Abstract
Development of intraocular drug delivery systems (DDSs) is urgently required for the treatment of eye diseases, especially in the posterior segment of the eye (the vitreous cavity, retina, and choroid), most of which are refractory to conventional pharmacologic approaches; eye drops and systemically administered drugs cannot achieve therapeutic drug concentrations in the posterior segment of the eye. Repeated intravitreal injections of anti-angiogenic agents are effective in the treatment of age-related macular degeneration, but there remain risks of serious side effects such as endophthalmitis associated with repeated injections. Intraocular DDSs may address these problems. Intraocular sustained drug release from implantable or injectable devices has been investigated to treat vitreoretinal diseases. A reservoir-type nonbiodegradable implant was first launched in the market in 1996 for the treatment of cytomegalovirus retinitis secondary to the acquired immunodeficiency syndrome, followed by clinical trials for a variety of potent devices to treat other challenging eye diseases. An injectable rod-shaped insert releasing a steroid is presently being assessed in a phase III trial to treat macular edema secondary to diabetic retinopathy or retinal vein occlusion. Thus various types of intraocular DDSs will be commercially available to treat vision-threatening intraocular diseases in the near future.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Age-related macular degeneration
- Biodegradable polymer
- Controlled release
- Intraocular drug delivery system
- Microsphere
1 Introduction
The eye is a photosensory organ with specific structures similar to those of a camera. The eye should preserve not only the transparency of ocular media but also its configuration, in order to stabilize refractory structures (e.g., cornea and lens). For this aim, the most effective shape is a balloon-like configuration with little vasculature, few cellular components, and transparent fluid inside. Aqueous humor, the intraocular circulating fluid, is well conditioned with sufficient nutrients for nonvascular structures and a strictly limited amount of macromolecules such as proteins and lipids for homeostasis and transparency. This forms the blood–aqueous barrier, composed of ciliary nonpigmented epithelium and iridal vascular endothelium with tight junctions. The outer and inner blood–retinal barriers, which are formed by the retinal pigment epithelium (RPE) and retinal vascular endothelium, respectively, regulate retinal homeostasis (Maurice and Mishima 1984; Geroski and Edelhauser 2001; Ambati and Adamis 2002; Yasukawa et al. 2004, 2006, 2007). In this way the intraocular space is separated from the systemic blood circulation (Fig. 1) and therefore systemically administered drugs cannot easily reach the intraocular space (Pharmacological Therapy for Macular Degeneration Study Group 1997; Ip and Gorin 1996). Therefore, high drug dosages must be used to achieve efficacy, frequently causing side effects in other healthy tissues. On the other hand, the eye is covered with collagenous layers (e.g., cornea and sclera) and epithelial and endothelial barriers (e.g., cornea and RPE). These barriers, continuous tear production, frontward flow of aqueous humor, and choroidal circulation limit the penetration of topically administered drugs (e.g., eye drops and ointments) (Lang 1995; Kim et al. 2007) (Fig. 1). Consequently, eye drops must be instilled frequently or at high concentrations to achieve therapeutic concentrations even in the anterior segment of the eye. It is much harder to deliver drugs to the posterior segment because of the longer diffusion distance and counterdirectional intraocular convection from the ciliary body to Schlemm’s canal.
Barriers which limit drug delivery into the posterior segment of the eye. The cornea, tear drainage, episcleral blood flow, and intraocular counterdirectional convection limit the delivery of locally administered drugs into the posterior segment of the eye. Systemically administered drugs cannot reach the vitreous cavity and the retina easily because of the blood–retinal barriers
Considering these problems, most recent therapies for vitreoretinal diseases, for example exudative (wet) age-related macular degeneration (AMD) and macular edema, have been administered by periocular or intraocular injection (Ip et al. 2004; Gillies et al. 2006; Rosenfeld et al. 2006; Brown et al. 2006; Augustin and Schmidt-Erfurth 2006). In the vitreous cavity, however, the half-life of most drugs with a low molecular weight is as short as a few hours, even large molecules such as antibodies have a half-life of a few days (Bakri et al. 2007a, b). Therefore, repeated intravitreal injections may be required, potentially associated with adverse effects such as cataract formation, vitreous hemorrhage, endophthalmitis, and retinal detachment (Cantrill et al. 1989; Cocherau-Massin et al. 1991; Heinemann 1989; Ussery et al. 1988).
Drug delivery systems (DDSs) may overcome the aforementioned problems of pharmaceutical approaches. Regarding DDSs to the anterior segment of the eye, some inserts used instead of eye drops are already commercially available: Ocusert® Pilo (controlled-release pilocarpine, Alza Co., Palo Alto, CA), Mydriasert® (IOLTech, La Rochelle, France), and Lacrisert® (hydroxypropyl cellulose ocular insert, Merck & CO., Inc., Whitehouse Station, NJ) (Fig. 2). Ocusert® Pilo inserts, which became commercially available in 1974, contain a core reservoir consisting of pilocarpine and alginic acid. The core is surrounded by a hydrophobic ethylene vinyl acetate (EVA) copolymer membrane that controls diffusion of pilocarpine, an active pharmaceutical ingredient (API), from the insert into the eye. Pilocarpine can decrease intraocular pressure in patients with glaucoma. While commonly used eye drops should be administered four times a day, the insert releases pilocarpine for a week after it is placed in contact with the conjunctival surface. Mydriasert® is an insoluble-matrix retropalpebral ophthalmic insert containing phenylephrine and tropicamide as APIs to obtain sustained mydriasis during surgery or fundus examination. Lacrisert® is biodegradable and inserted daily into the conjunctival sac instead of eye drops in the treatment of dry eye. These types of inserts could be easily removed if adverse effects develop. However, these inserts do not provide striking benefits over conventional use of eye drops. On the other hand, it must be beneficial but more complicated and hard to develop DDSs to the posterior segment of the eye. The implants should be placed into the sub-Tenon’s, intrascleral, or intravitreal space. In this case, any mechanical effects of the remaining matrix and any pharmacologic effects of the drug used should be considered.
In this section, we review medical devices for the treatment of diseases in the posterior segment of the eye which are clinically available, under clinical trial, or being tested preclinically.
