Abstract
Drug delivery for ophthalmic diseases is often difficult due to the anatomy and physiology of the eye. Limited absorption and the layers of ocular tissue inhibit adequate amounts of topically applied ocular drops from reaching the target tissues of the eye. Similarly, the blood–aqueous and blood–retinal barriers prevent an adequate amount of intravenously administered drugs from reaching the eye. While intravitreal injection can bypass some of these limitations, these injections are invasive and must be performed often. Implantable drug delivery devices have been designed to overcome many of the difficulties associated with other ocular treatment options. These devices can be biodegradable, soluble, or nonbiodegradable and can be placed in different parts of the eye depending on the target tissue. For example, they can be placed intracamerally, intravitreally, or in the cul-de-sac of the eye. To optimize the ocular drug delivery system, various factors such as water solubility, toxicity, efficacy, and chemical and biopharmaceutical properties are taken into consideration. Although these drug delivery devices also have limitations, they are a great alternative that can reduce treatment burden, provide more targeted delivery, and minimize systemic side effects.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Treatment of ophthalmic diseases is inherently challenging due to the anatomy and physiology of the eye. Although topical medical therapy is the most common initial administration route, physical and dynamic barriers, such as ocular tissue layers, tear turn over, and clearance mechanisms, restrict delivery to the anterior and posterior segments of the eye and lower bioavailability (Edelhauser et al. 2010; Gaudana et al. 2010). A small amount of a topically applied dose is absorbed into the anterior segment, and only a percentage of that can move into the posterior segment (Lee and Robinson 2001). This makes treating diseases of the posterior segment such as diabetic retinopathy, age-related macular degeneration (AMD), and retinal vein occlusion (RVO), particularly challenging due to the greater diffusional distance (Lee and Robinson 2001; Yasukawa et al. 2006). In order to maintain minimum therapeutic concentrations, topical ocular drugs need to be administered frequently, often resulting in poor patient compliance (Hermann et al. 2010; Nordmann et al. 2010; Salyani and Birt 2005). Oral or IV administration can also be inadequate because the blood–aqueous and blood–retinal barriers limit the entry of the drug into the eye from the bloodstream (Cunha-Vaz 1979). Although some can be effective, they are accompanied by significant systemic side effects (Farkouh et al. 2016). In the 1980s, the first clinical studies of intravitreal (IVT) injected medications, 5-fluorouracil and ganciclovir, were conducted with the objective of providing more effective and targeted therapy. The injected substances were found to move throughout the vitreous fairly readily. The success led to the evaluation of a number of other IVT agents and the pace of development of new applications for IVT injection has continued (Jager et al. 2004). Although intravitreal injection is the preferred method for drug delivery to the posterior segment, there are drawbacks such as its invasiveness, the requirement for frequent administration, and its association with retinal detachment, cataract, endophthalmitis, and increased intraocular pressure (IOP) (Jager et al. 2004; Macha and Mitra 2002).
Due to these challenges, biomaterial and biotechnology advances have translated into the development of unique alternative treatment approaches in the form of implantable drug devices (Ghate and Edelhauser 2006; Patel et al. 2013; Yasukawa et al. 2006). This chapter presents a comprehensive view of controlled drug delivery devices that are either approved/marketed or currently in development and highlights their distinguishing features.
Ocular Drug Delivery Systems
Alternatives to Typical Ophthalmic Drug Administration Routes
Implantable ocular drug delivery systems can provide localized, controlled drug release over an extended period of time, which lowers the number of treatments required, possibly reducing the number of physician office visits and overall treatment costs. Systemic side effects are minimized due to the blood–retina/blood–aqueous barriers, high peak drug concentrations associated with pulsed dosing that are avoided, an increase in treatment adherence, and a potential reduction in treatment-related AEs (Ghate and Edelhauser 2008; Lee et al. 2011; Patel et al. 2013; Streilein 2003; Yasukawa et al. 2006). Some of the advantages and limitations of the different ocular drug delivery methods are summarized in Table 1. Various factors such as water solubility, toxicity, efficacy, chemical and biopharmaceutical properties, as well as the anatomy of the targeted ocular tissue are taken into consideration when optimizing the ocular drug delivery system (Avitabile et al. 2001). These devices can be inserted in the conjunctival cul-de-sac or punctum of the eye, or implanted in the subconjunctival, episcleral, intravitreal, or intracameral regions, and are categorized according to their degree of invasiveness and route of administration (Fig. 1) (Jervis 2017). In this chapter, we focus on biodegradable and nonbiodegradable polymer-based implants, implantable drug pumps, and ocular inserts that are currently approved/marketed or under investigation.
Types and locations of ocular drug delivery implants. (a) Both biodegradable and nonbiodegradable implants, that can be free-floating or anchored, can be placed intravitreally. (b) Implantable drug pumps are permanent devices that can be refilled. They are typically anchored subconjunctivally or in the pars plana. (c) Intracameral implants are typically free floating, biodegradable, and placed in the anterior chamber of the eye. (d) Ocular inserts are typically placed in the conjunctival cul-de-sac or punctum of the eye. Inserts can be insoluble, soluble, or biodegradable
Biodegradable Ocular Drug Delivery Systems
Biodegradable systems have been developed for intracameral and intravitreal placement and typically consist of a homogeneous polymeric pellet containing a therapeutic agent/drug and biodegradable polymer (Lee et al. 2010). The medication is released from the pores and skeleton as the hydrophobic polymer is converted into a water-soluble material via bulk or surface erosion. Bulk erosion occurs when water penetrates the matrix at a rate that is greater than that of polymer hydrolysis, while surface erosion occurs when water penetrates at a rate lower than that of polymer hydrolysis (Fig. 2) (Kuno and Fujii 2010; Robinson and Whitcup 2012). The drug release rate is influenced by the type of polymer and its biodegradation kinetics, the total surface area of the implant, and the percentage of loaded drug (Anderson and Shive 1997). Some advantages of the biodegradable system are that they do not elicit permanent chronic foreign body reactions or require surgical removal after the drug supply has been exhausted (Conway 2008; Jain 2000; Kimura and Ogura 2001). Some limitations of the biodegradable system that could impact effectiveness and/or safety are variable drug release profiles, a shorter duration of action when compared with nonbiodegradable implants, and destruction of the loaded medication before release is possible (Alhalafi 2017; Lee 2015; Miller et al. 1977). Biodegradable implants in clinical use and under investigation are summarized in Table 2.
Drug release mechanisms and biodegradation of matrix implants. In biodegradable implants, the drug (yellow circles) is dispersed in a biodegradable matrix (blue oval). As water penetrates the pores of the matrix, the drug molecules diffuse out. (a) Illustrates the bulk erosion process. Water molecules enter into the core of the implant and drug molecules exit from the core. The polymer begins to break down from internal cavitation. (b) Illustrates the surface erosion process. Drug and polymer are solubilized and released only on the surface of the implant. Over time, the implant reduces in volume and surface area (Lee et al. 2010, 2011)
Common biodegradable polymers include polylactic acid (PLA), polyglycolic acid (PGA), polylactic-co-glycolic acid (PLGA), polycaprolactones (PCL), and polyanhydrides (PAH), which break down into nontoxic byproducts and can be eliminated safely by the human body (Lee et al. 2011). They are aliphatic polyesters that belong to the “bulk-eroding” class of polymers and are the most widely studied of the synthetic biodegradable polymers, due to their mechanical properties, low immunogenicity and toxicity, excellent biocompatibility, and predictable biodegradation kinetics (Jain 2000). They are degraded predominantly by nonenzymatic hydrolysis to form lactic and glycolic acid monomers that are ultimately metabolized to carbon dioxide and water via the Krebs cycle (Swati and Oshin 2018). When these polymers are used, drugs are released through pseudo first-order kinetics, which occurs in three phases: burst release, diffusion and chain scission, and biodegradation and mass loss. In the initial burst phase, a rapid release of drug molecules is associated with the surface. Next, water is able to infuse in and cause random hydrolytic scission of bonds leading to polymer degradation (Lee et al. 2010, 2011).
Other biodegradable polymers under investigation for ocular implant use are polyorthoesters (POEs), polycyclic aromatic hydrocarons (PAHs), and polycarprolactone (PCL). POEs are synthetic, hydrophobic polymers whose degradation rate can be controlled by incorporating acidic or basic excipients into the polymer matrix. PAHs are hydrophobic polymers with hydrolytically labile anhydride linkages. The tendency of these linkages to react with drugs containing free amino groups limits the use of PAHs (Park and Lakes 2007). PCL is a semicrystalline, hydrophobic polymer in which initial degradation by bulk erosion is followed by a second, slow phase characterized by mass loss due to chain cleavage and drug diffusion from the polymer matrix (Silva-Cunha et al. 2009). Overall, PCL contains fewer (CH)2 units in the main chain than PAHs and is characterized by slow degradation (≥1 year) and high drug permeability, making it an ideal candidate for drug delivery systems (Park and Lakes 2007; Swati and Oshin 2018).
