Abstract
The AmpliChip™ CYP450 Test, which analyzes patient genotypes for cytochrome P450 (CYP) genes CYP2D6 and CYP2C19, is a major step toward introducing personalized prescribing into the clinical environment. Interest in adverse drug reactions (ADRs), the genetic revolution, and pharmacogenetics have converged with the introduction of this tool, which is anticipated to be the first of a new wave of such tools to follow over the next 5–10 years. The AmpliChip™ CYP450 Test is based on microarray technology, which combines hybridization in precise locations on a glass microarray and a fluorescent labeling system. It classifies individuals into two CYP2C19 phenotypes (extensive metabolizers [EMs] and poor metabolizers [PMs]) by testing three alleles, and into four CYP2D6 phenotypes (ultrarapid metabolizers [UMs], EMs, intermediate metabolizers [IMs], and PMs) by testing 27 alleles, including seven duplications.
CYP2D6 is a metabolic enzyme with four activity levels (or phenotypes): UMs with unusually high activity; normal subjects, known as EMs; IMs with low activity; and PMs with no CYP2D6 activity (7% of Caucasians and 1–3% in other ethnic groups). Levels of evidence for the association between CYP2D6 PMs and ADRs are relatively reasonable and include systematic reviews of case-control studies of some typical antipsychotics and tricyclic antidepressants (TCAs). Evidence for other phenotypes is considerably more limited. The CYP2D6 PM phenotype may be associated with risperidone ADRs and discontinuation due to ADRs. Venlafaxine, aripiprazole, duloxetine, and atomoxetine are newer drugs metabolized by CYP2D6 but studies of the clinical relevance of CYP2D6 genotypes are needed. Non-psychiatric drugs metabolized by CYP2D6 include metoprolol, tamoxifen, and codeine-like drugs.
CYP2C19 PMs (3–4% of Caucasians and African Americans, and 14–21% of Asians) may require dose adjustment for some TCAs, moclobemide, and citalopram. Other drugs metabolized by CYP2C19 are diazepam and omeprazole.
The future of pharmacogenetics depends on the ability to overcome serious obstacles, including the difficulties of conducting and publishing studies in light of resistance from grant agencies, pharmaceutical companies, and some scientific reviewers. Assuming more studies are published, pharmacogenetic clinical applications may be compromised by economic factors and the lack of physician education. The combination of a US FDA-approved test, such as the AmpliChip™ CYP450 Test, and an FDA definition of CYP2D6 as a ‘valid biomarker’ makes CYP2D6 genotyping a prime candidate to be the first successful pharmacogenetic test in the clinical environment. One can use microarray technology to test for hundreds of single nucleotide polymorphisms (SNPs) but, taking into account the difficulties for single gene approaches such as CYP2D6, it is unlikely that very complex pharmacogenetic approaches will reach the clinical market in the next 5–10 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This article describes the AmpliChip™ CYP450 Test, the first commercially available clinical tool based on microarray technology. The introduction of this new technology is a major step toward introducing ‘personalized prescription’ into the clinical environment. We present a view of the main historical events leading to the development of the AmpliChip™ CYP450 Test, its current status and potential use, and finally an opinion on its future potential, focusing on obstacles and suggesting how to overcome them so that this tool and similar new technologies can be introduced into standard clinical practice. Obviously, of the three sections of this article (past, present, and future) the future is least supported by objective data and more tainted by our personal views and biases. These biases include a research clinician working for 10 years on integrating pharmacogenetics into clinical practice to improve his psychiatric patients’ treatment, and two of his research team members, a laboratory technician and a clinical research nurse, who are helping him accomplish this task.
1. The Past
The development of the first commercially available clinical application of microarray technology reflects the intersection of three major historical interests: adverse drug reactions (ADRs), the genetic revolution, and pharmacogenetics. These roads are finally converging with the approval and marketing of the AmpliChip™ CYP450 Test. It is anticipated that this tool is only the first of a new wave of pharmacogenetic tools that may reach the clinic in the next 5–10 years. A second pharmacogenetic test, the Invader® UGT1A1 Molecular Assay, has already been approved by the FDA.
1.1 Adverse Drug Reactions
Several studies and meta-analyses have focused on the monetary costs of ADRs.[1–3] In both the US and Europe, ADRs account for an estimated 3–7% of all hospitalizations.[4] ADR classification methods vary,[5,6] but from the pharmacogenetics viewpoint, it seems prudent to utilize the current knowledge available to clinicians to distinguish those that are preventable from those that are not.[6] According to Classen et al.,[7] almost half of ADRs, resulting from medication errors, overdose and drug-drug interactions, are preventable, and prevention programs have been encouraged.[8] Among ADRs that are not easily prevented, pharmacogenetics may have a role in prevention of some types, which may be associated with relatively frequent gene variations such as those expected based on pharmacological action and that are usually well characterized in pre-marketing studies (typically ~1500 patients). More difficult to prevent are the unusual or unexpected ADRs that are typically detected in post-marketing surveillance, although pharmacogenetics may have some role in those associated with rare gene variants. The major potential of pharmacogenetics can be understood if one considers that 10% of the new drugs introduced to the US market in the last 25 years were withdrawn or labeled with a ‘black box’ warning.[9]
Drug-related problems[10] include any deviation from the intended beneficial effect, thus including both ADRs and also lack of response to typical doses. Drug-related problems fit even better than ADRs with the economic benefit of pharmacogenetic testing and the idea that genetics may mean that individuals require treatment with lower or higher than the standard recommended doses of a drug. Using this concept, Ernst and Grizzle[11] estimated that in the year 2000 the mean cost in the US ambulatory care environment for a drug treatment failure was $US977, the mean cost for ADRs was $US 1105, and the combination cost $US 1488. The overall cost of drug-related problems in the US was estimated to be $US 177.4 billion. Furthermore, our pilot pharmacogenetic study in a psychiatric hospital suggested that CYP2D6 genetic variations that are probably associated with both lack of response and ADRs may increase costs.[12]
1.2 The Genetic Revolution
The genetic revolution has been the result of the development of new technologies permitting genetic testing in an automated, efficient way, and enabling the sequencing of the entire human genome. It has been stressed in both scientific[13] and lay journals[14] that the Human Genome Project has been a major and potentially revolutionary medical advance. Moreover, McKusick[15] compared it with an anatomy textbook written in 1543 that played a leading role in the development of modern medicine.
One major technological advance in genetic testing has been the development of DNA microarrays, also known as DNA chips or GeneChips®. The latter name was given by Fodor,[16] who developed this technology for massive parallel genotyping. Its biological base is the hybridization process, the capacity that each DNA strand carries to recognize its uniquely complementary sequence through base pairing. In developing the GeneChip®, Affymetrix, Inc., which was co-founded by Fodor in 1993, combined two key technologies: (i) a light-directed combinatorial chemistry enabling the synthesis of over 15 000 oligonucleotide sequences in precise locations on a glass microarray, and (ii) a laser fluorescence scanning system permitting identification of molecular interactions in some areas of the array and excluding inactive areas.[16] The GeneChip® originally allowed simultaneous testing of hundreds of DNA sequences in a relatively simple, inexpensive way by placing specific oligonucleotide sequences in different specific areas of a glass microarray. This has evolved to inserting other gene products including proteins in chips, such that the tissue microarrays permit simultaneous protein, RNA, and DNA expression testing in multiple tissue samples, changing basic medical and biological research.[17]
1.3 Pharmacogenetics and Personalized Prescription
The development of genomic medicine and genetic testing has helped in diagnosing some relatively rare and unusual disorders. Of potentially greater importance is the field of pharmacogenetics or pharmacogenomics, possibly the driving force for the implementation of genetic medicine in primary care.[18–20] Vogel[21] coined the term ‘pharmacogenetics’ in 1959; it is usually defined as the study of variability in drug response due to heredity.[22] For historical reasons, pharmacogenetics is frequently used to describe studies of the genes determining drug metabolism, as they are the best known group of genes involved in drug response, but the field also includes the study of the lesser known genes involved in drug pharmacodynamics. More recently, the term ‘pharmacogenomics’ is being used, a broader term encompassing all genes in the genome that may determine drug response.[22] The distinction is arbitrary, as both terms are used interchangeably.[22]
Other related terms are ‘personalized or individualized prescription.’ In 1997, the journal Science[23] included ‘personalized prescription’ or ‘tailoring drugs to a patient’s genetic makeup’ in the six research horizons for 1998. In 1999, the lay journal Time predicted that in 2015 a GeneChip® would be used to tailor medications to each patient’s genes and prevent ADRs.[24] In 2001, Collins and McKusick[25] predicted in JAMA that “By 2020 … The pharmacogenomic approach for predicting drug responsiveness will be standard practice for quite a number of disorders and drugs”.
The idea that ‘personalized prescription’ is coming soon is reflected by the fact that almost all pharmacological or general medical journals have published optimistic reviews on the subject since 1999. Similarly, reflecting the promise of the field, several pharmacogenomics-focused journals were created between 2000 and 2001. Although the literature is saturated with reviews promising that ‘personalized prescription’ is imminent, there is a lack of sufficient pharmacogenetic studies in the clinical environment. Dissenting views on the promise of pharmacogenetics/pharmacogenomics have only started to appear recently.[26,27] In section 1.3.1 we review the CYP2D6 pharmacogenetic story, leading to the application for US FDA approval of the first pharmacogenetic test using the microarray technology.
