Abstract
Amyotrophic lateral sclerosis (ALS) and spinal muscular atrophy (SMA) represent the two major forms of motoneuron disease. In both forms of disease, spinal and bulbar motoneurons become dysfunctional and degenerate. In ALS, cortical motoneurons are also affected, which contributes to the clinical phenotype. The gene defects for most familial forms of ALS and SMA have been discovered and they point to a broad spectrum of disease mechanisms, including defects in RNA processing, pathological protein aggregation, altered apoptotic signaling, and disturbed energy metabolism. Despite the fact that lack of neurotrophic factors or their corresponding receptors are not found as genetic cause of motoneuron disease, signaling pathways initiated by neurotrophic factors for motoneuron survival, axon growth, presynaptic development, and synaptic function are disturbed in ALS and SMA. Better understanding of how neurotrophic factors and downstream signaling pathways interfere with these disease mechanisms could help to develop new therapies for motoneuron disease and other neurodegenerative disorders.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Amyotrophic lateral sclerosis
- Superoxide dismutase
- Mitochondria
- Endoplasmic reticulum stress
- RNA metabolism
- Survival motoneuron protein
- Frontotemporal lobar degeneration
- TDP-43 gene
- Ciliary neurotrophic factor
- Cardiotropin-1
- Leukemia-inhibitory factor
- Neurotrophins
- BDNF
- Glial-derived neurotrophic factor
- Neurodegeneration
1 Introduction
During development of higher vertebrates, many types of neurons are generated in excess, and about half of the newly generated neurons undergo cell death. Spinal and bulbar motoneurons have been a central focus of research to understand the underlying mechanisms. These neurons become postmitotic at early stages of development; they grow out axons and make functional contacts with skeletal muscle, before this phase of physiological cell death occurs. Pioneering work by Viktor Hamburger and Rita Levi-Montalcini has shown that limiting amounts of survival factors from target tissue play a central regulatory role in this context, and this observation has been the basis for the discovery of neurotrophic factors in the twentieth century. It has long been suspected that dysregulation of neurotrophic signaling could also underlie the degeneration of motoneurons in amyotrophic lateral sclerosis and spinal muscular atrophy, the two major forms of human motoneuron disease. During the last three decades, gene defects underlying monogenetic forms of these disorders have been identified, and none of these gene defects point to a lack of neurotrophic factors or defective receptors as cause of motoneuron disease. Motoneurons that are isolated from mouse embryos and cultured in vitro also depend on neurotrophic factors for their survival. These cultures are a useful tool for studying signaling pathways for motoneuron survival, but also signaling for axon growth, presynaptic differentiation, dendrite growth and stabilization of neurites, and synaptic contacts. These parameters represent targets of motoneuron disease processes, and recent research has indicated that neurotrophic factor signaling also interferes with these mechanisms. The analysis of disease processes and mechanisms how neurotrophic factors interfere could help to develop new therapeutic strategies for amyotrophic laterals sclerosis and spinal muscular atrophy.
2 Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disorder causing dysfunction and death of lower motoneurons in the spinal cord and brain stem and of upper motoneurons in the motor cortex (Kiernan et al. 2011). This results in progressive dysfunction of neuromuscular innervation that normally causes death due to respiratory failure. The incidence of ALS is approximately 2 per 100,000 individuals worldwide, the mean age of onset is 55–60 years, and the disease more commonly affects men than women. Average survival from symptom onset is approximately 3 years, although some forms of the disease also have a much slower disease course, allowing patients to survive for several decades (Wood-Allum and Shaw 2010). Traditionally, ALS has been considered as a pure motor disorder. However, it has become increasingly evident that also other types of neurons are affected and that some forms of ALS are coupled with prefrontal dementia or with degeneration of dopaminergic neurons. Even in patients in which dysfunction of the motor systems predominates the clinical phenotype, histopathological alterations are also found in many types of neurons, including hippocampus and basal ganglia (Al-Sarraj et al. 2011). Therefore, ALS is now regarded as a more general neurodegenerative disorder in which the motor phenotype predominates the clinical picture.
In more than 90 % of all cases, ALS appears sporadic. Only 5–10 % of all cases are familial. In these cases, an autosomal-dominant inheritance is predominant (Andersen and Al-Chalabi 2011). Even this subset of familial ALS is highly heterogeneous on a genetic basis, and the so far identified genetic defects underlying familial forms of ALS point to multifactorial pathogenic processes (Table 1).
3 fALS with Mutations in the SOD-I Gene
The first identified gene defect which accounts for about 10–20 % of familial ALS were point mutations in the gene for Cu2+/Zn2+-dependent superoxide dismutase (SOD-I) (NM 000454) (Rosen et al. 1993). So far, more than 50 different mutations in this gene have been identified. Clinically, there seems to be no clear correlation between disease onset or severity with specific mutation in the SOD-I gene (Andersen and Al-Chalabi 2011), and the clinical appearance of ALS does not differ from the majority of sporadic cases in this disease. Some types of mutations in the SOD-I gene are prone to cause a severe and rapid course of disease, in particular the A4V mutation; other forms, i.e., E21G, G37R, D40A, G93C, I104F, L144S, and I151C, are associated with survival times that can exceed 10 years (reviewed in Ferraiuolo et al. 2011). Not all of these mutations are associated with loss of enzymatic function. In particular the G37A mutation which has been intensively studied in transgenic mouse models, but also the A90V or D91A mutations, does not primarily affect enzyme activity (reviewed in Al-Chalabi et al. 2012).
The SOD-I protein plays a central role in detoxifying superoxide radicals from the cell and preventing the generation of hydroxyl radicals that react with a great variety of molecules, in particular polyunsaturated fatty acids in cell membranes, but also proteins and nucleic acids. Cerebrospinal fluid (CSF), but also serum and urine, show elevated markers of free radical damage in patients with ALS (Smith et al. 1998; Simpson et al. 2004), and this does not only apply to patients and mouse models of fALS with mutations in the SOD-I gene. Interestingly, knockout of the SOD-I gene in mice does not result in motoneuron disease (Reaume et al. 1996), whereas transgenic overexpression of mutant SOD-I in general causes rapid and severe forms of the disease (Gurney et al. 1994). Mouse models overexpressing A4V or G93A mutant SOD-I molecules have most commonly been used in studies on the pathophysiological consequences of these mutations. The observation that SOD-I gene knockout does not lead to motoneuron disease in mice and that many of the mutations identified in patients with fALS do not show reduced enzyme activity points to pathogenic mechanisms other than loss of enzyme activity. These include actions of the mutant protein in cell types that appear not primarily affected such as microglia and astrocytes. Mutant SOD-I in microglia increases NADPH oxidase-mediated superoxide production (Harraz et al. 2008), resulting in prolonged ROS production. Mutant SOD-I protein has been found to interact with chromogranins (Urushitani et al. 2006) and by this way appears to be released from astrocytes and interneurons. Thus, extracellular mutant SOD-I can activate microglia and possibly also promote direct toxic effects on motoneurons. In chimeric mice expressing mutant SOD-I in astrocytes, motoneurons degenerate and show ALS pathology (Clement et al. 2003). Furthermore, mice in which the mutant allele encoding SOD-I G37R is deleted from motoneurons using Cre-lox technology (Boillee et al. 2006) show delayed disease onset, but no alteration in the disease course once first symptoms have become apparent. Also in cell culture, toxic effects of astrocytes expressing mutant SOD-I have been demonstrated when these cells are cocultured with primary motoneurons from embryonic mouse (Nagai et al. 2007) or human stem cell-derived motoneurons (Di Giorgio et al. 2008). This toxic effect of mutant astrocytes has been shown to involve the deregulation of glutamate receptor 2 (GluR2) in motoneurons, as a consequence of mutant SOD-I expression in astrocytes (Van Damme et al. 2007). Taken together, these findings indicate that non-neuronal cells expressing mutant forms of SOD-I exert toxic effects on motoneurons and contribute to disease.
Both in patients and mouse models with mutations in the SOD-I gene, protein inclusions are found in motoneurons and other types of neurons, but these inclusions differ from inclusions found in the vast majority of sporadic ALS patients and other forms of familial ALS because they do not include the TDP43 protein (Maekawa et al. 2009). Some of the protein aggregates that include the mutant SOD-I protein are associated with mitochondria and thus could contribute to mitochondrial dysfunction. The mutated SOD-I protein seems to aggregate in vacuoles in the mitochondrial intermembrane space (Wong et al. 1995), and this finding together with other reports showing interaction of mutant SOD-I protein with bcl-2 (Pasinelli et al. 2004) gives further support to the idea that the mutant SOD-I protein causes mitochondrial dysfunction and defective respiratory chain activity. These findings also correlate with observations that the calcium buffering capacity is impaired in mitochondria isolated from neural tissues of SOD-I mutant mice (Damiano et al. 2006; Grosskreutz et al. 2010). The altered calcium homeostasis caused by this defect might also correlate with susceptibility for glutamate-mediated excitotoxicity and ER stress, which is also observed in motoneurons from SOD-I mutant mouse models.
Mitochondrial dysfunction and morphological alterations such as vacuolation occur early during presymptomatic disease stages in mouse models, and they are thought to contribute to defective axonal transport of mitochondria (De Vos et al. 2007). It is thought that a reduction in the mitochondrial content in axon terminals could be a major mechanism for dying-back axonopathy, which is generally observed in ALS.
Because of the multitude of pathological mechanisms that apparently contribute to motoneuron disease in SOD-I mutant mouse and cell culture models, no clear conclusions can be drawn on which signaling pathways downstream of neurotrophic factor receptors are most important to interfere with pathomechanisms in this form of familial ALS. Overexpression of mutant SOD-I in motoneurons causes cytoplasmic aggregation of the enzyme, and neurons with such aggregates subsequently undergo apoptotic cell death (Durham et al. 1997). When SOD-I G93A mice are crossed with bcl-2-overexpressing mice, onset of disease is delayed (Kostic et al. 1997), suggesting that inhibition of classical pathways for apoptotic cell death interferes with the disease. However, bcl-2 overexpression cannot prevent disease. Similar observations were made when SOD-I G93A mutated mice were crossed with mice overexpressing a dominant-negative ICE isoform, which prevents caspases from activation of cell death pathways (Friedlander et al. 1997). Thus, interference with classical apoptotic signaling pathways apparently has some impact, but the effects are not sufficient to prevent disease in this mouse model of familial motoneuron disease. This indicates that interference with motoneuron cell death programs is not sufficient for therapy and that additional pathomechanisms, ranging from dysfunction of neuromuscular transmission to destabilization of axonal processes and depletion of dendritic synaptic inputs, also need to be targeted, at least in this form of motoneuron disease.
