Treatment of combat injury, defined as a casualty to military personnel resulting from combat, has become an increasingly important aspect of modern medicine. Advances in medical care and improvements in both body and vehicle armor have combined to increase a wounded soldier’s odds of survival from 76.4% during the Vietnam War [30] to 90.4% in Iraq [7].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Treatment of combat injury, defined as a casualty to military personnel resulting from combat, has become an increasingly important aspect of modern medicine. Advances in medical care and improvements in both body and vehicle armor have combined to increase a wounded soldier’s odds of survival from 76.4% during the Vietnam War [30] to 90.4% in Iraq [7]. In spite of this fact, many survivors have sustained traumatic orthopedic injuries: approximately 70% of war wounds are musculoskeletal injuries, and 55% are extremity wounds. Combat injuries often involve high-velocity shells, which are likely to result in injuries that are very different from those seen in civilian trauma centers, which are due to lower velocity bullets. In modern combat fields the principle type of injury is caused by blast mechanism. This pattern of injury can be complex, unpredictable, and diagnostically challenging [18]. Injuries from explosives are much more common in combat trauma, but terrorist acts that cause explosive injury are taking place at an increasing rate. Recent estimates show a fourfold rise from 1999 to 2006 [40]. Thus, health-care systems must be able to respond to those affected, military and civilian alike.
The radiologist has a central role in attempting to reduce mortality and morbidity in this kind of injury. He should be able to recognize the spectrum of injuries inflicted by explosive devices causing blast injury. Characteristically, explosive injury has a higher proportion of critically injured patients compared to other multitrauma events [18]. The role of radiology is not only to identify all the foreign bodies, but also to help surgeons decide which fragments need to be removed during thorough surgical debridement.
According to the Israeli trauma registry one third of terror victims suffer severe trauma [18].
7.1 Blast (Explosive) Injury
A detailed description and classification of blast injuries have been published elsewhere. Thus only a short simplified version will be presented in this chapter. Explosive’s injuries are classified into four categories: primary, secondary, tertiary and quaternary. Patients may be affected by one or more categories [18, 40].
7.1.1 Primary Injuries
These are a result of the initial very high pressure waves impacting at air–liquid interfaces [18]. The primary high-pressure wave spreads radially at the speed of sound displacing the surrounding air and generating winds of substantial velocity up to several hundred kilometers per hour [40]. In air it dissipates rapidly in proportion to the cube of the distance from the blast center. Thus the degree of tissue injury is directly related to the proximity of the victim to the explosion [18]. Several systems and organs are prone to primary blast injury: limbs and earlobes may be traumatically amputated, rupture of the inner ear and eardrum, blast lung and viscus perforation of the gastrointestinal tract may occur. Primary blast lung injury may lead to an immediate death due to massive cerebral or coronary air embolism [18] (Fig. 7.1).
7.1.2 Secondary Injuries
These are caused by flying bomb fragments and debris, metallic and nonmetallic, causing penetrating trauma similar to wounds seen in civilian trauma [18, 40]. Fragment injuries comprise the most frequent and important mechanism in combat trauma [6].
Patients can be hit by one (Fig. 7.2), by a few (Fig. 7.3), or by a multitude (Fig. 7.4) of flying objects with damage to soft tissues, blood vessels, and bone [18].
AP radiographs of a 19-year-old male with multiple shrapnel in the soft tissues of his (a) left buttock, (b) left lower extremity and scrotum, (c) soft tissue emphysema in the left thigh, (d, e) soft tissue hematoma in the left calf, burst fracture of the left fibula, and small undisplaced linear fracture of the left lateral malleolus
7.1.3 Tertiary Injuries
These occur as a result of a long phase of negative pressure displacing the whole body that impacts onto fixed objects. This causes blunt and penetrating injuries, head and cervical spine, as well as orthopedic injuries.
7.1.4 Quaternary Injuries
These include all other injuries mainly burns and smoke inhalation [18, 40].
7.2 Bone and Soft Tissue Injuries
As many blast victims die from the primary blast effects at the explosion scene, it is the secondary and tertiary injuries that predominate among survivors [18, 40]. Commonly, small puncture wounds hide multiple shrapnel fragments and severe underlying injuries [18, 40]. It is important to remember that there is usually a much higher proportion of critically ill patients in blast injury than in another type of multitrauma [18]. In combat injuries a higher proportion of extremities injury exists as the head and torso are usually protected by some kind of armor.
All critically ill patients require a chest x-ray and FAST (focused abdominal sonography in trauma) in the emergency department [18]. The surgeon in charge of the patient decides on following x-ray and CT studies based on the patient’s clinical condition. Unstable critically ill patients should be transferred straight to surgery for exploratory laparotomy/thoracotomy or other operative procedures to treat the cause for hemodynamic instability. Stable critically ill patients can be transferred to the radiology department for further x-ray and/or CT investigation. Screening radiography of the limbs with penetrating injuries is performed [18].
