Abstract
Intelligent virtual agents have been successfully used for interpersonal skills training of healthcare students by enabling simulated interactions between healthcare students and virtual patient agents. However, during these interactions, students do not get the opportunity to take the perspective of the patient. Taking the perspective of the patient is essential for healthcare students to learn critical interpersonal skills like empathy. We propose having healthcare students create virtual patient agents of a particular race to provide them the opportunity to take the perspective of patients from that race, leading to increased empathy during subsequent interactions with patients of that race. We conducted a semester-long user study with 24 healthcare students to explore the effects of having them create virtual patient agents. Results indicate that healthcare students who created and interviewed virtual patients of the same race were significantly more empathetic than students who created virtual patients with a race discordant to the one they interacted with.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Embodied conversational agents
- Virtual patients
- Agents in healthcare
- Interpersonal skills training
- Healthcare education
- Empathy training
1 Introduction
For the research reported in this paper, we explore the idea of having healthcare students create and interview virtual agents of a particular race to teach them the essential interpersonal skill of empathy. Virtual agents have been widely used for interpersonal skills training in areas like military [1] and medical education [2, 3]. Specifically, the validity of using virtual patients, which are virtual agents that play the role of a patient, for training healthcare students with their interpersonal skills has been established [2]. The virtual patients used for interpersonal skills training look and speak like humans and are predominantly question-answering virtual agents [1, 2]. Traditionally, interpersonal skills training happens during interactions between healthcare students and the virtual patient. During these interactions, the virtual patients respond with pre-recorded responses to natural language questions or comments made by the healthcare student, who plays the role of the healthcare provider. A sample interaction with a virtual patient is shown in Fig. 1.
Although virtual patient-based simulations have proven to be effective for interpersonal skills training, certain specific interpersonal skills are still challenging to teach through traditional usage of virtual patients. An example of an interpersonal skill that is difficult to train using only interactions with virtual patients is empathy towards patients [4]. Empathetic healthcare professionals construct more meaningful relationships with their patients that helps them to both elicit information efficiently and provide healthcare advice effectively. To train healthcare students to be more empathetic, virtual patient simulations need to provide students the opportunity to understand the patient’s perspective [5–7]. To get the patient’s perspective, healthcare students need to think from the patient’s shoes. During simulated interactions with virtual patients, the student is still playing the part of a healthcare provider and so current virtual patient simulations do not provide an opportunity for students to take the patient’s perspective.
In order to enable healthcare students to take the perspective of the patient for empathy training, we propose having healthcare students create virtual patients themselves. While creating a virtual patient, the healthcare student is forced to think from the perspective of the patient. Our hypothesis is that by having the student take the perspective of a certain type of patient, we can train the students to be more empathetic during subsequent interactions with patients of the same type. For example, if a female Caucasian student creates a male African American virtual patient, the student has the opportunity to take the perspective of a patient from a different gender and race and so can empathize with such patients during subsequent interactions.
To explore this idea, we integrated a virtual patient exercise that involved creating and interviewing virtual patients into a health professions course. Twenty four healthcare students studying to become speech language pathologists participated in a semester-long study as part of this exercise. The students who created virtual patients and then interacted with virtual patients of the same race as the ones they created were significantly more empathetic than students who created virtual patients that were of a different race compared to the virtual patients they interacted with. We also found that this positive effect of creating virtual patients for empathy training was more pronounced when students created patients with race discordant to their own race.
2 Related Work
Galinsky and Moskowitz have extensively studied the effect of perspective-taking on racial stereotypes and prejudice [8]. They have demonstrated through their work that the positive effect of perspective-taking is effective when working with a particular group characterized by a certain feature. For example, their results indicate that one can improve their understanding of all old people by taking the perspective of one old person. Researchers have explored providing alternate perspectives using virtual agent-based simulations to alter social behavior. Yee and Bailenson found that negative stereotyping of the elderly was significantly reduced by having participants placed in avatars of old people [9]. Peck et al. have shown that putting Caucasian participants in the skin of a black avatar reduces their implicit racial bias [10]. Raij et al. introduced the concept of virtual social perspective-taking which demonstrated that taking the perspective of the patient can be beneficial for healthcare professionals and students [11]. They constructed a virtual reality experience in which after an interaction with a virtual patient, healthcare professionals were immersed into a replay of the interaction, but this time from the perspective of the patient. Results indicate that this experience changes behavior in future, similar social interactions. Similarly, Kotranza et al. [12] demonstrated that having healthcare students themselves experience the double vision suffered by a virtual patient improves their concern for the patient’s safety.
