Abstract
Magnetic resonance imaging (MRI) has been widely used in intracerebral hemorrhage (ICH) animal models and patients. In the current study, we examined whether MRI can predict at-risk brain tissue during the acute phase and long-term brain tissue loss after ICH. Male Sprague–Dawley rats had an intracaudate injection of autologous whole blood (10, 50 or 100 μL). MRI (T2 and T2*) sequences were performed at days 1, 3, 7, 14, and 28. The volume of brain tissue at risk was calculated as the difference between T2 and T2* lesion volumes. Dopamine- and cAMP-regulated phosphoprotein, Mr 32 kDa (DARPP-32) was used as a neuronal marker in the basal ganglia. Brain swelling at day 3 and brain tissue loss at day 28 after ICH were also measured. We found that the difference in lesion volumes between T2 and T2* measured by MRI coincided well with the difference between the volume of the DARPP-32-negative area and that of the hematoma measured in brain sections. Volumes of brain tissue at risk at day 3 correlated with the brain swelling at day 3 (p < 0.01) as well as the final brain tissue loss at day 28 (n = 9, p < 0.05). The results suggest that the difference between T2 lesions and T2* lesions could be an indicator of at-risk brain tissue and it could be used as a predictor of neuronal loss in ICH patients.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
Intracerebral hemorrhage (ICH) accounts for 10–15 % of all strokes and is associated with higher mortality and more severe neurological deficits than other stroke subtypes [3, 13]. Perihematomal brain edema develops immediately after ICH and peaks several days later [12]. There is a close temporal relationship between brain edema and neurological deficits [6]. Brain atrophy was found in a rat ICH model [4].
Magnetic resonance imaging (MRI) is an ideal method for characterizing the temporal and spatial evolution of parenchymal alterations following ICH with high sensitivity [1]. T2* gradient-echo imaging has been used in ICH models and patients to evaluate the hematoma size and iron deposition [2, 10]. We hypothesized that a simple MRI examination at an early stage could provide more precise information for predicting brain atrophy. DARPP-32 is a specific marker of GABAergic neurons and is only expressed in the neuronal cell bodies and dendrites in the striatum [9, 15]. The fluorescence-negative area of DARPP-32 can be used as an indicator of damaged brain tissue.
This study examined whether or not early T2- and T2*-weighted MRI imaging can predict at-risk brain tissue during the acute phase and brain tissue loss during the late phase in ICH rats.
Materials and Methods
Animal Preparation and Intracerebral Infusion
Animal use protocols were approved by the University of Michigan Committee on the Use and Care of Animals. A total 39 male Sprague–Dawley rats (Charles River Laboratories, Portage, MI, USA), weighing 250–350 g, were used in this study. Rats were anesthetized with pentobarbital (50 mg/kg, i.p.). The right femoral artery was catheterized for continuous blood pressure monitoring and blood sampling. Blood was obtained from the catheter for analysis of blood pH, PaO2, PaCO2, hematocrit, and blood glucose. Core temperature was maintained at 37 °C. Rats were positioned in a stereotactic frame (Kopf Instruments), and a cranial burr hole (1 mm) was drilled on the right coronal suture 3.5 mm lateral to the midline. A 26-gauge needle was inserted stereotactically into the right basal ganglia (0.2 mm anterior, 5.5 mm ventral, 3.5 mm lateral to the bregma). Autologous whole blood at a volume of 10 μL (n = 4), 50 μL (n = 5), and 100 μL (n = 30) was injected using a microinfusion pump [11]. The rats that had 100 μL of blood injected were euthanized at days 1, 3, 7, 14, and 28 (n = 6 each time point) and the others were euthanized at day 28 after ICH.
Magnetic Resonance Imaging
Serial MRI, T2-weighted, and T2* gradient-echo imaging (GRE) were performed with a 7.0 T 183 cm Horizontal Bore (Unity Inova, Varian Inc.) imaging spectrometer at days 1, 3, 7, 14, and 28 after ICH. Fifteen 0.5-mm-thick slices were scanned (FOV = 35 × 35mm2, matrix = 256 × 256, slice gap = 0, flip angle = 25, TR/TE = 4,000 ms/60 ms and 200 ms/5 ms for T2 and T2* imaging respectively). Images were analyzed using NIH Image J. The entire lesion volume was measured on the T2-weighted images and the hematoma volume was measured on the T2*-weighted images. The measurements were as follows:
-
1.
At-risk brain tissue: lesion areas on T2 and T2* weighted images were combined separately and multiplied by section thickness (0.5 mm). At-risk brain tissue volume was obtained by the difference between T2 and T2* lesion volume [8].
-
2.
Brain tissue loss volume: bilateral hemispheres were outlined separately and the areas were measured excluding bilateral ventricle areas on T2-weighted images at day 28 after ICH. Bilateral brain tissue volume was obtained by combining the outlined areas over all slices. Brain tissue loss volume was obtained by the difference in volume between the contralateral and the ipsilateral hemisphere.
-
3.
