Abstract
Renal inflammation is the initial, healthy response to renal injury. However, prolonged inflammation promotes the fibrosis process, which leads to chronic pathology and eventually end-stage kidney disease. There are two major sources of inflammatory cells: first, bone marrow-derived leukocytes that include neutrophils, macrophages, fibrocytes and mast cells, and second, locally activated kidney cells such as mesangial cells, podocytes, tubular epithelial cells, endothelial cells and fibroblasts. These activated cells produce many profibrotic cytokines and growth factors that cause accumulation and activation of myofibroblasts, and enhance the production of the extracellular matrix. In particular, activated macrophages are key mediators that drive acute inflammation into chronic kidney disease. They produce large amounts of profibrotic factors and modify the microenvironment via a paracrine effect, and they also transdifferentiate to myofibroblasts directly, although the origin of myofibroblasts in the fibrosing kidney remains controversial. Collectively, understanding inflammatory cell functions and mechanisms during renal fibrosis is paramount to improving diagnosis and treatment of chronic kidney disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Renal fibrosis is the consequence of a diverse range of kidney diseases and is characterized by excessive accumulation of fibroblasts and extracellular matrix (ECM) (Djudjaj and Boor 2018; Humphreys 2018; Liu 2006; Zeisberg and Neilson 2010). It is also the common pathological pathway leading to end-stage renal disease (ESRD) (Eddy and Neilson 2006; Meng et al. 2013). However, the mechanisms of renal fibrosis remain largely unclear. Indeed, current treatments are non-specific and ineffective. Thus, it is essential to better understand the inflammatory process from acute injury to chronic kidney disease (CKD).
Renal inflammation serves as the initial response to kidney stress or injury, and it protects the kidney from further damage (Meng et al. 2014). However, unresolved inflammation destroys kidney structure and function, leading to CKD that is characterized by progressive renal fibrosis (Grande et al. 2010; Lee and Kalluri 2010). Several key steps are involved in this process: first, the renal injury itself, followed by recruitment of inflammatory cells and release of profibrotic mediators that trigger accumulation and activation of myofibroblasts, then production and deposition of extracellular matrix (ECM), followed finally by glomerulosclerosis and tubular atrophy that is accompanied by microvascular rarefaction (Lee and Kalluri 2010; Liu 2011).
Regardless of the initial trigger, renal inflammation is characterized by glomerular and tubulointerstitial infiltration of inflammatory cells like neutrophils, T cells, macrophages, fibrocytes and mast cells (Meng et al. 2014). Activated intrinsic kidney cells, such as mesangial cells (MCs), podocytes, tubular epithelial cells (TECs) and endothelial cells, function as inflammatory mediators that produce proinflammatory cytokines, chemokines and growth factors and also participate in the repair process (Boor et al. 2010). After prolonged inflammation, histological and functional dysfunction occurs from excessive fibroblast and myofibroblast accumulation and ECM production. In fact, accumulation of myofibroblasts is the predominant source for collagen production and the dominant event in renal fibrosis progression. However, the origin of myofibroblasts remains largely controversial. Some research shows epithelial–mesenchymal transition (EMT) and endothelial–mesenchymal transition (EndoMT) are sources of myofibroblasts (Allison 2013; LeBleu et al. 2013; Liu 2011). But, resident fibroblasts also contribute to renal fibrosis (Duffield and Humphreys 2011; Lin et al. 2008; Strutz and Zeisberg 2006). In addition, accumulating evidence suggests pericytes are a major source of myofibroblasts (Humphreys et al. 2010; Lin et al. 2008). And, bone marrow-derived cells like fibrocytes and macrophages also contribute to the local accumulation of myofibroblasts (Broekema et al. 2007; Meng et al. 2016b; Wang et al. 2016b, 2017b). Thus, understanding the origin of myofibroblasts may help to clarify the pathway from renal inflammation to fibrosis. The current chapter focuses on key inflammatory cell types and pathways linking renal inflammation with fibrosis.
2 Bone Marrow-Derived Inflammatory Cells in Renal Fibrosis
When renal injury occurs, circulating leukocytes are recruited to the kidney (Chung and Lan 2011). Lymphocytes, monocytes, macrophages, mast cells and fibrocytes produce tissue damage factors like reactive oxygen species, cytokines and growth factors (Boor et al. 2010; Grande et al. 2010; Lee and Kalluri 2010). These profibrotic mediators cause myofibroblast accumulation and ECM production. Collectively, unresolved inflammation drives the profibrotic pathways that lead to fibrosis (Kanasaki et al. 2013; Lee and Kalluri 2010).
2.1 Macrophages in Renal Inflammation and Fibrosis
In the injured kidney, monocytes transdifferentiate into macrophages in response to oxidative stress, toxins and hypoxia. This represents a critical component of the mononuclear phagocyte system (Anders and Ryu 2011; Vernon et al. 2010). Macrophages are divided into two subtypes, classically activated (M1) and alternatively activated (M2). Macrophages adopt the M1 phenotype when stimulated by interferon-γ (IFN-γ) and lipopolysaccharide (LPS). M2 phenotype is induced by interleukin (IL)-4 or IL-13. M2 macrophages are further categorized into three subsets according to their response to stimuli. M2a, wound healing macrophages, are induced by IL-4 and IL-13; M2b are induced by immune complexes; M2c, regulatory macrophages, are induced by IL-10, TGF-β or glucocorticoid. During the progression from kidney injury to repair processes, inflammatory M1 macrophages switch toward M2 phenotype and exert distinct functions supporting the pathological process (Anders and Ryu 2011). Accordingly, the proinflammatory M1 macrophages generate TNF-α, IL-1β and reactive oxygen species in response to renal injury. By contrast, the M2 macrophages secrete anti-inflammatory cytokines like IL-10 and insulin-like growth factor-1 that promote tissue healing and angiogenesis (Ricardo et al. 2008).
Macrophages are key inflammatory cells in proliferative glomerulonephritis (GN), particularly in crescentic GN (Han et al. 2011; Ma et al. 2009a, 2010). Macrophages are recruited from either circulation or local environment, which correlates with the severity of glomerular and tubulointerstitial damage, and renal function impairment, and is prognostic of disease progression (Eardley et al. 2008; Lan et al. 1995; Yang et al. 1998a). The findings that show co-localization of α-SMA + myofibroblasts and proliferative macrophages in areas of severe renal damage indicate a correlation between macrophages and renal fibrosis (Yang et al. 1998b). This is underscored by results from biopsies of patients with CKD and fibrotic kidney of animal models showing a similar relationship between macrophage recruitment and disease severity (Eardley et al. 2008; Nishida and Hamaoka 2008).
Inflammatory macrophages are a major source of proinflammatory cytokines, such as TNF-α and IL-1β, and chemokines like MCP-1(Ma et al. 2010). They also secrete macrophage migration inhibitory factor (MIF), a critical inflammatory mediator that promotes the progression of kidney diseases (Lan et al. 1997). Moreover, macrophages produce a number of growth factors like TGF-β and PDGF that play key roles linking renal inflammation with fibrosis.
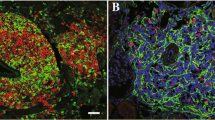
To date, the profibrotic role of macrophages has been studied exclusively by various depletion techniques. They showed macrophage deficiency attenuated renal fibrosis in various disease models, including ischemic acute kidney injury (Ko et al. 2008), crescentic glomerulonephritis (Han et al. 2013), membranoproliferative glomerulonephritis (Guo et al. 2011), obstructive nephropathy (Kitamoto et al. 2009) and diabetic nephropathy(Lin et al. 2009; You et al. 2013). In contrast, reconstitution of macrophages significantly aggravates existing fibrotic lesions. Much research has focused on the regulatory mechanisms of macrophages during the profibrotic effect. For example, a recent study revealed that genetic ablation of galectin-3, a β-galactosidase-binding lectin, protected against renal fibrosis in a unilateral ureteral obstruction (UUO) model without affecting the number of infiltrated macrophages. And, adoptive transfer of macrophages from wild-type mice, instead of galectin-3 KO mice, restored renal fibrosis (Henderson et al. 2008). Another study demonstrated that CpG-oligodeoxynucleotides-induced activation of TLR9 on macrophages accelerated interstitial fibrogenesis (Anders et al. 2004). This indicates the toll-like receptor-mediated signals on macrophages play critical roles in the progression of renal fibrosis. In addition, pharmacological inhibition of c-fms, the monocyte/macrophage receptor for CSF1, reduced the number of renal macrophages and tubular apoptosis, but had marginal impact on renal fibrosis (Han et al. 2013; Ma et al. 2009b). A recent study showed that macrophage-specific cyclooxygenase (Cox)-2 polarized and maintained a macrophage tissue-reparative M2 phenotype that protected against diabetic nephropathy (Wang et al. 2017a). This evidence shows that macrophages are a key bridge linking renal inflammation and renal fibrosis through several mechanisms. First, M1 macrophages secrete chemokines, cytokines and matrix metalloproteinases (MMPs) to accelerate the excessive infiltration of leukocytes into the injured region, destroying the original architecture of the kidney and aggravating renal injury (Ricardo et al. 2008). Second, cytokines and growth factors released by macrophages facilitate the proliferation and activation of resident fibroblasts. Macrophages promote transdifferentiation of other cells into myofibroblast-like cells through paracrine signaling. Macrophages are a major source of TGF-β1 in pathological conditions, and increased release enhances the number of infiltrated myofibroblasts by triggering the transdifferentiation of epithelial cells, endothelial cells and activation of pericytes and resident fibroblasts. M2 macrophages release IGF-1 and PDGF that promote myofibroblast survival (Floege et al. 2008; Wynes et al. 2004). Macrophage-derived PDGF also targets local fibroblasts and pericytes where the receptors for PDGF are highly expressed (Lin et al. 2008). And, macrophage-secreted MMP-9 induces EMT. Third, macrophages support extracellular matrix framework containing fibrinogen and collagens (Gratchev et al. 2001; Schnoor et al. 2008). Fourth, inflammatory macrophages induce vascular injury and capillary rarefaction, leading to tissue hypoxia and progression of renal fibrosis (Fine and Norman 2008). Finally, macrophages directly transdifferentiate into myofibroblast-like cells. Indeed, cells co-expressing the markers for both macrophage (CD68 +) and myofibroblast (α-SMA+) have been detected in patients with progressive renal fibrosis and animal models of obstructive nephropathy and chronic renal allograft injury (Wang et al. 2016b, 2017b). Furthermore, myeloid macrophages labeled with red fluorescence using lineage-tracing techniques show that bone marrow-derived macrophages, particularly M2, directly transdifferentiate into the collagen-producing myofibroblast in obstructive renal fibrosis model. This indicates macrophages contribute to renal fibrosis through direct mechanisms (Meng et al. 2016b). TGF-β/Smad3 signaling is a master regulator in this process (Wang et al. 2016b).
Several lines of evidence indicate that targeting the phenotypic alteration of macrophages has therapeutic potential in treating renal fibrosis. A recent study showed that transferring M2 macrophages significantly attenuated renal inflammation and fibrosis (Wang et al. 2007). Although M2a and M2c are both capable of attenuating renal injury by decreasing host macrophage and T cell infiltration, M2c is more effective at inducing Tregs and attenuating renal inflammation and fibrosis (Cao et al. 2013; Lu et al. 2013). Collectively, macrophages play a central role in linking renal inflammation and fibrosis (shown in Fig. 18.1). Inhibiting macrophage infiltration, modifying phenotype of macrophages by interfering with specific signaling molecules or transferring modified macrophages may represent a potential approach to treat renal fibrosis.
