Abstract
Compassionate end-of-life care matters deeply for patients and their caregivers, but studies continue to demonstrate ways in which physicians fall short. Despite specific training during medical school, many patients report lack of empathy in their providers with respect to end-of-life conversations. This is likely because empathy is simply hard to teach. Numerous activities have been tried to combat the decline in empathy during medical training with little to moderate success. However, virtual reality, which allows users to viscerally experience anything from another person’s point of view, could be a game changer for building empathy within medicine. This type of perspective-taking has previously shown to improve understanding, reduce biases, facilitate empathy, and promote prosocial behaviors. In this pilot study, virtual reality was used to allow students to “become a patient” virtually embodying their daily activities, symptoms, and interactions with caregivers. Using the Embodied Labs modules, first-year medical students were able to experience first-hand having a terminal illness, being told no further treatments are available and witnessing loved ones’ reactions. Data generated through surveys and reflections indicated a high level of place illusion, plausibility, and embodiment of users. This high level of immersion generated an increase in comfortability with talking about end-of-life issues, produced a better understanding of what patients and their families experience, and promoted a change in the way students would approach clinical skills. Analysis of reflections indicated a high level of empathy for the patient and his family members. Overall, the activity was highly received by students as a valuable learning activity. As such, we propose that virtual reality could be a useful pedagogical tool to facilitate empathy and clinical skills within medical education.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Empathy is the capacity to understand what another person is experiencing from within the other person's frame of reference, i.e., the capacity to place oneself in another’s shoes [1]. General empathy is considered to have both cognitive and emotional aspects. The cognitive aspect of empathy refers to the ability to comprehend another person’s inner experience and the capacity to understand the world from the other person’s viewpoint. The emotional aspect of empathy refers to the ability to share someone else’s experiences and feelings [2, 3, 4]. With respect to patient care, Hojat argues that clinical empathy relies predominantly on the cognitive (rather than an emotional) attribute encompassing understanding (rather than feeling) of experiences, concerns, and perspectives of the patient, combined with a capacity to communicate this understanding and an intention to help [5]. Neumann et al. argues that clinical empathy is a fundamental determinant of quality in medical care because it enables the clinician to fulfill key medical tasks more accurately, thus leading to enhanced health outcomes [6]. In fact, the importance of physician empathy is well documented in the literature with notable positive impacts on patient satisfaction, overall clinical outcomes, and litigation proceedings [5]. As such, strengthening the capacity for empathy in physician trainees has become a recent focus within medial education with various types of curricular interventions producing moderate success [7, 8].
Experiential learning, described by Kolb, relies on a framework grounded in experiencing, reflecting, integrating, and applying new knowledge into one’s work [9] which may be an effective pedagogy for enhancing empathy. Previous literature has detailed the use of experiential learning to increase empathy through patient immersion experiences, role-play, and case-based learning. In a randomized controlled trial, Bunn and Terpstra [10] exposed participants to a simulated auditory hallucination while simultaneously asking them to complete a psychiatric interview, cognitive testing, and social interactions. The group who experienced the simulation had increased levels of self-reported empathy. Another study used an “aging game” that simulates the loss of vision, hearing, manual dexterity, mobility, continence, independence, and dignity that occurs with advancing age [11]. Participants had a significant improvement in attitudes toward caring for elderly and in empathy towards elderly patients following the aging game. Chen et al. utilized a video game where students played the role of parents of a child with cancer navigating various environments and tasks involved in the child’s care [14]. After playing the game, students had an increase in scores on a modified version of the Jefferson Scale of Physician Empathy.
