Abstract
Objective
(1) To determine the accuracy of computed tomography (CT) in the evaluation of ligament tear and avulsion in patients with tibial plateau fracture. (2) To evaluate whether the presence or severity of fracture gap and articular depression can predict meniscal injury.
Design and patients
A fellowship-trained musculoskeletal radiologist retrospectively reviewed knee CT and MRI examinations of 41 consecutive patients presenting to a level 1 trauma center with tibial plateau fractures. Fracture gap, articular depression, ligament tear and footprint avulsions were assessed on CT examinations. The MRI studies were examined for osseous and soft tissue injuries, including meniscal tear, meniscal displacement, ligament tear, and ligament avulsion.
Results
CT demonstrated torn ligaments with 80% sensitivity and 98% specificity. Only 2% of ligaments deemed intact on careful CT evaluation had partial or complete tears on MRI. Although the degree of fracture gap and articular depression was significantly greater in patients with meniscal injury compared with those without meniscal injury, ROC analysis demonstrated no clear threshold for gap or depression that yielded a combination of high sensitivity and specificity.
Conclusions
In the acute setting, CT offers high sensitivity and specificity for depicting osseous avulsions, as well as high negative predictive value for excluding ligament injury. However, MRI remains necessary for the preoperative detection of meniscal injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Only recently has the true incidence of concomitant soft-tissue injury in the context of tibial plateau fractures been recognized. In 1979, Schatzker et al. [1] found a 7% incidence of soft-tissue injuries based on physical exam and intraoperative findings in a series of 94 patients with tibial plateau fractures. An arthroscopic series by Hung et al. [2] reported a 52% incidence of soft tissue injuries. A more recent large series using MRI as the “gold standard” demonstrated a 99% incidence of soft tissue injury in patients with operative tibial plateau fractures [3, 4].
Preoperative diagnosis of soft tissue injuries in patients with tibial plateau fractures aids in operative planning. Although the treatment of collateral ligament tear remains controversial [1, 5–7], it is generally agreed that anterior cruciate ligament (ACL) avulsions need to be repaired acutely in order to maintain knee joint stability [8]. Reconstruction of cruciate ligament tears is typically deferred after osseous healing [9]. Meniscal injuries are acutely repaired or debrided to maintain knee joint stability and congruency, and to minimize articular contact pressure [1, 3, 9].
Magnetic resonance imaging (MRI) has emerged as the cross-sectional imaging modality of choice for patients with tibial plateau fractures [3, 4, 10–12]. In addition to its high sensitivity at evaluating soft-tissue injuries, MRI has also been shown to accurately depict the osseous fracture comminution, displacement, and depression in patients with tibial plateau fractures [4, 10–12]. Although there is controversy surrounding the management of these concomitant soft-tissue injuries, Yacoubian et al. [4] found that MRI changed the treatment plan in 23% of 52 patients studied with tibial plateau fracture compared with the operative plan based on conventional radiographs and CT imaging.
Nevertheless, at many institutions, computed tomography (CT) remains the initial, and often the only, cross-sectional imaging study obtained in patients with tibial plateau fractures in the acute setting. The literature has not addressed the sensitivity and specificity of CT for soft-tissue injuries in the setting of tibial plateau fractures.
The purpose of this study was twofold: to determine the accuracy of CT in the evaluation of cruciate and collateral ligament tear and avulsion, and to evaluate whether the presence or severity of fracture gap and articular depression are useful indicators of meniscal injury.
Materials and methods
Patients
Forty-one consecutive patients with tibial plateau fractures examined by knee CT and MRI at a level 1 trauma center between December 2001 and August 2005 were identified retrospectively. Average age was 50 years (range 19–83), including 23 men and 18 women. The average interval between CT and MRI images was 3.3 days. Ninety percent (37/41) of the patients underwent surgical repair of their tibial plateau fractures, 5% were treated non-operatively, and 5% were lost to follow-up. MRI and CT examinations were reviewed at separate sessions by a fellowship trained musculoskeletal radiologist.