Biodegradable Implants in Clinical Use
Ozurdex/Posurdex
Ozurdex® (Allergan, an AbbVie company) is an intravitreal implant containing 0.7 mg of dexamethasone in a PLGA-based matrix (Novadur®, Allergan, an AbbVie company) that undergoes biphasic degradation, providing an initial loading/peak dose for 2 months, followed by a lower dose for up to 4 months. A specially designed preloaded, single-use applicator with a 22-gauge needle facilitates injection into the vitreous (Lee et al. 2010). It was approved by the United States Food and Drug Administration (FDA) in 2009 for the treatment of macular edema following branch retinal vein occlusion (RVO) and central RVO (CRVO), in 2010 for the treatment of noninfectious uveitis, and in 2014 for the treatment of diabetic macular edema (DME) (“Ozurdex approval history, Development History, and FDA Approval Process for Ozurdex” 2010). In phase 2 and phase 3 studies, conducted in patients with macular edema, the implant demonstrated significant improvements in visual acuity, vascular leakage, and central retinal thickness, compared with untreated or sham-controlled groups. Although the implant was shown to be well tolerated overall (Boyer et al. 2014; Haller et al. 2010, 2011; Kuppermann et al. 2007; Williams et al. 2009), the risk of cataract progression was increased in patients who received more than one implant (Boyer et al. 2014; Haller et al. 2011), and previous pars plana vitrectomy and the absence of lens capsule were found to be significant risk factors for implant migration into the anterior chamber (Khurana et al. 2014).
DEXYCU
Dexamethasone intraocular suspension 9% (DEXYCU) (EyePoint Pharmaceuticals, Inc.) was FDA approved in 2018 for the postoperative cataract surgery treatment of inflammation. It is administered by intracameral injection and uses the biodegradable sustained release Verisome® technology (“EyePoint Pharmaceuticals Announces U.S. Commercial Launch of DEXYCU (dexamethasone intracoular suspensio) 9%” 2019).
Bimatoprost Implant
Bimatoprost implant (Allergan, an AbbVie company) is an intracamerally injected, biodegradable implant that relies on an ophthalmic drug delivery system (DDS) to provide sustained-release of bimatoprost (Fig. 3). Bimatoprost implant is designed to provide long-term IOP-lowering to patients with open-angle glaucoma (OAG). In a phase 1/2 study, a single implant provided similar IOP lowering to topical bimatoprost 0.03% at 4 months. Overall, 91% of study eyes did not require rescue with topical bimatoprost or retreatment with an implant at 4 months. Moreover, bimatoprost implant lasted 6 months in 71% of patients. Most AEs reported in study eyes occurred within 2 days post-injection and were transient. Conjunctival hyperemia, the most frequent AE associated with bimatoprost and prostaglandin analogues, was less frequent with bimatoprost implant (6.7%) than the topical solution (17.3%) (Lewis et al. 2017). It recently gained FDA approval as the first intracameral, biodegradable sustained-release implant for the treatment of OAG or ocular hypertension (Allergan 2020).
Bimatoprost implant. (a) The Bimatoprost implant itself, next to a dime for size comparison. (b) The single-use implant applicator system for intracameral injection with a 28 gauge needle (Seal et al. 2019)
Investigational Biodegradable Implants
Brimonidine DDS
The injected intravitreal implant Brimonidine DDS , based off of Novadur® technology, provides sustained release of brimonidine. It has been evaluated in phase 2 studies involving patients with retinitis pigmentosa, glaucomatous optic neuropathy, geographic atrophy (GA) due to age-related macular degeneration, and rhegmatogenous (macula-off) retinal detachment (ClinicalTrials.gov identifiers: NCT00661479, NCT00693485, NCT00658619, and NCT00972374, respectively) (Lee et al. 2010). Results from the study of patients with GA indicated that treatment with the brimonidine implant, 132 μg or 264 μg, on day 1 and month 6 consistently produced smaller mean changes in GA lesion from baseline than sham treatment. At month 12, the primary endpoint, 18.8% and 27.5% reductions in GA progression rates were observed in the two treatment groups, respectively. Treatment-related ocular AEs were predominantly attributed to the injection procedure, the most common being conjunctival hemorrhage and conjunctival hyperemia (Freeman 2016). Although a study comparing the brimonidine implant (400 μg) and sham treatment every 3 months up to month 21 (ClinicalTrials.gov identifier: NCT02087085) was discontinued due to overall slow GA progression, the implant reduced the progression rate of GA by 10% at month 24 (P = 0.047) and 12% at month 30 (P = 0.017), compared with sham treatment (Freeman et al. 2019).
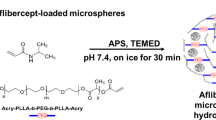
GB-102
GB-102 (Graybug Vision, Inc. Redwood City, CA) is a biodegradable intravitreal injection that is under investigation for the treatment of wet AMD. It is composed of microparticles made from PLGA and methoxy-polyethylene glycol (mPEG)-PLGA and sunitinib malate, a small molecule receptor tyrosine kinase inhibitor of vascular endothelial growth factor (VEGF)-1, -2, and -3. As the microparticles start to biodegrade, sunitinib malate is slowly released (“Graybug Vision Presents Top Line Results of Phase 1/2a ADAGIO Study at Hawaiian Eye & REtina 2019” 2019). In the phase 1/2a study (ClinitalTrial.gov identifier: NCT03249740), it met its primary endpoint of safety and tolerability. Although no serious adverse events were reported, there were reports of eye pain, photophobia, blurred vision, and vitreous haze. A single dose of GB-102 was able to maintain 90% of patients at 3 months and 70% of patients at 6 months (“Novel anti-VEGF for wet AMD meets safety, tolerability endpoint” 2019). Graybug is also developing drug-encapsulated microparticles for glaucoma treatments that will be injected in the subconjunctival space (GB-201, 202, 203) (‘GB-201, GB-202 and GB-203 – Glaucoma Products’ n.d.).
OTX-TKI
OTX-TKI (Ocular Therapeutix, Inc. Bedford, MA) is an investigational treatment for wet AMD that is delivered by intravitreal injection. It is composed of a bioresorbable hydrogel fiber containing tyrosine kinase inhibitor (TKI) particles that can potentially deliver the drug for a period of up to 9 months. A phase 1 clinical trial (ClinicalTrial.gov identifier: NCT03630315) is currently underway (“Ocular Therapeutix Announces Dosing of First Patient in Phase 1 Clinical Trial for the Treatment of Wet AMD” 2019).
OTX-TIC
Ocular Therapeutix has another investigational product that uses the bioresorbable material mentioned above. OTX-TIC is injected intracamerally (Fig. 4) and is composed of travoprost for the treatment of glaucoma. Preclinical studies have suggested that it can release drug for up to 4–6 months (“Ocular Therapeutix™ Announces Treatment of First Patient in Phase 1 Clinical Trial of OTX-TIC (travoprost intracameral implant) for the Treatment of Glaucoma and Ocular Hypertension” 2018).
OTX-TIC. The image shows the intracameral placement of OTX-TIC in the eye. (Image from Blizzard et al. (2019) and used under the terms of the Creative Commons Attribution 4.0 International License)
AR-13503
AR-13503 (Aerie Pharmaceuticals, Bedminster, NJ) was approved to start first-in-human clinical studies in 2019 (ClinicalTrial.gov identifier: NCT03835884). The novel drug is composed of a bioerodible polyesteramide polymer that releases a proprietary multi-kinase (Rho kinase/Protein kinase C) inhibitor. It is to be injected intravitreally for the treatment of nAMD and DME (“Aerie Pharmaceuticals Announces Acceptance of Its Investigational New Drug Application for AR-13504 Sustained Release Implant” 2019).
AR-1105
Also from Aerie Pharmaceuticals, AR-1105 is an implant that releases dexamethasone for the treatment of macular edema due to retinal vein occlusion (RVO). It is in phase 2 trials (ClinicalTrial.gov identifier: NCT03739593), and it uses the biodegradable PRINT® (Particle Replication In Non-Wetting Template) technology, which is a proprietary polymer that can be molded in the shape of a micropatterned template along with the drug. This implant can be injected intravitreally (“Aerie Pharmaceuticals Initiates Phase 2 Clinical Trials fo AR-1105 in Patients with Macular Edema Associated with RVO” 2019; “Drug Delivery Sustained Release Technology” 2017; Sandahl et al. 2018).
PA5108
PA5108 (PolyActiva Pty Ltd, Melbourne Australia) is composed of the drug latanoprost within a biodegradable polytriazole hydrogel system. It is placed intracamerally with a 27G needle for the treatment of glaucoma and is currently in Phase 1 clinical trials (ClinicalTrial.gov identifier: NCT03604328) (“PolyActiva Commences Its First Phase I Clinical Trial with Potential to Improve Daily Lives of Millions of Glaucoma Patients” 2018).
Discontinued Biodegradable Implants
Surodex
Surodex™ (Allergan, an AbbVie company, Dublin, Ireland) is a rod-shaped implant consisting of PLGA, 60 μg of dexamethasone an anti-inflammatory agent, and hydroxypropyl methylcellulose, which ensured drug release at a constant rate over 7–10 days (Lee et al. 2011). Following cataract surgery, the implant was inserted in the anterior chamber, without suture fixation, to control postoperative inflammation (Jain 2000; Lee 2015; Lee et al. 2011). In clinical studies, the implant was well tolerated and was shown to reduce anterior chamber cells and flare in the postoperative period. It exhibited anti-inflammatory properties that were at least as effective as those of topical steroids, while being less toxic (Kimura and Ogura 2001; Seah et al. 2005; Tan et al. 1999).
