included radiographic (hallux valgus and intermetatarsal angles) and clinical parameters such as visual analog scale (VAS), FAAM Activities of Daily Living (ADL), and FAAM Sport, AOFAS Score, and MOXFQ, preoperatively and at final follow-up (Minimum 18 months). A patient satisfaction survey was also performed. Pronation and length of the first metatarsal were also assessed. Secondary outcomes included fluoroscopic time, length of surgery, complications, recurrence, and re-operation rates.
Results
At 24.09 months on average, the AOFAS score improved from 52.1 points preoperatively to 91.1 (p < 0.001) at the latest follow-up. VAS decreased from 6.3 to 1. Also, FAAM ALD, FAAM Sport, and MOXFQ showed statistically significant differences (p < 0.001) when comparing pre-operative and post-operative periods. Patients found the procedure to be excellent in 82% and very good in 13.5% of cases. Our global complication and re-operation rates were 5.26% and 3.5% (screw removal), respectively.
Conclusion
PeICO combined with PATR proved to be a safe, reliable, and effective technique for the correction of mild-to-moderate HV deformity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment for hallux valgus (HV) remains challenging. It continues to have a high patient dissatisfaction rate (10.6%), and post-operative first metatarsophalangeal (MTP) pain remains at 1.5% [1], which means that the search for a better procedure must continue. Osteotomies—especially chevron-type—continue to be the method of choice to correct HV deformities [2, 3].
To improve the outcomes, percutaneous surgery (PS) or MIS (“minimally invasive surgery”) has been involved in the process of continuous change [4]. Third-generation or 3G [5,6,7,8,9] procedures reproduce chevron-type osteotomies to replicate their benefits, such as intrinsic stability and reproducibility. They are divided into extra-articular and intra-articular osteotomies. However, there is currently insufficient evidence to recommend PS over open procedures or to recommend one percutaneous approach over another for HV treatment [10, 11].
We report a prospective case series using a percutaneous, intra-articular, chevron osteotomy (PeICO) technique for the treatment of mild-to-moderate HV. PeICO technique is the first published PS technique mimicking the classic intra-articular open chevron procedure. A cadaveric study showed that it is a safe and reliable procedure [12].
Materials and methods
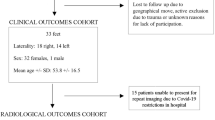
From May 2015 to October 2018, a total of 177 consecutive patients underwent surgical treatment of unilateral/bilateral, painful, mild-to-moderate HV after the failure of conservative treatment. The Bioethics Committee approved the study of our institution. Exclusion criteria for this study included stiffness of first MTP joint described as less than 75° of the full range of motion (ROM) measured by placing a lateral goniometer, osteoarthritis of the MTP-1-joint (grade 1–3), rheumatoid arthritis, patients with diabetes, neurological disorders, hypermobility of the first tarsometatarsal joint, and previous surgery on the same foot. After patient exclusion, 114 feet of 74 patients were included (Fig. 1). The drop-out rate (lost to follow-up) was 30.8%. A 13-year-experienced MIS surgeon performed all the PeICO procedures in association with percutaneous adductor tendon release (PATR).
The radiographic evaluation included pre- and post-operative assessment (minimum follow-up of 18 months) of hallux valgus angle (HVA), intermetatarsal angle (IMA), and distal metatarsal articular angle (DMAA). The severity of hallux valgus was classified according to the HVA (≤ 15°, normal; less than 20°, mild; less than 40°, moderate; equal to or more than 40°, severe) and the IMA (< 9°, normal; 9–11°, mild; 12–17°, moderate; ≥ 18°, severe). The tibial sesamoid position (TSP) was assessed, and the position was classified as grade I to VII. First, metatarsal length and post-operative shortening were also evaluated.
Patients were also evaluated by measuring the range of motion (ROM) of the first MTP joint, pre-operatively and at final follow-up (minimum 18 months). ROM was classified as normal (≥ 75°), moderate stiffness (30–74°), severe stiffness (< 30°), or extension (< 30°).
