Abstract
This study investigates the outcome prediction and calculation of optimal cerebral perfusion pressure (CPPopt) in 307 patients after severe traumatic brain injury (TBI) based on cerebrovascular reactivity calculation of a moving correlation correlation coefficient, named PRx, between mean arterial pressure (ABP) and intracranial pressure (ICP). The correlation coefficient was calculated from simultaneously recorded data using different frequencies. PRx was calculated from oscillations between 0.008 and 0.05Hz and the longPRx (L-PRx) was calculated from oscillations between 0.0008 and 0.016 Hz. PRx was a significant mortality predictor, whereas L-PRx was not. CPPopt for pooled data was higher for L-PRx than for PRx, with no statistical difference. Mortality was associated with mean CPP below CPPopt. Severe disability was associated with CPP above CPPopt (PRx). These relationships were not statistically significant for CPPopt (L-PRx). We conclude that PRx and L-PRx cannot be used interchangeably.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Traumatic brain injury
- Cerebral perfusion pressure
- Cerebrovascular circulation
- Cerebral hemodynamics
- Outcome prediction
- Cerebral autoregulation
- Intracranial pressure
Introduction
The ability of vascular smooth muscle of the cerebral arteries and arterioles to respond to variations in transmural pressure, which is called cerebral vasoreactivity, can be recorded in a graded fashion in an intensive care unit setting in patients after traumatic brain injury (TBI) using different techniques and indices [1, 2] The PRx is one index of this kind, and its utility for the determination of optimal cerebral perfusion pressure (CPPopt) and its predictive power for outcome prediction in patients with TBI have been confirmed [3, 4]. PRx is calculated as the correlation coefficient between slow spontaneous changes in mean intracranial pressure (ICP) and mean arterial blood pressure (ABP), which are recorded within a frequency range of 0.008–0.05 Hz [1]. Thirty consecutive samples of 10-s averages are used to calculate moving correlation.
A new pressure reactivity index, named L-PRx, which uses slower changes in ABP and ICP, within a frequency range of 0.0008–0.016 Hz, has recently been proposed [5, 6]. In this method, 21-min averages of ABP and ICP are used. The aim of the study was to investigate, by reference to PRx performance, the utility of the L-PRx for the prediction of long-term outcome and CPPopt calculation in patients with TBI.
Materials and Methods
We retrospectively analyzed digital recordings of ABP and ICP waveforms from 307 TBI patients. Their age was 36 ± 26 years (median ± quartile range). Seventy-seven percent of patients were male (n = 235). All patients were sedated and mechanically ventilated, receiving standard neurocritical care at Addenbrooke’s neurosurgical intensive care unit between 2003 and 2009. The ICM+ system and software were used for both online data recording and offline analysis [7].
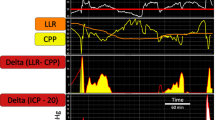
The PRx and L-PRx were each calculated as a moving linear correlation coefficient between 30 samples of time-averaged 10-s data points of ICP and ABP and 20 samples of time-averaged (60-s) data points of ICP and ABP respectively (Fig. 1).
A curve fitting method was applied to determine the optimal cerebral perfusion pressures: CPPopt(PRx) and CPPopt(L-PRx) for an individual patient. CPPopt for both indices is the individual CPP associated with the minimum value of PRx and L-PRx respectively, when plotted against CPP. This is in keeping with the mathematical model, in which a decreasing or low PRx indicates intact cerebrovascular reactivity, while an increasing PRX or positive PRx indicates impaired or lost cerebrovascular reactivity.
Logistic regression was used to examine the association between either PRx or L-PRx and outcome. Outcome was assessed using the Glasgow Outcome Scale (GOS) at the 6-month follow-up with adjustment for other predictive variables: age, CPP and Glasgow Coma Scale (GCS). The areas under the ROC curves (AUCs) were used to compare the discriminant abilities and predictive power of both indices.
Results
There was an overall good correlation between averaged values of PRx and L-PRx (R(Spearman) = 0.695, p < 0.00001). PRx, age, CPP, and GCS, but not L-PRx, are significant predictors of fatal outcome based on the Wald criterion (p < 0.05).
There was a significant difference between AUCs calculated for the PRx and the L-PRx (0.61 ± 0.04 vs 0.51 ± 0.04; z statistic = −3.26, p = 0.011). It suggests the better ability of PRx than L-PRx at predicting fatal outcome.
Individual CPPopt(PRx) was identified in 299 patients and CPPopt(L-PRx) in 300 patients. CPPopt for pooled data was 5 mmHg higher for L-PRx than for PRx. There was no statistical difference between CPPopt for PRx and L-PRx (median: 74.7 mmHg, quartile range ± 8.2 mmHg vs median: 76.9 mmHg, quartile range ± 10.1 mmHg).