ENV515
ENV515 (Travoprost XR; Envisia Therapeutics, Durham, NC) is an intracameral ocular implant designed to release travoprost using the PRINT® technology to provide sustained IOP lowering to patients with primary OAG (“Envisia Therapeutics releases interim ENV515 (Travoprost XR) phase 2 data demonstrating 11-month duration-of-action after a single dose in patients with glaucoma” 2017). Interim analysis of a phase 2 study (ClinicalTrial.gov identifier: NCT02371746) showed the IOP-lowering effect of travoprost XR was comparable to that of topical prostaglandin analogues (latanoprost [Xalatan®, Pfizer] and bimatoprost [Lumigan®, Allergan, an AbbVie company]) used before study initiation, as well as topical timolol maleate 0.5% ophthalmic solution. The mean IOP reduction from baseline (26.1 mmHg) following a single injection was reportedly 25% (6.7 mmHg) at 11 months, and the most common AE was early onset hyperemia (“Envisia Therapeutics releases interim ENV515 (Travoprost XR) phase 2 data demonstrating 11-month duration-of-action after a single dose in patients with glaucoma” 2017).
IBI 20089
IBI 20089 (EyePoint Pharmaceuticals, formerly ICON Biosciences, Inc.) is an intravitreal drug delivery implant that relied on a proprietary, nanopolymer-based technology (Verisome™; Ramscor, Inc., Menlo Park, CA) designed for sustained release of a broad range of pharmaceutical agents, including small molecules, peptides, proteins, and monoclonal antibodies (Haghjou et al. 2011; Lee et al. 2010). The technology was reportedly highly versatile and could be formulated into a biodegradable solid, gel, or liquid substance (Haghjou et al. 2011). Moreover, degradation was reportedly independent of the reactant(s) concentration (Lee et al. 2010). A liquid formulation that delivers 6.9 mg or 13.8 mg of triamcinolone acetonide was recently evaluated for safety and efficacy in an open-label phase 1 trial that enrolled 10 patients with cystoid RVO-associated macular edema RVO (Lim et al. 2010). The formulation was well tolerated, with two reports of AEs: elevated IOP, treated with an Ahmed glaucoma valve, and panretinal coagulation (Lim et al. 2010). Despite seemingly encouraging data, it appears the implant is no longer being investigated.
Nonbiodegradable Ocular Drug Delivery Systems
One shortcoming often associated with biodegradable polymers, the initial and final medication release bursts, can be avoided by storing the drug in a reservoir. A nonbiodegradable polymer that is semipermeable or has fixed openings for smaller areas of diffusion can surround the drug in order to avoid release bursts (Fig. 5) (Bourges et al. 2006; Liechty et al. 2010; Yasin et al. 2014). Alternatively, the drug can be stored in a nonbiodegradable matrix, although an initial burst can be observed in this system (Conway 2008; Yasin et al. 2014). With nonbiodegradable polymers, the main advantage is long-term drug release due to near zero-order kinetics, which means a consistent amount of the drug is released over time (Bourges et al. 2006; Lee et al. 2010; Liechty et al. 2010; Patel et al. 2013). These implants can be designed to be a free-floating pellet injected intravitreally or intracamerally or anchored to the sclera. Some disadvantages are that their placement may require a large incision and sutures or some other form of anchoring, the need to surgically remove the depleted implant, and the extra costs and increased risk of AEs associated with these additional procedures (Lee et al. 2010; Patel et al. 2013). Nonbiodegradable implants in clinical use and under investigation are summarized in Table 2.
Nonbiodegradable drug delivery system. In a reservoir system , the drug (yellow circles) is surrounded by a nonbiodegradable membrane (green ring) that is semipermeable. This membrane acts as the framework of the implant and regulates the rate of release, allowing it to be constant. As water diffuses into the device, the drug pellet is dissolved and a saturated solution is released by diffusion out of the device. In the matrix system, the drug (yellow circles) is dispersed in a nonbiodegradable matrix (light green circle) and released through diffusion (Bourges et al. 2006; Conway 2008; Liechty et al. 2010; Yasin et al. 2014)
Polymers typically used for fabricating nonbiodegradable implants include polyvinyl alcohol (PVA), ethylene vinyl acetate (EVA), and silicon (Jervis 2017). While EVA and silicon are relatively impermeable hydrophobic polymers often used as drug-restricting membranes, PVA is a hydrophilic and more permeable polymer (Conway 2008; Kearns and Williams 2009; Lee et al. 2010). The combination of both an EVA/silicon membrane and a PVA are often used. Drug release occurs when water diffuses through the outer EVA/silicon coating and partially dissolves the enclosed drug, forming a saturated drug solution that is then released into the surrounding tissue via diffusion (Conway 2008; Kearns and Williams 2009). The drug release rate can be slowed by increasing the surface area or thickness of the drug-restricting membrane and can be increased by maximizing the surface area available for drug diffusion or by using a more permeable membrane (Lee et al. 2010).
Nonbiodegradable Intravitreal Implants in Clinical Use
Retisert
Retisert® (Bausch & Lomb 2016) is an intravitreal disc-shaped implant that was FDA-approved in 2005 for the treatment of chronic noninfectious uveitis of the posterior segment (Jervis 2017; Lee et al. 2011). It consists of a fluocinolone tablet encased in a silicone reservoir containing a single release pore, coated with a PVA membrane (Durasert™, EyePoint Pharmaceuticals, Watertown, MA). The implant is attached to a 5.5-mm silicone tab used to suture the implant into the vitreous at the pars plana near the ciliary processes Lee et al. 2011). In randomized studies involving patients with noninfectious uveitis, the implant improved visual acuity (Callanan et al. 2008; Jaffe et al. 2006; Kempen et al. 2011; Sangwan et al. 2015), reduced recurrence rates of uveitis (Callanan et al. 2008; Jaffe et al. 2019; Sangwan et al. 2015), and required less adjunctive systemic immunosuppression therapy than nonimplanted eyes (Sangwan et al. 2015). Another study conducted in patients with DME showed that the implant significantly improved visual acuity and retinopathy severity scores, reduced macular edema, and prevented retinal thickening for up to 3 years when compared with standard care (Pearson et al. 2011). Some drawbacks include an elevated risk of cataract surgery and glaucoma (Callanan et al. 2008; Jaffe et al. 2006; Kempen et al. 2011; Pearson et al. 2011; Sangwan et al. 2015) and spontaneous intraocular dissociation of the implant occurring years after placement (Rofagha et al. 2013). Another limitation for the clinical use of the Retisert implant is the high cost when compared to the oral prednisone therapy (Mohammad et al. 2007).
Iluvien
Iluvien™ (Alimera Sciences, Alpharetta, GA) is an intravitreal implant consisting of 190 μg of fluocinolone acetate embedded in a PVA matrix that is encased in a polyimide tube (Durasert™, EyePoint Pharmaceuticals, Watertown, MA; formerly Medidur™, PSivida). The implant is capped at one end and open at the other end, which allows for diffusion of water into the matrix and drug release (Fig. 6) (“Iluvien Prescribing information” 2019). Although two doses of the implant have been evaluated, with an average delivery rate of 0.2 μg/day (lasting 24–36 months) and 0.5 μg/day (lasting 18–24 months) (Campochiaro et al. 2010, 2011; Lee et al. 2011; Lee and Robinson 2009), only the lower-dose version was FDA-approved in 2014 to treat DME (“Iluvien Approval History” 2019). The lower dose produced similar levels of visual improvement as the higher dose, but with a lower rate of side effects (Campochiaro et al. 2012). Patients with persistent DME, who had at least one previous laser photocoagulation treatment, were shown to improve visual acuity 3, 6, and 12 months after a single insertion, although the change from baseline was not statistically significant at 12 months (Campochiaro et al. 2010). An analysis of 2 randomized, controlled studies showed that, when compared with sham treatment, there was statistically significant improvement of visual acuity at 24 months. There was also improvements in retinal thickness, and patients were less likely to receive additional DME treatments (Campochiaro et al. 2011). Additionally, it was found that the treatment benefit was maintained over 3 years, with maximum benefit at 30 months (Campochiaro et al. 2012). Nonetheless, as expected with steroidal implants, the incidence of elevated IOP and cataract surgery was increased in Iluvien treated patients (Campochiaro et al. 2010, 2011).
Schematic view of Iluvien , a nonbiodegradable intravitreal implant. This implant consists of a polyimide tube that is capped on one end and open on the other. Within the tube, fluocinolone acetate is embedded in a PVA matrix, which allows water to diffuse in and release the drug (Haghjou et al. 2011)
YUTIQ
YUTIQ™ (EyePoint Pharmaceuticals) is an intravitreal implant (3.5 × 0.37 mm) that was FDA-approved for the treatment of chronic, noninfectious uveitis of the posterior segment in 2018 (EyePoint 2021; FDA 2019). The implant consists of 180 μg of fluocinolone acetonide contained in a polyamide polymer-based reservoir, capped with silicone on the one end and a permeable PVA membrane on the other end (Durasert™, EyePoint Pharmaceuticals, Watertown, MA) (Jaffe et al. 2019; FDA 2019). It is designed to release fluocinolone acetonide over 3 years, at an initial rate of 0.25 μg/day (‘Iluvien Prescribing information’ 2019; EyePoint 2021). Two studies comparing YUTIQ vs sham indicated that YUTIQ reduced recurrence rates of uveitis and chronic noninfectious posterior uveitis (EyePoint 2021; Jaffe et al. 2006, 2019).
