Abstract
Objective: Recently VA dissection has drawn attention as a relatively common cause of stroke because of the introduction of MRI as a diagnostic technique. Basiparallel anatomic scanning (BPAS) was designed to visualize the surface appearance of the vertebrobasilar artery within the cistern. Volumetric isotropic TSE acquisition (VISTA) is a sort of black blood imaging method to evaluate the arterial wall and lumen. In this study, we aimed to evaluate the efficacy of the new MRI modalities “BPAS and VISTA,” and to present a retrospective analysis of our experience with the diagnosis. Materials and methods: Between1995 and 2010, we experienced 24 cases of VA dissection at our institution. In our cases, we could obtain images of 15 in BPAS and VISTA in addition to MRA. The mean age of the 15 patients (12 male and 3 female) was 51 years old (range 18–80). Ten of fifteen patients presented with ischemia, and 5/15 with only headache. There were no cases of SAH. In BPAS, we evaluated dilatation of the external diameter of the affected artery. We compared the findings in BPAS with MRA to evaluate the discrepancy. In VISTA, we evaluated its capability to distinguish intramural hematoma. Result: Thirteen of fifteen patients presented with dilatation of the external diameter on BPAS. By comparing the findings in BPAS with MRA, we found a discrepancy in 8/15 cases (53%). We could detect intramural hematoma by using VISTA in 9/15 cases (60%). Thirteen of fifteen patients received follow-up MRI. Temporal change of the arterial shape was confirmed in 7/13 cases (53.8%). Conclusion: Dilatation of the external diameter was shown highly frequently in VA dissections. In addition, a discrepancy between BPAS and MRA as well as the intramural hematoma on VISTA was found comparatively frequently. BPAS and VISTA are minimally invasive and useful methods as screening tests.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
VA dissection has recently drawn attention as a relatively common cause of stroke because of the introduction of MRI as a diagnostic technique. In neuroimaging of dissections, confirming the arterial lumen abnormality was the old standard. Subsequently intramural hematoma was recognized as the definitive finding [3, 5, 6]. In recent reports, much attention has been paid to the surface appearance of the affected artery. According to the SCADS (Spontaneous Cervicocepharic Arterial Dissections Study) Japan criteria, in addition to findings of the arterial lumen and its temporal changes, detecting dilatation of the external diameter combined with narrowing or occlusion of the arterial lumen enabled to make the diagnosis of dissection. Recently, we have often used the new MRI modalities “BPAS and VISTA” for the diagnosis of VA dissection. BPAS is a simple MR imaging technique to visualize the surface appearance of the vertebrobasilar artery within the cistern. It is useful to judge the condition of the artery, whether it is dilatation, normal or hypoplasia. VISTA is a sort of black blood imaging method. It is effective to evaluate the arterial wall and lumen. In this study, we aimed to evaluate the efficacy of the new MRI modalities “BPAS and VISTA,” and to present a retrospective analysis of our experience in the diagnosis.
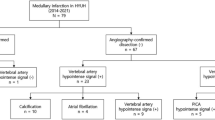
Material and Methods
Between 1995 and 2010, we experienced 24 cases of VA dissection at Fukuoka University Hospital. The diagnosis of VA dissection was made based on characteristic features, which were demonstrated on both the conventional angiography and MRI (pearl-and-string sign, string sign, tapered occlusion, intimal flap and intramural hematoma on T1-weighted image, dilatation of the extra-diameter on BPAS). In the 24 patients, we could obtain the images of 15 on conventional angiography, BPAS and VISTA in addition to MRA. In BPAS, we evaluated dilatation of the external diameter on the affected artery. We compared the findings in BPAS with MRA to evaluate the discrepancy. In VISTA, we evaluated its capability to distinguish intramural hematoma.
Patient Population
In our cases, we could obtain the images of 15 patients in BPAS and VISTA in addition to MRA. The mean age of the 15 patients (12 male and 3 female) was 51 years old (range 18–80). Ten of fifteen patients presented with ischemia, and 5/15 with only headache. There were no cases of SAH. In 9 patients, the initial MRI was performed within 2 weeks after the onsets.
MRI Protocol
MR imaging was performed with a 1.5-T unit (ACHIEVA; Philips Medical Systems, Best, The Netherlands). Cranial MRA was carried out using a 3D TOF technique. Imaging parameters were 24.7/9.6 (TR/TE), 20° flip angle, 150 × 150-mm field of view, 256 × 160 matrix, 140 sections with a 0.6-mm effective thickness that resulted in the coverage of a volume of 84 mm in the craniocaudal direction.