3 System Description: Virtual Patient Pipeline
Although there are several aspects to creating a virtual patient, we focus on having students construct the verbal or conversational capabilities of the virtual patient using a conversational corpus. The conversational corpus of a virtual patient consists of question-response pairs of what the students will say to the virtual patient (i.e., questions) and what the virtual patient will say back (i.e., responses). When a student poses a question or makes a comment to the virtual patient, the system searches the corpus for the most similar question and provides the paired answer. For example, if a healthcare student asked the virtual patient “Why are you here today?”, “How are you?” or “Can you tell me about your problem?” the virtual patient would respond with “It hurts at the back of my throat when I try to swallow my food”. To enable healthcare students to create virtual patients, we have built a web application called Virtual Patient Pipeline that uses techniques like crowdsourcing and reusing information from previously created virtual patients. The Virtual Patient Pipeline is a website that was built to enable users to create their own virtual patients by following a step-by-step process. The application has the following four main steps:
Step 1 – Name and Image:
Authors choose a name for the patient and write out a short description about the virtual patient. They also choose an image that is most representative of the virtual patient they want to create from an array of headshot images. The array of headshots include images of characters with different races, age and gender. Sample headshot images are shown in Table 1 in Sect. 4.2.
Step 2 – Virtual Patient Template:
In this step, authors fill out a virtual patient template - a form that has a pre-populated set of questions and allows authors to fill in just the response for each set of questions in order to create an initial version of the virtual patient. The response field is left blank for the student to fill out by playing the role of the patient. Examples of questions in the virtual patient template are name, age, marital status, medications and prior medical history. The patient template that was used in the course integration described in this paper had 135 question-response pairs. All pre-populated questions in the patient template have been gathered by mining questions from previously created virtual patients of similar pathologies.
Step 3 – Patient Training:
In this training step, students can interview the patient that has been created through the process in Step 1 to add more information to the patient. The interviewing process involves the creator typing questions to the virtual patient and receiving responses. While interviewing the patient, students can correct any incorrect responses or add new questions and responses to their patients. Since the template might not have all the questions that the student wants their patient to be able to answer, this step allows them to add new question-response pairs.
Step 4 – Crowdsourcing:
After the student has completed training their patient, he/she can share the virtual patient with his/her friends and acquaintances. While others interview the virtual patient, they will have the opportunity to flag any responses that they think are wrong. These incorrect responses are gathered in a list along with any questions to which the virtual patient did not know an answer to during the interview. This list can then be reviewed by the students and the virtual patient improved by correcting incorrect responses and adding responses to unanswered questions.
4 Experimental Study
4.1 Population
Participants in the study were speech and language pathology students taking a course titled “Dysphagia Management” during the spring of 2014 at the University of Florida. Dysphagia is a medical condition where the patient has difficulty swallowing food or liquids. There were 26 graduate students registered for the course. The study was offered as an extra-credit exercise as part of the course and students volunteered to participate. The extra-credit was 5 points on the final exam of the course. All but one student volunteered to participate in our study. One student failed to complete all the requirements for the study, so the data from 24 participants was analyzed [n = 24]. The course was taught for four months between January and April 2014 and the study ran throughout the duration of the course. All the students were either in the first or second semester of their graduate studies for a Master’s in Speech Language Pathology. In the future, as speech language pathologists, these students will have to interview real patients, some of them suffering from dysphagia. Hence this virtual patient exercise and the interpersonal skill of empathy is very relevant to this population.
On the first day of class, all the students were asked to fill out a background survey form that asked for demographic and educational information. All but one participant were female (96 %). The average age of the participants was 24.24 (S.D. = 4.06). All but two participants were Caucasian (92 %). One participant was Asian and another one was a Pacific Islander. As can be seen from these numbers, we have a fairly homogenous group of predominantly Caucasian female participants with an average age of 24. This composition is reflective of the general composition of speech language pathologists and students around the country. 84 % of the students reported that they have not received any prior interpersonal skills training. According to the instructor of the course, the students had very minimal exposure to real patients.
