Abstract
Objective: We developed a new minimally invasive method for intracranial pressure monitoring (ICPMI). The objective of this project is to verify the similarities between the ICPMI and the invasive method (ICPInv), for different components of the intracranial pressure signal—namely, the mean value (trend) as well as its pulsatile component.
Materials and methods: A 9 kg anesthetized pig was used for simultaneous ICP monitoring with both methods. ICP was increased by performing ten infusions of 6 ml 0.9% saline into the spinal subarachnoid space, using a catheter implanted in the lumbar region. For correlation analysis, the signals were decomposed into two components—trend and pulsatile signals. Pearson correlation coefficient was calculated between ICPInv and ICPMI.
Results: During the infusions, the correlation between the pulsatile components of the signals was above 0.5 for most of the time. The signal trends showed a good agreement (correlation above 0.5) for most of the time during infusions.
Conclusions: The ICPMI signal trends showed a good linear agreement with the signal obtained invasively. Based on the waveform analysis of the pulsatile component of ICP, our results indicate the possibility of using the minimally invasive method for assessing the neuroclinical state of the patient.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
Intracranial pressure (ICP) is a relevant parameter for the management of many neuropathologies [1]. Current procedures to access ICP are invasive and subject to risks of brain damage and infections. Increased ICP is commonly seen is traumatic brain injury, where the need to know this parameter overcomes the risks associated with its assessment. The possibility to evaluate ICP non-invasively would be valuable in several brain disorders, as it could lead to a better management of the patient in a broader variety of clinical conditions [2,3,4,5].
We present in this work the application of a minimally invasive ICP method (ICPMI) based on mechanical extensometers in an experimental model of intracranial hypertension. ICPMI basically consists of a strain gauge (mechanical extensometer) attached to the parietal region laterally to the sagittal suture. The sensor is able to detect small skull deformations resulting from changes in ICP. At the current state of development, this method does not yield pressure values calibrated in millimetres of mercury, but provides continuous information about the ICP waveform and changes in time.
The objective of this study was to verify the similarities between the ICPMI and the invasive method (ICPInv) for different components of the ICP signal—namely, the mean value (trend) and its pulsatile component.
Materials and Methods
Experimental Protocol
A 9 kg anesthetized pig (n = 1) was used for simultaneous ICP monitoring with ICPMI and ICPInv methods. The ICPMI (Braincare, São Carlos, Brazil) sensor was glued on the parietal bone. The ICPInv (Codman & Shurtleff) micro transducer was inserted into the brain parenchyma, in the contralateral side of ICPMI (Fig. 1). Both sensors were plugged to the device Braincare CR15. All procedures were approved by the local Ethics Committee (CEEA/FMRP: 014/2013). ICP was increased by performing ten 6 ml infusions of 0.9% saline into the spinal subarachnoid space, using a catheter implanted in the lumbar region. The ICP signals were recorded using the ICP monitor BC Research 1.5 (Braincare), Braincare BCR software v.1.2 and the data were analysed using the Braincare Analytics System.
Data Analysis
To perform the correlation analysis, the signals were decomposed into two components—trend and pulsatile signals. The trend signal was defined as the mean value of the signal envelope, obtained from the interpolation (cubic spline) [6] of the local minima and maxima. To avoid possible drift influences in ICPMI signal, we linearly interpolated the signal before the start of each infusion and subtracted this linear trend from the signals before, during and after each corresponding infusion.
Linear correlation coefficient (Pearson) was calculated between ICP and minimally invasive ICP within temporal windows of 60s, with an overlapping of 50s. We considered correlations above 0.5 as significant. The analysis was performed using custom programs written in Python language, using the libraries Scipy [7], Matplotlib [8] and Scikit-learn [9].
Results
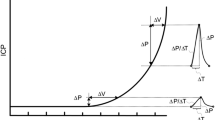
During the infusions, the correlation between the pulsatile components of the signals was above 0.5 for most of the time. The signal trends showed a good agreement (correlation above 0.5) for most of the time during infusions. Figure 2 shows comparisons between minimally invasive and invasive ICP monitoring methods for the first and last infusion procedures, respectively.
