Abstract
Ischemic heart disease remains the leading cause of death worldwide. Mitochondria are the power plant of the cardiomyocyte, generating more than 95% of the cardiac ATP. Complex cellular responses to myocardial ischemia converge on mitochondrial malfunction which persists and increases after reperfusion, determining the extent of cellular viability and post-ischemic functional recovery. In a quest to ameliorate various points in pathways from mitochondrial damage to myocardial necrosis, exhaustive pharmacologic and genetic tools have targeted various mediators of ischemia and reperfusion injury and procedural techniques without applicable success. The new concept of replacing damaged mitochondria with healthy mitochondria at the onset of reperfusion by auto-transplantation is emerging not only as potential therapy of myocardial rescue, but as gateway to a deeper understanding of mitochondrial metabolism and function. In this chapter, we explore the mechanisms of mitochondrial dysfunction during ischemia and reperfusion, current developments in the methodology of mitochondrial transplantation, mechanisms of cardioprotection and their clinical implications.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Mitochondria
- Mitochondrial transplantation
- Ischemia/reperfusion injury
- Cardiac metabolism
- Cardiac surgery
Ischemic heart disease remains the leading cause of death worldwide and ischemia and reperfusion injury hallmark the central pathophysiology that determines clinical outcomes [1]. Robust investigations have elucidated the mechanisms of myocardial ischemia [2,3,4] and reperfusion injury [5] as well as the intrinsic adaptive mechanisms of myocardial stunning [6], hibernation [7], preconditioning [8, 9] and postconditioning [10,11,12]. They enabled the current knowledge of cardiac metabolism, unraveling the complex biochemical and cellular changes resulting from myocardial ischemia and reperfusion including disruptions of cellular energy, ionic homeostasis and oxidative stress which all converge on mitochondrial dysfunction to culminate in cellular apoptosis and necrosis [13,14,15,16].
The functional and structural derangements governing the pathophysiology of ischemia-reperfusion injury as well as changes in myocardial survival pathways inspired many pharmacological, genetic and procedural therapies in a variety of models including energy substrates, antioxidants, inhibitors of calcium (Ca2+) and sodium accumulation, mitochondrial components, immunomodulation as well as procedural techniques. However, a major dichotomy exists between positive results of preclinical studies and equivocal or negative results of the same therapies on limiting infarct size in human clinical trials [17]. Meanwhile, multi-disciplinary approaches in both experimental and clinical research targeting myocardial ischemia continue to highlight mitochondrial malfunction as the common denominator of cardiomyocyte’s ischemic response, emphasizing that the preservation of mitochondrial function and energy production may be the essential gateway to cardioprotection.
Rather than ameliorating one mediator or a step within the vast array of mitochondrial responses to ischemia and reperfusion, a newly emerging method of replacing damaged cardiomyocyte mitochondria with healthy mitochondria isolated from non-ischemic tissue of the same patient is being explored in various in vitro and in vivo models with promising results. In this chapter, we will explore (1) the basic physiology of myocardial ischemia and reperfusion injury, (2) the key features of mitochondrial metabolism and changes in ischemia and reperfusion injury, (3) current methodologies of mitochondrial transplantation, and (4) potential mechanisms of cardioprotection conferred by mitochondrial transplantation based on the most current experimental developments.
Mitochondria in Cardiac Tissue
The heart is a syncytial, muscular network of cardiomyocytes specialized to propagate electrical impulses across communicating cells allowing the varied components of the heart to act as a single contractile apparatus. The incessant contractility of the myocardium and cellular homeostasis is almost exclusively powered by the production of ATP by the mitochondria which constitute about 30% of the myocardial cell volume and provide for the daily turnover rate of ATP up to 15–20 times the weight of the heart in humans [18]. Thus, tight coupling of metabolic proficiency and myocardial contraction is essential for normal cardiac function and govern the intricate set of metabolic pathways resulting in both ATP producing and non-ATP producing endpoints for different classes of substrates under normal physiological conditions and during severe energy deprivation.
ATP is produced by the process of oxidative phosphorylation carried out by a series of four multi-subunit complexes embedded in the inner mitochondrial membrane as the Electron Transport Chain (ETC). The components of the electron transport chain include: Complex I (NADH dehydrogenase), II (succinate ubiquinone oxidoreductase), III (ubiquinol: cytochrome c oxidoreductase), IV (cytochrome c oxidase), V (ATP synthase), and two main electron carriers ubiquinone and cytochrome c. Thirteen of these 76 protein subunits making up the five complexes of the electron transport chain are encoded by the mitochondrial DNA and the remaining are encoded by the nuclear DNA. The various catabolic pathways of energy-yielding substrates (fatty acid, glucose, amino acids and ketones) converge on Acetyl-CoA production which mainly enter the tricarboxylic acid cycle (TCA) in the mitochondrial matrix to generate reducing equivalents NADH and FADH2. As electrons from NADH and FADH2 flow through the ETC to reduce oxygen to water (by complex IV), the resultant release of potential energy is used to pump protons into the mitochondrial intermembrane space (by complex I, III and IV) that generates an electrochemical gradient (−200 mV) across the mitochondrial inner membrane which is harnessed by complex V (ATP synthase) to couple P i and ADP to ATP. The ATP synthesized in the matrix is transported into the intermembrane space by an inner membrane channel adenine nucleotide translocase (ANT), where mitochondrial creatine kinase (miCK) transfers the high energy phosphate of ATP to create phosphocreatine which is then stored in the cytosol as energy reserves. Additional ATP is transported out to the cytosol via a complex formed by ANT, miCK and the voltage-dependent anion channel (VDAC) located in the outer membrane, where miCK bridges the space between ANT and VDAC, allowing for low conductance transfer of ATP out into the cytosol. In addition to the maintenance of cellular homeostasis, ATP consuming reactions vital to cardiomyocytes are exemplified by three main reactions which include (1) Myosin-ATPase which provides energy for myosin filament sliding for muscle contraction, (2) Ca2+/Mg2+-ATPase which stores Ca2+ in the sarcoplasmic reticulum for activation of myocardial contraction upon release, and (3) Na+/K+-ATPase used to maintain cellular excitability and Ca2+ efflux [19].
Cardiac mitochondria consist of two spatially distinct subpopulations, namely subsarcolemmal mitochondria (SSM), located directly beneath the cellular membrane, and interfibrillar mitochondria (IFM) which reside in rows between the myofibrils [20, 21]. Scanning and transmission electron microscopy of left ventricular papillary muscle sections of Japanese Monkeys and humans have revealed many structural differences between SSM and IFM [22, 23]. IFM are generally elongated in shape (1.5–2.0 μm), and occupy the space between Z-lines flanked by the junctional sarcoplasmic reticulum, and have predominantly tubular cristae. SSM located beneath the sarcolemma have more variable lengths and sizes (0.4–3.0 μm), possessing more lamelliform and closely-packed cristae [23, 24]. Studies using three dimensional modeling approach coupled with MitoTracker Red staining also revealed that IFM were arranged in a more orderly pattern in contrast to SSM which had a more random arrangement [25, 26]. Numerous reports have also indicated that SSM and IFM possess distinct functional differences such as substrate utilizations [20, 27, 28], enzymatic rates [21] and ATP synthesis [29, 30] which have been found to be generally higher in IFM.
Mitochondrial subpopulations appear to be differentially influenced during different pathological insults. However, many inconsistencies exist across different animal models. For example, cardiac ischemia has been reported to primarily effect SSM in rats [31] and rabbit models [32, 33] but both SSM and IFM populations in canines [21, 34]. In contrast to some of the ischemic models, ischemia and reperfusion injury have been reported to effect both populations in the mouse, rat and rabbit models [35,36,37]. The clinical significance of spatial distinctions of cardiac mitochondria with regards to pathological conditions and therapeutic interventions thereof, remain to be investigated.
Mitochondria in Myocardial Ischemia and Reperfusion
Ischemia-reperfusion injury occurs as a result of attenuation or cessation of coronary blood flow such that oxygen delivery to the myocardium is insufficient to meet the myocardial oxygen requirements to preserve cellular function and contraction. The energy stores generated by the mitochondria are only sufficient to sustain myocardial contractions for a few seconds, and this explains the need for the robustness of the cardiac metabolism, consuming the highest rate of oxygen per unit weight basis. Under normal conditions, 75% of the oxygen supplied by the coronary vasculature is extracted by the myocardium during a single passage through the heart. Therefore, the heart is highly susceptible to alterations in oxygen delivery where an increase in myocardial oxygen consumption (MVO2) can only be met by an increase in coronary blood flow, a phenomena unique to the cardiac muscle. The loss of myocardial oxygen delivery has been shown to exhaust myocardial oxygen reserves within 8 seconds after the onset of normothermic global ischemia with subsequent decrease in energy reserves [38]. In addition, studies measuring energy content by phosphorous-31 NMR spectroscopy have demonstrated that decreases in myocardial energy reserves are directly associated with decreases in myocardial function and viability which in turn are associated with detrimental clinical pathologies [39,40,41,42,43].
Reversible Myocardial Ischemia
With the onset of coronary occlusion, myocardial injury begins in approximately 20 min, being first evident in the subendocardium and papillary muscle, then extending into the mid-myocardial bed-at-risk by about 60–90 min, such that the wave-front of irreversible transmural infarction is complete in 3–4 hrs [44,45,46,47]. The infarcted myocardium subsequently exhibits features of inflammation and necrosis. Depending on the extent and duration of the ischemic event, myocardial injury may be reversible where the myocardium activates physiologic adaptations of survival manifested by myocardial stunning, hibernation and pre- and post-ischemic conditioning. These conditions result from changes in gene expressions that sustain cell survival under oxygen deprivation and during the stresses of reperfusion.
Myocardial stunning, first described by Heyndrickx and colleagues in 1975, refers to a state of contractile dysfunction which persists after reperfusion despite the absence of irreversible myocellular damage and return of normal or near-normal perfusion. Heyndrickx demonstrated the reversibility of ischemic myocardium following a 5 min or 15 min episode of ischemia and reperfusion in dogs, which resulted in a prolonged regional contractile deficit that required 6 h to recover from a 5 min ischemic episode and greater than 24 h to recover from a 15 min ischemic episode [48]. Stress of reperfusion can be exemplified in cardiac surgery patients where, despite modern methods of cardioprotection, the heart weaning from cardiopulmonary bypass often exhibit varying degrees of myocardial stunning and requires inotropes hours to days after surgery without objective evidence of myocardial infarction [49, 50].