Role of macrophages in linking renal inflammation and fibrosis. Monocyte/macrophages are recruited by chemokines released in response to microenvironment of injured kidney, and then they are activated by proinflammatory cytokines. These classically activated M1 macrophages activate intrinsic renal cells including tubular epithelial cells, endothelial cells and mesangial cells via producing factors such as cytokines (IL-1, TNF) and ROS. In the progression of renal disease, alternative activated M2 macrophages are induced by Th2 cytokines, and macrophages also gain M2 phenotype after engulfing apoptotic cells. These profibrotic macrophages promote renal fibrosis by producing an abundance of growth factors and ECM, and they may also undergo transition into myofibroblasts via TGF-β/Smad3-mediated MMT. In the fibrotic stage, the activated intrinsic renal cells proliferate, activate or directly transdifferentiate into myofibroblast-like cells directly via different mechanisms, and thereby participate in renal fibrosis. Abbreviations: ECM—extracellular matrix; EMT—epithelial–mesenchymal transition; EndoMT—endothelial–mesenchymal transition; MMT—macrophage–myofibroblast transition; FGF-2—fibroblast growth factor 2; IGF-1—insulin-like growth factor-1; PDGF—platelet-derived growth factor; ROS—reactive oxygen species; TGF-β—transforming growth factor β; and TNF—tumor necrosis factor
2.2 T Cells in Renal Fibrosis
T cells are found in kidneys of patients and experimental animals with chronic kidney disease (Harris and Neilson 2006; Robertson et al. 2004). In early stages of renal inflammation, T lymphocytes migrate to the injured region and are activated by antigen stimulation. Activated T cells produce a variety of cytokines and chemokines that recruit and activate macrophages, facilitating the inflammatory response (Lin et al. 2008). The functional role of T cells has been studied extensively in different renal disease models (Tipping and Holdsworth 2006; Zheng et al. 2005). For example, deletion of CD4+ T cells with a monoclonal antibody largely attenuated renal fibrosis. And, adoptive transfer of CD4+ T cells, but not CD8+ T cells, restored the severity of UUO-induced renal fibrosis without affecting the number of infiltrating macrophages (Tapmeier et al. 2010). This indicates CD4+ T cells directly contribute to renal fibrosis in a macrophage-independent manner. Additionally, T cells were shown to indirectly regulate fibrocyte differentiation (Niedermeier et al. 2009). In a study using chronic renal allograft, intratubular T cells triggered local epithelial cells to transition into proliferating fibroblast phenotype (Robertson et al. 2004). Among T cell subsets, Th2 cells play a more critical role in renal fibrosis. Reconstitution of Th2 cells in mice with CD4+ T cell deletion resulted in more severe renal fibrosis compared with adoptive transfer of Th1 cells (Liu et al. 2012). This indicates that targeting CD4+ T cells, particularly Th2 cells, may be a potential therapy for renal fibrosis. In another study, CD4+ Foxp3+ T cells mediated the repair of AKI and attenuated renal fibrosis via mTOR signaling (Chen et al. 2016). The function of Th17 cells and IL-17 in renal fibrosis is still under debate. IL-17 is mainly produced by Th17 and γδT cells (Kim et al. 2015). The Th17/IL-17 axis is profibrotic, and it induces the production of chemokine (C-X-C motif) ligand 5 (CXCL5) and recruits neutrophils that contribute to glomerular nephropathy (Disteldorf et al. 2015). Disruption of IL-17A reduces myofibroblast activation and extracellular matrix production in UUO nephropathy (Peng et al. 2015). Moreover, exposure to elevated dietary salt promotes the progression from AKI to CKD through activation of Th17 cells (Mehrotra et al. 2015). This is consistent with the finding that disruption of IL-17 or IL-23 (a cytokine essential for the expansion and survival of Th17 cells) reduces albuminuria and glomerular crescent formation in experimental glomerulonephritis (Paust et al. 2009). In contrast, in a deoxycorticosterone acetate and angiotensin II-induced model of hypertensive nephropathy, loss of IL-17 accelerated hypertensive glomerular injury, which is correlated with reduced survival of TECs and more infiltration of γδT cells. Consistently, increased IL-17 suppressed renal inflammation and fibrosis in diabetic nephropathy by protecting against TECs and podocytes (Mohamed et al. 2016). All of these findings underscore Th17/IL-17 acts in a disease type- and dosage-dependent way. It is important to note that CD11c+ CD8+ T cells likely induce fibroblast apoptosis, thereby limiting renal fibrosis (Wang et al. 2016a). This is in agreement with a previous study that showed loss of CD8+ T cells increased CD4+ T cell-mediated monocyte-to-fibroblast transition and renal fibrosis (Dong et al. 2016).
2.3 Fibrocytes in Renal Fibrosis
Fibrocytes are bone marrow-derived circulating cells that originate from CD14+ monocytic lineage and share markers with leukocytes like CD45 and mesenchymal cells like type I collagen (Bucala et al. 1994; Chesney et al. 1998). In the injured kidney, fibrocytes are recruited via their highly expressed chemokine receptors CCR2, CCR7 and CXCR4 (Chen et al. 2011a; Reich et al. 2013; Sakai et al. 2006). The regulation of fibrocyte differentiation has been studied extensively. It is clear that profibrotic Th2 cytokines, like IL-4 and IL-13, induce the differentiation of fibrocytes into myofibroblasts in vitro. However, Th1 cytokines like IFN-γ exert inhibitory effects on this process (Shao et al. 2008). Further, inhibiting CCL21/CCR7 signaling with anti-CCL21 antibodies or genetic deletion inhibits fibrocyte recruitment and renal fibrosis (Wada et al. 2007). CCR2 is also a key mediator for migration of fibrocytes to the injured kidney (Reich et al. 2013). As monocyte-derived precursor cells, fibrocytes not only participate in renal inflammation but also contribute to renal fibrosis through several mechanisms. First, they produce a large amount of collagen and profibrotic growth factors such as TGF-β in response to stimuli (Buchtler et al., 2018). Second, they secrete a number of cytokines, such as TNF-α and MCP-1, that contribute to renal inflammation (Chesney et al. 1998; Reilkoff et al. 2011). Third, they directly convert into myofibroblast phenotype. Although this remains controversial, some studies report that a considerable ratio of collagen-producing fibroblasts in obstructive kidney diseases originates from fibrocytes or bone marrow (Broekema et al. 2007; Niedermeier et al. 2009).
2.4 Mast Cells in Renal Fibrosis
Mast cells are tissue-specific multifunctional cells found in low numbers in healthy kidneys, but are significantly increased in tubulointerstitial injury, regardless of the initiating disease (Holdsworth and Summers 2008). As granulated cells, mast cells produce an array of inflammatory cytokines, chemokines, growth factors and cell-specific neutral proteases that facilitate leukocyte recruitment and microbial destruction. Interestingly, infiltration of mast cells is positively correlated with disease severity (Kondo et al. 2001). However, the functional role of mast cells in fibrosis is still not clear (Mack and Rosenkranz 2009). It is possible that mast cells promote fibrosis by releasing profibrotic mediators, such as TGF-β and MMP, or by activating the AngII pathway through chymase-dependent mechanisms (Margulis et al. 2009; Wasse et al. 2012). Direct evidence of a role for mast cells in renal inflammation and fibrosis comes from a number of studies using mast cell-deficient mice. In one study, deletion of a key differentiation factor c-kit in KitW−sh/W−sh mice inhibited renal CD4+ T cells, macrophages and renal fibrosis. These were restored by adoptive transfer of bone marrow-derived mast cells from wild-type mice (Summers et al. 2012). In another, depletion of mast cells in the early phase of renal ischemia–reperfusion injury prevented CKD progression (Danelli et al. 2017). Consistent results were also found by deleting mouse mast cell protease 4 (mMCP4), the functional counterpart of human chymase, in mouse models of experimental anti-glomerular basement glomerulonephritis and UUO nephropathy. Results showed that mMCP4-deficient mice had significantly less renal inflammation and fibrosis; they were protected from progressive renal injury (Pons et al. 2017; Scandiuzzi et al. 2010). In contrast, results from other studies do not support the pathogenic role of mast cells in renal inflammation and fibrosis. For example, deletion of mMCP4 in UUO nephropathy increased kidney-infiltrating macrophages, T cells and local profibrotic TGF-β1 and CCL2 (Miyazawa et al. 2004). Similarly, in mast cell-deficient (Ws/Ws) rats, renal fibrosis in puromycin aminonucleoside nephrosis was measurably worse (Beghdadi et al. 2013; Miyazawa et al. 2004). This finding is further evidenced by a well-designed study that showed deficiency of mast cells in Kit(W)/Kit(W-v) mice enhanced renal fibrosis by increasing the infiltration of inflammatory cells (T cells and macrophages) and TGF-β production in obstructive kidney. The study also showed adoptive transfer of mast cells effectively suppressed renal fibrogenesis (Kim et al. 2009). Although the role of mast cells in renal inflammation and fibrosis remains unclear, there is no doubt that mast cells contribute to the pathological process from renal inflammation to fibrosis. The convincing and conflicting results from different animal models warrant further investigation.
3 Intrinsic Kidney Cells in Renal Inflammation and Fibrosis
Intrinsic kidney cells include tubular epithelial cells, podocytes, mesangial cells and endothelial cells. They actively participate in the disease process from inflammation to fibrosis after kidney injury. When activated, they produce a number of inflammatory cytokines, chemokines and growth factors, leading to progression of kidney diseases from acute inflammation to chronic fibrosing stage, resulting in ESRD (Gewin et al. 2017). In this regard, intrinsic kidney cells also function as inflammatory cells, like infiltrating leukocytes, and play critical roles in mediating fibrosis in CKD.
3.1 Tubular Epithelial Cells in Renal Inflammation and Fibrosis
Tubular epithelial cells (TECs) are the primary target of a variety of metabolic, immunologic, ischemic and toxic insults. TECs exhibit a wide range of responses including growth arrest, proliferation, apoptosis, autophagy and transdifferentiation that lead to tubular atrophy and renal fibrosis (Gewin 2018; Liu 2011). Several lines of evidence indicate TECs are not only common targets, but also major initiators of renal injury as producers of cytokines and chemokines (Hato et al. 2013; Liu et al. 2018; Nielsen et al. 2013). For instance, in a kidney transplantation model, activated TECs attracted all subsets of leukocytes and promoted their migration into the graft at early inflammatory stage of allograft rejection by releasing TEC-generated chemokines CCL2, CCL5, macrophage chemotactic osteopontin (OPN) and macrophage migration inhibitory factor (MIF) (Demmers et al. 2013; Nguan and Du 2009). Indeed, TEC itself is capable of producing abundant cytokines, including TNF-α, IL-1β, IL-15 and IL-6 to enhance local inflammation (Nguan and Du 2009). This proinflammatory property of TECs is highlighted by a study showing that deficiency of renal collecting duct epithelial cell-specific Klf5 largely attenuated renal inflammation by decreasing chemokine secretion (Fujiu et al. 2011). In addition, constitutive activation of TGF-β receptor type 1 (TβR1) kinase in tubular epithelial cells was sufficient to induce AKI, characterized by tubular cell apoptosis and necrosis, oxidative stress, interstitial accumulation of inflammatory cells and loss of renal function (Gentle et al. 2013). Consistently, blocking TGF-β signaling in tubular epithelial cells has significant impacts on renal inflammation, apoptosis and fibrogenesis in animal models of toxic nephropathy (Gewin et al. 2012) and obstructive nephropathy (Gewin et al. 2010; Meng et al. 2012a, b). Overactivation of TGF-β/Smad signaling in TEC promotes renal fibrosis in vivo and in vitro. In response to TGF-β1, TECs release a number of profibrotic factors like TGF-β1, which stimulate TECs to produce collagen extracellular matrix (Meng et al. 2010). Direct evidence comes from a number of studies that showed activated TEC transitions from epithelial into mesenchymal phenotype, the EMT process, which is mainly found in vitro in response to TGF-β, IL-1β and angiotensin II (AngII), in a number of animal models (Fan et al. 1999, 2001; Liu 2004, 2010; Yang et al. 2002). However, the EMT concept has been challenged by cell lineage-tracing studies showing myofibroblasts originate from TECs; it is rare to find EMT cells in renal biopsy samples from patients with chronic kidney disease (Allison 2013; LeBleu et al. 2013). It is worth noting that TECs undergo partial EMT, instead of completely transdifferentiating to myofibroblasts, and this is sufficient to drive renal interstitial fibrosis (Grande et al. 2015; Lovisa et al. 2015).
