Abstract
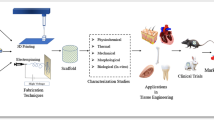
Tissue engineering is an interdisciplinary field aimed at the application of the principles and methods of engineering and life sciences toward the fundamental understanding of structure–function relationships in normal and pathological mammalian tissues and the development of biological substitutes to restore, maintain, or improve tissue functions [8, 38, 56, 57, 78, 111]. Typically, this involves collaborative efforts between materials scientists, cell and molecular biologists, immunologists, surgeons, and engineers to create replacement tissues that will be accepted by the body and promote native extracellular matrix (ECM) production. This requires the use of materials that do not activate catabolic pathways in the body, ultimately leading to fibrous encapsulation or destruction of the material [25, 78, 104, 111].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tissue Engineering
- Silk Fibroin
- Fabrication Technique
- Tissue Engineering Application
- Tissue Engineering Scaffold
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Tissue engineering is an interdisciplinary field aimed at the application of the principles and methods of engineering and life sciences toward the fundamental understanding of structure–function relationships in normal and pathological mammalian tissues and the development of biological substitutes to restore, maintain, or improve tissue functions [8, 38, 56, 57, 78, 111]. Typically, this involves collaborative efforts between materials scientists, cell and molecular biologists, immunologists, surgeons, and engineers to create replacement tissues that will be accepted by the body and promote native extracellular matrix (ECM) production. This requires the use of materials that do not activate catabolic pathways in the body, ultimately leading to fibrous encapsulation or destruction of the material [25, 78, 104, 111].
Natural and synthetic ECM analogues have played a vital role in the field of tissue engineering since the early 1980s [8, 17, 119]. Improvements in the fabrication process as well as scaffold structure continue to occur with hopes of finding an ideal scaffold for each specific tissue engineering application. The overall function of the biodegradable scaffold is to create a three-dimensional microenvironment that will provide the necessary support for the transplanted or host cells to induce normal physiologic regeneration and function. Ideally, the scaffold should mimic the native ECM it is going to replace. In order for this to happen, several design considerations should be taken into account including fabrication, structure, biocompatibility, and biodegradability [17]. Many different materials have been used to create scaffolds for different tissue engineering applications, each one offering different features and characteristics. More information will be given later in this chapter about these design considerations and the different materials used to fabricate various ECM analogues.
Fabrication techniques for scaffolds range from traditional engineering methods such as solvent casting and particulate leaching, to computer-aided design (CAD) technologies consisting of techniques such as 3D printing and solid-freeform fabrication (SFF). Other processes include textile techniques such as electrospinning and weaving, and decellularization of tissues [11]. This chapter focuses on some of these fabrication processes in greater detail.
Although tissue engineering scaffolds have come a long way since they were first introduced, there are currently very few products on the market to show for their success. As for the products that are available, even though they have made a remarkable impact in the medical industry and have improved the quality of life for many, there are still several limitations and drawbacks, which are discussed in Sect. 4.
2 Aim of the Discipline
2.1 Tissue Engineering ECM
The use of isolated cells or cell substitutes is the most direct tissue engineering approach, typically using autologous or allogenic cells as therapeutic agents. This allows for the replacement of cells in areas of damaged tissue, ultimately using the cell’s ability for replication to promote tissue repair and resume function [57, 78]. These cells can be differentiated and tissue specific (i.e., injecting chondrocytes into cartilage [40]) or can be undifferentiated, generic stem cells that could be injected into areas of damaged tissue and allowed to differentiate as needed [18, 104]. The upside of such an approach is the avoidance of surgery, as well as the ability to manipulate cells as needed in vitro prior to their implantation into the body. However, the major drawback of this approach is the time required to culture a usable number of cells. Without the presence of a large universal cell bank, cells must be taken from a donor and cultured to a usable number prior to the implantation in their eventual recipient [57, 104].
Another approach to tissue engineering is the use of either precellularized or acellular ECM analogues. The use of matrix analogues may be the most challenging, albeit potentially the most beneficial, approach to tissue engineering. The ultimate goal of this approach to tissue engineering is to enhance the body’s ability to heal and repair itself by introducing a scaffold that the body recognizes and incorporates directly into the reparative process of the tissue. These systems are meant to mimic the native ECM and can serve as a structural framework for both cells and signaling molecules using the body as a bioreactor, exerting normal physiologic, biomechanical, and biochemical signals upon the scaffold. The idea being that the ECM analog will induce cells to more accurately reproduce their normal physiological behavior, thereby improving tissue regeneration and repair [8, 9, 105]. A number of tissue-inducing signaling molecules have been incorporated into ECM analog scaffolds to aid this process. These signaling molecules can include a wide number of cytokines and chemokines to promote cell growth, instruct differentiation, and promote cellular migration [78]. Since they are open to immunological attack, much research has been done on the material composition of these matrix analog systems in order to produce matrices that elicit little to no immune response and most closely mimic both the structure and function of native ECM.
2.2 Native ECM
Mammalian tissue is composed of two major components: cells (both parenchymal and mesenchymal) and ECM. A large majority of the tissue volume is composed of the ECM component, which also provides much of a tissue’s geometric shape. From a structural standpoint, the ECM is a complex arrangement of proteins and polysaccharides such as collagen, hyaluronic acid, proteoglycans, glycosaminoglycans, and elastin (Table 3.1). These ECM components are constantly being synthesized, secreted, oriented, and modified by the cellular components that they support. Historically, the function of the native ECM was only believed to be a structural framework for tissues. However, it is now understood that the ECM, through interaction with receptors on the surfaces of cells, directly takes part in promoting cell adhesion, migration, growth, differentiation, and apoptosis. The ECM also plays a role in cytokine activity and intracellular signaling. Growth factors and signaling molecules can be stored within the ECM to preserve against their degradation, or they can attach to the surface of the ECM to present themselves more efficiently to the cell receptors [25, 65, 78].
Interactions between the cells and the ECM are complex and dynamic and play critical roles during development, wound healing, and environmental maintenance (Fig. 3.1). During development, the cell–ECM interaction is responsible for pattern formation, morphogenesis, and phenotype acquisition and maintenance. During the wound healing process, clot formation, inflammation, formation of granulation tissue, and remodeling are all mediated by the cell–ECM interaction. Initial attraction and adhesion of the cells to the ECM is induced by multiple, low affinity charge and hydrophobic interactions. During the spreading phase of adhesion, heterodimeric transmembrane proteins known as integrins on the cell surface bind to specific small peptide fragment sequences on the ECM molecules. This allows for the cells to bind to the ECM, through focal adhesions, and promote direct communication between the two. Integrin binding is both specific and reversible and allows the cells to differentiate, secrete and absorb the matrix, and transmit signals [25]. Signals are sent from the ECM across the cell membrane to the soluble molecules in the cytoplasm and through direct connections with the cytoskeleton into the cell nucleus, evoking a cellular response, termed “outside-in” signaling. This direct contact allows for stronger, more specific signaling than through the release of diffusible signaling molecules. The cell–ECM interactions can also be of an “inside-out” nature, when changes within the cell feed back to alter the activity of surface receptors, ultimately creating changes in the integrin and nonintegrin receptors in focal adhesions [25]. In what is known as dynamic reciprocity, the cellular response to the ECM signaling can often alter the state of the ECM. For example, the cells may release matrix metalloproteases to break down an overly dense ECM to allow for their migration or proliferation [65, 78].
ECM–cell interaction depicting integrin receptors. Reprinted from [78]
2.3 ECM Analog Scaffolds
As complex a structure as the native ECM has been revealed to be, it should be no surprise that the creation of a successful engineered ECM analog has proven to be extremely challenging. Ideally, one would like to mimic both the fibrillar form and the complex function of the native ECM [1, 11, 128]. To attain a successful ECM analog scaffold, there are several design and material criteria that must be met. First and foremost, the scaffolding material should be subjected to the same standards as any other biomaterial implanted in the body, namely, the scaffold should not initiate any adverse tissue or immune reactions. For many applications, scaffolding materials should be biodegradable or bioabsorbable at a rate that will allow for their gradual incorporation into the surrounding tissue without any fibrous encapsulation or residual evidence of their presence [1, 11, 111, 119]. ECM analog scaffolds have been fabricated from an extensive array of materials through a number of different fabrication techniques. A wide number of different polymers, both synthetic and natural in origin, have been used as ECM analogues. The most common matrix materials in use today are polymers such as poly(glycolic acid) (PGA), poly(lactic acid) (PLA), and their copolymer, polylactide-co-glycolide (PLGA). However, extensive work has also been done with polycaprolactone (PCL) and polydioxanone (PDO), as well as some polyanhydrides, polyorthoesters, polycarbonates, and polyfumarates [1, 111]. For ECM analogues engineered from natural materials, collagens [66], elastin [90], fibrinogen [113], and silk [4] have been used. ECM substitutes of this variety have the potential for a greater upside than their synthetic counterparts due to the fact that they are constructed from native ECM materials and may be expected to retain some of their biologic behavior [74, 111]. Inorganic materials such as hydroxyapatite, tricalcium phosphate, ceramics, and glass have also been used [91, 111]. Both the materials and their fabrication techniques will be discussed in detail later in this text.
The architecture of the scaffold is every bit as important as the material from which it is fabricated. As previously stated, an ECM analog should mimic the form of the native ECM. To be ideal, this ECM analog would need to mimic the topographical features and geometry on the macroscale, microscale, and even nanoscale levels, as each influences the cell response to the scaffold [77]. Native ECM is composed of nanoscale fibers that can provide structural integrity to the tissues. Recent advances in fabrication techniques (self-assembly, phase separation, and electrospinning) have made the creation of consistently nanofibrous scaffolds possible. The use of nanofibrous scaffolds creates structures with a very high surface area to volume ratio to support cell growth and infiltration [107, 119, 128]. In addition, the morphological similarities between the nanofibrous structures and the native ECM are believed to improve cellular response and overall biocompatibility [128].
Success of a tissue engineering scaffold in many applications is ultimately dependent upon the ability of the cells to infiltrate the ECM analog, migrate throughout its thickness, proliferate, and restore normal physiologic function [10, 100]. The scaffold’s porous structure, a combination of microporous (pore diameters <2 nm), mesoporous (pores with diameter 2–50 nm), or macroporous (pore diameters >50 nm) void spaces, plays a major role in cellular penetration [60, 74]. As yet, there has been no concrete claim to an ideal pore diameter, but it has been documented that pores with a small diameter, yet larger than the diameter of a cell, are favorable [119]. Not only do the pores of an ECM analog scaffold need to be of a sufficient size for tissue growth to occur, but they also need to be open and interconnected. Interconnectivity refers to the extent of which the pores are connected with their neighboring pores, and has a large effect on nutrient and waste diffusion, cell migration, and overall scaffold permeability [52, 61, 111]. The terms porosity and permeability are often incorrectly used interchangeably in the realm of tissue engineering and in the consideration of ECM analog scaffolds. By definition, porosity is the amount of void space contained within a structure, while permeability is a measure of the ease with which a fluid can move through the structure. Matrix permeability ultimately depends on the combination of scaffold porosity, pore size and distribution, pore interconnectivity, and pore orientation and scaffold porosity to determine the hydraulic permeability of an ECM analog scaffold [52, 61].
