Abstract
This chapter reviews the more than 100 meta-analyses and systematic reviews of relations between religion/spirituality (R/S) and health that have been published in refereed journals, a far larger number than is generally recognized. The 118 published reviews identified by 2017 were categorized as quantitative meta-analyses (n = 33), qualitative meta-syntheses (n = 7), meta-analyses of case studies (n = 1), or simple systematic reviews (n = 77). They addressed a wide range of substantive topics relevant to every major public health subfield, and incorporated a mean of 33.5 studies per review. Collectively authored by more than 200 distinct individuals, the reviews were published in 83 different journals, 20 in the category of public health. Multiple reviews were published by 14 journals, a majority possessing impact factors above 2.0. Reviewing empirical studies of R/S-health is clearly a very broad-based enterprise not limited to a few individuals or journals. Collectively, the reviews greatly strengthen the case, based on Hill’s criteria, that R/S exerts a causative influence on health. The case for causal influence may now be compelling, and in most cases R/S involvement is associated with better health, although negative associations also exist. Further investigation is warranted to explore the possibility that R/S is a “fundamental cause” of health that maintains an association even when intervening mediating pathways change. This possibility is consistent with the dynamic understandings of R/S presented elsewhere in this volume.
This chapter is one of thirteen reviews in this volume providing a public health perspective on the empirical evidence relating R/S to physical and mental health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Public health
- Spirituality
- Religion
- Systematic review
- Meta-analysis
- Causality
- Hill’s criteria
- Fundamental cause
- Physical health
- Mental health
When our research group at Berkeley ’s School of Public Health embarked on the series of empirical reviews that culminated in Part I of this volume, we knew from the recent Handbook by Koenig and his colleagues (2012) that there existed more than 3000 published studies of religion/spirituality (R/S) and health. We knew that the Handbook had systematically reviewed many of those studies in a way that was highly useful but had emphasized a clinical rather than a public health perspective. We also knew that there had been meta-analyses of a handful of other R/S-health topics, such as R/S engagement and longevity . As a crucial reference point for our own review, we wanted to identify all relevant pre-existing systematic reviews of relations between R/S factors and health variables. Therefore we embarked on searches of PubMed, PsycINFO, and other databases, expecting that we might find perhaps one or even two dozen published systematic reviews and meta-analyses of R/S-health relations.
We were astonished when we identified more than 100 refereed systematic reviews published about relations between religion/spirituality and one or more health-relevant variables. Not all of these systematic reviews were well-done or offered useful insights. But many were of high quality and had been published in journals with high impact factors. Many of these earlier reviews became useful building blocks that we cited in our own public health oriented reviews that appear in the preceding chapters in Part I of this volume. Along with the the two editions of Koenig and colleagues’ (2001, 2012) Handbook, these reviews and meta-analyses enabled us to leverage our resources and cover a much broader and more comprehensive set of public health subtopics than would otherwise have been possible. As a result, we were able to assemble public health perspectives on evidence for R/S-health relations from the perspectives of virtually every major subfield within public health (see chapter “Reviewing Religion/Spirituality Evidence from a Public Health Perspective: Introduction” this volume).
Yet this massive body of systematic reviews also represents an important phenomenon in itself, a valuable resource for many researchers , practitioners, and academic educators interested in the relevance of religion/spirituality to public health. We therefore analysed the systematic reviews themselves as a body of scientific literature.
Our goal in the present chapter is to enable readers to use these 100+ systematic reviews efficiently, and understand their overall implications and potential for research, teaching, and practice. Accordingly, the next section tabulates and offers various overview statistics and perspectives about the reviews. The third section suggests some substantimve implications for evaluating the causative aspect of R/S-health relations. The final section suggests needed future directions.