1.3.1 The Cytochrome P450 (CYP) 2D6 Story
The cytochrome P450 (CYP) enzyme CYP2D6 is a metabolic liver enzyme accounting for only 2–4% of hepatic CYPs.[28] CYP2D6 may be important for metabolizing plant toxins such as alkaloids and is estimated to be responsible for metabolizing approximately 25% of drugs known to be metabolized by CYPs.[29] Many of these drugs are antipsychotic or antidepressant drugs, making it an important metabolic enzyme for psychiatry. The gene encoding this enzyme (CYP2D6) is located on chromosome 22. The CYP2D6 enzyme is expressed constitutively in several tissues, particularly the liver, and enzyme activity (i.e. drug metabolism phenotype) is mainly determined by the type of CYP2D6 gene variant. The only significant environmental factor possibly modifying the phenotype is the intake of potent inhibitors such as quinidine, paroxetine, bupropion, or fluoxetine. This makes CYP2D6 a good candidate for pharmacogenetic testing, because the fewer important environmental influences there are on a metabolic enzyme, the easier it is to detect the effects of a genetic polymorphism.
Historical advances in our understanding of CYP2D6 are closely related to pharmacogenetic advances[29] since CYP2D6 has been one of the most important success stories in pharmacogenetics (table I).[19,30–35] More than 50 polymorphic alleles have been described in CYP2D6; the most frequent of these are described in table II. The activity of the CYP2D6 enzyme is extremely variable because of these polymorphisms and can be expressed as four main levels of activity (phenotypes).[36] In the traditional view, the ultrarapid metabolizer (UM) has three or more copies of the active CYP2D6 gene and exhibits extremely high CYP2D6 activity. Some authors suggest that only some UMs have additional copies. Lovlie et al.[37] proposed that current genotyping methods identified only approximately 20% of CYP2D6 UMs (80% are currently missed by genetic testing) and that upstream polymorphisms may also be associated with unusually high activity in some individuals. The normal subject, or extensive metabolizer (EM), has one or two functional copies of the CYP2D6 gene and displays typical CYP2D6 activity. Intermediate metabolizer (IM) usually refers to a subject with one non-functional CYP2D6 allele and an allele that expresses as an enzyme with low activity. Other groups consider individuals with one functional copy of CYP2D6 as IM instead of EM.[38] In reality, with our current limited knowledge, this distinction between IMs and EMs is more important for researchers than for clinicians since their clinical relevance needs to be demonstrated. Poor metabolizers (PMs) are individuals with two non-functional CYP2D6 alleles and no CYP2D6 activity.
The level of evidence for the association between the CYP2D6 PM phenotype and ADRs is relatively reasonable and includes systematic reviews of case-control studies of antipsychotics and antidepressants[38,39]. Information on the clinical meaning of the CYP2D6 IM phenotype and various EM phenotypes is very limited. Most information on CYP2D6 UMs comes from case reports. The identification of CYP2D6 PM phenotype is more reliable than the identification of other phenotypes and there is good and consistent agreement on the definition of a CYP2D6 PM. Thus, the presence or absence of a CYP2D6 PM phenotype after CYP2D6 genotyping is currently the most important clinical distinction. Moreover, although clinical laboratories do not currently test for all known alleles, a subject classified as a CYP2D6 PM today is unlikely to be reclassified as another CYP2D6 phenotype in 10 years. Similarly, a subject classified as another CYP2D6 phenotype today is unlikely to be reclassified as a CYP2D6 PM in 10 years. Unfortunately, patients in the other subgroups (CYP2D6 IMs, EMs, or UMs) may be subject to some classification instability because of advances in knowledge or in the genotyping technology. It will take several years to fully understand the clinical implications of UM, EM, and IM phenotypes.
European studies suggest that close to 90% of the Caucasian population are EMs, 7% are PMs, and 1–10% are UMs.[29] The proportion of PMs in other ethnic groups is 1–3%. The proportion of UMs is much higher in other populations; it is approximately one of four in North Africa and the Middle East. IMs are much more frequent in East Asian populations where the PM phenotype is rare. In the author’s area of the US (Kentucky), with approximately 88% Caucasians and 12% African Americans, we find approximately 6% CYP2D6 PMs and 3–4% CYP2D6 UMs.[39]
1.3.2 CYP2D6 Genotyping in Psychiatric Research in the 1990s
An increasing number of studies focused on the association of CYP2D6 allelic variations with therapeutic or toxic effects after psychopharmacological treatments for both antipsychotics[40–43] and antidepressants.[44–48] A small group of European pharmacologists and psychiatrists developed guidelines for antidepressant administration according to CYP genotyping;[49,50] more recently, a systematic review has been completed of all available data on antipsychotics and antidepressants.[38] As far as we can tell, there are few systematic attempts to test these guidelines in the clinical environment and they are not widely used by prescribing psychiatrists. A new, simpler guide for clinicians has recently been developed.[39]
Although all CYP2D6 phenotypes may have some effects on response to drugs dependent on CYP2D6 metabolism, it is reasonable to focus on CYP2D6 PMs first, since these individuals are most likely to show differences and increased risk of ADRs. However, in order to conduct such studies, one must recruit >400 Caucasians to get a reasonable number of CYP2D6 PMs (n = 30); other ethnic populations are not good study candidates, as thousands of subjects would be required in order to obtain a large number of CYP2D6 PMs. Thus far, most studies have included too few CYP2D6 PMs to rule out or firmly establish that CYP2D6 has a significant role in drug responses. The methodological difficulties are obvious: (i) randomized prospective studies using pharmacogenetics pose ethical difficulties in psychiatric populations; and (ii) naturalistic studies require even larger samples (several hundred patients) with corrections necessary for confounders using statistical methods.
Our interest has been in testing CYP2D6 genotyping in the real world. Our pilot study[51] included 100 consecutive psychiatric admissions genotyped using a primitive version of the CYP2D6 DNA microarray. The study suggested that the CYP2D6 PM phenotype was associated with a greater incidence of ADRs, and that both CYP2D6 PM and UM phenotypes appear to be associated with the potential for higher treatment costs due to the extended length of hospitalization.[12] The use of tricyclic antidepressants (TCAs) and typical antipsychotics has declined in US psychiatric clinical practice, so we focused on risperidone.[43] Studies from the marketer of risperidone have suggested that risperidone and its main metabolite 9-hydroxyrisperidone have similar pharmacodynamics, and implied that total plasma risperidone moiety (the sum of plasma risperidone and 9-hydroxyrisperidone concentrations) determines the clinical activity.[52] If this is correct, it would be very helpful for marketing purposes since CYP2D6 metabolizes risperidone to 9-hydroxyrisperidone; the equal activity of risperidone and 9-hydroxyrisperidone eliminates any concerns regarding the CYP2D6 polymorphism. The pharmaceutical company defended the idea of the irrelevance of CYP2D6 polymorphism based on one study using single doses, measuring prolactin levels and plasma levels where PMs and EMs had similar total plasma concentrations of the total risperidone moiety. Unfortunately, only 12 subjects (two PMs, one IM and nine EMs) were studied by CYP2D6 phenotyping;[52] furthermore, taking single risperidone doses by different routes can hardly be considered similar to clinical practice. This initial study led to the package insert for risperidone proposing that CYP2D6 expression polymorphism and CYP drug-drug interactions (DDIs) were therapeutically unimportant for risperidone. We were puzzled by the finding that DDI indicated that CYP3A also metabolized risperidone[53] (this was later verified by an in vitro study[54]), and, second, by the finding that all five CYP2D6 PMs we identified had problems with risperidone.[45]
2. The Present
This section includes a discussion on the current status of genotyping in oncology, then focuses on two genes included on the AmpliChip™ CYP450 (CYP2D6 and CYP2C19), and finishes with the current status of genotyping methods, focusing on the AmpliChip™ CYP450.
2.1 Current Status of Genotyping in Oncology and AIDS Therapy
Oncology is the medical specialty where molecularly targeted drugs appear most advanced and promising[55]. The availability of tumor tissue samples allows testing for very specific drug targets (expressed proteins) within the tumor cells and the use of monoclonal antibodies to treat the tumor. This has led to specific treatments, the first of which was trastuzumab, a humanized monoclonal antibody specific for HER2/neu, which has revolutionized the management of metastatic HER2-overexpressing breast cancers.[56] Other monoclonal antibodies are being tested.[57] Because oncology involves treating very lethal diseases with very toxic and expensive medications, new tests are welcome and often readily accepted.
Oncology as a focus of pharmacogenetic testing is also rapidly moving forward. A polymorphic glucuronidation enzyme (uridine diphosphate [UDP]-glucuronosyltransferase 1A1, UGT1A1) plays a role in detoxification of the active metabolite of irinotecan, a drug used to treat colorectal cancer.[58] In August of 2005, the FDA approved the Invader® UGT1A1 Molecular Assay by Third Wave Technologies, Inc., the first UGT1A1 pharmacogenetic test.[59]
Another genotyping testing used in medicine is the TRUGENE™ HIV-1 Genotyping Kit (Visible Genetics Inc.) that allows for detecting genetic variations that would make the virus resistant to some antiretroviral drugs. Recent review articles discuss whether this test is helpful or makes treatment more difficult.[60,61]
2.2 The Current Status of CYP2D6 and CYP2C19 Knowledge
2.2.1 Recent Psychiatric Studies Using CYP2D6 Genotyping
In their excellent and comprehensive review, Kirchheiner et al.[38] recommended the following doses for CYP2D6 PMs: (i) half of the average TCA dose; and (ii) approximately half to two-thirds of the dose for several typical antipsychotics (thioridazine, perphenazine, haloperidol, and zuclopenthixol). They reported that the CYP2D6 PM phenotype may have more potential to be associated with cardiotoxic events in patients receiving venlafaxine, and commented that CYP2D6 UM phenotypes may negatively impact TCA or haloperidol response, probably due to very high clearance.