The first metatarsal head pronation was also assessed using a modification of Yamaguchi’s method [13] (0 to 30°), based on a weight-bearing AP view. Recurrence was defined as an HVA of more than 15° at final follow-up. The length of the first metatarsal was also measured.
Clinical outcomes were assessed using the visual analog scale (VAS), FAAM ADL and FAAM Sport, AOFAS Score, and MOXFQ, pre-operatively and at final follow-up (minimum 18 months). A patient satisfaction survey was also performed, asking patients to assess their scale of satisfaction (scores from 1 to 5:1, unsatisfactory; 2, satisfactory; 3, good; 4, very good; 5, excellent) and whether they would go through the same technique again (question 2: yes/no). All patients were invited to complete the FAAM ADL, FAAM Sport, MOXFQ, VAS, and satisfaction scales by email.
Fluoroscopic time and length of surgery were recorded. Complications were identified by either the patient or the surgeon in outpatient clinics. We used a modification of the reliable adapted Clavien-Dindo-Sink classification for HV surgery and that already assessed a 3G procedure [14] (Table 2). The re-operation rate and screw removal were also evaluated.
Operative technique
The technique can be divided into five steps:
-
1.
A 2.0-mm K-wire was slid percutaneously in the medial surface of the first toe in a distal-to-proximal orientation. A medial portal (P1) was made with a percutaneous surgical blade (SM69, Swann-Morton®) in the limit between the proximal 1/3 and the distal 2/3 of the 1MT head (Fig. 2a–c).
-
2.
A percutaneous dorsal capsular release was made to allow lateral displacement of the first metatarsal head. The hallux must be passive dorsiflexed (30°) to prevent soft tissue lesions (Fig. 2d, e). Then, the ISFS was inserted in a medial-to-lateral direction (until reaching the lateral cortex) through the 1MT head to create the apex of the osteotomy. The dorsal limb describes a 20° angle proximally oriented while the plantar limb is parallel to the floor. It creates two limbs forming the 90° angle of a chevron osteotomy (Fig. 3a–d).
-
3.
First metatarsal displacement—the lateral shift (up to 60%) was performed through a 2-mm K-wire and an angled stem probe. The probe was inserted through the osteotomy, and the K-wire was advanced until proper correction was achieved (Fig. 3e, f).
-
4.
Then, a dorsomedial portal (P2: ≈15 mm proximal and 3 mm dorsal than the P1) was made for osteotomy stabilization. We prefer to use a 3.5-mm cannulated conical screw inserted from dorsal-medial to a lateral-plantar direction at a 45° orientation. After the 2-mm K-wire was removed, a resection of the medial eminence was made through portal 2 using a wedge burr 3.1 (Fig. 4).
-
5.
PATR (percutaneous adductor tendon release) was performed in association with all PeICO procedures, following published descriptions [15, 16].
-
6.
A first metatarsal (base) percutaneous Akin was added through a medial portal in cases of persistent valgus of the great toe, using a weight-bearing intraoperative test (Fig. 5).
Statistical analysis
All statistical analyses were performed using R version 4.0.2. The different variables between each posterior and anterior patient records were constructed, and their normality was analyzed using the Shapiro–Wilk test. Statistical significance was defined as a p value of ≤ 0.05.
Results
The mean age was 45 years (range, 20–75; SD 14), with 69 female and five male patients. The mean follow-up was 24.08 months (range, 18–49; SD 8.53). The mean BMI was 27 ± 4.3 kg/m2. We found 60.6% (69 feet) with mild and 39.4% (45 feet) with moderate HV deformity. The procedures additional to PeICO were one patient (1.35%) needed a DMMO (distal metatarsal minimally invasive osteotomy) of second-to-fourth metatarsals for the treatment of central metatarsalgia; five, sliding DMMO for the treatment of Tailor’s bunion; three, percutaneous osteotomies of the proximal phalanx for lesser toes deformities (2 to 4 toes); and four, Akin osteotomies for the proximal phalanx of the first toe because of residual phalanx malalignment.