1 Overview of Systematic Reviews and Meta-Analyses
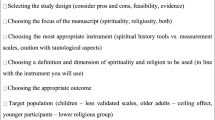
In December 2013 our Berkeley group conducted searches for reviews in refereed journals through PubMed as well as PsycINFO, Sociological Abstracts and seven other EBSCO databases,Footnote 1 without any restriction on date of publication. To meet the inclusion criterion of being systematic, each review was required to specify its search strategy (e.g., which databases) and enumerate the precise studies included in its final analyses. Our search terms specified that the title and/or abstract must refer to religion/spirituality.Footnote 2 We identified 599 unique records that were combined with 30 records in our files to yield 629 total records, reduced to 144 after inspection of abstracts, and to 128 after full-text retrieval and inspection.
The 128 retrieved systematic reviews were then divided into (i) reviews that focused on the association between R/S and a directly health-related variable such as health behaviors , social support , or mortality (k = 77); (ii) reviews of R/S and a variable such as education or personality , that is arguably but indirectly related to health (k = 16, e,g, Davis et al. 2013; Saroglou 2010); and (iii) reviews that were focused on methodological aspects of R/S-health relations, such as the frequency of R/S variables in studies published in top journals in a particular field, or reviews of measurement instruments (k = 35, e.g., Larson et al. 1986; Monod et al. 2011). In what follows, our primary focus is the first category concerning empirical findings about R/S-health relations.
Table 1 displays citation information for the 2013 list of 77 systematic reviews of R/S and directly health-related variables. The table also includes information about 41 additional systematic reviews identified subsequent to our original analyses, mostly published in 2014 or later (indicated by table footnote d). This combined (2017) total is 118 systematic reviews, meta-analyses, or qualitative meta-syntheses of relations between R/S and health-relevant variables.
Of the 2017 list of 118 reviews of direct R/S-health relations, 33 (28%) were quantitative meta-analyses, seven (6%) were qualitative meta-syntheses, one (1%) was a meta-analysis of case-studies, and 77 (65%) attempted neither qualitative nor quantitative aggregation, and might thus be called simple systematic reviews (SSRs). These reviews were published in a total of 83 journals, with multiple reviews appearing in 14 journals, a majority possessing impact factors above 2.0 (see Table 2, top). Twenty of the 118 (17%) appeared in journals classified as public health (see Table 2, bottom). The mean number of publications examined in the 118 systematic reviews was 33.5, and was somewhat larger among meta-analyses (43.7) and somewhat smaller among qualitative meta-syntheses (13.6). Similar patterns were apparent in 2013 (see Fig. 1). Already in 2013, a total of 223 distinct individuals were listed as authors, with only 18 individuals serving as author on multiple reviews, only one of whom authored or coauthored more than three reviews.Footnote 3
The reviews addressed a wide range of substantive topics, as shown in the headers in Table 1. Of 118 empirical reviews published by 2017, at least one offered evidence relevant to each major public health subfield (i.e., earlier chapters in Part I of this volume, as indicated in footnotes e through p in Table 1). Many reviews are relevant to more than one public health subfield. Clearly, the process of systematically reviewing empirical studies of R/S-health relations is a very broad-based enterprise that is not limited to a few individuals, a few journals, or to the two editions of the Handbook.
Quality and Usefulness of Reviews
Many reviews have appeared in high impact journals and reflect those journals’ high standards. Yet our group can also attest that the reviews listed in Table 1 varied considerably in their usefulness for preparing this volume. Some reviews are outdated, others identified only a very limited pool of relevant studies (e.g., #3, #47, #82), used poor methods, or contributed little new information beyond identification of studies. Every research literature is affected by limitations of various kinds. Conditions that affect the quality of R/S-health reviews may include the complexity and interdisciplinary nature of the R/S-health topic, its capacity to galvanize rank-and-file enthusiasm despite its relative dearth of a stable funding base, and its relatively recent emergence as an organized literature. In view of such conditions, it is not surprising that a number of limitations exist. And despite this variety of adverse conditions, many reviews are solid, and much can be learned from them.
2 Does Religion/Spirituality Cause Health?: Implications of Systematic Reviews
What can we conclude from the findings embedded in these 100-plus reviews? Do the available meta-analyses and systematic reviews “prove” that religious and/or spiritual involvement fosters health?