Although not commonly reported for tissue-engineered scaffolds, permeability and porosity are extremely important to the success of an ECM analogue. Healthy, living tissue in vivo relies on the microvasculature to distribute blood and exchange metabolites through a combination of diffusion over short distances and flow-limited exchange. There are currently no tissue-engineered products that contain their own prevascularized capillary bed to provide nutrients to the structure, chaining their initial effectiveness to the limits of passive diffusion [51]. The limitations of diffusion-based nutrient transport restrict the maximum thickness of avascular tissue-engineered constructs to less than 2 mm [34]. Scaffolds with increased porosity and permeability help promote the diffusion of nutrients to cellular constituents, while promoting the diffusion of metabolic waste away from the cells. An increase in nutrient penetration distance will promote cell migration away from the scaffold periphery, and the presence of interconnected macropores will augment their ability to migrate [52, 61]. The degradation behavior of synthetic polymer-based scaffolds is also controlled in part by the permeability of the ECM analog. Low porosity and permeability scaffolds made of poly(α-hydroxy acids) have exhibited increased rates of degradation due to an increase in autocatalytic activity. Essentially, as the polymers breakdown via hydrolysis, the acidic byproducts become trapped within the scaffold and lower the local pH. This reduced pH then accelerates the degradation of the polymer from the inside-out resulting in a rapid loss of mechanical stability [52, 88].
3 State of the Art
3.1 Synthetic Scaffolds
Synthetic scaffolds, as mentioned above, have been used as ECM analogues and offer many advantages over natural polymers, as well as limitations. For one, the material properties of the synthetic polymers can be controlled to suit specific functions, and therefore, can be more beneficial as a scaffold for multiple tissue engineering applications. In addition, many synthetic polymers are bioresorbable and have a known degradation rate, mechanical strength, and are readily available, and therefore, degradation time should not vary significantly between hosts [11]. Synthetic scaffolds provide many positive characteristics for their use as scaffolding materials, and almost seem to be the answer for ideal tissue engineering scaffolds, but the key dilemma is that they lack one of the major requirements of an ECM analog. Although the surface and structural characteristics of the synthetic polymers can be controlled, they are synthetic, as their name implies, and therefore, are deficient in the biological component of the native ECM [8, 114]. Another disadvantage is that the degradation products of these polymers can be toxic products, mostly weak acids, which can cause an adverse reaction if they accumulate locally [119].
Biodegradable synthetic polymers have been the primary focus for tissue-engineered scaffolds, with most belonging to the polyester family. Some of the most commonly used polymers will be more specifically outlined in the following paragraphs. A brief overview of the polymers’ characteristics is displayed in Table 3.1 [11, 35, 106, 119].
3.1.1 Poly(Glycolic Acid)
PGA is a biodegradable, linear, aliphatic polyester that possesses a compact, repeating structural unit [14, 114, 119] (Table 3.2; Fig. 3.2). It is currently used in a variety of medical applications, but was initially developed as a commercially available suture in the 1970s because of its superior biocompatibility and reproducible mechanical properties [8, 27]. PGA is formed from the ring opening polymerization of glycolide and produces high molecular weight materials [70]. Some characteristics of PGA include a high crystallinity (46–55%), a high melting point (185–225°C), a glass transition temperature of 35–40°C, and a low solubility in organic solvents [14, 27, 35, 70, 119]. The glass transition temperature of PGA is very close to physiological temperature (35–40°C), and thus, water infiltration and loss of mechanical strength may occur more easily after implantation. Mechanical properties of PGA sutures include a tensile strength of 106 Kpsi, an elongation of 24%, and a knot retention of 65 Kpsi [8, 12]. Due to its hydrophilic nature, PGA degrades into glycolic acid over a period of 2–4 weeks in vivo. The predictable bioabsorption of this polymer and the fact that its degradation product is metabolized in the body makes it an attractive option for many tissue engineering applications. More specifically, for applications where an initially tough, but fast degrading material is desired, this polymer is a superior choice, as 60% of its strength is lost by hydrolytic degradation during the first 2 weeks.
Chemical structures of biodegradable synthetic polymers. [114]
PGA scaffolds have previously been formed by traditional extrusion methods [71], electrospinning [13], and solvent casting or particulate leaching [35] (fabrication techniques discussed later). Extrusion methods produce fibers with a minimum diameter above 10 µm which is a highly unfavorable size compared to native ECM analogues. Electrospinning methods have produced fibers of 200 nm–1.5 µm, depending upon polymer concentration. During an in vitro biocompatibility study, PGA scaffolds that were pretreated with hydrochloric acid demonstrated the ability to increase the rates of proliferation of cardiac fibroblasts compared to the cells on tissue culture plastic. In vivo studies with the same scaffolds resulted in full incorporation of the scaffolds into the hind leg tissue of rats [14]. Freed et al. demonstrated that PGA nonwoven mesh scaffolds seeded with chondrocytes have the ability to aid in cellular attachment and proliferation and the regeneration of cartilaginous matrix [27].
3.1.2 Poly(Lactic Acid)
Another biodegradable, aliphatic polyester commonly used in clinical applications is PLA [8] (Table 3.2; Fig. 3.2). Formed from the polymerization of lactide, this polymer is present in two isoforms: d(-) for dexorotary, l(+) for levorotary, and the synthetic blend, dl for racimic [70]. P(l)LA and P(d)LA are semicrystalline solids, and P(dL)LA is amorphous. The difference in the polymer’s crystallinity has an effect on its clinical application. P(dL)LA is usually used in drug delivery applications because of its low tensile strength, high elongation, and rapid degradation time, while the semicrystalline PLA is preferred for load-bearing applications such as orthopedic fixations and sutures because of its higher tensile strength and modulus and lower elongation [114, 70]. Because of the extra methyl group in the monomer, PLA is more hydrophobic than PGA. The chemical structure of PLA contains an ester bond, which makes it less likely to undergo hydrolysis. Because of this, it degrades much slower than PGA (typically 30–50 weeks) and has a higher solubility in organic solvents. Since the degradation of PLA yields l-lactic acid, for most tissue engineering applications, P(l)LA is chosen over P(d)LA, because lactic acid is naturally present and metabolized in the body [8, 35, 114, 119]. Other characteristics of PLA include 37% crystallinity, a melting point of 96–185°C, and a glass transition temperature of 57–65°C [114, 70]. It is important to mention that caution should be taken when sterilizing this polymer via gamma-radiation, because this may cause chain separation, cross-linking, and a decrease in crystallinity.
PLA scaffolds have been processed using traditional fiber extrusion methods, similar to PGA, and have resulted in fiber diameters on the microscale. Electrospun PLA scaffolds produce fibers with diameters ranging from 100 nm to 10µm, depending upon the solvent and concentration. In vitro experiments done by Yang, et al. demonstrate neural stem cell elongation and outgrowth parallel to the direction of P(l)LA fibers and higher cell differentiation for P(l)LA nanofibers vs. microfibers [116]. Human articular chondrocytes cultured on PLA scaffolds formed from a spin-casting method revealed that cellular attachment was increased on P(dL)LA scaffolds vs. P(l)LA scaffolds. In contrast, cellular proliferation was greater on P(l)LA scaffolds as compared to P(dL)LA scaffolds. This is most likely due to the differences in crystallinity of the two polymers, which could cause a difference in the amount of serum proteins that are absorbed [45].
3.1.3 Poly(Lactide-Co-Glycolide)
PLGA (Table 3.2; Fig. 3.2) is the copolymer formed by PGA and PLA. Unlike each individual homopolymer, this copolymer is amorphous when either monomer is present below 70 mol% because of the disruption of the regularity of the polymer chain by the other monomer [70]. This characteristic results in a decrease in the degradation rates and mechanical strength [114, 119, 130]. If either homopolymer is present above 70 mol%, the copolymer exhibits some crystallinity. PLGA also exhibits lower crystallinity and melting temperature compared to PGA or PLA. This copolymer degrades in bulk by ester hydrolysis (Table 3.2), and the rate of degradation can be altered by adjusting the ratio of PLA/PGA.
PLGA has been used for many medical and tissue engineering applications such as surgical sutures, cardiac tissue regeneration, and drug delivery, because it is biodegradable and biocompatible [8, 55, 130]. Bone formation on PLGA foams fabricated by solvent casting/particulate leaching (to be discussed later) by mesenchymal stem cell-derived osteoblasts has also been reported [120]. PLGA scaffolds have also been shown to support the cell growth and function of a variety of other cell types including fibroblasts, chondrocytes, and smooth muscle cells (SMCs) [55, 119].
3.1.4 Polydioxanone
PDO is a biodegradable polyester formed from the ring opening polymerization of the monomer paradioxanone [16, 70] (Table 3.2; Fig. 3.2). Originally, this polymer was developed for use as a suture because of its superior degradation rate of 6–12 months, falling in between PGA and PLA. PDO exhibits a high crystallinity of 55% and a glass transition temperature of −10–0°C. Another attractive property is its excellent flexibility because of an ester oxygen group in the backbone structure [8, 16, 70]. In addition, PDO has shown no acute or toxic effects upon implantation. A negative aspect of the polymer when used as a suture is its shape memory. Because of the suture’s ability to retain its spooled shape, knot retention becomes very difficult. Although this may prevent PDO from being an ideal suture material, shape memory may be a positive aspect for tissue engineering applications. For example, if used in a vascular graft, it can provide rebound and kink resistance [8, 16, 70]. Also, the degradation rate of PDO sutures can be a negative aspect, because it may be too rapid to allow for a durable closure of wounds and may cause abnormal healing.
Electrospinning of PDO has been performed and has resulted in fiber diameters of 180 nm–1.4 µm, depending upon the solution concentration, and exhibits material properties within the same range as the major structural components of the native vascular ECM (collagen and elastin). As fiber diameter decreases, it has been shown that cell interaction improves and immune response is reduced [8, 16]. PDO scaffolds have also been used in other applications including orthopedics, plastic surgery, drug delivery, cardiovascular, and bone repair [16].
3.1.5 Polycaprolactone
PCL is another linear aliphatic polyester that has demonstrated good biocompatibility, favorable mechanical properties, and a slow degradation rate of 1–3 years [8, 35, 106] (Table 3.2; Fig. 3.2). Prepared by the ring opening polymerization of the cyclic monomer ε-caprolactone, PCL is a repeating unit of one ester group and five methylene groups [35, 70, 119]. This semicrystalline polymer is highly soluble and exhibits a low melting point of 58–64°C and a glass transition temperature of −60°C [35, 70, 119]. Degradation of PCL occurs by bulk or surface hydrolysis of the ester linkages, producing a byproduct of caproic acid [119]. To increase its degradation rate, PCL has been easily copolymerized with a variety of polymers including collagen, PGA, PLA, and poly(ethylene oxide) (PEO) [8, 35, 70, 119].
Electrospun scaffolds of PCL that were seeded with mesenchymal stem cell-derived osteoblasts promoted cellular penetration as well as ECM formation [120]. Other studies have shown that PCL scaffolds support human osteoblast and dermal fibroblast cell viability and the proliferation of human biliary epithelial cells [119]. PCL scaffolds have also been used for cartilage [26] and vascular tissue engineering applications [108].
