Abstract
Although liver cirrhosis is most commonly caused by hepatitis B and C viruses, alcohol, and nonalcoholic fatty liver disease, hereditary hemochromatosis also causes cirrhosis as one of the hereditary liver diseases. Hereditary hemochromatosis is characterized by iron deposition not only in the liver but also in heart and endocrine organs. Therefore, hereditary hemochromatosis potentially progresses to liver cirrhosis, diabetes mellitus, heart failure, and/or hypogonadism without early diagnosis and prompt initiation of treatment. On the other hand, the identification of important iron metabolic molecules and genes such as hepcidin, ferroportin, and HFE has made it possible to understand the molecular mechanisms underlying hereditary hemochromatosis and to introduce proper treatment at the early stage of disease. This chapter will review and discuss the iron metabolic regulation and the molecular and clinical characteristics of hereditary hemochromatosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Introduction
Essential trace elements such as iron, copper, and zinc are biologically indispensable for mitochondrial electron transport, signal transduction, redox reaction, oxygen transport, and/or physiological catalytic reaction such as hydrolysis. Because these elements are transition metal, they also function as active region of various enzymes, cytokines, and hormones. Thus, metabolic disturbance of these elements results in critical disorder of biological functions, leading to the development of various diseases.
On the other hand, liver is a crucial organ for metabolism of iron. Therefore, primary metabolic disorders of iron give rise to liver diseases such as liver cirrhosis and hepatocellular carcinoma (HCC) in addition to iron deposition in vital organs such as heart and endocrine organs. This chapter will review and discuss (1) iron absorption, (2) hepatocellular iron transport, (3) regulation of iron homeostasis, and (4) hereditary hemochromatosis as primary iron metabolic disorder.
4.2 Iron Absorption
Iron can be absorbed from the diet in two forms in the proximal intestine: as inorganic (nonheme) iron predominantly released from foods such as vegetables or cereals, or as heme iron from the breakdown of hemoglobin and myoglobin contained in red meat [1]. Heme (ferrous protoporphyrin IX) is more efficiently absorbed than inorganic iron from the diet. The mechanism responsible for heme uptake is not yet well understood, but it is known to occur by receptor-mediated endocytosis. The hem-carrier protein 1 (HCP1) has been identified as the most probable receptor involved in this process [2]. However, it has low-affinity to heme and is more involved in folate absorption [3]. Once in the enterocyte, heme is broken by heme oxygenase 1 (HO1) and iron is released in its ferric state.
Nonheme-iron exists primarily in the bio-unavailable, oxidized form (Fe3+), which must first be reduced to Fe2+ for transport across the intestinal epithelium. At the apical membrane, there is a cytochrome b-like ferrireductase (Dcytb) [4]. Fe2+ then enters the cell through divalent metal transporter 1 (Dmt1), an iron transporter. Dmt1 is responsible for the absorption of the ionic forms of iron, cobalt, zinc, cadmium, and others, and takes advantage of the proton gradient existing between the gut lumen and the enterocyte cytoplasm to perform the transport of Fe2+ coupled with H+ [5].
In the cytoplasm iron is transferred to the basolateral membrane of the enterocyte or stored in ferritin, a multi-subunit protein shell that can accommodate up to 4500 atoms of iron. The export of iron from the enterocyte to the circulation is a critical step for the entrance of iron in the body. The mammalian iron transporter, ferroportin-1, exists on the basolateral membrane of the enterocytes [6]. Ferroportin-1 transports Fe2+ to the extracellular side of the basolateral membrane, where Fe2+ is oxidized by the ferroxidase, hephaestin, and ceruloplasmin in order to be associated with the circulatory transferrin [7, 8].
4.3 Hepatocellular Iron Transport
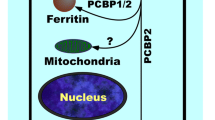
Hepatocytes take up iron through at least two distinct pathways. They have a functional transferrin cycle and a transport system to take up non-transferrin-bound iron. The cellular uptake of transferrin-bound iron is mainly mediated by the transferrin receptor 1 (TfR1). The molecules important for non-transferrin-bound iron transport have not yet been identified. Hepatocytes store iron in ferritin. When iron is needed elsewhere in the body, they can release it to transferrin through autophagy-dependent mechanism (ferritinophagy) [9, 10]. This mechanism is described in detail later. The mechanism of hepatocyte export is not well known, but it may involve ferroportin-1. Ceruloplasmin seems to aid in iron export from hepatocytes, but its precise function has not yet been defined.