The entire patient population presented normal ROM (≥ 75°) in the post-operative period. The preoperative total ROM of the first MTP joint, the plantarflexion, and the dorsiflexion were measured as 104° (normal ROM), 27.7°, and 75.8°, respectively. Following the operation, the values were 96.1°, 25.2°, and 70.9°. Following the operation, the total ROM in the first MTP joint was reduced by 7.4 ± 2.3° (p < 0.001). Passive dorsiflexion decreased by 4.9 ± 1.5° (p < 0.001) and passive plantar flexion by 2.5 ± 0.8° (p < 0.001).
Pre-operatively, 58 feet (51.6%) had radiological signs of pronation. The average rotation deformity was 4.45° (range 0 to 30; SD 6.5). According to recommendations, five patients (2 of 20°, 2 of 30°, and 1 of 25°) needed rotation. Although a rotational PeICO could have benefited these patients, radiological correction (average correction of IMA was 2.5°; HVA 9.14°; and TSP 1.4 mm) and clinical outcomes showed similar results compared to non-pronation cases.
Patients found the procedure to be excellent in 82% of cases (61 feet), very good in 13.5% (10 feet), and good in 4.1% (three feet). Clinical and radiological results are summarized in Table 1.
Fluoroscopic time was 19 seconds (range 11 to 38; SD 6.7). The average length of surgery was 25.4 minutes (range 16 to 50; SD 6.5).
Our global complication rate was 5.26% (6 feet). We had one (0.8%) major complication: a transfer metatarsalgia (to the second metatarsal) successfully treated with insoles. The minor complications presented were the following: three (2.6%) soft tissue irritations that needed screw removal after at least four months post-operatively; one (0.8%) case of superficial infection that needed oral antibiotic treatment for 14 days; one patient (0.8%) presented superficial skin necrosis, but no further surgical debridement was required. We observed no other complications involving the additional procedures. Finally, there was a reoperation rate of 3.5% for screw removal.
Discussion
The most important finding of the present study is that for the first time, a PS technique mimicking the intra-articular open chevron technique showed reliable and sustained radiological, clinical, and satisfaction outcomes, as demonstrated by other percutaneous procedures [9, 17]. Based on the results found in this study, PeICO can be indicated in mild-to-moderate HV deformities.
Reducing TSP has been proposed as a preventive factor for recurrent HV deformity. Chen et al. [18] recommend correcting the TSP to grade IV or less to improve functional outcomes and patient satisfaction when treating HV. Also, Kaufmann et al. [19] found that a chevron osteotomy can significantly correct sesamoid position using a seven part system from pre- to post-operative, and it remained stable throughout the follow-up. Adductor tendon release was shown to be a safe procedure when indicated on patients aged 60 years and associated with a distal chevron osteotomy [20]. Recently, Del Vecchio et al. demonstrate that PATR provides powerful and quantifiable correction of metatarsophalangeal valgus [21]. The present findings suggest that PeICO associated with PATR can achieve adequate TSP correction (average correction of 1.94 grades) without loss of correction at final follow-up.
Pronation of the first metatarsal has been shown as a risk factor for the formation and progression of HV [22, 23]. Therefore, the importance of correcting malrotation to reach a good position and decrease the risk of HV recurrence has been progressively acknowledged. This must be considered in the decision-making process, predominantly in moderate-to-severe cases. Some authors indicate rotational correction treatment when a considerable (> 15°) metatarsal pronation is present [23]. Although five patients needed rotation according to protocol, there were no clinical differences between those with < 15° of pronation deformity.