3.1.6 Poly(Ethylene Glycol)/Poly(Ethylene Oxide)
Poly(ethylene glycol) (PEG) is a linear-chained polymer consisting of an ethylene oxide repeating unit (Table 3.2). PEO has the same backbone as PEG, but a higher molecular weight because of its longer chain length [119]. PEG and PEO are both hydrophilic and are synthesized by anionic or cationic polymerization of ethylene oxide [59, 119]. They have the ability to act as swelling polymers, which has led to their use as a hydrogel, and makes them excellent polymers for medical applications such as drug delivery [82]. Another attractive property for their use in tissue engineering is their low toxicity and biocompatibility [59]. A limitation of PEG and PEO is their inability to naturally degrade, but if they are copolymerized with a hydrolytically or enzymatically degradable polymer, they can be made degradable [59, 119, 121]. PEO-based copolymers, such as the triblock copolymer with poly(propylene oxide) (PPO), PEO-PPO-PEO, could be designed to form gels at body temperature by forming a liquid crystalline phase, and have been mainly used in drug delivery applications, where they have been known to enhance drug penetration [59]. Riley et al. cultured chondrocytes on PEG-based hydrogel scaffolds and found that the scaffolds supported the survival of the cells and the deposition of a cartilage-like matrix [84].
3.2 Natural Scaffolds
To overcome the disadvantage that synthetic polymers have of lacking the biological component, natural polymers are widely used, either by themselves, or as a blend with synthetics. Derived from renewable resources such as plants, animals, and microorganisms, natural polymers used in scaffolds offer an advantage because of their excellent biocompatibility and biodegradability [33]. They are biologically similar to the native ECM, which allows the cells to interact with these polymers in a natural manner through receptors and signals, and also aids in the correct functioning of the cells such as attachment, proliferation, and differentiation. Disadvantages of natural polymers include variations in degradation rates, batch-to-batch inconsistency, and poor mechanical strength [8, 17, 119]. Another important disadvantage to consider is the ability of these polymers to induce a negative immune response due to the presence of impurities and endotoxins, depending on their source [33]. A detailed description of some of the most widely used natural polymers in tissue engineering is discussed below.
3.2.1 Collagen
Collagen is the most abundant protein found in the body. It functions to provide the overall structure and strength to the tissues and is the principal component of the native ECM. In addition, the collagen structure provides the cells with the appropriate microenvironment for embryologic development, organogenesis, cell growth, and wound repair and also stores and releases important cell mediators such as growth factors [8, 33]. Currently, there are over 20 different kinds of collagen that have been identified, with the basic structure composed of three polypeptide chains, coiled around each other to form a triple helix (Fig. 3.3).
Picture depicts triple-helical collagen structure. (a) Model of collagen peptide where Gly is green, Pro is gray, and Hyp is shown in magenta. (b) The schematic of the triple helix. [33]
The most common triple helix of collagen is formed by the peptides, proline, hydroxyproline, and glycine in the sequence Pro–Hyp–Gly. The individual triple helices arrange to form collagen fibrils, which account for the structural integrity of the tissue. Collagen fibril formation is an extracellular process, which occurs through the cleavage of terminal procollagen peptides by specific procollagen metalloproteinases. The different types of collagen are found in different areas of the body depending upon the role and makeup of the tissue. Type I collagen is the most common type, found in the dermis, bone, tendon, fasciae, sclera, organ capsules, and fibrous cartilage, and is a major component of mature scar tissue. Type II collagen is mostly found in hyaline and elastic cartilage, the developing cornea, and in the vitreous body of the eye. The wall of the blood vessels and hollow intestinal organs consist mostly of type III collagen, which also copolymerizes with type I. Types V and XI are less abundant and mostly occur copolymerized with type V and type XI [85]. One reason for collagen’s wide use in tissue engineering applications is that it can be isolated from many different sources and is relatively nonimmunogenic. The primary sources of collagen are animal tissues (porcine and calf skin, bovine tendon, rat tail), in which it is purified from the tissues using an enzymatic treatment and salt/acid extraction. Deriving this polymer from animals, although an easily accessible source, does pose some problems for its use as a scaffold because of the possibility of the transmission of infectious agents and rejection from the host tissue. Fortunately, many new attempts have been made to derive collagen from safer sources, such as jellyfish [95], and to produce human recombinant collagen [115]. These alternatives provide a more reliable and predictable source of collagen that is free of animal components.
One feature that is necessary for all types of collagen for their use in tissue engineering applications is chemical cross-linking. Although this process can be a disadvantage for this natural polymer’s use in tissue engineering applications because of the addition of toxic solvents, this is necessary to stabilize the polymer in order to control the mechanical properties. Cross-linking can be achieved in various ways, including chemically (glutaraldyhyde, EDC, genipin), physically (freeze drying, UV radiation, heating), and enzymatically [85, 33].
Degradation of collagen is done naturally by matrix metalloproteinases, specifically collagenase and serine proteases [85], which also provide an advantage for its use in tissue engineering. It is used in various medical applications, such as wound dressings and artificial skin, and collagen scaffolds have also been used in a variety of tissue engineering applications, such as vascular grafts [15], tendon/ligament [30, 31], cartilage [99], and breast tissue [41].
Some drawbacks of collagen for tissue engineering applications include the polymer’s low mechanical properties, the need for cross-linking (mentioned above), risk of viral infection, increased antigenicity potential, and an extremely fast biodegradation rate [85].
3.2.2 Gelatin
Gelatin is obtained by a controlled hydrolysis of collagen and is a natural polymer that is of interest in tissue engineering because of its excellent biocompatibility and biodegradability, and cost efficiency. Generally speaking, there are two types of gelatin: Type A and Type B. Type A is extracted from collagens, and processed by an acidic pretreatment, and Type B is obtained by an alkaline pretreatment, which causes it to have higher carboxylic acid content than Type A. For many years, it has been used as a vascular prosthetic sealant, a dressing for wounds, and a carrier for drug delivery, and recently, it has gained interest for its use as a scaffold for tissue engineering applications [8, 127]. One drawback of gelatin is that it dissolves as colloidal sol at temperatures at or above 37°C, and gels at lower temperatures around room temperature. However, when combined with other synthetic polymers, or cross-linked, this limitation can be reduced.
In a study done by Zhang et al., a mixture of gelatin and PCL solutions were electrospun to produce fibrous scaffolds. These scaffolds proved to have excellent biocompatibility with bone marrow stromal cells and also aided in the process of cellular migration, proliferation, and penetration [126]. Gelatin scaffolds have also been used for nerve [32], hepatic [48], and cartilage [98] tissue engineering applications.
3.2.3 Elastin
Elastin is the most linearly elastic biosolid known and is a key structural protein found in the native ECM of connective tissues where elasticity and recoil are critical parameters (Fig. 3.4). Elastin consists of several repetitive amino acid sequences, including VPGVG, APGVGV, VPGFGVGAG, and VPGG [33]. Mature elastin is formed from tropoelastin, a 70-kDa protein consisting of alternating hydrophobic regions (responsible for the elasticity) and cross-linking domains. Additionally, it ends with a hydrophilic carboxy-terminal sequence containing its only two cysteine residues [23]. A highly insoluble protein, elastin constitutes the walls of arteries and veins, ligaments, lung parenchyma, skin, and intestines.
Elastin structure reprinted from [33], © Elseiver
There are some drawbacks of elastin that have limited its use as a biomaterial. Upon implantation, elastin preparations have a strong tendency to calcify. This may be due to the microfibrillar components, such as calcium-binding fibrillin, within the elastic fiber that are difficult to remove, although there have been studies that disprove this theory. Another limitation of elastin is the complexity of its purification process [21]. Similar to collagen, pure elastin scaffolds need to be cross-linked to improve their mechanical integrity, which also presents a limitation [67].
Elastin scaffolds have mostly been fabricated by electrospinning [90], but others have used insoluble elastin in gels [81] and elastin-like polypeptide block copolymers [62]. In previous studies, electrospun elastin scaffolds have been shown to regulate the proliferation, migration, and differentiation of SMCs as well as reduce the vascular proliferative response to arterial injury in vivo [15, 21]. Several other studies have been performed using elastin scaffolds for cardiovascular tissue engineering purposes [22, 39, 93].
3.2.4 Fibrinogen
Fibrinogen is a naturally occurring plasma protein (340 kDa) that plays an important role in blood clotting, fibrinolysis, cellular and matrix interactions, inflammation, wound healing, and neoplasia [68, 69, 75]. Fibrinogen molecules are elongated 45-nm structures consisting of two outer D domains, each connected by a coiled-coil segment to a central E domain (Fig. 3.5).
Major structural features of fibrinogen. [75]
These molecules consist of six polypeptide chains: two Aα, two Bβ, and two γ, and when fibrinogen reacts with thrombin, two peptides are cleaved to produce fibrin monomers. In the presence of calcium and factor XIII, fibrous clots and other fibrous structures are formed by the fibrin monomers. These structures play a role in the wound healing process, serving as a provisional matrix on which tissues rebuild and repair themselves. For this reason, fibrinogen is an attractive protein for its use in tissue engineering applications.
Another advantage of fibrinogen is that it has two integrin binding sites, RGDF and RGDS, in which many cellular interactions occur through binding to these sites. Cells that have receptors for these binding sites include platelets, endothelial cells (ECs), melanoma cells, fibroblasts, monocytes, and neutrophils [75].
Fibrin-based scaffolds have been developed previously in the form of fibrin gels and wet extrusion fibronectin-fibrinogen cables. Although these gels were easily degradable, nonimmunogenic, and promoted cell migration, they lack the structural integrity needed for practical use in a tissue. The limitation of the wet extruded cables is their resulting large fiber size; 200–250 μm in diameter is many orders of magnitude larger than the native fibers of the ECM, resulting in an unfavorable environment for the cells to function correctly. Electrospun fibrinogen has also been accomplished and has shown excellent cellular interaction as well as mechanical properties similar to those of the native tissue [68, 69].
3.2.5 Silk
Silk is an extremely common fibrous protein that has been used as a medical grade suture for centuries. More recently, silk has become a material of interest in the creation of tissue engineering scaffolds due to its unique blend of material characteristics. Silk exhibits excellent biocompatibility with a foreign body response comparable to other degradable sutures, hemocompatibility, and oxygen and water permeability. Although it is classified as a nondegradable suture, it has been shown that silk will break down through proteolytic degradation and will be slowly absorbed in vivo as biocompatible amino acids. The rate of degradation varies based upon the implantation site and the size of the implanted fibers but has been reported to lose the majority of its tensile strength between 6 weeks and 1 year after implantation. Silk also possesses remarkable mechanical properties not seen in other naturally occurring proteins [3, 4, 110]. It has been reported that natural silk fibers have tensile strength and yield at fracture values comparable to synthetic fibers such as Kevlar [128].