Investigational Nonbiodegradable Implants
Travoprost Intraocular Implant
The Travoprost Intraocular Implant (Glaukos Corporation, San Clemente, CA) uses the iDose™ delivery system and is being developed for the treatment of OAG and ocular hypertension. It consists of an implantable reservoir housed in a titanium implant that is secured in the iridocorneal angle. The reservoir releases travoprost through a membrane over 1 year and can be replaced. Interim data from a phase 2 study indicated that the implant resulted in 30% IOP reduction from baseline at 12 months (Varma 2018; Stephenson 2018) and the safety profile appeared favorable with no cases of conjunctival hyperemia reported (Stephenson 2018). Two ongoing phase 3 studies (ClinicalTrial.gov identifiers: NCT02754596 and NCT03868124) are expected to be completed in 2020 and 2023, respectively.
Targeted Episcleral Delivery System (Episcleral Implant/Reservoir)
This device (3T Ophthalmics Targeted Therapy Technologies, LLC Irvine, CA) is placed under the conjunctiva attached to the episcleral, but does not penetrate the eye. It is impermeable, except for the side that is open on the sclera. It acts as a reservoir that maintains a concentration gradient favoring diffusion of the drug through the sclera and also allows for the sustained release of drug (Pontes de Carvalho et al. 2006). The device has been tested preclinically with a variety of drugs including brimonidine (De Carvalho et al. 2014), topotecan, melphalan (Carvalho et al. 2016), and celecoxib (Lima et al. 2018). In addition, a phase 1 clinical trial was started in 2019 using dexamethasone for the treatment of DME (ClinicalTrial.gov identifier: NCT04005430).
Discontinued Nonbiodegradable Implants
Vitrasert
Vitrasert® (Bausch & Lomb, Rochester, NY), a controlled-release (5–8 months) intravitreal implant that consisted of a ganciclovir tablet in a PVA matrix surrounded by a nonbiodegradable EVA coating (Durasert™ technology [formerly Medidur]), EyePoint Pharmaceuticals, Watertown, MA), was FDA-approved (1996) for the treatment of cytomegalovirus retinitis associated with acquired immune deficiency syndrome (Patel et al. 2013). Ganciclovir was released via passive diffusion through a small opening in the EVA membrane (at the base of the implant) (Jervis 2017). Notably, the implant was shown to be twice as effective at slowing disease progression, compared with intravenous ganciclovir (Musch et al. 1997). It was also thought to be the best treatment choice, compared with the oral or intravenous prodrug, for cytomegalovirus retinitis lesions that pose an immediate risk to vision (Kedhar and Jabs 2007). Nonetheless, the implant was discontinued in 2013 following patent expiration (“Psivida Corp Annual report 2016”).
I-Vation
I-Vation™ (SurModics, Eden Prairie, MN) consisted of a titanium helical coil coated with triamcinolone acetonide and encased in a proprietary blend of nonbiodegradable polybutyl methacrylate and EVA, the composition of which controlled the delivery rate (Jervis 2017; SurModics 2013). The device had a sharpened tip, which was used to make the incision for intravitreal implantation. Its helical shape maximized the surface area for drug coating while enabling secure anchoring to the pars plana/sclera (Conway 2008). The implant had been under investigation for the treatment of DME, but results from a phase 1 clinical trial indicated relatively high incidences of conjunctival hemorrhage (90%) and lenticular opacities (35%) (Kiernan and Mieler 2009). Perhaps as a consequence of these findings, enrollment in a phase 2 trial (ClinicalTrials.gov identifier: NCT00692614) (“A Study of MK0140 in Diabetic Patients With Macular Edema (0140-001)” n.d.) was low, and the study was terminated in 2008 (Kiernan and Mieler 2009).
Lumitect
Lumitect® (Lux Biosciences Inc., Jersey City, NJ), also known as LX201, was a silicone-based, drug-eluting, episcleral implant that was originally developed at the National Eye Institute (BioSpace 2006). It was designed to deliver cyclosporine for up to 3 years. However, they failed to meet the primary endpoint of a phase 3 study (ClinicalTrials.gov Identifier: NCT00447642) conducted to evaluate its effectiveness in preventing corneal allograft rejection/failure, and the study was terminated. The company is reportedly developing an alternative oral drug (voclosporin [Luveniq]) (Weintraub 2012).
NT-503
NT-503 (NeuroTech Pharmaceuticals, Inc. Cumberland, RD) used encapsulated cell therapy (ECT) to deliver a soluble anti-VEGF receptor protein for the treatment of wet AMD. ECT was implanted into the vitreous for up to 2 years and held in place with sutures. When more than the expected number of patients needed rescue medication, the phase 2 clinical study (ClinicalTrial.gov identifier: NCT02228304) was discontinued (“NT-502 ECT” 2016).
Implantable Drug Pumps
Implantable drug pumps are also nonbiodegradable implants. In contrast to other ocular drug delivery devices that hold only a predetermined amount of drug, implantable drug pumps are refillable (Pearce et al. 2015).
Replenish MicroPump
The Replenish MicroPump (RMP; Replenish, Pasadena, CA) is a surgically implantable drug pump. It is a subconjunctival/episcleral implant with a reservoir that is refillable by a transconjunctival injection (Pearce et al. 2015). It is designed to release nanoliter doses of medication at a preprogrammed interval through an intraocular cannula implanted in the pars plana. Anterior and posterior platforms that can target both ocular segments are in development (Lo et al. 2009; Saati et al. 2010). There were no intraoperative complications, no serious AEs, and no worsening of visual acuity or central foveal thickness, compared with baseline during the first-in-man 90-day safety study of the RMP in patients with DME. The RMP delivered the programmed ranibizumab dosage in 7/11 patients, while the remaining four patients received a lower dose, and treatment was complemented with standard intravitreal injection (Humayun et al. 2014).
Port Delivery System
The Port Delivery System (PDS, ForSight VISION4, Inc., acquired by Genentech/Roche Holding AG, Basel, Switzerland) is in development as a refillable drug delivery device (Joseph et al. 2017; Pearce et al. 2015). PDS is composed of polysulfone and is placed through a scleral incision in the pars plana. The device has a semipermeable titanium membrane that allows constant passive diffusion of the drug into the vitreous (Fig. 7). In a phase 2 study, the PDS (filled with ranibizumab 10, 40, or 100 mg/mL) was evaluated in 220 patients with neovascular AMD who had received ≥2 prior anti-VEGF intravitreal injections and were responsive to treatment. Only patients with the PDS 100-mg/mL treatment had improvements in best-corrected visual acuity and central foveal thickness that were comparable with the monthly intravitreal ranibizumab 0.5 mg injections. The optimized PDS implant insertion and refill procedures were generally well tolerated, with a rate of postoperative vitreous hemorrhage of 4.5% (7/157, including 1 serious event) (Campochiaro et al. 2019). The potential reduction in treatment burden supported further development in ongoing phase 3 studies that are expected to be completed in 2022 (ClinicalTrials.gov identifiers: NCT03677934 and NCT03683251) (“A Phase 3 Study to Evaluate the Port Delivery System Implant with Ranibizumab Compared with Monthly Ranibizumab Injections in Participants with Wet Age-Related Macular Degeneration (Archway)” 2021; “Extension Study for the Port Delivery System With Ranibizumab (Portal)” 2021). However, a phase 1/2 study of the PDS (filled with methotrexate 0.6 or 2.3 mg) in noninfectious uveitis (ClinicalTrials.gov identifier: NCT02125266) was terminated due to an unacceptable frequency of drug-related AEs (“Safety and Preliminary Efficacy Study of V404 PDS in Uveitis” n.d.). Assuming proper functioning of the PDS, further investigation of the device with other drugs might be warranted.
Schematic of the Port Delivery System (PDS) implanted in the eye. The device is anchored in the pars plana, and the drug reservoir portion of the device is in the vitreous. The device can be refilled multiple times with a special needle. The semipermeable titanium membrane allows continuous, passive diffusion of the drug in the reservoir into the vitreous. (Image used from Campochiaro et al. (2019) with permission conveyed through Copyright Clearance Center, Inc)
Ocular Inserts
Designed for placement in the cul-de-sac, conjunctival sac, or punctum of the eye, ocular inserts aim to increase the contact time between the medication and conjunctival tissue to ensure sustained release suited for topical or systemic treatment. Although less invasive and easier to place than intravitreal implants, ocular inserts have several potential disadvantages. For example, they can interfere with vision and cause foreign body sensation in the eye. This can cause discomfort leading to irritation and excessive tearing which dilutes the drug. The insert can also become lost during sleep or while rubbing the eye and movement around the eye can complicate the removal if an insoluble insert migrates to the upper fornix. Additionally, due to its rigidity, the insert can be difficult to place and remove. There are three types of ocular inserts: (1) insoluble inserts, (2) soluble inserts, and (3) biodegradable inserts (Kumari et al. 2010).
Insoluble Ocular Inserts in Clinical Use or In Development
Insoluble ocular inserts can be further broken down into three categories: diffusion insert, osmotic insert, and soft contact lens. Diffusion inserts typically consist of a drug reservoir enclosed in a specially designed semipermeable or microporous membrane. As tear fluid permeates through the membrane and inside the reservoir, internal pressure drives the drug out at a controlled rate. Osmotic inserts generally have two basic designs. In one, the drug is the central part of the insert and is surrounded by the polymer as discrete small deposit. While in the other, the drug and osmotic solutes are placed in two separate reservoirs surrounded by an elastic impermeable membrane and semipermeable membrane, respectively. Both types of osmotic inserts are covered with a peripheral film made of an insoluble semipermeable polymer and as tears diffuse through the semipermeable membrane of the reservoir, the osmotic pressure increases, causing the polymer matrix to rupture and form apertures through which the drug is released through zero-order kinetics (Kumari et al. 2010). Soft contact lens consists of covalently cross-linked hydrophilic or hydrophobic polymers forming a three-dimensional matrix capable of retaining water, aqueous solution, or solid components. They do not deliver drugs as uniformly as other insoluble ophthalmic systems, and generally, the drug release is very rapid at the beginning then declines exponentially with time. The initial release rate can be decreased by adding hydrophobic components (Kumari et al. 2010).