We found in a large case-control risperidone study[62] that CYP2D6 may have clinical relevance. This was a naturalistic non-controlled study; the patients were classified in two non-overlapping groups — risperidone treated (325 subjects) and discontinued from risperidone (212 subjects). Statistical analyses were corrected for confounders and established that the CYP2D6 PM phenotype determined by genotyping (including using the AmpliChip™ CYP450) predicted the risk of risperidone-associated ADRs, and whether the CYP2D6 PM phenotype predicted the risk of risperidone discontinuation due to ADRs. It was surprising that the CYP2D6 PM phenotype effect was detected in both groups, amidst the noise associated with multiple doctors prescribing different risperidone dosages, different co-medications, and for different indications. More importantly, the CYP2D6 PM phenotype obtained by genotyping was the only significant variable in the two patient groups.
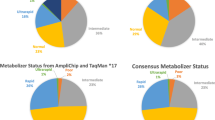
The clinical relevance of the CYP2D6 PM phenotype can be addressed from two points of view: that of the individual and that of the population as a whole (i.e. public health approach). The individual point of view addresses the rhetorical question: if I (or my family member) am a CYP2D6 PM, is it important to have a CYP2D6 genotype test? The data suggest that it is, since the risperidone ADR risk appears to increase 2.5- to 6-fold (table III) for this phenotype. Moreover, the CYP2D6 PM phenotype was the best, most consistent predictor of ADRs since it was the only significant variable in the two sample sets. From the public health perspective (e.g. how important is CYP2D6 genotyping for a psychiatric hospital administrator who wants to reduce risperidone ADRs?), one must examine the group data of patients with ADRs. The data appear to suggest that only 10–20% of risperidone problems may be explained by CYP2D6 PM phenotypes (figure 1 and figure 2). However, there was an identified cause of risperidone ADRs in only about half of the cases.
Causes of clinically relevant risperidone adverse drug reactions (ADRs) in 72 patients. This provides an idea of the public health (or group) importance of the cytochrome P450 (CYP) 2D6 poor metabolizer (PM) phenotype according to this case-control risperidone study of 325 patients taking risperidone.[62] Three variables were associated with an increase of ADRs in risperidone: (i) CYP2D6 PM phenotype, (ii) taking typical antipsychotics (APs) along with risperidone; and (iii) having an organic central nervous system (CNS) disorder. From the 72 with risperidone ADRs, 16% (12/72) had a CYP2D6 PM phenotype, 7% (5/72) were taking typical APs, 7% (5/72) were taking typical APs and had a CNS disorder, 29% (30/72) had a CNS disorder, and 41% (30/72) had no known cause.
Causes of risperidone adverse drug reactions (ADRs) in 81 patients discontinued from risperidone due to ADRs.[62] This provides an idea of the public health (or group) importance of the cytochrome P450 (CYP) 2D6 poor metabolizer (PM) phenotype according to this case-control risperidone study of 212 patients discontinued from risperidone. Two variables were significantly associated with an increase of discontinuation of risperidone due to ADRs: CYP2D6 PM phenotype and taking CYP-inhibiting drugs. Of this subset of patients, 9% (7/81) had a CYP2D6 PM phenotype, 38% (31/81) were taking CYP-inhibiting drugs, and 53% (43/81) had no known cause of the ADRs.
Risk of risperidone adverse drug reactions (ADRs) in a case-control risperidone study.[62] Relative importance of the CYP2D6 poor metabolizer (PM) phenotype compared with other significant causes in the analyses and with patients with no known cause of ADRs or discontinuation due to ADRs. This provides an idea of the importance of the cytochrome P450 (CYP) 2D6 PM phenotype for the individual.
This idea that CYP2D6 PMs are more prone to toxicity during risperidone treatment does not fit well with the idea defended by the risperidone marketer[52] that in in vitro studies, risperidone and its CYP2D6 metabolite (9-hydroxyrisperidone) have similar pharmacodynamic activity. Barnhill et al.[63] suspected that the CYP2D6 PM profile with higher relative plasma risperidone concentrations may be more ‘toxic.’ Although it has not been studied in humans, a recent rat study suggested that risperidone may cross the blood-brain barrier more easily than 9-hydoxyrisperidone,[64] which may contribute to major toxicity.
2.2.2 CYP2D6 Genotyping in Other Areas of Medicine
Codeine, oxycodone, hydrocodone, and possibly tramadol as well as dihydrocodeine are prodrugs activated by CYP2D6 (e.g. codeine is transformed to morphine by CYP2D6; morphine is the analgesic). It was initially reported that CYP2D6 PMs may be less prone to abuse codeine.[65] CYP2D6 PMs may have no analgesic effects from codeine-like drugs, while CYP2D6 UMs may have unusual responses to codeine-like drugs.[66] Metoprolol, a β-adrenoceptor antagonist, is metabolized by CYP2D6; CYP2D6 PMs appear to have a 4- to 5-fold increase in risk of metoprololassociated ADRs.[67] In patients with breast cancer, tamoxifen response may be influenced by the CYP2D6 genotype, and by selective serotonin reuptake inhibitors (SSRIs) that inhibit CYP2D6.[68]
2.2.3 CYP2C19 Genotyping
CYP2C19 was initially described as S-mephenytoin hydroxylase. Caucasians and African Americans comprise approximately 3–4% of CYP2C19 PMs (with no enzyme) versus 14–21% of Asians.[69]
Kirchheiner et al.[38] recommend adjusting the dose by approximately half (60%) in CYP2C19 PMs for some TCAs (amitriptyline, clomipramine, doxepin, imipramine, and trimipramine) and for two other antidepressants, moclobemide and citalopram. Diazepam is another psychiatric drug whose metabolism depends on CYP2C19. A non-psychiatric drug, omeprazole, is dependent on CYP2C19; low doses appear to be very effective in curing peptic ulcers in CYP2C19 PMs, but not in CYP2C19 EMs.[70]
2.2.4 Clinical Value of Combined CYP2D6 and CYP2C19 Genotyping
Steimer et al.[71] conducted a very interesting prospective blind study in 50 Caucasians with depression who received a fixed dose of amitriptyline. They propose combining CYP2D6 and CYP2C19 genotyping, and recommend using amitriptyline in the two-thirds of patients with low ADR risk, which may be much more cost effective than using new antidepressants as the first line of treatment. Unfortunately, in the US, this approach is not realistic. Physicians, including psychiatrists, have mostly abandoned the old TCAs (which tend to be CYP2D6-dependent) for new drugs, particularly the SSRIs. This limits the value of the strategy of combining amitriptyline with CYP2D6 and CYP2C19 genotyping.
2.3 Current Status of Genotyping Methods
Traditionally most genotype assays are conducted in research laboratories and involve the use of polymerase chain reaction (PCR) to amplify the DNA, followed by specific detection steps including restriction fragment length polymorphism-PCR (RFLPPCR) analysis, single-strand conformational polymorphism (SSCP) analysis, or allele-specific PCR analysis.[72]
2.3.1 Development of the AmpliChip™ CYP450
The AmpliChip™ CYP450 Test is based on five major processes: (i) PCR amplification of purified DNA, (ii) fragmenting and labeling of the amplified products, (iii) hybridization of the amplified products to the microarray and staining of the bound products, (iv) scanning of the microarray; and (v) determination of the CYP2D6and CYP2C19 genotypes and predicted phenotype.[73] The two first steps are relatively similar to allele-specific PCR conducted in a research laboratory. The microarray has many specific oligonucleotide probes synthesized on specific areas of the microarray that allow simultaneous multiple allele testing. The alleles are described in table IV. The AmpliChip™ CYP450 Test classifies individuals on two CYP2C19 phenotypes, EMs and PMs, and four CYP2D6 phenotypes: UMs, EMs, IMs, and PMs. For CYP2D6 UMs, the test does not determine the number of multiplied copies.[73]
Alleles tested by AmpliChip™ CYP450 Test[73]
According to the manufacturer’s instructions for the AmpliChip™ CYP450 Test for in vitro diagnostic use (the equivalent of a package insert),[73] the lowest level of genomic DNA input to determine a correct genotype with a positivity rate ≥95% is 25ng for CYP2D6 and 2.5ng for CYP2C19. At first glance, this number seems to be irrelevant for clinicians, but it has major practical implications. In the past, a blood collection was used to complete the CYP2D6 genotype. The AmpliChip™ CYP450 Test’s low DNA concentration detection limit remarkably simplifies the process, using buccal swabs to collect DNA. DNA collection is similar to brushing the cheek with a toothbrush and is more readily accepted by patients than venipuncture. The buccal swab is also easier to mail to genotyping laboratories if needed. This comment is based on the authors’ personal experience with buccal swabs, since Roche Molecular Systems, Inc., recommends genotyping patients with the AmpliChip™ CYP450 using blood.[73]
Using the AmpliChip™ CYP450 Test for in vitro diagnostic use, the overall genotype call rate (correct call and miscalls) for 403 CYP2D6-tested samples was 99.3%.[73]
2.3.2 AmpliChip™ CYP450 versus Traditional Genotyping Methods
In 232 volunteers, five CYP2D6 alleles (*3, *4, *6, *7, and *9) were tested by both allele-specific PCR and a prior version of the CYP450 GeneChip® assay in an independent and blind fashion. The CYP2D6*3, *4, *6, *7, and *9 alleles showed a high degree of concordance between the CYP450 GeneChip® and allele-specific PCR methods (>99% concordance).[36]
Clinicians will easily understand the AmpliChip™ CYP450 Test advantage when they realize that the test simultaneously analyzes one sample for 27 CYP2D6 alleles and three CYP2C19 alleles. If we used our research laboratory to test for the same alleles tested by the AmpliChip™ CYP450 Test with traditional allele-specific PCR methods, that sample would have to be tested 21 times: testing for 19 mutant CYP2D6 alleles and, if absent, assuming the default active (*1) allele; and testing for two CYP2C19 alleles and, if absent, assuming the default active (*1) allele. Testing the sample 21 times in our research laboratory would not even test for the seven CYP2D6 allele duplications. Thus, the AmpliChip™ CYP450 Test allows for multiple simultaneous testing of many alleles, and substantially reduces technician time by automating the process. The CYP2D6 literature has not yet definitively established the absolute minimal number of alleles to test in order to detect most clinically relevant variations in different races, or which other genetic variations may explain UMs that do not have duplications. However, as more advances in this area occur, and more genetic variants need to be tested, it becomes more obvious that new technologies allowing parallel testing of multiple genes (the AmpliChip™ CYP450 Test and other new technologies to be marketed) will have the advantage when compared with laboratories using conventional technologies.