4 Inclusions and Altered RNA Metabolism in ALS: TDP-43, FUS, C9orf72
Alterations in RNA metabolism have been suspected to contribute to ALS pathophysiology for a long time. Since the discovery that fragile X syndrome is caused by altered expression of FMR-1, a member of a large family of RNP proteins that are involved in RNA binding and transport (Ashley et al. 1993), the potential impact of defective RNA processing to neurodegeneration has increasingly become a focus of interest. However, the mechanisms how altered RNA metabolism could contribute to the pathomechanisms of ALS have only become more concrete in the last few years. An important finding in this context was the identification of the TAR DNA-binding protein-43 (TDP-43) protein as a major component of ubiquitin-positive cellular inclusions (Neumann et al. 2006). These inclusions have the appearance of threads, skeins, or compact bodies and are located in nuclei and soma of neurons, including proximal dendrites and axons. TDP-43-positive inclusions have also been found in other neurodegenerative disorders such as FTLD (Buratti and Baralle 2008). They have also been described in postmortem brain of patients with Huntington’s disease (Schwab et al. 2008), Alzheimer’s disease, and dementia with Lewy body inclusions (Higashi et al. 2007).
The cellular function of TDP-43 is not fully understood. TDP-43 is a 414-amino-acid protein of the hnRNP family (Krecic and Swanson 1999), with two RNA recognition motifs (RRM1 and RRM2) and a C-terminal glycine-rich domain, and thus resembles many other RNA-binding proteins such as fused in sarcoma (FUS) and hnRNP-R, the latter having been previously identified to interact with the survival motoneuron (Smn) protein (Rossoll et al. 2002), the central protein of the Smn complex that is deficient in spinal muscular atrophy.
After the identification of TDP-43 protein as the major component of proteinaceous inclusions in sporadic ALS and other neurodegenerative disorders, mutations in the gene encoding for TDP-43 were found in some ALS patients (Rutherford et al. 2008; Mackenzie et al. 2010), and also in patients with frontotemporal lobar degeneration (FTLD, new nomenclature FTLD-TDP). About 4 % of patients with familial ALS and 1.5 % of patients with sporadic ALS have mutations in the TDP-43 gene. All of the so far identified mutations in familial ALS are autosomal dominant, and most of them encode for a missense mutation within the C-terminal domain which encodes the glycine-rich domain (Pesiridis et al. 2009), a part of the protein that is important for interaction with other proteins and molecules, but it does not directly interact with RNA. Based on these data, it has been suggested that the mutations in the C-terminus are sufficient to induce neurodegeneration.
The TDP-43-positive inclusions are strongly ubiquitinylated and phosphorylated. It is not the full-length TDP-43 which is found in inclusions, but a truncated 20–25 kDa C-terminal fragment (Pesiridis et al. 2011). So far it is still unclear whether the associated loss of TDP-43 function, due to the cleavage of the N-terminus, which contains the RRM1 domain, is causative for neurodegeneration or a loss of function due to depletion of TDP-43 from the nucleus and other cytoplasmic regions where TDP-43 functions are necessary for neuronal maintenance or gain of function by the cleaved fragments.
TDP-43 interactions with RNA have been studied in detail, and these studies have revealed functions of TDP-43 in several aspects of RNA metabolism. The RRM1 domain of this protein binds to single-stranded RNA (Buratti and Baralle 2001), in particular to regions containing UG repeats. These UG regions are contained in many RNAs, and this fits with the observation that several thousand different RNA species can interact with the protein (Tollervey et al. 2011; Polymenidou and Lagier-Tourenne 2011), in particular intronic regions, but also 3′untranslated regions (UTRs), and also noncoding RNAs. The association of TDP-43 with intronic sequences and its predominant nuclear localization implicates TDP-43 in early steps of pre-mRNA processing in the nucleus. These functions could include transcriptional regulation, alternative splicing (Buratti et al. 2001), and in particular micro-RNA (miRNA) processing. Defects in miRNA malfunction have been shown to result in motoneuron disease (Haramati et al. 2010). Thus, TDP-43 (Buratti and Baralle 2010a) and other members of the hnRNP protein family (Pascale and Govoni 2012) like FUS (Morlando et al. 2012) could also contribute to motoneuron maintenance by regulating miRNA function.
Whether motoneuron injury is caused by loss of such nuclear function of TDP-43 is still not fully understood. Among the mRNAs that interact with TDP-43 are those encoding for FUS, VCP (Sephton et al. 2011), and TDP-43 mRNA itself (Buratti and Baralle 2010b). TDP-43 regulates processing of its own transcript by interaction of the protein with the 3′UTR of TDP-43 mRNA, leading to alternative splicing of the 3′UTR. As a consequence, high levels of TDP-43 cause reduced translation of TDP-43 mRNA. These functions involve interaction of TDP-43 with other proteins that bind to the C-terminus, in particular other members of the hnRNP family. These include hnRNP-A2/B1 (Buratti et al. 2005), hnRNP-A1, hnRNP-A3, and hnRNP-C1-C2 (Ling et al. 2010), but possibly also other members of this large family (Freibaum et al. 2010).
Blocking TDP-43 expression with antisense oligonucleotides in adult mouse brain alters the expression levels of more than 600 mRNA transcripts and changes splicing of more than 900 transcripts (Polymenidou and Lagier-Tourenne 2011), including such transcripts which are also relevant for motoneuron function, such as choline acetyl transferase, and transcripts for other RNA-binding proteins for which mutations lead to degeneration, such as FUS and progranulin.
Several animal models have been developed to study TDP-43 dysfunction, including mouse models in which the gene is knocked out or overexpressed in mutant form, but also Drosophila, zebrafish, and C. elegans models (reviewed in Wegorzewska and Baloh 2011). Many models available so far cannot give final hints about the pathomechanistic contributions of mutant TDP-43 to motoneuron disease, because those overexpressing TDP-43 might also lead to dysregulation of RNAs simply as a consequence of the TDP-43 overexpression itself, and a good example for this problem is the processing of the TDP-43 mRNA by TDP-43. Another potential problem is the interaction of the TDP-43 with intronic sequences, which are highly different between species, and interaction of TDP-43 with intronic sequences in human genes might not be found in mouse, fish, and C. elegans models, because the intronic sequences differ more than coding sequences between these species. Moreover, by overexpression of mutant TDP-43, the RRM1 domains are mostly preserved, allowing functions in pre-mRNA processing that either resemble the physiological function or alter these functions in a dominant-negative manner, for example, when the C-terminal mutations lead to altered distribution of the protein. Thus, the normal function of TDP-43 in regulating expression of mRNA levels of cyclin-dependent kinase 6 (Ayala et al. 2008), histone deacetylase 6 (Fiesel et al. 2010, 2011), low molecular weight neurofilament (Strong et al. 2007), or other transcripts with essential functions in motoneurons could contribute to the pathophysiology and generate additional pathological features in these mouse models that do not necessarily exist in humans with mutant TDP-43.
So far, the mechanisms that lead to altered subcellular distribution of TDP-43 and translocation between the nucleus and the cytoplasm are not fully understood. Different types of cell stress lead to TDP-43 redistribution from the nucleus to the cytoplasm (Moisse et al. 2009a, b), and the protein is then found within stress granules (Freibaum et al. 2010; Dewey et al. 2011; Kiebler and Bassell 2006), which are thought to stabilize mRNAs and prevent translation under these specific cellular conditions (Kiebler and Bassell 2006). This function seems to be central for understanding the role of TDP-43 in motoneuron disease. After axotomy, TDP-43 translocates to cytosolic compartments, and this translocation seems to be functionally connected with caspase-3 activation (Moisse et al. 2009a). Also after oxidative insult, TDP-43 is recruited to stress granules (Colombrita et al. 2009). There are also reports indicating that TDP-43 could interact with SOD-I and 14-3-3 proteins in the cytosol and thus modulate the stability of mRNAs such as the neurofilament-L chain mRNA (Volkening et al. 2009). Moreover, stress granule dynamics seems to be influenced by TDP-43 (Dewey et al. 2011; McDonald et al. 2011) under conditions such as oxidative stress or sorbitol-induced osmotic stress. It is still unclear at which stage of disease such stress granules occur and whether TDP-43 inclusion in stress granules is a consequence of other pathophysiological mechanisms, whether such stress granules are fully reversible, or whether such stress granules can give rise to insoluble proteinaceous aggregates. As a common observation made under different types of cell stress, TDP-43 seems to be redistributed from the nucleus to the cytosol. Sporadic ALS patients with slow progression of the disease have been reported to exhibit a relatively low number of TDP-43 inclusions (Nishihira et al. 2009), and this points to a correlation between the number of these aggregates in motoneurons and severity of disease. Thus, TDP-43 aggregates apparently do not protect neurons from degeneration. It remains to be shown whether these TDP-43 aggregates are toxic and contribute to the neurodegenerative process.
The TDP-43 protein also interacts with another RNA-binding protein named fused in sarcoma (FUS) (Zinszner et al. 1994) or translocated in liposarcoma (TLS) (Freibaum et al. 2010). TDP-43 and FUS are related (Drepper et al. 2011) and both are members of the hnRNP protein family with two RRM (RRM1 and RRM2) motifs. This protein is also involved in transcriptional regulation and mRNA processing. Mutations in the FUS genes are found in 4 % of fALS cases (Kwiatkowski et al. 2009) and only rarely (probably less than 1 %) in sporadic ALS cases (Ferraiuolo et al. 2011; Mackenzie et al. 2010). Similar to TDP-43, most mutations associated with ALS are found in the C-terminal regions containing the glycine-rich domain. Some of these mutations seem to disrupt a nuclear translocation signaling, thus leading to cytoplasmic accumulation of the FUS protein within cytoplasmic granules (Ito et al. 2011; Dormann et al. 2010). Alternatively, these mutations in the C-terminus could also disturb protein interaction in particular with other members of the hnRNP family, so that the altered subcellular distribution of the FUS protein in these ALS patients could also be caused by such defects. Similar to TDP-43, it is still not resolved whether loss of a physiological function of FUS due to instability of the protein, cellular misdistribution, or decreased stability causes motoneuron degeneration or a toxic gain of function.
Gene knockout mice have been generated that lack FUS gene function (Kuroda et al. 2000). These mice show male sterility and increased sensitivity to ionizing radiation, but no phenotype that could help to understand the role of this protein in neurons and in neurodegeneration.