BPAS was performed in a 25-mm-thick coronal section parallel to the clivus by using a fast spin-echo sequence. The following imaging parameters were used: 3,000/800 (TR/TE), 150 × 150-mm field of view, and 256 × 256 matrix. Acquisition time was 2 min 24 s with our pulse sequence. We added only the gray scale reversal in post-proceedings.
VISTA was performed as follows: the coronal 3D imaging slab centered at the basilar artery was prescribed based on the TOF angiogram (Fig. 1). Refocus control was set up at a 60° angle. ECG triggering was not used. Imaging parameters included: 450/19 (TR/TE), turbo factor 20, 150 × 150-mm field of view, and a 224 × 512 matrix. Acquisition time was 5 min 20 s.
Results
On the MRA, pearl-and-string sign was found in two patients, pearl sign in two cases, string sign in four and occlusion in seven. On the BPAS, all but two patients presented with dilatation of the external diameter of the affected artery. By comparing the findings in BPAS with MRA, we could find the discrepancy in 8/15 cases (53%). We could detect intramural hematoma by using VISTA in 10/15 cases (66.7%). Thirteen of fifteen patients received follow-up MRI. Temporal change of arterial shape was confirmed in 7/13 patients (53.8%). On the MRA, occlusive change was detected in one patient, and improvement of the patency in three. On the BPAS, the external dilatation had normalized in four patients. On the VISTA, regression or change in the signal intensity of the intramural hematoma was shown in seven patients (Table 1).
Case 5: A 47-year-old male presented with sudden onset of headache. MRA revealed a string sign, while VISTA showed an intramural hematoma. In this case, we could identify a pseudolumen and narrowed true lumen on VISTA (Fig. 2). He was treated conservatively and underwent follow-up MRI 1 month and 3 months later. VISTA and MRA revealed a normalized artery. On VISTA, the intramural hematoma had regressed. On MRA, the arterial patency had gradually improved. Besides, on BPAS, the external dilatation had normalized (Fig. 3).
Initial MRI was performed 2 days after the onset (a), follow-up MRI 1 month later (b), 3 months later (c). VISTA and MRA revealed a normalized artery. On VISTA, the intramural hematoma had regressed. On MRA, the arterial patency had gradually improved. Besides, the external dilatation had normalized on BPAS
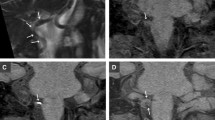
Case 12: The 34-year-old male presented with right Wallenberg syndrome. MRA revealed the occlusion of the right VA. VISTA presented an intramural hematoma at the same position. Follow-up MRI was performed 2 and 6 months later. On BPAS, the external dilatation had regressed (Fig. 4).
This 34-year-old male presented with a right Wallenberg syndrome. (a) MRA revealed the occlusion of the right VA (arrowhead). (b) VISTA presented an intramural hematoma at the same position (large white arrow). (c, d) Follow-up MRI was performed 2 and 6 months later. On BPAS, the external dilatation had regressed (small white arrow)
Case 7: A 46-year-old male presented with headache and left cerebellar infarction. MRA revealed a string sign at the left PICA. BPAS showed dilatation of the external diameter of the vertebral artery. VISTA indicated an intramural hematoma at the same position (Fig. 5).
This 46-year-old male presented with headache and left cerebellar infarction. (a) MRA revealed a string sign at the left PICA (large white arrow). (b) BPAS showed dilatation of external diameter of the vertebral artery (small white arrow). (c) VISTA indicated an intramural hematoma at the same position (arrowhead)
Case 15: A 38-year-old male presented with headache and left cerebellar infarction. On BPAS, we could not identify the external diameter of the vertebral artery, although our investigation was possible. On MRA, the left vertebral artery was shown in double contrast, which resulted in equivocal findings. Only VISTA indicated an intramural hematoma at the same position (Fig. 6).
This 38-year-old male presented with headache and left cerebellar infarction. (a) On the BPAS, we could not identify external diameter of vertebral artery, despite our investigation. (b) On the MRA, the left vertebral artery was shown in double contrast, which resulted in equivocal findings (small white arrow). (c) Only VISTA indicated an intramural hematoma at the same position (large white arrow)
Discussion
Intracranial VA dissections are reported to cause headache, brain stem infarction and SAH with an associated high morbidity and mortality [7, 8]. It has recently drawn attention as a relatively common cause of stroke because of the introduction of MRI as a diagnostic technique [2]. In neuroimaging of dissections, confirming the arterial lumen abnormality was the old standard. Subsequently, intramural hematoma on MRI has been recognized as the definitive finding [3, 5, 6]. In recent reports, much attention has been paid to the surface appearance of the affected artery.