4.2 Study Design
Although the exercise lasted an entire semester, we focus only on the first three tasks that were completed by the participants. The remaining tasks are beyond the scope of this paper. The first three tasks that students completed in the order of completion are:
-
1.
Interview a virtual dysphagia patient - (last week of January)
-
2.
Create a virtual dysphagia patient - (first two weeks of February)
-
3.
Interview a virtual dysphagia patient - (third week of February)
The virtual dysphagia patient interviews (tasks 1 and 3) were used as metrics to evaluate the effect of creating a virtual patient (task 2). On the first day of class, a 30-min tutorial was provided to the entire class demonstrating a virtual patient interaction and the steps involved in creating a virtual patient using the Virtual Patient Pipeline.
Virtual Patient Interviews:
All 24 participants participated in interviews with two virtual dysphagia patients. The two virtual patients interviewed were of the same gender but different race and medical diagnoses. One of the virtual patients was a Caucasian male while the other was an African American male. The order in which the virtual patients were interviewed was randomized. Half the participants interviewed the Caucasian male first and the African American male second and the other half interviewed the patients in the opposite order. Information about the two virtual patients interviewed by the participants is presented in Table 1.
The interviewing process involved students typing in questions to ask to the virtual patient and the virtual patient responding to the questions with both text and audio responses. The interaction interface is shown in Fig. 1. The virtual patient was represented as a 3D character with simple idle animations like blinking and breathing. The virtual patient had appropriate lip synching animations for the audio responses. The audio for the two virtual patients’ speeches were recorded by voice actors of the appropriate age and gender corresponding to the virtual patient. Students were instructed to interview each virtual patient for at least 10 min.
Virtual Patient Creation:
All 24 participants also individually created a virtual dysphagia patient in between the two virtual patient interviews. The participants were asked to create a 55-year old male virtual patient suffering from dysphagia due to a left brainstem stroke. Half the students were asked to create a Caucasian virtual patient and the other half were asked to create an African American virtual patient. Other than the ethnicity, age, gender and diagnosis which was given to them, the students were instructed to come up with all the other information for the virtual patient on their own. Due to time constraints, participants completed only the first three steps of the Virtual Patient Pipeline that is explained in Sect. 3.
To summarize, in task two all the 24 participants created either a Caucasian or African American male virtual patient and then in task three interviewed a Caucasian male virtual patient or an African American male virtual patient. Comparing the race of the virtual patient they created and the race of the second virtual patient they interviewed, the participants could be divided into two groups – concordant group and discordant group. The concordant group’s second virtual patient was of the same race as the virtual patient they created. The discordant group’s second virtual patient was of a different race than the virtual patient they created.
4.3 Metrics
The two virtual dysphagia patient interviews were used to measure the difference in empathy between the concordant and discordant groups and was measured using empathetic opportunities. An empathetic opportunity is an instance during a virtual patient interview where the virtual patient expresses a concern or asks a question to which the participant is expected to respond with empathy. For example, during an interaction with a patient suffering from stomach pain, the patient could ask “My brother recently died of peptic cancer. I’m afraid that this pain I’m having could be a symptom of stomach cancer. Am I going to die like my brother doctor? ”. The participant is expected to respond empathetically to this question. Each virtual patient had one empathetic opportunity that was spoken by the virtual patient approximately 7 min into the interview. While the virtual patient spoke the empathetic opportunity speech, a dialog box popped up that had the text for the opportunity and also a text area where the student could enter their response to the empathetic opportunity. The student had to respond to the opportunity to proceed with the interview. When the student submitted their typed response to the empathetic opportunity, the patient responded with a generic “Thank you, doctor” statement. The empathetic opportunities included in both the patients are listed in Table 1.
The participant’s responses to these empathetic opportunities were rated by three expert empathetic raters trained on the Empathic Communication Coding System (ECCS) scale. The ECCS scale is an established measure for rating healthcare provider’s empathy during an interaction with a patient [13]. The ECCS scale has seven levels of empathy for responses to empathetic opportunities. These seven levels are described in Table 2 along with examples of actual responses from study participants corresponding to each level of empathy. The ECCS scale has been successfully used to measure and rate empathy during virtual patient simulations [14]. The three raters were trained using empathetic opportunities from other virtual patient interactions prior to the actual rating of the responses from the experimental study. The rating for each response was the average rating from the three raters.