Mydriasert
Mydriasert (Thea Laboratories, Clermont-Ferrand, France) is an insoluble rod-shaped ophthalmic insert composed of tropicamide and phenylephrine hydrochloride. It is placed in the upper/lower conjunctival fornix and delivers mydriasis prior to surgery (Bertens et al. 2018). In studies comparing Mydriasert versus phenylephrine and tropicamide eye drops, the mydriatic effect was comparable after 60 min, but was superior after 90 min and maintained good pupil dilation during cataract surgery (Saenz-de-Viteri et al. 2013). Mydriasert has also been compared with eye drops in patients undergoing retinal angiography. Although they have similar efficacy, the low total drug dose administered with the insert may potentially reduce the risk of cardiovascular side effects (Cagini et al. 2014).
Punctal Plugs
Several punctal plugs of varying shapes and dimensions are currently under investigation, including some containing prostaglandin analogues for the reduction of IOP in the management of glaucoma. Mati Therapeutics (Austin, TX) is developing a product, known as latanoprost-punctal plug delivery system (L-PPDS), based on its proprietary punctal plug delivery system (Evolute®) to deliver latanoprost. Evolute’s drug core reportedly allows sustained, unidirectional drug release into the tear film, thus minimizing systemic absorption. Vistakon Pharmaceuticals (a division of Johnson & Johnson Vision Care, Inc.; Jacksonville, FL) is testing a different platform to deliver bimatoprost (Whitcup and Azar 2017). Phase 2 studies evaluating those plugs associated with sustained release of latanoprost or bimatoprost in glaucoma patients are either ongoing or have been completed but have not yet been published (ClinicalTrials.gov Identifiers: NCT00855517 and NCT01229982).
Bimatoprost Ring
The Bimatoprost Ring (Allergan, an AbbVie company; formerly Helios, ForSight) is a 1-mm-thick ring with a diameter of 24–29 mm consisting of an internal polypropylene support covered with bimatoprost-loaded silicone for the management of glaucoma. It is placed in the fornix and releases bimatoprost over 6 months (Fig. 8) (Varma 2018). In a phase 2 study comparing the ring to regular unpreserved timolol 0.5% ophthalmic solution over 6 months, IOP reduction was not significantly different and drop-out rate was high. Retention rate was improved after 13 months as patients gain experience using the ring (Macha and Mitra 2002).
Schematic of the bimatoprost ring ocular insert . The soft insert is constructed of a bimatoprost and silicone-matrix polymer with an internal polypropylene support structure. It is placed on the ocular surface of the eye (Brandt et al. 2016)
OphthaCoil
OphthaCoil is a coiled stainless-steel wire device being developed in the Netherlands for placement in the lower conjunctival sac (Fig. 9). Drugs, such as antibiotics or mydriatic agents, can be loaded on microspheres or filaments that are placed in the device lumen or deposited on the outside SlipSkin® surface as coating (Bertens et al. 2018). In human pilot trials, short-term high tolerance and comfort of the device was demonstrated for a period of 2 h (Pijls et al. 2005, 2007). Preclinical and clinical trials are being conducted to further explore the potential of an ocular coil as an ocular drug delivery device for an extended period of time, up to 28 days (Bertens et al. 2018).
Schematic of OphthaCoil . The coiled stainless-steel wire device can be loaded with drugs and placed in the lower conjunctival sac. (Image used from Pijls et al. (2005) with permission conveyed through Copyright Clearance Center, Inc)
TODDD
The topical ophthalmic drug delivery device (TODDD™, Amorphex Therapeutics, Andover, MA) is an “eight-shaped” elastomer, viscoelastic polymer (20-mm long, about 8-mm wide, and 1-mm thick) containing timolol or prostaglandin (Bertens et al. 2018). It is intended for placement on the sclera, below the upper eyelid of patients with glaucoma. The timolol-loaded device has demonstrated an IOP reduction of 16%–22% after 6 months (Bethke 2015).
Soluble Ocular Inserts
Soluble inserts utilize either natural or synthetic/semisynthetic polymers that release drug by diffusion when tears penetrate the insert and form a layer of gel around the core of the insert (Kumari et al. 2010). The advantages of these devices are that they are completely soluble and do not need to be removed (Calles et al. 2015; Kumari et al. 2010). Drawbacks include rapid penetration of the lacrimal fluid into the device, blurred vision due to solubilization of insert components, and the glassy constitution of the insert increases the risk of expulsion (Calles et al. 2015).
Lacrisert
Lacrisert® (Aton Pharma, Inc./Bausch Health Companies, Lawrenceville, NJ), which was introduced in 1981 for the treatment of dry eye, is a translucent, rod-shaped, water-soluble insert made of hydroxypropyl cellulose (HPC), a physiologically inert substance designed for daily placement into the inferior cul-de-sac of the eye. Preclinical dissolution studies have shown that the HPC inserts become softer within 1 h of placement and completely dissolved in 14–18 h. The release of HPC stabilizes and thickens the precorneal tear film, prolonging the tear breakup time (Lee et al. 2011). In a multicenter, crossover study, once-daily treatment with the insert was generally well tolerated with more patients preferring the insert and reporting greater comfort with the insert than with artificial tears. Side effects, which were typically mild and transient, include blurred vision, ocular discomfort/irritation, matting/stickiness of eyelashes, photophobia, hypersensitivity, eyelid edema, and hyperemia (Hill 1989; Bausch and Lomb 2016).
OTX-TP
OTX-TP (Ocular Therapeutix, Bedford, MA) is a cylindrical, resorbable punctal plug that contains preservative-free travoprost and is intended for glaucoma treatment. It expands when hydrated and releases drug over 3 months, by which time 90% of the plug has dissolved and drained into the nasolacrimal duct. Phase 2 studies have demonstrated 88% retention at 75 days and slightly less IOP lowering than timolol at 90 days (Varma 2018).
Bioerodible/Biodegradable Ocular Inserts
Biodegradable ocular inserts are typically composed of a homogeneous drug dispersion coated by a hydrophobic, polymeric matrix, such as POEs and orthocarbonates that are impermeable to the drug (Lee et al. 2011). Drug release occurs as the tear fluid makes contact with the device and induces superficial bioerosion of the matrix causing the insert to dissolve in the eye in days or months (Kumari et al. 2010).
NODS
The New Ophthalmic Delivery System (NODS®; Smith and Nephew Pharmaceuticals Ltd., Essex, UK) is made from water-soluble PVA and placed in the cul-de-sac of the lower eyelid. It has been loaded with drugs such as pilocarpine, chloramphenicol, and tropicamide (Bertens et al. 2018). Although commercially available, there have been reports of intense miosis (Greaves et al. 1992), as well as problems with the detachment of the insert from its applicator (Diestelhorst and Krieglstein 1994).
Investigational Ocular Inserts
Brimonidine-Based Insert
Development of a brimonidine tartrate-releasing insert for the treatment of glaucoma has been initiated, as evidenced by in vitro and in vivo findings published between 2011 and 2014 (Bhagav et al. 2011; Ravindran et al. 2014). Although various matrix types are being evaluated, none have been reported for investigation in clinical studies (Mealy et al. 2014).
Discontinued Ocular Inserts
Dextenza
Dextenza , the resorbable PEG punctal plug (Ocular Therapeutix, Bedford, MA), was designed for the treatment of inflammatory eye conditions. It initially showed encouraging results in phase 2 and 3 trials in terms of improving signs and symptoms of allergic conjunctivitis. However, in July 2017, the FDA rejected the company’s new drug application (NDA) due to deficiencies in the manufacturing process and analytical testing identified during inspection of a manufacturing facility (Bertens et al. 2018).
Gelfoam
Gelfoam® discs (Pharmacia & Upjohn Compnay LLC, Peapack, New Jersey, USA) are biodegradable inserts made of resorbable gelatin, which could be infused with mydriatic drugs or insulin and inserted in the lower conjunctival fornix to treat various ocular diseases (Bertens et al. 2018). In clinical studies involving volunteers, some developed a palpebral conjunctival infection (hyperemia), while others developed superficial punctate erosion (Lee et al. 2002; Niegvesky et al. 2000). There have been no reports that this ocular insert was ever commercialized, and it does not appear to be under further investigation (Bertens et al. 2018).
Ocusert Pilo
Ocusert Pilo (Alza Corporation, acquired by Johnson & Johnson, New Brunswick, NJ) is an oblong-shaped, sustained-release, nonbiodegradable ocular insert that was placed in the conjunctiva and was approved in 1974 for the treatment of glaucoma (Bertens et al. 2018). It consisted of pilocarpine hydrochloride and alginic acid, contained within a reservoir enclosed by two release-controlling EVA membranes and surrounded by a titanium oxide ring to aid in positioning and placement (Conway 2008; Ghate and Edelhauser 2006). Originally available in two doses, it was the first marketed device to achieve zero-order kinetics, but was discontinued in 1998 due to unexpected burst release and dislocation problems (Bertens et al. 2018; Ghate and Edelhauser 2006).
