Abstract
Circulating tumor cells offer promise as a surrogate source of cancer cells that can be obtained in real time and may provide opportunities to evaluate predictive biomarkers that can guide treatment decisions. In this review, we consider some of the technical hurdles around CTC numbers and suitability of various CTC capture and analysis platforms for biomarker evaluation. In addition, we consider the potential regulatory hurdles to development of CTC-based diagnostics. Finally, we suggest a path for co-development of anticancer therapeutics with CTC-based diagnostics that could enable clinical validation and qualification of CTC-based assays as companion diagnostics.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Early Stage Breast Cancer
- HER2 Status
- CRPC Patient
- Early Phase Clinical Trial
- Castrate Resistant Prostate Cancer
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Cells with morphological properties similar to neoplastic cells have been recognized to circulate in the blood of cancer patients for over 140 years [1]. Recent data has suggested that these cells exhibit hallmark characteristics of transformed cells. These findings have supported the notion that such circulating tumor cells (CTCs) are shed from tumor masses into the peripheral bloodstream [2, 3], though the relationship between CTCs and other cells that remain within the tumor proper remains somewhat unclear [4, 5]. In patients with late stage metastatic breast cancer (MBC), it has been demonstrated that the detection of elevated levels of CTCs at any time prior to, or during, the course of therapy is an independent predictor of disease progression and mortality [6–8]. As such, CTC levels constitute a prognostic biomarker. Other recent studies have shown that they may also have utility as a surrogate endpoint of anti-tumor activity in early phase clinical trials [9, 10]. CTCs can also be detected in patients with early stage breast cancer and elevated levels have been reported to be associated with poor prognosis, although these patients generally have fewer detectable CTCs than patients with more advanced breast cancer [11, 12].
The primary focus of this review is whether CTCs may provide additional value to biomarker studies. A key question is whether the molecular characteristics of CTCs can be used in predictive diagnostic assays for molecularly targeted therapeutics. As discussed in detail in the accompanying chapter by Taube and Lively, a predictive diagnostic can be defined as a test that can be performed prior to treatment to indicate the likelihood of response to a particular therapeutic or class of therapeutics. Following prospective clinical qualification with a technically and analytically validated assay, a predictive diagnostic can gain regulatory approval as a companion in vitro diagnostic (IVD) test intended to be used in conjunction with a therapeutic agent in order to identify patients likely to benefit or in whom the agent is expected to have little or no effect [13]. Examples include HercepTest™ and pharmDx™ tests used to determine HER2 protein and DNA copy number, respectively, as the basis for treatment with agents such as Herceptin® (trastuzumab) and Tykerb® (lapatinib) [14]. Current companion diagnostic assays rely predominantly on archival tissue that is collected at time of diagnosis through biopsy or surgical resection. Such tissue may not be representative of a patient’s current disease, particularly after multiple lines of therapy. As such, there is a pressing need for tissues that are more representative of disease at the time a patient is undergoing therapy. This chapter will consider a number of the technical and biological challenges that must be overcome if CTCs are to be successfully used as a source of cancer cells for biomarker analyses.
2 On the Relevance of CTCs as a Source of Representative Cancer Tissue for Predictive Dx
There are many reasons to suppose that diagnostic approaches that rely on archival tissue could be inadequate and result in inaccurate results. Consider for example prostate cancer, which can have a long indolent period of 10–15 years that can be managed through hormonal therapies, prior to progressing to late stage castrate resistant prostate cancer. Recent studies have shown that metastatic tumor samples can be quite different from the original primary tumor and acquire additional alterations. For example, large-scale genomic profiling of primary and metastatic prostate cancers revealed much more widespread activation of PI3K, PTEN, Rb and RAS/RAF signaling in metastatic tissues compared to primary tumors [15]. In some cases, upregulation of these signaling pathways may be an escape or evolutionary mechanism whereby tumors evade chemo- or hormonal therapies [16], again suggesting a need to obtain representative tissue at the time new therapies are being considered.
Even in cases where metastatic tissue can be obtained, it is not clear that tissue from a single site is representative of the majority of the metastatic lesions, and instances of substantial heterogeneity have been reported [17]. Similar considerations apply to other solid tumor types including breast cancer, which can also have long indolent periods punctuated by treatment that could cause changes in the molecular portrait of a patient’s metastatic disease. Recent analyses have indicated that biomarker status can, in some instances, be discordant between primary and metastatic breast cancer. A notable example is mutations in the PIK3CA oncogene that occur with greater frequency in metastatic compared to primary lesions [18].