Virtual reality (VR) allows for enhanced experiential learning because it facilitates the combination of multimodal sensory and motor simulations with first person perspective visual input. Unlike traditional media, the high level of immersion, feeling of presence, and the ability to vividly experience any situation from any perspective allow VR to be a highly effective perspective-taking medium [12]. Slater posits that the level of immersion, and therefore impact, of a virtual reality experience is determined by the participants’ belief that they are actually there (place illusion) and the belief that what appears to be happening is really happening (plausibility) [13]. As such, place illusion corresponds to the feeling of “being there” or presence in the virtual environment which depends upon the range of sensorimotor contingencies supported by the system (i.e., the degree of technological immersion). Plausibility refers to the illusion that the events happening virtually are indeed happening, and it is influenced by factors such as the extent to which the virtual environment responds to the presence of the user and the general credibility of the scenario. By leveraging immersion and body transfer within virtual reality, perspective taking and understanding is enhanced [14]. As such, VR has been described as the “ultimate empathy machine” since it allows people to viscerally experience anything from another person’s point of view [15]. In comparison studies of content presented in a 2-dimensional format verses a 3-dimensional virtual environment, VR resulted in greater engagement and a higher level of empathic perspective taking and empathic concern for the character featured in the story [16]. In an extensive study, Herrerra et al. showed that the positive effect of traditional perspective-taking on perceptions of the homeless (i.e., lack of dehumanization and better attitudes) were prolonged with the use of VR [12]. Additionally, participants of VR reported feeling more connected and empathetic toward the homeless and engaged in more long-term supportive behaviors. Similarly, content viewed on a VR platform, when compared against a traditional two-dimensional video media platform, enhanced empathy, increased responsibility, and instigated a higher intention to donate money and volunteer time towards a social cause [17]. With respect to empathy toward individuals with medical conditions, similar results have been found. Experiencing symptoms associated with a panic attack increased empathy, understanding, and sensitivity for panic attack sufferers after undergoing the VR experience [18]. When medical students virtually embodied a 74-year-old African American man with macular degeneration and hearing loss, their level of understanding and empathy towards age-related conditions improved [19, 20]. In a different study, using the same virtual lab, medical students not only increased their empathy but also decreased their usage of stereotypical words and showed a greater interest in geriatrics as a career choice [21].
Within medicine, empathy is often lauded as a critical component of end-of-life discussions. Throughout the process of dealing with suffering, it has been argued that the core task of the clinician must be to understand the patient's response to the serious news and the meaning ascribed to it. This understanding comes from a detailed and tolerant exploration of the patient’s unique experience of suffering [22]. Despite the inclusion of end of life curricular in most medical schools, healthcare providers report a lack of training in end-of-life care and limited opportunities to learn about the dying process in home settings where most prefer to die [23]. Therefore, we sought to explore the value of a novel, immersive VR experience whereby medical students embodied a terminally ill patient receiving serious news and progressing to home hospice. Specifically, the goals of this pilot study were to assess the utility of VR as a pedagogical tool, its effectiveness on knowledge and confidence of end of life care practices, and its impact on student empathy.
Methodology
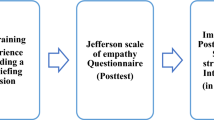
This pilot project was incorporated into the Mechanisms of Disease course occurring in the second semester of the first year of which 145 medical students (74 males/71 females) were enrolled. This module coincided with their clinical skills curriculum in which they learned and practiced breaking serious news to standardized patients. Previously, students had an introduction to ethics, palliative care, and hospice. This was a pre-post single arm study in which students were required to complete a pre-survey, engage in virtual reality labs, and complete a post-survey to receive credit for the activity which comprised one percent of their total course points. The entire activity took less than 30 min. The anonymous pre-survey (Table 1) consisted of a brief, five question online survey including Likert and multiple-choice questions related to comfortability with end-of-life discussions, experience with end-of-life care, feelings associated with receiving a terminal diagnosis, view of hospice care, and role of hospice team members. Data from the pre-survey was aggregated by the software company and reported back to the researcher.
Next, students completed two brief virtual reality labs using the Embodied Labs software with Oculus Rift goggles [24]. Embodied Labs is a virtual reality company that produces different interactive “labs” which allows individuals to walk in the shoes of patients with different diseases. In this study, students embodied Clay Crowder, a 66-year-old veteran who is diagnosed with terminal, stage IV lung cancer. During the first module, “Receiving a Terminal Diagnosis,” students virtually become Clay as he goes with his wife and daughter to his oncologist to determine the results of his latest round of chemotherapy. The family expresses hope for good news, but then unfortunately is told that the cancer was unresponsive. During the office visit, the family expresses confusion, frustration, and pushes for other options. The physician weighs the options but ultimately concludes there are no feasible remaining treatments. Clay can only communicate using text on his phone, so most of the communication is dominated by the family members. However, he does ask the physician how long he has left to live and she estimates no more than 6 months. Themes touched on in this module are effective communication skills when delivering serious news to the patient and with the family, changing adult and child relationships when healthcare decisions are made, veteran health issues, and cultural competency.