Brain swelling volume: bilateral hemispheres excluding bilateral ventricles were outlined and measured on T2-weighted images on day 3 after ICH. Brain swelling volume was acquired using the difference in volume between the ipsilateral and the contralateral hemisphere.
Immunofluorescent Staining
Immunofluorescent staining was performed as described previously [14]. The primary antibody was anti-dopamine-and cAMP-regulated phosphoprotein of 32-kDa (DARPP-32) antibody (Cell Signaling Technology, 1:800 dilution). Alexa Fluro 488-conjugated donkey anti-rabbit antibodies (Invitrogen, 1:500 dilution) were used as the secondary antibody.
Results
DARPP-32, a specific marker of GABAergic neurons in basal ganglia [15] was expressed in the neuronal cell bodies and dendrites. At-risk brain tissue area was obtained by two measurements: the difference between the DARPP-32 negative area (Fig. 1a) and the hematoma area (H&E, Fig. 1b), and the difference between T2 (Fig. 1c) and T2* (Fig. 1d) lesions. On day 1 and day 3 after ICH, the difference between T2 and T2* lesion areas on the MRI images was 5.5 ± 1.9 mm2 on day 1 and 6.7 ± 0.7 mm2 on day 3 after a 100-μL blood injection. These correlated well with the difference between the DARPP-32-negative area and the hematoma area (4.6 ± 1.0 mm2 on day 1, and 6.0 ± 0.8 mm2 on day 3) measured in the brain sections with DARPP-32 immunofluorescent staining. The results indicate that at-risk brain tissue areas measured by MRI reflect the histological measurements (Fig. 1e).
(a) DARPP-32-negative area showing acute neuronal death in the basal ganglia. (b) Hematoxylin and eosin stain showing hematoma size. Scale bar = 2 mm; (c, d) T2 and T2* MR images on day 3 after intracerebral hemorrhage (ICH). (e) At-risk brain tissue volumes 1 and 3 days after ICH were determined by the difference between the DARPP-32-negative area and clot size and that between T2 lesions and T2* lesions
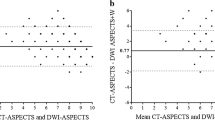
The volume of brain swelling measured on MR images on day 3 (39.7 ± 10.7 mm3) after rats had a 100-μL blood injection was significantly increased compared with other time points (20.4 ± 7.9 mm3 on day 1 and 8.4 ± 3.3 mm3 on day 7, p < 0.01). Volumes of at-risk brain tissue calculated as (T2–T2*) lesion volumes were significantly higher on day 3 (42.5 ± 8.2 mm3) after ICH compared with other time points (26.9 ± 4.9 mm3 at day 1 and 6.6 ± 2.8 mm3 at day 7, p < 0.01). Brain swelling volumes on day 3 in rats that had different volumes (10, 50, and 100 μL) of blood injection coincided well with the volume of at risk tissue (n = 15, r = 0.857, p < 0.01, Fig. 2a). Volume of at-risk brain on day 3 after a 10- or 50-μL blood injection also correlated with the final brain tissue loss measured on day 28 (n = 9, r = 0.678, p < 0.05, Fig. 2b). At-risk brain tissue volume measured on MRI images on day 3 could be a desired indicator for predicting long-term brain atrophy (Fig. 3).
At-risk tissue volumes correlated well with brain swelling volumes on day 3 (a) and with brain tissue loss on day 28 (b) after 10, 50 or 100 μL of blood injected into the right caudate of rats. Triangles refer to animals with a 10-μL autologous blood injection, circles to 50 μL, and small squares to 100 μL
Conclusion
The major findings in this study are: first, at-risk brain tissue areas measured on MRI images correlated well with lesions showing as DARPP-32 immunoreactivity loss during the first several days after ICH; second, at-risk tissue volumes measured at day 3 after ICH correlated not only with the brain swelling volumes on day 3, but also with brain tissue loss measured on day 28.
DARPP-32, a specific marker of GABAergic neurons, is located in the basal ganglia, and was used to confirm brain injury morphologically. T2- and T2*-weighted MR images are non-invasive measurements that can provide important information regarding hematoma, brain edema, as well as brain tissue damage. T2 relaxation times are considered to relate to the dynamic state of water at microscopic tissue levels and are sensitive to water binding [7]. We consider it to be the whole extent of at-risk tissue. T2* sequences are usually obtained to detect small areas of heme deposition. Recent research also demonstrated that it likely represents ferric iron deposition within the brain parenchyma [10]. In this study, T2*-weighted images were used to confirm the existence and evaluate hematoma size during the early phase of ICH [8]. Through the comparison of T2/T2* lesions with DARPP-32 negative/hematoma areas, we found that at-risk tissue areas determined on MR images correlated well with that shown in histological sections at different time points after ICH. This indicates that at-risk brain tissue areas can be determined by the T2/T2* MR images.