Silk is produced in nature by a wide variety of insects and spiders, with the silk from Bombyx mori silkworm cocoons being the most commonly harvested. Natural silk is composed of two distinct proteins: a glue-like sericin protein, which serves to hold the fibers together, and a fibroin filament component which acts as the mechanical backbone. As sericin has proven to elicit an adverse immune response inside the body, it is the degummed silk fibroin (SF) that is used in medical applications such as braided suture. This 325 kDa protein consists of repetitive hydrophobic blocks, which form crystalline β-sheets through hydrogen bonding, and amorphous hydrophilic regions. The β-sheets provide the structure with its tensile strength, while the amorphous regions provide elasticity and toughness [4, 110, 128]. SF fibers have been used as both knitted constructs [63, 92, 102] and as electrospun scaffolds of reconstituted SF [2, 47, 49, 50, 53, 72, 97, 109, 122]. It has been well documented that the reconstituted fibers of SF are almost completely amorphous in their structure and must be annealed in a methanol or ethanol solution to create β-sheet crystallization [2, 29, 47, 50, 53, 72, 109, 132]. Despite this annealing process, reconstituted SF scaffolds have proven to be highly conducive to cell seeding, with literature reporting successful proliferation of fibroblasts [2, 4, 72, 92], osteoblast-like cells [4], keratinocytes [72], and bone marrow stem cells [3, 4, 50, 63, 102, 110].
3.2.6 Acellular Matrix and Submucosa
Another natural-based material that has been used as a successful scaffold for tissue engineering applications is decellularized ECM. As mentioned before, nearly all the tissues are comprised of ECM that consists of structural proteins, polysaccharides, cytokines, and growth factors. While this process of decellularization aims at completely removing all the cellular and nuclear material from the tissues, the bulk composition, mechanical properties, and biological activity are still intact [6]. Using this type of scaffold eliminates some of the drawbacks and limitations of techniques that will be mentioned later, such as insufficient mechanical strength and possible undesirable inflammatory responses, but still has other disadvantages, including rapid degradation rates and calcification production. Native ECM structures are advantageous for their use as tissue-engineered scaffolds because they induce a positive host response that promotes cell infiltration, rapid scaffold degradation, formation of host-derived neomatrix, and tissue remodeling with a minimum amount of scarring [5].
Briefly, decellularization is the process by which cells are removed from an ECM through a series of mechanical, chemical, or enzymatic steps, leaving an acellular matrix that can serve as a tissue engineering scaffold. The main components of the native ECM that are left after the decellularization process are collagen and elastin [11]. ECMs that have been successfully processed this way include the urinary bladder, the dermis of the skin, small intestine, pericardium, basement membrane and stroma of the decellularized liver, and decellularized Achilles tendon [5].
The submucosa is the layer of tissue beneath a mucous membrane or the layer of connective tissue beneath the tunica mucosa. Similar to the decellularized ECM described above, subintestinal submucosa (SIS) is an attractive material for tissue engineering scaffolds because of the structural and biological factors present in the tissue [7, 20, 58, 96]. In vivo studies done with a bladder submucosa confirm that this tissue can contribute to bladder tissue regeneration. Normal cellular organization and phenotype were demonstrated, along with the presence of nerve fibers [117]. Two drawbacks of both decellularized ECM and SIS are that they exhibit a rapid rate of degradation in vivo, and may elicit calcification. This former problem is especially prevalent in the submucosal tissue, while the native ECM tissue also has problems with scaffold shrinkage in vivo.
Another method to process the ECM and submucosa include adding chemical cross-linking agents to modify the mechanical properties, but doing so may cause a fibrous response [117].
3.3 Fabrication Techniques
There are several fabrication techniques that are used to try and meet the design requirements listed above to produce an ideal tissue-engineered scaffold for specific applications. These techniques include electrospinning, phase separation [11, 46, 125], self-assembly [46, 36, 123], solvent casting/particulate leaching [11], melt molding [11], and CAD techniques such as rapid prototyping and SFF [42, 44, 64]. Each technique produces scaffolds that exhibit many different characteristics such as pore size, fiber diameter, mechanical strength, and types of polymers that can be used; each parameter is unique depending upon the tissue engineering application that the scaffolds are being made for. Some of these techniques will be discussed in further detail below.
3.3.1 Electrospinning
Electrospinning is a textile manufacturing process that is widely used as a fabrication technique for tissue-engineered scaffolds. It was first described as electrostatic spraying, which has been around for more than 100 years, and can produce polymeric scaffolds with fiber diameters ranging from nano- to micrometer range. The electrospinning process consists of a polymer solution, or melt, that is placed in a syringe or pipette. The tip of the pipette or needle that is attached to the syringe is charged with a voltage, and when the electric field produces a force that overcomes the surface tension of the solution, a jet of polymer is drawn from the syringe and attracted to a grounded collecting plate placed some distance away from the needle. The jet forms a Taylor Cone immediately after leaving the needle, and as it travels toward the grounded target, the solution gradually evaporates, leaving small fibers to collect on the target. The charge from the fibers dissipates into the surrounding environment, and a nonwoven fiber mat consisting of tiny fibers, ranging from 50 nm to 10 µm, is formed on the target [8, 11, 24, 64] (Fig. 3.6). Processing parameters including solution properties (viscosity, elasticity, conductivity, and surface tension), processing conditions (voltage, needle diameter, distance from the needle to the grounded target), and the environment (temperature, humidity, and static electricity) can be varied to modify the fibers for individual applications. For example, fiber diameter increases with increasing polymer concentration and increasing voltage [8, 46].
Electrospinning setup [16]
This fabrication technique has many attractive features to produce scaffolds for tissue engineering applications. For one, the mechanical properties of the scaffolds can be adjusted by changing the orientation of the fibers (parallel alignment or random arrangement), and the types of polymer(s) used (natural vs. synthetic). In addition to altering the orientation of the fibers, variations in the scaffolds themselves can be obtained for different applications. For example, multilayering electrospinning results in a hierarchically ordered structure composed of different types of polymers, while multicomponent electrospinning, where multiple polymers are simultaneously electrospun together, forms a mixed fiber mesh [54]. Also, the way the fibers are collected on the grounded target can influence the fiber orientation as well as scaffold fabrication. Collection schemes currently used include a single ground, rotating single ground, dual bar, dual ring, single horizontal ring, electrospinning in vitro onto cells, or electrospinning cells with polymer (Fig. 3.7) [44].
Different electrospinning collecting schemes. (a) Rotating single ground, (b) single ground, (c) dual ring, (d) dual bar, (e) electrospinning in vitro onto cells, (f) single horizontal ring (g) electrospinning cells with polymer, (h) dual spinneret electrospinning (with second pink fibers), (i) electrospinning/electrospraying with parallel and (j) perpendicular spinnerets. [44]
To date, many different polymers, both synthetic and natural, have been successfully electrospun. These polymers include synthetics such as PLA, PGA, PCL, and PDO, naturals including collagen, elastin, silk, and fibrinogen, and blends of naturals and synthetics [8, 11, 15, 16, 50, 68, 130] (Fig. 3.8). With these different polymer combinations, scaffolds can be produced with strengths and stiffness that mimic the native ECM. Many in vivo and in vitros studies have shown that electrospun scaffolds support cell infiltration and have excellent biocompatibility as well [11]. Cardiac myocytes have been shown to interact with electrospun PLGA-based scaffolds and these constructs provided both flexibility and guidance for cell growth [128]. Boland et al. demonstrated the ability of the electrospun collagen and elastin blended scaffolds to be used in vascular tissue engineering applications. These scaffolds, when cultured with ECs, SMCs, and fibroblasts, exhibited a three-layered structure, similar to a native artery, with a confluent EC lining on the intima, a complete cellular infiltration of SMCs throughout the media, and a dense population of fibroblasts and SMCs in the adventitia [15]. Mesenchymal stem cells (MSCs) have been cultured on electrospun scaffolds of PLGA and PCL. After 7 days, the MSCs showed a fivefold population increase on the PLGA scaffolds. On the PCL scaffolds, the cells migrated through 1 mm, depositing collagen along the way, and subsequently differentiated into osteoblasts, producing calcifications [94]. In addition, electrospinning of different polymers has been performed to develop scaffolds for wound dressings [73], cartilage [84, 91, 98, 99, 101], bone [4, 28, 120], ligament [87, 86], nerve tissue [32, 80], and breast tissue engineering [41].
SEM images of electrospun collagen type I (calf skin) (left, magnification 8,000×, left-middle, magnification 500×). Reprinted from [95], © Frontiers in Bioscience. Electrospun PDO (80 mg/mL) (right-middle, magnification 1,000×). Electrospun PLGA (80 mg/mL) (right, magnification 1,000×)
There are many benefits of using this technique, as well as some limitations. The simplicity of this process allows it to be used in a scaled-up setting for mass production purposes. Also, the fibers produced are similar in arrangement and size to those of the native ECM. As stated previously, the adjustment of many parameters to this technique allows for additional control and modification of scaffold characteristics. Drawbacks of this process include the use of toxic solvents (HFP) and cross-linking agents, which could adversely affect the cellular response if not fully extracted. Also, a lack of mechanical strength has been reported, especially when electrospinning natural polymers, although if they are blended with synthetic polymers, this limitation can be resolved [8, 11].
3.3.2 Phase Separation
Phase separation is a technique that produces three-dimensional, highly porous scaffolds with the aim of incorporating bioactive molecules. As a process that produces fibers in the submicron range, it can be accomplished in several ways, including nonsolvent-induced phase separation, chemically induced phase separation, and thermally induced phase separation (TIPS) [8, 11, 24, 124]. In the TIPS process, the temperature of a polymer solution is cooled to induce phase separation, that is, to form a polymer solution into a polymer-rich component and another into a polymer-poor/solvent-rich component. After the solvent has been removed by processes such as extraction, evaporation, or sublimation, the polymer in the polymer-rich phase solidifies into the skeleton, and the spaces originally occupied by the solvent in the polymer-lean phase become the pores of the polymer foam. The pore morphology of the membrane can be altered depending on the polymer, solvent, concentration of the polymer solution, and the phase separation temperature. An additional advantage to this process is that scaffolds can be molded into a variety of shapes and sizes [19, 44, 46, 125].
There are two methods of TIPS; liquid–liquid phase separation, which has been illustrated to produce foams with the potential for drug delivery, and solid–liquid phase separation, which has been developed to enhance the mechanical properties of the scaffolds [11]. Further detail is given below for both methods.
3.3.2.1 Liquid–Liquid Phase Separation
When the crystallization temperature of the solvent is much lower than the phase separation temperature of an amorphous polymer solution, the thermally induced liquid–liquid phase separation takes place by cooling the polymer solution below an upper critical solution temperature. Figure 3.9 shows a binary phase diagram of the amorphous polymer solution system to determine the solvent/polymer relationship. The phase boundaries are shown as a function of temperature and composition and such regions provide three different morphologies.
Binary phase diagram with TIPS properties representing the three distinct morphological types. [44]
In a polymer solution of very low concentration, when the temperature is lowered, the structure formation consists of a polymer-rich phase dispersed in the matrix of the polymer-lean phase (QP1). In this case, the powder-like polymer solid is obtained after the solvent has been removed and the result is a material without structural integrity.
When the composition-temperature point is in the metastable region of a solution with very high polymer concentration (QP3), droplets of the polymer-lean phase are formed in the matrix of the polymer-rich phase and results in foams with a closed-pore structure. This results in a noncell invasive material.
When the composition-temperature point is in the unstable region (QP2), a bicontinuous structure, where both the polymer-rich phase and polymer-lean phases are completely interconnected, will form because of the spinodal decomposition. Foams with a continuous pore network structure are obtained and are of interest to tissue engineering applications because they provide both mechanical integrity and interconnecting porosity for cell invasion.