During inflammatory responses, several signaling pathways, including β-catenin (He et al. 2009), ILK (Li et al. 2003), Notch1 (Bielesz et al. 2010; Sharma et al. 2011; Ueno et al. 2013) and hypoxia-inducible factor 1 (HIF1) (Higgins et al. 2007), are activated in TECs and contribute to the progression of renal fibrosis. TEC-specific toll-like receptors, like TLR4, are key mediators in renal inflammation (Cheng et al. 2013; Correa-Costa et al. 2011; Lin et al. 2012; Zhang et al. 2008) and promote renal fibrosis (Campbell et al. 2011; Lin and Tang 2013). TLR4 suppressed BAMBI, the membrane-bound competitive inhibitor of the TGF-β type 1 receptor, increased the susceptibility of renal cells to TGF-β signaling and enhanced renal fibrogenesis (Pulskens et al. 2010). TLR4-mediated signaling promotes inflammatory cytokine IL-18-induced α-SMA and collagen production, and also decreases E-cadherin levels through AP-1 activation (Meldrum et al. 2012). Interestingly, the inflammatory phase of TECs also affects the repair process after AKI. It is now clear that the c-reactive protein (CRP) pathway is induced in TECs and plays an active role in promoting renal inflammation and fibrosis in diabetic kidney injury (Liu et al. 2011). Activation of the CRP pathway in TECs also delays the recovery from acute ischemic renal injury by impairing the G1/S cell cycle (Liu et al. 2011). Moreover, a previous study highlighted a link between TECs and renal fibrosis by demonstrating that G2/M-arrested proximal tubular cells activated c-jun NH(2)-terminal kinase (JNK) signaling, thereby inducing profibrotic cytokine production (Yang et al. 2010).
3.2 Mesangial Cells in Renal Inflammation and Fibrosis
Glomerulosclerosis pathogenesis is correlated with activation and proliferation of MCs, abnormalities of podocytes and endothelial cell dysfunction (Abboud 2012; Schnaper et al. 2003). As the key cell type for glomerulosclerosis, MCs are the primary target of immune-mediated glomerular diseases like IgA nephropathy or metabolic diseases like diabetic nephropathy (Gomez-Guerrero et al. 2005). When challenged by stimuli, MCs produce inflammatory mediators, including chemokines (e.g., CCL2), cytokines (e.g., TNF-α and IL-6) and various oxygen species (Schlondorff and Banas 2009). Results of transcriptomic and proteomic profiling reveal that multiple inflammatory pathways, such as LXR/RXR, FXR/RXR, and acute-phase response signaling were activated in MCs from IgA nephropathy (Liu et al. 2017). Evidence from a recent study showed that parathyroid hormone-related protein (PTHrP) served as a critical modulator of inflammatory cytokine production in MCs (Hochane et al. 2018). Proinflammatory mediators released by MCs damage the endothelial barrier, exposing the mesangium to macromolecules that trigger a positive feedback loop of inflammatory cascades (Schlondorff and Banas 2009). Leukocyte migration and infiltration into the glomerulus cause initiation and amplification of glomerular injury and are mediated by adhesion molecules and chemokines, which can be locally synthesized by MCs (Lu et al. 2018). Thus, MCs function to amplify inflammatory processes in the inflamed glomerulus. Growing evidence shows that MC-derived cytokines induce podocyte injury, resulting in proteinuria (Lai et al. 2008, 2009). It is also worth noting that inflammatory mediators released by MCs promote activation and proliferation of MC themselves via an autocrine mechanism. Furthermore, activated MCs produce growth factors, including TGF-β, PDGF, FGF, HGF, EGF and CTGF (Crean et al. 2004; Floege et al. 1998, 2008; Laping et al. 2000; Schnaper et al. 2003). These induce MC proliferation, α-SMA + phenotype transformation and ECM production, leading to glomerulosclerosis (Taniguchi et al. 2013). The findings that ECM accumulation often appears to begin in the mesangium of glomerulosclerosis suggest a critical role for mesangial cells in glomerulosclerosis (Schnaper et al. 2003).
3.3 Podocytes in Renal Inflammation and Fibrosis
Podocytes are terminally differentiated epithelial cells with limited proliferative capacity. They play an important role in renal inflammation and fibrosis, especially in glomerular diseases (Fogo 2011; Grahammer et al. 2013). Functionally, one study showed podocyte-specific ablation of NEMO, an NF-κB essential modulator, decreased secretion of proinflammatory chemokines and increased remission of proteinuria, restoring podocyte morphology in a mouse model of nephrotoxic nephritis (Brahler et al. 2012). Consistently, conditional knockout of signal transducer and activator of transcription 3 (STAT3) from podocytes attenuated inflammatory response and development of crescentic glomerulonephritis (Dai et al. 2013). Further, a recent study showed that podocyte-specific chemokine receptor (CCR) 2 overexpression enhanced inflammatory response in diabetic nephropathy (You et al. 2017).
Podocytes also play pivotal roles in the development of glomerulosclerosis and tubulointerstitial fibrosis, which lead to progressive proteinuric kidney disease (Deelman and Sharma 2009; Shih et al. 1999). A previous study demonstrated that deficiency of Akt2 in podocytes exacerbated glomerulosclerosis and albuminuria (Canaud et al. 2013). In another, increased caspase-8-mediated apoptosis in podocytes significantly increased kidney damage, foot process effacement, mesangial expansion and glomerulosclerosis (Rutkowski et al. 2013). In addition, conditional knockout of yes-associated protein (YAP) from podocytes accelerated FSGS and progressive renal failure (Schwartzman et al. 2016).
Podocyte-related mechanisms in glomerular diseases, especially diabetic nephropathy (DN), are a hot topic. In diabetic models, Notch signaling plays a critical role in podocyte injury; overexpression of the intracellular domain of Notch (ICN) in podocytes induces proteinuria and glomerulosclerosis. This demonstrates a prominent role in podocyte dysfunction as a key step in glomerulosclerosis and renal fibrosis (Niranjan et al. 2008). Evidence also shows that vitamin D/vitamin D receptor (VDR) signaling in podocytes protects against podocyte loss and glomerular fibrosis in diabetic kidneys (Wang et al. 2012). The role of podocyte-specific mTOR is also important, as it is highly expressed in human DN samples. Indeed, increased activation of mTORC1 enhances proteinuria and progressive glomerulosclerosis in DN, but genetic reduction of mTORC1 decreases symptoms (Inoki et al. 2011). Interestingly, another study demonstrated that knockout of mTOR accelerated glomerular damage. However, inhibiting mTORC1 signaling by genetically reducing mTORC1 copy number prevented glomerulosclerosis and progression of glomerular disease in DN. This highlights the importance of a critical balance in mTOR activity as a regulator of the pathology of diabetic kidney diseases (Fogo 2011; Godel et al. 2011).
Podocyte-secreted growth factors also induce renal fibrosis by building new microenvironments in glomeruli. Vascular endothelial growth factor (VEGF) regulates endothelial functions, including endothelial cell migration, differentiation and survival. Podocytes are a major source of VEGF in the kidney (Mathieson 2009). Selective knockdown of VEGF in podocytes caused endothelial and mesangial cell dysfunction and progressive glomerulosclerosis (Eremina et al. 2006; Siddiqi and Advani 2013). In contrast, overexpression of VEGF in a mouse model of diabetes led to advanced diabetic glomerulopathy, characterized by proteinuria, glomerulomegaly, glomerular basement membrane thickening and excessive mesangial expansion (Veron et al. 2010, 2011). This is consistent with previous findings that showed doxycycline-induced overexpression of soluble VEGF receptor-1 (sFlt-1) in podocytes ameliorated glomerulopathy in diabetic mice (Ku et al. 2008). In addition, podocyte-specific PDGF overexpression induced mesangial cell proliferation and led to mesangioproliferative disease, glomerulosclerosis and crescentic glomerulonephritis (van Roeyen et al. 2011). CTGF, a matricellular protein, is also a critical pathogenic factor in podocytes. One study showed CTGF overexpression induced expansion of the mesangial matrix and exacerbated albuminuria in a mouse model of DN (Yokoi et al. 2008).
Renin–angiotensin system (RAS) is an important target in renal fibrosis (Mezzano et al. 2001). Several studies have shown that RAS components are highly expressed in podocytes (Durvasula and Shankland 2006, 2008), indicating a potential role in podocyte-mediated renal fibrosis. Moreover, podocyte-specific deletion of the mammalian homologue of yeast vacuolar protein sorting defective 34 (mVps34), a critical regulator in autophagy, led to glomerulosclerosis and interstitial fibrosis accompanied by podocyte vacuolization and proteinaceous casts (Chen et al. 2013).
A final note, EMT is found in podocytes in animal models (Li et al. 2008; Sam et al. 2006) and human biopsy samples of diabetic nephropathy, IgA nephropathy and lupus nephritis (Yamaguchi et al. 2009). Clearly, podocytes participate in disease states and regulate pathology when environmental conditions are primed.
3.4 Endothelial Cells in Renal Inflammation and Fibrosis
Endothelial cells play critical roles in the pathophysiological processes of regional blood flow regulation and leukocyte recruitment (Pober and Sessa 2007). When the kidney is injured, the interaction between endothelial cells and leukocytes is initiated. Recruited leukocytes roll along the activated endothelium that is mediated by selectins, E-selectin and P-selectin, and leukocyte surface antigens. Leukocyte adhesion is facilitated by endothelial expression of ICAM-1, VCAM-1 and PECAM; leukocytes transmigrate to injured tissue and exert proinflammatory functions (Guerrot et al. 2012). Evidence of this comes from a study that showed blocking P-selectin increased renal blood flow and promoted recovery of renal function in an ischemic model of renal failure (Bojakowski et al. 2001). Consistently, another study showed deficiency of CD147, a ligand for E-selectin, impaired neutrophil recruitment and attenuated kidney damage (Kato et al. 2009). Similarly, inhibition of ICAM-1 with monoclonal antibody or genetic knockdown techniques also protected against renal injury (Kelly et al. 1994, 1996). Taken together, these findings underscore the importance of endothelial activation in local inflammation at an early stage.
Endothelial activation and subsequent leukocyte adhesion create hemodynamic resistance that reduces regional blood flow (Guerrot et al. 2012). In such conditions, ischemia and oxidative stress trigger endothelial apoptosis that leads to rarefaction of peritubular capillaries (Kelly et al. 2009; Venkatachalam et al. 2010). A pathogenic role for endothelial dysfunction was described in a study that found Crim1 deficiency, a protein involved in endothelial maintenance and integrity, resulted in excessive deposition of collagen, dysfunction and permeability of peritubular capillaries, and eventually renal fibrosis (Wilkinson et al. 2009). Importantly, rarefaction of peritubular capillaries induces hypoxia, which has significant impacts on progression of renal fibrosis by triggering EMT and/or promoting matrix production from myofibroblasts (Higgins et al. 2007). Compelling evidence for the pathogenic role of hypoxia in renal fibrosis was provided by studies showing that degradation or inhibition of hypoxia-induced factor1α (HIF1α), a central regulator of cellular responses to hypoxia (Higgins et al. 2008), largely reduced renal fibrosis (Higgins et al. 2007; Kimura et al. 2008). The correlation between HIF1α and tubulointerstitial fibrosis was also confirmed in biopsy samples from patients (Higgins et al. 2007). Chronic hypoxia is accompanied by increased oxidative stress and generation of ROS, which trigger advanced glycation end products, advanced oxidative protein products and advanced lipoperoxidation end products (D’Agati and Schmidt 2010; Negre-Salvayre et al. 2008). These may target kidney cells as pathogenic mediators and enhance renal inflammation and fibrosis (Daroux et al. 2010; Shanmugam et al. 2008; Shi et al. 2008; Zhou et al. 2009).