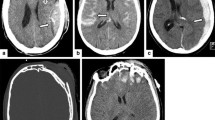
Injuries may include soft tissues injury only (Fig. 7.5), blood vessel injuries (see below), or bone fractures, with complex comminuted fractures which are common (Figs. 7.6 and 7.7).
Further investigation of the extremities may include CT or CTA. In our institution almost all of the further imaging performed was done to exclude blood vessel damage. Besides the answer to the presence of vascular damage, the CTA of the extremities could give more accurate information on: (a) damage to nerves with the sciatic nerve (Figs. 7.8 and 7.9) and common peroneal nerve (Fig. 7.10) as examples, (b) the presence of large soft tissue hematoma with the danger of compartment syndrome (Fig. 7.11) [16], (c) the location of shrapnel around blood vessels (Fig. 7.12), and (d) the exact location of shrapnel in the bone (Fig. 7.13).
(a) Axial CT images of a 21-year-old male with shrapnel in or adjacent to the left sciatic nerve (arrow), showing swelling of the left sciatic nerve (arrow) in a more proximal image, as compared to the normal right sciatic nerve; (b) two more metallic foreign bodies are seen in the left vastus medialis and vastus intermedius muscles
In patients with intra-articular fractures the CT study can add information in: (a) the exact location of intra-articular shrapnel (Figs. 7.14 and 7.15); (b) the severity of articular depression (Fig. 7.16) [23]; (c) the presence of ligament avulsion (Figs. 7.17 and 7.18) [22] or ligament tear (Fig. 7.19) [22]; (d) damage to tendons (Fig. 7.20); (e) rarely it can show meniscal entrapment into a fracture (Fig. 7.21); (f) rarely it can demonstrate meniscal tear (Fig. 7.22); and (g) the amount of lipohemarthrosis (Fig. 7.23) [8].
7.2.1 Limb Fractures and Traumatic Amputation
Limb fractures and traumatic amputations may be the result of a combination of primary and tertiary injuries (Figs. 7.24 and 7.25). The primary blast shearing wave runs along the bone and causes comminuted limb fracture; the limb subsequently flails in the tertiary blast wind, which completes amputation of the residual intact soft tissue structures. The radiographs show the extent of the injuries and help plan the surgical strategy.
7.3 Arterial Injury
Arterial damage may occur after combat injury to the extremities. Outcome depends on rapid diagnosis and repair of the injury [21]. Prompt repair of arterial injury to the extremities improves outcome in limb function and reduction of mortality related to blood loss [21]. Combat trauma is usually a result of blast trauma which includes penetrating and blunt trauma. Blunt trauma injures vessels by crushing tissue, dislocating joints, or breaking bones near arteries or veins. Penetrating injuries, caused by sharp object or high-velocity projectile may result in a large spectrum of injuries to the vessels: from complete tear to partial laceration or traumatic dissection complicated with thrombosis of an artery.
7.4 Types of Vascular Injuries
7.4.1 Hematoma
Hematoma is the outcome of vascular disruption through blunt or penetrating injury. It may be confined to the surrounding soft tissues or it may expand and tract through fascial planes [9].
On physical examination, there are skin ecchymoses and swelling, generally non-pulsating, of the soft tissues in the injured region. Pulse may be diminished or absent when the hematoma is compressing a vessel.
Large hematomas occurring within a fascial compartment may result in compartment syndrome.
7.4.2 Pseudoaneurysm
Pseudoaneurysm is a contained hematoma caused by the loss of the integrity of the three layers of the arterial wall. Penetrating trauma is the most common cause of this injury.
7.4.3 Arterio-Venous Fistula (AVF)
This is a direct connection between an artery and a vein. It is generally the result of a penetrating injury (Fig. 7.26).
(a, b) A 25-year-old male soldier with penetrating trauma to the left lower limb. CT maximum intensity projection (a) and volume rendering 3D reconstruction (b) images demonstrate multiple shrapnel throughout the left lower limb causing complete tear of the mid-popliteal artery (arrow) with arterio-venous fistula (AVF) formation. At surgery, a complete tear of the popliteal artery, vein, and nerve was found
Most frequently, AVF is asymptomatic; however, when it is large it can result in high output cardiac failure. AVF can also cause distal limb ischemia by a “steal” of blood from the extremity via the vein.
7.4.4 Arterial Embolization
Arterial embolization is caused by emboli dislodgement from an injured site in the artery, resulting in a sudden distal arterial occlusion and acute limb ischemia (Fig. 7.27).