2 Targeted Vitreoretinal Diseases
Vision loss easily impairs quality of life. In industrialized nations, AMD, diabetic retinopathy, and retinitis pigmentosa as well as glaucoma are main causes of legal blindness, while cataract and corneal diseases are still sight-threatening in developing countries. Retinal disorders are one of the most challenging diseases in the body, involving AMD, diabetic retinopathy, retinitis pigmentosa, and macular edema secondary to diabetic retinopathy, uveitis, pseudophakia, and retinal vein occlusion. Some eyes with glaucoma are refractory to any medications and surgical approaches. In such cases, retinal ganglion cells are damaged, resulting in progressive visual field defect. Thus, most hard-to-treat eye diseases are associated with alteration of retinal functions. Because the retina is a neurosensory organ with binocular harmonized function, the retina and, in particular, its center, called the macula, require homeostasis in (1) the structure and the location, (2) transparency, and (3) neurophysiology. AMD and macular dystrophy often lead to irreversible impairment of neurophysiologic functions at the macula. Macular edema impairs not only the structure but also the transparency and physiologic functions of the retina. To date, advances in surgery enable even the peeling of the internal limiting membrane, the innermost thin layer of the retina, by the use of special instruments, resulting in recent highly improved visual outcomes in eyes with macular holes. However, most other macular diseases are still refractory to any type of treatment.
Many vitreoretinal disorders are refractory to the effects of current medications because of the aforementioned difficulties in pharmacologic approaches. Therefore, a DDS may be necessary in the treatment of a variety of intraocular diseases. Potentially, an intraocular controlled (sustained) release system can be used for diseases in which repeated local administration of drugs is likely to be effective, such as wet AMD, macular edema, cytomegalovirus (CMV) retinitis, and uveitis. In addition, in diseases that initially require vitreoretinal surgery and in which complications or recurrence may occur postoperatively, intraocular controlled release devices implanted adjunctively during surgery may improve recovery (e.g., proliferative vitreoretinopathy (PVR), choroidal neovascularization (CNV), and diabetic retinopathy). Moreover, a controlled release system may be necessary to treat chronic diseases with no satisfactory therapies, such as geographic atrophy (dry AMD), macular edema, and retinitis pigmentosa.
2.1 Cytomegalovirus (CMV) Retinitis
CMV retinitis used to be an object of public concern, because it occurred in approximately 25% of patients with acquired immune deficiency syndrome (AIDS) and was a leading cause of blindness in terminally ill patients (Gross et al. 1990). This background urgently required the development of a new treatment modality. Early diagnosis and efficient management are necessary to preserve vision. Systemic administration of ganciclovir or foscarnet first proved effective in slowing the progression of CMV retinitis. However, these drugs frequently have serious side effects: ganciclovir causes myelosuppression and foscarnet kidney dysfunction, which may necessitate discontinuance of the therapy (Henderly et al 1987; Holland et al. 1986; Jabs et al. 1987). Therefore, intravitreal administration of ganciclovir was then carried out but needed to be repeated to maintain intraocular drug concentration in the therapeutic range, potentially associated with inherent risks of retinal detachment, cataract, vitreous hemorrhage, and endophthalmitis (Cantrill et al. 1989; Cocherau-Massin et al. 1991; Heinemann 1989; Ussery et al. 1988). A pressing need to preserve the quality of life in patients with AIDS focused on the development of new intraocular DDSs, leading to the first commercial use of a controlled release system for ganciclovir with a nonbiodegradable polymer device (Vitrasert®) (Sanborn et al. 1992). This proved to be effective and biocompatible clinically, although it required surgery to remove the exhausted unit or to repeat implantation (Morley et al. 1995; Sanborn et al. 1992; Smith et al. 1992). More recently, highly active antiretroviral therapy (HAART), a combination of reverse-transcriptase-inhibiting nucleosides and human immunodeficiency virus type 1-specific protease inhibitors, has been established to normalize immunity in patients with AIDS and promote the regression of several opportunistic infections including CMV retinitis (Autran et al. 1997; Mitchell et al. 1999; Vrabec et al. 1998). Thus HAART has significantly reduced the need for an intraocular device for patients with AIDS. Yet, a number of scientists that gained fundamental knowledge in the field of intraocular DDSs, and now continue to develop new devices to treat a variety of other challenging vitreoretinal diseases.
2.2 Noninfectious Uveitis
The uvea is the intraocular tissue with melanin granules, involving the iris, the ciliary body, and the choroid. Uveitis is an ocular autoimmune or inflammatory disease occurring in the uvea and adjacent tissues such as the sclera and the retina. Uveitis has acute or chronic features affecting local or diffuse areas of the eye, and it has the potential for recurrence. The disease often requires long-term medication with steroids, immunosuppressive agents, antibiotics, or their combination in order to suppress inflammation or prevent recurrence in specific cases. Persistent inflammation in the anterior segment sometimes results in posterior synechia of the iris limiting the dilation of the iris, secondary glaucoma with or without peripheral anterior synechia of the iris, and cataract formation, while longstanding inflammation in the posterior segment sometimes leads to hazy vitreous humor, macular edema, exudative or ischemic retinal vascular disorders, and other retinal dysfunctions. The necessity of long-term medication led to the development of a controlled release system for fluocinolone acetonide with a nonbiodegradable polymer device (Retisert®), which was approved by the US FDA in 2005 (Jaffe et al. 2000).
2.3 Macular Edema
Macular edema, if persistent, often leads to irreversible loss of visual acuity, accompanying a variety of diseases including diabetic retinopathy, uveitis, and retinal vein occlusion (Fig. 3). This disease is characterized by leakage of serum from retinal capillaries and subsequent swelling of the macula, the center of the retina.
Macular edema secondary to central retinal vein occlusion. (a) Fluorescein angiography revealed cystoid macular edema. (b) Optical coherence tomography showed a retinal section with cystic spaces at the macula. Visual acuity is 20/100. (c) Intravitreal injection of crystalline triamcinolone acetonide (4 mg) reduced the macular edema and improved visual acuity to 20/50. However, macular edema often recurs and requires repeated administration of drug, laser photocoagulation, or vitrectomy
Diabetic macular edema is one of major causes of legal blindness in patients with diabetes mellitus. There are approximately 500,000 cases requiring treatment in the USA every year. Permeability of retinal vasculature is enhanced by vascular endothelial growth factor (VEGF) secreted from retinal cellular components in response to occlusion of microcapillaries and subsequent ischemia. Also macular edema is affected by a variety of general conditions: degree of diabetic nephropathy as well as retinopathy, hypertension, anemia, and hyperlipidemia. Diabetic macular edema is classified into two types: focal and diffuse. Focal macular edema is often caused by microaneurysms with a compromise of the blood–retinal barrier integrity, which is treatable by laser photocoagulation of the microaneurysms. On the other hand, diffuse macular edema is caused by dilation of retinal capillaries around the macular area. Diffuse macular edema is currently treated by grid laser treatment, intravitreal or sub-Tenon’s injection of a steroid, triamcinolone acetonide (Ip et al. 2004; Gillies et al. 2006), or vitrectomy. More recently, some nonbiodegradable or biodegradable devices with various corticosteroids for intraocular use (Medidur®, I-vation®, and Posurdex®) as well as intraocular injection of anti-VEGF agents (Lucentis®, and Avastin®) are under clinical trial in the treatment of diffuse diabetic macular edema.
