Abstract
Hydrogen sulfide (H2S) formed by multiple enzymes including cystathionine-γ-lyase (CSE) targets Cav3.2 T-type Ca2+ channels (T-channels) and transient receptor potential ankyrin-1 (TRPA1). Intraplantar and intracolonic administration of H2S donors promotes somatic and visceral pain, respectively, via activation of Cav3.2 and TRPA1 in rats and/or mice. Injection of H2S donors into the plantar tissues, pancreatic duct, colonic lumen, or bladder causes T-channel-dependent excitation of nociceptors, determined as phosphorylation of ERK or expression of Fos in the spinal dorsal horn. Electrophysiological studies demonstrate that exogenous and/or endogenous H2S facilitates membrane currents through T-channels in NG108-15 cells and isolated mouse dorsal root ganglion (DRG) neurons that abundantly express Cav3.2 and also in Cav3.2-transfected HEK293 cells. In mice with cerulein-induced pancreatitis and cyclophosphamide-induced cystitis, visceral pain and/or referred hyperalgesia are inhibited by CSE inhibitors and by pharmacological blockade or genetic silencing of Cav3.2, and CSE protein is upregulated in the pancreas and bladder. In rats with neuropathy induced by L5 spinal nerve cutting or by repeated administration of paclitaxel, an anticancer drug, the neuropathic hyperalgesia is reversed by inhibitors of CSE or T-channels and by silencing of Cav3.2. Upregulation of Cav3.2 protein in DRG is detectable in the former, but not in the latter, neuropathic pain models. Thus, H2S appears to function as a nociceptive messenger by facilitating functions of Cav3.2 and TRPA1, and the enhanced function of the CSE/H2S/Cav3.2 pathway is considered to be involved in the pancreatitis- and cystitis-related pain and in neuropathic pain.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Hydrogen sulfide (H2S), an endogenous gasotransmitter, is generated from l-cysteine mainly by cystathionine-β-synthase (CBS), cystathionine-γ-lyase (CSE), or 3-mercaptopyruvate sulfurtransferase (3-MST) along with cysteine aminotransferase (CAT) throughout the mammalian body (Kimura 2010) including the heart (Geng et al. 2004), blood vessels (Zhao et al. 2001), and central nervous system (CNS) (Warenycia et al. 1989). H2S appears to play dual or complex roles in many tissues/organs. In the nervous system, there is evidence not only for the neurotoxicity of H2S through activation of glutamate receptors including NMDA receptors (Cheung et al. 2007) and activation of the MEK/ERK pathway (Kurokawa et al. 2011) but also for the neuroprotection by H2S via multiple mechanisms such as activation of ATP-sensitive K+ (KATP) and Cl− channels and elevation of intracellular glutathione levels (Kimura and Kimura 2004; Kimura et al. 2006). Endogenous H2S is also involved in neuronal excitation via the Ca2+/calmodulin-mediated pathway (Eto et al. 2002) and modification of long-term potentiation (Abe and Kimura 1996) via enhancement of the cAMP-induced NMDA receptor response (Kimura 2000).
H2S appears to cause excitation of sensory nerves and play important roles in neurogenic inflammation, since NaHS, an H2S donor, increases neuropeptide release in guinea-pig airways, an effect attenuated by capsaicin desensitization of C-fiber neurons and by the transient receptor potential vanilloid-1 (TRPV1) antagonist capsazepine. In addition, NaHS induces contraction of isolated airways, which is abolished by TRPV1 antagonism and pretreatment with the combination of tachykinin NK1 and NK2 receptor antagonists (Trevisani et al. 2005). It is consistent with the evidence that H2S stimulates capsaicin-sensitive primary afferent nerve terminals, from which tachykinins are released to produce concentration-dependent contractile responses by activating NK1 and NK2 receptors in the rat urinary bladder (Patacchini et al. 2004). Nonetheless, TRPV1 is not considered a direct target for H2S, and Cav3.2 T-type Ca2+ channels and transient receptor potential ankyrin-1(TRPA1) rather appear responsible for excitation of sensory neurons (Miyamoto et al. 2011; Andersson et al. 2012; Pozsgai et al. 2012; Sekiguchi and Kawabata 2013; Donatti et al. 2014). Sensory plasticity in nociception, known as sensitization, is thought to contribute significantly to the production of persistent, often pathological pain. Here, we review the role of H2S in somatic, visceral, and neuropathic pain processing.