A 26-year-old soldier accepted to emergency with multisystem penetrating trauma. Comminuted fractures of the right femur, multiple bony and metallic fragments are seen in the soft tissues. Segmental complete occlusions of the distal superficial femoral artery (white arrow) and the distal popliteal artery (black arrow) are seen on 3D reconstructed CT images. Operation revealed an intimal flap in the distal superficial femoral artery and arterio-arterial embolus in the distal popliteal artery
7.5 Clinical Signs of Arterial Injury
Clinical signs of arterial injury are divided into hard signs and soft signs:
-
Hard signs: loss of pulse, expanding hematoma, thrill or bruit, active bleeding, and neurological deficit [21]
-
Soft signs: cold limb, change in color, nonexpanding hematoma, and non-pulsatile bleeding
There is a high correlation between hard signs and arterial injury and a lower correlation when only soft signs are present. Thus, in most studies, the presence of hard signs is an indication for arterial injury evaluation [21, 36]. In other protocols hard signs are an indication for immediate surgical exploration, while imaging is used only in patients with soft signs and an abnormal ankle-brachial index [35].
A practical protocol, used in the authors’ institution, warrants imaging in patients with hard signs in cases of multiple injuries such as explosive injury, while patients with hard signs in single penetrating injuries, like stab wounds, are sent to surgery.
7.6 Imaging Modalities in Arterial Injury
The importance of immediate treatment in vascular trauma necessitates prompt diagnosis. The patient’s condition frequently raises the need to obtain maximum information in minimum diagnostic procedures. Wounded patients require rapid detection, localization, and characterization of the injury [10].
Different imaging modalities may be considered in the evaluation of the traumatized patient.
7.6.1 Doppler Sonography
The advantages of Duplex sonography are well known. It is a noninvasive examination, mostly not painful, and can be done in the patient’s bed in the Emergency Room or in the Operating Theater [32].
In experienced centers, it offers high sensitivity in comparison to the gold standards: digital angiography and surgery [19, 20, 41].
According to Bynoe et al. [4], color Doppler sonography can be used as a screening tool in vascular extremity injury in the stable patient who does not present hard signs of vascular trauma. Their study found that in identifying vascular injury, Doppler sonography demonstrates a sensitivity of 95% and has a specificity of 99% in excluding vascular injury. In an emergency, color flow Doppler and Duplex sonography have a role in the evaluation of a possible vascular damage, especially in proximity injuries [9].
However, Doppler sonography is a time-consuming method and is highly operator dependent [21]. Moreover, this examination is not feasible in open wounds with large soft tissue defects, with surrounding edema, hematoma, and bony fractures [19, 20, 41]. The use of Doppler sonography is limited in the assessment of flow distal to the injury, and the presence of collaterals may interfere with the correct diagnosis [10].
Duplex sonography is also limited by bulky dressings and orthopedic hardware [19]. In addition, Duplex sonography is focused to the suspected region of injury, while unsuspected pathology may be missed.
7.6.2 Magnetic Resonance Angiography (MRA)
Magnetic resonance angiography is an excellent tool in the demonstration of vascular structures.
However, in the setting of acute vascular trauma in most trauma centers, accessibility and monitoring of the critically wounded patient within the magnet is a major problem and not practical [19, 21]. In addition, with penetrating trauma there may be metal pellets that are not compatible with MRI and may result in artifacts [10].
7.6.2.1 Conventional Angiography (CA)
In the past the gold standard of diagnostic modalities in the evaluation of traumatized vessels has been catheter-based conventional angiography.
Conventional angiography, developed in the 1970s, allows an accurate diagnosis of arterial injury and is less invasive than open exploration. It carries an associated morbidity of 1–2% [21], but the benefits of its high diagnostic accuracy and the possibility of percutaneous interventions outweigh the risks.
Conventional angiography may result in significant complications with a 0.6% major complication rate [9]. These include damage to the access vessel like hematoma, thrombosis, dissection, pseudoaneurysm formation, and arterio-venous fistula; distal embolization of atheromatous or thrombotic material; and complications related to the administration of contrast media.
In addition, angiography is a costly and time-consuming procedure that requires the presence of a trained and specialized team including an interventional radiologist, a technician, and a specialized nurse. The time required for the team to arrive at the hospital and the duration of the procedure may delay the definitive treatment that might be critical in a state of emergency [19, 35].
Conventional angiography remains the tool of choice in diagnosing or excluding vascular injury when other noninvasive modalities, namely, CT angiography, fail to perform.
Conventional angiography has a major role when endovascular treatment is recommended.
7.6.3 CT Angiography (CTA)
Despite the high sensitivity, specificity, and accuracy of conventional angiography, its disadvantages raise the need for a noninvasive, quick, accurate, and easily accessible diagnostic imaging alternative.
Imaging of vascular injuries has undergone a dramatic change since the introduction of multi-detector computerized tomography (MDCT). Improved CT technology, providing rapid acquisition of thin axial slices, led to the development of CT angiography. Compared with conventional arteriography, CTA shows excellent sensitivity and specificity in diagnosing occlusive disease in the lower extremities and in other parts of the body [25, 33].