2.4 Retinitis Pigmentosa
Retinitis pigmentosa is a clinically and genetically heterogeneous group of eye diseases with primary retinal and RPE degeneration resulting from a variety of genetic alterations in physiologic functions of photoreceptors and underlying RPE cells as a sensor of visible light. Gene mutations involve autosomal dominant and recessive, X-linked, and mitochondrial modes. Most causal genes may be associated with the retinoid cycle, involving e.g., rpe65, abca4, vmd2. Generally, an electroretinogram is negative or non-recordable before the onset of visual field defect. Many cases have progressive visual field defect, in some cases accompanied by loss of visual acuity. To date, there have been no successful treatment modalities to improve genetic alteration or even delay the progression of symptoms. However, a recent report on gene therapy has shed hopeful light on the treatment. Intravitreal injection of rpe65-encoding adenovirus vector delayed the worsening of visual function in eyes with Leber’s congenital amaurosis (Maguire et al. 2008). This result suggests that long-term supply of defect or altered proteins derived from gene mutations may rescue eyes with retinitis pigmentosa. Intracellular delivery of proteins as well as gene therapies using viral or nonviral vectors, siRNAs, and so on may have great potential to treat retinitis pigmentosa.
2.5 Age-Related Macular Degeneration (AMD)
AMD is a leading cause of legal blindness in people over 50 years of age in most developed countries (Klein et al. 1992; Ryan et al. 1994). Fifteen million Americans and more in other western countries are affected by AMD. About 14–24% of US citizens aged 65–74 years and 35% of people over 75 years of age have the disease. There are approximately 200,000 new cases of AMD each year in USA, and the annual incidence is expected to grow as the population ages. AMD is classified into two types: choroidal neovascularization (CNV; exudative or wet AMD) and geographic atrophy (dry AMD). Geographic atrophy represents the death of photoreceptors and underlying RPE cells and the atrophy of underlying choriocapillaries, resulting in gradual impairment of central vision with no successful treatment. In contrast, CNV often results in acute or subacute irreversible visual loss (Ryan et al. 1994) (Fig. 4). CNV has been treated by surgical removal, macular translocation with scleral retraction sutures or 360° retinotomy, laser photocoagulation, photodynamic therapy, transpupillary thermotherapy, or radiation (American Academy of Ophthalmology 2000; Bressler 1997; Chakravarthy et al. 1993; Kaplan 1996; Macular Photocoagulation Study Group 1986, 1990, 1994a, b). Despite a variety of treatments, recovery of vision in eyes with CNV is still highly limited. In addition, the recurrence of CNV is a serious problem. Macular translocation with 360° retinotomy often dramatically improves visual acuity (Eckardt et al. 1999; Pertile and Glaes 2002). However, severe complications such as postoperative PVR and diplopia have yet to be minimized.
Recently, many clinicians, investigators, and pharmaceutical companies have been very interested in the development of pharmacologic therapies for AMD, because photodynamic therapy with a photosensitizer, topical steroid therapy, and more recently the use of anti-VEGF agents appeared relatively effective exudative AMD (Blumenkranz et al. 2002; Rosenfeld et al. 2006; Brown et al. 2006; Augustin and Schmidt-Erfurth 2006; Adamis and Shima 2005). A number of clinical trials are now completing, ongoing, or prepared. Recent successful cases have been performed by intravitreal or sub-Tenon’s injections because of the past history of the failures of pharmacologic approaches by systemic use of interferon alpha and thalidomide in the treatment of exudative AMD (Ip and Gorin 1996; Maguire et al. 2001; Pharmacologic Therapy for Macular Degeneration Study Group 1997). However, more recent new agents have been or are planned to be tested, not only by intravitreal or sub-Tenon’s injection but also by systemic administration or even by eye drops. Thus, recent major trends in the development of new compounds tend to make many subsequent innovators blind to the impaired access of pharmacologic agents to the posterior segment of the eye as a critical issue. The development of an intraocular controlled-release system or drug targeting is desired as eagerly as the development of a new potent anti-angiogenic agent.
2.6 Proliferative Vitreoretinopathy (PVR)
PVR, the major cause of failure of retinal detachment surgery, involves intraocular pathologic wound healing: the formation of fibrous membranes composed of RPE cells, glial cells, macrophages, and fibroblasts on or beneath the retina (Jerdan et al. 1989; Machemer and Laqua 1975; Retinal Society Terminology Committee 1983). RPE cells that scatter into the vitreous cavity or subretinal space after retinal detachment produce extracellular matrix proteins, proinflammatory cytokines, and chemokines. This results in breakdown of the blood–retinal barrier, recruitment of other inflammatory cells, and myofibroblastic transdifferentiation of RPE cells (Scheiffarth et al. 1988). Contractile forces generated within the fibrous tissue formed ultimately lead to tractional retinal detachment and/or macular pucker, which threaten vision. RPE cells and fibroblasts are usually the predominant cell types in the epiretinal membranes of PVR. A variety of cytokines may play a role in the pathogenesis of PVR, including transforming growth factor-beta (Gonzalez-Avila et al. 1995), platelet-derived growth factor (Milenkovic et al. 2003), basic fibroblast growth factor (Hueber et al. 1996–1997; La Heij et al. 2002), tumor necrosis factor-alpha (Armstrong et al. 1998), epidermal growth factor (Milenkovic et al. 2003), interleukin-1beta (El-Ghrably et al. 2001), interleukin 6 (El-Ghrably et al. 2001; La Heij et al. 2002), interleukin 8 (El-Ghrably et al. 2001), interferon gamma (El-Ghrably et al. 2001), hepatocyte growth factor (Hinton et al. 2002), connective tissue growth factor (Hinton et al. 2002), and VEGF (Armstrong et al. 1998). Thus many substances can be candidates in the treatment of PVR. On the other hand, a single treatment targeting one of these substances may be insufficient to treat PVR. Because surgical approaches are necessary in many cases to mechanically reduce the retinal traction, some devices for intraocular controlled release of drugs can be applied intraoperatively as an adjunct to decrease the incidence of PVR.