Structural morphology of liquid–liquid phase separated scaffolds is influenced by quenching rates, crystallinity and vitrification of the polymer phase, and crystallization of the solvent. Scaffolds formed by this method include PLGA, PLLA, and PDLA in tetrahydrofuran (THF) or dioxanone/water and provide a relatively uniform pore distribution with porosities of up to 87% and diameters of 50–100 µm [11, 44, 125]. An example of this scaffold is illustrated in Fig. 3.10.
SEM micrograph of a PLGA scaffold prepared with thermally induced liquid–liquid phase separation. Reprinted from [96]
In addition to the advantages given above, the foremost advantage of the liquid–liquid method is the potential use of the scaffold as a delivery vehicle for bioactive molecules.
3.3.2.2 Solid–Liquid Phase Separation
Solid–liquid phase separation process occurs when the freezing point of the solvent is higher than the liquid–liquid phase separation temperature of the solution. When the temperature of the solution decreases, the solvent crystallizes and the polymer is expelled from the solvent crystallization front [44, 125]. The scaffold morphology reflects the solvent crystal structure and can be altered with the solvent used, the polymer concentration, the crystallization temperature, and the temperature gradient applied to the polymer solution. Many scaffolds have been formed using solid–liquid phase separation, including the most common PLLA, PLGA, PDLA, and hydroxyapatite powder and mixtures of this in dioxanone/water (Fig. 3.11). This technique creates scaffolds with pores having diameters as large as 600µm and a porosity of up to 95% [11]. One advantage of this method, as stated before, is increased mechanical strength, which can be of interest in bone tissue engineering applications.
SEM micrograph of a PLLA scaffold prepared with a thermally induced solid–liquid phase separation process. Reprinted from [96]
Overall, using phase separation for the fabrication of tissue-engineered scaffolds provides advantages including simplicity compared to self-assembly (discussed below), and a low requirement of equipment. In addition, it is easy to achieve batch-to-batch consistency and controllable scaffold mechanical properties and architecture.
Both the methods use organic solvents that may have detrimental effects on the cells. This technique is also limited to only a select number of polymers [8, 46]. Also, for upper micrometer ranges, this process needs to be combined with salt leaching [125].
3.3.3 Self-Assembly
Self-assembly is the independent organization of individual components into functional structures and patterns with preprogrammed noncovalent bonds. Self-assembly processes are common throughout nature and technology, for example, nucleic acid synthesis, protein synthesis, energy transduction, weather systems, and crystals are all associated with this process [36, 37, 46, 112]. From an ECM analog perspective, this technique can be used to modify the chemical, physical, and biological properties of a scaffold to influence cell adhesion, differentiation, migration, and orientation [123]. This technique to create nanofibers has been accomplished for four kinds of polymer configurations: diblock copolymers, triblock copolymers, triblocks from peptide-amphiphile (PA), and dendrimers. The most common configuration for the production of nanoscale fibers is PA.
PA is a triblock polymer consisting of five key structural features: a long alkyl tail providing the hydrophobic driving force, a peptide region with four consecutive cysteine residues to create disulfide bonds for polymerization, the head group region (the C-terminal end) containing three glycine residues to provide flexibility, a phosphorylated serine residue that helps direct mineralization due to its interaction with calcium ions, and RGD, a cell adhesion ligand [46, 94]. Modifications to these regions have been made in a better attempt to explore the ways in which the molecule can be modified for use in other applications [36, 37, 123]. Specifically, Hartgerink et al. designed the standard PA configuration explained above for bone tissue engineering applications, and others have used this technique in nerve tissue engineering and cartilage repair [36, 37, 111].
This process creates nanofibers 5–8 nm in diameter and pores of around 5–200 nm, with an extremely high water content of 99.5%, or 1–5 mg/mL (Fig. 3.12). Because of these characteristics, these scaffolds have the potential for use specifically in three-dimensional cell culture. The porous structure mimics that of the native ECM and can allow for the molecules (growth factors and nutrients) to diffuse in and out slowly [123]. Other ways to induce self-assembly include acid-induced (addition of HCl in a sealed chamber), divalent ion-induced (adding Ca2 to cause gelation), and simply dissolving PA in water at pH 8 and allowing it to dry on a surface [37].
TEM images of a PA molecule (a) self-assembled by drying onto a grid, and (b) self-assembled by mixing with CaCl2. Reprinted from [36], © Elsevier
In contrast to the advantages of this technique listed above, drawbacks include the complexity of the laboratory procedure, a limited availability of polymer configurations, and restriction as a large-scale tissue engineering option. Most three-dimensional scaffolds formed from this technique are of the hydrogel type, which presents many limitations, including mechanical strength and the rate of degradation [112]. However, to overcome this limitation, artificial amphiphilic protein scaffolds have been synthesized with over 200 amino acids [36].
3.3.4 Leaching Techniques
Leaching techniques to produce porous scaffolds for tissue engineering applications are most commonly associated with solvent casting and particulate leaching and are based on the principle that porogens (NaCl, paraffin spheres, sugar crystals, or gelatin) are dispersed throughout a polymer solution and later dissolved by immersion, creating a highly porous, interconnected scaffold [11, 111]. Polymers such as PLLA, PLGA, and PEG have been used to produce pliable, highly porous scaffolds, with porosities of 90% and 500 µm diameter pores [11]. Riddle et al. demonstrated that scaffolds formed using smaller particulate sizes (in the range of 75–106 µm) result in scaffolds that allow for greater tissue infiltration in vivo because of their enhanced pore connectivity [83].
An advantage to this technique is that the pore size, porosity, molecular weight, and surface-to-volume ratio can be precisely controlled and readily manufactured [64, 83]. Limitations of this technique include the requirement of potentially toxic solvents, and rigorous processing conditions, which could potentially prevent the insertion of bioactive molecules [11].
Schematic of 3-DP setup. [44]
3.3.5 Computer-Aided Design Techniques
CAD techniques include three-dimensional printing (3-DP), rapid prototyping, and SFF. 3-DP, which was developed at Massachusetts Institute of Technology, creates a solid-freeform object by ink-jet printing a binder into areas of sequential layers of powder (Fig. 3.13). A thin layer of powder is spread over the surface of a powder bed to create each layer. Each layer is precisely constructed by a CAD representation of the component. The powder bed is set on a piston which has the ability to descend when the powder is spread and each layer is printed (or the bed remains stationary and the ink jets and spreader are raised after the printing of each layer). This layer-by-layer process continues until the part is completed. When the ink droplet impresses on each layer of the powder, the binder solution joins single powder particles, and causes the adjacent powder aggregates to merge. Each layer will form a solid powder-based band, which will finally compile to form the full, solid 3D structure. The powder that is not bound supports the unconnected portions of the component while the structure is built, but is removed after the printing is completed by air jet flow [42, 43, 44, 111].
Similarly, rapid prototyping and SFF are techniques in which scaffolds are produced from a model taken directly from a CAD data set. The specific structure is built up, layer-by-layer, from a selected material, and the process is lead by a computer program [111].
For these techniques, parameters such as porosity, interconnectivity, pore size, and geometric stability can be precisely controlled and present an advantage for tissue engineering applications. Furthermore, processing techniques where cells are printed on the surfaces have been accomplished, which implies that biological substances could be incorporated into the scaffold layers.
One limitation of this fabrication technique is timing. If a solvent that has a rapid drying rate is used, the printed component tends to warp. However, this factor can be eliminated if a solvent is chosen with a low vapor pressure. For example, PCL prepared with chloroform have undetectable amounts of warping, while PCL made with methylene chloride display significant amounts of warping. Combining solvents has also been shown to resolve the warping problem. Another drawback of this technique is that open pores must be present within the structure in order for the unbound powder to be removed to allow for a porous structure for tissue engineering applications. Also, the particle size of the powder used affects the thickness of each layer that is produced. The thickness of each layer ranges from 100–400 µm depending on the printer. Limitations also exist in the choice of materials available and the resolution obtained because of the small size of the scaffolds and imprecise machine tools used [44, 111].
4 Clinical Application
The use of ECM as a commercially available product has grown dramatically in recent years, with the majority of products consisting of decelullarized xenogenic ECM materials. SIS-based products such as Restore™, CuffPatch™, Surgisis®, Oasis®, and Durasis® are packaged as sheets and used for tissue reinforcement and wound repair. TEI Biosciences produces a number of products for specialized applications derived of fetal bovine skin. These include TissueMend® for rotator cuff repair, Durepair® for repair of cranial or spinal dura, Xenoform™ for gastrointestinal and urologic repair, SurgiMend™ for soft tissue membranes, and PriMatrix™ for general wound management. Horse and bovine pericardium-based products have been created and used for a number of different repair and reinforcement applications by Pegassus Biologicals (OrthADAPT™, and DurADAPT™) and Synovis Surgical (Veritas®, Dura-Guard®, Vascu-Guard®, and Peri-Guard®), respectively.
Allogenic decellularized ECM-based products have also made it to the market for a number of different applications. Alloderm is a human skin product that has been used in the abdominal wall, breast, and grafting applications. Graft Jacket® is a skin-based product used for foot ulcers, while Axis™ Dermis has been used for pelvic organ prolapse. Another allogenic product on the market is Suspend™, composed of decellularized human fascia lata and used as a urethral sling.
Currently, with the writing of this chapter, there are four cellular-based ECM products on the market. Smith & Nephew produces both Dermagraft™ and Transcyte™. Dermagraft™ is a full thickness diabetic ulcer graft composed of fibroblasts on a bioabsorbable ECM scaffold, while Transcyte™ is a graft for mid to intermediate partial thickness burns made from the ECM produced by human fibroblasts. Organogenesis, Inc. markets Apligraf®, composed of human fibroblasts on a matrix of collagen and secreted ECM, used to treat venous and diabetic foot ulcers. Finally, a product made from bovine collagen seeded with human fibroblasts, OrCel™ is manufactured by Ortec International to treat burn wounds [6].
To date, there are no engineered ECM analog products in clinical use. While there has been a large amount of funding and research committed to the development of such a product, engineered ECM products are currently limited strictly to the laboratory setting. There are a number of different limitations still to be overcome before such a product can reach the marketplace, and they will be discussed in a subsequent section.
5 Limitations/Critical View
As the engineering of ECM analog scaffolds is still in its infancy, there remain a large number of limitations, many of which are associated with the search to create an ideal scaffold. As stated in the previous section, the use of decellularized ECM has made it possible to create marketable products. However, these products are limited in their scope to patches and skin grafts. A SIS-based material would not be sufficient to support the level of biological complexity needed to engineer a whole tissue or organ. Moreover, the use of these mostly xenogenic materials brings with them the inherent risk of zoonotic disease transmission [6]. An engineered matrix will need to be created, be it natural or synthetic in origin, which can serve as an effective delivery vehicle for the cells or act as a catalyst for cellular remodeling. This will require a prevascularized construct capable of efficient mass transfer of nutrients over long distances. Currently, engineered ECM structures are limited in their overall thickness to the distance of passive diffusion to carry the nutrients to the cells [79]. In addition to the material limitations in matrix creation, there are fabrication limitations as well. Many of the fabrication techniques used to create synthetic ECM analogues in the laboratory currently require the use of toxic organic solvents, or would be nearly impossible to scale up, severely limiting their effectiveness in creating a mass producible product. As yet, no one has been able to mass produce an ideal scaffolding material that will exhibit the necessary mechanical strength and degradation time in vivo, while remaining bioactive.