In contrast to the stunned myocardium, the hibernating myocardium refers to a myocardium with chronically reduced contractility associated with local reduction in myocardial perfusion [51, 52]. Although the hypo-perfused cardiomyocytes can develop degenerative changes over time, the contractile function of the hibernating myocardium can be restored by reperfusion [53,54,55], allowing the myocardium to be called dysfunctional but ‘viable’. As in line with the ‘smart heart hypothesis’, hibernation is considered an adaptive mechanism of myocardial metabolism in which myocardial contractility and cellular activity is deliberately reduced to minimize metabolic demands and recruit coronary flow reserves in the face of severely depressed local perfusion [51]. However, hibernating myocardium cannot maintain viability indefinitely and delayed revascularization is associated with worse outcomes [56, 57]. It is now widely believed that repetitive episodes of stunning (i.e. ischemic dysfunction) create a sustained depression of contractile function as in hibernation and that stunning and hibernation are likely to be part of a continuous disease spectrum [58, 59]. In a swine model where the heart was subjected to repetitive episodes of 90 min of coronary occlusion followed by 12 h of reperfusion cycled up to six times, the regional myocardial function was depressed despite normalization of perfusion, reflecting myocardial stunning. However, additional episodes of coronary occlusion did not result in further decreases in ventricular function, reflecting the mismatch between perfusion and contractile function which characterizes hibernation [59]. This model along with several older studies demonstrated the hallmarks of chronic dysfunction in the human hibernating myocardium including loss of myofibrils, higher dependence on glucose and glycogen accumulation [60,61,62].
Irreversible Myocardial Ischemia and Mitochondrial Dysfunction
Despite regional differences in myocardial hypoxic tolerance and intrinsic adaptive mechanisms, irreversible myocardial injury inevitably follows prolonged ischemia. Countless studies have identified the pathological modulators of irreversible myocardial ischemic injury and the intricate linkages that converge on mitochondrial damage as the central culprit of cascade to myocardial cell death and tissue damage.
With the cessation of blood flow and oxygen supply, declines in the rate of oxygen consumption by oxidative phosphorylation and the synthesis of high energy phosphate products are immediately detectable. Mitochondrial function assessed by oximetry in many animal models have shown that ischemia significantly decreases state three oxygen consumption and respiratory control index in malate (complex I substrate) and succinate (complex III substrate) in energized mitochondria [63, 64]. Similar findings were measured for complex III and cytochrome oxidase in buffer-perfused rat hearts [32] and rabbit hearts [65] where global ischemia decreases their Vmax, mRNA levels as well as the content of cytochrome c. These declines were also shown to be paralleled with significant decreases in phosphocreatine, inorganic phosphate, ATP, and high energy stores, up to 36 ± 3% following 30 min of ischemia which remained decreased at 15 min post reperfusion via 31P nuclear magnetic resonance (NMR) [43].
With ischemic depletion of ATP synthesis, multiple biochemical and ultrastructural changes occur in the mitochondria that are hallmarked by several key cellular events which are cellular acidosis and accumulation of intracellular, mitochondrial and even nuclear Ca2+ ([Ca+2]n). With depletion of oxygen, the heart switches from fatty acid oxidation to anaerobic glycolysis resulting in a build-up of lactate and a decrease in the cellular pH. This rapid metabolic acidosis can be quantified by the measurement of tissue PCO2 and 21P NMR spectroscopy in the lab as well as with a pH probe in the operating room [66, 67]. Accumulation of intracellular hydrogen ion (H+) opens the sodium-hydrogen (Na+/H+) exchanger (NHE), resulting in the transport of H+ into the extracellular space and the movement of Na+ into the cytosol [68]. The excess Na+ is then extruded in exchange for the intake of Ca2+ through the reverse action of the plasma membrane sodium-Ca2+ (Na+/Ca2+) exchanger (NCX), increasing the cytosolic Ca2+concentration ([Ca2+])i. The increase in [Ca2+]i is further augmented by depolarization of the plasma membrane potential, which leads to the opening of the L-type Ca2+channels causing further Ca2+ influx, as well as the cessation of uptake of Ca2+ into the sarcoplasmic reticulum by the sarco/endoplasmic reticulum Ca2+-ATPase (SERCA) due to the decline in ATP [69]. Cellular Ca2+-dependent phospholipases and proteases are in turn activated inducing membrane injury and further Ca2+ entry into the cell.
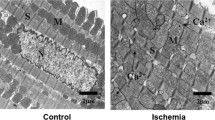
The increase in cytosolic Ca2+ leads to the augmented mitochondrial Ca2+ that has deleterious effects on their structure and function [70]. In a normal state, mitochondrial inner membrane pump H+ out to the cytosol creating a voltage gradient that provides the passive energy for Ca2+ influx into the matrix by the Ca2+-uniporter. During ischemia, increases in the intracellular Ca2+ ([Ca2+]i) lead to increased Ca2+ uptake by the mitochondria which destabilizes the inner membrane potential. As Ca2+ accumulates, mitochondria use ATP to transport excess Ca2+ out of the mitochondria against the electrochemical gradient which wastes more ATP required to maintain cellular viability, a mechanism called ‘futile Ca2+ cycling’ [70,71,72]. As Ca2+ overloads in the mitochondria, water passively follow and the mitochondria swell. This has been visualized via ECM and light scattering technique on isolated perfused heart and in vivo pig and sheep models, where greater than 88% of myocardial mitochondria are electron translucent and swollen following 20–30 min of global ischemia and exhibit increased intermembrane space, enlarged cristae and disrupted matrix [63, 64, 73, 74]. These alterations in mitochondrial structure are noted to be damaging to ATP transfer from the mitochondria via the adenine nucleotide translocase (ANT)-mitochondrial creatine kinase (miCK)-voltage-dependent anion carrier (VDAC) complex. It has been proposed that mitochondrial swelling increases intermembrane distance and dissociate the functional interaction between ANT, miCK and VDAC that compromise efficient energy transfer during reperfusion and decrease high energy synthesis in the myocardium post reperfusion [75].
The role of Ca2+ overload has been demonstrated by studies that showed warm global ischemia results in rapid accumulation of intracellular and mitochondrial Ca2+ which is associated with the depletion of ATP, and precedes the onset of ischemic contracture in various animal models [76,77,78]. Conversely, amelioration of this Ca2+ overload has been shown to correlate with maintenance of high energy phosphates in the myocardium, results of which formed the conceptual basis for optimization of many cardioplegic solutions in cardiac surgery. For example, Hearse et al. and many subsequent investigators showed that magnesium, when added to potassium cardioplegic solutions, significantly decreases cytosolic and nuclear Ca2+ accumulation during global ischemia [79, 80], enhances preservation and re-synthesis of high-energy phosphates, and significantly decreases myocardial injury upon reperfusion in perfused rabbit heart [43, 78, 81] and in situ blood-perfused sheep and pig heart models [47, 82, 83]. Furthermore, the addition of pharmacological agents such as diazoxide to the K+/Mg2+ cardioplegia solution, was shown to ameliorate mitochondrial Ca2+ accumulation by opening of the mitochondrial ATP-sensitive K+ channels which correlated with prevention of mitochondrial swelling, decrease in apoptosis and improved post-ischemic function [82, 84,85,86,87].
Myocardial Reperfusion and Mitochondrial Injury
While restoration of blood flow is the absolute therapeutic aim to salvage ischemic cell death, it is proposed that reperfusion itself independently activates a cascade of cellular injuries which inflate the damages in excess of those produced by ischemia alone. First described by Jennings et al. in 1960 in their description of histological features of reperfused ischemic canine myocardium, they reported that features of cellular injury after 3 h of ischemia followed by 1 h of reperfusion were far worse than changes observed after 4 h of ischemia alone; the reperfused myocardium had significantly more cell swelling, contracture of myofibrils and mitochondrial and sarcolemmal disruption [88]. Clinically, reperfusion injury leads to arrhythmias, conversion of myocardial necrosis into a hemorrhagic infarct with prominent contraction band necrosis, disruption of the microvasculature leading to the ‘no-reflow’ phenomenon, which refers to impairment of blood flow to an ischemic region in spite of opening the infarct-related artery [17, 89,90,91]. In addition, it is associated with activation of inflammatory reactions which can be extensive enough to cause inflammatory responses on distant, non-ischemic organs [92].
Extensive experimental efforts have identified the potential mechanisms of reperfusion injury that build on the existing elements of the damages sustained from ischemia, described by distinct biochemical changes that occur from reperfusion in the mitochondria. These changes include (1) rapid normalization of pH, (2) exacerbation of existing mitochondrial and intracellular Ca2+ overload, and (3) generation of reactive oxygen species.
Reperfusion and re-oxygenation results in rapid restoration of intracellular pH by lactic acid washout, clearance of H+ by the Na+/H+ exchanger (NHE) and Na+/HCO3 − exchanger, and the restoration of the mitochondrial membrane potential. As the mitochondrial membrane potential normalizes, the mitochondrial Ca2+-uniporter (MCU) opens causing an even more influx of Ca2+ into an already Ca2+-overloaded mitochondria [93]. Cytosolic Ca2+ is also proposed to be further increased by the damaged sarcolemmal membrane and oxidative stress-induced dysfunction of the sarcoplasmic reticulum, all of which can overwhelm the cardiomyocyte’s mechanisms for ionic homeostasis.