It seems clear that making treatment decisions based on diagnostic assays conducted on primary tumor tissue is a suboptimal solution to personalized medicine strategies. However, collecting metastatic tissue via biopsies imposes risks, anxiety and inconvenience to patients and is perceived to be a barrier in enrolling and conducting clinical trials [19]. For all of these reasons, characterization of predictive biomarkers in CTCs holds tremendous promise to potentially provide a real-time snapshot of the molecular makeup of a patient’s cancer prior to administration of therapy, essentially providing surrogate tissue from a “liquid biopsy.”
3 Technologies for Molecular Characterization of CTCs
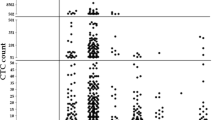
Development of new and robust technologies for the capture and characterization of CTCs will aid biomarker analyses and is an area of active investigation. A recent tally indicates that up to 30 devices are currently in development ranging from mature concept to prototype device to commercially available instrument. The Veridex CellSearch® platform is FDA approved for prognostic purposes based on CTC enumeration in colorectal, breast and prostate cancer [20], but to date no platform or instrument is approved for a companion diagnostic application. Without a gold standard, it is difficult to compare different technologies and to determine their true sensitivity and specificity to detect CTCs. Adding to this complexity is the heterogeneity observed in CTCs both in expression of phenotypic markers such as EpCAM and cytokeratin [3, 21, 22] as well as in size and morphology [23–25]. This complexity makes a “one size fits-all” platform for capturing all challenging CTCs. The ideal platform would isolate the majority of this rare cell population at high sensitivity, in an intact state, across multiple tumor types and with high purity from the surrounding blood cells. In addition, the ideal technology would lend itself to multiple types of downstream molecular analysis. These include the major methodologies used for biomarker assessment: (1) immunofluorescence (IF) or immunohistochemistry (IHC) to evaluate protein expression, (2) fluorescence in situ hybridization (FISH) to score cytogenetic lesions, (3) mRNA expression analysis by quantitative polymerase chain reaction (qPCR) and (4) mutation profiling and copy number analysis using DNA. These applications have distinct requirements in terms of yield and purity, presenting a formidable technological challenge for a single platform. It may thus be that distinct platforms with strengths in a particular type of application are required, at least initially. An example of an application with a requirement for high yield is cell-based assays (IF, IHC, FISH), which typically require deposition of CTCs with intact morphology for high resolution, multi-color microscopy. Yield is more important than purity for this type of assay, since contaminating surrounding blood cells can be excluded for analysis by using phenotypic criteria to define CTCs (Cytokeratin+, DAPI+, CD45−). However, sufficient numbers of CTCs are required to evaluate potential heterogeneity in the biomarker and to minimize errors due to false positives and negatives. For example, when comparing concordance between HER2 status in archival tumor with HER2 status in CTCs as measured by an IF assay on CellSearch, we found that a minimum of 3 CTCs were required to minimize type I and II errors [3]. Similarly, in a study evaluating ERG rearrangements and PTEN loss by FISH in CTCs from CRPC patients using CellSearch, results from a minimum of four individual CTCs were required to overcome the underlying false positive rate of assay [26]. Based on these experiments, we propose a minimum requirement of ≥5 CTCs for cell-based assays, albeit this number will have to be empirically determined for each assay during the validation stage of biomarker development. However, even a minimum cutoff of ≥5 CTCs poses a significant challenge in the number of patients that will meet these criteria and be suitable for biomarker analyses. For example, even in prostate cancer, the tumor type with the highest reported CTC counts, only 41% of prostate cancer patients have ≥5 CTCs [27]. This concern may be somewhat mitigated in patient populations with late stage disease, since we and others have found that CTC counts can be higher in more advanced disease when evaluating patients who have progressed beyond frontline therapy [3, 26, 28]. For example, in CRPC patients who have progressed on docetaxel treatment, ~70% had >5 CTCs using the CellSearch platform [9]. This underscores the importance of having a step in the assay validation process to be using blood samples from the target patient population of interest, and also suggests that proof-of-concept studies with molecular characterization of CTCs on the CellSearch platform may currently be best suited to patient populations with advanced disease.