BPAS-MR imaging can easily show the outer contour of vertebro-basilar arteries clearly. It only requires a 2-cm-thick, heavily T2-weighted coronal imaging, parallel to the clivus, with gray-scale reversal in post-proceedings. By comparing the findings in BPAS with MRA, we can precisely evaluate the condition of the vertebrobasilar artery. Nagahata et al. reported that BPAS was useful to confirm hypoplasia or occluded vertebral arteries, and to reveal the whole appearance of large or partially thrombosed aneurysms of the vertebrobasilar system [4]. It is the same procedure for the dissection. In our study, almost all of the patients presented with dilatation of the external diameter of the affected artery. In addition, a discrepancy between BPAS and MRA and temporal change in their findings were found comparatively frequently, which enabled us to make the diagnosis of dissection. In other words, to perform follow-up MRI as well as MRA with BPAS is recommended for making a diagnosis. With limited use of BPAS, it is difficult to evaluate the outer contour of arteries, which are distant from the median position of clivus. Therefore, it is also hard to evaluate VA dissection distal to the cranio-cervical junction with a single use of BPAS.
VISTA is a sort of black blood imaging method. The feature of the black blood imaging method is to reveal the structure of the arterial wall and lumen clearly. The black blood imaging method has been used in many ways to evaluate carotid plaque [1]. VISTA, which is 3D imaging, enables us to acquire the optimal dimension of the individual vessel. In addition, VISTA does not require the use of the ECG triggering with the refocus control technique. It enables us to shorten the acquisition time and consequently to obtain images with thinner slices as compared with 2D imaging. In our cases, we could identify intramural hematoma by using VISTA in 60%. In contrast to BPAS, it is possible to reveal the structure regardless of laterality.
Conclusion
Dilatation of the external diameter was shown highly frequently in VA dissections. In addition, a discrepancy between BPAS and MRA as well as the intramural hematoma on VISTA was found comparatively frequently. Therefore, performing follow-up MRI is recommended to evaluate the temporal change of the findings for making the diagnosis. BPAS and VISTA are minimally invasive and useful methods for screening tests.
References
Fan Z, Zhang Z, Chung Y et al (2010) Carotid arterial wall MRI at 3T using 3D variable-flip-angle turbo spin-echo (TSE) with flow-sensitive dephasing. J Magn Reson Imaging 31:645–654
Leclerc X, Lucas C, Pruvo JP et al (1999) Preliminary experience using contrast-enhanced MR angiography to assess vertebral artery structure for the follow-up of suspected dissection. Am J Neuroradiol 20:1482–1490
Lum C, Chakraborty S, Schlossmacher M et al (2009) Vertebral artery dissection with a normal appearing lumen at multisection CT angiography: the importance of identifying wall hematoma. Am J Neuroradiol 30:787–792
Nagahata M, Abe Y, Uno S et al (2005) Surface appearance of the vertebrobasilar artery revealed on basiparallel anatomic scanning (BPAS)-MR imaging: Its role for brain MR examination. Am J Neuroradiol 26:2508–2513
Ohkuma H, Suzuki S, Kikkawa T et al (2003) Neuroradiologic and clinical features of arterial dissection of the anterior cerebral artery. Am J Neuroradiol 24:691–699
Ohkuma H, Suzuki S, Shimamura N et al (2003) Dissecting aneurysms of the middle cerebral artery: neuroradiological and clinical features. Neuroradiology 45:143–148
Yamaura A, Watanabe Y, Saeki N (1990) Dissecting aneurysms of the intracranial vertebral artery. J Neurosurg 72:183–188
Yoshimoto Y, Wakai S (1997) Unruptured intracranial vertebral artery dissection. Clinical course and serial radiographic imagings. Stroke 28:370–374
Conflicts of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag/Wien
About this paper
Cite this paper
Takemoto, K. et al. (2011). The New MRI Modalities “BPAS and VISTA” for the Diagnosis of VA Dissection. In: Tsukahara, T., Regli, L., Hänggi, D., Turowski, B., Steiger, HJ. (eds) Trends in Neurovascular Surgery. Acta Neurochirurgica Supplementum, vol 112. Springer, Vienna. https://doi.org/10.1007/978-3-7091-0661-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-7091-0661-7_11
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-0660-0
Online ISBN: 978-3-7091-0661-7
eBook Packages: MedicineMedicine (R0)