Many experimental studies have also implicated Reactive Oxygen Species (ROS) as partial mediators of reperfusion injury and the damaged mitochondria as the potential primary source of ROS production. Various modalities including electron spin resonance spectrometer [94] have detected bursts of ROS during myocardial reperfusion in different animal models and patients undergoing coronary revascularization [95]. Examples include H2O2, HO−, HOCl, and O2 −, the superoxide anion radial which is considered to be the most toxic ROS generated primarily by the mitochondria. In addition, it has been recently proposed that mitochondrial alterations at complex I of the electron transport chain and the accumulation of succinate during ischemia may be related to mitochondrial oxidative injury during reperfusion. Succinate is the substrate of complex II, and the sole mitochondrial component to the three metabolites that accumulate during ischemia: succinate, xanthine and hypoxanthine [96]. Accumulation succinate is detected in the mitochondria when the electron transport chain comes to a halt during ischemia. It is proposed that upon reperfusion, succinate is abruptly hydrolyzed by complex II [97, 98] at a maximal rate that overwhelms the speed of ATP synthesis generating an excess pool of electrons that start to flow backwards by a process termed Reverse Electron Transport (RET) [99]. As the excess electrons are forced back through complex I, the reverse reaction of NADH dehydrogenase generates large amounts of superoxide. This has been demonstrated by various animal experiments which showed that inhibition of complex I slows reactivation of mitochondria during the early phase of reperfusion, reduce ROS and protects against ischemic-reperfusion injury [100,101,102,103]. Excessive ROS generated during reperfusion cause tissue damage by a myriad of mechanisms including peroxidation of lipids, inactivation of proteins/enzymes, nuclear and mitochondrial DNA strand breaks, oxidation of Cardiolipin, SER dysfunction and activate inflammation, all of which serve to activate apoptotic and necrotic signaling pathways. ROS also reduce the viability of the vasodilator nitric oxide (NO), removing its cardioprotective effects such as inactivation of superoxide radicals, inhibition of neutrophil accumulation and improvement of coronary flow [104].
Multitude of the acute fluctuations described above are proposed to act in concert to lead to the opening of the voltage dependent, nonspecific pore in the inner mitochondrial membrane known as the Mitochondrial Permeability Transition Pore (mTPT), which is thought to be the most noxious step marking the transition from reversible to irreversible reperfusion injury. The mTPT is closed during normal conditions and ischemia. Opening of mTPT pore at reperfusion allows the free passage of any molecule smaller than 1.5 kDa, causing a buildup of colloidal osmotic pressure leading to severe mitochondrial swelling, complete collapse of the mitochondrial membrane potential, uncoupling of oxidative phosphorylation and disruption of the mitochondrial membrane and eventual rupture. This process leads to release of the cytochrome c from the ETC, which is a potent activator of apoptotic signaling cascades leading to cardiomyocyte death [105, 106]. Systemically, activation of corresponding immune responses leads to leukocyte aggregation, leukocyte-mediated tissue destruction and endothelial dysfunction leading to platelet aggregation causing damage to the surrounding microvasculature.
Ischemia Versus Reperfusion Injury
The concept of reperfusion injury as an independent mediator of cardiomyocyte death distinct from ischemic injury has been controversial. The uncertainty relates to the inability to accurately assess the exact progression of necrosis during the transition from myocardial ischemia to reperfusion in situ [17]. Moreover, understanding the sequential evolution of mitochondrial damage in relation to the timeframe along myocardial ischemia and reperfusion is not straightforward. In spite of these challenges, studies demonstrate that critical events of mitochondrial damage occur at the time of ischemia and persist through reperfusion.
Transcriptomic and proteomic enrichment analyses in both Langendorff-perfused and in situ blood-perfused rabbit hearts have demonstrated that global ischemia downregulates genes/proteins associated with mitochondrial structure, function, energy production, cofactor metabolism, generation of precursor metabolites of energy, carbohydrate metabolism and regulation of biosynthesis and transcription [107]. In contrast, the same analyses in globally ischemic rabbit hearts treated with cardioplegia showed that cardioprotection was associated with significant increases in differentially expressed transcripts/proteins associated with mitochondrial function, energy production, fatty acid beta oxidation, cellular lipid metabolism as well as processes of muscle contraction [107]. These results indicate that (1) the mitochondrion plays a significant role in both global ischemia and cardioprotective pathways, (2) the mechanisms of mitochondrial damage resulting from global ischemia as well as pathways of cardioprotection are modulated, at least in part, by RNA- and protein-dependent mechanisms, and (3) these critical events occur at the time of ischemia rather than reperfusion.
The challenges of elucidating reperfusion injury are also demonstrated by the equivocal results of studies targeting the accepted mediators of reperfusion injury. While attractive targets of intervention such as the accumulation of Ca2+, reactive oxygen species, components of the electron transport chain and inflammation have yielded promising preclinical results, their clinical translations have been largely disappointing. For example, efforts to decrease Ca2+ overload with antagonists of the sarcolemmal Ca2+ ion channels, mitochondrial Ca2+ uniporter, or the Na+/H+ exchanger have shown to decrease myocardial infarct sizes up to 50% in animal models [108,109,110], but have been unsuccessful in the corresponding clinical studies [111,112,113]. The same trend is present in animal studies where these interventions were applied just at reperfusion to yield reductions in the final infarct sizes up to 50%, their applications in patients have been largely negative or inconclusive [17]. A host of antioxidants such as superoxide dismutase, trimetazimide, vitamin C and E with positive results in animal models failed to show meaningful improvement in infarct size, post-ischemic cardiac function nor mortality benefit in human clinical trials [114,115,116]. Similarly, attempts at targeting neutrophils such as leukocyte depleted blood [117], antibodies against the cell adhesion molecule P selection [118] as well as inhibitors of complement activation [119] have shown significant cardioprotection in animals with negative results in their corresponding clinical studies [120,121,122,123,124].
Several reasons may exist for the discrepancy between the experimental animal studies and human trials. First, although the existence of ischemia and reperfusion injury and the essential role of the mitochondria is well established in humans, variabilities may exist in the detailed biochemical mechanisms underlying cell death pathways amongst different species. Second, heterogeneities in a clinical setting in the varying degrees of ischemia as well as timing and context of intervention may contribute to the inconclusive results of clinical studies. Third, the interventions examined so far may have been of questionable benefit in preclinical studies or lacking in adequate knowledge of their pharmacological actions and kinetics in clinical subjects. Although the unequivocal role of mitochondrial dysfunction in myocardial ischemia and reperfusion is increasingly evident, the low rate of clinical success in the vast number of therapeutic targets investigated thus far calls for a need to evaluate our current understanding of the sequential mechanism of mitochondrial dysfunction during ischemia and reperfusion, as well as the way we devise our remedies.
Mitochondrial Transplantation
Mitochondrial dysfunction is the prominent feature of myocardial ischemic injury which are compounded by the process of reperfusion to have lasting effects on post-ischemic function and cellular viability. A myriad of experimental studies confirms that loss of mitochondrial function during ischemia significantly decreases cardiomyocyte viability and post-ischemic recovery. Despite this clear trend, there is currently no meaningful therapy for mitochondrial rescue from ischemia-reperfusion injury with growing discrepancies between preclinical and clinical studies. This calls for a review and a shift in the current paradigm and exploration of new approaches in therapeutic design. Instead of targeting a single step or one mediator of a complex, interconnected reactions of mitochondrial injury, a new therapy of mitochondrial transplantation is being investigated with the hypothesis that replacement of damaged mitochondria with viable, respiration-competent mitochondria isolated from non-ischemic tissue would overcome a host of deleterious effects of native mitochondrial dysfunction resulting in cardioprotection.
Mitochondrial Transplantation for Cardioprotection
Based on the hypothesis that myocardial mitochondrial injury occurs during ischemia and persists during reperfusion to significantly compromise post-ischemic myocardial function and viability, the concept of mitochondrial transplantation at the time of reperfusion was proposed in the recent decade. The first validation of mitochondrial transplantation in the ischemic heart model was demonstrated in the Langendorff-perfused ischemic rabbit heart in 2009 [125]. In this study, viable, respiration-competent mitochondria isolated from healthy left ventricular tissue of donor rabbits were directly injected into the ischemic zone of isolated hearts after 30 min of regional ischemia just prior to 120 min of reperfusion. Ischemic hearts that were transplanted with healthy mitochondria were found to have significantly enhanced cardioprotection by increased ATP content, reduction in infarct size, decreased cardiomyocyte loss, and improved post-ischemic myocardial function. Confocal microscopy showed that injected mitochondria were present and viable after 120 min of reperfusion and were distributed from the epicardium to the sub-endocardium. These findings heightened new interests in mitochondrial therapy calling for a deeper understanding of the mechanisms behind mitochondrial transfer, uptake, cardioprotection as well as the optimization of methods for enhancing clinical applicability.
Mitochondrial Source and Viability
In efforts to enhance clinical practicality and reduce immunogenic complications, rather than transplanting mitochondria from an allogenic source such as a donor organism, an approach of isolating mitochondria from a remote, nonischemic tissue in the same organism (autologous) to be transplanted into an ischemic region of the myocardium have been explored with promising results [126, 127]. A recent study in an in-vivo rabbit model of regional myocardial ischemia and reperfusion, autologous mitochondria from the pectoralis major muscle of the same organism were isolated via the newest isolation technique of standard homogenization and filtration, and injected in the myocardium following 29 min of ischemia immediately prior to reperfusion [126]. Results showed that transplantation of mitochondria isolated this way significantly decreased infarct size, improved cardiomyocyte viability and myocardial function at 4 weeks of recovery. Furthermore, additional studies showed that transplantation of autogenic mitochondria did not induce any autoimmunity via multiplex and ELISA assays which did not show any increases in inflammatory cytokines associated with immune responses seen in patients with heart transplant rejection such as C-Reactive Protein (CRP), Tumor Necrosis Factor-alpha (TNFα), Interleukins -1, -4, -6, -12, -18, Macrophage Inflammatory Protein -1 alpha and -1 beta (MIP-1α, -1β) [126].
In addition to the benefits of the autologous origin of mitochondria, efficacy of mitochondrial isolation from various sources of tissues has been investigated. As expected, different sources of tissues provide different absolute number of mitochondria, with liver being the highest, followed by skeletal muscle followed by cardiac muscle [127]. However, no differences were detected in the cardioprotective effects of mitochondria derived from different tissue types [125, 126], nor their subpopulations (subsarcolemmal or interfibrillar) [125]. On the other hand, mitochondrial viability is found to be a prime determinant of efficacy of mitochondrial transplantation for cardioprotection. Studies have shown that Nonviable mitochondria isolated from frozen tissue with confirmed absence of oxygen consumption failed to provide cardioprotection [125]. Similarly, mitochondrial proteins, mitochondrial complexes and mitochondrial RNA and DNA have not been found to provide cardioprotection [125]. Injection of exogenous ATP, ATP synthesis promoters, and exogenous ADP have also not shown to result in any protection against myocardial ischemia [125, 128]. These findings together indicate the imperative requirement of transplanted mitochondria to be viable, freshly-isolated and respiration-competent to be efficacious.
