Abstract
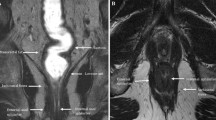
PURPOSE: We evaluated the usefulness of magnetic resonance imaging for the preoperative diagnosis of deep anorectal abscesses. METHODS: Subjects were 21 patients with deep anorectal abscesses. Deep anorectal abscesses were classified into two types, ischiorectal and pelvirectal, according to their location. Patients were also classified into a single abscess group, which showed either an ischiorectal or pelvirectal abscess, and a double abscess group, which showed both ischiorectal and pelvirectal abscesses. The final diagnosis was made from surgical findings, and the types of deep anorectal abscesses determined by digital examination and magnetic resonance imaging were compared. RESULTS: Sensitivity of ischiorectal abscesses (20 lesions) with digital examination and magnetic resonance imaging was 75 and 95 percent, respectively, and that of pelvirectal abscesses (10 lesions) with digital examination and magnetic resonance imaging was 60 and 70 percent, respectively. Sensitivity of the magnetic resonance imaging was significantly higher than that of digital examination in ischiorectal abscesses. Diagnostic accuracy of digital examination and magnetic resonance imaging were both 83 percent in the single abscess group (12 patients), whereas in the double abscess group (9 patients) it was 22 and 78 percent, respectively. The rate of accurate diagnosis of magnetic resonance imaging compared with digital examination in the double abscess group was significantly higher than that in the single abscess group. CONCLUSION: Magnetic resonance imaging was useful for diagnosing and differentiating ischiorectal and pelvirectal abscesses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.References
Ono C, Inoue T, Iai T, Ichikawa T, Hida Y. A case of Fournier's syndrome caused by a perianal abscess. J Jpn Surg Assoc 1996;57:2041–4.
Saigusa J, Saigusa S, Yoshida M. A case of Fournier syndrome after radical operation of anal fistula. J Jpn Soc Coloproctol 1989;42:1254–7.
Ralls PW, Henley DS, Colletti PM,et al. Amebic liver abscess: MR imaging. Radiology 1987;165:801–4.
Haimes AB, Zimmerman RD, Morgello S,et al. MR imaging of brain abscesses. AJNR Am J Neuroradiol 1989;10:279–91.
Goligher JC. Surgery of the anus, rectum and colon. 4th ed. London: Bailliere Tindall, 1980.
Takano M, Fujiyoshi T, Hidaka H,et al. One-staged radical sphincter function preserving operation for abscesses. J Jpn Soc Coloproctol 1987;40:777–85.
Guillaumin E, Jeffrey RB, Shea WJ,et al. Perirectal inflammatory disease: CT findings. Radiology 1986;161:153–7.
Yousem DM, Fishman EK, Jones B. Crohn disease: perirectal and perianal findings at CT. Radiology 1988;167:331–4.
Tuji Y, Fujiyoshi T, Takagi K,et al. Study on the pathogenesis of ischiorectal abscess and fistula viewed from the standpoint of transanal ultrasonic examination. J Jpn Soc Coloproctol 1991;44:146–52.
Takano M, Fujiyoshi K, Takagi K,et al. Comparison of the correct diagnosis of anal fistulas between digital and ultrasonic examination. J Jpn Soc Coloproctol 1992;45:1033–8.
Orsoni P, Barthet M, Portier F,et al. Prospective comparison of endosonography, magnetic resonance imaging and surgical findings in anorectal fistula and abscess complicating Crohn's disease. Br J Surg 1999;86:360–4.
deSouza NM, Puni R, Kmiot WA, Bartram CI, Hall AS, Bydder GM. MRI of the anal sphincter. J Comput Assist Tomogr 1995;19:745–51.
deSouza NM, Hall AS, Puni R, Gilderdale DJ, Young IR, Kmiot WA. High resolution magnetic resonance imaging of the anal sphincter using a dedicated endoanal coil: comparison of magnetic resonance imaging with surgical findings. Dis Colon Rectum 1996;39:926–34.
Lunniss PJ, Armstrong P, Barker PG, Reznek RH, Phillips RK. Magnetic resonance imaging of anal fistulae. Lancet 1992;340:394–6.
Barker PG, Lunniss PJ, Armstrong P, Reznek RH, Cottam K, Phillips RK. Magnetic resonance imaging of fistulain-ano: technique, interpretation and accuracy. Radiology 1994;49:7–13.
Scholefield JH, Berry DP, Armitage NC, Wastie ML. Magnetic resonance imaging in the management of fistula in ano. Int J Colorectal Dis 1997;12:276–9.
Author information
Authors and Affiliations
About this article
Cite this article
Maruyama, R., Noguchi, T., Takano, M. et al. Usefulness of magnetic resonance imaging for diagnosing deep anorectal abscesses. Dis Colon Rectum 43 (Suppl 10), S2–S5 (2000). https://doi.org/10.1007/BF02237218
Issue Date:
DOI: https://doi.org/10.1007/BF02237218