Finally, inflammatory endothelial cells also contribute to renal fibrosis through transdifferentiation into collagen-producing cells via EndoMT in response to stimuli (Zeisberg et al. 2008). Of note, TGF-β1 is the key mediator inducing EndoMT via Smad3-dependent mechanisms (Li et al. 2010; Xavier et al. 2015). A recent study showed EndoMT is regulated by SIRT (sirtuin)3/Foxo3a axis and integrin β1/dipeptidyl peptidase (DPP)-4 in vivo (Lin et al. 2018). Moreover, loss of heparin-binding EGF-like factor (HB-EGF) in endothelial cells attenuates angiotensin II (Ang II)-induced renal inflammation and fibrosis (Zeng et al. 2016). This emphasizes the critical role endothelial cells play in linking inflammation and fibrosis.
4 Key Fibrosis-Correlated Growth Factors Released by Inflammatory Cells
Resident and recruited inflammatory cells secrete growth factors such as TGF-β, PDGF, FGF, HGF, EGF and CTGF that exert pro- or anti-fibrotic roles in renal fibrosis (Boor and Floege 2011; Lv et al. 2018). TGF-β1 is the most abundant isoform of TGF-β family members and is secreted by all types of resident renal cells and infiltrated inflammatory cells. It is secreted as a latent precursor, called latent TGF-β1 that binds to latent TGF-β-binding protein (LTBP). When exposed to stimuli, including ROS, plasmin and acid (Meng et al. 2015, 2016a), TGF-β1 is released from latency-associated peptide (LAP) and LTBP (Lyons et al. 1990; Meng et al. 2013; Munger et al. 1999). Mature TGF-β1 then binds to its type II receptor to recruit type I receptors and activates downstream signals. The major source of TGF-β1 includes macrophages, tubular epithelial cells and myofibroblasts (Fukuda et al. 2001; Lee and Kalluri 2010; Ma et al. 2003). After release and activation, TGF-β1 activates Smad and non-Smad signaling in renal fibrosis, inflammation, cell growth, apoptosis and differentiation (Bottinger and Bitzer 2002). In general, TGF-β1 has both pro- and anti-inflammation properties (Huang et al. 2008a, b; Kitamura and Suto 1997; Zhang et al. 2009). In renal fibrosis, TGF-β and downstream Smad3 are pathogenic, while Smad2 and Smad7 seem to be renoprotective (Meng et al. 2013).
TGF-β1 behaves in renal disease in a cell-specific and dosage-dependent manner (Hathaway et al. 2015; Meng et al. 2016a). TGF-β1 recruits macrophages by secreting chemokines, including MCP-1 and OPN (Lan 2011; Zhang et al. 2009), and promotes macrophage polarization toward M2 phenotype (Sica and Mantovani 2012). Our recent results also show TGF-β1 initiates transdifferentiation of macrophages into myofibroblast-like cells (Wang et al. 2016b). In addition, TGF-β1 induces the production of Foxp3+ T regulatory cells (Tregs) (Fu et al. 2004) and inhibits the progression of autoimmune kidney disease (Wang et al. 2006). A recent study showed that combination treatment of rhTGF-β and ICG-001, an inhibitor of β-catenin/TCF, suppressed both renal inflammation and fibrosis in UUO nephropathy and kidney ischemia/reperfusion (Qiao et al. 2018). Several other studies confirm TGF-β1 plays regulatory roles in other types of T cells (Gorelik and Flavell 2002; Kitching and Holdsworth 2011; Turner et al. 2010). In addition, TGF-β mediates mast cell chemotaxis (Gruber et al. 1994) and production of mast cell protease (Funaba et al. 2006).
TGF-β1 also functions in resident inflammatory cells by enhancing ECM production from TECs and promoting EMT. TGF-β1 also induces apoptosis in tubular epithelial cells (Lopez-Hernandez and Lopez-Novoa 2012). In vitro, data indicate that podocytes produce ECM in response to TGF-β1 (Gruden et al. 2005). In TGF-β1 transgenic mice, apoptosis of podocytes is induced by overactivation of Smad7 (Schiffer et al. 2001). Further, a previous study indicated that TGF-β-induced apoptosis in cultured mouse podocytes acted through upregulation of mitochondrial Nox4 via Smad2/3-dependent mechanisms (Das et al. 2014). As terminally differentiated epithelial cells, podocytes also undergo EMT in response to TGF-β1 (Li et al. 2008). Furthermore, emerging evidence indicates that TGF-β1 stimulates mesangial cells to secrete type I, III and IV collagen, laminin and fibronectin, supporting glomerular ECM accumulation (Gruden et al. 2005; Lopez-Hernandez and Lopez-Novoa 2012). TGF-β1 also induces hypertrophy and proliferation of mesangial cells to accelerate glomerulosclerosis (Gruden et al. 2005). Additionally, TGF-β1 has an impact on apoptosis, proliferation and migration of endothelial cells (Lebrin et al. 2005). Although TGF-β1 has a proapoptotic effect on endothelial cells in most scenarios (Loeffler and Wolf 2013), it also promotes the release of VEGF from podocytes and TECs which protect endothelial cells from apoptosis (Kang et al. 2002). Notably, as a downstream molecule of TGF-β1, Smad2 triggers expression of antiangiogenic factors like TSP-1 and VEGF-A antagonist. In comparison, TGF-β1-induced VEGF mRNA and protein expression are Smad3-dependent (Nakagawa et al. 2004a, b). TGF-β1 is known classically to stimulate EndoMT (Zeisberg et al. 2008). Thus, data clearly show TGF-β1 could be secreted by inflammatory cells and may be one of the key growth factors that drives renal fibrogenesis.
The PDGF family contains four isoforms, PDGF-A, -B, -C and -D, and two receptor chains, PDGFR-α and -β, that are constitutively or inducibly expressed in most renal cells (Floege et al. 2008). PDGF exerts numerous biological functions in renal diseases, including production of pro- and anti-inflammatory mediators, ECM accumulation, cell proliferation and migration (Ostendorf et al. 2012). PDGF signaling is a crucial mediator in renal fibrosis (LeBleu and Kalluri 2011), as evidenced by the findings that show blocking PDGF-D attenuates tubulointerstitial fibrosis in both early and late stages of glomerulonephritis (Boor et al. 2007; Ostendorf et al. 2006). PDGF-D has a direct profibrotic effect on the tubular interstitium by promoting EMT (Kong et al. 2009) or by triggering expression of PDGFR-β from resident fibroblasts or pericytes, which are the major source of interstitial myofibroblasts (Humphreys et al. 2010; Lin et al. 2008). Inhibition of PDGFR signaling reduces the number of myofibroblasts and ameliorates renal damage in obstructive nephropathy (Chen et al. 2011b). This indicates a key role for PDGFR signaling in myofibroblast generation from pericytes. Compelling evidence for a role of PDGFRα and its ligand PDGF-CC in renal fibrosis is provided by results showing that inhibition of PDGF-CC suppresses renal fibrosis in obstructive nephropathy (Eitner et al. 2008). PDGF-CC also exerts profibrotic effects by directly enhancing fibroblast proliferation, as well as accelerating leukocyte infiltration (Eitner et al. 2008). Moreover, PDGF-CC serves as a pro-angiogenic mediator in glomeruli (Boor et al. 2015). In contrast to PDGF-A, which has limited effects in renal fibrosis (Tang et al. 1996), PDGF-B and PDGFR-β mediate mesangial proliferation both in vitro and in vivo; high doses of PDGF-BB induce proliferation of tubulointerstitial cells and promote the myofibroblast generation and fibrosis (Boor et al. 2014; Buhl et al. 2016; Das et al. 2017; Tang et al. 1996). Collectively, renal inflammatory cells produce plenty of PDGF, driving the progression of renal fibrosis.
5 Conclusion
Inflammation is the initial response to cellular injuries and is the key process in wound healing and renal repair. However, unresolved renal inflammation leads to fibrosis with loss of renal function. In this process, both circulating leukocytes and intrinsic kidney cells are key inflammatory cell types and play critical roles in driving acute renal inflammation to chronic fibrosis, leading to the end-stage kidney disease. There are two primary mechanisms regulating the pathway from renal inflammation to fibrosis. First, fibrogenetic growth factors produced by inflammatory cells promote local fibroblasts, or inflammatory cells themselves, to proliferate and produce ECM. Second, inflammatory cells convert into collagen-producing fibroblasts or myofibroblasts directly from EMT, EndoMT, pericytes, fibrocytes or MMT. Many inflammatory cytokines and growth factors, like TGF-β, are involved in the inflammation–fibrosis process. Collectively, blocking excessive inflammatory responses may represent an effective therapy for renal fibrotic diseases.