3 Nonbiodegradable Devices
The development of intraocular controlled release systems has been enthusiastically investigated since the late 1980s because of the urgent necessity to establish a new treatment modality alternative to repeated intravitreal injections of ganciclovir in the treatment of CMV retinitis in patients with AIDS. These efforts led to the first commercial product, Vitrasert®, which was a non-biodegradable implant containing ganciclovir (Fig. 2) (Sanborn et al. 1992). This reservoir-type implant is made up from non-biodegradable polymers such as poly(vinyl alcohol) (PVA), EVA, and silicon laminate, and contains an API in the inner space. This type exhibits the most stable and long-standing release profile of an API, as compared with other types of implants, because it can store a large amount of an API and regulate drug release merely by total surface area and thickness of PVA, a permeable polymer (Fig. 5a) (Okabe et al. 2003; Yasukawa et al 2004, 2006). EVA or silicon laminate, a nonpermeable polymer, is used to limit the practical surface area for drug permeability, while PVA is used to construct the framework of the device and regulate the rate of drug permeability. On the other hand, the disadvantages of this type involve the relatively large size of the device requiring a large incision for implantation, which may increase the risk of vitreous hemorrhage, subsequent epiretinal membrane and retinal detachment, and the potential need for removal surgery to exchange the implant or treat possible complications such as retinal detachment and API-induced adverse effects. In fact, the same type of implant, Retisert®, which releases fluocinolone acetonide for the treatment of chronic non-infectious uveitis, has a critically high incidence of steroid-induced cataract and glaucoma. The investigators must consider not only sustained effects but also possible adverse effects of APIs and nonbiodegradable devices in designing controlled release systems.
The release profiles of APIs from a non-biodegradable implant (a) and a biodegradable implant (b). A non-biodegradable implant is advantageous for stable and sustained release, while a biodegradable one requires no removal or exchange surgery. While a biodegradable implant (closed squares in b) generally exhibits a triphasic release pattern of APIs, a blend-type biodegradable implant (closed circles in b) can improve stability and period of API release. Reproduced from Okabe et al. (2003) and Yasukawa et al. (2000)
3.1 Vitrasert®: Nonbiodegradable Implant with Ganciclovir
Vitrasert® (Bausch & Lomb, Rochester, NY) is a reservoir-type implant that delivers ganciclovir, an antiviral drug, intraocularly in patients with AIDS-related CMV retinitis, approved in 1996 by FDA. Ganciclovir is a synthetic nucleoside analog of 2′-deoxyguanosine that inhibits replication of viruses including CMV, herpes simplex virus-1 and -2, Epstein–Barr virus, and varicella zoster virus. This intravitreal implant contains a ganciclovir tablet composed of 4.5 mg of ganciclovir and 0.25% of magnesium stearate as an inactive ingredient, coated with PVA and EVA. PVA and EVA are non-degradable polymers used for controlling the rate of drug release. Hydrophobic EVA was used to limit the surface area available for release of the hydrophilic drug. Ganciclovir is slowly released over a 5–8 month period of time across the water-permeable PVA membrane following the entrance of fluid into the device. Ganciclovir is partially dissolved with imbibed water up to the saturated concentration and continuously diffuses across the PVA membrane. The reservoir implant yields zero-order release kinetics, while the inner solution remains saturated with ganciclovir. Vitrasert® requires surgical implantation. A 5.5 mm sclerotomy is made circumferentially 4 mm posterior to the limbus. After trimming prolapsed vitreous humor, the ganciclovir implant is placed into the vitreous cavity through the sclerotomy and fixed with anchoring sutures. Then the sclerotomy and the conjunctiva are sutured. Caution is needed in handling the device so as not to damage the PVA membrane. After the implantation, most patients will experience an immediate decrease in visual acuity for the following 2–4 weeks. This temporal visual impairment may result from the surgical procedure itself. The implanted device will require the removal procedure if re-implantation is necessary or if any complications such as retinal detachment occur.
3.2 Retisert®: Nonbiodegradable Implant with Fluocinolone Acetonide
Retisert® (Bausch & Lomb, Rochester, NY) is a reservoir-type implant with the same shape as Vitrasert®, designed for the treatment of chronic non-infectious uveitis (Jaffe et al. 2000) (Fig. 6a). The implant consists of a tablet containing 0.59 mg of the active ingredient, fluocinolone acetonide, and inactive components such as microcrystalline cellulose, PVA, and magnesium stearate. The implant is coated with PVA and silicon laminate to yield sustained release of a corticosteroid, fluocinolone acetonide, at a steady rate of 0.3–0.6 µg/day to the posterior segment of the eye for a period of 30 months. The device is 5 mm long, 2 mm wide, and 1.5 mm thick, smaller than Vitrasert®. Fluocinolone acetonide reduces inflammation and lowers intravitreal VEGF levels in the eye. The recurrence rate of uveitis is reduced to 7–14% in the 34-week period post-implantation, in contrast to 40–54% in the control group. The implant also decreases the necessity to use systemic and topical administrations of steroid. The implantation procedure is same as that for Vitrasert®. Caution should be exercised in handling the implant in order to avoid damage to the PVA membrane, which may result in an unexpectedly increased rate of drug release from the implant. Intraocular sustained release of steroid, however, ironically results in a marked rate of steroid-induced intraocular complications. Within 34 weeks post-implantation, approximately 60% of patients will need medications to treat steroid-induced glaucoma. Moreover, within two years after implantation, approximately 32% of patients will require glaucoma (filtering) surgery (Callanan 2007). Also within a post-implantation period of two years, most phakic eyes will develop cataract formation and require cataract surgery. Nevertheless, because long-standing intraocular inflammation itself can be associated with incidence of secondary glaucoma and cataract, the sustained and excellent efficacy of the implant to treat chronic uveitis is highly appreciable.