2.3.3 Pharmacogenetic Testing versus Other Laboratory Testing
The best laboratory test to compare with pharmacogenetic testing is a drug blood level, technically called therapeutic drug monitoring (TDM),[74] which could be considered a phenotypic test of metabolic enzymes. Surprisingly, there are almost no studies on TDM cost effectiveness except for some studies on antibacterials.[75] However, TDM appears to be standard clinical practice (medical insurers pay routinely) for classic antiepileptic drugs, theophylline, digoxin, immunosuppressants, and some psychiatric drugs. Although samples for CYP2D6 genotyping may be easier to collect, risperidone TDM may offer additional information on some DDIs. However, DDIs may also contaminate risperidone TDM (table V). When compared in our risperidone study, the genotype-obtained CYP2D6 PM phenotype appeared to be a much more robust and meaningful predictor of ADRs than TDM.[39]
2.3.4 Sensitivity and Specificity of CYP2D6 Genotype and Other Clinical Variables
Obviously, CYP2D6 genotyping needs to be interpreted in the clinical context of all factors influencing drug response. Table VI compares the sensitivity and specificity of CYP2D6 genotyping and other relevant clinical variables in our CYP2D6 PM/risperidone ADR association study.[62] Some of the relevant clinical predictors of ADRs were environmental factors such as DDIs. Other ADR clinical predictors are likely to be independent of CYP2D6 genotyping and can be used complementarily as independent predictors. There were three clinical variables that were associated with risperidone ADRs or risperidone discontinuation due to ADRs. Knowledge of the three variables (taking typical antipsychotics, having any organic brain disorders (such as seizures, strokes, etc.), and taking CYP inhibitors (such as paroxetine or fluoxetine) was obtained by reviewing the chart and/or asking the patient. Unfortunately none of the three variables was significantly associated with both ADRs during risperidone treatment and risperidone discontinuation due to ADRs; they were only significant in one of the two non-overlapping patient groups. Taking CYP inhibitors, for example, was significantly associated with risperidone discontinuation due to ADRs, but it was not significantly associated with risperidone ADRs. It is likely that the latter lack of significance may reflect confounding factors.
Sensitivity, accuracy, specificity and likelihood ratios of predicting risperidone adverse drug reactions (ADRs) in a case-control study:[62] Comparing genotyping for the cytochrome P450 (CYP) 2D6 poor metabolizer (PM) phenotype with other variables
Table VI describes sensitivity (true positive rate, or how good the test is for identifying people with ADRs or who discontinued due to ADRs), specificity (true negative rate, or how good the test is for correctly excluding people without ADRs or who discontinued for other reasons), accuracy (what proportion of all tests have given the correct result), the likelihood ratio of a positive test (the likelihood of a positive test being found in a person with ADRs compared to a person without them, or in a person who discontinued due to ADRs compared to a person who discontinued for other reasons), and the likelihood ratio of a negative test (the likelihood of a negative test being found in a person without ADRs compared to a person with ADRs, or in a person who discontinued for other reasons compared to a person who discontinued due to ADRs).[76] Genotyping for the CYP2D6 PM phenotype was the only variable significant in both samples; it had low sensitivity (≤16%) but very high accuracy (≥94%). Specificity was ≥63% and the likelihood ratio of a positive test was ≥2.5). Thus, the accuracy of genotyping for the CYP2D6 PM phenotype in order to predict ADRs was similar or better than that of the three clinical variables, but the likelihood ratio of a positive test was always better. For comparing performance in predicting ADRs, risperidone TDM is probably a better test than the clinical variables described in table VI. However, TDM samples are harder to collect and analyze than DNA samples, and even when missing risperidone levels were excluded from calculations, genotyping for the CYP2D6 PM phenotype appeared to be a better test than risperidone TDM.[62]
To conclude, a genotyping test should not be a substitute for clinical wisdom or collecting clinical information; in our experience it provides additional information about subjects with unusual response to medications that cannot easily be obtained in other ways, but it has to be interpreted in the clinical context. Basic pharmacological knowledge needs to be used to apply CYP2D6 genotyping in each patient.
2.3.5 Cost of CYP2D6 Genotyping
The AmpliChip™ CYP450 Test was approved in Europe in September 2004 with the Conformité Européene (CE) mark and by the FDA in January 2005, and laboratories are now starting to consider using this new technology. The definitive costs to the patient are not known to us. Two major cost determinants are the equipment and the use of one DNA chip for each DNA sample tested. Laboratories will have to buy the Affymetrix GeneChip® 3000 Dx platform needed to run the test; the approximate retail value is $US200 000 (the actual sale price is unknown to us as it is the result of the discussion between Affymetrix and its customers). Each DNA chip may cost approximately $US400 (the actual sale price is unknown to us as it is the result of the discussion between Roche Molecular Systems, Inc., and its customers). These costs are difficult to compare since no other technology using massively parallel CYP genetic testing has yet been completely developed or approved by the FDA. Other companies are developing CYP testing, probably for research or clinical purposes[77] including General Electric Health Care (CodeLink™ P450 SNP Bioarray); Tm Bioscience (Tag-It™ Mutation Detection Kit), which uses the microsphere-based universal array genotyping platform developed by Luminex;[78] Third Wave Technologies Inc. (Invader® Technology); and Jurilab Ltd (DrugMet™ Genotyping Test). Finally, we know that two US academic laboratories and several commercial pharmacogenetic companies offer physicians the opportunity to genotype their patients for CYP genes (costs for an individual sample range from $US250 to $US500 depending on the number of genes tested). In some cases, the web pages do not explain what equipment is being used for the CYP2D6 genotyping and what alleles are tested. Frequently, CYP2D6 alleles with low activity are not tested.
Currently it is not known whether the AmpliChip™ CYP450 Test and/or any other system in development will become the most widely used systems for completing CYP testing or when these technologies will become less expensive and more readily available worldwide.
3. The Future
Wolf et al.[79] predicted in 2000 that in the future it may be considered unethical not to perform pharmacogenetic testing to avoid exposing individuals to ADRs. But before we reach that promising future, a number of obstacles need to be overcome. This section reviews the obstacles and explores the potential of pharmacogenetic testing in medical practice in the near (next 10 or 15 years) and more distant future.
3.1 Obstacles for the Future Implementation of Pharmacogenetic Testing
We are unaware of articles focused on obstacles in implementing pharmacogenetic testing in the real world. Our opinion expressed here may be somewhat biased by our limited success in advancing pharmacogenetic research during the last 10 years. We describe obstacles in conducting and publishing pharmacogenetic studies that may have been impacted by the different perspectives of grant agencies, pharmaceutical companies, and scientific reviewers. Even if more studies are completed and published, pharmacogenetic clinical applications may be compromised by economic factors and lack of physician education.