References
Abboud HE (2012) Mesangial cell biology. Exp Cell Res 318:979–985
Allison SJ (2013) Fibrosis: the source of myofibroblasts in kidney fibrosis. Nat Rev Nephrol 9:494
Anders HJ, Ryu M (2011) Renal microenvironments and macrophage phenotypes determine progression or resolution of renal inflammation and fibrosis. Kidney Int 80:915–925
Anders HJ, Vielhauer V, Eis V, Linde Y, Kretzler M et al (2004) Activation of toll-like receptor-9 induces progression of renal disease in MRL-Fas(lpr) mice. FASEB J 18:534–536
Beghdadi W, Madjene LC, Claver J, Pejler G, Beaudoin L, Lehuen A, Daugas E, Blank U (2013) Mast cell chymase protects against renal fibrosis in murine unilateral ureteral obstruction. Kidney Int 84:317–326
Bielesz B, Sirin Y, Si H, Niranjan T, Gruenwald A et al (2010) Epithelial Notch signaling regulates interstitial fibrosis development in the kidneys of mice and humans. J Clin Invest 120:4040–4054
Bojakowski K, Abramczyk P, Bojakowska M, Zwolinska A, Przybylski J, Gaciong Z (2001) Fucoidan improves the renal blood flow in the early stage of renal ischemia/reperfusion injury in the rat. J Physiol Pharmacol 52:137–143
Boor P, Floege J (2011) Chronic kidney disease growth factors in renal fibrosis. Clin Exp Pharmacol Physiol 38:441–450
Boor P, Konieczny A, Villa L, Kunter U, van Roeyen CR et al (2007) PDGF-D inhibition by CR10 ameliorates tubulointerstitial fibrosis following experimental glomerulonephritis. Nephrol Dial Transplant 22:1323–1331
Boor P, Ostendorf T, Floege J (2010) Renal fibrosis: novel insights into mechanisms and therapeutic targets. Nat Rev Nephrol 6:643–656
Boor P, Ostendorf T, Floege J (2014) PDGF and the progression of renal disease. Nephrol Dial Transplant 29(Suppl 1):i45–i54
Boor P, Babickova J, Steegh F, Hautvast P, Martin IV et al (2015) Role of platelet-derived growth factor-CC in capillary rarefaction in renal fibrosis. Am J Pathol 185:2132–2142
Bottinger EP, Bitzer M (2002) TGF-beta signaling in renal disease. J Am Soc Nephrol 13:2600–2610
Brahler S, Ising C, Hagmann H, Rasmus M, Hoehne M et al (2012) Intrinsic proinflammatory signaling in podocytes contributes to podocyte damage and prolonged proteinuria. Am J Physiol Renal Physiol 303:F1473–F1485
Broekema M, Harmsen MC, van Luyn MJ, Koerts JA, Petersen AH et al (2007) Bone marrow-derived myofibroblasts contribute to the renal interstitial myofibroblast population and produce procollagen I after ischemia/reperfusion in rats. J Am Soc Nephrol 18:165–175
Bucala R, Spiegel LA, Chesney J, Hogan M, Cerami A (1994) Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol Med 1:71–81
Buchtler S, Grill A, Hofmarksrichter S, Stockert P, Schiechl-Brachner G et al (2018) Cellular origin and functional relevance of collagen i production in the kidney. J Am Soc Nephrol 29:1859–1873
Buhl EM, Djudjaj S, Babickova J, Klinkhammer BM, Folestad E et al (2016) The role of PDGF-D in healthy and fibrotic kidneys. Kidney Int 8:848–861
Campbell MT, Hile KL, Zhang H, Asanuma H, Vanderbrink BA et al (2011) Toll-like receptor 4: a novel signaling pathway during renal fibrogenesis. J Surg Res 168:e61–e69
Canaud G, Bienaime F, Viau A, Treins C, Baron W et al (2013) AKT2 is essential to maintain podocyte viability and function during chronic kidney disease. Nat Med 19:1288–1296
Cao Q, Wang Y, Harris DC (2013) Pathogenic and protective role of macrophages in kidney disease. Am J Physiol Renal Physiol 305:F3–F11
Chen G, Lin SC, Chen J, He L, Dong F et al (2011a) CXCL16 recruits bone marrow-derived fibroblast precursors in renal fibrosis. J Am Soc Nephrol 22:1876–1886
Chen YT, Chang FC, Wu CF, Chou YH, Hsu HL et al (2011b) Platelet-derived growth factor receptor signaling activates pericyte-myofibroblast transition in obstructive and post-ischemic kidney fibrosis. Kidney Int 80:1170–1181
Chen J, Chen MX, Fogo AB, Harris RC, Chen JK (2013) mVps34 deletion in podocytes causes glomerulosclerosis by disrupting intracellular vesicle trafficking. J Am Soc Nephrol 24:198–207
Chen G, Dong Z, Liu H, Liu Y, Duan S, Liu F, Chen H (2016) mTOR signaling regulates protective activity of transferred CD4+ Foxp3+ T Cells in repair of acute kidney injury. J Immunol 197:3917–3926
Cheng A, Dong Y, Zhu F, Liu Y, Hou FF, Nie J (2013) AGE-LDL activates Toll like receptor 4 pathway and promotes inflammatory cytokines production in renal tubular epithelial cells. Int J Biol Sci 9:94–107
Chesney J, Metz C, Stavitsky AB, Bacher M, Bucala R (1998) Regulated production of type I collagen and inflammatory cytokines by peripheral blood fibrocytes. J Immunol 160:419–425
Chung AC, Lan HY (2011) Chemokines in renal injury. J Am Soc Nephrol 22:802–809
Correa-Costa M, Braga TT, Semedo P, Hayashida CY, Bechara LR et al (2011) Pivotal role of Toll-like receptors 2 and 4, its adaptor molecule MyD88, and inflammasome complex in experimental tubule-interstitial nephritis. PLoS ONE 6:e29004
Crean JK, Furlong F, Finlay D, Mitchell D, Murphy M et al (2004) Connective tissue growth factor [CTGF]/CCN2 stimulates mesangial cell migration through integrated dissolution of focal adhesion complexes and activation of cell polarization. FASEB J 18:1541–1543
D’Agati V, Schmidt AM (2010) RAGE and the pathogenesis of chronic kidney disease. Nat Rev Nephrol 6:352–360
Dai Y, Gu L, Yuan W, Yu Q, Ni Z et al (2013) Podocyte-specific deletion of signal transducer and activator of transcription 3 attenuates nephrotoxic serum-induced glomerulonephritis. Kidney Int 84:950–961
Danelli L, Madjene LC, Madera-Salcedo I, Gautier G, Pacreau E et al (2017) Early phase mast cell activation determines the chronic outcome of renal ischemia-reperfusion injury. J Immunol 198:2374–2382
Daroux M, Prevost G, Maillard-Lefebvre H, Gaxatte C, D’Agati VD et al (2010) Advanced glycation end-products: implications for diabetic and non-diabetic nephropathies. Diabetes Metab 36:1–10
Das R, Xu S, Quan X, Nguyen TT, Kong ID et al (2014) Upregulation of mitochondrial Nox4 mediates TGF-beta-induced apoptosis in cultured mouse podocytes. Am J Physiol Renal Physiol 306:F155–F167
Das F, Ghosh-Choudhury N, Venkatesan B, Kasinath BS, Ghosh Choudhury G (2017) PDGF receptor-beta uses Akt/mTORC1 signaling node to promote high glucose-induced renal proximal tubular cell collagen I (alpha2) expression. Am J Physiol Renal Physiol 313:F291–F307
Deelman L, Sharma K (2009) Mechanisms of kidney fibrosis and the role of antifibrotic therapies. Curr Opin Nephrol Hypertens 18:85–90
Demmers MW, Baan CC, van Beelen E, Ijzermans JN, Weimar W, Rowshani AT (2013) Differential effects of activated human renal epithelial cells on T-cell migration. PLoS ONE 8:e64916
Disteldorf EM, Krebs CF, Paust HJ, Turner JE, Nouailles G et al (2015) CXCL5 drives neutrophil recruitment in TH17-mediated GN. J Am Soc Nephrol 26:55–66
Djudjaj S, Boor P (2018) Cellular and molecular mechanisms of kidney fibrosis. Mol Aspects Med
Dong Y, Yang M, Zhang J, Peng X, Cheng J, Cui T, Du J (2016) Depletion of CD8+ T cells exacerbates CD4+ T cell-induced monocyte-to-fibroblast transition in renal fibrosis. J Immunol 196:1874–1881
Duffield JS, Humphreys BD (2011) Origin of new cells in the adult kidney: results from genetic labeling techniques. Kidney Int 79:494–501
Durvasula RV, Shankland SJ (2006) The renin-angiotensin system in glomerular podocytes: mediator of glomerulosclerosis and link to hypertensive nephropathy. Curr Hypertens Rep 8:132–138
Durvasula RV, Shankland SJ (2008) Activation of a local renin angiotensin system in podocytes by glucose. Am J Physiol Renal Physiol 294:F830–F839
Eardley KS, Kubal C, Zehnder D, Quinkler M, Lepenies J et al (2008) The role of capillary density, macrophage infiltration and interstitial scarring in the pathogenesis of human chronic kidney disease. Kidney Int 74:495–504
Eddy AA, Neilson EG (2006) Chronic kidney disease progression. J Am Soc Nephrol 17:2964–2966
Eitner F, Bucher E, van Roeyen C, Kunter U, Rong S et al (2008) PDGF-C is a proinflammatory cytokine that mediates renal interstitial fibrosis. J Am Soc Nephrol 19:281–289
Eremina V, Cui S, Gerber H, Ferrara N, Haigh J et al (2006) Vascular endothelial growth factor a signaling in the podocyte-endothelial compartment is required for mesangial cell migration and survival. J Am Soc Nephrol 17:724–735
Fan JM, Ng YY, Hill PA, Nikolic-Paterson DJ, Mu W et al (1999) Transforming growth factor-beta regulates tubular epithelial-myofibroblast transdifferentiation in vitro. Kidney Int 56:1455–1467
Fan JM, Huang XR, Ng YY, Nikolic-Paterson DJ, Mu W et al (2001) Interleukin-1 induces tubular epithelial-myofibroblast transdifferentiation through a transforming growth factor-beta1-dependent mechanism in vitro. Am J Kidney Dis 37:820–831
Fine LG, Norman JT (2008) Chronic hypoxia as a mechanism of progression of chronic kidney diseases: from hypothesis to novel therapeutics. Kidney Int 74:867–872
Floege J, Burg M, Hugo C, Gordon KL, Van Goor H et al (1998) Endogenous fibroblast growth factor-2 mediates cytotoxicity in experimental mesangioproliferative glomerulonephritis. J Am Soc Nephrol 9:792–801
Floege J, Eitner F, Alpers CE (2008) A new look at platelet-derived growth factor in renal disease. J Am Soc Nephrol 19:12–23
Fogo AB (2011) The targeted podocyte. J Clin Invest 121:2142–2145
Fu S, Zhang N, Yopp AC, Chen D, Mao M et al (2004) TGF-beta induces Foxp3+ T-regulatory cells from CD4+ CD25-precursors. Am J Transplant 4:1614–1627
Fujiu K, Manabe I, Nagai R (2011) Renal collecting duct epithelial cells regulate inflammation in tubulointerstitial damage in mice. J Clin Invest 121:3425–3441
Fukuda K, Yoshitomi K, Yanagida T, Tokumoto M, Hirakata H (2001) Quantification of TGF-beta1 mRNA along rat nephron in obstructive nephropathy. Am J Physiol Renal Physiol 281:F513–F521
Funaba M, Ikeda T, Murakami M, Ogawa K, Nishino Y et al (2006) Transcriptional regulation of mouse mast cell protease-7 by TGF-beta. Biochem Biophys Acta 1759:166–170
Gentle ME, Shi S, Daehn I, Zhang T, Qi H et al (2013) Epithelial cell TGFbeta signaling induces acute tubular injury and interstitial inflammation. J Am Soc Nephrol 24:787–799
Gewin LS (2018) Renal fibrosis: primacy of the proximal tubule. Matrix Biol 68–69:248–262
Gewin L, Bulus N, Mernaugh G, Moeckel G, Harris RC et al (2010) TGF-beta receptor deletion in the renal collecting system exacerbates fibrosis. J Am Soc Nephrol 21:1334–1343