A variety of medical devices for DDSs to the posterior segment of the eye. (a) Retisert® (Bausch & Lomb) contains a tablet with fluocinolone acetonide encapsulated with nonbiodegradable polymers. (b) I-vationTM (SurModics) is a helical nonbiodegradable implant with triamcinolone acetonide, implantable through a small incision. (c) Posurdex® (Allergan) is an injectable rod with dexamethasone placed with a special applicator
3.3 I-vationTM: Nonbiodegradable Implant with Triamcinolone Acetonide
A unique nonbiodegradable implant, I-vationTM (SurModics, Irvine, CA), is currently in a phase I clinical trial for the treatment of diabetic macular edema. This device contains and releases 0.925 mg of a corticosteroid, triamcinolone acetonide, slowly to the posterior segment of the eye. The shape of the device is a unique scaffold designed for minimally invasive implantation, different from those of Vitrasert® and Retisert® which require more invasive surgery for implantation (Fig. 6b). The implant’s small diameter enables implantation through a sclerotomy with a 25-gauge needle. The unique helical design maximizes the surface area available for drug release as well as enabling anchoring of the implant against the sclera. The thin cap attached is placed under the subconjunctival space. The triamcinolone acetonide is coated with a blend of polybutyl methacrylate and polyEVA. The safety and biocompatibility of I-vationTM have been derived from preclinical studies for up to 9 months post-implantation. SurModics is sponsoring a Phase I safety study called STRIDE (Sustained Triamcinolone Release for Inhibition of Diabetic Macular Edema) for the treatment of diabetic macular edema. Early clinical results show I-vationTM to be safe and well tolerated. Average macular thickness in eyes with diabetic macular edema decreased to 230 µm at month 6, as compared with preoperative thickness of 376 µm. The study subjects will be followed for three years. The release profile of drugs can be customized by varying ratios, thickness, and total surface area of constituent polymers in the coating. It remains to be seen whether the sclera tolerates anchoring of the device for long periods and after removal of the device.
3.4 Medidur®: Nonbiodegradable Insert with Fluocinolone Acetonide
Medidur® (Alimera Sciences Inc., Alpharetta, GA; pSivida Inc., Watertown, MA) is an injectable nonbiodegradable intravitreal implant for the treatment of diabetic macular edema. The Medidur® insert is only 3.5 mm in length and 0.37 mm in diameter, designed to release a constant amount fluocinolone acetonide to the posterior segment of the eye over a period between 18 and 36 months. The insert is a reservoir-type implant like other nonbiodegradable implants. In contrast to them, however, it is designed for sutureless insertion in an office setting by use of 25-gauge transconjunctival injector system without the necessity for surgical incisions in the conjunctiva and the sclera and subsequent suturing. The insert releases 0.2 µg or 0.5 µg of fluocinolone acetonide to the vitreous cavity per day. A phase III trial is under way for the treatment of diabetic macular edema. It should be ascertained whether the insert that is suspended without any fixation in the vitreous cavity will have any adverse effects and, if necessary, can easily be surgically removed.
4 Biodegradable Devices
Compared with non-biodegradable implants, biodegradable implants have the following merits: no need of removal surgery, and flexibility in shape. They can be processed into a variety of configurations such as microparticles, rods, discs, tablets, and implants (Fig. 2) (Yasukawa et al. 2004, 2006, 2007). Recently, Posurdex®, a rod that is injectable using a special injector with a 22-gauge needle, is under phase III clinical trial in the treatment of macular edema secondary to retinal vein occlusion or diabetic macular edema. This implant is composed of the homogenous mixture of dexamethasone as an API and poly(lactic-co-glycolic acid) (PLGA), a biodegradable polymer, categorized as the monolithic type. In general, this type has three phases of release of an API: (1) the first burst derived from APIs deposited on the surface of the implant; (2) the diffusion phase driven by osmotic pressure and polymer biodegradation; and (3) the final burst originating from sudden disintegration of matrix of the implant (Fig. 5b) (Yasukawa et al. 2004). Therefore, if the API possesses toxic effects at high concentrations, investigators should take the first and the final bursts into consideration. In contrast to reservoir-type implants, API release profiles for monolithic-type devices should be affected by a variety of factors involving types and molecular weight of polymers, mixing rate of polymers and APIs, and total surface area of the device. Yasukawa and Kunou et al. demonstrated that a blend of two kinds of polymers with different molecular weights resulted in reduction of the final burst and more stable and long-standing release of APIs (Fig. 5b) (Yasukawa et al. 2000; Kunou et al. 2000). Thus the release profile of APIs from biodegradable implants may become as stable as non-biodegradable ones, while the duration of API release may be shorter due to the limited amount of APIs contained.
4.1 Posurdex®: Biodegradable Insert with Dexamethasone
Posurdex® (Allergan Inc., Irvine, CA) is a biodegradable polymer matrix prepared with PLGA that releases dexamethasone over approximately five weeks and phase III clinical trials have been evaluating its usefulness in persistent macular edema associated with diabetic retinopathy, retinal vein occlusions, uveitis, and post-cataract surgery. The prototype of this insert was implanted through a 20-gauge scleral incision into the vitreous cavity in the operation area. A phase II clinical trial showed that patients who had been implanted with the insert containing 0.7 mg of dexamethasone had the greatest improvement in vision, and most of these patients exhibited a three-line increase in an eye chart to measure visual acuity. Adverse effects such as elevated intraocular pressure or cataract formation were not observed in the treated group. Thereafter, a novel insertion system employing a disposable applicator with a 22-gauge needle was developed for Posurdex® (Fig. 6c). The insert is injected in the office setting using this applicator. The clinical trials are currently in phase III to investigate efficacy and safety in larger numbers of patients with diabetic macular edema.
Surodex® (Oculex Pharmaceuticals, Sunnyvale, CA) is a PLGA pellet with 0.06 mg of dexamethasone to provide sustained release of dexamethasone over 7–10 days after insertion into the anterior chamber. Surodex® achieves higher intraocular drug levels than with conventional dexamethasone eye drops, effectively reducing post-cataract surgery inflammation (Tan et al. 1999). This insert is approved for use in cataract surgery in Singapore.
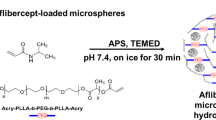
4.2 Injectable Microspheres
While it is advantageous that microspheres are injectable, in the 1990s intravitreally injected microspheres had been assumed to impair the transparency of intraocular media. Thereafter, intravitreal injection of crystalline triamcinolone acetonide began to be carried out in the treatment of macular edema and exudative AMD (Ip et al. 2004; Augustin and Schmidt-Erfurth 2006; Gillies et al. 2006). Triamcinolone acetonide is hydrophobic and mostly suspended in the vehicle. Nevertheless, crystalline triamcinolone acetonide mostly sinks down into the inferior part of the vitreous cavity, where it does not impair the ocular media and visual functions. This successful use of drug suspensions will provide great opportunities for intraocular DDSs using microparticles. The ongoing clinical trial of Posurdex® clearly indicates that biodegradable polymers are biocompatible. In the near future, many types of biodegradable implants and microparticles will proceed to clinical trial. In Japan, sub-Tenon’s injection of microspheres with betamethasone (DE-102, Santen Pharmaceuticals, Ikoma, Japan) is currently in phase II/III clinical trial for the treatment of diabetic macular edema. Also, microspheres with pegaptanib, an aptamer with affinity to VEGF (Macugen; Pfizer Inc., New York, NY), have been investigated in the laboratory. These microspheres, when injected intravitreally in rabbits, slowly release pegaptanib into the vitreous cavity for four months.