The last major gap in the identification of gene defects responsible for familial ALS was closed by two independent groups identifying a hexanucleotide (GGGGCC) repeat expansion in the first intron of the C9ORF72 gene on human chromosome 5 as a frequent genetic cause of ALS (Renton et al. 2011; DeJesus-Hernandez et al. 2011). These mutations, which are associated with both frontotemporal dementia and ALS, cause disease with high penetrance with autosomal-dominant inheritance. There are first indications that this pathophysiology also influences RNA metabolism and that the expanded pre-mRNA also binds to members of the hnRNP family, in particular hnRNP-A3 (Mori et al. 2013a). The repeat domain forms a G-quadruplex structure in the corresponding mRNA (Fratta et al. 2012), exactly the same as those found in specific mRNAs that are highly sorted in neurons such as the mRNA for PSD95 and CaMKIIa (Subramanian et al. 2011; Drepper and Sendtner 2011). It is possibly that this structure encoded by mutant C9orf72 transcripts disturbs transport and sorting of mRNAs from the nucleus to the cytoplasm and subsequently into axons and dendrites. As an alternative disease mechanism, the formation of proteinaceous aggregates has been suggested. The (GGGGCC) repeat expansion seems to be translated, and the corresponding protein products are found as poly-(Gly-Ala) or poly-(Gly-Pro) or poly-(Gly-Arg) dipeptide repeat proteins in nuclei and the cytoplasm of neuronal cells (Ash et al. 2013; Mori et al. 2013b). These are presumably generated by novel translation initiation sites allowing the expanded GGGGCC repeat to be translated into proteins. Whether altered RNA metabolism by interaction of the corresponding mRNAs with hnRNP proteins or the formation of a quadruplex structure is the primary pathomechanism, or the formation of protein aggregates, and how these mechanisms relate to TDP-43 and FUS pathomechanisms is currently unknown.
Besides TDP-43, FUS, and C9orf72, two other proteins play a role in neurodegenerative disorders like FTLD and in ALS: progranulin and sortilin: Reduced progranulin levels and activity are thought to be of broad relevance for these diseases (Hu et al. 2010). Recently, sortilin was identified as a key progranulin-binding partner on the surface of cortical neurons. In the stressed nervous system, progranulin is not expressed in neurons, but in nearby glial cells. Sortilin rapidly internalizes progranulin to lysosomes. Mice that do not express Sortilin exhibit high levels of extracellular progranulin. Importantly, mice with a progranulin deficiency similar to that seen in FTLD were fully normalized with regard to progranulin levels when sortilin was deleted. These findings implicate sortilin-mediated progranulin endocytosis in FTLD and ALS pathophysiology and identify sortilin binding as a potential therapeutic site to alter progranulin pathology. Sortilin is also a co-receptor for the p75 neurotrophin receptor (P75NTR) and modifies a broad spectrum of actions through this receptor. In addition, sortilin is also involved in subcellular transport of complexes including BACE and other membrane proteins relevant for APP processing. Therefore, the interaction of p75NTR with sortilin could be a modifier for proganulin actions and thus modify disease mechanisms in those forms of motoneuron disease that suffer from altered progranulin metabolism.
5 Spinal Muscular Atrophy
Spinal muscular atrophy is the most common form of motoneuron disease in children and young adults (Hausmanowa-Petrusewicz 1978; Crawford and Pardo 1996). In contrast to amyotrophic lateral sclerosis, more than 90 % of all cases of this disease are caused by homozygous deletion or in rare cases mutation of the SMN1 gene on human chromosome 5. In contrast to most forms of familial ALS, this form of motoneuron disease is autosomal recessive and represents one of the rare cases where loss of function of a specific gene and the corresponding protein is responsible for the disease. The Smn protein is a central component of a complex that is necessary for assembly of spliceosomal snRNP particles (Pellizzoni 2007) and the regeneration of such particles in the nucleus. This so-called Smn complex has been characterized in much detail, the interaction partners of Smn called gemins have been identified, and the structural basis of the interaction and of the function of these components in the assembly of snRNP particles investigated. However, the Smn protein is also localized in axons (Rossoll et al. 2002) and axon terminals of motoneurons that are very distant from the cell body in which the assembly of spliceosomal snRNP particles normally occurs. This has led to the conclusions that, in addition to its role in the assembly of snRNP particles, the Smn protein could serve an additional function in RNA metabolism in axons and axon terminals (Sendtner 2001; Burghes and Beattie 2009).
In contrast to the human genome which contains two copies of SMN called SMN1 and SMN2, both of which are expressed, the mouse genome only contains one copy of the Smn gene. Conventional gene knockout of Smn in the mouse is embryonic lethal at early developmental stages (Schrank et al. 1997), before blastocysts form. This is consistent with an essential role of the Smn protein in the assembly of spliceosomes: Abolishing pre-mRNA splicing and nuclear processing is considered not to be compatible with life. Interestingly, when the SMN2 gene, which is still present in patients with this disease, is overexpressed on a Smn knockout background in mice (Monani et al. 2000), these mice develop to term and then show typical signs of the disease. The SMN1 and SMN2 genes differ only by five nucleotide exchanges (Wirth 2000), two of them within exons. A translationally silent cytosine to thymidine exchange at position 6 of exon 7 is responsible for the skipping of exon 7 in the majority of transcripts from the SMN2 gene. It has been shown that this mutation abolishes an exonic splice enhancer site (Cartegni and Krainer 2002) and generates a new exonic splicing silencer domain (Kashima and Manley 2003) for the last coding exon of the SMN2 gene. Therefore, at least 80 % of the resulting SMN protein from SMN2 transcripts lack the C-terminal 16 amino acids which are replaced by four amino acids encoded by exon 8 sequences. As a consequence, the corresponding protein is unstable (Cho and Dreyfuss 2010), the truncated SMN protein with altered C-terminus cannot self-associate, and thus it is less active in forming SMN complexes and probably also less active in a putative axonal function.
A large variety of animal models has been generated in which the consequences of Smn deficiency have been investigated (reviewed in Burghes and Beattie 2009). In all of these organisms, complete loss of Smn is lethal, and the time point of lethality depends on the levels of maternal Smn protein. For example, this explains why death in Smn-deficient Drosophila melanogaster (Chan et al. 2003) occurs later during development than in early mouse embryos. Interestingly, expression of a high number of SMN2 gene copies in Smn−/− mice completely reverses the phenotype (Monani et al. 2000). Such mice appear healthy, indicating that high expression of SMN2 can fully restore function.
Overexpression of Smn via the prion promoter only in the nervous system in mice with low Smn expression in non-neuronal tissues also has a major effect on survival of these animals (Gavrilina et al. 2008). Thus, low levels of functional Smn proteins produced from at least two copies of SMN2 gene are sufficient for normal function in most organs and cell types. Apparently, motoneurons need more SMN protein than other types of neurons and non-neuronal cell types, and this could explain why the disease expresses itself as a relatively pure motoneuron disease. Interestingly, efforts to restore Smn expression in muscle in mouse models with reduced Smn expression had much less effect than restoring Smn in neurons (Gavrilina et al. 2008). This correlates with observations that isolated motoneurons from Smn−/−SMN2tg mice already show a clear dysmorphic phenotype in cell culture (Rossoll et al. 2003). Survival of Smn-deficient motoneurons in cell culture is normal: No difference in neuronal numbers is observed in the presence or absence of neurotrophic factors when Smn−/−SMN2tg and control motoneurons are compared in culture. However, axon growth is altered (Rossoll et al. 2003). Within the first 3 days in culture, these motoneurons show normal axon growth, but further extension of the axons between day 3 and 7 is severely disturbed (Jablonka et al. 2007). Axonal growth cones are smaller, and a specific lack of actin protein is observed in axon terminals. This correlates with the finding that actin mRNA levels are highly reduced in axons of Smn-deficient motoneurons (Rossoll et al. 2003).
The Smn protein itself does not interact with specific mRNAs such as the β-actin mRNA. However, the Smn protein does not only bind to components of the classical Smn complex (Gubitz et al. 2004), but also with other proteins of the hnRNP family, in particular hnRNP-R (Rossoll et al. 2002; Mourelatos et al. 2001). There are also reports that the Smn protein interacts with TDP-43 (Wang et al. 2002) and also with the FUS protein (Yamazaki et al. 2012). However, in the case of TDP-43 and FUS, it is still not fully resolved whether these interactions occur directly in postnatal motoneurons, or whether the Smn interacts with hnRNP complexes containing TDP-43, FUS, and other members of the hnRNP family. Studies aimed at identifying TDP-43-binding partners in nuclear and cytosolic extracts point to the fact that the TDP-43 and FUS proteins are normally present in large protein complexes involving several members of the hnRNP family (Ling et al. 2010; Freibaum et al. 2010). Therefore, it is possible that Smn does not directly interact with each of these proteins, but with different preference to individual members of the hnRNP family. This needs further experimental analyses.
Smn and hnRNP-R proteins are co-localized in axons of motoneurons (Rossoll et al. 2002). The hnRNP-R protein is capable of directly interacting with the β-actin mRNA, and this interaction is reduced when the Smn-binding domain of hnRNP-R is deleted (Rossoll et al. 2003). The consequences of reduced interaction of Smn with hnRNP-R are not known. However, the observation that Smn-deficient motoneurons show reduced β-actin translocation into axons indicates that the Smn protein could play a role for axonal translocation of this and probably also other mRNAs into axons. Knockdown of hnRNP-R in isolated motoneurons or in zebrafish embryos (Glinka et al. 2010) leads to a similar phenotype as Smn deficiency. This points to an involvement of Smn in the formation and function of hnRNP complexes for axonal translocation of specific mRNAs. Whether Smn plays an essential role in the assembly of hnRNP complexes in the nucleus, in nuclear exports of such mRNA transport complexes, and in the translocation of these protein/mRNA complexes to axons, and whether it also has a role in regulating the translation of these mRNAs in the axon terminals, remains to be determined.
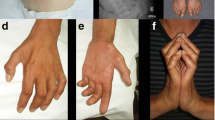
Reduced axon growth has also been observed in zebrafish embryos in which Smn has been knocked down by Morpholino technologies (McWhorter et al. 2003). Axons are shorter and many of them are truncated or branched, so that they do not reach their physiological target muscles. There is no evidence that axon growth is reduced in Smn-deficient mouse models in vivo (McGovern et al. 2008). However, motor axons grow out very early during embryonic development, and reduced speed of axon elongation could be compensated in vivo, so that even motoneurons with reduced axon growth rates in cell culture reach their target and make synaptic connections. Smn-deficient motoneurons in cell culture show altered growth behavior on laminin-β2/merosin (Jablonka et al. 2007). Wild-type motoneurons normally exhibit reduced axon growth on the synapse-specific form of laminin, but Smn-deficient motoneurons do not. This is due to altered distribution of CaV2.2 voltage-gated Ca2+ channels in axon terminals of Smn-deficient motoneurons (Fig. 1). The altered distribution of these voltage-gated Ca2+ channels correlates with altered excitability and altered Ca2+ influx after the initiation of action potentials in the cell body of Smn-deficient motoneurons (Jablonka et al. 2007). Only a small proportion of action potential-like depolarizations in isolated Smn-deficient motoneurons leads to Ca2+ transients in axon terminals of motoneurons from the SMA mouse model. These alterations predict defects in presynaptic function and neurotransmission at the neuromuscular endplates. Indeed, such defects are also observed in mouse models. Reduced folds at neuromuscular junctions have been observed in Smn-deficient mouse models during postnatal development, and neurotransmission at the synapses is also altered (Kong et al. 2009; Torres-Benito et al. 2012; Ruiz et al. 2010) (Fig. 1).