It is important to develop a measurement that can be used to estimate acute brain injury. The measurement can then be used to predict ICH patient brain tissue loss and assess the effectiveness of therapies. Brain atrophy after ICH develops gradually and peaks between 1 and 2 months in rats [5]. Our current results showed that at-risk brain tissue volumes measured on day 3 after ICH correlated well with brain tissue loss on day 28. At-risk brain tissue volumes measured by MRI could be an indicator for predicting long-term brain atrophy. In addition, the fact that at-risk brain tissue areas induced by 100 μL of autologous whole blood were much larger than those induced by a 50- or 10-μL blood injection indicates that the key factor affecting ICH outcome is hemorrhagic volume [13].
Our previous studies found a correlation between acute edema formation and ICH-induced neurological deficits during the acute phase [6]. It is not clear whether or not there is connection between edema and the brain tissue at risk measured on MR images. According to the current study, the degree of brain swelling on day 3 after ICH did correlate with volume of at-risk brain tissue on day 3 measured on T2/T2* images.
In summary, the present study shows for the first time to our knowledge the utility of using MRI (T2, T2*) as a tool in evaluating early brain injury and predicting long-term brain tissue loss after ICH.
References
Allkemper T, Tombach B, Schwindt W, Kugel H, Schilling M, Debus O, Mollmann F, Heindel W (2004) Acute and subacute intracerebral hemorrhages: comparison of MR imaging at 1.5 and 3.0 T–initial experience. Radiology 232:874–881
Belayev L, Obenaus A, Zhao W, Saul I, Busto R, Wu C, Vigdorchik A, Lin B, Ginsberg MD (2007) Experimental intracerebral hematoma in the rat: characterization by sequential magnetic resonance imaging, behavior, and histopathology. Effect of albumin therapy. Brain Res 1157:146–155
Broderick JP, Adams HP Jr, Barsan W, Feinberg W, Feldmann E, Grotta J, Kase C, Krieger D, Mayberg M, Tilley B, Zabramski JM, Zuccarello M (1999) Guidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 30:905–915
Felberg RA, Grotta JC, Shirzadi AL, Strong R, Narayana P, Hill-Felberg SJ, Aronowski J (2002) Cell death in experimental intracerebral hemorrhage: the “black hole” model of hemorrhagic damage. Ann Neurol 51:517–524
Hua Y, Nakamura T, Keep RF, Wu J, Schallert T, Hoff JT, Xi G (2006) Long-term effects of experimental intracerebral hemorrhage: the role of iron. J Neurosurg 104:305–312
Hua Y, Schallert T, Keep RF, Wu J, Hoff JT, Xi G (2002) Behavioral tests after intracerebral hemorrhage in the rat. Stroke 33:2478–2484
Jadhav V, Sugawara T, Zhang J, Jacobson P, Obenaus A (2008) Magnetic resonance imaging detects and predicts early brain injury after subarachnoid hemorrhage in a canine experimental model. J Neurotrauma 25:1099–1106
Kharatishvili I, Sierra A, Immonen RJ, Grohn OH, Pitkanen A (2009) Quantitative T2 mapping as a potential marker for the initial assessment of the severity of damage after traumatic brain injury in rat. Exp Neurol 217:154–164
Svenningsson P, Nishi A, Fisone G, Girault JA, Nairn AC, Greengard P (2004) DARPP-32: an integrator of neurotransmission. Annu Rev Pharmacol Toxicol 44:269–296
Wu G, Xi G, Hua Y, Sagher O (2010) T2* magnetic resonance imaging sequences reflect brain tissue iron deposition following intracerebral hemorrhage. Transl Stroke Res 1:31–34
Wu J, Hua Y, Keep RF, Nakamura T, Hoff JT, Xi G (2003) Iron and iron-handling proteins in the brain after intracerebral hemorrhage. Stroke 34:2964–2969
Xi G, Hua Y, Bhasin RR, Ennis SR, Keep RF, Hoff JT (2001) Mechanisms of edema formation after intracerebral hemorrhage: effects of extravasated red blood cells on blood flow and blood-brain barrier integrity. Stroke 32:2932–2938
Xi G, Keep RF, Hoff JT (2006) Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol 5:53–63
Xi G, Keep RF, Hua Y, Xiang J, Hoff JT (1999) Attenuation of thrombin-induced brain edema by cerebral thrombin preconditioning. Stroke 30:1247–1255
Yoshioka H, Niizuma K, Katsu M, Okami N, Sakata H, Kim GS, Narasimhan P, Chan PH (2011) NADPH oxidase mediates striatal neuronal injury after transient global cerebral ischemia. J Cereb Blood Flow Metab 31:868–880
Acknowledgements
This study was supported by grants NS-017760, NS-039866, and NS-057539 from the National Institutes of Health (NIH) and 0840016N from the American Heart Association (AHA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH and AHA.
Conflict of InterestWe declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Wien
About this paper
Cite this paper
Jin, H. et al. (2013). T2 and T2* Magnetic Resonance Imaging Sequences Predict Brain Injury After Intracerebral Hemorrhage in Rats. In: Katayama, Y., Maeda, T., Kuroiwa, T. (eds) Brain Edema XV. Acta Neurochirurgica Supplement, vol 118. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1434-6_28
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1434-6_28
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1433-9
Online ISBN: 978-3-7091-1434-6
eBook Packages: MedicineMedicine (R0)