4.4 Regulation of Iron Homeostasis
Systemic iron homeostasis, the control of iron balance throughout the body, requires controlled absorption, recycling, and storage, because there is no efficient pathway for iron excretion in the human body. All the stages required for keeping iron homeostasis are strictly regulated at both systemic and cellular levels.
4.4.1 Hepcidin
The major systemic regulator of iron homeostasis is hepcidin, which is a 25 amino-acid peptide hormone exclusively synthesized in the liver and a soluble regulator that acts to attenuate both intestinal iron absorption and iron release from reticuloendothelial macrophages [11, 12]. Hepcidin acts by triggering internalization of ferroportin-1 and consequent degradation, and traps iron in absorptive enterocytes, macrophages, and hepatocytes [13]. Thus, coupling the internalization of ferroportin-1 to hepcidin levels generates a homeostatic loop regulating the iron plasma level and the tissue distribution of iron. Hepcidin is expressed from the human antimicrobial peptide (HAMP) gene located at the long arm of chromosome 19. The increase of iron levels and inflammation upregulate the transcription of HAMP gene, while reactive oxygen species (ROS), hypoxia, and anemia/erythropoiesis repress its expression [14,15,16,17,18].
Hemojuvelin (Hjv), HFE, TfR1, and TfR2 that are located at the surface of hepatocytes are considered to be “iron sensors.” The Hjv-hepcidin axis is the most important mechanism for the upregulation of HAMP expression during iron overload. Bone morphogenic protein (BMP) binding to the Hjv and BMP receptor complexes induces the phosphorylation of cytosolic sons of mothers against decapentaplegic (SMADs) 1, 5, and 8 [14, 19]. The phosphorylated SMADs form complexes with SMAD4, which are translocated to the nucleus where they bind to the BMP responsive elements present at HAMP promoter, inducing its transcription [20]. Proinflammatory cytokine interleukin 6 (IL-6) activates HAMP gene transcription through a pathway that involves Janus kinase (JAK)-signal transducer and activator of transcription (STAT) signaling and a binding site for the transcription factor STAT3 [17, 21]. The transcription factor CCAAT/enhancer-binding protein α (C/EBPα) is also clearly involved in regulating hepcidin transcription [22].
4.4.2 Iron Regulatory Protein (IRP)/Iron Responsive Element (IRE) System
Besides the systemic regulation of iron homeostasis by hepcidin, the IRP/IRE system controls both mRNA stability and translation of transcripts coding proteins involved in iron uptake (Dmt1 and TfR1), storage (ferritin), and export (ferroportin-1) [23, 24]. The IPP1 and IRP2 proteins are the main regulators of cellular iron in humans, but the IPR2 protein is assumed to play a central role in IRP/IRE system [25]. Under iron deficient conditions, IRP binds to the IRE present at the 5′ or 3′-untranslated regions (UTRs) of mRNAs that code for iron regulatory proteins. Under iron depleted condition in cells, IRPs bind to the IREs present at 5′-UTRs of FTH, FHL (genes coding heavy chain and light chain of ferritin), and SLC40A1 (gene coding ferroportin-1), preventing ribosome assembly and further translation [26, 27], while they bind to the IREs present at 3′-UTR of TfR1 and SLC11A2 (gene coding Dmt1), increasing the transcripts stability and subsequently their translation [28, 29]. Thus, cellular iron depletion downregulates iron storage and export, and upregulates iron uptake. Alternatively, cellular iron increase makes IRPs unable to bind to the IREs, resulting in suppression of iron acquisition. Cellular regulation other than IRP/IRE system for iron homeostasis will be discussed elsewhere.