Axonal defects in Smn-deficient motoneurons. (a) Smn−/−SMN2tg motoneurons show defects in formation of presynaptic structures. They lack the accumulation of voltage-gated calcium channels (Cav2.2) in the tip of axonal growth cones where active zones form. This is also reflected by reduced colocalization with other proteins of the active zone, such as piccolo (green). Reproduced from Jablonka et al. (2007) (b) Diminished neuromuscular endplate currents (EPC) in tibialis anterior muscle of postnatal Smn-deficient (SMA) mice. The deficit in neurotransmission is caused by a deficit in release of synaptic vesicles. CL control; *P < 0.01. Reproduced from Kong et al. (2009)
Additional defects affecting excitability and neurotransmission have been discovered in Smn-deficient mouse and Drosophila models. In Smn-deficient mice, synaptic input to spinal motoneurons is reduced (Mentis et al. 2011), and the majority of the proprioceptive sensory afferents that normally make direct synaptic contact with spinal motoneurons are defective. It is still not clear whether this sensory defect is a consequence of altered excitablilty of motoneurons or reflects a primary defect in sensory neurons (Gogliotti et al. 2012). Such alterations in sensory afferent have also been observed in fly models. Smn deficiency in Drosophila melanogaster leads to aberrant splicing of stasimon in cholinergic sensory neurons and interneurons (Imlach et al. 2012; Lotti et al. 2012), due to severely impaired U12 splicing in Smn-deficient neurons, including neural cell types other than motoneurons. This leads to decreased excitation of motoneurons and thus possibly to malfunction and degeneration.
Taken together, the cellular basis of spinal muscular atrophy is complex. Smn deficiency on the one side could lead to altered splicing of gene products that are important for the function of neurons that project to motoneurons and are necessary for giving them excitatory signals. Furthermore, Smn deficiency in motoneurons could impair axon growth and presynaptic differentiation, resulting in impaired neurotransmission at neuromuscular endplates. In any case, therapy has to focus on restoration of Smn function, and this could be through increasing full-length Smn expression in neurons, i.e., through strategies that improve the inclusion of exon 7-encoded domains from the SMN2 gene, or in increasing promoter activity for the SMN2 gene with the aim to increase overall transcript levels of the Smn mRNA (Sendtner 2010). In addition, strategies to restore physiological innervation of motoneurons, motoneuron excitability, and neurotransmission at neuromuscular endplates appear essential. Such strategies could go beyond increasing the levels of functional Smn protein in motoneurons. Evidence for this has been given by depleting PTEN in Smn-deficient motoneurons in cell culture and in vivo in mouse models. PTEN depletion leads to a normalization of axon elongation, increases axonal growth cone size, and restores excitability of Smn-deficient motoneurons (Ning et al. 2010). These changes are associated with increased pAKT and p70S6 levels in Smn-deficient motor axons. This treatment also restores actin protein levels in axonal growth cones of Smn-deficient motoneurons. In vivo, the injection of siPTEN constructs in limb muscles of Smn-deficient motoneurons increases motoneuron survival (Ning et al. 2010). The hypothesis that defective actin cytoskeleton in axon terminals contributes to disease is also supported by genetic evidence in humans. Plastin-3, a protein that stabilizes filamentous actin, has been shown as modifier of SMA in patients (Oprea et al. 2008). This genetic observation in patients has recently been confirmed by a corresponding mouse model (Ackermann et al. 2013), and this opens perspectives for therapeutic strategies that stabilize the actin cytoskeleton in presynaptic compartments of neuromuscular endplates as another target for therapy development.
6 Developmental Motoneuron Cell Death
Neuronal cell death is often considered as a pathological feature, disregarding that many neurons undergo cell death during normal development. Although some observations on this phenomenon go back to the early twentieth century, it was the work of Viktor Hamburger (1934, 1975) and other pioneer researchers who discovered the principles and physiological meaning of this phenomenon. Spinal motoneurons played a central role in this discovery process. Viktor Hamburger and his colleagues showed that developmental motoneuron cell death is guided by influences provided from target tissue. Removal of limb buds in developing chick embryos enhances massively developmental motoneuron cell death and transplantation of an additional limb reduces the number of dying motoneurons. This kind of plasticity does not only allow the individual organism to react to deviations from genetically determined developmental programs, it also allows plasticity to generate an individual architecture of the nervous system in response to environmental cues, and thus might have contributed during evolution to the generation of a highly complex nervous system in higher vertebrates. On the other hand, the complex nature of such regulatory mechanisms also implies vulnerability and any disturbance of the regulatory processes theoretically could lead to pathological losses of neurons and neuronal function. Since the cloning of BDNF (Leibrock et al. 1989) and CNTF (Stockli et al. 1989) in 1989, a broad variety of neurotrophic factors were identified that can support motoneuron survival. At least three neurotrophins, brain derived neurotrophic factor, neurotrophin-4, and neurotrophin-3, but not NGF, support motoneuron survival. The CNTF/LIF family, which mediates pro-survival actions through a cytokine receptor involving LIFR-β and gp130, also includes several members, besides CNTF leukemia-inhibitory factor (LIF), cardiotrophin-1 (CT-1) (Pennica et al. 1996), and cardiotrophin-1-like cytokine (CLC) (Elson et al. 2000).
Survival of cultured motoneurons is also supported by members of the glial-derived neurotrophic factor (GDNF) gene families. Factors supporting motoneuron survival include GDNF (Henderson et al. 1994), neurturin (Klein et al. 1997), persephin (Milbrandt et al. 1998), and artemin (Baloh et al. 1998), and these molecules mediate their survival effects through C-Ret-tyrosine kinase and specific α-receptors. Motoneurons are also supported by insulin-like growth factor 1 and 2 (Arakawa et al. 1990). In cultures of isolated embryonic chick spinal motoneurons, the survival-promoting effect of IGF is relatively low. However, when IGFs are combined with other neurotrophic factors such as CNTF, this leads to supra-additive survival effects, indicating that neurotrophic factors potentate each other. The relatively low survival effect of IGF-1 on chick embryonic motoneurons could be due to cell culture conditions that include serum in culture medium with inhibitory insulin-like growth factor-binding proteins. Not very much is known on how insulin-like growth factor-binding proteins modulate the action of IGFs on motoneuron survival during development and in the adult.
Also other types of pluripotent growth factors support motoneuron survival such as members of the FGF family (Arakawa et al. 1990; Hughes et al. 1993a), members of the vascular endothelial growth factor (VEGF) family (Poesen et al. 2008; Azzouz et al. 2004; Carmeliet and Storkebaum 2002), or hepatocyte growth factor family (Yamamoto et al. 1997). HGF is a heterodimer protein with similarities to plasminogen. However, it lacks the enzymatic activity of plasminogen (Weidner et al. 1991). Interestingly, only lumbar motoneurons from 5-day-old chick embryos survive with HGF, but not motoneurons from thoracic or cervical spinal cord (Novak et al. 2000). In developing chick embryos, the c-met tyrosine kinase is expressed in lumbar but not in thoracic motoneurons between embryonic day 5 and 10 during the period of physiological motoneuron cell death. Additional experiments have shown that the expression of c-met in lumbar motoneurons seems to be regulated by target tissue-derived factors other than HGF. This was concluded from experiments showing that the massive cell death of motoneurons in the lumbar spinal cord after limb removal cannot be rescued by HGF treatment because the receptor was downregulated by target deprivation. HGF thus represents another neurotrophic factor that influences survival of only specific subpopulations of motoneurons and needs cooperation with other signals in order to exert a survival-promoting effect. Together with the observation that IGF acts in a supra-additive way with other factors on cultured motoneurons, this supports the conclusion that motoneuron survival during development is regulated by a complex orchestra of many factors that play together in supporting survival, presynaptic differentiation, and maturation of neuromuscular endplates, regulating preservation and stabilization of axons and by this way also the long-term functionality of these cells in the nervous system.
Such interactions are also observed experimentally after lesion in peripheral nerves. For example, when the facial nerve is transected in newborn rats, individual application of CNTF (Sendtner et al. 1990) or BDNF (Sendtner et al. 1992a) supports survival, but does not prevent atrophy of motoneuron cell bodies. Atrophy is significantly reduced when both factors are applied (Gravel et al. 1997). Not all of these factors that support survival of isolated embryonic motoneurons are also expressed in developing skeletal muscle. For example, CNTF is not expressed in muscle. The high expression found in adult mice is confined to myelinating Schwann cells, and expression of this factor only starts in the postnatal period in rodents when the period of physiological cell death is over. Similarly, only low quantities of BDNF are found in skeletal muscle (Hughes et al. 1993b). Levels of BDNF expression are much higher in Schwann cells after nerve lesion (Meyer et al. 1992). Gene knockout experiments have been performed and it has been shown that depletion of BDNF and/or NT-4 does not increase developmental cell death of motoneurons (Liu et al. 1995). The same is true in animal models lacking CNTF and/or LIF (Holtmann et al. 2005). Only in mouse models in which GDNF is depleted (Oppenheim et al. 2000) or cardiotrophin-1 (Oppenheim et al. 2001), subsets of motoneurons are lost during this physiological cell death period. Also these genetic data point to a collaboration of several neurotrophic factors in developmental maintenance and regulation of survival during the period of physiological cell death.
These data also show that Schwann cells play a role in motoneuron maintenance. Mice in which Schwann cell-derived CNTF and LIF are eliminated show progressive loss of motoneurons and of motoneuron functions, which correlates with loss of muscle strength in adult mice (Holtmann et al. 2005). Similarly, mice deficient for erb-B3, the receptor for glial growth factor (GGF), which exhibit severely disturbed development of Schwann cells, show as a consequence significant reduction (79 %) in motoneurons (Riethmacher et al. 1997). Thus, Schwann cells apparently do not only play a role as source of survival and maintenance factor in the adult peripheral nervous system, but apparently also during development. Developing Schwann cells either play a role in helping motoneurons to contact skeletal muscle and to become functionally active, which then leads to upregulation of neurotrophic support from skeletal muscle, or alternatively, they could provide trophic support in addition to that of motoneurons, and only those motoneurons that receive sufficient signals from developing Schwann cells and muscles are supported, and those that do not receive the support are eliminated. When limb buds are completely removed from chick embryos, motoneuron survival is severely impaired (Oppenheim 1985). Similar observation is made when only skeletal muscle is destroyed (Grieshammer et al. 1998), indicating that the remaining Schwann cells are not sufficient to support survival, and therefore, additional support from muscle is necessary.