Mitochondrial Isolation and Purification
To assure the viability of the transplanted mitochondria and the clinical practicality of mitochondrial transplantation, it is critical that the isolation process of mitochondria is simple, cost-effective and feasible within the clinical timeframe of intervention for myocardial ischemia. For example, in the case of ST-elevation myocardial infarction (STEMI), the goal time from the onset of evaluation to revascularization via PCI (door-to-balloon time) is less than 90 min. For cardiac surgery, most operations last from 40 min to several hours in duration. However, the time from the onset of actual incision to revascularization or to the time to wean from bypass are often less than 1 h. This makes the standard technique of mitochondrial isolation which takes over 90 min at best, impractical and unreliable for yielding viable mitochondria. In 2014, a new method of rapid isolation and purification of mitochondria was developed by Preble and colleagues, who employ standardized tissue dissociator and differential filtration rather than centrifugation, cutting the isolation time to less than 30 min [129]. The purity and viability of the mitochondria isolated from this method have been validated by many different quality control parameters involving oxygen consumption rates via the Clarke-type electrode, ATP assays, fluorescent probe analysis, as well as light microscopy using fluorescent mitochondrial labels (MitoTracker CMXros) and transmission electron microscopy [125, 126, 129, 130].
Mitochondrial Delivery, Mode of Uptake and Distribution
To further enhance the therapeutic potential of mitochondrial transplantation, different modes of delivery of exogenous mitochondria have been investigated which include direct myocardial injection and intracoronary vascular infusion. From initial studies in both Langendorff-perfused and in situ-blood perfused rabbit hearts, respiration competent, autologous mitochondria were injected directly into eight to ten sites in the ischemic left ventricular free wall which showed significant improvement in infarct size and myocardial function. In a recent study using Langendorff-perfused rabbit heart model of both regional and global ischemia, the mode of vascular delivery via intracoronary infusion was validated and compared to the method of direct injection with regards to myocardial distribution using 18F-rhodamine 6G and iron oxide nanoparticles labeling followed by visualization with positron emission tomography, microcomputed tomography and magnetic resonance imaging [127]. Intracoronary delivery of mitochondria was shown to result in a rapid and a more widespread distribution throughout the myocardium as compared to direct injection, which permitted higher concentrations of mitochondria in the targeted region. The efficacy of cardioprotection via intracoronary delivery of autologous mitochondria paralleled that of direct injection in another experiment using Langendorff-perfused rabbit hearts of regional ischemia which showed similar decrease in myocardial infarct size and improvement in both global and regional myocardial function [127]. While additional in vivo studies are needed, the ability to deliver mitochondria by vascular infusion expands the therapeutic potential such as global delivery to the ischemic heart just prior to reperfusion after cardiopulmonary bypass or delivery into the coronary artery at time of percutaneous coronary interventions (PCI) for revascularization.
On a histological level, both in situ and in isolated heart models, transplanted mitochondria have been shown to be initially present in the interstitial spaces surrounding cardiomyocytes coinciding with the time of increase in myocardial function, approximately 10 min post injection. Within 1–2 h post-delivery, the transplanted mitochondria were detectable within cardiomyocytes residing near the sarcolemma between Z-lines of the sarcomeres, in clusters around endogenous damaged mitochondria as well as near the nucleus. This internalization has been confirmed using human mitochondria isolated from HeLA cells in a rabbit heart. The use of human mitochondria in the rabbit model allows for the differentiation between native rabbit mitochondria and transplanted human mitochondria based on immune reactivity to a monoclonal anti-human mitochondrion, and internalization of the mitochondria into cardiomyocytes were visualized via transmission electron microscopy using immune-gold staining [125, 126]. These studies along with other in vitro studies demonstrated that the uptake of mitochondria is linear and time dependent, and remain viable for at least 24 h, significantly enhancing rate of oxygen consumption and high-energy synthesis in both neonatal and adult cardiomyocytes [125, 126, 131].
Many hypotheses have been proposed as to the mechanism of mitochondrial internalization by cardiomyocytes such as actin-meditated endocytosis, Caveolae-dependent-clathrin dependent endocytosis [132], tunneling nanotubes [133] and macro-pinocytosis [134] based on prior experiments in cell types other than cardiomyocytes. A recent in vitro study of cardiomyocytes using specific inhibitors of these mechanisms showed that only Cyctochalasin D, a specific inhibitor of actin polymerization, decreased internalization of mitochondria into cardiomyocytes and deceased ATP content, suggesting actin-mediated endocytosis as a potential mechanism of mitochondrial internalization by cardiomyocytes [131]. Additionally, the internalized mitochondrial did not co-localize with lysosomal or autophagocytosis markers raising another mechanism by which the internalized mitochondria escape endosomes. Actin-mediated endocytosis of mitochondria is in agreement with the widely accepted theory of the endosymbiotic origin of mitochondria. While externally presented mitochondria may be internalized via actin-mediated endocytosis in cardiomyocytes, intercellular transfer of mitochondria between cells may involve tunneling nanotubes within the syncytial architecture of cardiomyocytes in vivo [135].
Mechanisms of Cardioprotection
The mechanism through which transplanted mitochondria provide cardioprotection reflect the mediators of mitochondrial damage accrued during ischemic injury. Based on the established observations, at the least, cardioprotection via autologous mitochondrial transplantation are considered to involve (1) increased myocardial ATP content and metabolic recovery (2) change in proteomic and transcriptomics (3) upregulations of cytokine and chemokines that enhance post-infarct myocardial function and (4) replacement of damaged mitochondrial DNA.
To date, all studies of mitochondrial transplantation in cardiac tissue have shown that transplanted mitochondria increase cellular ATP content and oxygen consumption. In the in vivo rabbit model of regional ischemia/reperfusion injury, total tissue ATP content in the area of risk in mitochondria-transplanted hearts were significantly increased starting as early as 15 min of mitochondrial delivery and present even at 21 days of recovery compared to their controls. On the other hand, the use of exogenous ATP or ADP have not shown to restore high-energy phosphate stores nor have beneficial effects on post-ischemic functional recovery [126, 128, 136]. This is believed to be due, in part, to the lability of ATP and its short half-life in vivo. In line with this observation, cardioprotection by mitochondrial transplantation requires mitochondria that are intact, viable and respiration competent. Use of non-viable mitochondria or mitochondrial components such as mitochondrial RNA and DNA have not shown to confer improvement in postischemic function or cellular viability, although some mitochondrial complexes such as cytochrome c [137] and coenzyme Q10 have been shown to have modest benefit at very high doses [138].
The increases in the energy level and metabolic recovery is also reflected by the changes in myocardial proteomics and increases in differentially expressed proteins post mitochondrial transplantation. Study using proteomic analysis and functional annotation clustering in post-ischemic rabbit myocardial tissue have shown that proteome clusters of the mitochondrion, the generations of precursor metabolites for energy, and cellular respiration were significantly increased in hearts treated with mitochondrial transplantation compared with their controls [126].
Mitochondrial transplantation has also been shown to result in downregulation of inflammatory cytokines and upregulation of chemokines that play key roles in angiogenesis, ateriogenesis, progenitor cell migration, prevention and protection against cardiomyocyte apoptosis and enhanced cardiac functional recovery. Rabbit hearts with regional ischemia treated with autologous mitochondrial transplantation were shown in vivo to have significantly decreased inflammatory markers when compared to untreated regional ischemic hearts, including tumor necrosis factor alpha (TNFα), interleukin -6 and -10 (IL-6, -10), monocyte chemoattractant protein-1 (MCP-1) and high-sensitivity C-reactive protein (hsCRP). Multiplex analysis indicated that autologous mitochondria significantly upregulated expression of epidermal growth factor (EGF), growth-related oncogene (GRO), interleukin-6 (IL-6) and monocyte chemoattractant protein-3 (MCP-3). EGF been shown to play a key protective role in myocardial ischemic injury by stimulating cell growth, proliferation and migration [139, 140]. GRO and IL-6 have been implicated in reconstitution of cardiac tissue mass post myocardial infarction by acting as chemoattractants for vascularization and protection against cardiomyocyte apoptosis [141]. These chemokines all act with MCP-3 to enhance post-infarct myocardial function and improve myocardial remodeling. It has been proposed that together with increased tissue ATP levels in the area of ischemic injury, induction of cardioprotective cytokines augment the role of differentially expressed proteins and mitochondrial pathways to enhance metabolic recovery and post ischemic cardiac function.
The effect on reactive oxygen species (ROS) by mitochondrial transplantation remains to be delineated, although results are gearing more towards the idea that ROS may not to play a major role in cardioprotection provided by mitochondrial transplantation. In Langendorff-perfused rabbit hearts of regional ischemia, ROS in form of thiobarbituric acid-reactive substances (TBARS) were found to be significantly decreased in hearts that received mitochondrial transplantation when compared to untreated hearts. However, ROS scavenger 2-Mercaptopropionylglycine (MPG) failed to block cardioprotection afforded by mitochondrial mitochondria when used throughout reperfusion, or added to the transplanted mitochondria, suggesting that cardioprotection by transplanted mitochondria occurs through mechanism that are not significantly modified by ROS [126]. Whether these observations represent primary or secondary effects along with more clear role of ROS in the spectrum of mitochondrial injury and recue remain open to continued investigation.
Consistent with studies in many other fields, recent studies have also shown that mitochondrial transplantation not only rescues cellular energy and function, but also replaces damaged mitochondrial DNA [131]. In vitro studies using human HeLa cells depleted of mitochondrial DNA (HeLa p0) incapable of oxygen consumption were rescued by co-incubation with mitochondria containing intact mtDNA with significantly increased ATP content and oxygen consumption rates detected even at 2 weeks post co-incubation. Quantitative real-time RT-PCR analysis confirmed replacement of mtDNA in HeLa p0 cells following mitochondrial transplantation. Whether the mechanism of this type of mitochondrial rescue is related to the replication of mtDNA in the transplanted mitochondria or expansion of transplanted mitochondrial population requires further characterization.