During the second module, “Transitioning to Home Hospice” Clay has a fall and is in the emergency room with his other daughter. His daughter and nurse are having a conversation about his doctor’s recommendation for hospice care. Initially, the daughter wants a second opinion but then probes more about the details and experience of hospice. The nurse gives her personal experience with hospice and asks Clay what a good day for him would be, suggesting that is the goal of hospice care. In the next scene, Clay is at home in a wheelchair and awakes to a conversation about him and his care occurring between his wife, daughters, and social worker. He expresses to his family that he has been in the company of a blue heron which turns out to be a hallucination he experiences towards the end of the scene. Throughout this module, students were exposed to interprofessional teams, information about hospice, effective communication during family conflict and resolution, and end-of-life symptom presentation, management, and control.
Immediately following each lab, students were asked to complete a post-survey (Table 1). Open-ended questions were categorized as first-person immersion if pronouns such as “I,” “my,” or “we” were used to answer the question as if the participants were actually Clay (the patient) independently by two separate researchers. Responses that included “the patient,” “his,” or “Clay” were reported as detached from the experience. Comments that only referred to the medical scenario without mention of pronouns or the patient were considered neutral language. Data was downloaded from Blackboard by the course director and scrubbed of any student identifiable information before utilized for the research.
All data were analyzed using Excel and Prism Graphpad software Version 8.0.0 for Windows, GraphPad Software, San Diego, CA, USA, www.graphpad.com. Descriptive statistics including mean and standard deviations were calculated. Data from identical questions on the pre- and post-surveys were compared using a Welch’s t-test due to unequal sample sizes. Open-ended comments were automatically thematically analyzed using the quick word frequency query and automated insights function in QSR International Pty Ltd. (2018) NVivo (Version 12 Plus) software, https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home. All data associated with this study was collected and analyzed with approval and compliance from the Institutional Review Board.
Results
End-of-Life Care and Hospice
One hundred forty-five first-year medical students completed the pre-survey (100%). Two students with severe visual deficits were unable to see clearly using the VR goggles and instead just viewed the modules on the computer screen. Two students failed to complete the modules due to motion sickness or fear on induction of a migraine. Those students and three others did not complete the post-survey, accounting for a 95% completion rate of the entire activity.
The primary focus of the VR labs was end-of-life discussions, patient care and transitioning to home hospice. Students in general came in the session with a positive view of hospice care (mean of 8.10) when asked on a 10-point Likert scale with 1 being negative and 10 being positive. However, they were less knowledgeable about the roles of nurses, social workers and chaplains in a hospice team. When asked to correctly match the roles of each team member, 50% correctly matched the nurse, 52% the social worker, and 54% the chaplain. Prior to the lab, students were asked about their level of experience in dealing with issues surrounding end of life care. On a 10-point Likert scale, with 10 being the most experienced, students reported an average of 4.06. Students were also asked about comfortability with talking about issues related to end-of-life care. The average student response was 5.79 on a Likert scale of 1–10 with 10 being most comfortable prior to the VR experience. After completion of both VR modules, students reported a statistically significant increase in their comfortability (6.757, p < 0.0001) (Fig. 1).
VR Experience
To evaluate the level of immersion achieved within the VR experience, open-ended comments were analyzed to determine the extent of place illusion and plausibility using the real-as-if-framework [23] within the VR scenario. Representative answers to the questions “How did it feel to receive information about the diagnosis from Dr. Chatterjee?” are shown in Table 2. Fear and helplessness were the most common themes that emerged after receiving the diagnosis. When the statements about receiving the diagnosis were analyzed for person-centeredness, the majority (74%) of students answered the question in first-person as Clay utilizing pronouns such as “I” or “my” or “we.” Only 16% of students answered in a detached voice referring specifically to “the patient” or “Clay.” Eight percent of the students gave a neutral answer where the tone related specifically to the practice of delivering serious news without mention any pronouns. Representative comments are shown in Table 3 to the question “How did you feel when the nurse told you that your chart said that hospice care was the recommendation of your doctor?” The most common themes from these responses included relief of not being a burden to family members, dread, frustration with my family and comfort. Similar results on the use of first-person language were noted.