Comparison between minimally invasive and invasive ICP recording methods. (a, b) Invasive ICP recording. (c, d) Non-invasive ICP recording. (e, f) Linear correlations between trend (continuous) and pulsatile (dashed) components of the recordings, for the first infusion of the experiment. The green shadow represents the period in which the infusion was performed
Discussion
In this work, skull deformations could be associated with changes in ICPInv using ICPMI. Nevertheless, the calibration in absolute values (mmHg) for the minimally invasive ICP measurement still needs to be developed.
Our findings suggest that the minimally invasive method can be safely used as a simple and cost-effective alternative tool for ICP monitoring. Translated to clinical practice, the ICPMI could be applied where ICP monitoring has been limited due to the risks associated with the invasive procedures.
A potential limitation of this study is associated with the insertion of the needle into the spinal canal without externalizing the animal spine; thus, adequate control of the dural puncture was not feasible and leakage of saline possibly occurred after reaching a certain pressure threshold. The occurrence of a plateau phase for both methods indicates the moment when the pressure caused the balance between the volume of fluid infused and the fluid leaking through the lumbar puncture. The drift presented by the ICPMI sensor signal is mainly caused by the variation in temperature over the extensometer is subjected. This may have caused a mismatch in the correlation coefficients, as ICPInv is less influenced by temperature once it is in contact with the brain parenchyma.
Conclusions
The ICPMI signal trends showed a good linear agreement with the signal obtained invasively, despite occasional drifts caused by temperature variations or other sources of interference that might influence the minimally invasive sensor’s performance. Based on the waveform analysis of the pulsatile component of ICP, our results indicate the possibility of using the minimally invasive method for monitoring changes of ICP.
References
Andrews PD, Citerio G. Intracranial pressure. Intensive Care Med. 2004;30:1730–3. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00134-004-2376-4.
Kashif FM, Verghese GC, Novak V, Czosnyka M, Heldt T. Model-based noninvasive estimation of intracranial pressure from cerebral blood flow velocity and arterial pressure. Sci Transl Med. 2012;4:129ra44. Available from: http://stm.sciencemag.org/cgi/doi/10.1126/scitranslmed.3003249.
Barone DG, Czosnyka M. Brain Monitoring: do we need a hole? An update on invasive and noninvasive brain monitoring modalities. Sci World J. 2014;2014:1–6. Available from: http://www.hindawi.com/journals/tswj/2014/795762/.
Padayachy LC. Non-invasive intracranial pressure assessment. .Child’s Nerv Syst. 2016;1–11. Available from: https://doi.org/10.1007/s00381-016-3159-2.
Ferreira MCPD. Multimodal brain monitoring and evaluation of cerebrovascular reactivity after severe head injury. Porto: University of Porto; 2015.
Press WH, Teukolsky SA, Vetterling WT, Flannery BP. Numerical recipes. 3rd ed. Cambridge: Cambridge University Press; 2007.
Jones E, Oliphant T, Peterson P. Scipy: open source scientific tools for Python. 2001. Available from: http://www.scipy.org/.
Hunter JD. Matplotlib: a 2D graphics environment. Comput Sci Eng. 2007;9:90–5.
Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, et al. Scikit-learn: machine learning in Python. J Mach Learn Res. 2011;12:2825–30.
Conflicts of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this paper
Cite this paper
Frigieri, G. et al. (2018). Analysis of a Minimally Invasive Intracranial Pressure Signals During Infusion at the Subarachnoid Spinal Space of Pigs. In: Heldt, T. (eds) Intracranial Pressure & Neuromonitoring XVI. Acta Neurochirurgica Supplement, vol 126. Springer, Cham. https://doi.org/10.1007/978-3-319-65798-1_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-65798-1_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65797-4
Online ISBN: 978-3-319-65798-1
eBook Packages: MedicineMedicine (R0)