5 Triamcinolone Acetonide Crystal Suspensions
Crystal suspensions of triamcinolone acetonide have made great impact in the treatment of vitreoretinal diseases; intravitreal and sub-Tenon’s administrations of triamcinolone acetonide have been widely used in the treatment of macular edema, exudative AMD, and uveitis (Ip et al. 2004; Gillies et al. 2006; Augustin and Schmidt-Erfurth 2006) (Fig. 3c). Because of its hydrophobicity, injected crystals gradually dissolve, resulting in sustained release of triamcinolone acetonide. Intravitreal injection of 4 mg or sub-Tenon’s injection of 20 mg of triamcinolone acetonide provides 3-month efficacy in the chorioretinal tissue. While intravitreal injection is more effective than sub-Tenon’s injection, it has more frequent risk of steroid-induced glaucoma and cataract progression. Nevertheless, both complications are treatable in most cases. Thus the crystal suspensions are considered in a sense as DDSs without any polymer matrix as a base. Future candidates for devices to release steroids may need to have a release profile superior to that of intravitreally injected crystalline triamcinolone acetonide.
6 NT-501: Encapsulated Cell Technology (ECT)
ECT is a novel technology developed by Neurotech Pharmaceuticals, Inc. (Lincoln, RI, USA) to allow sustained delivery of cell-derived factors to the posterior segment of the eye. ECT implants consist of cells, which have been genetically modified to secrete therapeutic factors, and envelopes of semi-permeable hollow fiber membrane (Fig. 2). The permeability of the hollow fiber membrane enables long-term cell survival by allowing influx of oxygen and nutrients and preventing direct contact of encapsulated cells with cellular and molecular elements of the immune system. Encapsulated cells continuously produce the therapeutic protein, which diffuses out of the implant at the target site. Protein delivery in the vitreous cavity for as long as 18 months has been achieved by an ECT device, NT-501, containing human cells genetically engineered to secrete ciliary neurotrophic factor. NT-501 is fixed with suturing at the pars plana as for Vitrasert® and Retisert®. A phase I clinical trial was completed in early 2006 in ten patients diagnosed with retinitis pigmentosa at the National Eye Institute in the USA. ECT-mediated delivery of ciliary neurotrophic factor was found to be safe over a six-month treatment period. In addition, unexpectedly, visual acuities tended to improve a variable extend from baseline. NT-501 is currently in a phase II/III clinical trial for the treatment of retinitis pigmentosa and in a phase II clinical trial for the treatment of dry AMD. ECT devices can potentially release antibodies and cytokines, too.
7 Conclusion
In the treatment of exudative AMD, repeated intraocular injections of anti-VEGF agents recently exhibited remarkable inhibitory effects in contrast to other existing treatment modalities such as photodynamic therapy, laser photocoagulation, and surgery. A great number of drug candidates are now in clinical or preclinical trials. However, some trials are by systemic use or even by eye drops, not taking specificity in ocular pharmacokinetics into consideration. Some scientists have forgotten or did not recognize the previous unsuccessful history of interferon and thalidomide. Other therapies by a single compound may be less effective than anti-VEGF therapies, because VEGF must be a key regulator in many steps of inflammation and angiogenesis and thus its blockage can inhibit inflammatory reaction and angiogenesis directly and rapidly. Controlled release systems may be necessary to further improve efficacy and to reduce the incidence of adverse effects as compared with repeated intravitreal injections of anti-VEGF agents. In the 1980s, AIDS-associated cytomegalovirus retinitis accelerated advances in intraocular drug delivery systems, having realized the clinical use of non-biodegradable implants. Today, a variety of biodegradable implants and microparticles are also available for clinical use. Now, most challenging vitreoretinal diseases are targeted.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- AMD:
-
Age-related macular degeneration
- API:
-
Active pharmaceutical ingredient
- CMV:
-
Cytomegalovirus
- CNV:
-
Choroidal neovascularization
- DDS:
-
Drug delivery system
- ECT:
-
Encapsulated cell technology
- EVA:
-
Ethylene vinyl acetate
- HAART:
-
Highly active antiretroviral therapy
- PLGA:
-
Poly(lactic-co-glycolic acid)
- PVA:
-
Poly(vinyl alcohol)
- PVR:
-
Proliferative vitreoretinopathy
- RPE:
-
Retinal pigment epithelium
- VEGF:
-
Vascular endothelial growth factor
References
Adamis AP, Shima DT (2005) The role of vascular endothelial growth factor in ocular health and disease. Retina 25:111–118
Ambati J, Adamis AP (2002) Transscleral drug delivery to the retina and choroid. Prog Retin Eye Res 21:145–151
American Academy of Ophthalmology (2000) Photodynamic therapy with verteporfin for age-related macular degeneration. Ophthalmology 107:2314–2317
Armstrong D, Augustin AJ, Spengler R, Al-Jada A, Nickola T, Grus F, Koch F (1998) Detection of vascular endothelial growth factor and tumor necrosis factor alpha in epiretinal membranes of proliferative diabetic retinopathy, proliferative vitreoretinopathy and macular pucker. Ophthalmologica 212:410–414
Augustin AJ, Schmidt-Erfurth U (2006) Verteporfin therapy combined with intravitreal triamcinolone in all types of choroidal neovascularization due to age-related macular degeneration. Ophthalmology 113:14–22
Autran B, Carcelain G, Li TS, Blanc C, Mathez D, Tubiana R, Katlama C, Debré P, Leibowitch J (1997) Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. Science 277:112–116