Arguably most fundamental is the question of whether R/S engagement with religion/spirituality by an individual can have a causal effect on that same person’s health, through any pathway. For example, according to the “generic” model that is presented in this volume’s chapter entitled “Model of Individual Health Effects from Religion/Spirituality: Supporting Evidence”, engagement with R/S might plausibly benefit physical health through pathways that include improved health behaviors , heightened social support , enhanced mental health , and greater ability to draw strength from religious/spiritual methods of coping with stress. Many reviews and meta-analyses present evidence relevant to the primary question of whether R/S causally affects health through any pathway (e.g., Table 1, reviews #7, #17, #28, #30, #31).
Secondary causative questions of interest concern whether R/S engagement affects health through specific pathways or groups of pathways. For example, one may ask whether R/S causally affects health through enhanced social support. One may also ask whether R/S causally affects health through any pathways apart from enhanced social support – which would imply that benefits from R/S are not “just” social support. In popular discourse, such questions are commonly confused with the more fundamental causative question of whether religious/spiritual involvement may affect health through any pathway (Oman and Thoresen 2002). Happily, some meta-analyses do also present evidence relevant to specific secondary questions. For example, in 2009, Chida et al. (Table 2, review #28) reported that among 26 mortality studies in healthy populations that controlled for social support , R/S engagement predicted a statistically significant overall reduction of 16% in mortality risk after controls (hazard ration [HR] = 0.84, 95%CI = 0.78–0.91). Such findings suggest that R/S effects on mortality are not mediated solely by social support. Similarly, some systematic reviews have separately tabulated, wherever possible, each study’s estimates from not only a “mediated model” that adjusted for potentially confounding factors, but also from an “independent model” that adjusted for confounders plus “established risk factors” that include health behaviors , social support and mental health (i.e., depression ) (p. 39 of Powell et al., review #31 in Table 1). Such studies do offer support for influence of R/S on health through all major generic pathways (for a fuller review of major pathways, see chapter “Model of Individual Health Effects from Religion/Spirituality: Supporting Evidence”, this volume).
Inferring Causality Without Randomization
Rigorously gauging causal effects, however, remains a difficult task, because a person’s religious/spiritual engagemen is largely incapable of being randomized , and randomized studies are often the easiest means of ruling out the possibility that an observed relation is an artifact of unobserved confounding factors . Even if it was ethical , a randomized study of religious engagement and health would likely pose intractible challenges for recruitment and adherence . But tobacco smoking and many other health factors also cannot be randomized, yet have come to be considered as causal . For such non-randomizable variables, how can causality be inferred?
Jeff Levin’s (1994) analysis of evidence for religion-health causality was published more than 20 years ago, but remains a valuable introduction to the issue. As he explains, British epidemiologist Austin Bradford Hill (1965) developed what have come to be known as “Hill’s criteria for causality” (Rothman and Greenland 2005). Since Hill viewed none of these nine “criteria” as either necessary or sufficient, they are perhaps better characterized as perspectives or guidelines for evaluating causality. These nine guidelines emerged from Hill’s pioneering work to infer the causal effects of smoking. Commonly studied by epidemiology students, these guidelines are often summarized as consistency, coherence, strength, temporality, plausibility, specificity, biological gradient , experiment, and analogy.
Based on the much smaller body of studies available in the early 1990s, Levin (1994) evaluated evidence for R/S-health causality from each of these perspectives. While none of the nine perspectives undermined arguments for causality, several possessed little relevant evidence, and Levin (1994, p. 1480) concluded that
the question, “Is it causal?‘, can be answered with a “maybe”…. examining the evidence in light of Hill’s guidelines is inconclusive, but promising. Judging this literature in terms of consistency, plausibility, and analogy, the answer is yes. In terms of coherence, the answer is probably yes, but one cannot be certain. In terms of temporality and biological gradient , there is insufficient evidence, but recent gerontological findings may change this to a yes. In terms of strength and experiment, there is insufficient evidence. Finally, specificity does not seem to be applicable.