4.4.3 Ferritinophagy
In mammalian cells, iron homeostasis is maintained by compensatory regulation of iron uptake and storage depending on the availability of iron. Ferritin is the major iron storage protein in mammals. Ferritin forms a three-dimensional protein shell consisting of 24 protein subunits that can store up to 4500 atoms of iron [30]. Two isoforms of ferritin, ferritin heavy chain (H chain) and light chain (L chain), cooperate in storing iron in the ferritin shell. The production of H and L chains is regulated by iron availability at the posttranscriptional level through IRP/IRE system as mentioned above. While the mechanism of iron-mediated regulation of ferritin expression has been well defined, comparatively little is known so far regarding the fate of the iron that is stored by ferritin. Ferritin is degraded via lysosomal in response to iron deficiency [31]. This process is mediated with autophagy [9]. Recently, nuclear receptor coactivator 4 (NCOA4) has been identified as the cargo receptor mediating autophagic turnover of ferritin (ferritinophagy) [10]. These results suggest that the targeting of ferritin to autophagosomes by NCOA4 is a general cellular mechanism for regulating bioavailable iron.
4.5 Inherited Iron Metabolic Disorder
Iron overload, especially excess divalent iron can be highly toxic, mainly via the Fenton reaction producing hydroxyl radicals [32]. This is particularly relevant for hereditary iron-overloaded liver diseases such as hemochromatosis, in which oxidative stress has been proposed as a major mechanism of liver injury. Oxidative stress and increased iron levels strongly favor DNA damage, genetic instability, and tumorgenesis. Indeed, a significant correlation between 8-hydroxy-2′-deoxyguanosine (8-OHdG), a marker of oxidatively generated DNA damage [33], and hepatic iron excess has been shown in iron-overloaded liver diseases.
4.5.1 Hereditary Hemochromatosis
Hereditary hemochromatosis is a heterogeneous group of inherited iron-overload conditions that is characterized by increased intestinal absorption and deposition in vital organs, including the liver, heart, and endocrine organs. The hemochromatosis group shows common features with respect to increased transferrin saturation and parenchymal iron deposition in organs, resulting in the development of liver cirrhosis, HCC, heart failure, diabetes mellitus (DM), and hypogonadism, even though the severity of the different forms of hemochromatosis varies. Hereditary hemochromatosis has been clinically classified into two phenotypes. The classical form induces mainly cirrhosis, DM, and/or skin pigmentation in middle-aged patients, while the other form, juvenile hemochromatosis, results in cardiac failure and hypogonadism before patients reach the age of 30 [34]. On the other hand, four types (type 1, 2, 3, and 4) of hemochromatosis have been genetically classified on the basis of mutation in five genes (HFE, HAMP, Hiv, TFR2, and SLC40A1). Responsible genes and dysregulated iron metabolism in hereditary hemochromatosis are summarized in Table 4.1. The molecular mechanism common to all types but type 4 hereditary hemochromatosis fails to regulate hepcidin expression in response to cellular iron levels [35]. Figure 4.1 depicts the molecular mechanisms underlying various types of hereditary hemochromatosis.
The impaired hepcidin–ferroportin system in genetic hereditary hemochromatosis. Hepcidin secreted by the liver regulates iron release from macrophages and duodenal enterocytes by interacting with the ferroportin expressed on their surface. Ferroportin transports Fe2+ to the extracellular side of the basolateral membrane. HFE, transferrin receptor 2 (TfR2), and hemojuvelin (HJV) are all required to adjust hepcidin expression to current iron needs. In hemochromatosis except for type 4, loss of any one of these hepcidin regulators diminishes intracellular hepcidin signal transduction and hepcidin secretion, leading to unrestricted flow of iron into the plasma iron pool. In type 4A hemochromatosis, loss of function mutants of ferroportin is unable to export iron from cells, resulting in iron accumulation predominantly in reticuloendothelial cells. In type 4B, ferroportin mutations are responsible for a gain of function with full iron export capability but insensitivity to downregulation by hepcidin, leading to iron accumulation in parenchymal cells and a phenotype similar to other hepcidin deficiency-based types of hemochromatosis
4.5.1.1 Type 1 Hereditary Hemochromatosis (Classical Form)
Type 1 hereditary hemochromatosis, known as classic hemochromatosis, is affected by HFE mutations and accounts for approximately 90% of all cases of hereditary hemochromatosis. It is characterized by mild disease progression with a gradual iron deposition in organs [36, 37]. HFE encodes an atypical histocompatibility class I protein that heterodimerizes with β-2 microglobulin [37]. Most affected patients are homozygous for a missense mutation (C282Y) that partially disrupts HFE function [37]. The C282Y mutation is known to be widespread in populations of Northern European descent [38], but its prevalence is extremely low in Asians [39]. Mutated HFE protein cannot bind to β-2 microglobulin and be transferred to the cell surface, which presumably results in failure to regulate hepcidin transcription, since HFE protein is considered to be one of “iron sensors” at the surface of hepatocytes.