3.1.1 Obstacles in Conducting and Publishing Pharmacogenetic Research Studies
Funding Agencies
The US National Institute of Health (NIH) does not seem to see its role as stimulating the translation of pharmacogenomics into the clinical world, but rather envisions this role for the pharmaceutical industry and drug regulatory agencies.[80] A recent editorial comment in Nature[81] stressed the need for good clinical data, stating, “Weakness in clinical data collection is universally acknowledged as a serious hindrance to pharmacogenetics”. Good clinical data collection is expensive and cannot easily be done unless supported by large grants such as those coming from the NIH. Unfortunately, physician-proposed clinical studies have not traditionally fared well in the NIH review process.[82]
Pharmaceutical Companies
Applying Pharmacogenetic Tests to Approved Drugs
There are no positive incentives for pharmaceutical companies to incorporate new CYP knowledge, concerning pharmacogenetics and/or DDIs, on already marketed drugs. Such knowledge would complicate package inserts and may reduce sales. This disincentive can be readily demonstrated by comparing amount of the package insert quality for atypical antipsychotics introduced into the US market in the last 15 years. Those approved in the early 1990s had poor package inserts not reflecting current pharmacokinetic knowledge.[83] The realization of deaths associated with terfenadine treatment in 1996 led to the withdrawal of the drug in 1998[9] and to the FDA request to progressively increase CYP study requirements before any new drugs were approved. Since then the new approved atypical antipsychotics have progressively more informative package inserts. A major problem arises when pharmaceutical companies lose drug patents and drugs become generic; at that time drug companies seem to lose interest in updating package inserts almost completely.
Three psychiatric medications (aripiprazole, duloxetine, and atomoxatine) that include CYP2D6 genotype information in their package inserts were approved in the last 3–4 years. The described effects of the CYP2D6 PM phenotype are very limited; CYP2D6 studies relating the CYP2D6 PM phenotype and ADRs from these drugs, if completed, have never been published in peer-reviewed scientific journals. Unfortunately, it takes several years and much effort from clinicians and researchers to publish independent pharmacokinetic and/or pharmacogenetic studies that are not supported by the pharmaceutical companies.
Developing Future Drugs
Pharmaceutical companies have been slow to implement pharmacogenetics into future drug development, sometimes opting to eliminate drugs metabolized mainly by CYP2D6 as marketing candidates,[84] or taking a ‘wait and see’ stance regarding incorporating pharmacogenetic studies into pre-marketing trials. Completing prospective, randomized, placebo-controlled studies is a very expensive task that requires major economic investments from pharmaceutical companies. No drug has yet been approved with recommendations for pharmacogenetic testing (although the HER2 gene amplification or protein overexpression tests for prescribing trastuzumab may be a form of personalized prescription, but not a ‘pharmacogenetic test’ in the strictest sense). Thus, the first drug approved with pharmacogenetic limitations or recommendations may be a more expensive prescription with great marketing risk, since prescribing physicians may hesitate to prescribe a drug that requires pharmacogenetic testing while another drug from the same family would not. A drug approved with such a requirement may be at a disadvantage for marketing compared with rival drugs that do not require a test. Moreover, pharmaceutical companies may fear that pharmacogenetic testing can only lead to a reduced market share for their drug.[85] Danzon and Towse[86] stressed that issue, recommending public policy decisions at the regulatory agency level, since pharmacogenetic testing may increase development costs and reduce population eligibility, thus decreasing pharmaceutical company interest. It appears that only enforcement by government agencies may be able to expedite the use of pharmacogenetic testing; however, the FDA has only recently (2005) developed guidelines for pharmaceutical companies on collecting and including genetic information for drug applications.[87] According to the FDA, CYP2D6 and thiopurine S-methyltransferase (TPMT) are ‘valid biomarkers.’ When submitting an investigational new drug (IND) application to the FDA, pharmaceutical companies need to send relevant data on valid biomarkers, while other pharmacogenetic data will be submitted voluntarily.
Publication of Real-World Pharmacogenetic Studies in Scientific Journals
Our experience indicates that real-world pharmacogenetic studies, in comparison with laboratory research studies, are difficult to advance through grant agencies and scientific reviewers of journals. Laboratory research is usually considered the gold standard for scientific research, wherein an experiment is designed to test a unique hypothesis by controlling one variable and using significance testing to rule out chance as the explanation for the hypothesis. Pharmacogenetic research, like other biomedical research, can be seen as a scientific discipline following the methods of ‘basic’ biomedical sciences or ‘applied’ science. However, each approach has a substantially different way of thinking, associated with its own cognitive style for interpreting reality.
Basic scientists may be surprised to know that most daily decisions made by physicians are not based on evidence or scientific studies. Most physicians doing clinical work are ‘applied’ scientists with some scientific knowledge, using their interpretation of the complex world to make personal clinical judgments. In a first approximation, the clinical judgments appear to be algorithmic dichotomous decisions with a final outcome of yes or no. However, physicians may frequently use their experience to make balanced (probabilistic) decisions regarding positive and negative aspects (the Bayesian approach, vs the typical approach of drawing statistical inferences using p-values, called the frequentist approach).[88] In pharmacological treatment, the physician’s decision may reflect a balance between risks and benefits to the patient. If the benefit outweighs the risk, the drug is continued; if the risk outweighs the benefit, the drug is discontinued. Physicians do not, however, make all their pharmacological decisions using ‘applied’ scientific concepts. Arbitrary decisions, including personal or group biases, frequently play a role in pharmacological decisions; that is part of the ‘noise’ of the clinical environment.
The differences in approach used by basic and applied scientists are fundamental to understanding why pharmacogenetic studies may have difficulty in being implemented and published. The basic scientist approach is characterized by smaller, well-controlled experiments with only one dependent variable, use of the design to control for confounding variables, and the belief that lack of statistical significance represents failure. The applied scientist approach is characterized by larger studies of many uncontrolled variables, use of statistics to control for confounding variables, and the beliefs that lack of statistical significance is not failure but reflects relative lack of relevance, and effect sizes being more important than statistical significance. The reliance of the basic approach in pharmacogenetic studies on the use of very controlled designs may lead to pharmacogenetic results that cannot be replicated in less-controlled clinical environments. The reliance of the applied scientist approach in pharmacogenetics may lead to lack of significance, due to effect sizes that are too small to be detected in the midst of the ‘noise’ of the clinical environment. The differences in approach between basic and applied scientists are fundamental to understanding the difficulties of taking pharmacogenetics from the laboratory to the real world (an example of ‘translational research’), or to understanding the problems involved in extrapolation from pre-marketing to postmarketing drug studies. The first author has worked over 10 years in pharmacogenetic research of atypical antipsychotics, yet has been unable to predict the variables associated with using high dosages of atypical antipsychotics in the clinical environment (the applied scientist approach) by using the variables that predict high dosing in controlled clinical trials information (the basic scientist approach).
Predicting the variables associated with the clinician’s use of high doses of any drug is a fundamental issue in pharmacogenetic research, since high doses may reflect the presence of rapid metabolism explained by environmental or genetic causes (e.g., CYP2D6 UMs). Based on risperidone placebo-controlled randomized studies, one would easily predict that high risperidone doses produce more ADRs. Thus, one would think that high risperidone doses would be associated with ADRs in a naturalistic study. Surprisingly, in our study high risperidone doses were not associated with ADRs.[62] In hindsight, the lack of significant association between high risperidone doses and ADRs is not so unreasonable. Physicians may correct doses in patients who experience ADRs by avoiding doses that were too high in patients that they have treated previously, or that may appear too high for a specific patient. In summary, the lack of association between high risperidone dosage and ADRs in this naturalistic study[62] may only reflect physician ability to learn how to avoid ADRs. Similarly, based on controlled studies, the first author predicted that two known pharmacokinetic factors (smoking and gender) would be associated with high olanzapine dose in the clinical environment. Neither gender nor smoking was associated with requirement for high olanzapine dose in a large naturalistic study, but individual physician practice and hospital unit type had some influence.[89] These two pharmacological examples of real world prescription of high atypical antipsychotic doses point out extrapolation difficulties from controlled clinical trials to the clinical arena, and from studies based on the basic scientist approach to the clinical environment where applied scientists conduct research.
The two prior examples clearly show that we are far from understanding how to extrapolate from pre-marketing studies to understand how physicians prescribe medications in the real world. Unless the differences between basic and applied pharmacogenetic research are better understood, pharmacogenetic progress will be delayed. Basic CYP2D6 knowledge is relatively well developed, but studies about its real-world applications are missing. It is obvious that one needs a very well-controlled and sufficiently powered study with negative results to rule out the effect of a gene. Uncontrolled, clinical real-world studies with negative results cannot rule out effects because negative results may be caused by confounding factors. A positive, strong pharmacogenetic finding in an uncontrolled study suggests a real effect that may be easily replicable; however, a positive pharmacogenetic finding in an experimental design may not be replicated in the clinical environment or in another experimental design.
3.1.2 Obstacles at the Clinician Level
Financial Obstacles
It is a complicated task in the present climate of increasing health costs to convince a hospital director of the need to purchase new and expensive pharmacogenetic equipment for the hospital laboratory, and to cover the cost of each patient’s test (a few hundred dollars per patient). One needs to study a few thousand patients looking into the cost and savings in the real-world hospital setting. Completing such an expensive study requires surmounting the first and most formidable barrier: finding a funding agency willing to fund such a large naturalistic study. Starting such pharmacogenetic studies in hospitals may be a good first step, but the information must also extend to outpatient physicians and pharmacies so that pharmacogenetic testing may help future prescribing.
The fragmented nature of the US healthcare system complicates cost-effectiveness studies of pharmacogenetic testing. Pharmacogenetic testing may be cost effective if one considers the patient’s long-term outcome; it may predict response to some specific drugs for the patient’s lifetime. However, managed care agencies with short-term (e.g. 5-year) contracts may not find this cost effective. On the other hand, the US healthcare system is open to new biomedical advances and emphasizes quality improvement, possibly making the US more receptive to implementing pharmacogenetics in the clinical environment than other countries. Once patients and families understand the potential of pharmacogenetics to improve patient care and reduce ADR risks, we suspect they will demand its use. However, cost issues will need to be addressed.