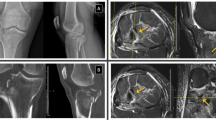
CT images were acquired using either a single-detector helical CT (GE Hi-Speed, General Electric Medical Systems, Milwaukee, Wis.) (n=19 patients) or a 16-detector CT scan (GE Lightspeed, General Electric Medical Systems, Milwaukee, Wis.) (n=19 patients). Axial source images of the knee joint were obtained, along with reformatted coronal and sagittal images. CT images were reviewed for fracture gap and articular depression. The ACL, posterior cruciate ligament (PCL), medial collateral ligament (MCL), fibular collateral ligament (FCL), biceps femoris and iliotibial bands were evaluated using CT in 38 patients for tear or footprint avulsion. Smooth visible ligament contours without obscuration by adjacent soft tissue density suggested intact ligaments (Fig. 1a–c). Insertion site avulsions were deemed indicative of intact corresponding ligaments. Three of the 41 patients were excluded from the CT evaluation of ligament injury due to reconstruction artifact or inadequate coverage of the knee.
A case of intact ligaments. A 36-year-old male struck by a car with resultant Schatzker VI tibial plateau fracture of left knee. Intact ligaments on CT: a PCL; b ACL and PCL; c FCL, biceps femoris, and medial collateral ligament (MCL) d–h Corresponding intact ligaments are demonstrated on MRI. Note that intrasubstance high signal within the ACL and PCL on d, e did not extend to the surface and were classified as sprains. A non-displaced avulsion of the fibular head as seen on image h was not evident on CT. (Long black arrow PCL, long white arrow ACL, black arrow, stippled outline MCL, short white arrow FCL, thick outline arrow biceps femoris)
The MRI studies of all 41 patients were examined for osseous and soft-tissue injuries. The fractures were characterized by Schatzker criteria [1]. Soft-tissue injuries included ligament tear, ligament avulsion, meniscal tear, and meniscal capsular injury. Partial tears were defined as intrasubstance high signal with fiber disruption extending to the surface with some residual intact fibers. Complete tears were defined as complete discontinuity of ligament fibers. Ligament tears were diagnosed if there was partial or complete tear (Fig. 2). Intrasubstance high signal without contour defects, reflecting low-grade ligament sprain, were not considered tears for the purposes of this study, as these do not warrant surgical intervention (Fig. 1). Ligament injury was defined as either ligament tear or ligament avulsion. Meniscal tear was defined as high signal intensity reaching the articular surface or contour abnormality. Meniscal capsular injury was defined as disruption of the meniscofemoral and/or meniscotibial collateral ligament fibers with central meniscal displacement. Meniscal injury was defined as either meniscal tear and/or meniscal capsular injury.
A case of torn ACL, PCL, and MCL ligaments. A 60-year-old female struck by a car, with resultant right knee Schatzker I tibial plateau fracture. a, b On CT images, the normal contours of the ACL (long white arrow) and PCL (long black arrow) are not visible. c The MCL (short black arrow, stippled outline) is obscured by adjacent soft tissue swelling. MRI images (d–f) confirm ligament tears
Statistical methods
The sensitivity, specificity, positive predictive value and negative predictive value of CT for predicting ligament injury were calculated, using MRI findings as the reference standard. SPSS statistical software was used to apply t-tests to examine the statistical significance of the difference in average fracture gap and articular depression in patients with and without meniscal injury. ROC analysis was performed to detect a threshold for fracture gap or depression that yielded a high combination of sensitivity and specificity for predicting meniscal injury.
Results
The classification of the 41 tibial plateau fractures by Schatzker criteria was: 7% (3) Type I, 39% (16) Type II, 12% (5) Type III, 10% (4) Type IV, 12% (5) Type V, and 20% (8) Type VI.
Ligament tear or footprint avulsion
Twenty-five of 38 patients (66%) were found to have ligament injury. The distribution of ligament tears and avulsions, as well as the sensitivity, specificity, positive and negative predictive values of CT, are outlined in Table 1. Two patients had tears of the lateral collateral ligament complex. One patient had an FCL tear seen on CT and MRI, and another patient had a tear of the conjoint tendon seen on MRI with contour obscuration of all three components on CT.