Now, more than 20 years later, after the publication of at least 2000 additional empirical studies and many dozens of meta-analyses and systematic reviews, is the answer still “maybe”? Pondering this question, we reread Levin’s paper, and noticed that the evidence base in many respects had expanded dramatically . What in 1994 could be addressed through only a small handfull or a single study, can in 2017 in many cases be addressed through one or more meta-analyses or systematic reviews. Table 3 displays various ways that the case for causality has been strengthened, in many cases dramatically. Levin viewed the evidence for consistency as already strong, and for ccoherence as “probably yes” (p. 1480) – both can now be backed with diverse meta-analyses . Evidence for strength was viewed by Levin as “inconclusive,” but clinically consequential relations are now backed by meta-analyses. Evidence for temporality was “insufficient” but now includes meta-analyses of topics such as mortality , as well as unrefereed yet high quality systematic reviews in the Handbook (Koenig et al. 2012).
From the standpoint of the Hill guidelines, the case for a causative relation between religion/spirituality and health has been enormously strengthened. On balance, we believe the case is compelling. Can anyone sincerely maintain that religion and spirituality are entirely non-causal epiphenomenal byproducts of other variables, and that all of the R/S-health relationships documented in Table 3, and in other systematic reviews listed in Table 1, are purely due to confounding?
Even as Hill-based assessments via systematic reviews are pointing increasingly strongly and perhaps compellingly toward causal effects, complementary causative evidence is also emerging from increasingly sophisticated individual studies. More specifically, innovative statistical methods now permit better estimates of robustness of certain estimates against unmeasured confounding (e.g., VanderWeele et al. 2016). A pioneering study that used such methods reported evidence for bidirectional effects between religious service attendance and depression that were of approximately equal magnitude. The possibility of unmeasured confounding cannot be completely analytically eliminated in any nonrandomized design. But the investigators were able to infer that “for an unmeasured confounder to fully explain away the association of service attendance with subsequent depression, it would have to both increase the likelihood of service attendance and decrease the likelihood of depression by 2.1-fold, above and beyond the measured covariates, which may not be likely” (Li et al. 2016, pp. 881–882).
3 Future Directions
Even if the case for causative effects is regarded as compelling, many closely connected questions remain to be addressed. Perhaps most important, we believe the focus of attention should shift – and for many researchers has already shifted – from whether R/S exerts causative effects on health, to understanding when such effects are positive and favorable to health (apparently the most common effect), when they may be negative, and when causative influences are small or tend to cancel each other out. Such questions are important for designing optimal public health programs and interventions , activities that are already the focus of multiple systematic reviews (e.g., Table 1, reviews #54–#59, #61–#73).
Further insight may also be obtained by probing the secondary questions noted earlier about whether R/S-health relations are independent from or occur through particular subsets of mediating pathways. Support for major generic pathways such as R/S coping, enhanced mental health , and improved health behaviors , is now documented in systematic reviews and meta-analyses (e.g., reviews #14, #88, and Handbook, pp. 753–780, as analyzed in Table 1; for fuller discussion see also chapter “Model of Individual Health Effects from Religion/Spirituality: Supporting Evidence”, this volume).
A larger and more ambitious question is whether religion/spirituality might be a “fundamental cause ” of health in the sense that they tend to “maintain an association with [health or] disease even when intervening mechanisms change” (Link and Phelan 1995, p. 80), a speculation offered nearly two decades ago by Hummer et al. (1999). The dynamic and evolving model of R/S that undergirds several chapters in this volume is compatible with such a view of R/S-health relations, and perhaps even required to accommodate the smaller but non-negligible presence of negative R/S-health associations in some circumstances (see chapter “Social and Community-Level Factors in Health Effects from Religion/Spirituality”, and Question 6 in chapter on “Questions on Assessing the Evidence Linking Religion/Spirituality to Health,” this volume).