Since 1999, CTA has shown excellent results for imaging traumatic arterial injuries [11, 19, 21] and is continuously replacing conventional catheter angiography as it is in other nontraumatic vascular evaluation [3, 35–37].
Despite the growing use of CTA as the main diagnostic tool in vascular trauma, there are a few disadvantages that must be brought into consideration. Radiation exposure and the use of iodinated contrast material with the possible allergic reaction or renal toxicity are of concern [38]. Radiopaque metallic fragments create beam-hardening artifacts impairing CT angiography. In addition, in CT angiography there is difficulty in the demonstration of the pedal arteries [11, 25]; segmentation of anterior tibial artery from bone is impossible due to the proximity of the vessel to the fibula.
7.6.3.1 CTA Signs of Vascular Injury in the Extremities
CTA signs of vascular injury in the extremities include: active contrast medium extravasation – indicates an ongoing bleeding manifested as a blush of extraluminal contrast material in vicinity to the injured vessel [13, 15] (Fig. 7.28).
A 21-year-old male patient with penetrating trauma to the right lower limb.(a) CT axial image at the level of the thighs shows a large hematoma (arrowhead) in the anterior aspect of the thigh, with air bubbles in an anteroposterior path (thin arrows). Inside the hematoma a blush of extravasated contrast material is noted (thick arrow). Superficial femoral artery is well opacified. (b) 3D-reconstructed image shows torn branches of superficial and deep femoral arteries (arrowhead). The wounded was rushed to surgery because of an unstable cardiovascular state. CT diagnosis was verified
Pseudoaneurysm – formation of an extraluminal sac filled with contrast material, that is, connected to the injured vessel by a neck at the site of mural disruption. Hematoma around an active bleeding or a pseudoaneurysm sac can vary considerably in size [15, 34].
Arterio-venous fistula – early venous filling on arterial phase, raises suspicion of AVF. Sometimes the exact site and nature of the communication between the artery and vein are not defined by CTA and conventional angiography is recommended [15, 37] (Fig. 7.29).
A 21-year-old soldier with penetrating injury to the lower extremity. CT 3D MIP (maximum intensity projection) reconstruction of the lower extremities (a, b) shows a comminuted fracture of the tibia, many metallic pellets below the right knee (thin arrow). Early venous filling in the right lower limb, suspicious of arterio-venous fistula (AVF) is noted (thick arrow). The numerous pellets below the right knee interfere with the visualization of the proximal part of the anterior tibial artery. Conventional catheter angiography was recommended. On conventional angiography (c, d) there was no evidence of AVF; the arteries at the region of the fracture were normal
Acute vessel change in caliber or contour – focal stenosis on CTA may indicate the presence of spasm, dissection, or external compression (Fig. 7.30).
A 22-year-old male with severe multisystem-blast injury. (a) Volume rendering and MIP (b, c) reconstructions of right lower limb shows comminuted fracture of tibia and fibula with multiple bony and metal fragments in the soft tissues. Occlusion of the posterior tibial and peroneal arteries (arrows) as well as segmental narrowing of the proximal anterior tibial artery (arrowhead) due to secondary spasm are noted
Irregularity of the vessel wall with lumen narrowing represents wall injury with partial thrombosis [38]. Intraluminal filling defect – can represent thrombus or intimal flap.
Intimal flap appears linear denoting the presence of focal dissection. Dissection may also appear semilunar, eccentric stenosis, or segmental thrombotic occlusion [15, 37].
Lack of segmental filling and occlusion – segmental vessel occlusion may result from transection or complete rupture (Fig. 7.30). Stenosis of a vessel can progress to lack of opacification and segmental occlusion [31].
The occlusion may vary in length and distal reconstitution may occur via collaterals [15]. Proximity of a projectile tract to a neurovascular bundle and shrapnel less than 5 mm from a vessel, should raise high suspicion of arterial injury [28] (Figs. 7.31–7.33).
A 21-year-old male presented with penetrating blast trauma to the left thigh. Axial image (a), maximum intensity projection (MIP) (b), and volume rendering reconstructions (c), are demonstrated. Hematoma and air are seen in the soft tissues of the left thigh. A large shrapnel (thick arrow) is detected in proximity (0.8 mm) to the superficial femoral artery (SFA) (thin arrow). At surgery, contusion of the SFA was found
A 21-year-old male soldier with a gunshot wound to the left leg. On axial slice (a), beam-hardening artifacts interfere with diagnosis (thin arrows). Coronal 3D reconstruction (b) shows a comminuted fracture in the left fibula. Big shrapnel (thick arrow) is located in proximity to the posterior tibial artery (arrowhead) that is intact
A 22-year-old patient with penetrating trauma to both lower extremities. (a) Reconstructed coronal 3D images show multiple shrapnel in both lower extremities. (b) Axial image at the level of the thighs demonstrates hematoma and air bubbles in the posterior aspect of the left thigh (thick arrow). Two shrapnel are seen in the posteromedial muscles (thin arrows) while no vascular damage is detected. (c) Axial image of the lower pelvis and upper thighs shows a pellet between the femoral artery and vein (arrowhead). At surgery, a hole in the medial aspect of the common femoral artery was found
7.6.3.2 Pitfalls
Occasionally, CT angiography studies may result in poor diagnostic quality. These are due to improper technique, to patient factors, and to source artifacts [21, 28]. Poor timing of contrast material bolus resulting in inadequate vessels opacification is one of the most frequent pitfalls.