Of course, scaffolds cellularized in vitros bring with them their own set of risks and limitations; chief among these are the problems associated with immunogenicity. Nearly, every differentiated cell line in the body will elicit an immune response. Even adult stem cells, nonimmunogenic in their undifferentiated state, will cause an immune reaction when they are fully differentiated. Depending on the intended usage time in the body, the degree of immunogenicity may or may not be acceptable. Additionally, allogenic cells have been shown to exhibit phenotypic and functional differences based on sex, age, and location in the body. They may not behave in the same way in a recipient as they did in their donor. To skirt the issues associated with allogenic cells, autologous cells are an option. However, the use of autologous cells no longer makes the product an off-the-shelf option, as it takes time to extract, culture, and seed a product prior to its usage. Ideally, a tissue-engineered product would need to be readily available as a cost and time-effective off-the-shelf option to warrant commercial success. The use of embryonic stem cells are an option to bypass these technical limitations, but bring with them their own set of moral and legal complications [76, 103].
As with the use of the embryonic stem cells, there are challenges and limitations outside the realm of basic science and engineering that must be addressed to ensure the success of ECM analog materials. The FDA, which must provide the approval for all the medical products prior to their clinical usage, categorizes products as either a device, biologic, drug, or blood based. In the past, this gross characterization severely limited as to which devices would readily gain approval to cell therapies (biologic) or acellular products (device). Combinations of the two, which have the potential for greater effectiveness, were often miscategorized. This inadvertently forced companies in need of getting a product on the market to produce simplified products, rather than complex combinations of cells, scaffolds, and growth factors, in hopes of gaining rapid approval. The creation of the Office of Combination Products as a coordinating body in 2002 was designed to assuage some of the difficulties associated with passing a complex combination ECM analog; however, this office does not have any authoritative power [76].
6 Expert Opinion
The basis of our being is a nanofabric, the ECM, which creates a complex microenvironment of structural elements, cells, and ground substance that act as the structural framework for each tissue and organ. As tissue engineers, our ultimate end goal is to replicate, for repair and/or replacement, the damaged and diseased tissues and organs. In order to create such structures one must replicate the basis for each tissue or organ, the ECM, via some fabrication method. Unfortunately for the tissue engineer, each tissue and organ presents a unique challenge by possessing an ECM with an exclusive composition and organization. In order to be successful in tissue engineering, we must be able to replicate the ECM to provide the proper microenvironment for tissue regeneration and maintenance. Without proper cellular microenvironments, the best one can achieve will be the pathological tissue. Thus, as the field continues to move forward a major obstacle remains: Can we engineer an ECM analog for individual tissues or organs to allow for functional, yet marketable, tissue-engineered products to improve the quality of life? This is a daunting challenge and one that must be overcome to produce successful tissue-engineered products. It is this author’s belief that through the use and refinement of the current nanoscale fabrication techniques, or a combination of these fabrication techniques, an acceptable ECM analog will be produced which will allow for the successful creation of tissue-engineered products for a number of different applications.
7 Five-Year Perspective
The past two decades have seen tissue engineering grow from a fledgling field, to a field filled with the promise of new commercially available ECM analogues entering the market. Tissue engineering has expanded from its infancy of simple cell injection treatments to complex bioactive scaffolds created from a marriage of cells and nanotechnology-based biomaterials. As tissue engineering has grown, our knowledge base in the fields of cell and molecular biology, polymers science, immunology, and tissue mechanics has grown symbiotically, spawning further collaboration and more multidisciplinary approaches, and creating the possibility for continued exponential growth. However, we have reached a point where the public eye needs to see tissue engineering as a viable, product producing field capable of improving their quality of life. The benchtop successes we have seen in the laboratory need to translate to the marketplace to ensure success and enhance the probability of achieving long-term goals, namely the creation of fully engineered tissues and organs.
Our understanding of cell behavior during development and the reparative process has increased substantially in recent years since the boom of stem cell science, and should continue to grow at a torrid pace. The discovery and continued rise in popularity of MSCs in tissues such as processed lipoaspirate (PLA), obtained through cosmetic liposuction procedures, will make the usage of adult stem cells more widespread and their incorporation into ECM analogues more prevalent. These cells have proven to be plentiful and are more readily extracted than MSCs from bone marrow, while exhibiting equal if not superior proliferation and differentiation ability. The nonimmunogenic nature of the adult stem cells will make it possible to create a cellularized off-the-shelf ECM analog product containing allogenic cells, rather than extracting autologous cells and seeding them on an acellular scaffold. This type of product would be very effective as a short-term aid to repair, but would run into immunogenicity issues once the stem cells became fully differentiated.
Another area of growth in the near future would be in the creation of vascularized ECM analogues. Currently, there are no prevascularized products on the market, which handcuffs the maximum thickness of an ECM construct to the limits of nutrient diffusion. This requires all the engineered scaffolding to be no more than a couple of millimeters thick, and hinders the creation of tissue constructs of substantial volume. To achieve the end goal of creating a completely engineered tissue or organ, it is necessary to create a structure that has conduits to supply nutrients to its entirety as opposed to limiting ourselves to the thicknesses allowable by diffusion. Current work in the field of computer-aided tissue engineering, such as 3-DP and rapid prototyping, has the ability to create intricately designed scaffolds with ever increasing precision. The creation of a scaffold, designed and constructed with computer accuracy, containing a highly organized network of cellularized conduits throughout to promote capillary formation, would enhance the ability of the nutrients to travel longer distances. Current research into the promotion of angiogenesis through the use of a number of different growth factors incorporated into ECM constructs, coupled with the use of ECs, stem cells, and macrophages to create vascularized structures has proven to be promising and may prove to be the answer.
Finally, further refinement of the biomaterials and their fabrication techniques will drive tissue engineering down a path toward an increasingly ideal ECM analog construct. The ability of the polymer scientists to create novel polymers, with bulk properties (mechanical strength, thermal properties, degradation, etc.) tailored to specific tissue applications, will have the potential to enhance the overall effectiveness of engineered scaffolds. These polymers can also be combined with any number of growth factors and signaling molecules to improve their bioactivity and promote positive cellular interactions. Further collaborations between the polymer scientists and other members of the tissue engineering community will only benefit the creation of successfully engineered ECM.
8 Conclusion/Summary
Tissue engineering has made a profound impact on the quality of life for many, and with the field growing at a rapid rate, that number will continue to increase as more exciting and path breaking discoveries are made. Polymeric scaffolds, both synthetic and natural, used as ECM analogues have the potential to replace, and further regenerate new tissue by providing a suitable environment for the cells to be able to communicate through signals and function properly through attachment, differentiation, migration, and proliferation. Multiple fabrication techniques used to create ECM analogues design the structural characteristics needed to mimic the native ECM. These ideal ECM analogues will open the doors to many new clinical options for applications including bone, cartilage, cardiovascular, nerve, skin, ligament, tendon, breast, and liver. Although there are limitations that still stand in the way of having an ideal scaffold, the challenge of designing a successful ECM analog is slowly being conquered as professionals in the field continue to make significant improvements on a daily basis.
9 Literature with Abstracts
Badylak SF, et al. Small intestinal submucosa as a large diameter vascular graft in the dog. J Surg Res. 1989;47(1):74-80.
The first publication from Dr. Badylak utilizing decellularized SIS as a large diameter vascular graft in the dog.
Hartgerink JD, Beniash E, Stupp SI. Self-assembly and mineralization of peptide-amphiphile nanofibers. Science. 2001; 294(5547):1684-8.
The use of ph-induced self-assembly to create a nanostructured fibrous scaffold for use as an ECM analog.
Hutmacher, DW, Sittinger M, Risbud MV. Scaffold-based tissue engineering: rationale for CAD and SFF systems. Trends Biotechnol. 2004;22(7):354-62.
Review and rationale for the use of computer-aided tissue engineering, design, and construction of ECM analog scaffolds. Discusses the application, advancement, and future of computer-aided tissue engineering.
Langer R, Vacanti JP, Tissue engineering. Science. 1993; 260(5110):920-6.
An overview, defining the field of tissue engineering, and discussing the foundations and challenges of the field.
Matthews JA, Wnek GE, Simpson DG, Bowlin GL. Electrospinning of collagen nanofibers. Biomacromolecules. 2002; 3:232-8.
The first publication on the electrospinning of collagen. The authors electrospun collagen type I in order to create nanofibrous, nonwoven structures for use as a bioresorbable tissue engineering scaffold.
Vacanti JP, et al. Selective cell transplantation using bioabsorbable artificial polymers as matrices. J Pediatr Surg. 1988; 23(1 pt 2):3-9.
The first publication to utilize a biodegradable polymer scaffold as a delivery vehicle for cell transplantation. Cells were harvested from rat donors, cultured, and seeded onto degradable polymer scaffolds consisting of polyglactin, polyanhydrides, and polyorthoesters and implanted into recipient rats.
Zhang R, Ma PX. Synthetic nano-fibrillar extracellular matrices with predesigned macroporous architectures. J Biomed Mater Res. 2000;52(2):430-8.
The first publication on thermal phase separation created ECM analog scaffolds with a predesigned macroporous structure designed to enhance cellular penetration. The macroporous structure was created by the leaching of sugar and salt porogens.
10 Suggested Readings with Abstracts
Badylak S, Gilbert T, Myers-Irvin J. The extracellular matrix as a biologic scaffold for tissue engineering. In: van Blitterswijk J, et al., editors. Tissue engineering. London: Academic; 2008. p. 121-43.
This chapter contains information on the composition and organization of the native ECM, along with commercially available scaffolds composed of ECM.
Farach-Carson MC, Wagner RC, Kiick KL. Extracellular matrix: structure, function, and applications to tissue engineering. In: Fisher JP, Mikos AG, Bronzino JD, editors. Tissue engineering. Boca Raton: CRC; 2007. p. 3-1–22.
This chapter summarizes the composition and function of the native ECM and the present status of using it in tissue engineering applications.
Gomes M, et al. Natural polymers in tissue engineering applications. In: van Blitterswijk C, editor. Tissue engineering. San Diego: Elsevier; 2008. p. 145-92.
An overview of the origin, structure, and applications of natural polymers used in tissue engineering is given in this chapter. Advantages and disadvantages of natural polymers are discussed as well.
Hutmacher D, et al. Scaffold design and fabrication. In: van Blitterswijk C, editor. Tissue engineering. San Diego: Elsevier; 2008. p. 403-54.
This chapter reviews scaffold design and fabrication techniques including porogen leaching, phase separation, electrospinning, knitting and braiding, three-dimensional printing, indirect SFF, and others.
Palsson, BO, Bhatia SN. Tissue engineering. Upper Saddle River: Pearson Prentice Hall; 2004.
This book reviews the field of tissue engineering as a whole and is divided into parts labeled quantitative cell and tissue biology, cell and tissue characterization, engineering methods and design, and clinical implementation. The book discusses the challenges of the field and the requirement of the understanding of many subject areas including tissue dynamics, stem cell biology, cell communications, biomaterials, physico-chemical-rate processes, and bioengineering design.
Sell S, et al. Extracellular matrix regenerated: tissue engineering via electrospun biomimetic nanofibers. Polym Int. 2007; 56(11):1349-60.