Such a dynamic and evolving model, which assumes that religious traditions adapt and learn, need not imply uniformly positive learning-induced changes over time within each R/S tradition and its offshoots. In fact, in individual human development, U-shaped developmental trajectories “appear to be normative across developmental domains including language, cognition, and physical abilities and may be a general property of dynamic systems…. [and may] signal periods of increased attention to new elements… and mark transitions to more complex integrations [and] newer levels of competence and complexity ” (Nucci and Turiel 2009, p. 156). Religious/spiritual communities worldwide face the challenge of learning how to integrate essential R/S commitments and insights with the opportunities and disruptions of modern technology. Viewed from a dynamical systems perspective, inconsistencies in how religion/spirituality relate to health might reflect the irregularities inherent in how R/S-based behavior – like other human behavior – is “softly assembled… as a function of both… history and the current contexts” (Gershkoff-Stowe and Thelen 2004, p. 16).
By strengthening the case for causative R/S-health relations, the reviews examined in this chapter open up new questions and new theoretical and practical vistas. We believe that future work on R/S health should focus on both consolidation and expansion. Virtually every systematic review in Table 1 can offer some helpful information for future work, although the depth of the yielded insight varies greatly. As in every field, investigators must also use discernment to extract from each review the information that is based on solid methodological foundations. For many topics that are addressed by existing reviews, there is much scope for improved follow-up reviews that employ greater rigor, offer better insight into underlying patterns and processes, or offer meta-analytically aggregated estimates. Future work – individual studies as well as reviews, and by students as well as by senior researchers – should also attend to investigating and building theoretically cogent accounts of moderating factors that predict when R/S-health relations are stronger and more beneficial, when they are weaker or even negative, and how best to collaborate with R/S communities and enhance the health of their members. Up to now, the bulk of R/S-health work has been in individually oriented fields such as medicine and psycholog y. With its special concern for community-level perspectives and processes, public health can make an enormous contribution, and perhaps orchestrate increasingly sophisticated interdisciplinary collaboration to investigate religion, spirituality , and health.
Notes
- 1.
The searched EBSCO databases focused primarily on social science: EconLit 1969 – current, Environmental Sciences and Pollution Management 1967 – current, ERIC 1966 – current, International Bibliography of the Social Sciences 1951 – current, PILOTS: Published International Literature On Traumatic Stress 1871 – current, PsycINFO 1806-current, Social Services Abstracts 1979 – current, Sociological Abstracts 1952 – current, Worldwide Political Science Abstracts 1975 – current.
- 2.
Strings for R/S specified “relig*,” “spiritu*,” or a term for a specific tradition such as “Christ*,” “Islam*,” “Buddhi*”; Strings for review specified “systematic* review*,” “meta-analy*,” or “meta-s*” (for meta-synthesis).
- 3.
Authors of multiple reviews in the 2013 list were Michael E. McCullough (5 reviews); Harold G. Koenig, Kenneth I. Pargament, and Everett L. Worthington (3 each); Hana Ayele, Edzard Ernst, David R. Hodge, Violet E. Horvath, David B. Larson, Hung-Ru Lin, Thomas Mulligan, Lynda H. Powell, Lynn Rew, Timothy B. Smith, Melinda A. Stanley, Carl E. Thoresen, Joel Y. Wong, and Jerf W. K. Yeung (2 each).
References
Davis, D. E., Worthington, E. L., Jr., Hook, J. N., & Hill, P. C. (2013). Research on religion/spirituality and forgiveness: A meta-analytic review. Psychology of Religion and Spirituality, 5(4), 233–241. https://doi.org/10.1037/a0033637.
Gershkoff-Stowe, L., & Thelen, E. (2004). U-shaped changes in behavior: A dynamic systems perspective. Journal of Cognition and Development, 5(1), 11–36. https://doi.org/10.1207/s15327647jcd0501_2
Hill, A. B. (1965). The environment and disease: Association or causation? Proceedings of the Royal Society of Medicine, 58, 1217–1219.
Hummer, R. A., Rogers, R. G., Nam, C. B., & Ellison, C. G. (1999). Religious involvement and U.S. adult mortality. Demography, 36(2), 273–285. https://doi.org/10.2307/2648114.
Koenig, H. G., McCullough, M. E., & Larson, D. B. (2001). Handbook of religion and health. New York: Oxford University Press.