Physician-Level Obstacles
The principle behind ‘individualized prescription’ appears simple and appealing, but currently pharmaceutical companies base their marketing and continuing medical education on conducted placebo-controlled studies, and recommend that physicians prescribe ‘average’ doses for the ‘average’ patient. Unfortunately, some patients experience ADRs with average doses. From our experience, these patients and their families favor the idea of ‘individualized prescription’ and feel relief when a genetic condition explains their long-term history of medication problems. However, our experience in providing pharmacogenetic recommendations to physicians is mixed: some embrace the idea of individualized prescription, whereas others resist modifying their longstanding methods of prescribing medications.
The differences between ‘old’ and ‘new’ ways of practicing medicine may have a major impact on implementing pharmacogenetic testing in the clinical environment. Medical practice has radically changed in the last 10–15 years due to rapid advances in biomedical research. Younger physicians may be more up-to-date with recent medical guidelines, providing the best medicine accordingly.[90] In the traditional medical system, experience was most valued, whereas now the ability to assimilate new concepts is fundamental to the rapidly changing medical system. Recently, several authors recommended including pharmacogenetics early in medical school so that physicians in practice 10 years from now may be more receptive to pharmacogenetic advances.[79,91]
3.2 Future Potential of Pharmacogenetic Testing in Medical Practice
3.2.1 Potential of Pharmacogenetic Testing in Medical Practice for the Next 10–15 Years
Will pharmacogenetic testing be widely used in clinical medicine in 2015 as Time predicted,[24] or in 2020 as JAMA predicted?[25] It is unclear. We believe the key to timely incorporation of pharmacogenetics into clinical practice depends on two issues: (i) the ability to integrate basic and applied science knowledge into new pharmacogenetic studies so that the basic knowledge ‘translation’ to the clinical world is smooth and successful; and (ii) the finding of one or more cases in which a drug combination (or a group of drugs) and a pharmacogenetic test become widely used in clinical practice. One or more successful examples of combining a test with a drug may catalyze pharmacogenetics, an area that appears close to exploding. Developing a successful combination of a pharmacogenetic test and drug group or combination is not an easy task in light of the obstacles we described.
Pharmacological obstacles may add to the human obstacles. Proving the clinical relevance of pharmacogenetic testing in drugs with limited ADR liability or wide therapeutic windows may be difficult. On the other hand, a widely prescribed drug with a narrow therapeutic window and sufficient clinically relevant ADRs is probably the best choice to launch pharmacogenetics into the clinical world.
Potential for CYP2D6 Genotyping in Medical Practice for the Next 10–15 Years
CYP2D6 genotyping certainly is a prime candidate for the first successful pharmacogenetic testing in the clinical environment. Basic and applied knowledge is sufficiently integrated and advanced to the point that the FDA defines CYP2D6 genotyping as one of two “valid biomarkers” in pharmacogenetics,[26] an FDA-approved test is available, and other microarray devices are being developed.
By chance, many CYP2D6-dependent drugs are psychiatric drugs; thus, pharmacogenetics may move faster in psychiatry than in other areas of medicine, but it is difficult to predict which drug will become the first to include pharmacogenetic testing as standard practice. Our experience with risperidone, and the fact that generic forms will soon reach the market, lead us to believe that generic risperidone with CYP2D6 genotyping for best dose selection may be a very reasonable first-choice antipsychotic and a way to introduce pharmacogenetic testing in psychiatry. New risperidone studies are needed to prove that CYP2D6 genotyping may help dose selection. Other relatively new psychiatric drugs, such as venlafaxine, aripiprazole, duloxetine, and atomoxetine, may also benefit from CYP2D6 genotyping, but almost no published knowledge supports CYP2D6 genotyping use; thus studies are needed.
Kirchheiner et al.[38] developed a dosing guideline focused on the use of some typical antipsychotics and TCAs according to the four CYP2D6 phenotypes. In the US typical antipsychotics are no longer frequently used. Likewise, TCAs are rarely used and will never again become first choice antidepressants in the US. One reason is that pharmaceutical marketing encourages the use of new antidepressants as first-line antidepressants. Even pharmacogenetic testing cannot prevent TCAs’ narrow therapeutic range and lethal overdose potential, which is a major concern in patients with depression, who have higher suicide risk. Although fluoxetine and paroxetine are extensively metabolized by CYP2D6, they are poor candidates for CYP2D6 genotyping, as they are also CYP2D6 inhibitors. After multiple doses, one-half to two-thirds of CYP2D6 EMs became CYP2D6 PMs in phenotypical tests with these drugs.[92] Thus, large fluoxetine and paroxetine studies are needed to prove statistical differences between CYP2D6 PMs and EMs (which include many EMs who appear to behave as PMs). CYP2D6 auto-inhibition may make CY2PD6 polymorphism effects hard to detect in the already ‘noisy’ clinical environment.
A new guideline for psychiatrists interested in using CYP2D6 and CYP2C19 in the clinical world has recently been developed.[39] This new guideline tries to expand and simplify for clinicians the guidelines by Kirchheiner et al.[49] The potential of CYP2D6 in other medical subspecialties is smaller than in psychiatry. Codeine-like drugs may also be highly dependent on CYP2D6 for their action.[93] Thus, although there is a lack of published studies in the literature, pain clinics using TCAs and codeine-like drugs may be a good environment for studying the potential of CYP2D6 genotyping.
Potential for Other Gene Genotyping in Medical Practice for the Next 10–15 Years
CYP2C19 has less potential than CYP2D6 as a pharmacogenetic test candidate, since fewer drugs appear dependent on CYP2C19. The ethnic/racial differences in CYP2C19 genotype frequencies may increase the potential of CYP2C19 in East Asian countries. The current potential for a genotype test for another CYP gene, CYP2C9, is focused on warfarin, acenocoumarol, and phenytoin. To make CYP2C9 genotyping successful as a pharmacogenetic test, cost-effectiveness studies are needed in patients taking warfarin, the most important CYP2C9-metabolized drug.[94,95] Other potential drugs include some antihyperglycemic agents and anti-inflammatory drugs.[94]
TPMT is another ‘valid biomarker’ according to the FDA, but the clinical uses of TPMT genotyping are limited by the scarcity of drugs this metabolized by this enzyme. Azathioprine and mercaptopurine are inactive prodrugs that require activation by TPMT. Although the number of individuals with low TMTP activity is low (<5% in Caucasians), leading hospitals treating children with childhood leukemia routinely phenotype by measuring the patient’s TMTP activity before starting treatment with mercaptopurine. This is not a genetic test, but a phenotypic test measuring red blood cell enzyme activity.[96] A genetic test to detect the UGT1A1*28 allele as a marker of irinotecan-induced toxicity in colorectal cancer patients (the recently FDA-approved Invader® UGT1A1 Molecular Assay[59]) has already been described.
3.2.2 Role of Pharmacogenetic Testing in the More Distant Future (Beyond 10–15 Years)
Based on current genetic technology developments, one can use microarrays to test several functional genetic variations of a single well known gene (e.g. CYP2D6 and AmpliChip™ CYP450 Test) or to test multiple single nucleotide polymorphisms (SNPs) from multiple genes[81,97] that help identify a complex pattern predicting drug response. Pharmacodynamic gene variations such as those occurring on the serotonin transporter or the dopamine receptor genes have been studied in psychiatry,[38] but the use of these gene variations as pharmacogenetic markers may be many years away from incorporation into clinical practice.
The progression of pharmacogenetic testing of single genes from bench to bedside has been described,[98] but the development of tests for multiple SNPs seems much more complex. Basic scientists use microarrays to study hundreds or thousands of genes in one of a few biological samples.[17] Similarly, one can test for thousands of SNPs of known genes (some of these SNPs may be functional and others may not be) by including them in one microarray to explore ADR associations in a pharmacogenetic study. Then, complex statistical analyses (which are not well validated or established) can be used to determine SNP patterns associated with drug response in a group of patients. Knowing the multiple factors affecting drug response in the clinical environment, it is unlikely that this type of pharmacogenetic result will be easily replicated in different clinical settings. Difficulties are based on ‘noise’ associated with (i) testing hundreds of SNPs with unknown meaning and using complex (and not well validated) statistical analyses; and (ii) those resulting from variability in the clinical environment.
Kirchheiner et al.[38] stress that pharmacogenetic s will only be used as a diagnostic tool in clinical practice if precise and specific treatment options and guidelines based on genetic tests can be provided. It is difficult to do that with well-known polymorphic variations of one well-known gene (e.g. CYP2D6) and appears a nearly insurmountable task if one attempts to use microarray data including hundreds or thousands of SNPs from hundreds or thousands of genes. It is unknown if translating a complex statistical pattern from a microarray with thousands of SNPs to a clear recommendation for clinicians is even possible.
4. Conclusions
The AmpliChip™ CYP450 Test for CYP2D6 and CYP2C9 genotypes is the first pharmacogenetic clinical tool based on microarray technology that has been introduced into clinical practice. The introduction of this new technology is a major step in ushering ‘personalized prescription’ into the clinical environment. Because of the large number of CYP2D6 drugs in psychiatry, pharmacogenetics may move faster in psychiatry than in other areas of medicine, but it is difficult to predict which drug will become the first to be prescribed in conjunction with pharmacogenetic testing as standard practice.