Clearly, it would also be advantageous to be able to capture higher numbers of CTCs for biomarker analyses in order to meet the suggested criteria of ≥5 CTCs per patient, and there are emerging platforms with surfaces amenable to high-resolution imaging and higher reported CTC counts. These include the fiber-optic array scanning technology from EPIC Sciences [25], which uses immunostain and morphological features determined by automated scanning on a histology slide to distinguish CTCs from WBCs. The isolation by size of epithelial tumor cell (ISET) method from Rarecell Inc also holds some promise in this regard, as a recent report identified 41% of patients with morphologically malignant circulating non-hematological cells using standard cytopathology staining and microscopic analysis in patients with resectable non-small cell lung cancer [29]. These platforms need to be evaluated in side-by-side comparisons with CellSearch on matched patient blood samples to determine the utility and feasibility of use for cell-based assays.
In contrast to cell-based assays where CTC purity is not as critical, molecular assays on CTC-derived DNA or RNA typically require high purity (upwards of 50%). Such purity is required to overcome the background “noise” from contaminating blood cells that are included in the initial cell lysate preparation step. Impressive levels of purity (~50%) as well as high capture rates (median, 50 CTCs per mL) have been reported for the microfluidic CTC-chip platform [30]. In a study evaluating EGFR mutations in metastatic lung cancer, they observed the expected EGFR mutation in 12 of 13 patients [31], suggesting sufficient purity for this type of downstream molecular analysis. However, maintaining this level of purity through scale-up and standardization process has been a challenge, with increased variability observed in CTC purity ranging from 50 to 0.1% [32]. At the lower end, this level of purity is similar to what is observed on CellSearch and the commercial CTC-chip technologies from Cellective and Biocept [3].
An architecturally distinct next generation microfluidic CTC-chip, the herringbone (HB)-chip, was developed in order to overcome some of the shortcomings of the original three-dimensional micropost-based platform [33]. Using the HB-chip, the Haber and Toner labs demonstrated the ability to detect the TMPRSS2-ERG fusion transcript in RNA extracted from CTCs in metastatic prostate cancer [34]. It will be interesting to determine the utility of this new design for other molecular assays.
Another approach to circumvent the purity requirements for molecular assays is to use laser capture microscopy (LCM) to further purify CTCs from enriched CTC preparations. LCM has been used to purify CTCs captured on the Cellective microfluidic CTC-chip and transcripts derived from CTCs showed strong concordance to those from primary and metastatic tissues from an orthotopic xenograft model [35]. Another technology that has reported >50% purity as assessed by cell line spike-in experiments is the MagSweeper, an immunomagnetic separation technology that enriches target cells while eliminating cells unbound to magnetic particles [36]. This device has been coupled with Illumina’s genomic platforms to analyze CTCs at the single cell level by RNA sequencing (RNA-Seq).
Technologies suitable for cell-based assays:
Technology | Surface | Capture method | Assays |
|---|---|---|---|
CellSearch, Veridex LLC | CTCs held planar by magnetic field | Immunomagnetic capture by EpCAM | IF, FISH |
EPIC sciences | Blood cells are visualized on microscope slide | No selection. CTC identified by morphology and immunophenotype | IF, FISH |
ISET, Rarecells Inc. | Filter based membrane | CTC captured by size | IHC, IF, FISH |
Technologies suitable for molecular assays:
Technology | Purity (%) | Capture method | Assays |
|---|---|---|---|
Microfluidic CTC-chip | 0.1–50 | EpCAM or other antibodies | Mutation assays, RNA expression |
HB-chip (2nd generation microfluidic CTC-chip) | 14 | PSA or other antibodies | Mutation assays, RNA expression |
Cellective CTC-chip + LCM | 0.1 further enriched by LCM | EpCAM | Gene expression (RNA) |
MagSweeper + Illumina genomic analysis | 51 | EpCAM | RNA-Seq |
4 HER2 Diagnostics in CTCs
Demonstrating that the molecular phenotype in CTCs accurately represents the molecular characteristics of the tumor cell is an important step in qualifying CTCs for molecular biomarker detection and patient selection. A test case investigated by several labs has been to compare HER2 status in CTCs from breast cancer patients to that in matched tumor tissue. HER2 is a gold standard for biomarker validation because it is a well-characterized marker where the metrics for HER2 positivity have been tested and correlated with response to trastuzumab treatment. The neoadjuvant GeparQuattro study showed that while CTC numbers are low in early stage breast cancer patients, it is possible to quantitate HER2 levels in these CTCs [37]. Furthermore, this study identified a number of patients with HER2-negative primary tumors who had HER2-positive CTCs, and suggested that HER2 biomarker analyses in CTCs might be helpful for stratification and monitoring of HER2-directed therapies [37].