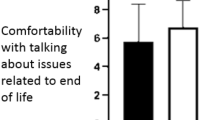
5 Results
The ratings based on the ECCS scale by the three raters had high inter-rater reliability measured by Intraclass Correlations (ICC) ratings of 0.925 and 0.862 for the Caucasian and African American virtual patient ratings respectively. Since the ratings are ordinal and not normally distributed, Mann-Whitney U-tests were run to compare ratings between the concordant and discordant groups at each virtual patient interview. Results from this analysis are plotted in Fig. 2. There were no significant differences in the empathy ratings between the two groups during the first virtual patient interview. Empathy ratings during the second patient interview for concordant group participants (Mdn = 4.0) were significantly higher than for discordant group participants (Mdn = 3.67), U = 34.5, z = −2.181, p < 0.05, r = −0.45. Also, a within-subjects Wilcoxon signed-rank test was used to compare the ratings within each group. No significant differences were observed between the interviews within both the groups.
Mann-Whitney U-tests were run to compare the empathy ratings of the concordant and discordant groups depending on whether the second virtual patient was Caucasian or African American. When the second virtual patient was African American [n = 12], there was a significant difference between the empathy ratings of the race concordant (Mdn = 5) and discordant (Mdn = 3.67) groups, U = 2.0, z = −2.234, p < 0.05, r = −0.70. When the second virtual patient was Caucasian [n = 12], there was only a marginally significant difference between the empathy ratings of the race concordant (Mdn = 4) and discordant (Mdn = 3.33) groups, U = 9.0, z = −1.774, p = 0.07, r = −0.51.
6 Discussion
Since there were no significant differences between the concordant and discordant group empathy ratings during the first patient interview and the only difference in treatment for the two groups was whether they created a race concordant or discordant virtual patient, we conclude that the reason for enhanced empathy was the process of creating a race concordant virtual patient. This validates the applicability of virtual patient creation as a tool for empathy training.
It was observed that there was a significant difference between the empathy ratings of concordant and discordant groups when the second virtual patient was African American and only a marginal significance when the virtual patient was Caucasian. All the 12 participants for whom the second virtual patient was African American were Caucasian. So creating and interviewing an African American virtual patient would mean taking the perspective of a patient population discordant to their own race. These results indicate that the effect of creating a virtual patient might be more pronounced when creating and interviewing a virtual patient that is race discordant to the student. These results are in-line with findings by Peck et al. in their study [10] and also in the psychosocial experiments conducted by Galinsky and Moskowitz [8].
In addition to the empathy training benefits presented above, we would like to present two additional contributions in this paper:
Feasibility for Virtual Patient Creation by end Users in an Educational Environment:
We would like to highlight that the experimental study was conducted in a real-world educational environment as part of a health professions course and present this as one of the contributions of this paper. Although prior experiments have investigated the feasibility of having healthcare students create virtual patients [15], the contribution of this paper is in the setting of empathy training. This demonstrates that virtual agent creation exercises can be integrated into educational environments, as part of coursework, for teaching interpersonal skills.
Virtual Patients Created are Educational Artifacts:
In the process of creating virtual patients for the sake of learning interpersonal skills, students are actually also creating virtual patients that can be used for training other students in the future. Each virtual patient created by these students has a different personality, backstory and background information that the students have come up with. Interestingly, the two virtual patients used for interviews in the described study were also created by students back in 2011 as part of a virtual patient creation exercise.
7 Conclusion
In this paper, we have explored the idea of healthcare students creating virtual patients for learning empathy. Although the idea has been introduced in the context of virtual patients and explored in the domain of healthcare education, the idea can be extended to domains like social training, specifically for gaining cultural competency. A person can create a virtual agent representing a particular culture and others belonging to the target culture can then interact with the agent created and provide feedback. The feedback will help the creator address any misconceptions or stereotypes that the creator has about the target culture.