Mitochondrial Transplantation in Human Subjects
First clinical application of mitochondrial transplantation therapy has been done in 2016 in pediatric patients who suffered myocardial ischemia-reperfusion injury at our institution. Five pediatric patients in critical condition who were unable to be weaned off extracorporeal membrane oxygenation (ECMO) support due to myocardial dysfunction related to ischemia and reperfusion were treated with autologous mitochondria isolated from the patients’ rectus abdominis muscle and were injected at ten different places in the most hypokinetic regions of the myocardium [142]. All five patients had significant improvement in their myocardial systolic function and all but one patient were successfully weaned off ECMO support by the second day post mitochondrial transplantation. The single patient who was unable to wean off ECMO support suffered irreversible multi-organ failure despite the recovery of myocardial function following mitochondrial transplantation. As shown in animal models, mitochondrial auto-transplantation successfully improved post-ischemic myocardial function and was not associated with adverse short-term complications related to mitochondrial delivery such as arrhythmia, intramyocardial hematoma or scarring. This case demonstrates the potential role of the novel therapy of mitochondrial transplantation to improve ventricular dysfunction following ischemia-reperfusion injury in humans. Additional experimental investigations and larger scale trials are necessary to evaluate details of safety, efficacy, dosing and modes of transplantation with paralleled improvements in our understanding of ischemia and reperfusion injury and the role of mitochondria.
Conclusion
Mitochondrial dysfunction is the principal feature of myocardial ischemic injury which prevails through reperfusion to severely compromise cardiomyocyte survival and post-ischemic ventricular function. These include alterations in mitochondrial structure, function, ionic accumulations, mitochondrial enzyme and complex activity, high energy synthesis, mitochondrial DNA structure, transcriptomics, proteomics, and mitochondria-mediated apoptotic pathways. Mitochondrial auto-transplantation involves replacing damaged mitochondria in the ischemic heart with fresh, viable, and respiration competent mitochondria isolated from a nonischemic area of the patient’s own body to circumvent damaged mitochondrial function accrued during ischemia and rescue myocardial function. This novel method has been shown to improve myocardial infarct severity, cellular viability, and ventricular function in many different animal models and preliminarily, in humans. The known mechanisms of cardioprotection by mitochondrial transplantation include increase in myocardial ATP content, changes in mitochondrial proteomics and transcriptomics, upregulation of cytokine and chemokines that enhance post-infarct myocardial function, as well as replacement of damaged mitochondrial DNA. Moreover, the advent of mitochondrial isolation to a simple, rapid and highly pure technique, permits application of this method within the clinical timeframe of most medical and surgical procedures.
Possible applications of mitochondrial transplantation abound, as mitochondrial damage underlie a vast number of disorders including Alzheimer’s disease, Parkinson’s disease, ischemia-reperfusion injury of the liver, kidney, brain and muscle compartments, as well as rare mitochondrial genetic disorders. Recently, mitochondrial transplantation has been shown to restore damaged mitochondrial function in Parkinson’s’ disease brain in rats [143], decrease cell death from ischemia-reperfusion injury in rat liver [144] and attenuate hypoxic pulmonary hypertension in rats [145]. A recent study by Hayakawa et al. described the transfer of healthy mitochondria from astrocytes to surrounding neuronal cells during transient focal cerebral ischemia to induce cell survival pathways [146].
From natural phenomena to constructed therapies, the diversified transmissibility of mitochondria and their exertive roles on cellular transformation and survival are difficult to underestimate. Much remains in question with regards to the mechanism of mitochondrial influence on cell survival as well as their specific roles in different disease models; and optimizations of safety and long-term outcomes provoke future experimental tasks and innovation. Along with many varied fields of mitochondrial disorders, mitochondrial transplantation offers a valuable strategy for cardioprotection in ischemic heart disease and opens the gateway to deeper understanding of mitochondrial function and therapeutic potential.
References
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603.
Jennings RB, Reimer KA. Lethal myocardial ischemic injury. Am J Pathol. 1981;102:241–55.
Buja LM, Willerson JT. Abnormalities of volume regulation and membrane integrity in myocardial tissue slides after early ischemic injury in the dog: effects of mannitol, polyethylene glycol, and propranolol. Am J Pathol. 1981;103:79–95.
Santulli G, Nakashima R, Yuan Q, Marks AR. Intracellular calcium release channels: an update. J Physiol. 2017 (in press). doi: 10.1113/JP272781.
Braunwald E, Kloner RA. Myocardial reperfusion: a double-edge sword? J Clin Invest. 1985;76:1713–9.
Fassina L, Rozzi G, Rossi S, Scacchi S, Galetti M, Lo Muzio FP, Del Bianco F, Colli Franzone P, Petrilli G, Faggian G, Miragoli M. Cardiac kinematic parameters computed from video of in situ beating heart. Sci Rep. 2017;7:46143 doi:10.1038/srep46143.
Kloner RA, Przyklenk K, Patel B. Altered myocardial states: the stunned and hibernating myocardium. Am J Med. 1989;86:14–22.
Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74:1124–36.
Murry CE, Richard VJ, Reimer KA, Jennings RB. Ischemic preconditioning slows energy metabolism and delays ultrastructural damage during a sustained ischemic episode. Circ Res. 1990;66:913–31.
Zhao ZQ, Corvera JS, Halkos ME, Kerendi F, Wang NP, Guyton RA, Vinten-Johansen J. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;285:H579–88.
Zhao ZQ, Vinten-Johansen J. Postconditioning: reduction of reperfusion-induced injury. Cardiovasc Res. 2006;70:200–11.
Cohen MV, Yang XM, Downey JM. The pH hypothesis of postconditioning: staccato reperfusion reintroduces oxygen and perpetuates myocardial acidosis. Circulation. 2007;115:1895–903.
Kolwicz Jr SC, Purohit S, Tian R. Cardiac metabolism and its interactions with contraction, growth and survival of cardiomyocytes. Circ Res. 2013;113:603–16.
Carden DL, Granger DN. Pathophysiology of ischemia-reperfusion injury. J Pathol. 2000;190:255–66.
Collard CD, Gelman S. Pathophysiology, clinical manifestations, and prevention of ischemia-reperfusion injury. Anesthesiology. 2001;94:1133–8.
Turer AT, Hill JA. Pathogenesis of myocardial ischemia-reperfusion injury and rationale for therapy. Am J Cardiol. 2010;106:360–8.
Yellon DM, Hausenloy DJ. Myocardial reperfusion injury. N Engl J Med. 2007;357:1121–35.
Meerson FZ, Zaletayeva TA, Lagutchev SS, Pshennikova MG. Structure and mass of mitochondria in the process of compensatory hyperfunction and hypertrophy of the heart. Exp Cell Res. 1964;36:568–78.
Feinberg H, Levitsky S. Biochemical rationale of cardioplegia. In: Engelman RM, Levitsky S, editors. A textbook of clinical cardioplegia. Mt Kisco, New York: Futura; 1982. p. 131–9.
Palmer JW, Tandler B, Hoppel CL. Biochemical properties of subsarcolemmal and interfibrillar mitochondria isolated from rat cardiac muscle. J Biol Chem. 1977;252:8731–9.
Weinstein ES, Benson DW, Fry ED. Subpopulations in human heart mitochondria. J Surg Res. 1986;40:495–8.
Dalen H, Odegarden S, Saetersdal T. The application of various electron microscopic techniques for ultrastructural characterization of the human papillary heart muscle cell in biopsy material. Virchows Arch A Pathol Anat Histopathol. 1987;410:265–79.
Shimada T, Horita K, Murakami M, Ogura R. Morphological studies of different mitochondrial populations in monkey myocardial cells. Cell Tissue Res. 1984;238:577–82.
Lukyanenko V, Chikando A, Lederer WJ. Mitochondria in cardiomyocyte Ca2+ signaling. Int J Biochem Cell Biol. 2009;41:1957–71.
Birkedal R, Shiels HA, Vendelin M. Three-dimensional mitochondrial arrangement in ventricular myocytes: from chaos to order. Am J Physiol Cell Physiol. 2006;291:C1148–58.
Hollander JM, Thapa D, Shepherd D. Physiological and structural differences in spatially distinct subpopulations of cardiac mitochondria. Am J Physiol Heart Circ Physiol. 2014;307:H1–14.
Muller W. Subsarcolemmal mitochondria and capillarization of soleus muscle fibers in young rats subjected to an endurance training. A morphometric study of semithin sections. Cell Tissue Res. 1976;174:367–89.
Rosca MG, Hoppel CL. Mitochondrial dysfunction in heart failure. Heart Fail Rev. 2013;18:607–22.
Baseler WA, Thapa D, Jagannathan R, Dabkowski ER, Crsoton TL, Hollander JM. miR-141 as a regulator of the mitochondrial phosphate carrier (Slc25a3) in the type 1 diabetic heart. Am J Physiol Cell Physiol. 2012;303:C1244–51.
Croston TL, Shepherd DL, Thapa D, Nichols CE, Lewis SE, Dabkowski ER, Jagannathan R, Baseler WA, Hollander JM. Evaluation of the cardiolipin biosynthetic pathway and its interactions in the diabetic heart. Life Sci. 2013;93:313–22.
Chen Q, Moghaddas S, Hoppel CL, Lesnefsky EJ. Ischemic defects in the electron transport chain increase the production of reactive oxygen species from isolated rat heart mitochondria. Am J Physiol Cell Physiol. 2008;294:C460–6.
Lesnefsky EJ, Gudz TI, Migita CT, Ikeda-Saito M, Hassan MO, Turkaly PJ, Hoppel CL. Ischemic injury to mitochondrial electron transport in the aging heart: damage to the iron-sulfur protein subunit of electron transport complex III. Arch Biochem Biophys. 2001;385:117–28.
Lesnefsky EJ, Chen Q, Moghaddas S, Hassan MO, Tandler B, Hoppel CL. Blockade of electron transport chain during ischemia protects cardiac mitochondria. J Biol Chem. 2004;279:47961–7.
Rosca MG, Vazquez EJ, Kerner J, Parland W, Chandler MP, Stanely W, Sabbah HN, Hoppel CL. (2008)Cardiac mitochondria in heart failure: decrease in respirasomes and oxidative phosphorylation. Cardiovasc Res. 2008;80:30–9.
Dabkowski ER, Williamson CL, Hollander JM. Mitochondria-specific transgenic overexpression of phospholipid hydroperoxide glutathione peroxidase (GPx4) attenuates ischemia/reperfusion-associated cardiac dysfunction. Free Radic Biol Med. 2008;45:855–65.