Embodiment, Understanding, and Empathy
Given the consistent comments supporting place illusion and plausibility coupled with the overwhelming first-person language, we next explored the effect of embodiment afforded by the VR lab. Embodiment is described as the virtual body (in this case, Clay) being portrayed co-located with the real physical body of the student user [13]. As such, when the user lifts his/her hands in front of their eyes in the physical world, they see the same movement in the virtual world portrayed as the hands of Clay Crowder. Since the level of embodiment has been shown to positively correlate with empathy [25, 26], we next investigated the users empathy. Halpern argues that empathy involves using resonance to attune another’s emotional views through imagination work and that we can cultivate empathy in students by developing their curiosity about other people’s distinct experiences [27]. To get at this cognitive domain of empathy, we asked students to reflect prior to the VR lab. Students were told they were about to embody a man with a terminal cancer diagnosis and then asked to think about how they might feel if they were told they have a disease that is incurable. They were asked to select from a list of feelings and allowed to choose as many as they felt. Responses are shown in Fig. 2. The most common responses reported were feelings of being scared, sad, helpless, and angry.
Affective empathy is when providers internalize the emotions a patient feels and truly feels those emotions themselves. In essence, it is the ability to vicariously experience the emotional experience of others, as well as, the correct identification of one’s own corresponding emotional state perhaps via self-reflection and insight [28]. Examples of this initiated by virtually embodying Clay are certainly reflected in the comments presented in Tables 2 and 3. However, to investigate this further, we asked students to describe any symptoms they might have felt as Clay while participating in the VR lab. As shown in Table 4, student were able to not only experience emotional responses but also reported physical symptoms they experienced as Clay such as increased heart rate, difficulty breathing/speaking, pain, fatigue, loss of alertness, and nausea. However, only 65.3% of students said they were emotionally affected by “being” Clay during the VR lab.
Bellet and Maloney suggest that to be empathetic “the physician does not have to experience the intense feelings or emotions that grip the patient … but only to understand these feelings and relate to them while maintaining a sense of self.” [29] This capacity for understanding another person's feelings is the foundation of the physician–patient relationship. After completing the labs as Clay, 84.2% of students felt like they had a better understanding of what terminal cancer patients’ experience. Interestingly, 90.3% also said they thought they also had a better understanding of what family members of a terminal cancer patient experiences. Since empathetic responses are linked to prosocial behaviors [30], we attempted to see if this experience would have an impact on their clinical skills. While we have not carried out this experiment yet, we did ask the participants if this VR experience made them think about the way they would approach their own clinical skills and 92.5% of them responded yes.
In general, students responded positively to the overall educational activity and enjoyed the addition to the medical curriculum. On a scale of 1–5 students rated the VR lab as a 4.15 and 92.5% reported it as a valuable learning experience. Additionally, 84% of students said they would like to see more virtual labs incorporated into the curriculum in the future. On the end of the course evaluations, the VR lab was consistently ranked as one of the top three learning experiences within the 8-week course.
Discussion
In summary, we report positive effects of an immersive VR experience in which medical students virtually embodied a patient with a terminal illness and experienced his interactions with family members and various members of the care team as he transitioned to home hospice. The experience resulted in students’ self-reported increase in comfortability with talking about end-of-life issues. This content is important and relevant as numerous reports have demonstrated shortcomings in end-of-life care curricula for medical students [31, 32]. Additionally, the impact and credibility of the VR experience was documented in students’ statements demonstrating plausibility, place illusion, and embodiment. These key tenants of immersive VR storytelling helped promote the perception that the story was real and facilitated user empathy [25]. Empathy was further documented through the frequent use of first-person language in student reflections of the experience. At the conclusion of the activity, most students reported having a better understanding of what terminal cancer patients experience, as well as the experience of the family. Overall students found the activity to be a highly valuable learning experience. Thus, within less than 30 min of class-time, we were able to model delivering serious news, improve student comfort with end-of-life discussions, augment their understanding of terminal cancer patients and their families, enhance their empathy, and potentially change their approach to clinical skills.