7 Interactions of Neurotrophic Signaling with Pathomechanisms of Motoneuron Disease
The identification of underlying gene defects for most of the familial forms of spinal muscular atrophy and amyotrophic lateral sclerosis has pointed to a large variety of disease mechanisms. There are two major groups of pathomechanisms that have emerged: On the one side, dysfunctional RNA processing in spinal muscular atrophy and familial forms with mutations in TDP-43, FUS, and abnormal protein aggregates and dysfunctional signaling pathways for mitochondrial metabolisms due to mutations in the SOD-I genes and potentially also the c9Orf72 gene. These two groups of pathomechanisms do not exclude each other: TDP-43 C-terminal fragments are a major component of inclusions in most cases of ALS, including the majority of sporadic ALS. Axonal swellings containing protein aggregates and dysmorphic mitochondria are commonly found in motoneurons and also in mouse models of motoneuron disease such as pmn mutant mice (Bommel et al. 2002; Selvaraj et al. 2012) (Fig. 2). None of the gene products named above are directly connected to neurotrophic factors or their receptors. Therefore, deficiency of individual neurotrophic factors that lead to enhanced developmental cell death, i.e., in the case of CT-1, GDNF, or HGF, or progressive postnatal motoneuron loss after depletion of CNTF, LIF, or IGF-1, apparently does not seem to be a primary cause of motoneuron disease, at least on a genetic level. Nevertheless, the signaling pathways exerted downstream from receptor for neurotrophic factors for motoneuron survival, for axon maintenance and regeneration, and for presynaptic function and stabilization of neuromuscular endplates apparently seem to be disturbed are not fully functional in motoneuron disease, and several possibilities exist that need to be considered.
Axonal swellings in isolated motoneurons from progressive motor neuropathy (pmn) mutant mice. Based on a mutation in the TBCE gene (Bommel et al. 2002) motoneurons develop axonal swellings containing protein aggregates and dysmorphic mitochondria. Scale bar: 1,000 nm
First, neurotrophic factors could play a role in compensating for neurodegeneration of spinal motoneurons by promoting sprouting. The central role of neurotrophic factors in axonal and terminal sprouting has been known for a long time (Caroni 1997). Indeed, in a mouse model of a mild form of spinal muscular atrophy, Smn+/− mice that exhibit a reduction of Smn protein by only 50 % and thus resemble mild forms of spinal muscular atrophy in humans do not show an overt phenotype (Simon et al. 2010). Nevertheless, there is progressive loss of motoneurons that reaches more than 50 % at an age of 1 year in this mouse model. For comparison, Smn−/−SMN2tg mice, the mouse model for the severe form of SMA type I only exhibits a loss of about 20 % above control (Monani et al. 2000) when mice are terminally sick and completely paralyzed early after birth. This indicates that loss of motor function does not necessarily correlate with the loss of motoneurons, in particular not in cases with slowly progressive forms of motoneuron disease that allow remaining motoneurons to sprout and compensate for lost neurons by reinnervating denervated skeletal muscle fibers. Indeed, massive sprouting occurs in Smn+/− mice and this explains the lack of any loss of muscle strength in these mice. Electrophysiological analysis shows an increase of motor units by a factor of at least 2, and morphological analysis provides evidence for massive sprouting, including terminal sprouting and axonal sprouting to reinnervate neuromuscular endplates in different muscle groups. This type of sprouting depends on neurotrophic factors provided from myelinating Schwann cells, in particular CNTF. When these Smn+/− mice are crossbred with CNTF-deficient mice, sprouting does not occur, and the compensatory increase in motor unit size detected by electromyographical analysis is also not found. Thus, neurotrophic signaling could help to compensate for loss of motoneuron function over prolonged periods, and it is possible that this contributes to the observation that most forms of ALS only become apparent at higher age.
This is also suggested by experiments when SOD-1 G93A mice are crossbred with CNTF-deficient mice (Giess et al. 2002) (Fig. 3). When CNTF is lacking, disease onset occurs earlier, providing evidence that this and probably also other factors contribute to plasticity that helps animal models or individuals with SOD-I gene defects to maintain motor function before disease finally becomes apparent. Also in patients with ALS, the presence or absence of CNTF seems to play a role. Due to an abundant polymorphism in the splice acceptor site of exon 2 of the CNTF gene, about 2 % of the population worldwide is homozygous CNTF deficient and express only a truncated CNTF protein without function. Average disease onset in such patients is at least 10 years earlier, and in one family with an SOD-I mutation, the additional homozygous deletion of CNTF leads to very early disease onset, whereas other members of the same family with the same SOD-I mutation develop the disease only 20 years later (Giess et al. 2002).
Modifier effect of CNTF in a family with fALS patients (SOD V148G) and in SOD G93A tg mice: (a) A family with autosomal-dominant ALS with SOD-I V148G mutation showed highly variable disease onset, ranging from 25 to 56 years. Search for candidate modifier gene defects revealed a homozygous CNTF null mutation in the patient with early onset at 25 years. (b) Depletion of CNTF from SOD G93A mice confirms that CNTF deficiency leads to earlier disease onset in mice. Reproduced from (Giess et al. 2002)
The question is open as to which parameters determine the time point when compensation is lost and disease becomes apparent. In SOD-I mutant mice, depletion of synaptic vesicles in presynaptic motor terminals at neuromuscular junctions precedes the loss of presynaptic branches (Pun et al. 2006) and the progressive degeneration of the motoneurons. Interestingly, when CNTF was injected, the depletion of synaptic vesicles and pruning of nerve terminals are delayed. Even more interestingly, the injection of the neurotrophic factor GDNF was without effect in this context. This is interesting insofar as both CNTF and GDNF are potent survival factors for developing motoneurons, but apparently, they seem to differ with respect to their function in maintaining nerve terminals.
Such differences between different groups of neurotrophic factors have also been observed in other mouse models of motoneuron disease. For example, in pmn mutant mice, which develop a motoneuron disease on the basis of a gene defect in tubulin-specific chaperone-E gene (Bommel et al. 2002), CNTF can delay disease onset and prolong survival (Sendtner et al. 1992b), whereas treatment with GDNF (Sagot et al. 1996a) or BDNF cannot. The mutation in the TBCE gene leads to instability of microtubules that correspond to defective axon growth in isolated pmn mutant motoneurons in cell culture (Fig. 4).
CNTF rescues defective axon elongation in pmn mutant motoneurons (Bommel et al. 2002; Selvaraj et al. 2012; Sendtner et al. 1992b): Wild-type and pmn mutant motoneurons were cultured for 5 days in the presence of BDNF or BDNF+CNTF and stained with alpha-tubulin. Pmn mutant motoneurons cultured with BDNF have shorter axons when compared to wild-type controls. CNTF application restores axon elongation in pmn mutant motoneurons. Scale bar: 100 μm
Survival of pmn mutant motoneurons is primarily not affected, but axons are shorter and exhibit swellings that contain dysmorphic filaments and accumulations of mitochondria (Fig. 2). Microtubule stability is altered in pmn mutant motoneurons (Selvaraj et al. 2012): There is an increase of tyrosinated highly dynamic microtubules, and this correlates with reduced axonal transport of mitochondria. Interestingly, CNTF, but not GDNF or BDNF, can rescue this axonal phenotype. The CNTF effect is mediated by the activation of STAT-3, which exerts a local, non-transcriptional function in the axon via interaction with Stathmin, a microtubule-destabilizing protein. Destabilization of microtubules in cultured motoneurons shows that the capacity to regrow microtubules is highly reduced in isolated motoneurons from this mouse model of motoneuron disease and that CNTF treatment can help pmn mutant motoneurons to regrow stable microtubules (Fig. 5). Similarly, Stathmin knockdown also rescues the phenotype. Stabilization of microtubules with Taxol has a similar effect. Treatment of pmn mutant mice with CNTF delays disease onset (Sendtner et al. 1992b), but transgenic overexpression of bcl-2 (Sagot et al. 1996b) or treatment with GDNF only rescues cell bodies without any effect on axons, and the consequence is that onset and course of the disease are not altered by bcl-2 overexpression or GDNF treatment. Thus, the local effect of neurotrophic signaling on axon stability, in the case of CNTF, via STAT-3 and Stathmin seems to be more important for modulating disease than the classical neurotrophic signaling pathways for neuronal survival, and it is possible that similar effects are also contributing to the modulatory effect of CNTF in fALS with mutations in the SOD-I gene.
CNTF promotes microtubule polymerization: Primary motoneurons isolated from wild-type and pmn mutant embryos were treated with nocodazole for 6 h to depolymerize the microtubule network. Nocodazole was washed out and microtubule regrowth was analyzed at 5 min after CNTF application. Polymerized microtubules were labeled with antibodies against α-tubulin (red) and microtubule organization center was labeled with antibodies against γ-tubulin (green). Number of microtubules and length of microtubules formed in pmn mutant motoneurons were significantly less when compared to wild-type motoneurons. Application of CNTF increased the number of microtubules and length of microtubules formed in pmn mutant motoneurons (Selvaraj et al. 2012). Scale bar: 2 μm
Some neurotrophic factors, in particular members of the neurotrophin family and their receptors, could also mediate additional effects via the p75 neurotrophin receptor (p75NTR). This transmembrane protein shares structural and functional similarities with other transmembrane molecules of the FAS/APO-1 CD95 and TNF-receptor-1 family (Chao 2003). In a variety of cellular contexts in vitro and in vivo, p75NTR mediates cell death after binding of neurotrophins and in particular pro-neurotrophins, in particular when Trk receptors are not expressed, and binding of pro-neurotrophins to p75NTR has been shown in a variety of physiological contexts to destabilize neurites and cause neuronal cell death. Injection of neutralizing antibodies against p75NTR into the eye of early chick embryos has shown that early developmental cell death of retinal ganglion cells can be mediated through this receptor (Frade et al. 1996). Some mediators of p75NTR signaling also specifically destabilize axons (Plachta et al. 2007). Activation of p75NTR upregulates expression of the sugar-binding protein galectin-1. Increased amounts of galectin-1 destroy neuronal processes, both in cell culture and in vivo. The p75NTR receptor is highly upregulated in degenerating motoneurons in ALS (Kerkhoff et al. 1991; Seeburger et al. 1993), and it is likely that activation of this receptor contributes to the degenerative effects, in particular pruning of neuromuscular synapses and degeneration of neural processes (Singh et al. 2008).