Duan J, Karmazyn M. Relationship between oxidative phosphorylation and adenine nucleotide translocase activity of two populations of cardiac mitochondria and mechanical recovery of ischemic hearts following reperfusion. Can J Physiol Pharmacol. 1989;67:704–9.
Lesnefsky EJ, Chen Q, Slabe TJ, Stoll MS, Minkler PE, Hassan MO, Tandler B, Hoppel CL. Ischemia, rather than reperfusion, inhibits respiration through cytochrome oxidase in the isolated, perfused rabbit heart: role of cardiolipin. Am J Physiol Heart Circ Physiol. 2004;287:H258–67.
Kubler W, Spieckermann PG. Regulation of glycolysis in the ischemic and anoxic myocardium. J Mol Cell Cardiol. 1970;1:351–77.
Conway MA, Allis J, Ouwerkerk R, Niioka T, Rajagopalan B, Radda GK. Detection of low phosphocreatine to ATP ratio in failing hypertrophied human myocardium by 31P magnetic resonance spectroscopy. Lancet. 1991;338:973–6.
Hardy CJ, Weiss RG, Bottomley PA, Gerstenblith G. Altered myocardial high-energy phosphate metabolites in patients with dilated cardiomyopathy. Am Heart J. 1991;112:795–801.
Neubauer S, Krahe T, Schindler R, Horn M, Hillenbrand H, Entzeroth C, Mader H, Kromer EP, Riegger GA, Lackner K. 31P magnetic resonance spectroscopy in dilated cardiomyopathy and coronary artery disease. Altered cardiac high-energy phosphate metabolism in heart failure. Circulation. 1992;86:1810–8.
Neubauer S, Horn M, Cramer M, Harre K, Newell JB, Peters W, Pabst T, Ertl G, Hahn D, Ingwall JS, Kochsiek K. Myocardial phosphocreatine-to-ATP ratio is a predictor of mortality in patients with dilated cardiomyopathy. Circulation. 1997;96:2190–6.
Tsukube T, McCully JD, Metz KR, Cook CU, Levitsky S. Amelioration of ischemic calcium overload correlates with high-energy phosphates in the senescent myocardium. Am J Phys. 1997;273:H418–25.
Reimer KA, Lowe JE, Rasmussen MM, Jennings RB. The wavefront phenomenon of ischemic cell death: 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation. 1977;56:786–94.
Reimer KA, Jennings RB. The “wavefront phenomenon” of myocardial ischemic cell death: II. Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Lab Investig. 1979;40:633–44.
Reimer KA, Jennings RB. Myocardial ischemia, hypoxia, and infarction. In: Fozzard HA, Haber E, Jennings RB, Katz AM, Morgan HE, editors. The heart and cardiovascular system: scientific foundations, vol. II. 2nd ed. New York: Raven Press; 1992. p. 1875–973.
McCully JD, Levitsky S. Mitochondrial ATP-sensitive potassium channels in surgical cardioprotection. Arch Biochem Biophys. 2003;420:237–45.
Heyndrickx GR, Millard RW, McRitchie RJ, Maroko PR, Vatner SF. Regional myocardial functional and electrophysiological alterations after brief coronary artery occlusion in conscious dogs. J Clin Invest. 1975;56:978–85.
Gray R, Maddahi J, Bernan D, Raymond M, Waxman A, Ganz W, Matloff J, Swan HJ. Scintigraphic and hemodynamic demonstration of transient left ventricular dysfunction immediately after uncomplicated coronary artery bypass grafting. J Thorac Cardiovasc Surg. 1979;77:504–10.
Kloner RA, Przyklenk K, Kay GL. Clinical evidence for stunned myocardium after coronary artery bypass surgery. J Card Surg. 1994;9:397–402.
Rahimtoola SH. A perspective on the three large multicenter randomized clinical trials of coronary bypass surgery for chronic stable angina. Circulation. 1985;72:V123–35.
Buja LM, Vander Heide RS. Pathobiology of ischemic heart disease: past, present and future. Cardiovasc Pathol. 2016;25:214–20.
Chen C, Liu J, Hua D, Ma L, Lai T, Fallon JT, Knibbs D, Gillam L, Mangion J, Knight DR, Waters D. Impact of delayed reperfusion of myocardial hibernation on myocardial ultrastructure and function and their recoveries after reperfusion in a pig model of myocardial hibernation. Cardiovasc Pathol. 2000;9:67–84.
Lai T, Fallon JT, Liu J, Mangion J, Gillam L, Waters D, Chen C. Reversibility and pathohistological basis of left ventricular remodeling in hibernating myocardium. Cardiovasc Pathol. 2000;9:323–35.
Shah BN, Khattar RS, Senior R. The hibernating myocardium: current concepts, diagnostic dilemmas, and clinical challenges in the post-STICH era. Eur Heart J. 2013;34:1323–36.
Bax JJ, Schinkel AF, Boersma E, Rizzello V, Elhendy A, Maat A, Roelandt JR, van der Wall EE, Poldermans D. Early versus delayed revascularization in patients with ischemic cardiomyopathy and substantial viability: impact on outcome. Circulation. 2003;108:II39–42.
Beanlands RS, Hendry PJ, Masters RG, de Kemp RA, Woodend K, Ruddy TD. Delay in revascularization is associated with increased mortality rate in patients with severe left ventricular dysfunction and viable myocardium on fluorine 18-fluorodeoxyglucose positron emission tomography imaging. Circulation. 1998;98:II51–6.
Vanoverschelde JL, Wijns W, Depre C, Essamri B, Heyndrickx GR, Borgers M, Bol A, Melin JA. Mechanisms of chronic regional postischemic dysfunction in humans. New insights from the study of noninfarcted collateral-dependent myocardium. Circulation. 1993;87:1513–23.
Kim SJ, Peppas A, Hong SK, Yang G, Huang Y, Diaz G, Sadoshima J, Vatner DE, Vatner SF. Persistent stunning induces myocardial hibernation and protection: flow/function and metabolic mechanisms. Circ Res. 2003;92:1233–9.
Borgers M, Ausma J. Structural aspects of the chronic hibernating myocardium in man. Basic Res Cardiol. 1995;90:44–6.
Arai AE, Pantely GA, Anselone CG, Bristow J, Bristow JD. Active downregulation of myocardial energy requirements during prolonged moderate ischemia in swine. Circ Res. 1991;69:1458–69.
Schulz R, Rose J, Martin C, Brodde OE, Heusch G. Development of short-term myocardial hibernation. Its limitation by the severity of ischemia and inotropic stimulation. Circulation. 1993;88:684–95.
Rousou AJ, Ericsson M, Federman M, Levitsky S, McCully JD. Opening of mitochondrial KATP channels enhances cardioprotection through the modulation of mitochondrial matrix volume, calcium accumulation and respiration. Am J Physiol Heart Circ Physiol. 2004;287:H1967–76.
McCully JD, Rousou AJ, Parker RA, Levitsky S. Age and gender-related differences in mitochondrial oxygen consumption and calcium with cardioplegia and diazoxide. Ann Thorac Surg. 2007;83:1102–9.
Faulk EA, McCully JD, Hadlow NC, Tsukube T, Krukenkamp IB, Federman M, Levitsky S. Magnesium cardioplegia enhances mRNA levels and the maximal velocity of cytochrome oxidase I in the senescent myocardium during global ischemia. Circulation. 1995;92:II405–12.
Walker CA, Crawford Jr FA, Spinale FG. Myoctye contractile dysfunction with hypertrophy and failure: relevance to cardiac surgery. J Thorac Cardiovasc Surg. 2000;119:388–400.
Khabbaz KR, Zankoul F, Warner KG. Operative metabolic monitoring of the heart II. Online measurement of myocardial tissue pH. Ann Thorac Surg. 2001;72:S2227–33.
Karmazyn M. The role of the myocardial sodium-hydrogen exchanger (NHE) and its role in mediating ischemic and reperfusion injury. Keio J Med. 1998;47:65–72.
Kaplan P, Hendrikx M, Mattheussen M, Mubagwa K, Flameng W. Effect of ischemia and reperfusion on sarcoplasmic reticulum calcium uptake. Circ Res. 1992;71:1123–30.
Santulli G, Xie W, Reiken SR, Marks AR. Mitochondrial calcium overload is a key determinant in heart failure. Proc Natl Acad Sci U S A. 2015;112:11389–94.
Frolkis VV, Frolkis RA, Mkhitarian LS, Shevchuk VG, Fraifeld VE, Vakulenko LG, Syrovy I. Contractile function and Ca2+ transport system of myocardium in ageing. Gerontology. 1988;34:64–74.
Peng CF, Kane JJ, Murphy ML, Straub KD. Abnormal mitochondrial oxidative phosphorylation of ischemic myocardium by calcium chelating agents. J Mol Cell Cardiol. 1977;9:897–908.
Suleiman MS, Halestrap AP, Griffiths EJ. Mitochondria: a target for myocardial protection. Pharmacol Ther. 2001;89:29–46.
Ozcan C, Holmuhamedov EL, Jahangir A, Terzic A. Diazoxide protects mitochondria from anoxic injury: implication for myopreservation. J Thorac Cardiovasc Surg. 2001;121:298–306.
Garlid KD. Opening mitochondrial K(ATP) in the heart-what happens, and what does not happen. Basic Res Cardiol. 2000;95:275–9.
Steenbergen C, Murphy E, Watts JA, London RE. Correlation between cytosolic free calcium, contracture, ATP, and irreversible ischemic injury in perfused rat heart. Circ Res. 1990;66:135–46.
Ataka K, Chen D, Levitsky S, Jimenez E, Feinberg H. Effect of aging on intracellular Ca2+, pHi, and contractility during ischemia and reperfusion. Circulation. 1992;86:II371–6.
Tsukube T, McCully JD, Faulk EA, Federman M, LoCicero 3rd J, Krukenkamp IB, Levitsky S. Magnesium cardioplegia reduces cytosolic and nuclear calcium and DNA fragmentation in the senescent myocardium. Ann Thorac Surg. 1994;58:1005–11.
Hearse DJ, Garlick PB, Humphrey SM. Ischemic contracture of the myocardium: mechanism and prevention. Am J Cardiol. 1977;39:986–93.