Injured patients’ restlessness due to pain or altered mental status may result in motion artifacts. Inability of a wounded patient to raise his upper extremities overhead when performing upper extremity CT angiography may lead to streak artifacts from the adjacent torso.
Streak artifacts as a result of metallic fragments in the soft tissues may interfere with the evaluation of an adjacent vessel and prevent exact diagnosis (Figs. 7.32 and 7.34).
A 32-year-old male with penetrating injury to the chest, abdomen, and lower extremities. Peripheral CTA was performed after chest and abdominal exploration. An axial slice of the lower limbs at the level of the calves shows two pellets in the left posterior muscle, accompanied by hematoma and air bubbles. The arteries below the popliteal trifurcation are intact. Note beam artifacts obscuring but not interfering with the diagnosis
According to Soto et al., in an early study in 1999 using a single detector helical CT, and evaluating traumatized extremities, the sensitivity and specificity of CTA were 90–100% and 100%, respectively [36].
The same group published one more study several years later. Based on this study which also used a single detector helical CT, CTA had a sensitivity of 95.1% and a specificity of 98.7% in significant blunt and penetrating trauma to large extremity arteries [37]. Even better results are achieved in more recent studies, using MDCT.
According to the study of Seamon et al. [35], when comparing CTA, using a multi-detector CT system, to conventional angiography in extremity vascular injury, the sensitivity and specificity of CTA is 100%. The addition of conventional angiography or surgery to extremity CTA studies had no significant contribution to the diagnosis.
Inaba et al. also claim a sensitivity and specificity of 100% in a 3-year study employing MDCT in 59 patients with 63 injured lower extremities evaluated by CTA [19].
Busquets et al. also reported a sensitivity of 100% in evaluating extremity trauma [3].
In addition to the high sensitivity and specificity, CTA offers a number of advantages over conventional angiography. It is a noninvasive examination, readily available in most institutions; it is not as time-consuming as CA and it is cost effective. Moreover, in order to carry out a CTA examination there is no need to assemble a specialized team; it allows the presence of monitoring equipment in close proximity to the critically wounded patient and the clinical team can remain at the CT console observing the patient and the evolving examination [11, 19].
Following data acquisition, multiplanar 3D reconstructions can be easily obtained, facilitating the diagnosis and the planning of further management.
However, axial images should always be reviewed carefully because on the 3D images arterial lumen might be obscured by vascular calcifications as well as by foreign bodies and partial thrombosis [5, 10, 13, 14] (Fig. 7.35).
The authors conclude that in suspected vascular injury, the first diagnostic examination is CT angiography. Conventional angiography is performed only when CTA is suboptimal due to metallic fragments’ streak artifacts, when CTA findings are not definitive and when endovascular treatment is needed, based on CTA findings [11, 19, 31, 36, 37].
Considering radiation exposure, the CT dose index (CTDI) can be received or calculated for the study performed. This is the radiation dose delivered by the CT scanning. The effective dose is a generic estimate of the overall harm to the patient caused by the radiation exposure during the scan [2]. The Health Physics Society (HPS, 1313 Dolley Madison Boulevard, Suite 402, McLean, Virginia 22101) and the Radiological Society of North America (RSNA) estimate the effective dose of abdominal CT to be 10 millisieverts (mSv), which is equal to 3 years of natural background radiation. Brenner and Hall in their review published in the New England Journal of Medicine [2] concluded that when a CT scan is justified by medical need, the associated risk is small relative to the diagnostic information obtained.
7.6.3.3 CTA Technique
A variety of protocols exist, most utilizing a 64 Multi-detector CT [38] or less preferentially a 16 slice machine. Images are transferred through a local hospital network system to a dedicated work station. Images are initially assessed using axial slices followed by 3D reconstructions made by a radiologist or a dedicated technician. Data reconstructions using volume rendering, maximum intensity projection, and multiplanar reconstructions are vital in visualization of the arteries. In many institutes the radiologist and vascular surgeon view the images jointly [38].