Excessive shortening of the first metatarsal during first metatarsal osteotomy represents a frequent risk factor for transfer metatarsalgia to the second metatarsal head [24, 25]. This has been reported to occur at rates from 12 to 43% [26]. Recently, Kaufmann et al. showed significant shortening, with a decrease from 62.2 ± 5.3 to 58.8 ± 5.4 mm (P < 0.001) [19]. Nakagawa et al. [25] showed that post-operative shortening of the first metatarsal might lead to transfer metatarsalgia. Their results were 60.6 ± 4.7 (range 52 to 73) in the pre-operative period and 58.7 ± 4.7 (range 45 to 68) in the post-operative period [26]. However, Greeff et al. found just one case of transfer metatarsalgia, with a statistically significant degree of shortening of the first metatarsal relative length, when performing a modified Lapidus procedure. The authors mentioned that the subsequent low transfer metatarsalgia rate could be attributed to the sagittal plane correction and stability [27]. The series presented showed one case of transfer metatarsalgia with a metatarsal shortening of 3.2 mm (before surgery, it was 4.1 shorter than the second metatarsal).
Stiffness of the MTP joint may be a challenging complication after HV correction, especially after intra-articular procedures. Distal open chevron osteotomies showed rigid MTP joints between 1.13 and 27.3% of cases [28]. First-generation (1G) percutaneous osteotomies (Reverdin-Isham) revealed a reduction of the ROM by 15° and moderate or severe stiffness (ROM < 30°) in 2 to 100% of cases [29,30,31]. Also, Bosch-type procedures (2G) showed stiffness rates in 4 to 14% of cases [32, 33]. 3G techniques showed the lowest rate of this postoperative complication: 0 to 7.7% [5, 34]. Although PeICO is a 3G intra-articular osteotomy, it showed no postoperative stiffness. The reason that explains these results may be that a dorsal capsulotomy is needed to shift the first metatarsal head, and the fact that it does not need a capsulorrhaphy may contribute to preserving motion; patients were advised to do active and passive toe movements after 4 weeks.
Recently, a systematic review showed that 2G or Bosch-type osteotomies had an average complication rate of 10% (6% major and 4% minor). 3G or chevron-type procedures presented a 19% rate (8% major and 11% minor) [10]. In the latter procedures, the authors mentioned that if the subgroup (learning curve completed) of patients from the Jowett and Bedi study [5] is excluded, the average complication rate reduces to 12%. Besides this, if we evaluate 2G or 3G studies over 100 feet, the complication rate goes down to 13.4% (Table 2). Our results showed a lower complication rate (5.26% between major and minor ones) than those of 2G or 3G type procedures. Indeed, using two or three screws [5, 8, 14] or not using osteosynthesis [17] may lead to more related complications (fracture of the lateral cortex, screw skin irritation, and delayed bone union, respectively) and a higher re-operation rate.
The average recurrence rate with chevron-type osteotomies is 19.1% (range, between 0 and 75.6%) [35,36,37]. Recurrence is defined as the clinical development of HV after surgical correction (alignment). All patients in our study underwent the PeICO procedure associated with a PATR [15, 16] even in congruent MTP joints. This may have contributed to preventing recurrence (no cases seen at final follow-up).
Screw removal seems to be a frequent indication for a new surgical procedure in 3G procedures [34, 38], ranging from10 to 24%. Recently, Holme et al. [34] showed the results of a MICA procedure for HV treatment, with a complication rate of 10%, representing four patients that required Akin screw removal due to soft tissue irritation. Also, Lee et al. [38] presented a screw removal rate of 24% (6 out of 25 patients). Our screw removal rate was 2.6%. This complication might be avoidable by using specific screws and/or getting adequate oblique radioscopic images.
Some authors report the average mean operating time of percutaneous chevron osteotomy as 64.3 min [7, 34, 39] (range 44.3 to 94.3) to correct mild-to-severe HV deformities. PeICO proved to be a significantly faster procedure (25.4 min on average). Further studies should assess whether PeICO is cost-effective compared with other procedures. Lai et al. showed a fluoroscopic time of 44.6 ± 5.9 seconds when performing a percutaneous chevron-Akin osteotomy [6]. Recently, Palmanovich et al. showed that mean surgery time was reduced to 45 minutes. The number of fluoroscopy expositions was decreased to 70 after two years of experience doing MICA (advanced learning curve) [39]. The average fluoroscopy time of PeICO was 19 seconds. It seems that using fewer screws is crucial, making PeICO faster and dramatically diminishing the need for radiation exposure.