Gewin L, Vadivelu S, Neelisetty S, Srichai MB, Paueksakon P et al (2012) Deleting the TGF-beta receptor attenuates acute proximal tubule injury. J Am Soc Nephrol 23:2001–2011
Gewin L, Zent R, Pozzi A (2017) Progression of chronic kidney disease: too much cellular talk causes damage. Kidney Int 91:552–560
Godel M, Hartleben B, Herbach N, Liu S, Zschiedrich S et al (2011) Role of mTOR in podocyte function and diabetic nephropathy in humans and mice. J Clin Invest 121:2197–2209
Gomez-Guerrero C, Hernandez-Vargas P, Lopez-Franco O, Ortiz-Munoz G, Egido J (2005) Mesangial cells and glomerular inflammation: from the pathogenesis to novel therapeutic approaches. Curr Drug Targets Inflamm Allergy 4:341–351
Gorelik L, Flavell RA (2002) Transforming growth factor-beta in T-cell biology. Nat Rev Immunol 2:46–53
Grahammer F, Schell C, Huber TB (2013) The podocyte slit diaphragm–from a thin grey line to a complex signalling hub. Nat Rev Nephrol 9:587–598
Grande MT, Perez-Barriocanal F, Lopez-Novoa JM (2010) Role of inflammation in tubulo-interstitial damage associated to obstructive nephropathy. J Inflamm (Lond) 7:19
Grande MT, Sanchez-Laorden B, Lopez-Blau C, De Frutos CA, Boutet A et al (2015) Snail1-induced partial epithelial-to-mesenchymal transition drives renal fibrosis in mice and can be targeted to reverse established disease. Nat Med 21:989–997
Gratchev A, Guillot P, Hakiy N, Politz O, Orfanos CE, Schledzewski K, Goerdt S (2001) Alternatively activated macrophages differentially express fibronectin and its splice variants and the extracellular matrix protein betaIG-H3. Scand J Immunol 53:386–392
Gruber BL, Marchese MJ, Kew RR (1994) Transforming growth factor-beta 1 mediates mast cell chemotaxis. J Immunol 152:5860–5867
Gruden G, Perin PC, Camussi G (2005) Insight on the pathogenesis of diabetic nephropathy from the study of podocyte and mesangial cell biology. Curr Diab Rev 1:27–40
Guerrot D, Dussaule JC, Kavvadas P, Boffa JJ, Chadjichristos CE, Chatziantoniou C (2012) Progression of renal fibrosis: the underestimated role of endothelial alterations. Fibrogenesis Tissue repair 5(Suppl 1):S15
Guo S, Wietecha TA, Hudkins KL, Kida Y, Spencer MW et al (2011) Macrophages are essential contributors to kidney injury in murine cryoglobulinemic membranoproliferative glomerulonephritis. Kidney Int 80:946–958
Han Y, Ma FY, Tesch GH, Manthey CL, Nikolic-Paterson DJ (2011) c-fms blockade reverses glomerular macrophage infiltration and halts development of crescentic anti-GBM glomerulonephritis in the rat. Lab Invest 91:978–991
Han Y, Ma FY, Tesch GH, Manthey CL, Nikolic-Paterson DJ (2013) Role of macrophages in the fibrotic phase of rat crescentic glomerulonephritis. Am J Physiol Renal Physiol 304:F1043–F1053
Harris RC, Neilson EG (2006) Toward a unified theory of renal progression. Annu Rev Med 57:365–380
Hathaway CK, Gasim AM, Grant R, Chang AS, Kim HS et al (2015) Low TGFbeta1 expression prevents and high expression exacerbates diabetic nephropathy in mice. Proc Natl Acad Sci USA 112:5815–5820
Hato T, El-Achkar TM, Dagher PC (2013) Sisters in arms: myeloid and tubular epithelial cells shape renal innate immunity. Am J Physiol Renal Physiol 304:F1243–F1251
He W, Dai C, Li Y, Zeng G, Monga SP, Liu Y (2009) Wnt/beta-catenin signaling promotes renal interstitial fibrosis. J Am Soc Nephrol 20:765–776
Henderson NC, Mackinnon AC, Farnworth SL, Kipari T, Haslett C et al (2008) Galectin-3 expression and secretion links macrophages to the promotion of renal fibrosis. Am J Pathol 172:288–298
Higgins DF, Kimura K, Bernhardt WM, Shrimanker N, Akai Y et al (2007) Hypoxia promotes fibrogenesis in vivo via HIF-1 stimulation of epithelial-to-mesenchymal transition. J Clin Invest 117:3810–3820
Higgins DF, Kimura K, Iwano M, Haase VH (2008) Hypoxia-inducible factor signaling in the development of tissue fibrosis. Cell Cycle 7:1128–1132
Hochane M, Raison D, Coquard C, Beraud C, Bethry A et al (2018) Parathyroid hormone-related protein modulates inflammation in mouse mesangial cells and blunts apoptosis by enhancing COX-2 expression. Am J Physiol Cell Physiol 314:C242–C253
Holdsworth SR, Summers SA (2008) Role of mast cells in progressive renal diseases. J Am Soc Nephrol 19:2254–2261
Huang XR, Chung AC, Wang XJ, Lai KN, Lan HY (2008a) Mice overexpressing latent TGF-beta1 are protected against renal fibrosis in obstructive kidney disease. Am J Physiol Renal Physiol 295:F118–F127
Huang XR, Chung AC, Zhou L, Wang XJ, Lan HY (2008b) Latent TGF-beta1 protects against crescentic glomerulonephritis. J Am Soc Nephrol 19:233–242
Humphreys BD (2018) Mechanisms of renal fibrosis. Annu Rev Physiol 80:309–326
Humphreys BD, Lin SL, Kobayashi A, Hudson TE, Nowlin BT et al (2010) Fate tracing reveals the pericyte and not epithelial origin of myofibroblasts in kidney fibrosis. Am J Pathol 176:85–97
Inoki K, Mori H, Wang J, Suzuki T, Hong S et al (2011) mTORC1 activation in podocytes is a critical step in the development of diabetic nephropathy in mice. J Clin Invest 121:2181–2196
Kanasaki K, Taduri G, Koya D (2013) Diabetic nephropathy: the role of inflammation in fibroblast activation and kidney fibrosis. Front Endocrinol 4:7
Kang DH, Kanellis J, Hugo C, Truong L, Anderson S et al (2002) Role of the microvascular endothelium in progressive renal disease. J Am Soc Nephrol 13:806–816
Kato N, Yuzawa Y, Kosugi T, Hobo A, Sato W et al (2009) The E-selectin ligand basigin/CD147 is responsible for neutrophil recruitment in renal ischemia/reperfusion. J Am Soc Nephrol 20:1565–1576
Kelly KJ, Williams WW Jr, Colvin RB, Bonventre JV (1994) Antibody to intercellular adhesion molecule 1 protects the kidney against ischemic injury. Proc Nati Acad Sci USA 91:812–816
Kelly KJ, Williams WW Jr, Colvin RB, Meehan SM, Springer TA et al (1996) Intercellular adhesion molecule-1-deficient mice are protected against ischemic renal injury. J Clin Invest 97:1056–1063
Kelly KJ, Burford JL, Dominguez JH (2009) Postischemic inflammatory syndrome: a critical mechanism of progression in diabetic nephropathy. Am J Physiol Renal Physiol 297:F923–F931
Kim DH, Moon SO, Jung YJ, Lee AS, Kang KP et al (2009) Mast cells decrease renal fibrosis in unilateral ureteral obstruction. Kidney Int 75:1031–1038
Kim SM, Lee SH, Lee A, Kim DJ, Kim YG et al (2015) Targeting T helper 17 by mycophenolate mofetil attenuates diabetic nephropathy progression. Transl Res 166:375–383
Kimura K, Iwano M, Higgins DF, Yamaguchi Y, Nakatani K et al (2008) Stable expression of HIF-1alpha in tubular epithelial cells promotes interstitial fibrosis. Am J Physiol Renal Physiol 295:F1023–F1029
Kitamoto K, Machida Y, Uchida J, Izumi Y, Shiota M et al (2009) Effects of liposome clodronate on renal leukocyte populations and renal fibrosis in murine obstructive nephropathy. J Pharmacol Sci 111:285–292
Kitamura M, Suto TS (1997) TGF-beta and glomerulonephritis: anti-inflammatory versus prosclerotic actions. Nephrol Dial Transplant 12:669–679
Kitching AR, Holdsworth SR (2011) The emergence of TH17 cells as effectors of renal injury. J Am Soc Nephrol 22:235–238
Ko GJ, Boo CS, Jo SK, Cho WY, Kim HK (2008) Macrophages contribute to the development of renal fibrosis following ischaemia/reperfusion-induced acute kidney injury. Nephrol Dial Transplant 23:842–852
Kondo S, Kagami S, Kido H, Strutz F, Muller GA, Kuroda Y (2001) Role of mast cell tryptase in renal interstitial fibrosis. J Am Soc Nephrol 12:1668–1676
Kong D, Li Y, Wang Z, Banerjee S, Ahmad A et al (2009) miR-200 regulates PDGF-D-mediated epithelial-mesenchymal transition, adhesion, and invasion of prostate cancer cells. Stem Cells 27:1712–1721
Ku CH, White KE, Dei Cas A, Hayward A, Webster Z et al (2008) Inducible overexpression of sFlt-1 in podocytes ameliorates glomerulopathy in diabetic mice. Diabetes 57:2824–2833
Lai KN, Leung JC, Chan LY, Saleem MA, Mathieson PW et al (2008) Activation of podocytes by mesangial-derived TNF-alpha: glomerulo-podocytic communication in IgA nephropathy. Am J Physiol Renal Physiol 294:F945–F955
Lai KN, Leung JC, Chan LY, Saleem MA, Mathieson PW et al (2009) Podocyte injury induced by mesangial-derived cytokines in IgA nephropathy. Nephrol Dial Transplant 24:62–72
Lan HY (2011) Diverse roles of TGF-beta/Smads in renal fibrosis and inflammation. Int J Biol Sci 7:1056–1067
Lan HY, Nikolic-Paterson DJ, Mu W, Atkins RC (1995) Local macrophage proliferation in the progression of glomerular and tubulointerstitial injury in rat anti-GBM glomerulonephritis. Kidney Int 48:753–760
Lan HY, Bacher M, Yang N, Mu W, Nikolic-Paterson DJ et al (1997) The pathogenic role of macrophage migration inhibitory factor in immunologically induced kidney disease in the rat. J Exp Med 185:1455–1465
Laping NJ, Olson BA, Ho T, Ziyadeh FN, Albrightson CR (2000) Hepatocyte growth factor: a regulator of extracellular matrix genes in mouse mesangial cells. Biochem Pharmacol 59:847–853
LeBleu VS, Kalluri R (2011) Blockade of PDGF receptor signaling reduces myofibroblast number and attenuates renal fibrosis. Kidney Int 80:1119–1121
LeBleu VS, Taduri G, O’Connell J, Teng Y, Cooke VG et al (2013) Origin and function of myofibroblasts in kidney fibrosis. Nat Med 19:1047–1053
Lebrin F, Deckers M, Bertolino P, Ten Dijke P (2005) TGF-beta receptor function in the endothelium. Cardiovascular Res 65:599–608
Lee SB, Kalluri R (2010) Mechanistic connection between inflammation and fibrosis. Kidney Int Suppl S22–S26
Li Y, Yang J, Dai C, Wu C, Liu Y (2003) Role for integrin-linked kinase in mediating tubular epithelial to mesenchymal transition and renal interstitial fibrogenesis. J Clin Invest 112:503–516
Li Y, Kang YS, Dai C, Kiss LP, Wen X, Liu Y (2008) Epithelial-to-mesenchymal transition is a potential pathway leading to podocyte dysfunction and proteinuria. Am J Pathol 172:299–308
Li J, Qu X, Yao J, Caruana G, Ricardo SD et al (2010) Blockade of endothelial-mesenchymal transition by a Smad3 inhibitor delays the early development of streptozotocin-induced diabetic nephropathy. Diabetes 59:2612–2624
Lin M, Tang SC (2013) Toll-like receptors: sensing and reacting to diabetic injury in the kidney. Nephrol Dial Transplant
Lin SL, Kisseleva T, Brenner DA, Duffield JS (2008) Pericytes and perivascular fibroblasts are the primary source of collagen-producing cells in obstructive fibrosis of the kidney. Am J Pathol 173:1617–1627