4.5.1.2 Type 2 Hereditary Hemochromatosis (Juvenile Hemochromatosis)
Type 2 hereditary hemochromatosis, known as juvenile hemochromatosis, is an autosomal recessive disease and affected by Hjv or HAMP mutations. This type of hemochromatosis is a rare but more progressive disease which includes hypogonadism, diabetes, and cardiomyopathy. Severe iron overload and organ damages usually occur before patients reach the age of 30. Juvenile hemochromatosis is further classified into two types: (A) Hjv-associated hemochromatosis [40], and (B) HAMP-associated hemochromatosis [41]. Hjv protein is also one of the “iron sensors” at the surface of hepatocytes.
4.5.1.3 Type 3 Hereditary Hemochromatosis
Camaschella et al. reported six patients who met the diagnostic criteria for hereditary hemochromatosis but were not linked to HFE from two families of Sicilian origin, and identified homozygous Y250X mutation in TRF2 in these patients [42]. This type of hemochromatosis affects middle-aged adults but also adolescents and young adults and resembles type 1 hemochromatosis. The Y245X mutation of this gene in mice, equivalent to Y250X in humans, causes downregulation of hepcidin expression and iron accumulation in the liver [43]. In type 1, 2, and 3 hereditary hemochromatosis, serum hepcidin level is inappropriately low despite iron overload, and the diseases are inherited in the autosomal recessive pattern.
4.5.1.4 Type 4 Hereditary Hemochromatosis
Type 4 hemochromatosis, which is affected by SLC40A1 mutations, is also known as ferroportin disease, and is less rare than type II or III [36]. The inheritance pattern is autosomal dominant. This disease is phenotypically heterogeneous with two forms (A and B). In form A, the loss of function mutants of ferroportin are unable to export iron from cells, resulting in iron accumulation predominantly in reticuloendothelial cells and decreased availability of iron for transferrin [36]. In form B, ferroportin mutations are responsible for a gain of function with full iron export capability but insensitivity to downregulation by hepcidin, leading to iron accumulation in parenchymal cells and a phenotype similar to other hepcidin deficiency-based types of hemochromatosis [36, 44]. Thus, ferroportin disease form B shows elevated transferrin saturation-associated tissue iron accumulation, preferentially within hepatocytes.
4.5.1.5 Other Type of Hereditary Hemochromatosis
Mutations in BMP6 gene have recently been reported in several families [45, 46]. It has been reported that serum hepcidin levels of patients with heterozygous mutations of this gene were markedly low or inappropriately low for the iron overload. Also, a heterozygous mutation in the IRE in the 5′-UTR of FTH gene has been demonstrated in patients with systemic iron overload [47]. The proband had iron deposition in hepatocytes and Kupffer cells/macrophages in the liver and spleen.
4.5.2 Management of Hereditary Hemochromatosis
Early diagnosis and prompt initiation of iron depletion therapy are essential for preventing irreversible organ damage. Although the penetrance of HFE C282Y is low among the general population except for northern European population, it is important to consider biochemical screening for hemochromatosis (followed by genetic testing when indicated) when we see the patients with iron overload. Phlebotomy is the standard treatment for hereditary hemochromatosis, but there are no evidence-based guidelines on the use of therapeutic phlebotomy. It should be repeated at appropriate intervals for at least 1 week [48]. Treatment is conventionally initiated when serum ferritin levels exceed the normal range [36]. The standard volume of phlebotomy is 400–500 mL which contains approximately 200–250 mg of iron, and it should be modified according to the patient’s age, body weight, hemoglobin level, and comorbidities [48]. Maintenance therapy is performed to keep serum ferritin levels 50 to 100 ng/mL, but iron deficiency with lower serum ferritin levels should be avoided. In patients with both iron overload and anemia, phlebotomy is inappropriate. In such cases, iron chelation therapy using desferrioxamine, deferasirox, or deferiprone may be considered [48].