This article reviews the role of electrospinning in the engineering of different tissues and applications such as skin/wound healing, cartilage, bone, vascular tissue, urological tissues, nerve, and ligament.
Weigel T, Schinkel G, Lendlein A. Design and preparation of polymeric scaffolds for tissue engineering. Expert Rev Med Devices. 2006;3(6):835-51.
This review article describes conventional preparation methods for polymeric scaffolds for tissue engineering including electrospinning, phase separation, porogen leaching, rapid prototyping, SFF, 3-D printing, and self-assembly.
Yoon DM, Fisher JP. Polymeric scaffolds for tissue engineering applications. In: Fisher JP, Mikos AG, Bronzino JD, editors. Tissue engineering. Boca Raton: CRC; 2007. p. 8-1–18.
This chapter discusses natural and synthetic polymers used for scaffold fabrication for tissue engineering applications. It also reviews scaffold design properties such as fabrication, biocompatibility, biodegradability, and mechanical strength.
References
Agrawal CM, Ray RB. Biodegradable polymeric scaffolds for musculoskeletal tissue engineering. J Biomed Mater Res. 2001;55(2):141–50.
Alessandrino A et al. Electrospun silk fibroin mats for tissue engineering. Eng Life Sci. 2008;8(3):219–25.
Altman GH et al. Silk matrix for tissue engineered anterior cruciate ligaments. Biomaterials. 2002;23:4131–41.
Altman GH et al. Silk-based biomaterials. Biomaterials. 2003;24:401–16.
Badylak SF. The extracellular matrix as a scaffold for tissue reconstruction. Cell Dev Biol. 2002;13:377–83.
Badylak S, Gilbert T, Myers-Irvin J. The extracellular matrix as a biologic scaffold for tissue engineering. In: van Blitterswijk C, editor. Tissue engineering. London: Academic; 2008. p. 121–43.
Badylak SF et al. Small intestinal submucosa as a large diameter vascular graft in the dog. J Surg Res. 1989;47(1):74–80.
Barnes CP et al. Nanofiber technology: designing the next generation of tissue engineering scaffolds. Adv Drug Deliv Rev. 2007;59:1413–33.
Bell E. Tissue engineering: a perspective. J Cell Biochem. 1991;45:239–41.
Berry CC, Campbell G, Spadiccino A, Robertson M, Curtis AS. The influence of microscale topography on fibroblast attachment and motility. Biomaterials. 2004;25:5781–8.
Boland ED, Espy PG, Bowlin GL. Tissue engineering scaffolds. In: Wnek G, Bowlin G, editors. Encyclopedia of biomaterials and biomedical engineering. New York: Marcel Dekker; 2004. p. 1–9.
Boland ED et al. Tailoring tissue engineering scaffolds using electrostatic processing techniques: a study of poly(glycolic acid) electrospinning. J Macromol Sci. 2001; A38(12):1231–43.
Boland ED et al. Utilizing acid pretreatment and electrospinning to improve biocompatibility of poly(glycolic acid) for tissue engineering. J Biomed Mater Res B Appl Biomater. 2004;71B:144–52.
Boland ED et al. Electrospinning collagen and elastin: preliminary vascular tissue engineering. Front Biosci. 2004; 9:1422–32.
Boland ED et al. Electrospinning polydioxanone for biomedical applications. Acta Biomater. 2005;1:115–23.
Bowlin GL, Simpson DG. Tissue-engineering scaffolds: can we re-engineer mother nature? Expert Rev Med Devices. 2006;3(1):9–15.
Chamberlain G et al. Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells. 2007;25:2739–49.
Chen VJ, Ma PX. Nano-fibrous poly(l-lactic acid) scaffolds with interconnected spherical macropores. Biomaterials. 2004;25:2065–73.
Cobb MA et al. Porcine small intestinal submucosa as a dural substitute. Surg Neurol. 1999;51(1):99–104.
Daamen WF et al. Tissue response of defined collagen-elastin scaffolds in young and adult rats with special attention to calcification. Biomaterials. 2005;26:81–92.
Daamen WF et al. A biomaterial composed of collagen and solubilized elastin enhances angiogenesis and elastic fiber formation without calcification. Tissue Eng A. 2007; 14(3):349–60.
Debelle L et al. The secondary structure and architecture of human elastin. Eur J Biochem. 1998;258:533–9.
Engel E et al. Nanotechnology in regenerative medicine: the materials side. Trends Biotechnol. 2007;26(1):39–47.
Farach-Carson MC, Wagner RC, Kiick KL. Extracellular matrix: structure, function, and applications to tissue engineering. In: Fisher JP, Mikos AG, Bronzino JD, editors. Tissue engineering. Boca Raton: CRC Press; 2007. p.3-1–22.
Fecek C et al. Chondrogenic derivatives of embryonic stem cells seeded into 3D polycaprolactone scaffolds generated cartilage tissue in vivo. Tissue Eng A. 2008;8:1403–13.
Freed LE et al. Biodegradable polymer scaffolds for tissue engineering. Biotechnology. 1994;12:689–93.
Fujihara K, Kotaki M, Ramakrishna S. Guided bone regeneration membrane made of polycaprolactone/calcium carbonate composite nano-fibers. Biomaterials. 2005;26:4139–47.
Garcia-Fuentes M et al. The effect of hyaluronic acid on silk fibroin conformation. Biomaterials. 2008;29:633–42.
Gentleman E et al. Mechanical characterization of collagen fibers and scaffolds for tissue engineering. Biomaterials. 2003;24(21):3805–13.
Gentleman E et al. Development of ligament-like structural organization and properties in cell-seeded collagen scaffolds in vitros. Ann Biomed Eng. 2006;34(5):726–36.
Ghasemi-Mobarakeh L et al. Electrospun poly(e-carpolactone)/gelatin nanofibrous scaffolds for nerve tissue engineering. Biomaterials. 2008;29:4532–9.
Gomes M et al. Natural polymers in tissue engineering applications. In: van Blitterswijk C, editor. Tissue engineering. San Diego: Elsevier; 2008. p. 145–92.
Griffith CK, Miller C, Sainson RC, Calvert JW, Jeon NL, Hughes CC, et al. Diffusion limits of an in vitros thick prevascularized scaffold. Tissue Eng. 2005;11(1/2):257–66.
Gunatillake PA, Adhikari R. Biodegradable synthetic polymers for tissue engineering. Eur Cells Mater. 2003;5:1–16.
Hartgerink JD, Beniash E, Stupp SL. Self-assembly and mineralization of peptide-amphiphil nanofibers. Science. 2001;294:1684–8.
Hartgerink JD, Beniash E, Stupp SL. Peptide-amphiphile nanofibers: a versatile scaffold for the preparation of self-assembling materials. Chemistry. 2002;99(8):5133–8.
Heineken FG, Skalak R. Tissue engineering: a brief overview. J Biomech Eng. 1991;113:111.
Heydarkhan-Hagvall S et al. Three-dimensional electrospun ECM-based hybrid scaffolds for cardiovascular tissue engineering. Biomaterials. 2008;29(19):2907–14.
Huang JI, Yoo JU, Goldberg VM. Orthopedic applications of stem cells. In: Lanza R et al., editors. Essentials of stem cell biology. Burlington: Elsevier Academic; 2006. p. 449–56.
Huss FRM, Kratz G. Mammary epithelial cell and adipocyte co-culture in a 3-D matrix: the first step towards tissue-engineered human breast tissue. Cells Tissues Organs. 2001;169:361–7.
Hutmacher DW. Scaffold design and fabrication technologies for engineering tissues-state of the art and future perspectives. J Biomater Sci Polym Ed. 2001;12(1):107–24.
Hutmacher DW, Sittinger M, Risbud MV. Scaffold-based tissue engineering: rationale for computer-aided design and solid free-form fabrication systems. Trends Biotechnol. 2004;22(7):354–62.
Hutmacher D et al. Scaffold design and fabrication. In: van Blitterswijk C, editor. Tissue engineering. San Diego: Elsevier; 2008. p. 403–54.
Ishaug-Riley SL et al. Human articular chondrocyte adhesion and proliferation on synthetic biodegradable polymer films. Biomaterials. 1999;20:2245–56.
Jayaraman K et al. Recent advances in polymer nanofibers. J Nanosci Nanotechnol. 2004;4(1):52–65.
Jeong SI et al. Tissue-engineered vascular grafts composed of marine collagen and PLGA fibers using pulsatile perfusion bioreactors. Biomaterials. 2007;28:1115–22.
Jiankang H et al. Preparation of chitosan-gelatin hybrid scaffolds with well-organized microstructures for hepatic tissue engineering. Acta Biomater. 2008;5(1):453–61.
Jin HJ et al. Electrospinning Bombyx mori silk with poly(ethylene oxide). Biomacromolecules. 2002;5(3): 786–92.
Jin HJ et al. Human bone marrow stromal cell responses on electrospun silk fibroin mats. Biomaterials. 2004;25(6): 1039–47.
Kannan RY, Salacinski HJ, Sales K, Butler P, Seifalian AM. The roles of tissue engineering and vascularisation in the development of micro-vascular networks: a review. Biomaterials. 2005;26:1857–75.
Karande TS, Ong JL, Agrawal CM. Diffusion in musculoskeletal tissue engineering scaffolds: design issues related to porosity, permeability, architecture, and nutrient mixing. Ann Biomed Eng. 2004;32(12):1728–43.
Kawahara Y et al. Structure for electro-spun silk fibroin nanofibers. J Appl Polym Sci Symp. 2008;107:3681–4.
Kidoaki S, Kwon IK, Matsuda T. Mesoscopic spatial designs of nano- and microfiber meshes for tissue-engineering matrix and scaffold based on newly devised multilayering and mixing electrospinning techniques. Biomaterials. 2005;26:37–46.
Kim K-S et al. Control of degradation rate and hydrophilicity in electrospun non-woven poly(D, L-lactide) nanofiber scaffolds for biomedical applications. Biomaterials. 2003; 24:4977–85.
Langer R. Editorial: tissue engineering: perspectives, challenges, and future directions. Tissue Eng. 2007;13(1):1.
Langer R, Vacanti JP. Tissue engineering. Science. 1993;260(5110):920–6.
Lantz GC et al. Small intestinal submucosa as a vascular graft: a review. J Invest Surg. 1993;6(3):297–310.
Lee KY, Mooney DJ. Hydrogels for tissue engineering. Chem Rev. 2001;101(7):1869–79.
Levesque SG, Lim RM, Shoichet MS. Macroporous interconnected dextran scaffolds of controlled porosity for tissue-engineering applications. Biomaterials. 2005;26:7436–46.
Li S, De Wijn JR, Li J, Layrolle P, De Groot K. Macroporous biphasic calcium phosphate scaffold with high permeability/porosity ratio. Tissue Eng. 2003;9(3):535–48.
Lim DW et al. In situ cross-linking of elastin-like polypeptide block copolymers for tissue repair. Biomacromolecules. 2008;9(1):222–30.
Liu H et al. The interaction between a combined knitted silk scaffold and microporous silk sponge with human mesenchymal stem cells for ligament tissue engineering. Biomaterials. 2008;29:662–74.
Mano JF et al. Natural origin biodegradable systems in tissue engineering and regenerative medicine: present status and some moving trends. J R Soc Interface. 2007;4: 999–1030.