2 Targets of H2S in Pain Processing
2.1 Cav3.2 T-Type Ca2+ Channels
Cav3.2 T-type Ca2+ channels (T-channels) are activated at near-resting membrane potential and play a crucial role in excitability of both central and peripheral neurons. T-channels are expressed in dorsal root ganglion (DRG) neurons including the peripheral and central axons/endings, suggesting the role of T-channels in sensory transmission (Fig. 1) (Nelson et al. 2005; Todorovic and Jevtovic-Todorovic 2011; Rose et al. 2013). Three isoforms of T-channels have been identified, i.e., Cav3.1, Cav3.2, and Cav3.3 (Perez-Reyes 2003). Studies using in situ hybridization have demonstrated that mRNA for Cav3.2 is the most abundant isoform of T-channels in peripheral sensory neurons (Todorovic and Jevtovic-Todorovic 2011). Bourinet and his coworkers have demonstrated thermal and mechanical analgesia in rats with molecular knockdown of Cav3.2 T-channels in DRG neurons (Bourinet et al. 2005). Cav3.2 T-channels are much more sensitive to inhibition by metals, such as zinc, copper, and nickel, than Cav3.1 or Cav3.3 (Todorovic and Jevtovic-Todorovic 2011; Sekiguchi and Kawabata 2013). It is now clear that a histidine residue at position 191 (His191) in the second extracellular loop of domain I of Cav3.2 is a critical determinant for the trace metal inhibition and is not conserved in Cav3.1 or Cav3.3 (Iftinca and Zamponi 2009). Cav3.2 T-channels appear to be tonically exposed to inhibition by Zn2+ in cultured cells and possibly in mammalian tissues under physiological conditions, and compounds that chemically interact with Zn2+, such as l-cysteine and H2S, selectively enhance the channel functions of Cav3.2 among the three T-channel isoforms (Nelson et al. 2007a; Matsunami et al. 2011; Sekiguchi and Kawabata 2013). Moreover, l-ascorbic acid, a reducing compound, at physiologically relevant concentrations selectively inhibits native T-currents in the DRG and thalamus and diminishes T-channel-dependent burst firing in reticular thalamic cells. This highly subtype-specific effect was achieved via metal-catalyzed oxidation of critical metal-binding and Cav3.2-unique His191 residue (Nelson et al. 2007b). NaHS, an H2S donor, facilitates membrane currents through T-channels in NG108-15 cells that naturally express Cav3.2 (Kawabata et al. 2007; Nagasawa et al. 2009) and in isolated mouse DRG neurons that abundantly express Cav3.2 (Matsunami et al. 2009). In Cav3.2-transfected HEK293 cells, T-currents are not altered by H2S donors, NaHS at 1.5 mM and Na2S at 0.1 mM, but strongly suppressed by DL-propargylglycine (PPG), an inhibitor of CSE, an H2S-forming enzyme. Further, in the presence of the CSE inhibitor, the H2S donors, NaHS at 1.5 mM and Na2S at 0.1–0.3 mM, enhance the decreased Cav3.2 T-currents, and CSE is abundantly expressed in both Cav3.2-transfected and background HEK293 cells (Sekiguchi et al. 2014). Collectively, endogenous and exogenous H2S appears to positively regulate the functions of Cav3.2 T-channels (Fig. 1). An independent group has reported that NaHS at low (0.1–1 mM) and high concentrations (3 mM) suppresses and enhances T-currents by 25–30 %, respectively, in Cav3.2-transfected HEK293 cells or randomly chosen rat DRG cells (Elies et al. 2014), whereas we have never detected the suppressive effect of NaHS or Na2S even at low concentrations on T-currents in our Cav3.2-transfected HEK293 cells (Sekiguchi et al. 2014), NG108-15 cells (Kawabata et al. 2007), or small mouse DRG neurons (less than 30 μm in cell body diameter) (Matsunami et al. 2009), known to be rich in T-type Ca2+ channels (Todorovic and Jevtovic-Todorovic 2011). Particularly, Na2S at 0.1–0.3 mM rather augments T-currents in Cav3.2-transfected HEK293 cells pretreated with the CSE inhibitor (Sekiguchi et al. 2014), as mentioned above, being inconsistent to the suppressive effect of NaHS at equivalent concentrations in their report (Elies et al. 2014). The discrepancy has yet