Although glucose tolerance, cardiac function, and gonadal function should be monitored in patients with hereditary hemochromatosis, we also should bear in mind that HCC is at least twice as frequent among patients with hereditary hemochromatosis compared with those who have other types of liver diseases because hepatic iron overload strongly favors DNA damage, genetic instability, and tumorgenesis through enhanced oxidative stress.
4.6 Conclusion
Because of the identification of important iron metabolic molecules and genes such as hepcidin, ferroportin, and HFE, our understanding of systemic iron regulation and the mechanisms of iron overload-related diseases has largely progressed in the past two decades. As liver is a crucial organ for iron metabolism, liver is likely to be involved in iron overload-related disorder. Hereditary hemochromatosis is one of the inherited liver diseases and occasionally diagnosed after the development of liver cirrhosis and/or HCC. Liver cirrhosis significantly reduces survival in concert with disorders in vital organs due to the parenchymal iron deposition. Therefore, early diagnosis and prompt initiation of iron depletion therapy are essential for improving the prognosis of patients with hereditary hemochromatosis. Recognition of this disease is critical for hepatologists, hematologists, cardiologists, endocrinologists, and family physicians because inadequate management is fatal for patients with hereditary hemochromatosis.
References
Silva B, Faustino R. An overview of molecular basis of iron metabolism regulation and the associated pathologies. Biochim Biophys Acta. 2015;1852:1347–59.
Shayeghi M, Latunde-Dada GO, Oakhill JS, Laftah AH, Takeuchi K, Halliday N, et al. Identification of an intestinal heme transporter. Cell. 2005;122:789–801.
Laftah AH, Latunde-Dada GO, Fakih S, Hider RC, Simpson RJ, McKie AT. Haem and folate transport by proton-coupled folate transporter/haem carrier protein 1 (SLC46A1). Br J Nutr. 2009;101:1150–6.
McKie AT, Barrow D, Latunde-Dada GO, Rolfs A, Sager G, Mudaly E, et al. An iron-regulated ferric reductase associated with the absorption of dietary iron. Science. 2001;291:1755–9.
Gunshin H, Mackenzie B, Berger UV, Gunshin Y, Romero MF, Boron WF, et al. Cloning and characterization of a mammalian proton-coupled metal-ion transporter. Nature. 1997;388:482–8.
Donovan A, Brownlie A, Zhou Y, Shepard J, Pratt SJ, Moynihan J, et al. Positional cloning of zebrafish ferroportin1 identifies a conserved vertebrate iron exporter. Nature. 2000;403:776–81.
Yeh KY, Yeh M, Mims L, Glass J. Iron feeding induces ferroportin 1 and hephaestin migration and interaction in rat duodenal epithelium. Am J Physiol Gastrointest Liver Physiol. 2009;296:G55–65.
Brittin GM, Chee QT. Relation of ferroxidase (ceruloplasmin) to iron absorption. J Lab Clin Med. 1969;74:53–9.
Asano T, Komatsu M, Yamaguchi-Iwai Y, Ishikawa F, Mizushima N, Iwai K. Distinct mechanisms of ferritin delivery to lysosomes in iron-depleted and iron-replete cells. Mol Cell Biol. 2011;31:2040–52.
Mancias JD, Wang X, Gygi SP, Harper JW, Kimmelman AC. Quantitative proteomics identifies NCOA4 as the cargo receptor mediating ferritinophagy. Nature. 2014;509:105–9.
Park CH, Valore EV, Waring AJ, Ganz T. Hepcidin, a urinary antimicrobial peptide synthesized in the liver. J Biol Chem. 2001;276:7806–10.
Ganz T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood. 2003;102:783–8.
Nemeth E, Tuttle MS, Powelson J, Vaughn MB, Donovan A, Ward DM, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306:2090–3.