In summary, neurotrophic factors modulate motoneuron disease on several levels. On the one side, they play a role in compensating the loss of motoneurons at early stages by sprouting, by stabilizing neuromuscular synapses, by stabilizing axons, and also by acting on motoneuron survival. On the other side, p75NTR signaling could contribute to degenerative mechanisms responsible for denervation of neuromuscular endplates and axon destruction, possibly even motoneuron cell death at later stages of disease. This offers many options how neurotrophic factors and their signaling pathways could be used as targets for therapy. So far, clinical trials with CNTF, IGF-1, and BDNF have not been successful in motoneuron disease (Thoenen and Sendtner 2002), but this is mainly due to side effects in the case of CNTF and adverse pharmacokinetic properties in the case of BDNF and possible also IGF-1. Future developments to overcome these problems could help to develop new therapies for motoneuron disease. Similarly, approaches that inhibit potential destructive signaling through p75NTR could also be of benefit for treatment of motoneuron disease. These strategies could be even more efficient when combined with therapies aiming at counteracting the consequences of primary causes of motoneuron disease, such as Smn deficiency in spinal muscular atrophy, or of altered TDP-43, Fus, or C9orf72 processing in familial or sporadic forms of motoneuron disease.
References
Ackermann B et al (2013) Plastin 3 ameliorates spinal muscular atrophy via delayed axon pruning and improves neuromuscular junction functionality. Hum Mol Genet 22(7):1328–1347
Al-Chalabi A et al (2012) The genetics and neuropathology of amyotrophic lateral sclerosis. Acta Neuropathol 124:339–352
Al-Sarraj S et al (2011) p62 positive, TDP-43 negative, neuronal cytoplasmic and intranuclear inclusions in the cerebellum and hippocampus define the pathology of C9orf72-linked FTLD and MND/ALS. Acta Neuropathol 122:691–702
Andersen PM, Al-Chalabi A (2011) Clinical genetics of amyotrophic lateral sclerosis: what do we really know? Nat Rev Neurol 7:603–615
Arakawa Y, Sendtner M, Thoenen H (1990) Survival effect of ciliary neurotrophic factor (CNTF) on chick embryonic motoneurons in culture: comparison with other neurotrophic factors and cytokines. J Neurosci 10:3507–3515
Ash PE et al (2013) Unconventional translation of C9ORF72 GGGGCC expansion generates insoluble polypeptides specific to c9FTD/ALS. Neuron 77(4):639–646
Ashley CT Jr, Wilkinson KD, Reines D, Warren ST (1993) FMR1 protein: conserved RNP family domains and selective RNA binding. Science 262:563–566
Ayala YM, Misteli T, Baralle FE (2008) TDP-43 regulates retinoblastoma protein phosphorylation through the repression of cyclin-dependent kinase 6 expression. Proc Natl Acad Sci U S A 105:3785–3789
Azzouz M et al (2004) VEGF delivery with retrogradely transported lentivector prolongs survival in a mouse ALS model. Nature 429:413–417, 1995 Sep 28; 377(6547):340–344
Baloh RH et al (1998) Artemin, a novel member of the GDNF ligand family, supports peripheral and central neurons and signals through the GFRalpha3-RET receptor complex. Neuron 21:1291–1302
Boillee S et al (2006) Onset and progression in inherited ALS determined by motor neurons and microglia. Science 312:1389–1392
Bommel H et al (2002) Missense mutation in the tubulin-specific chaperone E (Tbce) gene in the mouse mutant progressive motor neuronopathy, a model of human motoneuron disease. J Cell Biol 159:563–569
Buratti E, Baralle FE (2001) Characterization and functional implications of the RNA binding properties of nuclear factor TDP-43, a novel splicing regulator of CFTR exon 9. J Biol Chem 276:36337–36343
Buratti E, Baralle FE (2010) TDP-43 regulates its mRNA levels through a negative feedback loop. EMBO J 30:277–288
Buratti E, Baralle FE (2008) Multiple roles of TDP-43 in gene expression, splicing regulation, and human disease. Front Biosci 13:867–878
Buratti E, Baralle FE (2010a) The multiple roles of TDP-43 in pre-mRNA processing and gene expression regulation. RNA Biol 7(4):420–429
Buratti E, Baralle FE (2010b) TDP-43 regulates its mRNA levels through a negative feedback loop. EMBO J 30: 277–288
Buratti E et al (2001) Nuclear factor TDP-43 and SR proteins promote in vitro and in vivo CFTR exon 9 skipping. EMBO J 20:1774–1784
Buratti E et al (2005) TDP-43 binds heterogeneous nuclear ribonucleoprotein A/B through its C-terminal tail: an important region for the inhibition of cystic fibrosis transmembrane conductance regulator exon 9 splicing. J Biol Chem 280:37572–37584
Burghes AH, Beattie CE (2009) Spinal muscular atrophy: why do low levels of survival motor neuron protein make motor neurons sick? Nat Rev Neurosci 10:597–609
Carmeliet P, Storkebaum E (2002) Vascular and neuronal effects of VEGF in the nervous system: implications for neurological disorders. Semin Cell Dev Biol 13:39–53
Caroni P (1997) Intrinsic neuronal determinants that promote axonal sprouting and elongation. Bioessays 19:767–775
Cartegni L, Krainer AR (2002) Disruption of an SF2/ASF-dependent exonic splicing enhancer in SMN2 causes spinal muscular atrophy in the absence of SMN1. Nat Genet 30:377–384
Chan YB et al (2003) Neuromuscular defects in a Drosophila survival motor neuron gene mutant. Hum Mol Genet 12:1367–1376
Chao MV (2003) Neurotrophins and their receptors: a convergence point for many signalling pathways. Nat Rev Neurosci 4:299–309
Chen YZ et al (2004) DNA/RNA helicase gene mutations in a form of juvenile amyotrophic lateral sclerosis (ALS4). Am J Hum Genet 74(6):1128–1135
Cho S, Dreyfuss G (2010) A degron created by SMN2 exon 7 skipping is a principal contributor to spinal muscular atrophy severity. Genes Dev 24:438–442
Chow CY et al (2009) Deleterious variants of FIG4, a phosphoinositide phosphatase, in patients with ALS. Am J Hum Genet 84(1):85–88
Clement AM et al (2003) Wild-type nonneuronal cells extend survival of SOD1 mutant motor neurons in ALS mice. Science 302:113–117
Colombrita C et al (2009) TDP-43 is recruited to stress granules in conditions of oxidative insult. J Neurochem 111:1051–1061
Crawford TO, Pardo CA (1996) The neurobiology of childhood spinal muscular atrophy. Neurobiol Dis 3:97–110
Damiano M et al (2006) Neural mitochondrial Ca2+ capacity impairment precedes the onset of motor symptoms in G93A Cu/Zn-superoxide dismutase mutant mice. J Neurochem 96:1349–1361
De Vos KJ et al (2007) Familial amyotrophic lateral sclerosis-linked SOD1 mutants perturb fast axonal transport to reduce axonal mitochondria content. Hum Mol Genet 16:2720–2728
DeJesus-Hernandez M et al (2011) Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron 72:245–256
Deng HX et al (2011) Mutations in UBQLN2 cause dominant X-linked juvenile and adult-onset ALS and ALS/dementia. Nature 477(7363):211–215
Dewey CM et al (2011) TDP-43 is directed to stress granules by sorbitol, a novel physiological osmotic and oxidative stressor. Mol Cell Biol 31:1098–1108
Di Giorgio FP, Boulting GL, Bobrowicz S, Eggan KC (2008) Human embryonic stem cell-derived motor neurons are sensitive to the toxic effect of glial cells carrying an ALS-causing mutation. Cell Stem Cell 3:637–648
Dormann D et al (2010) ALS-associated fused in sarcoma (FUS) mutations disrupt Transportin-mediated nuclear import. EMBO J 29:2841–2857
Drepper C, Sendtner M (2011) A new postal code for dendritic mRNA transport in neurons. EMBO Rep 12:614–616
Drepper C, Herrmann T, Wessig C, Beck M, Sendtner M (2011) C-terminal FUS/TLS mutations in familial and sporadic ALS in Germany. Neurobiol Aging 32(3):548.e1–4
Durham HD, Roy J, Dong L, Figlewicz DA (1997) Aggregation of mutant Cu/Zn superoxide dismutase proteins in a culture model of ALS. J Neuropathol Exp Neurol 56:523–530
Elden AC et al (2010) Ataxin-2 intermediate-length polyglutamine expansions are associated with increased risk for ALS. Nature 466(7310):1069–1075
Elson GC et al (2000) CLF associates with CLC to form a functional heteromeric ligand for the CNTF receptor complex. Nat Neurosci 3:867–872
Ferraiuolo L, Kirby J, Grierson AJ, Sendtner M, Shaw PJ (2011) Molecular pathways of motor neuron injury in amyotrophic lateral sclerosis. Nat Rev Neurol 7:616–630
Fiesel FC et al (2010) Knockdown of transactive response DNA-binding protein (TDP-43) downregulates histone deacetylase 6. EMBO J 29:209–221
Fiesel FC, Schurr C, Weber SS, Kahle PJ (2011) TDP-43 knockdown impairs neurite outgrowth dependent on its target histone deacetylase 6. Mol Neurodegener 6:64
Frade JM, RodriguezTebar A, Barde YA (1996) Induction of cell death by endogenous nerve growth factor through its p75 receptor. Nature 383:166–168
Fratta P et al (2012) C9orf72 hexanucleotide repeat associated with amyotrophic lateral sclerosis and frontotemporal dementia forms RNA G-quadruplexes. Sci Rep 2:1016
Freibaum BD, Chitta RK, High AA, Taylor JP (2010) Global analysis of TDP-43 interacting proteins reveals strong association with RNA splicing and translation machinery. J Proteome Res 9:1104–1120
Friedlander RM, Brown RH, Gagliardini V, Wang J, Yuan J (1997) Inhibition of ICE slows ALS in mice. Nature 388:31
Gavrilina TO et al (2008) Neuronal SMN expression corrects spinal muscular atrophy in severe SMA mice while muscle-specific SMN expression has no phenotypic effect. Hum Mol Genet 17:1063–1075
Giess R et al (2002) Early onset of severe familial amyotrophic lateral sclerosis with a SOD-1 mutation: potential impact of CNTF as a candidate modifier gene. Am J Hum Genet 70:1277–1286
Glinka M et al (2010) The heterogeneous nuclear ribonucleoprotein-R is necessary for axonal beta-actin mRNA translocation in spinal motor neurons. Hum Mol Genet 19:1951–1966
Gogliotti RG et al (2012) Motor neuron rescue in spinal muscular atrophy mice demonstrates that sensory-motor defects are a consequence, not a cause, of motor neuron dysfunction. J Neurosci 32:3818–3829