Hearse DJ, Stewart DA, Braimbridge MV. Myocardial protection during ischemic cardiac arrest: the importance of magnesium in cardioplegic infusates. J Thorac Cardiovasc Surg. 1978;75:877–85.
Faulk EA, McCully JD, Tsukube T, Hadlow NC, Krukenkamp IB, Levitsky S. Myocardial mitochondrial calcium accumulation modulates nuclear calcium accumulation and DNA fragmentation. Ann Thorac Surg. 1995;60:338–44.
McCully JD, Wakiyama H, Cowan DB, Federman M, Levitsky S. Diazoxide amelioration of myocardial injury and mitochondrial damage during cardiac surgery. Ann Thorac Surg. 2002;74:2138–45.
Wakiyama H, Cowan DB, Toyoda Y, Federman M, Levitsky S, McCully JD. Selective opening of mitochondrial ATP-sensitive potassium channels during surgically induced myocardial ischemia increases necrosis and apoptosis. Eur J Cardiothorac Surg. 2002;21:424–33.
Halestrap AP, Kerr PM, Javadov S, Suleiman S. The mitochondrial permeability transition: role in ischemia/reperfusion injury. Sepsis. 1998;2:313–25.
Holmuhamedov EL, Jovanovic S, Dzeja PP, Jovanovic A, Terzic A. Mitochondrial ATP-sensitive K+ channels modulate cardiac mitochondrial function. Am J Phys. 1998;275:H1567–76.
Holmuhamedov EL, Wang L, Terzic A. ATP-sensitive K+ channel openers prevent CA2+ overload in rat cardiac mitochondria. J Physiol. 1999;519:347–60.
Murata M, Akao M, O’Rourke B, Marban E. Mitochondrial ATP-sensitive potassium channels attenuate matrix CA2+ overload during stimulated ischemia and reperfusion: possible mechanism of cardioprotection. Circ Res. 2001;89:891–8.
Jennings RB, Sommers HM, Smyth GA, Flack HA, Linn H. Myocardial necrosis induced by temporary occlusion of a coronary artery in the dog. Arch Pathol. 1960;70:68–78.
Ito H. No-reflow phenomenon and prognosis in patients with acute myocardial infarction. Nat Clin Pract Cardiovasc Med. 2006;499:506.
Buja LM. Myocardial ischemia and reperfusion injury. Cardiovasc Pathol. 2005;14:170–5.
Gross GJ, Auchampach JA. Reperfusion injury: does it exist? J Mol Cell Cardiol. 2007;42:12–8.
Barry MC, Kelly C, Burke P, Sheehan S, Redmond HP, Bouchier-Hayes D. Immunological and physiological responses to aortic surgery: effect of reperfusion on neutrophil and monocyte activation and pulmonary function. Br J Surg. 1997;84:513–9.
Pan X, Liu J, Nguyen T, Liu C, Sun J, Teng Y, Fergusson MM, Rovira II, Allen M, Springer DA, Aponte AM, Gucek M, Balaban RS, Murphy E, Finkel T. The physiological role of mitochondrial calcium revealed by mice lacking the mitochondrial calcium uniporter. Nat Cell Biol. 2013;15:1464–72.
Arroyo CM, Kramer JH, Dickens BF, Weglicki WB. Identification of free radicals in myocardial ischemia/reperfusion by spin trapping with nitrone DMPO. FEBS Lett. 1987;221:101–4.
Ferrari R, Alfieri O, Curello S, Ceconi C, Cargnoni A, Marzollo P, Pardini A, Caradonna E, Visioli O. Occurrence of oxidative stress during reperfusion of the human heart. Circulation. 1990;81:201–11.
Pacher P, Nivorozhkin A, Szabó C. (2006)Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol. Pharmacol Rev. 2006;58:87–114.
Chouchani ET, Pell VR, Guade E, Aksentijevic D, Sundier SY, Robb EL, Logan A, Nadtochiy SM, Ord EN, Smith AC, Eyassu F, Shirley R, Hu CH, Dare AJ, James AM, Rogatti S, Hartley RC, Eaton S, Costa AS, Brookes PS, Davidson SM, Duchen MR, Saeb-Parsy K, Shattock MJ, Robinson AJ, Work LM, Frezza C, Krieg T, Murphy MP. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature. 2014;515:431–5.
Ashrafian H, Czibik G, Bellahcene M, Aksentijevic D, Smith AC, Mitchell SJ, Dodd MS, Kirwan J, Byrne JJ, Ludwig C, Isackson H, Yavari A, Stottrup NB, Contractor H, Cahill TJ, Sahgal N, Ball DR, Birkler RI, Hargreaves I, Tennant DA, Land J, Lygate CA, Johannsen M, Kharbanda RK, Neubauer S, Redwood C, de Cabo R, Ahmet I, Talan M, Günther UL, Robinson AJ, Viant MR, Pollard PJ, Tyler DJ, Watkins H. Fumarate is cardioprotective via activation of the Nrf2 antioxidant pathway. Cell Metab. 2012;15:361–71.
Murphy MP. How mitochondria produce reactive oxygen species. Biochem J. 2009;417:1–3.
Chouchani ET, Methner C, Nadtochiy SM, Logan A, Pell VR, Ding S, James AM, Cochemé HM, Reinhold J, Lilley KS, Partridge L, Fearnley IM, Robinson AJ, Hartley RC, Smith RA, Krieg T, Brookes PS, Murphy MP. Cardioprotection by S-nitrosation of cysteine switch on mitochondrial complex I. Nat Med. 2013;19:753–9.
Stewart S, Lesnefsky EJ, Chen Q. Reversible blockade of electron transport chain with amobarbital at the onset of reperfusion attenuates cardiac injury. Transl Res. 2009;153:224–31.
Burwell LS, Nadtochiy SM, Tompkins AJ, Young S, Brookes PS. Direct evidence for S-nitrosation of mitochondrial complex I. Biochem J. 2006;394:627–34.
Methner C, Chouchani ET, Buonincontri G, Pell VR, Sawiak SJ, Murphy MP, Krieg T. Mitochondria selective S-nitrosation by mitochondria-targeted S-nitrosothiol protects against post-infarct heart failure in mouse hearts. Eur J Heart Fail. 2014;16:712–7.
Zweier JL, Talukder MA. The role of oxidants and free radicals in reperfusion injury. Cardiovasc Res. 2006;70:181–90.
Crompton M. The mitochondrial permeability transition pore and its role in cell death. Biochem J. 1999;341:233–49.
Halestrap AP, Clarke SJ, Javadov SA. Mitochondrial permeability transition pore opening during myocardial reperfusion- a target for cardioprotection. Cardiovasc Res. 2004;61:372–85.
McCully JD, Bhasin MK, Daly C, Guerrero MC, Dillon S, Liberman TA, Cowan DB, Mably JD, McGowan FX, Levitsky S. Transcriptomic and proteomic analysis of global ischemia and cardioprotection in the rabbit heart. Physiol Genomics. 2009;38:125–37.
Klein HH, Pich S, Lindert S, Nebendahl K, Warneke G, Kreuzer H. Treatment of reperfusion injury with intracoronary calcium channel antagonists and reduced coronary free calcium concentration in regionally ischemic, reperfused porcine hearts. J Am Coll Cardiol. 1989;13:1395–401.
Carry MM, Mrak RE, Murphy ML, Peng CF, Straub KD, Fody EP. Reperfusion injury in ischemic myocardium: protective effects of ruthenium red and of nitroprusside. Am J Cardiovasc Pathol. 1989;2:335–44.
Gumina RJ, Buerger E, Eickmeier C, Moore J, Daemmgen J, Gross GJ. Inhibition of the Na+/H+ exchanger confers greater cardioprotection against 90 minutes of myocardial ischemia than ischemic preconditioning in dogs. Circulation. 1999;100:2519–26.
Boden WE, van Gilst W, Scheldewaert RG, Starkey IR, Carlier MF, Julian DG, Whitehead A, Bertrand ME, Col JJ, Pedersen OL, Lie KI, Santoni JP, Fox KM. Diltiazem in acute myocardial infarction treated with thrombolytic agents: a randomized placebo-controlled trial. Incomplete Infarction Trial of European Research Collaborators Evaluating Prognosis post-Thrombolysis (INTERCEPT). Lancet. 2000;355:1751–6.
Théroux P, Chaitman BR, Danchin N, Erhardt L, Meinertz T, Schroeder JS, Tognoni G, White HD, Willerson JT, Jessel A. (2000)Inhibition of the sodium-hydrogen exchanger with cariporide to prevent myocardial infarction in high-risk ischemic situations. Main results of the GUARDIAN trial. Guard during ischemia against necrosis (GUARDIAN) investigators. Circulation. 2000;102:3032–8.
Zeymer U, Suryapranata H, Monassier JP, Opolski G, Davies J, Rasmanis G, Linssen G, Tebbe U, Schröder R, Tiemann R, Machnig T, Neuhaus KL, ESCAMI Investigators. The Na(+)/H(+) exchange inhibitor eniporide as an adjunct to early reperfusion therapy for acute myocardial infarction. Results of the evaluation of the safety and cardioprotective effects of eniporide in acute myocardial infarction (ESCAMI) trial. J Am Coll Cardiol. 2001;38:1644–50.
Flaherty JT, Pitt B, Gruber JW, Heuser RR, Rothbaum DA, Burwell LR, George BS, Kereiakes DJ, Deitchman D, Gustafson N. Recombinant human superoxide dismutase (h-SOD) fails to improve recovery of ventricular function in patients undergoing coronary angioplasty for acute myocardial infarction. Circulation. 1994;89:1982–91.
Downey JM. Free radicals and their involvement during long-term myocardial ischemia and reperfusion. Annu Rev Physiol. 1990;52:487–504.
Sesso HD, Buring JE, Christen WG, Kurth T, Belanger C, MacFadyen J, Manson JE, Glynn RJ, Gaziano JM. Vitamins E and C in the prevention of cardiovascular disease in men: the Physicians’ Health Study II randomized controlled trial. JAMA. 2008;300:2123–33.
Litt MR, Jeremy RW, Weisman HF, Winkelstein JA, Becker LC. Neutrophil depletion limited to reperfusion reduces myocardial infarct size after 90 minutes of ischemia: evidence for neutrophil-mediated reperfusion injury. Circulation. 1989;80:1816–27.