Many protocols for a variety of scanners exist. A typical protocol for a 64 slice CTA of the lower extremities usually includes the following parameters: scan length 1,200 mm, slice thickness 2 mm, increment 1 mm, kV 120, mAs 300, resolution standard, collimation 64 × 0.625, pitch 0.703, rotation time 0.5 s. FOV 350 mm, a sharp filter [35], matrix 512, and scan time 22–26 s. For contrast injection an 18 or 20 gauge venous access in the antecubital fossa is needed. Injection of contrast media is preformed with a dual head injector enabling a “chaser” injection of 40 cc saline. And 80–100 cc of contrast media is injected at a rate of 4 cc/s.
Delay of scan is usually determined with a bolus tracking protocol with threshold set at 180 HU and a post-threshold delay of 3 s. Oral contrast agent is not given.
Scanning is done from the level of the superior mesenteric artery for a full length lower extremity CTA or from the inguinal ligament to the feet for a limited CTA. For upper extremity CTA the injured limb is raised above the head to decrease the beam-hardening artifact from the torso, and injection of contrast media is done from the contralateral arm. The 64-row multi-detector CT offers the ability to integrate peripheral CTA into the routine thoracoabdominal trauma imaging protocols [28]. Increased acquisition speed of 3–6 s/body segment allows peripheral CTA and chest or abdominal CTAs to be preformed sequentially as needed. This is especially important in combat injury with multiple penetrating and blunt injuries in multilevel sites.
7.6.4 Endovascular Treatment
The introduction of CTA in the evaluation of suspected vascular injury is changing the role of conventional arteriography in the traumatized patient.
In the author’s institution, conventional arteriography’s main role is in the need for endovascular treatment. Another indication is inconclusive CTA due to metal fragments artifacts.
7.6.4.1 Percutaneous Transcatheter Embolization
Embolization to control active bleeding in the extremities is mainly done in the pelvic vessels and in the proximal branches of the femoral arteries [12, 24].
Grossman et al. recommend embolization also below the trifurcation of the popliteal artery in cases of bleeding and AVF, provided that one continuous vessel remains intact beyond the ankle joint [17].
When treating a pseudoaneurysm, distal and proximal embolization is important. This method, known as “the sandwich technique,” is substantial for the obliteration of antegrade and retrograde flow to the pseudoaneurysm [10].
Embolic agents in use include gelfoam, coils, and glue. A single agent or a combination may be used [10].
7.6.4.2 Stent/Stent Graft
Indications for stent or stent-graft insertion in the setup of vascular injuries include acute pseudoaneurysm, perforation, AVFs, and dissection [26, 32, 39].
There are two types of uncovered stents available: self-expandable and balloon-mounted stents.
Self-expandable stents are preferable in vascular injury because balloon-mounted stents may cause further damage to the arterial wall. Furthermore, in tortuous vessels, the flexibility of self-expandable stents enables rapid deployment whereas with balloon-mounted stents deployment may be difficult [29].
In general, in the traumatized patient, uncovered stents are indicated in dissections and covered stents in pseudoaneurysms and arterio-venous fistulae [29].
In a large series of treatment with covered stents, in 62 patients with peripheral vascular injuries, White et al. report injuries exclusion success rate of 94% [39].
Stent grafts occlude the tear in the arterial wall. They may at the same time also occlude side branches of the artery. In order to prevent this undesired outcome, it is possible to use a combination of uncovered stent with trans-stent coiling of the pseudoaneurysm [1].
Piffaretti et al. report ten cases of blunt trauma to peripheral arteries containing pseudoaneurysms, AVFs, dissections, and expanding hematomas, being treated successfully with endovascular stents [29]. Limb salvage in this retrospective study was 100%.
In this study, in a mean follow-up period of 16 months, only one major late complication, complete stent-graft thrombosis, was detected and was treated successfully endovascularly [29].
Parodi et al. report 29 cases of posttraumatic pseudoaneurysms and AVFs of which 9 were in the extremities, all treated successfully with stent grafts [27].
7.7 Conclusions
In modern combat events, the major number of injuries is caused by blast trauma. Due to the helmet and chest armor that soldiers wear, a growing number of extremity injuries are encountered.
Bones and soft tissue injuries are evaluated by screening radiography and/or computerized tomography.
Vascular damages in the extremities is sometimes limb threatening and even life threatening.
Therefore, prompt and accurate diagnosis is needed for early and precise treatment. Immediate repair of vascular injuries to the limbs improves limb function and reduces mortality from blood loss.
CT angiography is the main diagnostic tool in suspected vascular trauma. It is efficient and accurate in the evaluation of arterial injuries.
Specific CTA signs of vascular injury can be easily detected and additional information regarding bone and surrounding soft tissues is obtained [15].
When CTA is not diagnostic and when endovascular treatment is needed based on CTA findings, conventional catheter angiography is performed.