Gravel C, Götz R, Lorrain A, Sendtner M (1997) Adenoviral gene transfer of ciliary neurotrophic factor and brain-derived neurotrophic factor leads to longterm survival of axotomized motoneurons. Nat Med 3:765–770
Greenway MJ et al (2006) ANG mutations segregate with familial and ‘sporadic’ amyotrophic lateral sclerosis. Nat Genet 38(4):411–413
Grieshammer U et al (1998) Muscle-specific cell ablation conditional upon Cre-mediated DNA recombination in transgenic mice leads to massive spinal and cranial motoneuron loss Neuronal cell death. Neuron 20:633–647
Grosskreutz J, Van Den Bosch L, Keller BU (2010) Calcium dysregulation in amyotrophic lateral sclerosis. Cell Calcium 47:165–174
Gubitz AK, Feng W, Dreyfuss G (2004) The SMN complex. Exp Cell Res 296:51–56
Gurney ME et al (1994) Motor neuron degeneration in mice that express a human Cu, Zn superoxide dismutase mutation. Science 264:1772–1775
Hadano S et al (2001) A gene encoding a putative GTPase regulator is mutated in familial amyotrophic lateral sclerosis 2. Nat Genet 29(2):166–173
Hamburger V (1934) The effects of wing bud extirpation on the development of the central nervous system in chick embryos. J Exp Zool 68:449–494
Hamburger V (1975) Cell death in the development of the lateral column of the chick embryo. J Comp Neurol 160:535–546
Hand CK et al (2002) A novel locus for familial amyotrophic lateral sclerosis, on chromosome 18q. Am J Hum Genet 70(1):251–256
Haramati S et al (2010) miRNA malfunction causes spinal motor neuron disease. Proc Natl Acad Sci U S A 107:13111–13116
Harraz MM et al (2008) SOD1 mutations disrupt redox-sensitive Rac regulation of NADPH oxidase in a familial ALS model. J Clin Invest 118:659–670
Hausmanowa-Petrusewicz I (1978) In: Spinal muscular atrophy: infantile and juvenile type. National Library of Medicine & The National Science Foundation, Washington DC
Henderson CE et al (1994) GDNF: a potent survival factor for motoneurons present in peripheral nerve and muscle. Science 266:1062–1064
Higashi S et al (2007) Concurrence of TDP-43, tau and alpha-synuclein pathology in brains of Alzheimer’s disease and dementia with Lewy bodies. Brain Res 1184:284–294
Holtmann B et al (2005) Triple knock-out of CNTF, LIF, and CT-1 defines cooperative and distinct roles of these neurotrophic factors for motoneuron maintenance and function. J Neurosci 25:1778–1787
Hu F et al (2010) Sortilin-mediated endocytosis determines levels of the frontotemporal dementia protein, progranulin. Neuron 68:654–667
Hughes RA, Sendtner M, Goldfarb M, Lindholm D, Thoenen H (1993a) Evidence that fibroblast growth factor 5 is a major muscle derived survival factor for cultured spinal motoneurons. Neuron 10:369–377
Hughes RA, Sendtner M, Thoenen H (1993b) Members of several gene families influence survival of rat motoneurons in vitro and in vivo. J Neurosci Res 36(6):663–671
Imlach WL et al (2012) SMN is required for sensory-motor circuit function in Drosophila. Cell 151:427–439
Ito D, Seki M, Tsunoda Y, Uchiyama H, Suzuki N (2011) Nuclear transport impairment of amyotrophic lateral sclerosis-linked mutations in FUS/TLS. Ann Neurol 69:152–162
Jablonka S, Beck M, Lechner BD, Mayer C, Sendtner M (2007) Defective Ca2+ channel clustering in axon terminals disturbs excitability in motoneurons in spinal muscular atrophy. J Cell Biol 179:139–149
Johnson JO et al (2010) Exome sequencing reveals VCP mutations as a cause of familial ALS. Neuron 68(5):857–864
Kabashi E et al (2008) TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat Genet 40(5):572–574
Kashima T, Manley JL (2003) A negative element in SMN2 exon 7 inhibits splicing in spinal muscular atrophy. Nat Genet 34:460–463
Kerkhoff H, Jennekens FGI, Troost D, Veldman H (1991) Nerve growth factor receptor immunostaining in the spinal cord and peripheral nerves in amyotrophic lateral sclerosis. Acta Neuropathol (Berl) 81:649–656
Kiebler MA, Bassell GJ (2006) Neuronal RNA granules: movers and makers. Neuron 51:685–690
Kiernan MC et al (2011) Amyotrophic lateral sclerosis. Lancet 377:942–955
Klein RD et al (1997) A GPI-linked protein that interacts with Ret to form a candidate neurturin receptor. Nature 387:717–721
Kong L et al (2009) Impaired synaptic vesicle release and immaturity of neuromuscular junctions in spinal muscular atrophy mice. J Neurosci 29:842–851
Kostic V, Jackson-Lewis V, de Bilbao F, Dubois-Dauphin M, Przedborski S (1997) Bcl-2: prolonging life in a transgenic mouse model of familial amyotrophic lateral sclerosis. Science 277:559–562
Krecic AM, Swanson MS (1999) hnRNP complexes: composition, structure, and function. Curr Opin Cell Biol 11:363–371
Kuroda M et al (2000) Male sterility and enhanced radiation sensitivity in TLS(-/-) mice. EMBO J 19:453–462
Kwiatkowski TJ Jr et al (2009) Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science 323:1205–1208
Leibrock J et al (1989) Molecular cloning and expression of brain-derived neurotrophic factor. Nature 341:149–152
Ling SC et al (2010) ALS-associated mutations in TDP-43 increase its stability and promote TDP-43 complexes with FUS/TLS. Proc Natl Acad Sci U S A 107:13318–13323
Liu X, Ernfors P, Wu H, Jaenisch R (1995) Sensory but not motor neuron deficits in mice lacking NT4 and BDNF. Nature 375:238–241
Lotti F et al (2012) An SMN-dependent U12 splicing event essential for motor circuit function. Cell 151:440–454
Luty AA et al (2010) Sigma nonopioid intracellular receptor 1 mutations cause frontotemporal lobar degeneration-motor neuron disease. Ann Neurol 68(5):639–649
Mackenzie IRA, Rademakers R, Neumann M (2010) TDP-43 and FUS in amyotrophic lateral sclerosis and frontotemporal dementia. Lancet Neurol 9:995–1007
Maekawa S et al (2009) TDP-43 is consistently co-localized with ubiquitinated inclusions in sporadic and Guam amyotrophic lateral sclerosis but not in familial amyotrophic lateral sclerosis with and without SOD1 mutations. Neuropathology 29:672–683
Maruyama H et al (2010) Mutations of optineurin in amyotrophic lateral sclerosis. Nature 465(7295):223–226
McDonald KK et al (2011) TAR DNA-binding protein 43 (TDP-43) regulates stress granule dynamics via differential regulation of G3BP and TIA-1. Hum Mol Genet 20:1400–1410
McGovern VL, Gavrilina TO, Beattie CE, Burghes AH (2008) Embryonic motor axon development in the severe SMA mouse. Hum Mol Genet 17:2900–2909
McWhorter ML, Monani UR, Burghes AH, Beattie CE (2003) Knockdown of the survival motor neuron (Smn) protein in zebrafish causes defects in motor axon outgrowth and pathfinding. J Cell Biol 162:919–931
Mentis GZ et al (2011) Early functional impairment of sensory-motor connectivity in a mouse model of spinal muscular atrophy. Neuron 69:453–467
Meyer M, Matsuoka I, Wetmore C, Olson L, Thoenen H (1992) Enhanced synthesis of brain-derived neurotrophic factor in the lesioned peripheral nerve: different mechanisms are responsible for the regulation of BDNF and NGF mRNA. J Cell Biol 119:45–54
Milbrandt J et al (1998) Persephin, a novel neurotrophic factor related to GDNF and neurturin. Neuron 20:245–253
Moisse K et al (2009a) Divergent patterns of cytosolic TDP-43 and neuronal progranulin expression following axotomy: implications for TDP-43 in the physiological response to neuronal injury. Brain Res 1249:202–211
Moisse K et al (2009b) Cytosolic TDP-43 expression following axotomy is associated with caspase 3 activation in NFL-/- mice: support for a role for TDP-43 in the physiological response to neuronal injury. Brain Res 1296:176–186
Monani UR et al (2000) The human centromeric survival motor neuron gene (SMN2) rescues embryonic lethality in Smn(-/-) mice and results in a mouse with spinal muscular atrophy [In Process Citation]. Hum Mol Genet 9:333–339
Mori K et al (2013a) hnRNP A3 binds to GGGGCC repeats and is a constituent of p62-positive/TDP43-negative inclusions in the hippocampus of patients with C9orf72 mutations. Acta Neuropathol 125(3):413–423
Mori K et al (2013b) The C9orf72 GGGGCC repeat is translated into aggregating dipeptide-repeat proteins in FTLD/ALS. Science 339(6125):1335–1338
Morlando M et al (2012) FUS stimulates microRNA biogenesis by facilitating co-transcriptional Drosha recruitment. EMBO J 31:4502–4510
Mourelatos Z, Abel L, Yong J, Kataoka N, Dreyfuss G (2001) SMN interacts with a novel family of hnRNP and spliceosomal proteins. EMBO J 20:5443–5452
Nagai M et al (2007) Astrocytes expressing ALS-linked mutated SOD1 release factors selectively toxic to motor neurons. Nat Neurosci 10:615–622
Neumann M et al (2006) Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science 314:130–133
Ning K et al (2010) PTEN depletion rescues axonal growth defect and improves survival in SMN-deficient motor neurons. Hum Mol Genet 19:3159–3168
Nishihira Y et al (2009) Sporadic amyotrophic lateral sclerosis of long duration is associated with relatively mild TDP-43 pathology. Acta Neuropathol 117:45–53
Nishimura AL et al (2004) A mutation in the vesicle-trafficking protein VAPB causes late-onset spinal muscular atrophy and amyotrophic lateral sclerosis. Am J Hum Genet 75(5):822–831
Novak KD, Prevette D, Wang S, Gould TW, Oppenheim RW (2000) Hepatocyte growth factor/scatter factor is a neurotrophic survival factor for lumbar but not for other somatic motoneurons in the chick embryo. J Neurosci 20:326–337
Oppenheim RW (1985) Naturally occuring cell death during neural development. Trends Neurosci 8:487–493
Oppenheim RW et al (2000) Glial cell line-derived neurotrophic factor and developing mammalian motoneurons: regulation of programmed cell death among motoneuron subtypes. J Neurosci 20:5001–5011
Oppenheim RW et al (2001) Cardiotrophin-1, a muscle-derived cytokine, is required for the survival of subpopulations of developing motoneurons. J Neurosci 21:1283–1291