Koenig, H. G., King, D. E., & Carson, V. B. (2012). Handbook of religion and health (2nd ed.). Oxford/New York: Oxford University Press.
Larson, D. B., Pattison, E. M., Blazer, D. G., Omran, A. R., & Kaplan, B. H. (1986). Systematic analysis of research on religious variables in four major psychiatric journals, 1978-1982. American Journal of Psychiatry, 143(3), 329–334. https://doi.org/10.1176/ajp.143.3.32
Levin, J. S. (1994). Religion and health: Is there an association, is it valid, and is it causal? Social Science and Medicine, 38(11), 1475–1482. https://doi.org/10.1016/0277-9536(94)90109-0.
Li, S., Okereke, O. I., Chang, S.-C., Kawachi, I., & VanderWeele, T. J. (2016). Religious service attendance and lower depression among women—A prospective cohort study. Annals of Behavioral Medicine, 50(6), 876–884. https://doi.org/10.1007/s12160-016-9813-9.
Link, B. G., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 35(Supp), 80–94. https://doi.org/10.1177/0022146510383498.
Lucchetti, G., Lucchetti, A. L. G., & Koenig, H. G. (2011). Impact of spirituality/religiosity on mortality: Comparison with other health interventions. Explore, 7(4), 234–238. https://doi.org/10.1016/j.explore.2011.04.005.
Masters, K. S., Spielmans, G. I., & Goodson, J. T. (2006). Are there demonstrable effects of distant intercessory prayer? A meta-analytic review. Annals of Behavioral Medicine, 32(1), 21–26.
McCullough, M. E., Hoyt, W. T., & Larson, D. B. (2001). Small, robust, and important: Reply to Sloan and Bagiella (2001). Health Psychology, 20(3), 228–229. https://doi.org/10.1037/h0092533
Monod, S., Brennan, M., Rochat, E., Martin, E., Rochat, S., & Bula, C. J. (2011). Instruments measuring spirituality in clinical research: A systematic review. Journal of General Internal Medicine, 26(11), 1345–1357. https://doi.org/10.1007/s11606-011-1769-7.
Nucci, L. P., & Turiel, E. (2009). Capturing the complexity of moral development and education. Mind, Brain, and Education, 3(3), 151–159. https://doi.org/10.1111/j.1751-228X.2009.01065.x
Oman, D., & Thoresen, C. E. (2002). “Does religion cause health?” Differing interpretations and diverse meanings. Journal of Health Psychology, 7(4), 365–380. https://doi.org/10.1177/1359105302007004326.
Rothman, K. J., & Greenland, S. (2005). Hill’s criteria for causality. In P. Armitage & T. Colton (Eds.), Encyclopedia of biostatistics (Vol. 4, 2nd ed.). Chichester: Wiley. https://doi.org/10.1002/0470011815.b2a03072
Saroglou, V. (2010). Religiousness as a cultural adaptation of basic traits: A five-factor model perspective. Personality and Social Psychology Review, 14(1), 108–125. https://doi.org/10.1177/1088868309352322
Shaw, S. A., & El-Bassel, N. (2014). The influence of religion on sexual HIV risk. AIDS and Behavior, 18(8), 1569–1594. https://doi.org/10.1007/s10461-014-0714-2
VanderWeele, T. J., Jackson, J. W., & Li, S. (2016). Causal inference and longitudinal data: A case study of religion and mental health. Social Psychiatry and Psychiatric Epidemiology, 51(11), 1457–1466. https://doi.org/10.1007/s00127-016-1281-9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Oman, D., Syme, S.L. (2018). Weighing the Evidence: What Is Revealed by 100+ Meta-Analyses and Systematic Reviews of Religion/Spirituality and Health?. In: Oman, D. (eds) Why Religion and Spirituality Matter for Public Health. Religion, Spirituality and Health: A Social Scientific Approach, vol 2. Springer, Cham. https://doi.org/10.1007/978-3-319-73966-3_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-73966-3_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-73965-6
Online ISBN: 978-3-319-73966-3
eBook Packages: Social SciencesSocial Sciences (R0)