We recently evaluated HER2 status by IF in CTCs from 29 patients with advanced metastatic breast cancer whose HER2 primary tumor status was known and found a high degree of concordance at 89% [3]. Other reports have shown lower concordance in the range of 50–70%, with HER2-positive CTCs observed in patients where the primary tumor was HER2-negative, as well as HER2-negative CTCs in patients with HER2+ primary tumors [38–41]. These results suggest the possibility that HER2 status can change over time, though further study is required to rule out testing errors as a source of the differences. Prospective clinical studies will be required to qualify HER2 status in CTCs as a relevant predictive biomarker that can be used in real-time assessments. Several such studies are underway to determine whether positive HER2 status in CTCs are indicative of benefit to HER2 targeted therapies. These include Phase II study of the HER2 targeted inhibitor lapatinib in breast cancer patients with HER2 non-amplified primary tumors and HER2-positive CTCs (NCT00820924 clinicaltrials.gov), and a Phase II study evaluating the effects of trastuzumab in combination with the chemotherapeutic agent vinorelbine in patients that are positive for HER2. The latter study also includes patients whose original breast cancer was negative but whose CTCs are positive for HER2 (NCT01185509 clinicaltrials.gov). The outcome of these and other studies will inform the clinical utility of molecular analysis in CTCs for predictive biomarker analysis and patient selection.
5 Applications of Predictive Biomarker Analyses in CTCs to Treatment of Metastatic and Early Stage Disease
Metastasis of solid tumor malignancies to distant organs almost always results in patient mortality and accumulating evidence suggests that the process of metastasis may be mediated by CTCs in peripheral circulation or by disseminated tumor cells (DTCs) that can be found in bone marrow [42]. Early stage breast cancer without obvious local or distant metastases is often cured by surgical intervention, though a subset of these patients relapse due to metastatic disease which is likely attributable to minimal residual disease in the form of micrometastatic lesions, DTCs and/or CTCs [43]. This phenomenon is the basis for adjuvant therapy wherein patients are treated with systemic chemo- or targeted therapies following surgical resection of primary tumors in order to eradicate the remaining residual cancer cells. A key limitation of this approach is that treatment is almost always made without knowledge of the molecular makeup of the residual cancer cells, and could surely be improved if treatment could be tailored based on the molecular characteristics of CTCs or DTCs from an individual patient. Incorporation of CTC biomarker evaluations in patients in the adjuvant setting may be initially more challenging, since these patients not only have fewer CTCs, but also generally have better survival prospects and longer time to clinical events that prolongs drug development timelines. Based on this, it may be prudent to focus initial efforts on validating CTC predictive biomarker assays in metastatic patients. Success in this setting could then be followed by application to early stage breast cancer, analogous to the development of novel therapeutics, which are typically validated in the metastatic setting prior to testing in the adjuvant setting.
6 The Path Forward
The current drug-diagnostic co-development paradigm requires early identification of predictive biomarkers to allow prospective validation in clinical trials, ultimately leading to joint regulatory filings on the drug and diagnostic test [44]. For CTC-based diagnostics to conform to these expectations, a number of challenges will need to be overcome. First, indications need to be identified where the majority of patients have CTCs in sufficient numbers to allow molecular characterization of the biomarker of interest. Second, the platform most suitable to performing the assays needs to be determined. Third, in the USA, all predictive biomarker tests used for patient management must be run under appropriate laboratory conditions. Specifically, assays must comply with the Clinical Laboratory Improvement Amendments (CLIA) act of 1988 [45, 46], or the guidelines of the office of in vitro diagnostics (OIVD) of the FDA. This creates a challenging regulatory path for new and unproven diagnostic technologies [46]. Below, and in the accompanying Fig. 1, we propose a stepwise process to address technical and regulatory development hurdles and clinically validate CTC-based predictive diagnostic tests.