Proving that pharmacogenetics works in the real world requires completing large pharmacogenetic studies in real-world conditions. Reviewers from grant agencies and scientific journals stress the need for well controlled experimental designs, which are difficult in the naturalistic clinical setting. Pharmaceutical companies have yet to fully embrace the pharmacogenetic approach. Even if more studies are completed and published, pharmacogenetic clinical applications may be compromised by economic factors and lack of physician education.
The next 5–10 years will identify new genes and polymorphisms that may be relevant to pharmacogenetic response. Prior pharmacology history and current experience with pharmacogenetics have led us to predict that finding genetic variations that help minimize ADRs may be easier than finding the genetic variations predicting the best drug response. In summary, pharmacogenetics may be more helpful in recommending the appropriate dosage or determining which specific drugs a patient should not take, than it may be in recommending the best drug for a particular patient. Based on current genetic technology developments, microarrays could test multiple SNPs from multiple genes that help identify a complex pattern predicting drug response. However, considering how difficult it is to take a well understood polymorphic gene such as CYP2D6 to the clinical environment, it is unlikely that an approach using multiple SNPs of multiple genes may reach the market in the near future.
References
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients. JAMA 1998; 279: 1200–5
Bordet R, Gautier S, Le Louet H, et al. Analysis of the direct cost of adverse drug reactions in hospitalized patients. Eur J Clin Pharmacol 2001; 56: 935–41
Lacoste-Roussillon C, Pouyanne P, Haramburu F, et al. Incidence of serious adverse drug reactions in general practice: a prospective study. Clin Pharmacol Ther 2001;69: 458–62
Lundkvist J, Jonsson B. Pharmacoeconomics of adverse drug reactions. Fundam Clin Pharmacol 2004; 18: 275–80
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet 2000; 356: 1255–9
Pirmohamed M, Breckenridge AM, Kitteringham NR, et al. Adverse drug reactions. BMJ 1998; 316: 1295–8
Classen DC, Pestotnik SL, Evans RS, et al. Adverse drug events in hospitalized patients. JAMA 1997; 277: 301–6
Institute of Medicine: To err is human: building a safer health system. Washington, DC: National Academic Press, 2000
Lasser KE, Allen PD, Woolhandler SJ, et al. Timing of new black box warnings and withdrawals for prescription medications. JAMA 2002 May 1; 287(17): 2215–20
Johnson JA, Bootman JL. Drug-related morbidity and mortality: a cost-of-illness model. Arch Intern Med 1995; 155: 1949–56
Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc 2001; 41: 192–9
Chou WH, Yan FX, de Leon J, et al. An extension of a pilot study: impact from the cytochrome P450-2D6 (CYP2D6) polymorphism on outcome and costs in severe mental illness. J Clin Psychopharmacol 2000; 20: 246–51
Collins FS, Green ED, Guttmacher AE, et al. A vision for the future of genomics research. Nature 2003; 422: 835–7
Gibbs N. The secret of life. Time 2003 Feb 17; 161(7): 42–5
McKusick VA. The anatomy of the humane genome: a neo-vesalian basis for medicine in the 21st century. JAMA 2001; 286: 2289–95
Fodor SP. Massively parallel genomics. Science 1997; 277: 393–5
Chaudhuri JD. Gene arrays out of you: the amazing world of microarrays. Med Sci Monit 2005; 11: RA52–62
Emery J, Hayflick S. The challenge of integrating genetic medicine into primary care. BMJ 2001; 322: 1027–30
Hammer W, Sjoqvist F. Plasma levels of monomethylated tricyclic antidepressants during treatment with imipramine-like compounds. Life Sci 1967; 6: 1895–903
Phillips KA, Veenstra DL, Oren E, et al. Potential role of pharmacogenomics in reducing adverse drug reactions: a systematic review. JAMA 2001; 286: 2270–9
Vogel F. Moderne probleme der Humangenetik. Ergeb Inn Med Kinderheilkd 1959; 12: 52–125
Pirmohamed M. Pharmacogenetics and pharmacogenomics. J Clin Pharmacol 2001; 52: 345–7
Editor: new research horizons. Science 1997; 278: 2039
Lertola J. Deciphering the code and what might come from it. Time 1999 Nov 8; 68-9
Collins FS, McKusick VA. Implications of the human genome project for medical science. JAMA 2001; 285: 540–4
Pirazzoli A, Recchia G. Pharmacogenetics and pharmacogenomics: are they still promising? Pharmacol Res 2004; 49: 357–61
Nebert DW, Jorge-Nebert L, Vesell ES. Pharmacogenomics and “individualized drug therapy”: high expectations and disappointing achievements. Am J Pharmacogenomics 2003; 3: 361–70
Ingelman-Sundberg M. Human drug metabolising cytochrome P450 enzymes: properties and polymorphisms. Naunyan Schmiedbergs Arch Pharmacol 2004; 369: 89–104
Ingelman-Sundberg M. Genetic polymorphisms of cytochrome P450 2D6 (CYP2D6): clinical consequences, evolutionary aspects and functionary diversity. Pharmacogenomics J 2005; 5: 6–13
Mahgoub A, Idle JR, Dring LG, et al. Polymorphic hydroxylation of debrisoquine in man. Lancet 1977; II(8038): 584–6
Eichelbaum M, Spannbrucker N, Dengler HJ. Influence on the defective metabolism of sparteine on its pharmacokinetics. Eur J Clin Pharmacol 1979; 16: 189–94
Skoda RC, Gonzalez FJ, Demierre A, et al. Two mutant alleles of the human cytochrome P-450db1 gene (P450C2D1) associated with genetically deficient metabolism of debrisoquine and other drugs. Proc Natl Acad Sci U S A 1988; 85: 5240–3
Heim M, Meyer UA. Genotyping of poor metabolisers of debrisoquine by allele-specific PCR amplification. Lancet 1990; 336: 529–32
Bertilsson L, Dahl ML, Sjoqvist F, et al. Molecular basis for rational megaprescribing in ultrarapid hydroxylators of debrisoquine. Lancet 1993; 341: 63
Johansson I, Oscarson M, Yue QY, et al. Genetic analysis of the Chinese cytochrome P4502D locus: characterization of variant CYP2D6 genes present in subjects with diminished capacity for debrisoquine hydroxylation. Mol Pharmacol 1994; 271: 1250–7
Chou WH, Yan FX, Robbins-Weilert DK, et al. Comparison of two CYP2D6 genotyping methods and assessments of genotype-phenotype relationships. Clin Chem 2003; 49: 542–51
Lovlie R, Daly AK, Matre GE, et al. Polymorphisms in CYP2D6 duplicationnegative individuals with the ultrarapid metabolizer phenotype: a role for the CYP2D6*35 allele in ultrarapid metabolism? Pharmacogenetics 2001; 11: 45–55
Kirchheiner J, Nickchen K, Bauer M, et al. Pharmacogenetics of antidepressants and antipsychotics: the contribution of allelic variations to the phenotype of drug response. Mol Psychiatry 2004; 9: 442–73
deLeon J, Armstrong SC, Cozza KL. Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychoso-matics 2006; 47: 75–85
Arthur H, Dahl ML, Siwers B, et al. Polymorphic drug metabolism in schizophrenic patients with tardive dyskinesia. J Clin Psychopharmacol 1995; 15: 211–6
Armstrong M, Daly AK, Blennerhassett R, et al. Antipsychotic drug-induced movement disorders in schizophrenics in relation to CYP2D6 genotype. Br J Psychiatry 1997; 170: 23–6
Pollock BG, Mulsant BH, Sweet RA, et al. Prospective cytochrome P450 phenotyping for neuroleptic treatment in dementia. Psychopharmacol Bull 1995; 31: 327–32
Bork J, Rogers T, Wedlund P, et al. A pilot study of risperidone metabolism: the role of cytochrome P450 2D6 and 3A. J Clin Psychiatry 1999; 60: 469–76
Bertilsson L, Aberg-Wistedt A, Gustafsson LL, et al. Extremely rapid hydroxylation of debrisoquine: a case report with implication for treatment with nortriptyline and other tricyclic antidepressants. Ther Drug Monit 1985; 7: 478–80
Chen S, Chou W, Blouin R, et al. Clinical and practical aspects to screening for the cytochrome P450-2D6 (CYP2D6) enzyme polymorphism. Clin Pharmacol Ther 1996; 60: 522–34
Krau RP, Diaz P, McEachran A. Managing rapid metabolizers of antidepressants. Depress Anxiety 1996–1997; 4: 320–7
Spina E, Gitto C, Avenoso A, et al. Relationship between plasma desipramine levels, CYP2D6 phenotype and clinical response to desipramine: a prospective study. Eur J Clin Pharmacol 1997; 51: 395–8
Meyer JW, Woggon B, Küpfer A. Importance of oxidative polymorphism on clinical efficacy and side-effects of imipramine: a retrospective study. Pharmacopsychiatry 1988; 21: 365–6
Kirchheiner J, Brøsen K, Dahl ML, et al. CYP2D6 and CYP2C19 genotyped-based recommendations for antidepressants: a first step towards subpopulation-specific dosages. Acta Psychiatr Scand 2001; 104: 173–92