Zhang AS, Gao J, Koeberl DD, Enns CA. The role of hepatocyte hemojuvelin in the regulation of bone morphogenic protein-6 and hepcidin expression in vivo. J Biol Chem. 2010;285:16416–23.
Schmidt PJ, Toran PT, Giannetti AM, Bjorkman PJ, Andrews NC. The transferrin receptor modulates Hfe-dependent regulation of hepcidin expression. Cell Metab. 2008;7:205–14.
Gao J, Chen J, Kramer M, Tsukamoto H, Zhang AS, Enns CA. Interaction of the hereditary hemochromatosis protein HFE with transferrin receptor 2 is required for transferrin-induced hepcidin expression. Cell Metab. 2009;9:217–27.
Pietrangelo A, Dierssen U, Valli L, Garuti C, Rump A, Corradini E, et al. STAT3 is required for IL-6-gp130-dependent activation of hepcidin in vivo. Gastroenterology. 2007;132:294–300.
Harrison-Findik DD, Schafer D, Klein E, Timchenko NA, Kulaksiz H, Clemens D, et al. Alcohol metabolism-mediated oxidative stress down-regulates hepcidin transcription and leads to increased duodenal iron transporter expression. J Biol Chem. 2006;281:22974–82.
Babitt JL, Huang FW, Wrighting DM, Xia Y, Sidis Y, Samad TA, et al. Bone morphogenetic protein signaling by hemojuvelin regulates hepcidin expression. Nat Genet. 2006;38:531–9.
Truksa J, Lee P, Beutler E. Two BMP responsive elements, STAT, and bZIP/HNF4/COUP motifs of the hepcidin promoter are critical for BMP, SMAD1, and HJV responsiveness. Blood. 2009;113:688–95.
Wrighting DM, Andrews NC. Interleukin-6 induces hepcidin expression through STAT3. Blood. 2006;108:3204–9.
Courselaud B, Pigeon C, Inoue Y, Inoue J, Gonzalez FJ, Leroyer P, et al. C/EBPalpha regulates hepatic transcription of hepcidin, an antimicrobial peptide and regulator of iron metabolism. Cross-talk between C/EBP pathway and iron metabolism. J Biol Chem. 2002;277:41163–70.
Anderson CP, Shen M, Eisenstein RS, Leibold EA. Mammalian iron metabolism and its control by iron regulatory proteins. Biochim Biophys Acta. 2012;1823:1468–83.
Hentze MW, Muckenthaler MU, Andrews NC. Balancing acts: molecular control of mammalian iron metabolism. Cell. 2004;117:285–97.
Meyron-Holtz EG, Ghosh MC, Iwai K, LaVaute T, Brazzolotto X, Berger UV, et al. Genetic ablations of iron regulatory proteins 1 and 2 reveal why iron regulatory protein 2 dominates iron homeostasis. EMBO J. 2004;23:386–95.
Sammarco MC, Ditch S, Banerjee A, Grabczyk E. Ferritin L and H subunits are differentially regulated on a post-transcriptional level. J Biol Chem. 2008;283:4578–87.
Lymboussaki A, Pignatti E, Montosi G, Garuti C, Haile DJ, Pietrangelo A. The role of the iron responsive element in the control of ferroportin1/IREG1/MTP1 gene expression. J Hepatol. 2003;39:710–5.
Casey JL, Koeller DM, Ramin VC, Klausner RD, Harford JB. Iron regulation of transferrin receptor mRNA levels requires iron-responsive elements and a rapid turnover determinant in the 3′ untranslated region of the mRNA. EMBO J. 1989;8:3693–9.
Gunshin H, Allerson CR, Polycarpou-Schwarz M, Rofts A, Rogers JT, Kishi F, et al. Iron-dependent regulation of the divalent metal ion transporter. FEBS Lett. 2001;509:309–16.
Harrison PM, Arosio P. Ferritins: molecular properties, iron storage function and cellular regulation. Biochim Biophys Acta. 1996;1275:161–203.
Kidane TZ, Sauble E, Linder MC. Release of iron from ferritin requires lysosomal activity. Am J Physiol Cell Physiol. 2006;291:C445–55.