Hayward R, Campbell B, Shin YK, Scalia R, Lefer AM. Recombinant soluble P-selectin glycoprotein ligand-1 protects against myocardial ischemic reperfusion injury in cats. Cardiovasc Res. 1999;41:65–76.
Vakeva AP, Agah A, Rollins SA, Matis LA, Li L, Stahl GL. Myocardial infarction and apoptosis after myocardial ischemia and reperfusion: role of the terminal complement components and inhibition by anti-C5 therapy. Circulation. 1998;97:2259–67.
Baran KW, Nguyen M, McKendall GR, Lambrew CT, Dykstra G, Palmeri ST, Gibbons RJ, Borzak S, Sobel BE, Gourlay SG, Rundle AC, Gibson CM, Barron HV, Limitation of Myocardial Infarction Following Thrombolysis in Acute Myocardial Infarction (LIMIT AMI) Study Group. Double-blind, randomized trial of anti-CD18 antibody in conjunction with recombinant tissue plasminogen activator for acute myocardial infarction: limitation of myocardial infarction following thrombolysis in acute myocardial infarction (LIMIT AMI) study. Circulation. 2001;104:2778–83.
Faxon DP, Gibbons RJ, Chronos NA, Gurbel PA, Sheehan F, HALT-MI Investigators. The effect of blockade of the CD11/CD18 integrin receptor on infarct size in patients with acute myocardial infarction treated with direct angioplasty: the results of the HALT-MI study. J Am Coll Cardiol. 2002;40:1199–204.
Mertens P, Maes A, Nuyts J, Belmans A, Desmet W, Esplugas E, Charlier F, Figueras J, Sambuceti G, Schwaiger M, Mortelmans L, Van de Werf F, PSALM investigators. Recombinant P-selectin glycoprotein ligand-immunoglobulin, a P-selectin antagonist, as an adjunct to thrombolysis in acute myocardial infarction. The P-Selectin Antagonist Limiting Myonecrosis (PSALM) trial. Am Heart J. 2006;152:125.e1–8.
Mahaffey KW, Granger CB, Nicolau JC, Ruzyllo W, Weaver WD, Theroux P, Hochman JS, Filloon TG, Mojcik CF, Todaro TG, Armstrong PW, COMPLY Investigators. Effect of pexelizumab, an anti-C5 complement antibody, as adjunctive therapy to fibrinolysis in acute myocardial infarction: the COMPlement inhibition in myocardial infarction treated with thromboLYtics (COMPLY) trial. Circulation. 2003;108:1176–83.
Granger CB, Mahaffey KW, Weaver WD, Theroux P, Hochman JS, Filloon TG, Rollins S, Todaro TG, Nicolau JC, Ruzyllo W, Armstrong PW, COMMA Investigators. Pexelizumab, an anti-C5 complement antibody, as adjunctive therapy to primary percutaneous coronary intervention in acute myocardial infarction: the COMplement inhibition in Myocardial infarction treated with Angioplasty (COMMA) trial. Circulation. 2003;108:1184–90.
McCully JD, Cowan DB, Pacak CA, Toumpoulis IK, Dayalan H, Levitsky S. Injection of isolated mitochondria during early reperfusion for cardioprotection. Am J Physiol Heart Circ Physiol. 2009;296:H94–H105.
Masuzawa A, Black KM, Pacak CA, Ericsson M, Barnett RJ, Drumm C, Seth P, Bloch DB, Levitsky S, Cowan DB, McCully JD. Transplantation of autologously-derived mitochondria protects the heart from ischemia-reperfusion injury. Am J Phys Heart Circ Physiol. 2013;304:H966–82.
Cowan DB, Yao R, Akurathi V, Snay ER, Thedsanamoorthy JK, Zurakowski D, Ericsson M, Friehs I, Wu Y, Levitsky S, Del Nido PJ, Packard AB, McCully JD. Intracoronary delivery of mitochondria to the ischemic heart for cardioprotection. PLoS ONE. 2016;11:e0160889.
Bolling SF, Le B, Bove EL. Effect of ATP synthesis promoters on postischemic myocardial recovery. J Surg Res. 1990;49:205–11.
Preble JM, Pacak CA, Kondo H, MacKay AA, Cowan DB, McCully JD. Rapid isolation and purification of mitochondria for transplantation by tissue dissociation and differential filtration. J Vis Exp. 2014;91:e51682. doi:10.3791/51682.
Preble JM, Kondo H, Levitsky S, McCully JD. Quality control parameters for mitochondria transplant in cardiac tissue. JSM Biochem Mol Biol. 2014;2:1008.
Pacak AP, Preble JM, Kondo H, Seibel P, Levitsky S, Del Nido PJ, Cowan DB, McCully JD. Actin-dependent mitochondrial internalization in cardiomyocytes: evidence for rescue of mitochondrial function. Biol Open. 2015;4:622–6.
Pfeiffer ER, Wright AT, Edwards AG, Stowe JC, McNall K, Tan J, Niesman I, Patel HH, Roth DM, Omens JH, McCulloch AD. Caveolae in ventricular myocytes are required for stretch-dependent conduction slowing. J Mol Cell Cardiol. 2014;76:265–74.
Lou E, Fujisawa S, Morozov A, Barlas A, Romin Y, Dogan Y, Gholami S, Moreira AL, Manova-Todorova K, Moore MA. Tunneling nanotubes provide a unique conduit for intercellular transfer of cellular contents in human malignant pleural mesothelioma. PLoS ONE. 2012;7(3):e33093.
Kitani T, Kami D, Matoba S, Gojo S. Internalization of isolated functional mitochondria: involvement of micropinocytosis. J Cell Mol Med. 2014;18:1694–703.
Huang X, Sun L, Ji S, Zhao T, Zhang W, Xu J, Zhang J, Wang Y, Wang X, Franzini-Armstrong C, Zheng M, Cheng H. Kissing and nanotunneling mediate intermitochondrial communication in the heart. Proc Natl Acad Sci U S A. 2013;110(8):2846–51.
Stark G, Domanowits H, Sterz F, Startk U, Bachernegg M, Kickenweiz E, Decrinis M, Laggner AN, Tritthart HA. Action of ATP on ventricular automaticity. J Cardiovasc Pharmacol. 1994;24:740–4.
Piel DA, Gruber PJ, Weinheimer CJ, Courtois MR, Robertson CM, Coopersmith CM, Deutschman CS, Levy RJ. Mitochondrial resuscitation with exogenous cytochrome c in the septic heart. Crit Care Med. 2007;35:2120–7.
Pepe S, Marasco SF, Haaas SJ, Sheeran FL, Krum H, Rosenfeldt FL. Coenzyme Q10 in cardiovascular disease. Mitochondrion. 2007;7(Suppl):S154–67.
Lorita J, Soley M, Ramirez I. Epidermal growth factor protects the heart against low-flow ischemia-induced injury. J Phys Biochem. 2012;66:55–62.
Roche S, D’lppolito G, Gomez LA, Bouckenooghe T, Lehmann S, Monteromenei CN, Schiller PC. Comparative analysis of protein expression of three stem cell populations: models of cytokine delivery system in vivo. Int J Pharm. 2012; doi:10.1016/j.ijpharm.2011.12.041.
Kocher AA, Schuster MD, Bonaros N, Lietz K, Xiang G, Martens TP, Kurlansky PA, Sondermeijer H, Witkowski P, Boyle A, Homma S, Wang SF, Itescu S. Myocardial homing and neovascularization by human bone marrow blasts is regulated by IL-8/Gro CXC chemochines. J Mol Cell Cardiol. 2006;40:455–64.
Emani SM, Piekarski BL, Baird C, Kaza A, Harrild D, del Nido PJ, McCully JD. Autologous mitochondria transplantation by ventricular dysfunction following myocardial ischemia-reperfusion injury. (personal communication). n.d.
Chang JC, Wu SL, Liu KH, Chen YH, Chuang CS, Cheng FC, Su HL, Wei YH, Kuo SJ, Liu CS. Allogenic/xenogenic transplantation of peptide-labeled mitochondria in Parkinson’s disease: restoration of mitochondria functions and attenuation of 6-hydroxydopamine-induced neurotoxicity. Transl Res. 2016;170:40–56.
Lin HC, Liu SY, Lai HS, Lai IR. Isolated mitochondria infusion mitigates ischemia-reperfusion injury of the liver in rats. Shock. 2013;39:304–10.
Zhu L, Zhang J, Zhou J, Lu Y, Huang S, Xiao R, Yu X, Zeng X, Liu B, Liu F, Sun M, Dai M, Hao Q, Li J, Wang T, Li T, Lu Q. Mitochondrial transplantation attenuates hypoxic pulmonary hypertension. Oncotarget. 2016; doi:10.18632/oncotarget.10596.
Hayakawa K, Esposito E, Wang X, Terasaki Y, Liu Y, Xing C, Ji X, Lo EH. Transfer of mitochondria from astrocytes to neurons after stroke. Nature. 2016;535:551–5.
Acknowledgments
This work was supported by: The Richard A. and Susan F. Smith Foundation, President’s Innovation Award, Boston Children’s Hospital, Michael B. Klein and Family, the Sidman Family Foundation, the Bulens/Capozzi Foundation, the Boston Children’s Hospital Anesthesia Foundation, the Kenneth C. Griffin Charitable Research Fund and the Boston Investment Council. This work in part was funded by NIH 5T32HL007734 fellowship to Dr. Shin.
Disclosures
Dr. McCully, Dr. Cowan and Dr. del Nido have patents pending for the isolation and usage of mitochondria. There are no other conflicts of interest by any of the authors. The authors attest they had full freedom to explore the data, analyze the results independent from any sponsor and that they had sole authority to make the final decision to submit the material for publication.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Shin, B., Cowan, D.B., Emani, S.M., del Nido, P.J., McCully, J.D. (2017). Mitochondrial Transplantation in Myocardial Ischemia and Reperfusion Injury. In: Santulli, G. (eds) Mitochondrial Dynamics in Cardiovascular Medicine. Advances in Experimental Medicine and Biology, vol 982. Springer, Cham. https://doi.org/10.1007/978-3-319-55330-6_31
Download citation
DOI: https://doi.org/10.1007/978-3-319-55330-6_31
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55329-0
Online ISBN: 978-3-319-55330-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)