Empathy is a major element of professionalism in medicine and has been described as the most frequently mentioned personal quality of the humanistic physician [33]. Therefore, the erosion of students’ and residents’ humanistic attitudes during their clinical training has been a source of concern for medical educators. Research suggests that while most students enter training with a high capacity for empathic engagement with patients, this capability erodes as students enter clinical training. While mixed data exist, several longitudinal studies report that empathy among medical students tends to decline in the third year of medical school [34]. Reasons for this include an emphasis on emotional detachment and clinical neutrality, over-reliance on technology that limits human interactions, and inappropriate treatment of medical students [35]. Other authors have argued that a hidden curriculum of emotional detachment with inadequate role models have driven this decline in empathy [36].
In a large-scale study with practicing physicians, researchers concluded that regulating one’s emotions through perspective-taking was pivotal to the adaptive experience of empathy in clinical practice [37]. Thus, curricular interventions targeting perspective-taking, such as role-play, are likely to and have been shown to facilitate empathy in trainees [38].
Moving perspective-taking exercises into immersive virtual environments is a new area of research that shows great promise and allows for engagement in experiences which would typically be prohibitively difficult or impossible [39]. Compared to training with people (e.g., simulated patients, role plays, patient encounters), VR software may be more reliable, economical, and easier to disseminate. VR also helps eliminates common methodological problems such as the experimental control–mundane realism trade-off, lack of replication, and unrepresentative sampling [40]. The beauty of VR is it allows users to vividly and viscerally experience any situation as if it were happening to them from any perspective. As such, VR has been shown to invoke empathy through a process of total embodiment which allows users to virtually step into the shoes of others and see the world from their perspective [12]. Similar to our results, other studies where students virtually embodied a patient with advanced macular degeneration and high-frequency hearing loss demonstrated an increase in empathy, a decrease in stereotypical biases and an impact on career interests [19,20,21]. In a longitudinal study, Bailenson and Yee [41] found that, over time, VR users change the way they behave inside virtual environments and suggest that the novelty of VR technology has an effect on virtual social interactions and prosocial behaviors.
Empathy generated through the unique affordances of virtual environments can promote prosocial behavior when leveraged. Data has shown that even brief virtual interventions can increase environmental awareness, reduce racial bias, and enhance general altruistic behavior [42]. Within medicine, empathy has been linked to dutifulness [43], and it has been reported that training physicians in empathy can improve their communication skills [44, 45]. Data within this study further suggests that training within virtual environments may also improve the clinical skill of delivering serious news. Our data suggested a small but significant increase in comfortability when talking about end of life issues. The small change is likely due to the fact that this was a singular brief intervention; it is likely that a longitudinal program could have achieved a larger response. While students reported embodying a terminal cancer patient made them think about how they would approach the task of breaking serious news, we have yet to test this effect. Fisher argues that VR does not facilitate a direct relationship between a user and an experience’s subject in reality to achieve empathy and instead, users end up empathizing directly with a VR designer and their presented representations, not their subjects in lived reality [46]. Therefore, it would be interesting to challenge this perception by combining training in virtual reality with clinical skills practice and assessment. Future studies with standardized patients or real patients could provide valuable insight into the transferability of this experience. As empathy has also been identified as a protective factor against the stress experienced by clinicians and as a potential factor for their well-being [47], it would also be interesting to investigate its applicability within graduate medical education.