Fenton HJH. Oxidation of tartaric acid in presence of iron. J Chem Soc. 1894;65:899–910.
Shibutani S, Takeshita M, Grollman AP. Insertion of specific bases during DNA synthesis past the oxidation-damaged base 8-oxodG. Nature. 1991;349:431–4.
Hattori A, Miyajima H, Tomosugi N, Tatsumi Y, Hayashi H, Wakusawa S. Clinicopathological study of Japanese patients with genetic iron overload syndromes. Pathol Int. 2012;62:612–8.
Hino K, Harada M. Metal metabolism and liver. In: Ohira H, editor. The liver in systemic diseases. Cham: Springer; 2016. p. 123–46.
Pietrangelo A. Hereditary hemochromatosis: pathogenesis, diagnosis, and treatment. Gastroenterology. 2010;139:393–408.
Feder JN, Gnirke A, Thomas W, Tsuchihashi Z, Ruddy DA, Basava A, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996;13:399–408.
Merryweather-Clarke AT, Pointon JJ, Shearman JD, Robson KJ. Global prevalence of putative hemochromatosis mutations. J Med Genet. 1997;34:275–8.
Distante S, Robson KJ, Graham-Campbell J, Arnaiz-Villena A, Brissot P, Worwood M. The origin and spread of the HFE-C282Y haemochromatosis mutation. Hum Genet. 2004;115:269–79.
Papanikolaou G, Samuels ME, Ludwig EH, MacDonald ML, Franchini PL, Dube MP, et al. Mutations in HFE2 cause iron overload in chromosome 1q-linked juvenile hemochromatosis. Nat Genet. 2004;36:77–82.
Roetto A, Papanikolaou G, Politou M, Alberti F, Girelli D, Christakis J, et al. Mutant antimicrobial peptide hepcidin is associated with severe juvenile hemochromatosis. Nat Genet. 2003;33:21–2.
Camaschella C, Roetto A, Cali A, De Gobbi M, Garozzo G, Carella M, et al. The gene TFR2 is mutated in a new type of haemochromatosis mapping to 7q22. Nat Genet. 2000;25:14–5.
Kawabata H, Fkeming RE, Gui D, Moon SY, Saitoh T, O’Kelly J, et al. Expression of hepcidin is down-regulated in TfR2 mutant mice manifesting a phenotype of hereditary hemochromatosis. Blood. 2005;105:376–81.
Sham RL, Phatak PD, West C, Lee P, Andrews C, Beutler E. Autosomal dominant hereditary hemochromatosis associated with a novel ferroportin mutation and unique clinical features. Blood Cells Mol Dis. 2005;34:157–61.
Piubelli C, Castagna A, Marchi G, Rizzi M, Busti F, Bardar S, et al. Identification of new BMP6 pro-peptide mutations in patients with iron overload. Am J Hematol. 2017;92:562–8.
Daher R, Kannengiesser C, Houamel D, Lefebvre T, Bardou-Jacquet E, Ducrot H, et al. Heterozygous mutations in BMP6 pro-peptide lead to inappropriate hepcidin synthesis and moderate iron overload in humans. Gastroenterology. 2016;150(672-83):e4.
Kato J, Fujiwara K, Kanda M, Fukuda N, Sasaki K, Takayama T, et al. A mutation, in the iron-responsive element of H ferritin mRNA, causing autosomal dominant iron overload. Am J Hum Genet. 2001;69:191–7.
Kawabata H. The mechanisms of systemic iron homeostasis and etiology. Diagnosis, and treatment of hereditary hemochromatosis. Int J Hematol. 2018;107:31–43.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Hino, K., Nishina, S. (2019). Liver Cirrhosis with Inherited Liver Disease: Hemochromatosis. In: Yoshiji, H., Kaji, K. (eds) The Evolving Landscape of Liver Cirrhosis Management. Springer, Singapore. https://doi.org/10.1007/978-981-13-7979-6_4
Download citation
DOI: https://doi.org/10.1007/978-981-13-7979-6_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-7663-4
Online ISBN: 978-981-13-7979-6
eBook Packages: MedicineMedicine (R0)