As discussed in the accompanying chapter, a first step in biomarker development is the creation of a robust prototype assay that is technically and analytically validated and can be applied to early phase clinical trials. Important considerations in this process include detailed specification of the technical protocol and defined assay validation criteria [44]. This encompasses both pre-analytical parameters such as effects of specimen handling, processing, shipping and storage, as well as post-analytical parameters such as establishing inter-and intra-assay precision, linearity and standardization [47]. While this is feasible for tumor tissues that can be fixed and stored embedded in paraffin, it imposes special challenges in the area of CTCs, since current technologies require fresh blood collection and processing within a time frame of 72–96 h [3]. A possible path forward here would be for the drug sponsor to work closely with clinical investigators on pre-analytical validation prior to initiating clinical studies. Steps here would be to prospectively procure blood samples with basic clinical data and appropriate pre-analytical variables, and use these samples for analytic validation of the prototype diagnostic. It should also be possible and may be desirable to include cell line controls representing differing biomarker status in “spike-in” experiments as a basic quality control for inter-experiment variability and to calibrate results between runs. The next step in the process is clinical qualification, the process of linking biomarker status with clinical outcomes or endpoints in a trial appropriately designed to test the biomarker hypothesis. A robust prototype assay that met the above validation criteria would ideally be used at this point in biomarker qualification, initially in proof-of-concept studies but culminating in prospective analysis in a pivotal study.
The next consideration is whether the assay should be a laboratory developed test (LDT) run at a single reference lab, or a kit that can be widely distributed and run in community laboratories. As discussed by Taube and Lively, both paths have pluses and minuses that can impact the overall chances of success, though the regulatory and analytical hurdles may be easier to achieve in a single laboratory setting under the LDT model. Given that numerous CTC capture platforms are in development and a clear winner has yet to emerge that is superior for all forms of molecular characterization, a practical solution may be for the drug developing entity to form an early partnership with a lab that offers a technology suitable for the biomarker question of interest. The early phase of the partnership could consist of the preclinical validation studies described above, with a plan to coordinate clinical evaluation of the drug and diagnostic in appropriately designed early phase clinical studies. At the same time, the diagnostic company could take steps to obtain FDA clearance of the CTC platform or instrument for biomarker testing, and could plan the path with the drug sponsor for biomarker data collection and analysis in pivotal studies, leading to a joint regulatory filing for approval of the drug and CTC-based diagnostic.
7 Conclusions
Molecular characterization of CTCs holds significant promise to aid in companion diagnostics development by providing a representative source of tumor material from a minimally invasive procedure. For this promise to be fully realized, both additional advances in technology as well as careful consideration of drug and CTC diagnostic co-development will be required.
References
Ashworth T (1869) A case of cancer in which cells similar to those in the tumors were seen in the blood after death. Aust Med J 14:146
Attard G, de Bono JS (2011) Utilizing circulating tumor cells: challenges and pitfalls. Curr Opin Genet Dev 21:50–58
Punnoose EA, Atwal SK, Spoerke JM, Savage H, Pandita A, Yeh RF, Pirzkall A, Fine BM, Amler LC, Chen DS, Lackner MR (2011) Molecular biomarker analyses using circulating tumor cells. PloS one 5:e12517