Finally, we acknowledge the limitations of the present investigation and suggest some additional directions for future research. As this was an initial pilot study, its design has some limitations including lack of a control group, pre-post data, and lack of long-term follow-up. The pre-post design was chosen because it is useful for demonstrating the immediate impacts of a short-term program, and since our activity only took 30 min, threats to internal validity were unlikely. However, because the design was single armed and lacked a control group, we cannot definitively conclude our results were not impacted but external factors. Students within this study only completed the first two parts of the Clay Lab. In the third lab, users experience death as Clay and the emotional toll on his family. At the time of the pilot, school administration thought this component to be too emotionally charged for our students so near an exam. Given the emotional heaviness of this content, we would recommend following the virtual reality with a debrief session that includes a professional grief counselor or psychologist. It is also important to note that within our study, not all students reported being emotionally affected by the experience. This was not unexpected as empathy has been related to gender, race, ethnicity, and academic background [48]. Since we did not collect personal characteristics from our participants, it is likely that these factors affected the level of engagement and response to the VR simulation. Previous research has also shown that VR interventions are most impactful for those who have low levels of empathy prior to the intervention. Therefore, stratifying students based on their initial empathy may shed more light onto the effectiveness of this type of learning experience. As empathy reportedly declines as students progress through the clinical years [34], it would also be beneficial to compare the response to the virtual reality lab between pre-clerkship and clerkship students. Further, we did not directly measure empathy with a validated empathy scale; however, data suggests that self-perceptions of empathy positively correlate with scores on the Jefferson Scale of Empathy for Physician [49], the most commonly used instrument for assessing empathy within medicine. Interestingly, this paper also reported lack of congruence between residents’ self-reported empathy and patients’ perceived empathy. This emphasizes the need for future research that integrates VR embodiment with clinical assessments and patient experiences. While virtual reality is more associated with surgical and procedural training in the clinical years; it is of value to determine if it could also augment patient-physician interactions and humanism within our trainees during clerkships.
Data Availability
All data generated or analyzed during this study are included in this published article.
References
Berger DM. Clinical empathy. Aronson; 1987.
Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61:349–65. https://doi.org/10.1177/00131640121971158.
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: Definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–9. https://doi.org/10.1176/appi.ajp.159.9.1563.
Kerasidou A, Horn R. Making space for empathy: supporting doctors in the emotional labour of clinical care Ethics in Clinical Practice. BMC Med Ethics. 2016;17:8. https://doi.org/10.1186/s12910-016-0091-7.
Hojat M. Empathy in health professions education and patient care. Springer International Publishing; 2016. https://doi.org/10.1007/978-3-319-27625-0.
Neumann MA, Bensing JB, Mercer SC, Ernstmann NA, Ommen OA, Pfaff HA. H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient education and counseling analyzing the ‘nature’ and ‘specific effectiveness’ of clinical empathy: A theoretical overview and contribution towards a theory-based research agenda. Elsevier 2009;74:339–46. https://doi.org/10.1016/j.pec.2008.11.013.
Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88:1171–7. https://doi.org/10.1097/ACM.0b013e318299f3e3.
Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ. 2014;14:219. https://doi.org/10.1186/1472-6920-14-219.
Sugarman L. Experiential learning: Experience as the source of learning and development, David A. Kolb, Prentice-Hall International, Hemel Hempstead, Herts., 1984. No. of pages: xiii + 256. J Organ Behav 1987;8:359–60. https://doi.org/10.1002/job.4030080408.
Bunn W, Terpstra J. Cultivating empathy for the mentally ill using simulated auditory hallucinations. Acad Psychiatry. 2009;33:457–60. https://doi.org/10.1176/appi.ap.33.6.457.
Varkey P, Chutka DS, Lesnick TG. The aging game: improving medical students’ attitudes toward caring for the elderly. J Am Med Dir Assoc. 2006;7:224–9. https://doi.org/10.1016/j.jamda.2005.07.009.
Herrera F, Bailenson J, Weisz E, Ogle E, Zaki J. Building long-term empathy: a large-scale comparison of traditional and virtual reality perspective-taking. PLoS One. 2018;13:e0204494. https://doi.org/10.1371/journal.pone.0204494.
Slater M. Place illusion and plausibility can lead to realistic behaviour in immersive virtual environments. Philos Trans R Soc B Biol Sci. 2009;364:3549–57. https://doi.org/10.1098/rstb.2009.0138.
Louie AK, Coverdale JH, Balon R, Beresin EV, Brenner AM, Guerrero APS, et al. Enhancing empathy: a role for virtual reality? Acad Psychiatry. 2018;42:747–52. https://doi.org/10.1007/s40596-018-0995-2.