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Ezzat MK, Singh RJ (2007a) Pharmacokinetics of intravitreal ranibizumab (Lucentis). Ophthalmology 114:2179–2182
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Singh RJ (2007b) Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology 114:855–859
Blumenkranz MS, Bressler NM, Bressler SB, Donati G, Fish GE, Haynes LA, Lewis H, Miller JW, MonÕs JM, Potter MJ, Pournaras C, Reaves A, Rosenfeld PJ, Schachat AP, Schmidt-Erfurth U, Sickenburg M, Singerman LJ, Slakter JS, Strong A, Vannier S; Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group (2002) Verteporfin therapy for subfoveal choroidal neovascularization in age-related macular degeneration: 3-year results of an open-label extension of 2 randomized clinical trials–TAP Report no. 5. Arch Ophthalmol 120:1307–1314
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, Sy JP, Schneider S; ANCHOR Study Group (2006) Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 355:1432–1444
Callanan DG (2007) Novel intravitreal fluocinolone acetonide implant in the treatment of chronic noninfectious posterior uveitis. Expert Rev Ophthalmol 2:33–44
Cantrill WH, Henry K, Melroe NH, Knobloch WH, Ramsay RC, Balfour HH (1989) Treatment of cytomegalovirus retinitis with intravitreal ganciclovir: long-term results. Ophthalmology 96:367–374
Chakravarthy U, Houston RF, Archer DB (1993) Treatment of age-related subfoveal neovascular membranes by teletherapy. Br J Ophthalmol 77:265–273
Cochereau-Massin I, Lehoang P, Lautier-Frau M, Zazoun L, Marcel P, Robinet M, Matheron S, Katlama C, Gharakhanian S, Rozenbaum W, et al. (1991) Efficacy and tolerance of intravitreal ganciclovir in cytomegalovirus retinitis in acquired immune deficiency syndrome. Ophthalmology 98:1348–1355
Eckardt C, Eckardt U, Conrad HG (1999) Macular rotation with and without counter-rotation of the globe in patients with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 237:313–325
El-Ghrably IA, Dua HS, Orr GM, Fischer D, Tighe PJ (2001) Intravitreal invading cells contribute to vitreal cytokine milieu in proliferative vitreoretinopathy. Br J Ophthalmol 85:461–470
Geroski DH, Edelhauser HF (2001) Transscleral drug delivery for posterior segment disease. Adv Drug Deliv Rev 52:37–48
Gillies MC, Sutter FKP, Simpson JM, Larsson J, Ali H, Zhu M (2006) Intravitreal triamcinolone for refractory diabetic macular edema. 2-year results of a double-masked, placebo-controlled, randomized clinical trial. Ophthalmology 113:1533–1538
Gonzalez-Avila G, Lozano D, Manjarrez ME, Ruiz VM, TerÃn L, Vadillo-Ortega F, Selman M (1995) Influence on collagen metabolism of vitreous from eyes with proliferative vitreoretinopathy. Ophthalmology 102:1400–1405
Gross JB, Bozzete SA, Mathews WC, Spector SA, Abramson IS, McCutchan JA, Mendez T, Munguia D, Freeman WR (1990) Longitudinal study of cytomegalovirus retinitis in acquired immune deficiency syndrome. Ophthalmology 97:681–686
Heinemann MH (1989) Long-term intravitreal ganciclovir therapy for cytomegalovirus retinopathy. Arch Ophthalmol 107:1767–1772
Henderly DE, Freeman WR, Causey DM, Rao NA (1987) Cytomegalovirus retinitis and response to therapy with ganciclovir. Ophthalmology 94:425–434
Hinton DR, He S, Jin ML, Barron E, Ryan SJ (2002) Novel growth factors involved in the pathogenesis of proliferative vitreoretinopathy. Eye 16:422–428
Holland GN, Sakamoto MJ, Hardy D, Sidikaro Y, Kreiger AE, Frenkel LM (1986) Treatment of cytomegalovirus retinopathy in patients with acquired immunodeficiency syndrome. Use of the experimental drug 9-[2-hydroxyl-1-(hydroxy-methyl)ethoxymethyl] guanine. Arch Ophthalmol 104:1794–1800
Hueber A, Wiedemann P, Esser P, Heimann K (1996–1997) Basic fibroblast growth factor mRNA, bFGF peptide and FGF receptor in epiretinal membranes of intraocular proliferative disorders (PVR and PDR). Int Ophthalmol 20:345–350
Ip M, Gorin MB (1996) Recurrence of a choroidal neovascular membrane in a patient with punctate inner choroidopathy treated with daily doses of thalidomide. Am J Ophthalmol 122:594–595
Ip MS, Gottlieb JL, Kahana A, Scott IU, Altaweel MM, Blodi BA, Gangnon RE, Puliafito CA (2004) Intravitreal triamcinolone for the treatment of macular edema associated with central retinal vein occlusion. Arch Ophthalmol 122:1131–1136
Jabs DA, Newman C, De Bustros S, Polk BF (1987) Treatment of cytomegalovirus retinitis with ganciclovir. Ophthalmology 94:824–830
Jaffe GJ, Ben-nun J, Guo H, Dunn JP, Ashton P (2000) Fluocinolone acetonide sustained drug delivery device to treat severe uveitis. Ophthalmology 107:2024–2033
Jerdan JA, Pepose JS, Michels RG, Hayashi H, de Bustros S, Sebag M, Glaser BM (1989) Proliferative vitreoretinopathy membranes. An immunohistochemical study. Ophthalmology 96:801–810
Kaplan H (1996) Submacular surgery for choroidal neovascularization. Br J Ophthalmol 80:101
Kim SH, Galban CJ, Lutz RJ, Dedrick RL, Csaky KG, Lizak MJ, Wang NS, Tansey G, Robinson MR (2007) Assessment of subconjunctival and intrascleral drug delivery to the posterior segment using dynamic contrast-enhanced magnetic resonance imaging. Invest Ophthalmol Vis Sci 48:808–814
Klein R, Klein BEK, Linton KLP (1992) Prevalence of age-related maculopathy: the beaver dam eye study. Ophthalmology 99:933–943
Kunou N, Ogura Y, Yasukawa T, Kimura H, Miyamoto H, Honda Y, Ikada Y (2000) Long-term sustained release of ganciclovir from biodegradable scleral implant for the treatment of cytomegalovirus retinitis. J Control Release 68:263–271
La Heij EC, van de Waarenburg MP, Blaauwgeers HG, Kessels AG, Liem AT, Theunissen C, Steinbusch H, Hendrikse F (2002) Basic fibroblast growth factor, glutamine synthetase, and interleukin-6 in vitreous fluid from eyes with retinal detachment complicated by proliferative vitreoretinopathy. Am J Ophthalmol 134:367–375