References
Assali, A.R., Sdringola, S., Mustapha, A., Rhiner, M., Denktas, A.E., Lefkowitz, M.A., Campbell, M., Smalling, R.W.: Endovascular repair of traumatic pseudoaneurysm by uncovered self-expandable stenting with or without transstent coiling of the aneurysm cavity. Catheter Cardiovasc. Interv. 53(2), 253–258 (2001)
Brenner, D.J., Hall, E.J.: Computed tomography: an increasing source of radiation exposure. N. Engl. J. Med. 357(22), 2277–2284 (2007)
Busquets, A.R., Acosta, J.A., Colon, E., Alejandro, K., Rodriguez, P.: Helical computed tomographic angiography for the diagnosis of traumatic arterial injuries of the extremities. J. Trauma 56, 625–628 (2004)
Bynoe, R.P., Miles, W.S., Bell, R.M., Greenwold, D.R., Sessions, G., Haynes, J.L., Rush, D.S.: Non invasive diagnosis of vascular trauma by duplex ultrasonogrphy. J. Vasc. Surg. 14, 346–352 (1991)
Catalano, C., Fraioli, F., Laghi, A., Napoli, A., Bezzi, M., Pediconi, F., Danti, M., Nofroni, J., Passariello, R.: Infrarenal aortic and lower extremity arterial disease: diagnostic performance of multidetector row CT angiography. Radiology 231, 555–563 (2004)
Cernak, I., Savic, J., Ignajatovic, D., Jevtic, M.: Blast injury form explosive munitions. J. Trauma 47(1), 96–103 (1999)
Clouse, W.D., Rasmussen, T.E., Eliason, P.M.A., JL, C.M.W., Bowser, A.N., Jenkins, D.H., Smith, D.L., Rich, N.M.: In-theater management of vascular injury: 2 years of the Balad vascular registry. J. Am. Coll. Surg. 204, 625–632 (2007)
Costa, D.N., Calvacanti, C.F.A., Sernik, R.A.: Sonographic and CT findings in lipohemarthrosis. AJR 188, W389 (2007)
Davidson, B.D., Polack, J.F.: Arterial injuries: a sonographic approach. Radiol. Clin. North Am. 42, 383–396 (2004)
Doody, O., Given, M.F., Lyon, S.M.: Extremities-indications and techniques for treatment of extremity vascular injuries. Injury 39, 1295–1303 (2008)
Engel, A., Soudack, M., Ofer, A., Nitecki, S.S., Ghersin, E., Gaitini, D.E.: Coping with war mass casualties in a hospital under fire: the radiology experience. AJR 193, 1212–1221 (2009)
Entwisle, J.J., De Nunzio, M., Hinwood, D.: Case report: transcatheter embolization of pseudoaneurysm of profunda femoris artery complicating fracture of the femoral neck. Clin. Radiol. 56, 424–427 (2001)
Fishman, E.K., Horton, K.M., Johnson, P.T.: Multidetector CT and three dimensional CT angiography for suspected vascular trauma of the extremities. Radiographics 28, 653–665 (2008)
Fleiter, T., Mervis, S.: The role of 3D-CTA in the assessment of peripheral vascular lesions in trauma patients. Eur. J. Radiol. 64, 92–102 (2007)
Gakhal, M.S., Kamyar, A.S.: CT angiography signs of lower extremity vascular trauma. AJR 193, W49–W57 (2009)
Gonzalez, R.P., Scott, W., Wright, A., Phelan, H.A., Rodning, C.B.: Anatomic location of penetrating lower-extremity trauma predicts compartment syndrome development. Am. J. Surg. 197, 371–375 (2009)
Grossman, M.D., Reilly, P., McMahan, D., Kauder, D., Schwab, C.W.: Gunshot wounds below the popliteal fossa: a contemporary review. Am. Surg. 65, 360–365 (1999)
Hare, S.S., Goddard, I., Ward, P., Naraghi, A., Dick, E.A.: The radiological management of bomb blast injury. Clin. Radiol. 62, 1–9 (2007)
Inaba, K., Potzman, J., Munera, F., Mckenny, M., Munoz, R., Rivas, L., Dunham, M., DuBose, J.: Multi-slice CT angiography for arterial evaluation in the injured lower extremity. J. Trauma 60, 502–507 (2006)
Knudson, M.M., Lewis, F.R., Atkinson, K., Neuhaus, A.: The role of duplex ultrasound arterial imaging in patients with penetrating extremity trauma. Arch. Surg. 128, 1033–1038 (1993)
Miller-Thomas, M.M., West, O.C., Cohen, A.M.: Diagnosing traumatic arterial injury in the extremities with CT angiography: pearls and pitfalls. Radiographics 25, S133–S142 (2005)
Mui, L.W., Engelsohn, E., Umans, H.: Comparison of CT and MRI in patients with tibial plateau fracture: can CT findings predict ligament tear or meniscal injury? Skeletal Radiol. 36(2), 145–151 (2007)