Martins-Green M. The dynamics of cell–ECM interactions with implications for tissue engineering. In: Lanza R, Langer R, Chick W, editors. Principles of tissue engineering. Georgetown: R. G. Landes; 1997. p. 23–46.
Matthews JA, Simpson DG, Wnek GE, Bowlin GL. Electrospinning of collagen nanofibers. Biomacromolecules. 2002;3:232–8.
McClure MJ et al. Cross-linking electrospun polydioxanone-soluble elastin blends: material characterization. J Eng Fibers Fabrics. 2008;3(1):1–10.
McManus M et al. Mechanical properties of electrospun fibrinogen structures. Acta Biomater. 2006;2:19–28.
McManus MC et al. Electrospun fibrinogen: feasibility as a tissue engineering scaffold in a rat cell culture model. J Biomed Mater Res A. 2007;81(2):299–309.
Middleton JC, Tipton AJ. Synthetic biodegradable polymers as orthopedic devices. Biomaterials. 2000;21:2335–46.
Mikos AG, Temenoff JS. Formation of highly porous biodegradable scaffolds for tissue engineering. Electron J Biotechnol. 2000;3:114–9.
Min B-M et al. Electrospinning of silk fibroin nanofibers and its effect on the adhesion and spreading of normal human keratinocytes and fibroblasts in vitros. Biomaterials. 2004;25:1289–97.
Min B-M et al. Regenerated silk fibroin nanofibers: water vapor-induced structural changes and their effects on the behavior of normal human cells. Macromol Biosci. 2006; 6:285–92.
Mooney DJ, Langer RS. Engineering biomaterials for tissue engineering: the 10–100 micron size scale. In: Palsson B, Hubbell JA, Plonsey R, Bronzino JD, editors. Tissue engineering. Boca Raton: CRC Press; 2000.
Mosesson MW, Siebenlist KR, Meh DA. The structure and biological features of fibrinogen and fibrin. Ann NY Acad Sci. 2001;936:11–30.
Nerem RM. Tissue engineering: the hope, the hype and the future. Tissue Eng. 2006;12(5):1143–50.
Norman JJ, Desai TA. Methods for fabrication of nanoscale topography for tissue engineering scaffolds. Ann Biomed Eng. 2006;34(1):89–101.
Palsson BO, Sangeeta NB. Tissue engineering. Upper Saddle River: Pearson Prentice Hall; 2004.
Pancrazio JJ, Wang F, Kelley CA. Enabling tools for tissue engineering. Biosens Bioelectron. 2007;22:2803–11.
Prabhakaran MP et al. Electrospun biocomposite nanofibrous scaffolds for neural tissue engineering. Tissue Eng A. 2008;14(11):1787–97.
Rabaud M, Lefebvre F, Ducassou D. In vitro association of type III collagen with elastin and with its solubilized peptides. Biomaterials. 1991;12(3):313–9.
Ratner BD, Bryant SJ. Biomaterials: where we have been and where we are going. Annu Rev Biomed Eng. 2004; 6:41–75.
Riddle KW, Mooney DJ. Role of poly(lactide-co-glycolide) particle size on gas-foamed scaffolds. J Biomater Sci Polym Ed. 2004;15(12):1561–70.
Riley SL et al. Formulation of PEG-based hydrogels affects tissue-engineered cartilage construct charateristics. J Mater Sci Mater Med. 2001;12:983–90.
Rosso F et al. Smart materials as scaffolds for tissue engineering. J Cell Physiol. 2005;203:465–70.
Sahoo S et al. Characterization of a novel polymeric scaffold for potential application in tendon/ligament tissue engineering. Tissue Eng. 2006;12(1):91–9.
Sahoo, S., et al. Towards an ideal polymer scaffold for tendon/ligament tissue engineering. In: The International Society for Optical Engineering. Singapore: Third Intl Conf on Experimental Mechanics and Third Conf. of the Asian Committee on Experimental Mechanics. 2005.
Sander EA, Nauman EA. Permeability of musculoskeletal tissues and scaffolding materials: experimental results and theoretical predictions. Crit Rev Biomed Eng. 2003;31(1): 1–26.
Sell SA et al. Electrospun polydioxanone-elastin blends: potential for bioresorbable vascular grafts. Biomed Mater. 2006;1:72–80.
Sell S et al. Extracellular matrix regenerated: tissue engineering via electrospun biomimetic nanofibers. Poly Int. 2007;56(11):1349–60.
Seo Y-K et al. The biocompatibility of silk scaffold for tissue engineering ligaments. Key Eng Mater. 2007; 342–343:73–6.
Simionescu DT et al. Biocompatibility and remodeling potential of pure arterial elastin and collagen scaffolds. Biomaterials. 2006;27(5):702–13.
Smith LA, Ma PX. Nano-fibrous scaffolds for tissue engineering. Colloids Surf B Biointerfaces. 2004;39:125–31.
Song E et al. Collagen scaffolds derived from a marine source and their biocompatibility. Biomaterials. 2006; 27(15):2951–61.
Suckow MA et al. Enhanced bone regeneration using porcine small intestinal submucosa. J Invest Surg. 1999;12(5): 277–87.
Sukigara S et al. Regeneration of Bombyx mori silk by electrospinning – part 1: processing parameters and geometric properties. Polymer. 2003;44:5721–7.
Tan H et al. Gelatin/chitosan/hyaluronan scaffold integrated with PLGA microspheres for cartilage tissue engineering. Acta Biomater. 2008;5(1):328–37.
Tang S, Spector M. Incorporation of hyaluronic acid into collagen scaffolds for the control of chondrocyte-mediated contraction and chondrogenesis. Biomed Mater. 2007; 2(3):S135–41.
Telemeco TA, Ayres C, Bowlin GL, Wnek GE, Boland ED, Cohen N, et al. Regulation of cellular infiltration into tissue engineering scaffolds composed of submicron diameter fibrils produced by electrospinning. Acta Biomater. 2005; 1(4):377–85.
Thorvaldsson A et al. Electrospinning of highly porous scaffolds for cartilage regeneration. Biomacromolecules. 2008;9:1044–9.
Toh SL et al. Novel silk scaffolds for ligament tissue engineering applications. Key Eng Mater. 2006;326–328(1): 727–30.
Vacanti CA. History of tissue engineering and a glimpse into its future. Tissue Eng. 2006;12(5):1137–42.
Vacanti JP, Vacanti CA. The challenge of tissue engineering. In: Lanza R, Langer R, Chick W, editors. Principles of tissue engineering. Georgetown: R.G. Landes; 1997.
Vacanti JP et al. Selective cell transplantation using bioabsorbable artificial polymers as matrices. J Pediatr Surg. 1988;23(1 pt 2):3–9.
van Dijkhuizen-Radersma R et al. Degradable polymers for tissue engineering. In: van Blitterswijk C, editor. Tissue engineering. San Diego: Elsevier; 2008. p. 193–221.
Venugopal J, Ramakrishna S. Applications of polymer nanofibers in biomedicine and biotechnology. Appl Biochem Biotechnol. 2005;125:147–57.
Walpoth BH, Bowlin GL. The daunting quest for a small diameter vascular graft. Expert Rev Med Devices. 2005;2(6):647–51.
Wang M et al. Mechanical properties of electrospun silk fibers. Macromolecules. 2004;37:6856–64.
Wang Y et al. Stem cell-based tissue engineering with silk biomaterials. Biomaterials. 2006;27:6064–82.
Weigel T, Schinkel G, Lendlein A. Design and preparation of polymeric scaffolds for tissue engineering. Expert Rev Med Devices. 2006;3(6):835–51.
Wen X, Shi D, Zhang N. Applications of nanotechnology in tissue engineering. In: Nalwa HS, editor. Handbook of nanostructured biomaterials and their applications in nanobiotechnology. Los Angeles: American Scientific Publishers; 2005.
Wnek GE, Carr ME, Simpson DG, Bowlin GL. Electrospinning of nanofiber fibrinogen structures. Nano Lett. 2003;3(2):213–6.
Wong WH, Mooney DJ. Synthesis and properties of biodegradable polymers used as synthetic matrices for tissue engineering. In: Atala A, Mooney D, editors. Synthetic biodegradable polymer scaffold. Boston: Birkhauser; 1997. p. 50–82.
Yang C et al. The application of recombinant human collagen in tissue engineering. BioDrugs. 2004;18(2):103–19.
Yang F et al. Electrospinning of nano/micro scale poly(l-lactic acid) aligned fibers and their potential in neural tissue engineering. Biomaterials. 2005;26:2603–10.
Yoo JJ et al. Bladder augmentation using allogenic bladder submucosa seeded with cells. Urology. 1998;51:221–5.
Yoon DM, Fisher JP. Polymeric scaffolds for tissue engineering applications. In: Fisher JP, Mikos AG, Bronzino JD, editors. Tissue engineering. Boca Raton: CRC Press; 2007. p. 8-1–18.
Yoshimoto H et al. A biodegradable nanofiber scaffold by electrospinning and its potential for bone tissue engineering. Biomaterials. 2003;24(12):2077–82.
Zalipsky S. Functionalized poly(ethylene glycol) for preparation of biologically relevant conjugates. Bioconjug Chem. 1995;6(2):150–65.
Zarkoob S et al. Structure and morphology of electrospun silk nanofibers. Polymer. 2004;45:3973–7.
Zhang S. Fabrication of novel biomaterials through molecular self-assembly. Nat Biotechnol. 2003;21(10):1171–8.
Zhang R, Ma PX. Synthetic nano-fibrillar extracellular matrices with predesigned macroporous architectures. J Biomed Mater Res. 2000;52(2):430–8.
Zhang R, Ma PX. Processing of polymer scaffolds: phase separation. In: Atala A, Lanza RP, editors. Methods of tissue engineering. San Diego: Academic; 2002. p. 715–24.
Zhang Y et al. Electrospinning of gelatin fibers and gelatin/PCL composite fibrous scaffolds. J Biomed Mater Res B Appl Biomater. 2005;72B:156–65.
Zhang S et al. Gelatin nanofibrous membrane fabricated by electrospinning of aqueous gelatin solution for guided tissue regeneration. J Biomed Mater Res A. 2008;90(3): 671–9.
Zhao C, Asakura T. Structure of silk studied with NMR. Prog Nucl Magn Reson Spectrosc. 2001;39:301–52.
Zong X, Bien H, Chung CY, Yin L, Fang D, Hsiao BS, et al. Electrospun fine-textured scaffolds for heart tissue constructs. Biomaterials. 2005;26:5330–8.
Zong X et al. Structure and morphology changes during in vitros degradation of electrospun poly(glycolide-co-lactide) nanofiber membrane. Biomacromolecules. 2003;4: 416–23.
Zuo B, Liu L, Wu Z. Effect on properties of regenerated silk fibroin fiber coagulated with aqueous methanol/ethanol. J Appl Polym Sci Symp. 2007;106:53–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Berlin Heidelberg
About this chapter
Cite this chapter
Wolfe, P.S., Sell, S.A., Bowlin, G.L. (2011). Natural and Synthetic Scaffolds. In: Pallua, N., Suscheck, C. (eds) Tissue Engineering. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-02824-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-642-02824-3_3
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-02823-6
Online ISBN: 978-3-642-02824-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)