Kirchheiner J, Bertilsson L, Brass H, et al. Individualized medicine: implementation of pharmacogenetic diagnostics antidepressant drag treatment of major depressive disorders. Pharmacopsychiatry 2003; 36(3 Suppl.): S235–43
deLeon J, Barnhill J, Rogers T, et al. A pilot study of the cytochrome P450-2D6 genotype in a psychiatric state hospital. Am J Psychiatry 1998; 155: 1278–80
Huang M, VanPeer A, Woestenborghs R, et al. Pharmacokinetics of the novel antipsychotic agent risperidone and the prolactin response in healthy subjects. Clin Pharmacol Ther 1993; 54: 257–68
deLeon J, Bork JA. Risperidone and the cytochrome P450 3A [letter]. J Clin Psychiatry 1997; 58: 450
Fang J, Bourin M, Baker GB. Metabolism of risperidone to 9-hydroxyrisperidone by human cytochromes P450 2D6 and 3A4. Naunyn Schmiedebergs Arch Pharmacol 1999; 359: 147–51
Cappell K, Arndt M, Carey J. Drags get smart. Business Week 2005 Sep 5; 76-85
Emens LA. Trastuzumab: targeted therapy for the management of HER-2/neuoverexpressing metastatic breast cancer. Am J Ther 2005; 12: 243–53
Adams GP, Weiner LM. Monoclonal antibody therapy of cancer. Nat Biotechnol 2005; 23: 1147–57
Iyer L. Inherited variations in drug-metabolizing enzymes: significance in clinical oncology. Mol Diagn 1999; 4: 327–33
US Food and Drug Administration. FDA clears genetic test that advances personalized medicine: test helps determine safety of drug therapy [online]. Available from URL: http://www.fda.gov/bbs/topics/NEWS/2005/NEW01220.html [Accessed 2005 Oct 17]
MacArthur RD. An updated guide to genotype interpretation. AIDS Read 2004; 14: 256–8, 261-4, 266
Sturmer M, Doerr HW, Preiser W. Variety of interpretation systems for human immunodeficiency virus type 1 genotyping: confirmatory information or additional confusion? Curr Drug Targets Infect Disord 2003; 3: 373–82
deLeon J, Susce MT, Pan RM. The CYP2D6 poor metabolizer phenotype may be associated with risperidone adverse drug reactions and discontinuation. J Clin Psychiatry 2005; 66: 15–27
Barnhill J, Susce MT, Diaz FJ, et al. Risperidone half-life in a patient taking paroxetine: a case report [letter]. Pharmacopsychiatry 2005; 38(5): 223–5
Wang JS, Ruan Y, Taylor RM, et al. The brain entry of risperidone and 9-hydroxyrisperidone is greatly limited by p-glycoprotein. Int J Neurop-sychopharmacol 2004; 7: 415–9
Tyndale RF, Droll KP, Sellers EM. Genetically deficient CYP2D6 metabolism provides protection against oral opiate dependence. Pharmacogenetics 1997; 7: 375–9
deLeon J, Dinsomore L, Wedlund PJ. Adverse drug reactions to oxycodone and hydrocodone in CYP2D6 ultrarapid metabolizers [letter]. J Clin Psychopharmacol 2003; 23: 420–1
Wuttke H, Rau T, Heide R, et al. Increased frequency of cytochrome P450 2D6 poor metabolizers among patients with metoprolol-associated adverse effects. Clin Pharmacol Ther 2002; 72: 429–37
Jin Y, Desta Z, Stearns V, et al. CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 2005; 97: 30–9
Wedlund PJ. The CYP2C19 enzyme polymorphism. Pharmacology 2000; 6: 174–85
Furuta T, Ohashi K, Kamata T, et al. Effect of genetic differences in omeprazole metabolism on cure rates for Helicobacter pylori infection and peptic ulcer. Ann Intern Med 1998; 129: 1027–30
Steimer W, Zoph K, Von Amelunxen S, et al. Amitriptyline or not, that is the question: pharmacogenetic testing of CYP2D6 and CYP2C19 identifies patients with low or high risk for side effects in amitriptyline therapy. Clin Chem 2005; 51: 376–85
Daly AK. Development of analytical technology in pharmacogenetic research. Naunyn Schmiedebergs Arch Pharmacol 2004; 369: 133–40
Roche Molecular Systems Inc. AmpliChip CYP450 Test for in vitro diagnostic use [equivalent to the package insert]. Branchburg (NJ): Roche Molecular Systems Inc., 2005
Ensom MH, Chang TK, Patel P. Pharmacogenetics: the therapeutic drug monitoring of the future? Clin Pharmacokinet 2001; 40: 783–802
Touw DJ, Neef C, Thomson AH, et al. Cost-effectiveness of therapeutic drug monitoring: a systematic review. Ther Drug Monit 2005; 27: 10–7
Greenhalgh T. How to read a paper: papers that report diagnostic or screening test. BMJ 1997; 315: 540–3
Blue Cross and Blue Shield Association. Special report: genotyping for cyto-chrome P450 polymorphisms to determine drug-metabolizer status [online]. Technical Assessment Program 2004 Dec; 19 (9). Available from URL: http://www.bcbs.com/tec/voll9/19._09.pdf [Accessed 2005 Sep 13]
Bortolin S, Black M, Modi H, et al. Analytical validation of the Tag-It high throughput microsphere-based universals array genotyping platform: application to the multiplex detection of a panel of thrombophilia-associated single-nucleotide polymorphisms. Clin Chem 2004; 50: 2028–36
Wolf CR, Smith G, Smith RL. Science, medicine, and the future: pharmacogenetics. BMJ 2000; 320: 987–90
Weinshilboum R, Wang L. Pharmacogenomics: bench to bedside. Nat Rev 2004; 3: 739–48
Pharmacogenomics to come [editorial]. Nature 2003; 425: 749
Inouye SK, Fiellin D. An evidence-based guide to writing grant proposals for clinical research. Ann Intern Med 2005; 142: 274–82
deLeon J, Armstrong SC, Cozza KL. Med-psych drug-drug interaction update: the dosing of atypical antipsychotics. Psychosomatics 2005; 46: 262–73
Sadee W. Pharmacogenomics: the implementation phase. AAPS PharmSci 2002; 4(2): E5.
Kerwin RW. A perspective on progress in pharmacogenomics. Am J Pharmacogenomics 2003; 3: 371–3
Danzon P, Towse A. The economics of gene therapy and of pharmacogenetics. Value Health 2002; 5: 5–13
US Department of Health and Human Services, Food and Drug Administration. Drug-diagnostic co-development: concept paper [online]. Available from URL: http://www.fda.gov/cder/genomics/pharmacoconceptfn.pdf [Accessed 2005 Jun 10]
Gill CJ, Sabin L, Schmid CH. Why clinicians are natural Bayesians. BMJ 2005; 330: 1080–3
Botts S, Littrell R, de Leon J. Variables associated with high olanzapine dosing in a state hospital. J Clin Psychiatry 2004; 65: 1138–43
Choudry NT, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med 2005; 142: 260–73
Gurtwitz D, Weizman A, Rehavi M. Education: teaching pharmacogenomics to prepare future physicians and researchers for personalized medicine. Trends Pharmacol Sci 2003; 24: 122–5
Alfaro CL, Lam YW, Simpson J, et al. CYP2D6 status of extensive metabolizers after multiple-dose fluoxetine, fluvoxamine, paroxetine, or sertraline. J Clin Psychopharmacol 1999; 19: 155–63
Susce MT, Murray-Carmichael E, de Leon J. Response to hydrocodone, codeine and oxycodone in a CYP2D6 poor metabolizer. Prog NeuroPsychopharmacol Biol Psychiatry 2006 Apr 20; [Epub ahead of print].
Kirchheiner J, Brockmoller J. Clinical consequences of cytochrome P450 2C9 polymorphisms. Clin Pharmacol Ther 2005; 77: 1–16
Veenstra DL, Higashi MK. Assessing the cost-effectiveness of pharmacogenomics. AAPS Pharmsci 2000; 2: 1–11
Corominas H, Baiget M. Clinical utility of thiopurine S-methyltransferase genotyping. Am J Pharmacogenomics 2004; 4: 1–8
Ruano G. Quo vadis personalized medicine. Personalized Med 2004; 1: 1–7
Wedlund PJ, deLeon J. Pharmacogenetic testing: the cost factor. Pharmacogenomics J 2001; 1: 171–4
Acknowledgments
The genotyping studies of psychiatric patients included in this article were conducted at the University of Kentucky Mental Health Research Center at Eastern State Hospital, Lexington, Kentucky, USA.
Jose de Leon, M.D., has received support for his laboratory and research-initiated grants and honoraria from Roche-Molecular Systems, Inc., but has not received any consultant payments and has no other financial arrangements with Roche Molecular Systems, Inc. He has no stocks from Roche or Affymetrix. Dr de Leon has also served on an advisory board for Bristol-Myers Squibb, and has received researcher-initiated grants and honoraria from Eli Lilly. Many of the ideas presented in this article are the distillation of years of discussion and collaboration of Jose de Leon with Dr Walter Koch. The authors thank Lorraine Maw, Tita Forrest and Michele Nikoloff for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Leon, J., Susce, M.T. & Murray-Carmichael, E. The AmpliChip™ CYP450 Genotyping Test. Mol Diag Ther 10, 135–151 (2006). https://doi.org/10.1007/BF03256453
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256453