Mustonen, A.O., Koskinen, S.K., Kiuru, M.J.: Acute knee trauma: analysis of multidetector computed tomography findings and comparison with conventional radiography. Acta Radiol. 46(8), 866–874 (2005)
Nicholson, A.A.: Vascular radiology in trauma. Cardiovasc. Intervent. Radiol. 27(2), 105–120 (2004)
Ofer, A., Nitecki, S., Linn, S., Epelman, M., Fischer, D., Karram, T., Litmanovich, D., Schwartz, H., Hoffman, A., Engel, A.: Multidetector CT angiography of peripheral vascular disease: a prospective comparison with intraarterial digital subtraction angiography. AJR 180(3), 719–724 (2003)
Onal, B., Ilgit, E.T., Kosar, K., Akkan, K., Gumus, T., Akpek, S.: Endovascular treatment of peripheral vascular lesions with stent-grafts. Diagn. Intervent. Radiol. 11, 170–174 (2005)
Parodi, J.C., Schonholz, C., Ferreira, L.M., Bergan, J.: Endovascular stent-graft treatment of traumatic arterial lesions. Ann. Vasc. Surg. 13(2), 121–129 (1999)
Pieroni, S., Foster, B.R., Anderson, S.W., Kertesz, J.L., Rhea, J.T., Soto, J.A.: Use of 64-row multidetector CT angiography in blunt and penetrating trauma of the upper and lower extremities. Radiographics 29, 863–876 (2009)
Piffaretti, G., Tozzi, M., Lomazzi, C., Rivolta, N., Caronno, R., Lagana, D., Carrafiello, G.: Endovascular treatment for traumatic injuries of the peripheral arteries following blunt trauma. Injury 38(9), 1091–1097 (2007)
Rich, N.M., Hughes, C.W.: Vietnam vascular registry: a preliminary report. Surgery 62, 218–226 (1969)
Rieger, M., Mallouhi, A., Tascher, T., Lutz, M., Jaschke, W.: Traumatic arterial injuries of the extremities: initial evaluation with MDCT angiography. AJR 186, 656–664 (2006)
Rowe, V.L., Lee, W., Weaver, F.A.: Acute arterial occlusion secondary to trauma. Semin. Vasc. Surg. 22, 25–28 (2009)
Rubin, G.D., Schmidt, A.J., Logan, L.J., Sofilos, M.C.: Multi-detector row CT angiography of lower extremity arterial inflow and runoff: initial experience. Radiology 221, 146–158 (2001)
Saad, N.E.A., Saad, W.E.A., Davies, M.G., Waldman, D.L., Fultz, P.J., Rubens, D.J.: Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics 25, 5173–5189 (2005)
Seamon, M.J., Smoger, D., Torres, D.M., Pathak, A.S., Gaughan, J.P., Santora, T.A., Cohen, G., Goldberg, A.J.: A prospective validation of a current practice: the detection of extremity vascular injury with CT angiography. J. Trauma 67(2), 238–244 (2009)
Soto, J.A., Munera, F., Cardoso, N., Guarin, O., Medina, S.: Diagnostic performance of helical CT angiography in trauma to large arteries of the extremities. J. Comput. Assist. Tomogr. 23(2), 188–196 (1999)
Soto, J.A., Munera, F., Morales, C., Lopera, J.E., Holguin, D., Guarin, O., Castrillon, G., Sanabria, A., Garcia, G.: Focal arterial injuries of the proximal extremities: helical CT arteriography as the initial method of diagnosis. Radiology 218, 188–194 (2001)
White, P.W., Gillespie, D.L., Feurstein, I., Aidinian, G., Phinney, S., Cox, M.W., Adams, E., Fox, C.J.: Sixty-four slice multidetector computer tomographic angiography in the evaluation of vascular trauma. J. Trauma 68, 96–102 (2010)
White, R., Krajcer, Z., Johnson, M., Williams, D., Bacharach, M., O’malley, E.: Results of a multicenter trial for the treatment of traumatic vascular injury with a covered stent. J. Trauma 60, 1189–1195 (2006)
Wolf, S.J., Bebarta, V.S., Bonnett, B.C., Pons, P.T., Cantrill, S.V.: Blast injuries. Lancet 374, 405–415 (2009)
Zierler, R.E., Zierler, B.K.: Duplex sonography of lower extremity arteries. Semin. Ultrasound CT MR 18, 39–56 (1997)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Berlin Heidelberg
About this chapter
Cite this chapter
Engel, A., Militianu, D., Ofer, A. (2011). Diagnostic Imaging in Combat Trauma. In: Lerner, A., Soudry, M. (eds) Armed Conflict Injuries to the Extremities. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-16155-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-642-16155-1_7
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-16154-4
Online ISBN: 978-3-642-16155-1
eBook Packages: MedicineMedicine (R0)