Conclusion
This chapter has provided an overview of ocular implantable drug devices, which have been engineered to overcome some of the challenges with treating ocular diseases. While topically administered drops are convenient, they have limited uptake, must be applied often, and have a risk of poor patient adherence. Systemic administration is easy but has restricted ocular penetration and systemic side effects. While intravitreal injections have targeted delivery, they required frequent injections due to short lasting treatment. Implantable drug devices are longer lasting, decreasing the treatment burden, and typically have more targeted delivery when compared to other methods of ocular delivery. Some shortcomings of nonbiodegradable implants are that they require invasive surgeries for implantation and removal, both processes have associated adverse events. While biodegradable implants do not have to be removed, they have the potential for erratic drug release and typically do not last as long as nonbiodegradable implants. Biological and technological advances continue to improve treatment options for ocular disease, and continual effort is being made to improve ocular drug delivery systems to minimize adverse events and other issues while maximizing the benefits.
Abbreviations
- AMD:
-
Age-related macular degeneration
- BRVO:
-
Branch RVO
- CRVO:
-
Central RVO
- DME:
-
Diabetic macular edema
- EVA:
-
Ethylene vinyl acetate
- GA:
-
Geographic atrophy
- PAH:
-
Polyanhydrides
- PCL:
-
Polycaprolactones
- PDS:
-
Port delivery system
- PGA:
-
Polyglycolic acid
- PLA:
-
Polylactic acid
- PLGA:
-
Polylactic-co-glycolic acid
- POE:
-
Polyorthoesters
- PVA:
-
Polyvinyl alcohol
- RMP:
-
Replenish MicroPump
- RVO:
-
Retinal vein occlusion
- VEGF:
-
Vascular endothelial growth factor
References
A study of MK0140 in diabetic patients with macular edema (0140-001) a study of MK0140 in diabetic patients with macular edema (0140-001). Available from: https://clinicaltrials.gov/ct2/results?term=NCT00692614&Search=Search. Accessed 27-Oct-2021.
Aerie Pharmaceuticals Announces Acceptance of Its Investigational New Drug Application for AR-13504 Sustained Release Implant. BioSpace; 2019.
Aerie Pharmaceuticals Initiates Phase 2 Clinical Trials of AR-1105 in Patients with Macular Edema Associated with RVO. Eyewire; 2019.
Alhalafi A. Applications of polymers in intraocular drug delivery systems. Oman J Ophthalmol. 2017;10:3–8.
Allergan. Allergan receives FDA approval for DURYSTA™ (BIMATOPROST implant) the FIRST and only INTRACAMERAL biodegradable sustained-release implant to lower intraocular pressure in open-angle GLAUCOMA or ocular hypertension patients. 2020.
Anderson JM, Shive MS. Biodegradation and biocompatibility of PLA and PLGA microspheres. Adv Drug Deliv Rev. 1997;28:5–24.
Avitabile T, Marano F, Castiglione F, Bucolo C, Cro M, Ambrosio L, Ferrauto C, Reibaldi A. Biocompatibility and biodegradation of intravitreal hyaluronan implants in rabbits. Biomaterials. 2001;22:195–200.
Bausch & Lomb. Lacrisert Prescribing Information. 2016.
Bertens CJF, Gijs M, van den Biggelaar FJHM, Nuijts RMMA. Topical drug delivery devices: a review. Exp Eye Res. 2018;168:149–60.
Bethke W. New frontiers in sustained release. Rev Ophthalmol. 2015.
Bhagav P, Trivedi V, Shah D, Chandran S. Sustained release ocular inserts of brimonidine tartrate for better treatment in open-angle glaucoma. Drug Deliv Transl Res. 2011;1:161–74.
BioSpace. Lux Biosciences Announces Exclusive Worldwide License Agreement With National Institutes of Health (NIH) For Late Stage Ophthalmic Product. 2006. https://www.biospace.com/article/releases/lux-biosciences-announces-exclusive-worldwide-license-agreement-with-national-institutes-of-health-nih-for-late-stage-ophthalmic-product-.
Blizzard C, Desai A, Langh J, Buff N, Metzinger J, Goldstein M, Gelormini A, Driscoll A. Pharmacokinetics of OTX-TIC, a sustained release Travoprost Intracameral implant in rabbits. In: ARVO. Vancouver, BC: IOVS; 2019. p. 3777.
Bourges JL, Bloquel C, Thomas A, Froussart F, Bochot A, Azan F, Gurny R, BenEzra D, Behar-Cohen F. Intraocular implants for extended drug delivery: therapeutic applications. Adv Drug Deliv Rev. 2006;58:1182–202.
Boyer DS, Yoon YH, Belfort R, Bandello F, Maturi RK, Augustin AJ, Li X-Y, Cui H, Hashad Y, Whitcup SM. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014;121:1904–14.
Brandt JD, Sall K, DuBiner H, Benza R, Alster Y, Walker G, Semba CP, Budenz D, Day D, Flowers B, Lee S, Nguyen Q, Wirta D. Six-month intraocular pressure reduction with a topical Bimatoprost ocular insert: results of a phase II randomized controlled study. Ophthalmology. 2016;123:1685–94.
Cagini C, Caricato A, Tosi G, Pascale A, Cesari C, Fiore T. Evaluation of the efficacy and safety of the ophthalmic insert Mydriasert in patients undergoing retinal angiography. Eur J Ophthalmol. 2014;24:728–34.
Callanan DG, Jaffe GJ, Martin DF, Peasron PA, Comstock TL. Treatment of posterior uveitis with a Fluocinolone Acetonide implant: three-year clinical trial results. JAMA Ophthalmol. 2008;126:1191–201.
Calles JA, Bermúdez J, Vallés E, Allemandi D, Palma S. Polymers in ophthalmology. In: Puoci F, editor. Advanced polymers in medicine. Cham: Springer International; 2015.
Campochiaro PA, Hafiz G, Shah SM, Bloom S, Brown DM, Busquets M, Ciulla T, Feiner L, Sabates N, Billman K, Kapik B, Green K, Kane F. Sustained ocular delivery of fluocinolone acetonide by an intravitreal insert. Ophthalmology. 2010;117:1393–99.e3.
Campochiaro PA, Brown DM, Pearson A, Ciulla T, Boyer D, Holz FG, Tolentino M, Gupta A, Duarte L, Madreperla S, Gonder J, Kapik B, Billman K, Kane FE. Long-term benefit of sustained-delivery Fluocinolone Acetonide vitreous inserts for diabetic macular edema. Ophthalmology. 2011;118:626–35.e2.
Campochiaro PA, Brown DM, Pearson A, Chen S, Boyer D, Ruiz-Moreno J, Garretson B, Gupta A, Hariprasad SM, Bailey C, Reichel E, Soubrane G, Kapik B, Billman K, Kane FE, Green K. Sustained delivery Fluocinolone Acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology. 2012;119:2125–32.
Campochiaro PA, Marcus DM, Awh CC, Regillo C, Adamis AP, Bantseev V, Chiang Y, Ehrlich JS, Erickson S, Hanley WD, Horvath J, Maass KF, Singh N, Tang F, Barteselli G. The port delivery system with Ranibizumab for Neovascular age-related macular degeneration: results from the randomized phase 2 ladder clinical trial. Ophthalmology. 2019;126(8):1141–15.
Carvalho R, Ko P, Murphree A, Brito R, Morenonn J, Wahjudi P, Vargas-Dougherty M, Mendes C, Matsutani G, Manders J. The preclinical safety, toxicity and pharmacokinetics (Pk) of targeted Episcleral delivery of Topotecan (TPT), Melphalan (MEL) and its combination with dexamethasone (DEX). Investig Ophthalmol Visual Sci. 2016;57.
Conway B. Recent patents on ocular drug delivery systems. Recent Pat Drug Deliv Formul. 2008;2:1–8.
Cunha-Vaz J. The blood-ocular barriers. Surv Ophthalmol. 1979;23:279–96.
De Carvalho R, Wahjudi P, Moreno J, Mendes C, Ko P, Matsutani G. Selective and sustained episcleral delivery of brimonidine: in vivo safety, toxiciy and pharmacokinetics. Investig Ophthalmol Visual Sci. 2014;55:13.
Diestelhorst M, Krieglstein GK. The ocular tolerability of a new ophthalmic drug delivery system (NODS). Int Ophthalmol. 1994;18:1–4.
Drug Delivery Sustained Release Technology. 2017. Available from: https://www.businesswire.com/news/home/20171005005490/en/Aerie-Pharmaceuticals-Announces-Drug-Delivery-Asset-Acquisition. Accessed Oct 27, 2021.
Edelhauser HF, Rowe-Rendleman CL, Robinson MR, Dawson DG, Chader GJ, Grossniklaus HE, Rittenhouse KD, Wilson CG, Weber DA, Kuppermann BD, Csaky KG, Olsen TW, Kompella UB, Holers VM, Hageman GS, Gilger BC, Campochiaro PA, Whitcup SM, Wong WT. Ophthalmic drug delivery systems for the treatment of retinal diseases: basic research to clinical applications. Invest Ophthalmol Vis Sci. 2010;51:5403–20.
Envisia Therapeutics. Envisia Therapeutics releases interim ENV515 (Travoprost XR) phase 2 data demonstrating 11-month duration-of-action after a single dose in patients with glaucoma. 2017. https://prn.to/2xECIcW. Accessed 21 May 2019.