Mortality was associated with mean CPP below CPPopt for PRx (χ 2 = 30.6, p < 0.00001) whereas severe disability was associated with CPP above CPPopt for PRx (χ 2 = 7.8, p = 0.005). These relationships were not statistically significant for CPPopt calculated for L-PRx.
Discussion
This study confirms that cerebrovascular reactivity can be calculated in a graded fashion in TBI patients using both PRx and L-PRX. Calculated from different frequencies they correlate well, although the PRx is superior to L-PRx for mortality prediction in TBI patients.
Santos et al. report a PRx–L-PRx correlation of R = 0.84, which is higher than in our study (R = 0.7) [6]. It must be noted, however, that their series consists of 18 patients with spontaneous intracerebral hemorrhage, which is likely to represent a less variable clinical entity than our series of 307 TBI patients. These numerical and etiological differences are likely to explain those numbers, at least in part.
In their second series of 29 TBI patients the same authors report a significant L-PRx difference between survivors and nonsurvivors, which we cannot report from our series’ analysis [5]. In another attempt to explain this difference the population differences listed above can be repeated.
Other than these attempts it is important to take a close look at the frequencies from which the indices are calculated: Spontanaeous oscillations of ABP and ICP occur in different frequencies. The PRx is calculated from oscillations that occur at a rate of 0.5–3/min (0.008–0.5Hz). These oscillations are the so-called B-waves [8]. The L-PRX is calculated from oscillations that occur at a rate of 0.05–1/min (0.0008–0.16Hz). This frequency range covers only the slow-wave range of the entire B-wave bandwidth and yields approximately 30 % of B-wave activity. This in turn leads to a 70 % loss of the B-wave bandwidth, which is not available for index calculation and may represent another cause of the differences observed.
Conclusions
The PRx predicts outcome better in patients with TBI than L-PRx. Even though the individual values of CPPopt for L-PRx and PRx were not statistically different, deviations from CPPopt obtained for PRx were more predictive than those calculated for L-PRx. It is concluded that PRx and L-PRx cannot be used interchangeably.
References
Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD (1997) Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery 41:11–17; discussion 17–19
Steinmeier R, Bauhuf C, Hubner U, Bauer RD, Fahlbusch R, Laumer R, Bondar I (1996) Slow rhythmic oscillations of blood pressure, intracranial pressure, microcirculation, and cerebral oxygenation. Dynamic interrelation and time course in humans. Stroke 27:2236–2243
Lang EW, Lagopoulos J, Griffith J, Yip K, Yam A, Mudaliar Y, Mehdorn HM, Dorsch NW (2003) Cerebral vasomotor reactivity testing in head injury: the link between pressure and flow. J Neurol Neurosurg Psychiatry 74:1053–1059
Steiner LA, Czosnyka M, Piechnik SK, Smielewski P, Chatfield D, Menon DK, Pickard JD (2002) Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med 30:733–738
Sanchez-Porras R, Santos E, Czosnyka M, Zheng Z, Unterberg AW, Sakowitz OW (2012) ‘Long’ pressure reactivity index (L-PRx) as a measure of autoregulation correlates with outcome in traumatic brain injury patients. Acta Neurochir 154:1575–1581
Santos E, Diedler J, Sykora M, Orakcioglu B, Kentar M, Czosnyka M, Unterberg A, Sakowitz OW (2011) Low-frequency sampling for PRx calculation does not reduce prognostication and produces similar CPPopt in intracerebral haemorrhage patients. Acta Neurochir 153:2189–2195
Auer LM, Sayama I (1983) Intracranial pressure oscillations (B-waves) caused by oscillations in cerebrovascular volume. Acta Neurochir 68:93–100
Conflict of Interest
ICM+ is licensed by Cambridge Enterprise Ltd. PS and MC have a financial interest in part of the licensing fee.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lang, E.W., Kasprowicz, M., Smielewski, P., Santos, E., Pickard, J., Czosnyka, M. (2016). Outcome, Pressure Reactivity and Optimal Cerebral Perfusion Pressure Calculation in Traumatic Brain Injury: A Comparison of Two Variants. In: Ang, BT. (eds) Intracranial Pressure and Brain Monitoring XV. Acta Neurochirurgica Supplement, vol 122. Springer, Cham. https://doi.org/10.1007/978-3-319-22533-3_44
Download citation
DOI: https://doi.org/10.1007/978-3-319-22533-3_44
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22532-6
Online ISBN: 978-3-319-22533-3
eBook Packages: MedicineMedicine (R0)