Lang LC (1995) Ocular drug delivery: conventional ocular formulations. Adv Drug Deliv Rev 16:39–43
Machemer R, Laqua H (1975) Pigment epithelium proliferation in retinal detachment (massive periretinal proliferation). Am J Ophthalmol 80:1–23
Macular Photocoagulation Study Group (1986) Recurrent choroidal neovascularization after argon laser photocoagulation for neovascular maculopathy. Arch Ophthalmol 104:503–512
Macular Photocoagulation Study Group (1990) Persistent and recurrent neovascularization after krypton laser photocoagulation for neovascular lesions of age-related macular degeneration. Arch Ophthalmol 108:825–831
Macular Photocoagulation Study Group (1994a) Visual outcome after laser photocoagulation for subfoveal choroidal neovascularization secondary to age-related macular degeneration: the influence of initial lesion size and initial visual acuity. Arch Ophthalmol 112:480–488
Macular Photocoagulation Study Group (1994b) Laser photocoagulation for juxtafoveal choroidal neovascularization: 5-year results from randomized clinical trials. Arch Ophthalmol 112:500–509
Maguire MG, Fine SL, Maguire AM, D'Amato RJ, Singerman LJ (2001) Results of the age-related macular degeneration and thalidomide study (AMDATS). Invest Ophthalmol Vis Sci 42:S233
Maguire AM, Simonelli F, Pierce EA, Pugh EN Jr, Mingozzi F, Bennicelli J, Banfi S, Marshall KA, Testa F, Surace EM, Rossi S, Lyubarsky A, Arruda VR, Konkle B, Stone E, Sun J, Jacobs J, Dell'Osso L, Hertle R, Ma JX, Redmond TM, Zhu X, Hauck B, Zelenaia O, Shindler KS, Maguire MG, Wright JF, Volpe NJ, McDonnell JW, Auricchio A, High KA, Bennett J (2008) Safety and efficacy of gene transfer for Leber’s congenital amaurosis. N Engl J Med 358:2240–2248
Maurice DM, Mishima S (1984) Ocular pharmacokinetics. In: Sears ML (ed) Pharmacology of the eye. Springer, New York
Milenkovic I, Weick M, Wiedemann P, Reichenbach A, Bringmann A (2003) P2Y receptor-mediated stimulation of Muller glial cell DNA synthesis: dependence on EGF and PDGF receptor transactivation. Invest Ophthalmol Vis Sci 44:1211–1220
Mitchell SM, Membrey WL, Youle MS, Obi A, Worrell S, Gazzard BG (1999) Cytomegalovirus retinitis after the initiation of highly active antiretroviral therapy: a 2 year prospective study. Br J Ophthalmol 83:652–655
Morley MG, Duker JS, Ashton P, Robinson MR (1995) Replacing ganciclovir implants. Ophthalmology 102:388–392
Okabe K, Kimura H, Okabe J, Kato A, Kunou N, Ogura Y (2003) Intraocular tissue distribution of betamethasone after intrascleral administration using a nonbiodegradable sustained drug delivery device. Invest Ophthalmol Vis Sci 44:2702–2707
Pertile G, Glaes C (2002) Macular translocation with 360-degree retinotomy for management of age-related macular degeneration with subfoveal choroidal neovascularization. Am J Ophthalmol 134:560–565
Pharmacological Therapy for Macular Degeneration Study Group (1997) Interferon alfa-2a is ineffective for patients with choroidal neovascularization secondary to age-related macular degeneration. Results of a prospective randomized placebo-controlled clinical trial. Arch Ophthalmol 115:865–872
Retinal Society Terminology Committee (1983) The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology 90:121–125
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, Kim RY; MARINA Study Group (2006) Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 355:1419–1431
Ryan SJ, Stout JT, Dugel PU (1994) Subretinal neovascularization. In: Ryan SJ (ed) Retina. Mosby, St. Louis
Sanborn GE, Anald R, Torti RE, Nightingale SD, Cal SX, Yates B, Ashton P, Smith T (1992) Sustained-release ganciclovir therapy for treatment of cytomegalovirus retinitis. Use of an intravitreal device. Arch Ophthalmol 110:188–195
Scheiffarth OF, Kampik A, Gunther H, von der Mark K (1988) Proteins of the extracellular matrix in vitreoretinal membranes. Graefes Arch Clin Exp Ophthalmol 226:357–361
Smith TJ, Pearson PA, Blandford DL, Brown JD, Goins KA, Hollins JL, Schmeisser ET, Glavinos P, Baldwin LB, Ashton P (1992) Intravitreal sustained-release ganciclovir. Arch Ophthalmol 110:255–258
Tan DTH, Chee SP, Lim L, Lim ASM (1999) Randomized clinical trial of a new dexamethasone delivery system (Surodex) for treatment of post-cataract surgery inflammation. Ophthalmology 106:223–231
Ussery FM, Gibson SR, Conklin RH, Piot DF, Stool EW, Conklin AJ (1988) Intravitreal ganciclovir in the treatment of AIDS-associated cytomegalovirus retinitis. Ophthalmology 95:640–648
Vrabec TR, Baldassano VF, Whitcup SM (1998) Discontinuation of maintenance therapy in patients with quiescent cytomegalovirus retinitis and elevated CD4+ counts. Ophthalmology 105:1259–1264
Yasukawa T, Kimura H, Kunou N, Miyamoto H, Honda Y, Ogura Y, Ikada Y (2000) Biodegradable scleral implant for intravitreal controlled release of ganciclovir. Graefes Arch Clin Exp Ophthalmol 238:186–190
Yasukawa T, Ogura Y, Kimura H, Sakurai E, Tabata Y (2006) Drug delivery from ocular implants. Expert Opin Drug Deliv 3:261–273
Yasukawa T, Ogura Y, Tabata Y, Kimura H, Wiedemann P, Honda Y (2004) Drug delivery systems for vitreoretinal diseases. Prog Retin Eye Res 23:253–281
Yasukawa T, Tabata Y, Kimura H, Kunou N, Ogura Y (2007) Development of drug-delivery systems to the posterior segments of the eye. Expert Rev Ophthalmol 2:197–211
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Yasukawa, T., Ogura, Y. (2010). Medical Devices for the Treatment of Eye Diseases. In: Schäfer-Korting, M. (eds) Drug Delivery. Handbook of Experimental Pharmacology, vol 197. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-00477-3_16
Download citation
DOI: https://doi.org/10.1007/978-3-642-00477-3_16
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-00476-6
Online ISBN: 978-3-642-00477-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)