Maheswaran S, Haber DA (2010) Circulating tumor cells: a window into cancer biology and metastasis. Curr Opin Genet Dev 20(1):96–99
Pantel K, Alix-Panabieres C (2010) Circulating tumour cells in cancer patients: challenges and perspectives. Trends Mol Med 16:398–406
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351:781–791
Cristofanilli M, Hayes DF, Budd GT, Ellis MJ, Stopeck A, Reuben JM, Doyle GV, Matera J, Allard WJ, Miller MC, Fritsche HA, Hortobagyi GN, Terstappen LW (2005) Circulating tumor cells: a novel prognostic factor for newly diagnosed metastatic breast cancer. J Clin Oncol 23:1420–1430
Hayes DF, Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Miller MC, Matera J, Allard WJ, Doyle GV, Terstappen LW (2006) Circulating tumor cells at each follow-up time point during therapy of metastatic breast cancer patients predict progression-free and overall survival. Clin Cancer Res 12:4218–4224
Danila DC, Morris MJ, de Bono JS, Ryan CJ, Denmeade SR, Smith MR, Taplin ME, Bubley GJ, Kheoh T, Haqq C, Molina A, Anand A, Koscuiszka M, Larson SM, Schwartz LH, Fleisher M, Scher HI (2010) Phase II multicenter study of abiraterone acetate plus prednisone therapy in patients with docetaxel-treated castration-resistant prostate cancer. J Clin Oncol 28:1496–1501
Reid AH, Attard G, Danila DC, Oommen NB, Olmos D, Fong PC, Molife LR, Hunt J, Messiou C, Parker C, Dearnaley D, Swennenhuis JF, Terstappen LW, Lee G, Kheoh T, Molina A, Ryan CJ, Small E, Scher HI, de Bono JS (2010) Significant and sustained antitumor activity in post-docetaxel, castration-resistant prostate cancer with the CYP17 inhibitor abiraterone acetate. J Clin Oncol 28:1489–1495
Bidard FC, Mathiot C, Delaloge S, Brain E, Giachetti S, de Cremoux P, Marty M, Pierga JY (2010) Single circulating tumor cell detection and overall survival in nonmetastatic breast cancer. Ann Oncol 21:729–733
Ignatiadis M, Kallergi G, Ntoulia M, Perraki M, Apostolaki S, Kafousi M, Chlouverakis G, Stathopoulos E, Lianidou E, Georgoulias V, Mavroudis D (2008) Prognostic value of the molecular detection of circulating tumor cells using a multimarker reverse transcription-PCR assay for cytokeratin 19, mammaglobin A, and HER2 in early breast cancer. Clin Cancer Res 14:2593–2600
Philip R, Carrington L, Chan M (2011) US FDA perspective on challenges in co-developing in vitro companion diagnostics and targeted cancer therapeutics. Bioanalysis 3:383–389
Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, Harris LN, Fehrenbacher L, Slamon DJ, Murphy M, Novotny WF, Burchmore M, Shak S, Stewart SJ, Press M (2002) Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol 20:719–726
Taylor BS, Schultz N, Hieronymus H, Gopalan A, Xiao Y, Carver BS, Arora VK, Kaushik P, Cerami E, Reva B, Antipin Y, Mitsiades N, Landers T, Dolgalev I, Major JE, Wilson M, Socci ND, Lash AE, Heguy A, Eastham JA, Scher HI, Reuter VE, Scardino PT, Sander C, Sawyers CL, Gerald WL (2010) Integrative genomic profiling of human prostate cancer. Cancer Cell 18:11–22
Carver BS, Chapinski C, Wongvipat J, Hieronymus H, Chen Y, Chandarlapaty S, Arora VK, Le C, Koutcher J, Scher H, Scardino PT, Rosen N, Sawyers CL (2011) Reciprocal feedback regulation of PI3K and androgen receptor signaling in PTEN-deficient prostate cancer. Cancer Cell 19:575–586
Suzuki H, Freije D, Nusskern DR, Okami K, Cairns P, Sidransky D, Isaacs WB, Bova GS (1998) Interfocal heterogeneity of PTEN/MMAC1 gene alterations in multiple metastatic prostate cancer tissues. Cancer Res 58:204–209
Dupont Jensen J, Laenkholm AV, Knoop A, Ewertz M, Bandaru R, Liu W, Hackl W, Barrett JC, Gardner H (2010) PIK3CA mutations may be discordant between primary and corresponding metastatic disease in breast cancer. Clin Cancer Res 17:667–677
Agulnik M, Oza AM, Pond GR, Siu LL (2006) Impact and perceptions of mandatory tumor biopsies for correlative studies in clinical trials of novel anticancer agents. J Clin Oncol 24:4801–4807