Chris Milk: How virtual reality can create the ultimate empathy machine | TED Talk n.d. https://www.ted.com/talks/chris_milk_how_virtual_reality_can_create_the_ultimate_empathy_machine/discussion?la (accessed 31 Jan 2020).
Schutte NS, Stilinović EJ. Facilitating empathy through virtual reality. Motiv Emot. 2017;41:708–12. https://doi.org/10.1007/s11031-017-9641-7.
Kandaurova M, Lee SH (Mark). The effects of virtual reality (VR) on charitable giving: the role of empathy, guilt, responsibility, and social exclusion. J Bus Res 2019;100:571–80. https://doi.org/10.1016/j.jbusres.2018.
Russell V, Barry R, Murphy D. HAVE experience: an investigation into vr empathy for panic disorder. 2018 IEEE Games, Entertain. Media Conf. GEM 2018, Institute of Electrical and Electronics Engineers Inc.; 2018, p. 167–72. https://doi.org/10.1109/GEM.2018.8516461.
Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Med Libr Assoc. 2018;106:498–500. https://doi.org/10.5195/jmla.2018.518.
Gugliucci MR. Virtual reality medical education project enhances empathy. Innov Aging. 2019;3:S298. https://doi.org/10.1093/GERONI/IGZ038.1096.
Washington E, Shaw C. The effects of a VR intervention on career interest, empathy, communication skills, and learning with second-year medical students, Springer, Cham; 2019, p. 67–80. https://doi.org/10.1007/978-3-030-27986-8_7.
Rabow MW, McPhee SJ. Beyond breaking bad news: how to help patients who suffer. West J Med. 1999;171:260–3. https://doi.org/10.1136/sbmj.000365.
Weisse CS, Melekis K, Hutchins B. Providing end-of-life care: increased empathy and self-efficacy among student caregivers in residential homes for the dying. Am J Hosp Palliat Care. 2019;36:538–45. https://doi.org/10.1177/1049909118820844.
Embodied Labs n.d. https://embodiedlabs.com/ (accessed 24 Mar 2020).
Shin D. Empathy and embodied experience in virtual environment: To what extent can virtual reality stimulate empathy and embodied experience? Comput Human Behav. 2018;78:64–73. https://doi.org/10.1016/j.chb.2017.09.012.
Nicovich SG, Boller GW, Cornwell TB. Experienced presence within computer-mediated communications: initial explorations on the effects of gender with respect to empathy and immersion. J Comput Commun. 2006;10:00–00. https://doi.org/10.1111/j.1083-6101.2005.tb00243.x.
Halpern J. From detached concern to empathy : humanizing medical practice. Oxford University Press; 2001.
Reniers RLEP, Corcoran R, Drake R, Shryane NM, Völlm BA. The QCAE: A questionnaire of cognitive and affective empathy. J Pers Assess. 2011;93:84–95. https://doi.org/10.1080/00223891.2010.528484.
Bellet PS, Maloney MJ. The importance of empathy as an interviewing skill in medicine. JAMA J Am Med Assoc. 1991;266:1831–2. https://doi.org/10.1001/jama.1991.03470130111039.
Telle NT, Pfister HR. Positive empathy and prosocial behavior: a neglected link. Emot Rev. 2014;8:154–63. https://doi.org/10.1177/1754073915586817.
Barzansky B, Vesloski JJ, Miller R, Jonas HS. Education in end-of-life care during medical school and residency training. Acad Med. 1999;74:s102–4. https://doi.org/10.1097/00001888-199910000-00054.
Mermann AC, Gunn DB, Dickinson GE. Learning to care for the dying: a survey of medical schools and a model course. Acad Med. 1991;66:35–8. https://doi.org/10.1097/00001888-199101000-00010.
Linn LS, DiMatteo MR, Cope DW, Robbins A. Measuring physicians’ humanistic attitudes, values, and behaviors. Med Care. 1987;25:504–15. https://doi.org/10.1097/00005650-198706000-00005.
Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. [1] Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: a scoping review. Adv Heal Sci Educ 2017;22:1293–313. https://doi.org/10.1007/s10459-016-9704-7.
Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–91. https://doi.org/10.1097/ACM.0b013e3181b17e55.
Preusche I, Lamm C. Reflections on empathy in medical education: what can we learn from social neurosciences? Adv Heal Sci Educ. 2016;21:235–49. https://doi.org/10.1007/s10459-015-9581-5.
Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS One. 2013;8:e61526. https://doi.org/10.1371/journal.pone.0061526.
Patel S, Pelletier-Bui A, Smith S, Roberts MB, Kilgannon H, Trzeciak S, et al. Curricula for empathy and compassion training in medical education: a systematic review. PLoS One. 2019;14:e0221412. https://doi.org/10.1371/journal.pone.0221412.
van Loon A, Bailenson J, Zaki J, Bostick J, Willer R. Virtual reality perspective-taking increases cognitive empathy for specific others. PLoS ONE. 2018;13:e0202442. https://doi.org/10.1371/journal.pone.0202442.
Blascovich J, Loomis J, Beall AC, Swinth KR, Hoyt CL, Bailenson JN. Immersive virtual environment technology: just another methodological tool for social psychology? Psychol Inq. 2002;13:146–9. https://doi.org/10.1207/S15327965PLI1302_03.
Bailenson JN, Yee N. A longitudinal study of task performance, head movements, subjective report, simulator sickness, and transformed social interaction in collaborative virtual environments. Presence Teleoperators Virtual Environ. 2006;15:699–716. https://doi.org/10.1162/pres.15.6.699.
Shriram K, Oh SY, Bailenson J. Virtual Reality and Prosocial Behavior. In: Burgoon JK, Magnenat-Thalmann N, Pantic M, Vinciarelli A, editors. Soc. Signal Process., Cambridge: Cambridge University Press; 2017, p. 304–16. https://doi.org/10.1017/9781316676202.022.
Psychiatry EW-HJ of C, 1980 undefined. The dutiful physician: the central role of empathy in psychoanalysis, psychotherapy, and medical practice. PsycnetApaOrg n.d.
Feighny KM, Monaco M, Arnold L. Empathy training to improve physician-patient communication skills. Acad Med. 1995;70:435–6. https://doi.org/10.1097/00001888-199505000-00031.
Real F, DeBlasio D, Ollberding N, Davis D, Cruse B, Mclinden D, et al. Resident perspectives on communication training that utilizes immersive virtual reality. Educ Heal. 2017;30:228. https://doi.org/10.4103/efh.EfH_9_17.
Fisher JA. Empathic actualities: toward a taxonomy of empathy in virtual reality. Lect. Notes Comput. Sci. (including Subser. Lect. Notes Artif. Intell. Lect. Notes Bioinformatics), vol. 10690 LNCS, Springer Verlag; 2017, p. 233–44. https://doi.org/10.1007/978-3-319-71027-3_19.
Shamasundar C. Understanding empathy and related phenomena. Am J Psychother. 1999;53:232–45. https://doi.org/10.1176/appi.psychotherapy.1999.53.2.232.
Hojat M, DeSantis J, Shannon SC, Speicher MR, Bragan L, Calabrese LH. Empathy as related to gender, age, race and ethnicity, academic background and career interest: a nationwide study of osteopathic medical students in the United States. Med Educ. 2020. https://doi.org/10.1111/medu.14138.
Grosseman S, Novack DH, Duke P, Mennin S, Rosenzweig S, Davis TJ, et al. Residents’ and standardized patients’ perspectives on empathy: Issues of agreement. Patient Educ Couns. 2014;96:22–8. https://doi.org/10.1016/j.pec.2014.04.007.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Carrie Elzie and Jacqueline Shaia. The first draft of the manuscript was written by Carrie Elzie, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Human Research Ethics committee of Eastern Virginia Medical School (IRB # 19-10-WC-0246).
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elzie, C.A., Shaia, J. A Pilot Study of the Impact of Virtually Embodying a Patient with a Terminal Illness. Med.Sci.Educ. 31, 665–675 (2021). https://doi.org/10.1007/s40670-021-01243-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-021-01243-9