Extension Study for the Port Delivery System With Ranibizumab (Portal) ClinicalTrials.gov. Available from: https://clinicaltrials.gov/ct2/show/NCT03683251. Accessed Oct 27, 2021.
EyePoint. YUTIQ Prescribing Information. 2021. Available from: https://yutiq.com/downloads/YUTIQ%20Prescribing%20Information_May%202021.pdf.
EyePoint Pharmaceuticals Announces U.S. Commercial Launch of DEXYCU (dexamethasone intracoular suspensio) 9%. GlobeNewswire; 2019.
Farkouh A, Frigo P, Czejka M. Systemic side effects of eye drops: a pharmacokinetic perspective. Clin Ophthalmol. 2016;10:2433–41.
FDA. FDA Approved Drug Products. 2019. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=210331. Accessed 12 May 2019.
Freeman WR. Intravitreal Brimonidine drug delivery system (Brimonidine DDS) in patients with geographic at-rophy: a phase 2 study. In: AAO retina subspecialty Day annual meeting; 2016.
Freeman WR, Francesco B, Souied EH, Guymer RH, Garg S, Chen FK, Rich RM, Holz FG, Li Y, Lopez FJ Kerr K. Phase 2b study of Brimonidine DDS: potential novel treatment for geographic atrophy. AVRO. 2019.
Gaudana R, Ananthula HK, Parenky A, Mitra AK. Ocular drug delivery. AAPS J. 2010;12:348–60.
GB-201, GB-202 and GB-203—Glaucoma Products. n.d. https://www.graybug.vision/our-technologies-and-pipeline/#pipeline.
Ghate D, Edelhauser HF. Ocular drug delivery. Expert Opin Drug Deliv. 2006;3:275–87.
Ghate D, Edelhauser HF. Barriers to glaucoma drug delivery. J Glaucoma. 2008;17:147–56.
Graybug Vision Presents Top Line Results of Phase 1/2a ADAGIO Study at Hawaiian Eye & REtina 2019. Business Wire. 2019.
Greaves JL, Wilson CG, Birmingham AT, Richardson MC, Bentley PH. Scintigraphic studies on the corneal residence of a new ophthalmic delivery system (NODS): rate of clearance of a soluble marker in relation to duration of pharmacological action of pilocarpine. Br J Clin Pharmacol. 1992;33:603–9.
Haghjou N, Soheilian M, Abdekhodaie MJ. Sustained release intraocular drug delivery devices for treatment of uveitis. J Ophthalmic Vis Res. 2011;6:317–29.
Haller JA, Bandello F, Belfort R, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon Y-H, Jacques M-L, Jiao J, Li X-Y, Whitcup SM. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117:1134–46.e3.
Haller JA, Bandello F, Belfort R, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jiao J, Li X-Y, Whitcup SM. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion: twelve-month study results. Ophthalmology. 2011;118:2453–60.
Hermann MM, Üstündag C, Diestelhorst M. Electronic compliance monitoring of topical treatment after ophthalmic surgery. Int Ophthalmol. 2010;30:385–90.
Hill JC. Slow-release artificial tear inserts in the treatment of dry eyes in patients with rheumatoid arthritis. Br J Ophthalmol. 1989;73:151–4.
Humayun M, Santos A, Altamirano JC, Ribeiro R, Gonzalez R, de la Rosa A, Shih J, Pang C, Jiang F, Calvillo P, Huculak J, Zimmerman J, Caffey S. Implantable MicroPump for drug delivery in patients with diabetic macular edema. Transl Vis Sci Technol. 2014;3:5–5.
Iluvien Approval History. www.drugs.com/history/iluvien.html. Accessed 12 May 2019.
Iluvien Prescribing information. Alimera Sciences. alimerasciences.com/wp-content/uploads/2016/02/Prescribing-Information.pdf. Accessed 12 May 2019.
Jaffe GJ, Martin D, David C, Andrew Pearson P, Levy B, Comstock T. Fluocinolone Acetonide implant (Retisert) for noninfectious posterior uveitis: thirty-four–week results of a multicenter randomized clinical study. Ophthalmology. 2006;113:1020–7.
Jaffe GJ, Stephen Foster C, Pavesio CE, Paggiarino DA, Riedel GE. Effect of an injectable Fluocinolone Acetonide insert on recurrence rates in chronic noninfectious uveitis affecting the posterior segment: twelve-month results. Ophthalmology. 2019;126:601–10.
Jager RD, Aiello LP, Patel SC, Cunningham ET Jr. Risks of intravitreous injection: a comprehensive review. Retina. 2004;24:676–98.
Jain RA. The manufacturing techniques of various drug loaded biodegradable poly(lactide-co-glycolide) (PLGA) devices. Biomaterials. 2000;21:2475–90.
Jervis LP. A summary of recent advances in ocular inserts and implants. J Bioequiv. 2017;9:320–3.
Joseph M, Trinh HM, Cholkar K, Pal D, Mitra AK. Recent perspectives on the delivery of biologics to back of the eye. Expert Opin Drug Deliv. 2017;14:631–45.
Kearns VR, Williams RL. Drug delivery systems for the eye. Expert Rev Med Devices. 2009;6:277–90.
Kedhar SR, Jabs DA. Cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Herpes. 2007;14:66–71.
Kempen JH, Altaweel MM, Holbrook JT, Jabs DA, Louis TA, Sugar EA, Thorne JE. Randomized comparison of systemic anti-inflammatory therapy versus Fluocinolone Acetonide implant for intermediate, posterior, and Panuveitis: the multicenter uveitis steroid treatment trial. Ophthalmology. 2011;118:1916–26.
Khurana RN, Appa SN, McCannel CA, Elman MJ, Wittenberg SE, Parks DJ, Ahmad S, Yeh S. Dexamethasone implant anterior chamber migration: risk factors, complications, and management strategies. Ophthalmology. 2014;121:67–71.
Kiernan DF, Mieler WF. The use of intraocular corticosteroids. Expert Opin Pharmacother. 2009;10:2511–25.
Kimura H, Ogura Y. Biodegradable polymers for ocular drug delivery. Ophthalmologica. 2001;215:143–55.
Kumari A, Sharma P, Garg V, Garg G. Ocular inserts—advancement in therapy of eye diseases. J Adv Pharm Technol Res. 2010;1:291–6.
Kuno N, Fujii S. Biodegradable intraocular therapies for retinal disorders. Drugs Aging. 2010;27:117–34.
Kuppermann BD, Blumenkranz MS, Haller JA, Williams GA, Weinberg DV, Chou C, Whitcup SM, Dexamethasone DDS Phase II Study Group. Randomized controlled study of an Intravitreous dexamethasone drug delivery system in patients with persistent macular edema. JAMA Ophthalmol. 2007;125:309–17.
Lee DJ. Intraocular implants for the treatment of autoimmune uveitis. J Funct Biomater. 2015;6:650–66.
Lee TW, Robinson JR. Drug delivery to the posterior segment of the eye: some insights on the penetration pathways after subconjunctival injection. J Ocul Pharmacol Ther. 2001;17:565–72.
Lee SS, Robinson MR. Novel drug delivery systems for retinal diseases. Ophthalmic Res. 2009;41:124–35.
Lee Y-C, Simamora P, Pinsuwan S, Yalkowsky SH. Review on the systemic delivery of insulin via the ocular route. Int J Pharm. 2002;233:1–18.
Lee SS, Hughes P, Ross AD, Robinson MR. Biodegradable implants for sustained drug release in the eye. Pharm Res. 2010;27:2043–53.
Lee SS, Hughes P, Ross AD, Robinson MR. Advances in biodegradable ocular drug delivery systems. In: Kompella UB, Edelhauser HF, editors. Drug product development for the back of the eye. Boston, MA: Springer US; 2011.
Lewis RA, Christie WC, Day DG, Randy Craven E, Walters T, Bejanian M, Lee SS, Goodkin ML, Zhang J, Whitcup SM, Robinson MR, Aung T, Beck AD, Christie WC, Coote M, Crane CJ, Randy Craven E, Crichton A, Day DG, Jane Durcan F, Flynn WJ, Gagné S, Goldberg DF, Delan J, Starck Johnson C, Kurtz S, Lewis RA, Mansberger SL, Perera SA, Rotberg MH, Saltzmann RM, Schenker HI, Tepedino ME, Yap-Veloso MIR, Uy HS, Walters TR. Bimatoprost sustained-release implants for glaucoma therapy: 6-month results from a phase I/II clinical trial. Am J Ophthalmol. 2017;175:137–47.
Liechty WB, Kryscio DR, Slaughter BV, Peppas NA. Polymers for drug delivery systems. Annu Rev Chem Biomol Eng. 2010;1:149–73.
Lim J, Hung D, Fung A, Wieland M, Wong V. A phase 1 study evaluating the safety and evidence of efficacy of IBI-20089, a triamcinolone intravi-treal injection formulated with the Verisome ™ drug delivery technology, in patients with cystoid macular edema. Invest Ophthalmol Vis Sci. 2010;51.
Lima LH, Farah ME, Gum G, Ko P, de Carvalho RAP. Sustained and targeted episcleral delivery of celecoxib in a rabbit model of retinal and choroidal neovascularization. Int J Retina Vitreous. 2018;4:31.
Lo R, Li P-Y, Saati S, Agrawal RN, Humayun MS, Meng E. A passive MEMS drug delivery pump for treatment of ocular diseases. Biomed Microdevices. 2009;11:959.