Miller MC, Doyle GV, Terstappen LW (2010) Significance of circulating tumor cells detected by the cellSearch system in patients with metastatic breast colorectal and prostate cancer. J Oncol 2010:617421
Mikolajczyk SD, Millar LS, Tsinberg P, Coutts SM, Zomorrodi M, Pham T, Bischoff FZ, Pircher TJ (2011) Detection of EpCAM-negative and cytokeratin-negative circulating tumor cells in peripheral blood. J Oncol 2011:252361
Sieuwerts AM, Kraan J, Bolt J, van der Spoel P, Elstrodt F, Schutte M, Martens JW, Gratama JW, Sleijfer S, Foekens JA (2009) Anti-epithelial cell adhesion molecule antibodies and the detection of circulating normal-like breast tumor cells. J Natl Cancer Inst 101:61–66
Coumans FA, Doggen CJ, Attard G, de Bono JS, Terstappen LW (2010) All circulating EpCAM + CK + CD45- objects predict overall survival in castration-resistant prostate cancer. Ann Oncol 21:1851–1857
Marrinucci D, Bethel K, Bruce RH, Curry DN, Hsieh B, Humphrey M, Krivacic RT, Kroener J, Kroener L, Ladanyi A, Lazarus NH, Nieva J, Kuhn P (2007) Case study of the morphologic variation of circulating tumor cells. Hum Pathol 38:514–519
Marrinucci D, Bethel K, Lazar D, Fisher J, Huynh E, Clark P, Bruce R, Nieva J, Kuhn P (2010) Cytomorphology of circulating colorectal tumor cells: a small case series. J Oncol 2010:861341
Attard G, Swennenhuis JF, Olmos D, Reid AH, Vickers E, A’Hern R, Levink R, Coumans F, Moreira J, Riisnaes R, Oommen NB, Hawche G, Jameson C, Thompson E, Sipkema R, Carden CP, Parker C, Dearnaley D, Kaye SB, Cooper CS, Molina A, Cox ME, Terstappen LW, de Bono JS (2009) Characterization of ERG, AR and PTEN gene status in circulating tumor cells from patients with castration-resistant prostate cancer. Cancer Res 69:2912–2918
Allard WJ, Matera J, Miller MC, Repollet M, Connelly MC, Rao C, Tibbe AG, Uhr JW, Terstappen LW (2004) Tumor cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clin Cancer Res 10:6897–6904
Leversha MA, Han J, Asgari Z, Danila DC, Lin O, Gonzalez-Espinoza R, Anand A, Lilja H, Heller G, Fleisher M, Scher HI (2009) Fluorescence in situ hybridization analysis of circulating tumor cells in metastatic prostate cancer. Clin Cancer Res 15:2091–2097
Hofman V, Long E, Ilie M, Bonnetaud C, Vignaud JM, Flejou JF, Lantuejoul S, Piaton E, Mourad N, Butori C, Selva E, Marquette CH, Poudenx M, Sibon S, Kelhef S, Venissac N, Jais JP, Mouroux J, Molina TJ, Vielh P, Hofman P (2012) Morphological analysis of circulating tumour cells in patients undergoing surgery for non-small cell lung carcinoma using the isolation by size of epithelial tumour cell (ISET) method. Cytopathology 23(1):30–38.
Nagrath S, Sequist LV, Maheswaran S, Bell DW, Irimia D, Ulkus L, Smith MR, Kwak EL, Digumarthy S, Muzikansky A, Ryan P, Balis UJ, Tompkins RG, Haber DA, Toner M (2007) Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature 450:1235–1239
Maheswaran S, Sequist LV, Nagrath S, Ulkus L, Brannigan B, Collura CV, Inserra E, Diederichs S, Iafrate AJ, Bell DW, Digumarthy S, Muzikansky A, Irimia D, Settleman J, Tompkins RG, Lynch TJ, Toner M, Haber DA (2008) Detection of mutations in EGFR in circulating lung-cancer cells. N Engl J Med 359:366–377
Yu M, Stott S, Toner M, Maheswaran S, Haber DA (2011) Circulating tumor cells: approaches to isolation and characterization. J cell Biol 192:373–382
Stott SL, Hsu CH, Tsukrov DI, Yu M, Miyamoto DT, Waltman BA, Rothenberg SM, Shah AM, Smas ME, Korir GK, Floyd FP Jr, Gilman AJ, Lord JB, Winokur D, Springer S, Irimia D, Nagrath S, Sequist LV, Lee RJ, Isselbacher KJ, Maheswaran S, Haber DA, Toner M (2011) Isolation of circulating tumor cells using a microvortex-generating herringbone-chip. Proc Natl Acad Sci U S A 107:18392–18397
Stott SL, Lee RJ, Nagrath S, Yu M, Miyamoto DT, Ulkus L, Inserra EJ, Ulman M, Springer S, Nakamura Z, Moore AL, Tsukrov DI, Kempner ME, Dahl DM, Wu CL, Iafrate AJ, Smith MR, Tompkins RG, Sequist LV, Toner M, Haber DA, Maheswaran S (2011) Isolation and characterization of circulating tumor cells from patients with localized and metastatic prostate cancer. Sci Transl Med 2:25ra23