Oprea GE et al (2008) Plastin 3 is a protective modifier of autosomal recessive spinal muscular atrophy. Science 320:524–527
Orlacchio A et al (2010) SPATACSIN mutations cause autosomal recessive juvenile amyotrophic lateral sclerosis. Brain 133(Pt 2):591–598
Parkinson N et al (2006) ALS phenotypes with mutations in CHMP2B (charged multivesicular body protein 2B). Neurology 67(6):1074–1077
Pascale A, Govoni S (2012) The complex world of post-transcriptional mechanisms: is their deregulation a common link for diseases? Focus on ELAV-like RNA-binding proteins. Cell Mol Life Sci 69:501–517
Pasinelli P et al (2004) Amyotrophic lateral sclerosis-associated SOD1 mutant proteins bind and aggregate with Bcl-2 in spinal cord mitochondria. Neuron 43:19–30
Pellizzoni L (2007) Chaperoning ribonucleoprotein biogenesis in health and disease. EMBO Rep 8:340–345
Pennica D et al (1996) Cardiotrophin-1, a cytokine present in embryonic muscle, supports long-term survival of spinal motoneurons. Neuron 17:63–74
Pesiridis GS, Lee VM, Trojanowski JQ (2009) Mutations in TDP-43 link glycine-rich domain functions to amyotrophic lateral sclerosis. Hum Mol Genet 18:R156–R162
Pesiridis GS, Tripathy K, Tanik S, Trojanowski JQ, Lee VM (2011) A “two-hit” hypothesis for inclusion formation by carboxyl-terminal fragments of TDP-43 protein linked to RNA depletion and impaired microtubule-dependent transport. J Biol Chem 286:18845–18855
Plachta N et al (2007) Identification of a lectin causing the degeneration of neuronal processes using engineered embryonic stem cells. Nat Neurosci 10:712–719
Poesen K et al (2008) Novel role for vascular endothelial growth factor (VEGF) receptor-1 and its ligand VEGF-B in motor neuron degeneration. J Neurosci 28:10451–10459
Polymenidou M et al (2011) Long pre-mRNA depletion and RNA missplicing contribute to neuronal vulnerability from loss of TDP-43. Nat Neurosci 14(4):459–468
Pun S, Santos AF, Saxena S, Xu L, Caroni P (2006) Selective vulnerability and pruning of phasic motoneuron axons in motoneuron disease alleviated by CNTF. Nat Neurosci 9:408–419
Rayaprolu S et al (2012) Angiogenin variation and Parkinson disease. Ann Neurol 71(5):725–727; author reply 727–728
Reaume AG et al (1996) Motor neurons in Cu/Zn superoxide dismutase-deficient mice develop normally but exhibit enhanced cell death after axonal injury. Nat Genet 13:43–47
Renton AE et al (2011) A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron 72:257–268
Riethmacher D et al (1997) Severe neuropathies in mice with targeted mutations in the ErbB3 receptor. Nature 389:725–730
Rosen DR et al (1993) Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature 362:59–62
Rossoll W et al (2002) Specific interaction of Smn, the spinal muscular atrophy determining gene product, with hnRNP-R and gry-rbp/hnRNP-Q: a role for Smn in RNA processing in motor axons? Hum Mol Genet 11:93–105
Rossoll W et al (2003) Smn, the spinal muscular atrophy-determining gene product, modulates axon growth and localization of beta-actin mRNA in growth cones of motoneurons. J Cell Biol 163:801–812
Ruiz R, Casanas JJ, Torres-Benito L, Cano R, Tabares L (2010) Altered intracellular Ca2+ homeostasis in nerve terminals of severe spinal muscular atrophy mice. J Neurosci 30:849–857
Rutherford NJ et al (2008) Novel mutations in TARDBP (TDP-43) in patients with familial amyotrophic lateral sclerosis. PLoS Genet 4:e1000193
Sagot Y, Tan SA, Hammang JP, Aebischer P, Kato AC (1996a) GDNF slows loss of motoneurons but not axonal degeneration or premature death of pmn/pmn mice. J Neurosci 16:2335–2341
Sagot Y et al (1996b) Bcl-2 overexpression prevents motoneuron cell body loss but not axonal degeneration in a mouse model of a neurodegenerative disease. J Neurosci 11:7727–7733
Sapp PC et al (2003) Identification of two novel loci for dominantly inherited familial amyotrophic lateral sclerosis. Am J Hum Genet 73(2):397–403
Schrank B et al (1997) Inactivation of the survival motor neuron gene, a candidate gene for human spinal muscular atrophy, leads to massive cell death in early mouse embryos. Proc Natl Acad Sci U S A 94:9920–9925
Schwab C, Arai T, Hasegawa M, Yu S, McGeer PL (2008) Colocalization of transactivation-responsive DNA-binding protein 43 and huntingtin in inclusions of Huntington disease. J Neuropathol Exp Neurol 67:1159–1165
Seeburger JL, Tarras S, Natter H, Springer JE (1993) Spinal cord motoneurons express p75 NGFR and p145 trkB mRNA in amyotrophic lateral sclerosis. Brain Res 621:111–115
Selvaraj BT, Frank N, Bender FL, Asan E, Sendtner M (2012) Local axonal function of STAT3 rescues axon degeneration in the pmn model of motoneuron disease. J Cell Biol 199:437–451
Sendtner M (2001) Molecular mechanisms in spinal muscular atrophy: models and perspectives. Curr Opin Neurol 14:629–634
Sendtner M (2010) Therapy development in spinal muscular atrophy. Nat Neurosci 13:795–799
Sendtner M, Kreutzberg GW, Thoenen H (1990) Ciliary neurotrophic factor prevents the degeneration of motor neurons after axotomy. Nature 345:440–441
Sendtner M, Holtmann B, Kolbeck R, Thoenen H, Barde YA (1992a) Brain-derived neurotrophic factor prevents the death of motoneurons in newborn rats after nerve section. Nature 360:757–758, 1995 Sep 28; 377(6547):340–344
Sendtner M et al (1992b) Ciliary neurotrophic factor prevents degeneration of motor neurons in mouse mutant progressive motor neuronopathy. Nature 358:502–504
Sephton CF et al (2011) Identification of neuronal RNA targets of TDP-43-containing ribonucleoprotein complexes. J Biol Chem 286:1204–1215
Simon CM, Jablonka S, Ruiz R, Tabares L, Sendtner M (2010) Ciliary neurotrophic factor-induced sprouting preserves motor function in a mouse model of mild spinal muscular atrophy. Hum Mol Genet 19:973–986
Simpson EP, Henry YK, Henkel JS, Smith RG, Appel SH (2004) Increased lipid peroxidation in sera of ALS patients: a potential biomarker of disease burden. Neurology 62:1758–1765
Singh KK et al (2008) Developmental axon pruning mediated by BDNF-p75NTR-dependent axon degeneration. Nat Neurosci 11:649–658
Smith RG, Henry YK, Mattson MP, Appel SH (1998) Presence of 4-hydroxynonenal in cerebrospinal fluid of patients with sporadic amyotrophic lateral sclerosis. Ann Neurol 44:696–699
Sreedharan J et al (2008) TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science 319(5870):1668–1672
Stockli KA et al (1989) Molecular cloning, expression and regional distribution of rat ciliary neurotrophic factor. Nature 342:920–923
Strong MJ et al (2007) TDP43 is a human low molecular weight neurofilament (hNFL) mRNA-binding protein. Mol Cell Neurosci 35:320–327
Subramanian M et al (2011) G-quadruplex RNA structure as a signal for neurite mRNA targeting. EMBO Rep 12:697–704
Thoenen H, Sendtner M (2002) Neurotrophins: from enthusiastic expectations through sobering experiences to rational therapeutic approaches. Nat Neurosci 5(Suppl):1046–1050
Tollervey JR et al (2011) Characterizing the RNA targets and position-dependent splicing regulation by TDP-43. Nat Neurosci 14:452–458
Torres-Benito L, Ruiz R, Tabares L (2012) Synaptic defects in spinal muscular atrophy animal models. Dev Neurobiol 72:126–133
Urushitani M et al (2006) Chromogranin-mediated secretion of mutant superoxide dismutase proteins linked to amyotrophic lateral sclerosis. Nat Neurosci 9:108–118
Van Damme P et al (2007) Astrocytes regulate GluR2 expression in motor neurons and their vulnerability to excitotoxicity. Proc Natl Acad Sci U S A 104:14825–14830
Vance C et al (2009) Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science 323(5918):1208–1211
Volkening K, Leystra-Lantz C, Yang W, Jaffee H, Strong MJ (2009) Tar DNA binding protein of 43 kDa (TDP-43), 14-3-3 proteins and copper/zinc superoxide dismutase (SOD1) interact to modulate NFL mRNA stability. Implications for altered RNA processing in amyotrophic lateral sclerosis (ALS). Brain Res 1305:168–182
Wang IF, Reddy NM, Shen CK (2002) Higher order arrangement of the eukaryotic nuclear bodies. Proc Natl Acad Sci U S A 99:13583–13588
Wegorzewska I, Baloh RH (2011) TDP-43-based animal models of neurodegeneration: new insights into ALS pathology and pathophysiology. Neurodegener Dis 8:262–274
Weidner KM et al (1991) Evidence for the identity of human scatter factor and human hepatocyte growth factor. Proc Natl Acad Sci U S A 88:7001–7005
Wirth B (2000) An update of the mutation spectrum of the survival motor neuron gene (SMN1) in autosomal recessive spinal muscular atrophy (SMA). Hum Mutat 15:228–237
Wong PC et al (1995) An adverse property of a familial ALS-linked SOD1 mutation causes motor neuron disease characterized by vacuolar degeneration of mitochondria. Neuron 14:1105–1116
Wood-Allum C, Shaw PJ (2010) Motor neurone disease: a practical update on diagnosis and management. Clin Med 10:252–258
Wu CH et al (2012) Mutations in the profilin 1 gene cause familial amyotrophic lateral sclerosis. Nature 488(7412):499–503
Yamamoto Y et al (1997) Hepatocyte growth factor (HGF/SF) is a muscle-derived survival factor for a subpopulation of embryonic motoneurons. Development 124:2903–2913
Yamazaki T et al (2012) FUS-SMN protein interactions link the motor neuron diseases ALS and SMA. Cell Rep 2:799–806
Zinszner H, Albalat R, Ron D (1994) A novel effector domain from the RNA-binding protein TLS or EWS is required for oncogenic transformation by CHOP. Genes Dev 8:2513–2526
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg 2014
About this chapter
Cite this chapter
Sendtner, M. (2014). Motoneuron Disease. In: Lewin, G., Carter, B. (eds) Neurotrophic Factors. Handbook of Experimental Pharmacology, vol 220. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-45106-5_15
Download citation
DOI: https://doi.org/10.1007/978-3-642-45106-5_15
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-45105-8
Online ISBN: 978-3-642-45106-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)