Forty-two percent of patients (16/38) had ligament footprint avulsions, of which ACL avulsions were the most common. Avulsions were detected on CT and MR imaging in all patients, except one patient with non-displaced ACL and FCL avulsions, demonstrated on MRI only. The negative predictive value of CT in the evaluation of individual ligament tear was 98%. Seven percent of patients with no ligament injury detected on CT had at least one torn ligament on MRI. The accuracy of knee evaluations by single-slice helical CT and 16-slice CT was concordant (Table 2).
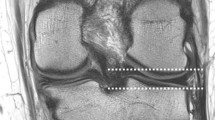
Meniscal tears and/or displacement
Meniscal tear or displacement occurred in 59% (24/41) of patients. Forty-four percent (18/41) of patients had meniscal tear (Table 3). There was no medial meniscal capsular injury. Thirty-four percent (14/41) had lateral capsular injury with central meniscal displacement. Central displacement of the lateral meniscus ranged from 0.4–1.9 cm in the sagittal plane and 0–3.5 cm in the coronal plane.
Fracture gap was significantly greater in patients with meniscal injury (average 1.2 cm, range 0–2.9 cm) compared with patients without meniscal injury (average 0.5 cm, range 0–1.5 cm), P=0.04. Average articular depression in those with and without meniscal injury was 0.9 cm (range 0–2.2 cm) and 0.4 cm (range 0–1.1 cm), respectively (P=0.003).
However, ROC analysis demonstrated no clear threshold for gap or depression that yielded a combination of high sensitivity and specificity. Using fracture gap to identify meniscal injury, the area under the ROC curve was 0.71 (95% confidence interval 0.55–0.87; n=41) (Fig. 3a). Using articular depression to predict meniscal injury, the area under the ROC curve was 0.70 (95% confidence interval 0.54–0.86; n=41) (Fig. 3b).
Discussion
Although orthopedic surgeons have traditionally relied on physical exam, operative findings, and arthroscopy for detection of ligament injury, orthopedists have increasingly accepted MRI as playing a critical role in preoperative assessment [4]. The prevalence of ligament tear or avulsion in our study was 66%, which is comparable to previously reported series. Kode et al. [10] in a study of 22 patients with tibial plateau fractures found 68% had partial or complete ligament tears. A recent study by Gardner et al. [2] in 103 patients with operative fractures demonstrated 77% with complete ligament rupture. The slight variations in ligament injury detection are related in part to the varying definition of injury. We subdivided ligament tears and avulsions since avulsions necessitate acute repair with screw stabilization. We chose to exclude ligament sprain from the ligament injury group since they are not treated operatively.
Our study demonstrated the value of CT in the evaluation of ligament tears and avulsions in patients with tibial plateau fracture. Smooth visible ligament contour without obscuration by adjacent soft tissue density was a reliable CT indicator for excluding ligament injury. Despite the relatively high occurrence of ligament injury, we found that only 2% of ligaments deemed intact on careful CT evaluation had partial or complete tears on MRI. Conversely, CT correctly identified 80% of torn ligaments. It is notable that sensitivity and specificity were not improved by use of 16-detector CT compared with single-detector CT.
As expected, CT reliably demonstrated ligament footprint avulsions due to its excellent spatial resolution and contrast between mineralized cortical bone and adjacent soft tissues. All fractures were detected on CT, except in one patient with non-displaced ACL and FCL avulsions seen only on MR images. This reinforces the superiority of MR imaging at depicting subtle fractures.