This study’s main limitation is the lack of a control group, which would have been helpful to compare the results with open chevron osteotomies. There is also inherent selection and observer bias because the patients were recruited from a single hospital. Also, surgeries were made by an experienced surgeon. Although it can avoid a performance bias, a complete percutaneous learning curve is needed to achieve the results shown in this study.
The study had some strengths. First, we included a large number of patients available for analysis. Second, the MOXFQ score was used, which is a validated assessment tool to record patient outcomes. Complications were divided and comprehensively evaluated to make future analysis easier.
Conclusion
To our knowledge, the present study is the first to describe the radiological and clinical outcomes of a percutaneous intra-articular chevron-type osteotomy that resembles an open chevron. PeICO combined with PATR proved to be a safe, reliable, and effective technique for correcting mild-to-moderate HV deformity. This technique presented excellent satisfaction rates at a minimum of 18 months of follow-up. It also resulted in a significantly shorter operation and fluoroscopic and a lower rate of surgical site infections when compared with other techniques.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Barg A, Harmer JR, Presson AP et al (2018) Unfavorable outcomes following surgical treatment of hallux valgus deformity: a systematic literature review. J Bone Joint Surg Am 100(18):1563–1573. https://doi.org/10.2106/JBJS.17.00975
Klugarova J, Hood V, Bath-Hextall F et al. (2017) Effectiveness of surgery for adults with hallux valgus deformity: a systematic review. JBI Database System Rev Implement Rep 15(6):1671–1710. https://doi.org/10.11124/JBISRIR-2017-003422.
Matar HE (2020) Platt SR (2020) Overview of randomised controlled trials in hallux valgus surgery (2,184 patients). Foot Ankle Surg S1268–7731(20):30078–30083. https://doi.org/10.1016/j.fas.2020.04.013
Del Vecchio JJ, Ghioldi ME (2020) Evolution of minimally invasive surgery in hallux valgus. Foot Ankle Clin 25(1):79–95. https://doi.org/10.1016/j.fcl.2019.10.010
Jowett CRJ, Bedi HS (2017) Preliminary results and learning curve of the minimally invasive chevron Akin operation for hallux valgus. J Foot Ankle Surg 56(3):445–452. https://doi.org/10.1053/j.jfas.2017.01.002
Kaufmann G, Dammerer D, Heyenbrock F et al (2019) Minimally invasive versus open chevron osteotomy for hallux valgus correction: a randomized controlled trial. Int Orthop 43(2):343–350. https://doi.org/10.1007/s00264-018-4006-8
Lai MC, Rikhraj IS, Woo YL et al (2018) Clinical and radiological outcomes comparing percutaneous chevron-Akin osteotomies vs open scarf-Akin osteotomies for hallux valgus. Foot Ankle Int 39(3):311–317. https://doi.org/10.1177/1071100717745282
Liszka H Gądek A(2020) Percutaneous transosseous suture fixation of the Akin osteotomy and minimally invasive chevron for correction of hallux valgus. Foot Ankle Int 41(9):1079–1091. https://doi.org/10.1177/1071100720935036
Vernois J, Redfern D (2013) Percutaneous chevron; the union of classic stable fixed approach and percutaneous technique. FußSprunggelenk 11(2):70–75
Jeyaseelan L, Malagelada F (2020) Minimally invasive hallux valgus surgery-a systematic review and assessment of state of the art. Foot Ankle Clin 25(3):345–359. https://doi.org/10.1016/j.fcl.2020.05.001
Malagelada F, Sahirad C, Dalmau-Pastor M et al (2019) Minimally invasive surgery for hallux valgus: a systematic review of current surgical techniques. Int Orthop 43(3):625–637. https://doi.org/10.1007/s00264-018-4138-x