Lin SL, Castano AP, Nowlin BT, Lupher ML Jr, Duffield JS (2009) Bone marrow Ly6Chigh monocytes are selectively recruited to injured kidney and differentiate into functionally distinct populations. J Immunol 183:6733–6743
Lin M, Yiu WH, Wu HJ, Chan LY, Leung JC et al (2012) Toll-like receptor 4 promotes tubular inflammation in diabetic nephropathy. J Am Soc Nephrol 23:86–102
Lin JR, Zheng YJ, Zhang ZB, Shen WL, Li XD et al (2018) Suppression of endothelial-to-mesenchymal transition by SIRT (Sirtuin) 3 alleviated the development of hypertensive renal injury. Hypertension
Liu Y (2004) Epithelial to mesenchymal transition in renal fibrogenesis: pathologic significance, molecular mechanism, and therapeutic intervention. J Am Soc Nephrol 15:1–12
Liu Y (2006) Renal fibrosis: new insights into the pathogenesis and therapeutics. Kidney Int 69:213–217
Liu Y (2010) New insights into epithelial-mesenchymal transition in kidney fibrosis. J Am Soc Nephrol 21:212–222
Liu Y (2011) Cellular and molecular mechanisms of renal fibrosis. Nat Rev Nephrol 7:684–696
Liu F, Chen HY, Huang XR, Chung AC, Zhou L et al (2011) C-reactive protein promotes diabetic kidney disease in a mouse model of type 1 diabetes. Diabetologia 54:2713–2723
Liu L, Kou P, Zeng Q, Pei G, Li Y et al (2012) CD4+ T Lymphocytes, especially Th2 cells, contribute to the progress of renal fibrosis. Am J Nephrol 36:386–396
Liu P, Lassen E, Nair V, Berthier CC, Suguro M et al (2017) Transcriptomic and proteomic profiling provides insight into mesangial cell function in IgA nephropathy. J Am Soc Nephrol 28:2961–2972
Liu BC, Tang TT, Lv LL, Lan HY (2018) Renal tubule injury: a driving force toward chronic kidney disease. Kidney Int 93:568–579
Loeffler I, Wolf G (2013) Transforming growth factor-beta and the progression of renal disease. Nephrol Dial Transplant
Lopez-Hernandez FJ, Lopez-Novoa JM (2012) Role of TGF-beta in chronic kidney disease: an integration of tubular, glomerular and vascular effects. Cell Tissue Res 347:141–154
Lovisa S, LeBleu VS, Tampe B, Sugimoto H, Vadnagara K et al (2015) Epithelial-to-mesenchymal transition induces cell cycle arrest and parenchymal damage in renal fibrosis. Nat Med 21:998–1009
Lu J, Cao Q, Zheng D, Sun Y, Wang C et al (2013) Discrete functions of M2a and M2c macrophage subsets determine their relative efficacy in treating chronic kidney disease. Kidney Int 84:745–755
Lu Y, Mei Y, Chen L, Wu L, Wang X et al (2018) The role of transcriptional factor D-site-binding protein in circadian CCL2 gene expression in anti-Thy1 nephritis. Cell Mol Immunol
Lv W, Booz GW, Wang Y, Fan F, Roman RJ (2018) Inflammation and renal fibrosis: recent developments on key signaling molecules as potential therapeutic targets. Eur J Pharmacol 820:65–76
Lyons RM, Gentry LE, Purchio AF, Moses HL (1990) Mechanism of activation of latent recombinant transforming growth factor beta 1 by plasmin. J Cell Biol 110:1361–1367
Ma LJ, Yang H, Gaspert A, Carlesso G, Barty MM et al (2003) Transforming growth factor-beta-dependent and -independent pathways of induction of tubulointerstitial fibrosis in beta6(−/−) mice. Am J Pathol 163:1261–1273
Ma FY, Flanc RS, Tesch GH, Bennett BL, Friedman GC et al (2009a) Blockade of the c-Jun amino terminal kinase prevents crescent formation and halts established anti-GBM glomerulonephritis in the rat. Lab Inves 89:470–484
Ma FY, Liu J, Kitching AR, Manthey CL, Nikolic-Paterson DJ (2009b) Targeting renal macrophage accumulation via c-fms kinase reduces tubular apoptosis but fails to modify progressive fibrosis in the obstructed rat kidney. Am J Physiol Renal Physiol 296:F177–F185
Ma FY, Ikezumi Y, Nikolic-Paterson DJ (2010) Macrophage signaling pathways: a novel target in renal disease. Semin Nephrol 30:334–344
Mack M, Rosenkranz AR (2009) Basophils and mast cells in renal injury. Kidney Int 76:1142–1147
Margulis A, Nocka KH, Brennan AM, Deng B, Fleming M et al (2009) Mast cell-dependent contraction of human airway smooth muscle cell-containing collagen gels: influence of cytokines, matrix metalloproteases, and serine proteases. J Immunol 183:1739–1750
Mathieson PW (2009) Update on the podocyte. Curr Opin Nephrol Hypertens 18:206–211
Mehrotra P, Patel JB, Ivancic CM, Collett JA, Basile DP (2015) Th-17 cell activation in response to high salt following acute kidney injury is associated with progressive fibrosis and attenuated by AT-1R antagonism. Kidney Int 88:776–784
Meldrum KK, Zhang H, Hile KL, Moldower LL, Dong Z, Meldrum DR (2012) Profibrotic effect of interleukin-18 in HK-2 cells is dependent on stimulation of the Toll-like receptor 4 (TLR4) promoter and increased TLR4 expression. J Biol Chem 287:40391–40399
Meng XM, Huang XR, Chung AC, Qin W, Shao X et al (2010) Smad2 protects against TGF-beta/Smad3-mediated renal fibrosis. J Am Soc Nephrol 21:1477–1487
Meng XM, Huang XR, Xiao J, Chen HY, Zhong X, Chung AC, Lan HY (2012a) Diverse roles of TGF-beta receptor II in renal fibrosis and inflammation in vivo and in vitro. J Pathol 227:175–188
Meng XM, Huang XR, Xiao J, Chung AC, Qin W et al (2012b) Disruption of Smad4 impairs TGF-beta/Smad3 and Smad7 transcriptional regulation during renal inflammation and fibrosis in vivo and in vitro. Kidney Int 81:266–279
Meng XM, Chung AC, Lan HY (2013) Role of the TGF-beta/BMP-7/Smad pathways in renal diseases. Clin Sci (Lond) 124:243–254
Meng XM, Nikolic-Paterson DJ, Lan HY (2014) Inflammatory processes in renal fibrosis. Nat Rev Nephrol 10:493–503
Meng XM, Tang PM, Li J, Lan HY (2015) TGF-beta/Smad signaling in renal fibrosis. Front Physiol 6:82
Meng XM, Nikolic-Paterson DJ, Lan HY (2016a) TGF-beta: the master regulator of fibrosis. Nat Rev Nephrol 12:325–338
Meng XM, Wang S, Huang XR, Yang C, Xiao J et al (2016b) Inflammatory macrophages can transdifferentiate into myofibroblasts during renal fibrosis. Cell Death Dis 7:e2495
Mezzano SA, Ruiz-Ortega M, Egido J (2001) Angiotensin II and renal fibrosis. Hypertension 38:635–638
Miyazawa S, Hotta O, Doi N, Natori Y, Nishikawa K (2004) Role of mast cells in the development of renal fibrosis: use of mast cell-deficient rats. Kidney Int 65: 2228–2237
Mohamed R, Jayakumar C, Chen F, Fulton D, Stepp D et al (2016) Low-dose IL-17 therapy prevents and reverses diabetic nephropathy, metabolic syndrome, and associated organ fibrosis. J Am Soc Nephrol 27:745–765
Munger JS, Huang X, Kawakatsu H, Griffiths MJ, Dalton SL et al (1999) The integrin alpha v beta 6 binds and activates latent TGF beta 1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell 96:319–328
Nakagawa T, Lan HY, Zhu HJ, Kang DH, Schreiner GF, Johnson RJ (2004a) Differential regulation of VEGF by TGF-beta and hypoxia in rat proximal tubular cells. Am J Physiol Renal Physiol 287:F658–F664
Nakagawa T, Li JH, Garcia G, Mu W, Piek E et al (2004b) TGF-beta induces proangiogenic and antiangiogenic factors via parallel but distinct Smad pathways. Kidney Int 66:605–613
Negre-Salvayre A, Coatrieux C, Ingueneau C, Salvayre R (2008) Advanced lipid peroxidation end products in oxidative damage to proteins. Potential role in diseases and therapeutic prospects for the inhibitors. Br J Pharmacol 153:6–20
Nguan CY, Du C (2009) Renal tubular epithelial cells as immunoregulatory cells in renal allograft rejection. Transplant Rev (Orlando) 23:129–138
Niedermeier M, Reich B, Rodriguez Gomez M, Denzel A, Schmidbauer K et al (2009) CD4 +T cells control the differentiation of Gr1+ monocytes into fibrocytes. Proc Nati Acad Sci USA 106:17892–17897
Nielsen R, Mollet G, Esquivel EL, Weyer K, Nielsen PK et al (2013) Increased lysosomal proteolysis counteracts protein accumulation in the proximal tubule during focal segmental glomerulosclerosis. Kidney Int 84:902–910
Niranjan T, Bielesz B, Gruenwald A, Ponda MP, Kopp JB et al (2008) The Notch pathway in podocytes plays a role in the development of glomerular disease. Nat Med 14:290–298
Nishida M, Hamaoka K (2008) Macrophage phenotype and renal fibrosis in obstructive nephropathy. Nephron Exp Nephrol 110:e31–e36
Ostendorf T, Rong S, Boor P, Wiedemann S, Kunter U et al (2006) Antagonism of PDGF-D by human antibody CR170 prevents renal scarring in experimental glomerulonephritis. J Am Soc Nephrol 17:1054–1062
Ostendorf T, Eitner F, Floege J (2012) The PDGF family in renal fibrosis. Pediatr Nephrol 27:1041–1050
Paust HJ, Turner JE, Steinmetz OM, Peters A, Heymann F et al (2009) The IL-23/Th17 axis contributes to renal injury in experimental glomerulonephritis. J Am Soc Nephrol 2:969–979
Peng X, Xiao Z, Zhang J, Li Y, Dong Y, Du J (2015) IL-17A produced by both gammadelta T and Th17 cells promotes renal fibrosis via RANTES-mediated leukocyte infiltration after renal obstruction. J Pathol 235:79–89
Pober JS, Sessa WC (2007) Evolving functions of endothelial cells in inflammation. Nat Rev Immunol 7:803–815
Pons M, Ali L, Beghdadi W, Danelli L, Alison M et al (2017) Mast cells and MCPT4 chymase promote renal impairment after partial ureteral obstruction. Front Immunol 8:450
Pulskens WP, Rampanelli E, Teske GJ, Butter LM, Claessen N et al (2010) TLR4 promotes fibrosis but attenuates tubular damage in progressive renal injury. J Am Soc Nephrol 21:1299–1308
Qiao X, Rao P, Zhang Y, Liu L, Pang M et al (2018) Redirecting TGF-beta signaling through the beta-catenin/Foxo complex prevents kidney fibrosis. J Am Soc Nephrol 29:557–570
Reich B, Schmidbauer K, Rodriguez Gomez M, Johannes Hermann F, Gobel N et al (2013) Fibrocytes develop outside the kidney but contribute to renal fibrosis in a mouse model. Kidney Int 84:78–89
Reilkoff RA, Bucala R, Herzog EL (2011) Fibrocytes: emerging effector cells in chronic inflammation. Nat Rev Immunol 11:427–435
Ricardo SD, van Goor H, Eddy AA (2008) Macrophage diversity in renal injury and repair. J Clin Invest 118:3522–3530
Robertson H, Ali S, McDonnell BJ, Burt AD, Kirby JA (2004) Chronic renal allograft dysfunction: the role of T cell-mediated tubular epithelial to mesenchymal cell transition. J Am Soc Nephrol 15:390–397
Rutkowski JM, Wang ZV, Park AS, Zhang J, Zhang D et al (2013) Adiponectin promotes functional recovery after podocyte ablation. J Am Soc Nephrol 24:268–282
Sakai N, Wada T, Yokoyama H, Lipp M, Ueha S, Matsushima K, Kaneko S (2006) Secondary lymphoid tissue chemokine (SLC/CCL21)/CCR182 signaling regulates fibrocytes in renal fibrosis. Proc Nati Acad Sci USA 103:14098–14103