In our series, meniscal injury occurred in 59% of patients with tibial plateau fractures, which is comparable with the incidences published reported by Kode et al. [10] based on MRI. In as much as menisci cannot be directly examined utilizing CT, we evaluated if fracture severity could be used to determine meniscal injury. Although we found that average fracture gap and articular depression were significantly greater in patients with meniscal injury compared with those without, we were not able to find a threshold for fracture gap or articular depression that reliably predicted or excluded meniscal injury. In fact, three of the six patients in our series with no fracture gap or depression had meniscal tears. Gardner et al. [7] studied fracture depression and gap using conventional radiographs and found that in individuals with at least 6 mm depression and 5 mm widening, 83% had lateral meniscal tear or capsular separation on MRI. However, below these thresholds, 50% of patients still had lateral meniscal damage. Shepherd et al. [13] found an incidence of 80% meniscal tear based on MR in patients with non-displaced or minimally displaced tibial plateau fractures which would be deemed non-operative by accepted orthopedic criteria. Thus, the severity of fracture displacement does not predict meniscal injury.
Limitations must be acknowledged. In this retrospective analysis of 41 patients, MR findings of ligament and meniscal injury were used as the gold standard for soft tissue injury without operative or arthroscopic confirmation. Interobserver variability was not evaluated, nor was the impact of subspecialty musculoskeletal radiology training on accuracy.
Globally, CT machines are more widely available than MR imaging. In the acute setting, CT examination is readily accessible for the immediate investigation of tibial plateau fracture pattern. A high-quality and carefully interpreted CT examination provides reliable information about tibial plateau fracture pattern, avulsive fractures and concomitant ligament tears. It must be recognized that the shortcoming of CT is that it remains unreliable for predicting unstable meniscal injuries that would require operative treatment.
References
Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res 1979;99:94–104.
Hung SS, Chao EK, Chan YS, et al. Arthroscopically assisted osteosynthess for tibial plateau fractures. J Trauma 2003;54:356–63.
Gardner MJ, Yacoubian S, Geller D, et al. The incidence of soft tissue injury in operative tibial plateau fractures. A magnetic resonance imaging analysis of 103 patients. J Orthop Trauma 2005;19:79–84.
Yacoubian SV, Nevins RT, Sallis JG, Potter HG, Lorich DG. Impact of MRI on treatment plan and fracture classification of tibial plateau fractures. J Orthop Trauma 2002;16:632–7.
Delamarter RB, Hohl M, Hopp E Jr. Ligament injuries associated with tibial plateau fractures. Clin Orthop Relat Res 1990;226–33.
Moore TM, Meyers MH, Harvey JP Jr. Collateral ligament laxity of the knee. Long-term comparison between plateau fractures and normal. J Bone Joint Surg Am 1976;58:594–8.
Gardner MJ, Yacoubian S, Geller D, Pode M, Mintz D, Helfet DL, Lorich DG. Prediction of soft-tissue injuries in Schatzker II tibial plateau fractures based on measurements of plain radiographs. J Trauma 2006;60:319–23.
Burri C, Bartzke G, Coldewey J, Muggler E. Fractures of the tibial plateau. Clin Orthop Relat Res 1979;84–93.
Honkonen SE. Indications for surgical treatment of tibial condyle fractures. Clin Orthop Relat Res 1994;302:199–205.
Kode L, Lieberman JM, Motta AO, Wilber JH, Vasen A, Yagan R. Evaluation of tibial plateau fractures: efficacy of MR imaging compared with CT. Radiology 1994;163:141–7.
Holt, MD, Williams LA, Dent CM. MRI in the management of tibial plateau fractures. Injury 1995;26:595–9.
Brophy DP, O’Malley M, Lui D, Denison B, Eustace S. MR imaging of tibial plateau fractures. Clinical Radiology 1996;51:873–8.
Shepherd L, Abdollahi K, Lee J, and Vangsness CT Jr. The prevalence of soft tissue injuries in nonoperative tibial plateau fractures as determined by magnetic resonance imaging. J Orthop Trauma 2002;16:628–31.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
W. Mui, L., Engelsohn, E. & Umans, H. Comparison of CT and MRI in patients with tibial plateau fracture: can CT findings predict ligament tear or meniscal injury?. Skeletal Radiol 36, 145–151 (2007). https://doi.org/10.1007/s00256-006-0216-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-006-0216-z