Macha S, Mitra AK. Ocular disposition of ganciclovir and its monoester prodrugs following intravitreal administration using microdialysis. Drug Metab Dispos. 2002;30:670–5.
Mealy JE, Fedorchak MV, Little SR. In vitro characterization of a controlled-release ocular insert for delivery of brimonidine tartrate. Acta Biomater. 2014;10:87–93.
Miller RA, Brady JM, Cutright DE. Degradation rates of oral resorbable implants (polylactates and polyglycolates): rate modification with changes in PLA/PGA copolymer ratios. J Biomed Mater Res. 1977;11:711–9.
Mohammad DA, Sweet BV, Elner SG. Retisert: is the new advance in treatment of uveitis a good one? Ann Pharmacother. 2007;41:449–55.
Musch DC, Martin DF, Gordon JF, Davis MD, Kuppermann BD. Treatment of cytomegalovirus retinitis with a sustained-release ganciclovir implant. N Engl J Med. 1997;337:83–90.
Nancy M. Holekamp, Peter A. Campochiaro, Margaret Chang, Daniel Miller, Dante Pieramici, Anthony P. Adamis, Christopher Brittain, Erica Evans, Derrick Kaufman, Katie F. Maass, Shienal Patel, Shrirang Ranade, Natasha Singh, Giulio Barteselli, Carl Regillo, Archway Randomized Phase 3 Trial of the Port Delivery System With Ranibizumab for Neovascular Age-Related Macular Degeneration, Ophthalmology. 2021.
Niegvesky G, Butrus S, Abifarah H, Lee Y, Yalkowsky S. Ocular Gelfoam disc-applicator for pupillary dilation in humans. J Ocul Pharmacol Ther. 2000;16:311–5.
Nordmann J-P, Baudouin C, Renard J-P, Denis P, Lafuma A, Laurendeau C, Jeanbat V, Berdeaux G. Measurement of treatment compliance using a medical device for glaucoma patients associated with intraocular pressure control: a survey. Clin Ophthalmol. 2010;4:731.
Novel anti-VEGF for wet AMD meets safety, tolerability endpoint. Retina/vitreous. Healio; 2019.
NT-502 ECT. Neurotech Press Release; 2016.
Ocular Therapeutix Announces Dosing of First Patient in Phase 1 Clinical Trial for the Treatment of Wet AMD. Eyewire. 2019.
Ocular Therapeutix™ Announces Treatment of First Patient in Phase 1 Clinical Trial of OTX-TIC (travoprost intracameral implant) for the Treatment of Glaucoma and Ocular Hypertension. BioSpace. 2018.
Ozurdex Approval History. Development history and FDA approval process for Ozurdex. https://www.drugs.com/history/ozurdex.html.
Park JB, Lakes RS. Biomaterials : an introduction. New York: Springer; 2007.
Patel A, Cholkar K, Agrahari V, Mitra AK. Ocular drug delivery systems: an overview. World J Pharmacol. 2013;2:47–64.
Pearce W, Hsu J, Yeh S. Advances in drug delivery to the posterior segment. Curr Opin Ophthalmol. 2015;26:233–9.
Pearson PA, Comstock TL, Ip M, Callanan D, Morse LS, Ashton P, Levy B, Mann ES, Eliott D. Fluocinolone Acetonide intravitreal implant for diabetic macular edema: a 3-year multicenter, randomized, controlled clinical trial. Ophthalmology. 2011;118:1580–7.
Pijls RT, Sonderkamp T, Daube GW, Krebber R, Hanssen HH, Nuijts RM, Koole LH. Studies on a new device for drug delivery to the eye. Eur J Pharm Biopharm. 2005;59:283–8.
Pijls RT, Cruysberg LPJ, Nuijts RMMA, Dias AA, Koole LH. Capacity and tolerance of a new device for ocular drug delivery. Int J Pharm. 2007;341:152–61.
PolyActiva commences its first phase I clinical trial with potential to improve daily lives of millions of glaucoma patients. Business Wire; 2018.
Pontes de Carvalho RA, Krausse ML, Murphree AL, Schmitt EE, Campochiaro PA, Maumenee IH. Delivery from episcleral exoplants. Invest Ophthalmol Vis Sci. 2006;47:4532–9.
Psivida Corp Annual Report. 2016. http://investors.psivida.com/static-files/020cf090-42dd-467b-961c-52ded762c3d9.
Ravindran VK, Repala S, Subadhra S, Appapurapu AK. Chick chorioallantoic membrane model for in ovo evaluation of timolol maleate–brimonidine tartrate ocular inserts. Drug Deliv. 2014;21:307–14.
Robinson MR, Whitcup SM. Pharmacologic and clinical profile of dexamethasone intravitreal implant. Expert Rev Clin Pharmacol. 2012;5:629–47.
Rofagha S, Prechanond T, Stewart JM. Late spontaneous dissociation of a Fluocinolone Acetonide implant (Retisert). Ocul Immunol Inflamm. 2013;21:77–8.
Saati S, Lo R, Li P-Y, Meng E, Varma R, Humayun MS. Mini drug pump for ophthalmic use. Curr Eye Res. 2010;35:192–201.
Saenz-de-Viteri M, Fernandez-Robredo P, de Nova E, Bonet-Farriol E, Sabater AL, Zarranz-Ventura J, Caire J, Sadaba LM, Salinas-Alaman A, Garcia-Layana A. Comparative study measuring the dilatory effect of a mydriatic device (Mydriasert((R))) versus topical drops. Int J Ophthalmol. 2013;6:801–4.
Safety and preliminary efficacy study of V404 PDS in Uveitis. n.d. Available from: https://clinicaltrials.gov/ct2/show/NCT02125266.
Salyani A, Birt C. Evaluation of an eye drop guide to aid self-administration by patients experienced with topical use of glaucoma medication. Can J Ophthalmol. 2005;40:170–4.
Sandahl M, Melton D, Tully J, Yang M, Garcia A, Trevino L, Williams S. Evaluation of reproducibility and uniformity of PRINT implant manufacturing. In: Association for Research in Vision and Ophthalmology annual meeting. Honolulu, HI; 2018.
Sangwan VS, Andrew Pearson P, Paul H, Comstock TL. Use of the Fluocinolone Acetonide intravitreal implant for the treatment of noninfectious posterior uveitis: 3-year results of a randomized clinical trial in a predominantly Asian population. Ophthalmol Ther. 2015;4:1–19.
Seah SKL, Husain R, Gazzard G, Lim MCC, Hoh S-T, Oen FTS, Aung T. Use of Surodex in Phacotrabeculectomy surgery. Am J Ophthalmol. 2005;139:927–8.
Seal JR, Robinson MR, Burke J, Bejanian M, Coote M, Attar M. Intracameral sustained-release Bimatoprost implant delivers Bimatoprost to target tissues with reduced drug exposure to off-target tissues. J Ocul Pharmacol Ther. 2019;35:50–7.
Silva-Cunha A, Fialho SL, Naud M-C, Behar-Cohen F. Poly-ε-caprolactone intravitreous devices: an in vivo study. Invest Ophthalmol Vis Sci. 2009;50:2312–8.
Stephenson M. Can sustained release deliver the goods?. Rev Ophthalmol. 2018.
Streilein JW. Ocular immune privilege: the eye takes a dim but practical view of immunity and inflammation. J Leukoc Biol. 2003;74:179–85.
SurModics. Durable drug delivery coatings. 2013. http://www.surmodics.com/assets/uploads/documents/SurModics_Durable_Drug_Delivery_0513.pdf.
Swati M, Oshin M. Recent advancements in biodegradable ocular implants. Curr Drug Deliv. 2018;15:144–54.
Tan DTH, Chee S-P, Lim L, Lim ASM. Randomized clinical trial of a new dexamethasone delivery system (surodex) for treatment of post-cataract surgery inflammation. Ophthalmology. 1999;106:223–31.
Varma D. Sustained release drug delivery: closer than you think; 2018.
Weintraub A. Lux bio resurfaces with defined path for pill for rare eye disease. In: Xconomy; 2012.
Whitcup SM, Azar DT. Pharmacologic therapy of ocular disease. Berlin, Heidelberg, New York: Springer; 2017.
Williams GA, Haller JA, Kuppermann BD, Blumenkranz MS, Weinberg DV, Chou C, Whitcup SM. Dexamethasone posterior-segment drug delivery system in the treatment of macular edema resulting from uveitis or Irvine-Gass syndrome. Am J Ophthalmol. 2009;147:1048–54.e2.
Yasin MN, Svirskis D, Seyfoddin A, Rupenthal ID. Implants for drug delivery to the posterior segment of the eye: a focus on stimuli-responsive and tunable release systems. J Control Release. 2014;196:208–21.
Yasukawa T, Ogura Y, Kimura H, Sakurai E, Tabata Y. Drug delivery from ocular implants. Expert Opin Drug Deliv. 2006;3:261–73.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 American Association of Pharmaceutical Scientists
About this chapter
Cite this chapter
Lee, S., Romoda, L., Robinson, M. (2021). Implantable Devices to Treat Ophthalmic Conditions: Drug Delivery Systems. In: Neervannan, S., Kompella, U.B. (eds) Ophthalmic Product Development. AAPS Advances in the Pharmaceutical Sciences Series, vol 37. Springer, Cham. https://doi.org/10.1007/978-3-030-76367-1_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-76367-1_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-76366-4
Online ISBN: 978-3-030-76367-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)