Sam R, Wanna L, Gudehithlu KP, Garber SL, Dunea G et al (2006) Glomerular epithelial cells transform to myofibroblasts: early but not late removal of TGF-beta1 reverses transformation. Transl Res 148:142–148
Scandiuzzi L, Beghdadi W, Daugas E, Abrink M, Tiwari N et al (2010) Mouse mast cell protease-4 deteriorates renal function by contributing to inflammation and fibrosis in immune complex-mediated glomerulonephritis. J Immunol 185:624–633
Schiffer M, Bitzer M, Roberts IS, Kopp JB, ten Dijke P et al (2001) Apoptosis in podocytes induced by TGF-beta and Smad7. J Clin Invest 108:807–816
Schlondorff D, Banas B (2009) The mesangial cell revisited: no cell is an island. J Am Soc Nephrol 20:1179–1187
Schnaper HW, Hayashida T, Hubchak SC, Poncelet AC (2003) TGF-beta signal transduction and mesangial cell fibrogenesis. Am J Physiol Renal Physiol 284:F243–F252
Schnoor M, Cullen P, Lorkowski J, Stolle K, Robenek H et al (2008) Production of type VI collagen by human macrophages: a new dimension in macrophage functional heterogeneity. J Immunol 180:5707–5719
Schwartzman M, Reginensi A, Wong JS, Basgen JM, Meliambro K et al (2016) Podocyte-specific deletion of yes-associated protein causes FSGS and progressive renal failure. J Am Soc Nephrol 27:216–226
Shanmugam N, Figarola JL, Li Y, Swiderski PM, Rahbar S, Natarajan R (2008) Proinflammatory effects of advanced lipoxidation end products in monocytes. Diabetes 57:879–888
Shao DD, Suresh R, Vakil V, Gomer RH, Pilling D (2008) Pivotal Advance: Th-1 cytokines inhibit, and Th-2 cytokines promote fibrocyte differentiation. J Leukoc Biol 83:1323–1333
Sharma S, Sirin Y, Susztak K (2011) The story of Notch and chronic kidney disease. Curr Opin Nephrol Hypertens 20:56–61
Shi XY, Hou FF, Niu HX, Wang GB, Xie D (2008) Advanced oxidation protein products promote inflammation in diabetic kidney through activation of renal nicotinamide adenine dinucleotide phosphate oxidase. Endocrinology 149:1829–1839
Shih NY, Li J, Karpitskii V, Nguyen A, Dustin ML, Kanagawa O et al (1999) Congenital nephrotic syndrome in mice lacking CD2-associated protein. Science 286:312–315
Sica A, Mantovani A (2012) Macrophage plasticity and polarization: in vivo veritas. J Clin Invest 122:787–795
Siddiqi FS, Advani A (2013) Endothelial-podocyte crosstalk: the missing link between endothelial dysfunction and albuminuria in diabetes. Diabetes 62:3647–3655
Strutz F, Zeisberg M (2006) Renal fibroblasts and myofibroblasts in chronic kidney disease. J Am Soc Nephrol 17:2992–2998
Summers SA, Gan PY, Dewage L, Ma FT, Ooi JD et al (2012) Mast cell activation and degranulation promotes renal fibrosis in experimental unilateral ureteric obstruction. Kidney Int 82:676–685
Tang WW, Ulich TR, Lacey DL, Hill DC, Qi M et al (1996) Platelet-derived growth factor-BB induces renal tubulointerstitial myofibroblast formation and tubulointerstitial fibrosis. Am J Pathol 148:1169–1180
Taniguchi K, Xia L, Goldberg HJ, Lee KW, Shah A et al (2013) Inhibition of Src kinase blocks high glucose-induced EGFR transactivation and collagen synthesis in mesangial cells and prevents diabetic nephropathy in mice. Diabetes 62:3874–3886
Tapmeier TT, Fearn A, Brown K, Chowdhury P, Sacks SH et al (2010) Pivotal role of CD4+ T cells in renal fibrosis following ureteric obstruction. Kidney Int 78:351–362
Tipping PG, Holdsworth SR (2006) T cells in crescentic glomerulonephritis. J Am Soc Nephrol 17:1253–1263
Turner JE, Paust HJ, Steinmetz OM, Panzer U (2010) The Th17 immune response in renal inflammation. Kidney Int 77:1070–1075
Ueno T, Kobayashi N, Nakayama M, Takashima Y, Ohse T et al (2013) Aberrant Notch1-dependent effects on glomerular parietal epithelial cells promotes collapsing focal segmental glomerulosclerosis with progressive podocyte loss. Kidney Int 83:1065–1075
van Roeyen CR, Eitner F, Boor P, Moeller MJ, Raffetseder U et al (2011) Induction of progressive glomerulonephritis by podocyte-specific overexpression of platelet-derived growth factor-D. Kidney Int 80:1292–1305
Venkatachalam MA, Griffin KA, Lan R, Geng H, Saikumar P, Bidani AK (2010) Acute kidney injury: a springboard for progression in chronic kidney disease. Am J Physiol Renal Physiol 298:F1078–F1094
Vernon MA, Mylonas KJ, Hughes J (2010) Macrophages and renal fibrosis. Semin Nephrol 30:302–317
Veron D, Reidy KJ, Bertuccio C, Teichman J, Villegas G et al (2010) Overexpression of VEGF-A in podocytes of adult mice causes glomerular disease. Kidney Int 77:989–999
Veron D, Bertuccio CA, Marlier A, Reidy K, Garcia AM et al (2011) Podocyte vascular endothelial growth factor (Vegf(1)(6)(4)) overexpression causes severe nodular glomerulosclerosis in a mouse model of type 1 diabetes. Diabetologia 54:1227–1241
Wada T, Sakai N, Matsushima K, Kaneko S (2007) Fibrocytes: a new insight into kidney fibrosis. Kidney Int 72:269–273
Wang YM, Zhang GY, Wang Y, Hu M, Wu H et al (2006) Foxp3-transduced polyclonal regulatory T cells protect against chronic renal injury from adriamycin. J Am Soc Nephrol 17:697–706
Wang Y, Wang YP, Zheng G, Lee VW, Ouyang L et al (2007) Ex vivo programmed macrophages ameliorate experimental chronic inflammatory renal disease. Kidney Int 72:290–299
Wang Y, Deb DK, Zhang Z, Sun T, Liu W et al (2012) Vitamin D receptor signaling in podocytes protects against diabetic nephropathy. J Am Soc Nephrol 23:1977–1986
Wang H, Wang J, Bai Y, Li J, Li L, Dong Y (2016a) CD11c(+) CD8(+) T Cells Reduce Renal Fibrosis Following Ureteric Obstruction by Inducing Fibroblast Apoptosis. Int J Mol Sci 18
Wang S, Meng XM, Ng YY, Ma FY, Zhou S et al (2016b) TGF-beta/Smad3 signalling regulates the transition of bone marrow-derived macrophages into myofibroblasts during tissue fibrosis. Oncotarget 7:8809–8822
Wang X, Yao B, Wang Y, Fan X, Wang S et al (2017a) Macrophage cyclooxygenase-2 protects against development of diabetic nephropathy. Diabetes 66:494–504
Wang YY, Jiang H, Pan J, Huang XR, Wang YC et al (2017b) Macrophage-to- myofibroblast transition contributes to interstitial fibrosis in chronic renal allograft injury. J Am Soc Nephrol 28:2053–2067
Wasse H, Naqvi N, Husain A (2012) Impact of mast cell chymase on renal disease progression. Curr Hypertens Rev 8:15–23
Wilkinson L, Gilbert T, Sipos A, Toma I, Pennisi DJ et al (2009) Loss of renal microvascular integrity in postnatal Crim1 hypomorphic transgenic mice. Kidney Int 76:1161–1171
Wynes MW, Frankel SK, Riches DW (2004) IL-4-induced macrophage-derived IGF-I protects myofibroblasts from apoptosis following growth factor withdrawal. J Leukoc Biol 76:1019–1027
Xavier S, Vasko R, Matsumoto K, Zullo JA, Chen R et al (2015) Curtailing endothelial TGF-beta signaling is sufficient to reduce endothelial-mesenchymal transition and fibrosis in CKD. J Am Soc Nephrol 26:817–829
Yamaguchi Y, Iwano M, Suzuki D, Nakatani K, Kimura K et al (2009) Epithelial-mesenchymal transition as a potential explanation for podocyte depletion in diabetic nephropathy. Am J Kidney Dis 54:653–664
Yang N, Isbel NM, Nikolic-Paterson DJ, Li Y, Ye R et al (1998a) Local macrophage proliferation in human glomerulonephritis. Kidney Int 54:143–151
Yang N, Wu LL, Nikolic-Paterson DJ, Ng YY, Yang WC et al (1998b) Local macrophage and myofibroblast proliferation in progressive renal injury in the rat remnant kidney. Nephrol Dial Transplant 13:1967–1974
Yang J, Dai C, Liu Y (2002) Hepatocyte growth factor gene therapy and angiotensin II blockade synergistically attenuate renal interstitial fibrosis in mice. J Am Soc Nephrol 13:2464–2477
Yang L, Besschetnova TY, Brooks CR, Shah JV, Bonventre JV (2010) Epithelial cell cycle arrest in G2/M mediates kidney fibrosis after injury. Nat Med 16:535–543, 531p following 143
Yokoi H, Mukoyama M, Mori K, Kasahara M, Suganami T et al (2008) Overexpression of connective tissue growth factor in podocytes worsens diabetic nephropathy in mice. Kidney Int 73:446–455
You H, Gao T, Cooper TK, Brian Reeves W, Awad AS (2013) Macrophages directly mediate diabetic renal injury. Am J Physiol Renal Physiol 305:F1719–F1727
You H, Gao T, Raup-Konsavage WM, Cooper TK, Bronson SK et al (2017) Podocyte-specific chemokine (C-C motif) receptor 2 overexpression mediates diabetic renal injury in mice. Kidney Int 91:671–682
Zeisberg M, Neilson EG (2010) Mechanisms of tubulointerstitial fibrosis. J Am Soc Nephrol 21:1819–1834
Zeisberg EM, Potenta SE, Sugimoto H, Zeisberg M, Kalluri R (2008) Fibroblasts in kidney fibrosis emerge via endothelial-to-mesenchymal transition. J Am Soc Nephrol 19:2282–2287
Zeng F, Kloepfer LA, Finney C, Diedrich A, Harris RC (2016) Specific endothelial heparin-binding EGF-like growth factor deletion ameliorates renal injury induced by chronic angiotensin II infusion. Am J Physiol Renal Physiol 311:F695–F707
Zhang B, Ramesh G, Uematsu S, Akira S, Reeves WB (2008) TLR4 signaling mediates inflammation and tissue injury in nephrotoxicity. J Am Soc Nephrol 19:923–932
Zhang F, Tsai S, Kato K, Yamanouchi D, Wang C et al (2009) Transforming growth factor-beta promotes recruitment of bone marrow cells and bone marrow-derived mesenchymal stem cells through stimulation of MCP-1 production in vascular smooth muscle cells. J Biol Chem 284:17564–17574
Zheng G, Wang Y, Mahajan D, Qin X, Alexander SI, Harris DC (2005) The role of tubulointerstitial inflammation. Kidney Int Suppl S96–S100
Zhou LL, Hou FF, Wang GB, Yang F, Xie D, Wang YP, Tian JW (2009) Accumulation of advanced oxidation protein products induces podocyte apoptosis and deletion through NADPH-dependent mechanisms. Kidney Int 76:1148–1160
Acknowledgements
This laboratory is supported by grants from National Natural Science Foundation of China (National Science Foundation of China 81300580 and 81570623) and by Science and Technological Fund of Anhui Province for Outstanding Youth of China (Grant number: 1608085J07).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Meng, XM. (2019). Inflammatory Mediators and Renal Fibrosis. In: Liu, BC., Lan, HY., Lv, LL. (eds) Renal Fibrosis: Mechanisms and Therapies. Advances in Experimental Medicine and Biology, vol 1165. Springer, Singapore. https://doi.org/10.1007/978-981-13-8871-2_18
Download citation
DOI: https://doi.org/10.1007/978-981-13-8871-2_18
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-8870-5
Online ISBN: 978-981-13-8871-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)