Helzer KT, Barnes HE, Day L, Harvey J, Billings PR, Forsyth A (2009) Circulating tumor cells are transcriptionally similar to the primary tumor in a murine prostate model. Cancer Res 69:7860–7866
Talasaz AH, Powell AA, Huber DE, Berbee JG, Roh KH, Yu W, Xiao W, Davis MM, Pease RF, Mindrinos MN, Jeffrey SS, Davis RW (2009) Isolating highly enriched populations of circulating epithelial cells and other rare cells from blood using a magnetic sweeper device. Proc Natl Acad Sci U S A 106:3970–3975
Riethdorf S, Muller V, Zhang L, Rau T, Loibl S, Komor M, Roller M, Huober J, Fehm T, Schrader I, Hilfrich J, Holms F, Tesch H, Eidtmann H, Untch M, von Minckwitz G, Pantel K (2010) Detection and HER2 expression of circulating tumor cells: prospective monitoring in breast cancer patients treated in the neoadjuvant GeparQuattro trial. Clin Cancer Res 16:2634–2645
Fehm T, Muller V, Aktas B, Janni W, Schneeweiss A, Stickeler E, Lattrich C, Lohberg CR, Solomayer E, Rack B, Riethdorf S, Klein C, Schindlbeck C, Brocker K, Kasimir-Bauer S, Wallwiener D, Pantel K (2010) HER2 status of circulating tumor cells in patients with metastatic breast cancer: a prospective, multicenter trial. Breast Cancer Res Treat 124:403–412
Flores LM, Kindelberger DW, Ligon AH, Capelletti M, Fiorentino M, Loda M, Cibas ES, Janne PA, Krop IE (2010) Improving the yield of circulating tumour cells facilitates molecular characterisation and recognition of discordant HER2 amplification in breast cancer. Br J Cancer 102:1495–1502
Meng S, Tripathy D, Shete S, Ashfaq R, Haley B, Perkins S, Beitsch P, Khan A, Euhus D, Osborne C, Frenkel E, Hoover S, Leitch M, Clifford E, Vitetta E, Morrison L, Herlyn D, Terstappen LW, Fleming T, Fehm T, Tucker T, Lane N, Wang J, Uhr J (2004) HER-2 gene amplification can be acquired as breast cancer progresses. Proc Natl Acad Sci U S A 101:9393–9398
Pestrin M, Bessi S, Galardi F, Truglia M, Biggeri A, Biagioni C, Cappadona S, Biganzoli L, Giannini A, Di Leo A (2009) Correlation of HER2 status between primary tumors and corresponding circulating tumor cells in advanced breast cancer patients. Breast Cancer Res Treat 118:523–530
Pantel K, Brakenhoff RH, Brandt B (2008) Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat Rev Cancer 8:329–340
Hayashi N, Yamauchi H (2011) Role of circulating tumor cells and disseminated tumor cells in primary breast cancer. Breast cancer. (Tokyo, Japan)
Taube SE, Clark GM, Dancey JE, McShane LM, Sigman CC, Gutman SI (2009) A perspective on challenges and issues in biomarker development and drug and biomarker codevelopment. J Natl Cancer Inst 101:1453–1463
Clinical Laboratory Improvement Amendments (CLIA) (1988) Clinical Laboratory Improvement Amendments (CLIA) US Department of Health and Human Services. URL: https://www.cms.gov/clia/
Wistuba II, Gelovani JG, Jacoby JJ, Davis SE, Herbst RS (2011) Methodological and practical challenges for personalized cancer therapies. Nat Rev 8:135–141
Danila D, Fleisher M, Scher H (2011) Circulating tumor cells as biomarkers in prostate cancer. Clin Cancer Res 17:3903–3912
Acknowledgments
The authors would like to thank Garret Hampton and Andrea Pirzkall for their comments on the manuscript and useful discussions.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Punnoose, E.A., Lackner, M.R. (2012). Challenges and Opportunities in the Use of CTCs for Companion Diagnostic Development. In: Ignatiadis, M., Sotiriou, C., Pantel, K. (eds) Minimal Residual Disease and Circulating Tumor Cells in Breast Cancer. Recent Results in Cancer Research, vol 195. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-28160-0_22
Download citation
DOI: https://doi.org/10.1007/978-3-642-28160-0_22
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-28159-4
Online ISBN: 978-3-642-28160-0
eBook Packages: MedicineMedicine (R0)