Del Vecchio JJ, Ghioldi ME, Uzair AE et al (2019) Percutaneous, intra-articular, chevron osteotomy (PeICO) for the treatment of hallux valgus: a cadaveric study. Foot Ankle Int 40(5):586–595. https://doi.org/10.1177/1071100718820696
Yamaguchi S, Sasho T, Endo J et al (2015) Shape of the lateral edge of the first metatarsal head changes depending on the rotation and inclination of the first metatarsal: a study using digitally reconstructed radiographs. J Orthop Sci 20(5):868–874. https://doi.org/10.1007/s00776-015-0749-x
Lewis TL, Ray R, Miller G et al (2021) Third-generation minimally invasive chevron and Akin osteotomies (MICA) in hallux valgus surgery: two-year follow-up of 292 cases. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.20.01178
Dalmau-Pastor M, Malagelada F, Cordier G et al (2020) Anatomical study of minimally invasive lateral release techniques for hallux valgus treatment. Foot Ankle Int 1071100720920863. https://doi.org/10.1177/1071100720920863
Del Vecchio JJ, Dalmau-Pastor M (2020) Percutaneous lateral release in hallux valgus: anatomic basis and indications. Foot Ankle Clin 25(3):373–383. https://doi.org/10.1016/j.fcl.2020.05.003
Lucattelli G, Catani O, Sergio F et al (2020) Preliminary experience with a minimally invasive technique for hallux valgus correction with no fixation. Foot Ankle Int 41(1):37–43. https://doi.org/10.1177/1071100719868725
Chen JY, Rikhraj K, Gatot C et al (2016) Tibial sesamoid position influence on functional outcome and satisfaction after hallux valgus surgery. Foot Ankle Int 37(11):1178–1182. https://doi.org/10.1177/1071100716658456
Kaufmann G, Sinz S, Giesinger JM et al (2019) Loss of correction after chevron osteotomy for hallux valgus as a function of preoperative deformity. Foot Ankle Int 40(3):287–296. https://doi.org/10.1177/1071100718807699
Seo JH, Lee HS, Choi YR, Park SH (2020) Distal chevron osteotomy with lateral release for moderate to severe hallux valgus patients aged sixty years and over. Int Orthop 44(6):1099–1105. https://doi.org/10.1007/s00264-020-04562-5
Del Vecchio JJ, Cordier G, Dealbera ED et al (2021) Correction power of percutaneous adductor tendon release (PATR) for the treatment of hallux valgus: a cadaveric study. J Foot Ankle Surg 9:S1067–2516(21)00121–6. https://doi.org/10.1053/j.jfas.2021.02.012.
Okuda R, Kinoshita M, Yasuda T et al (2007) The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am 89(10):2163–2172. https://doi.org/10.2106/JBJS.F.01455
Wagner P, Wagner E (2018)Is the rotational deformity important in our decision-making process for correction of hallux valgus deformity? Foot Ankle Clin 23(2):205–217. https://doi.org/10.1016/j.fcl.2018.01.009
Espinosa N, Maceira E, Myerson MS (2008) Current concept review: metatarsalgia. Foot Ankle Int 29(8):871–879. https://doi.org/10.3113/fai.2008.0000
Nakagawa S, Fukushi J, Nakagawa T et al (2016) Association of metatarsalgia after hallux valgus correction with relative first metatarsal length. Foot Ankle Int 37(6):582–588. https://doi.org/10.1177/1071100716634792
Foran IM, Mehraban N, Jacobsen SK et al (2020) Radiographic impact of Lapidus, proximal lateral closing wedge osteotomy, and suture button procedures on first ray length and dorsiflexion for hallux valgus. Foot Ankle Int 41(8):964–971. https://doi.org/10.1177/1071100720925438
Greeff W, Strydom A, Saragas NP et al (2020) radiographic assessment of relative first metatarsal length following modified Lapidus procedure. Foot Ankle Int 41(8):972–977. https://doi.org/10.1177/1071100720924016