As future work, we would like to explore other categories in which interpersonal skills through virtual patient creation can be useful like gender, age, ethnicity etc. Our eventual goal is to make virtual patient creation an enjoyable and effective tool for healthcare students to learn important skills like empathy. With more and more successful completions of virtual patient creation exercises, we would also be able to build a library of virtual patient agents that can be used for both research and educational purposes around the world.
References
Swartout, W., Gratch, J., Hill, R.W.W., Hovy, E., Marsella, S., Rickel, J., Traum, D.: Toward virtual humans. AI Mag. 27(2), 96 (2006)
Johnsen, K., Raij, A., Stevens, A., Lind, D.S., Lok, B.: The validity of a virtual human experience for interpersonal skills education. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems - CHI 2007, p. 1049 (2007)
Johnsen, K., Dickerson, R., Jackson, J., Shin, M., Hernandez, J., Stevens, A., Raij, A., Lok, B., Lind, D.S.: Experiences in using immersive virtual characters to educate medical communication skills. In: IEEE Proceedings on Virtual Reality (VR 2005), pp. 179–324 (2005)
Deladisma, A.M., et al.: Do medical students respond empathetically to a virtual patient? Am. J. Surg. 193(6), 756–760 (2007)
Maxfield, H., Delzell, J.E., Chumley, H.: Eliciting the patient’s perspective: does experience or type of case make a difference? Patient Educ. Couns. 82(2), 222–225 (2011)
DasGupta, S., Charon, R.: Personal illness narratives: using reflective writing to teach empathy. Acad. Med. 79(4), 351–356 (2004)
Moore, R.J., Hallenbeck, J.: Narrative empathy and how dealing with stories helps: creating a space for empathy in culturally diverse care settings. J. Pain Symptom Manag. 40(3), 471–476 (2010)
Galinsky, A.D., Moskowitz, G.B.: Perspective-taking: decreasing stereotype expression, stereotype accessibility, and in-group favoritism. J. Pers. Soc. Psychol. 78(4), 708–724 (2000)
Yee, N., Bailenson, J.: Walk a mile in digital shoes: the impact of embodied perspective-taking on the reduction of negative stereotyping in immersive virtual environments. In: Proceedings of PRESENCE, pp. 147–156 (2006)
Peck, T.C., Seinfeld, S., Aglioti, S.M., Slater, M.: Putting yourself in the skin of a black avatar reduces implicit racial bias. Conscious. Cogn. 22(3), 779–787 (2013)
Raij, A., Kotranza, A., Lind, D.S., Lok, B.: Virtual experiences for social perspective-taking. In: 2009 IEEE Virtual Reality Conference, pp. 99–102 (2009)
Kotranza, A., Cendan, J.C., Johnsen, K., Lok, B.: Virtual patient with cranial nerve injury augments physician-learner concern for patient safety. J. Bio-algorithms Med-Syst. 6(11), 25–34 (2010)
Bylund, C.L., Makoul, G.: Examining empathy in medical encounters: an observational study using the empathic communication coding system. Health Commun. 18(2), 123–140 (2005)
Borish, M., Cordar, A., Foster, A., Kim, T., Murphy, J., Lok, B.: Utilizing real-time human-assisted virtual humans to increase real-world interaction empathy. In: Kansei Engineering and Emotion Research (KEER) (2014)
Halan, S., Lok, B., Sia, I., Crary, M.: Virtual agent constructionism: experiences from health professions students creating virtual conversational agent representations of patients. In: IEEE Proceedings, International Conference on Advanced Learning Technologies, pp. 249–253 (2014)
Acknowledgements
The authors would like to thank Dr. Andrea Kleinsmith for her advice and assistance in conducting the study reported. This work was made possible by a Veterans Administration Rehabilitation Research and Development Grant (Grant ID: B0339-R).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this paper
Cite this paper
Halan, S., Sia, I., Crary, M., Lok, B. (2015). Exploring the Effects of Healthcare Students Creating Virtual Patients for Empathy Training. In: Brinkman, WP., Broekens, J., Heylen, D. (eds) Intelligent Virtual Agents. IVA 2015. Lecture Notes in Computer Science(), vol 9238. Springer, Cham. https://doi.org/10.1007/978-3-319-21996-7_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-21996-7_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-21995-0
Online ISBN: 978-3-319-21996-7
eBook Packages: Computer ScienceComputer Science (R0)