Vopat BG, Lareau CR, Johnson J et al (2013) Comparative study of scarf and extended chevron osteotomies for correction of hallux valgus. Foot Ankle Spec 6(6):409–16. https://doi.org/10.1177/1938640013508431
Bauer T, de Lavigne C, Biau D et al (2009) Percutaneous hallux valgus surgery: a prospective multicenter study of 189 cases. Orthop Clin North Am 40(4):505–514. https://doi.org/10.1016/j.ocl.2009.05.002
Biz C, Fosser M, Dalmau-Pastor M et al (2016) Functional and radiographic outcomes of hallux valgus correction by mini-invasive surgery with Reverdin-Isham and Akin percutaneous osteotomies: a longitudinal prospective study with a 48-month follow-up. J Orthop Surg Res 11(1):157. https://doi.org/10.1186/s13018-016-0491-x
Severyns M, Carret P, Brunier-Agot L et al (2019) Reverdin-Isham procedure for mild or moderate hallux valgus: clinical and radiographic outcomes. Musculoskelet Surg 103(2):161–166. https://doi.org/10.1007/s12306-018-0563-7
Bia A, Guerra-Pinto F, Pereira BS et al (2018) Percutaneous osteotomies in hallux valgus: a systematic review. J Foot Ankle Surg 57(1):123–130. https://doi.org/10.1053/j.jfas.2017.06.027
Faour-Martín O, Martín-Ferrero MA, Valverde García JA et al (2013) Long-term results of the retrocapital metatarsal percutaneous osteotomy for hallux valgus. Int Orthop 37(9):1799–803. https://doi.org/10.1007/s00264-013-1934-1
Holme TJ, Sivaloganathan SS, Patel B (2020) Third-generation minimally invasive chevron Akin osteotomy for hallux valgus. Foot Ankle Int 41(1):50–56. https://doi.org/10.1177/1071100719874360
Choi GW, Kim HJ, Kim TS et al (2016) Comparison of the modified McBride procedure and the distal chevron osteotomy for mild to moderate hallux valgus. J Foot Ankle Surg. 55(4):808–11. https://doi.org/10.1053/j.jfas.2016.02.014
Jeuken RM, Schotanus MG, Kort NP et al (2016) Long-term follow-up of a randomized controlled trial comparing scarf to chevron osteotomy in hallux valgus correction. Foot Ankle Int 37(7):687–95. https://doi.org/10.1177/1071100716639574
Lagaay PM, Hamilton GA, Ford LA et al (2008) Rates of revision surgery using Chevron-Austin osteotomy, Lapidus arthrodesis, and closing base wedge osteotomy for correction of hallux valgus deformity. J Foot Ankle Surg Jul-Aug 47(4):267–272. https://doi.org/10.1053/j.jfas.2008.03.002
Lee M, Walsh J, Smith MM et al (2017) Hallux valgus correction comparing percutaneous chevron/Akin (PECA) and open scarf/Akin osteotomies. Foot Ankle Int 38(8):838–846. https://doi.org/10.1177/1071100717704941
Palmanovich E, Ohana N, Atzmon R et al (2020) MICA: a learning curve. J Foot Ankle Surg 59(4):781–783. https://doi.org/10.1053/j.jfas.2019.07.027
Acknowledgements
We would like to thank Debora Chan for her contribution to this study (statistical analysis). Also, we would like to acknowledge Patricia Plantarrosa, Javier Prieto, Andrés Caporaso, and Pablo Morgillo for their help during surgeries.
Author information
Authors and Affiliations
Contributions
All the authors participated in the study design, have contributed to the collection of the data, have participated in the writing of the manuscript, and assume full responsibility for the content of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Bioethics Committee of our institution.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Del Vecchio, J.J., Ghioldi, M.E., Chemes, L.N. et al. Percutaneous, intra-articular, chevron osteotomy (PeICO) for the treatment of mild-to-moderate hallux valgus: a case series. International Orthopaedics (SICOT) 45, 2251–2260 (2021). https://doi.org/10.1007/s00264-021-05111-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05111-4