to be interpreted, although the effect of H2S on Cav3.2 channels in vitro and in vivo might be dependent on the abundance of H2S-forming enzymes including CSE, the formation or contamination of polysulfides, and the concentrations of Zn2+ and ascorbic acid that negatively regulate Cav3.2 functions (Todorovic and Jevtovic-Todorovic 2011; Kimura et al. 2013; Sekiguchi and Kawabata 2013; Sekiguchi et al. 2014). Particularly, levels of Zn2+ would have great impact on the Cav3.2 channel activity and its regulation by H2S, since Zn2+ binds to not only His191 of Cav3.2 (Todorovic and Jevtovic-Todorovic 2011; Sekiguchi and Kawabata 2013) but also H2S itself (Munchberg et al. 2007). Given that Cav3.2 is involved in somatic and visceral nociceptive processing and in neuropathic pain (Todorovic and Jevtovic-Todorovic 2011; Francois et al. 2014), regulation of Cav3.2 by endogenous and exogenous H2S is considered to have great impact on the pathophysiology of inflammatory and neuropathic pain (Sekiguchi et al. 2014). The T-channel suppression by NaHS at low doses, if any, might be overcome by TRPA1 activation by NaHS in vivo, as described below.
2.2 Transient Receptor Potential Ankyrin-1
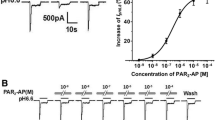
Transient receptor potential ankyrin-1 (TRPA1), a member of the TRP channel family, is abundantly expressed in a subpopulation of unmyelinated nociceptors that also express TRPV1. It is activated by a diverse assortment of pungent or irritating reactive chemical compounds including those found in mustard oil (allylisothiocyanate), cinnamon oil (cinnamaldehyde), exhaust (acrolein), raw garlic, and onions (allicin). Moreover, TRPA1 has been put forth as a putative transducer of natural physical stimuli including both cold (<17 °C) and mechanical force (Stucky et al. 2009). It has been reported that TRPA1 is sensitized by proteinase-activated receptor-2 (PAR2) activation, contributing to inflammatory pain (Dai et al. 2007). We have provided evidence that pharmacological inhibition of TRPA1 prevents the spinal Fos expression following infusion of SLIGRL-NH2, a PAR2-activating peptide, into the pancreatic duct, suggesting the pronociceptive role of TRPA1 as a downstream signal of PAR2 activation in the pancreatic nociceptors (Terada et al. 2013). Most interestingly, it has been reported that NaHS evokes a time- and concentration-dependent increase in cytosolic calcium concentration in TRPA1-transfected cells (Streng et al. 2008) and that NaHS induces calcium influx and inward currents in rat DRG cells, an effect inhibited by a TRPA1 antagonist (Miyamoto et al. 2011; Ogawa et al. 2012). The H2S-induced TRPA1 activation appears to involve H2S modulation of two cysteine residues located in the N-terminal intracellular domain of the TRPA1 (Ogawa et al. 2012). These findings suggest that TRPA1 in collaboration with Cav3.2 mediates H2S-induced excitation of nociceptors, participating in pain processing (Fig. 1).
3 Somatic Pain
We first reported that intraplantar (i.pl.) administration of NaHS produces prompt hyperalgesia in rats, accompanied by expression of Fos protein, a marker for neuronal excitation, in the spinal dorsal horn, and that the H2S-evoked hyperalgesia is blocked by ethosuximide and mibefradil, T-channel blockers (Kawabata et al. 2007). Another H2S donor, Na2S, also facilitates hyperalgesia by i.pl. administration, an effect completely blocked by pretreatment with NNC 55-0396 (NNC), a T-channel blocker (Sekiguchi et al. 2014). l-Cysteine, an endogenous source for H2S, given i.pl., mimics the H2S-induced hyperalgesia, an effect being abolished by PPG and β-cyanoalanine (BCA), inhibitors of CSE, in rats (Kawabata et al. 2007). The NaHS-induced hyperalgesia is also suppressed by pretreatment with i.pl. zinc chloride and/or ascorbic acid, known to selectively inhibit Cav3.2 among three T-channel isoforms, and by silencing of Cav3.2 T-channels in the sensory neurons by repeated intrathecal (i.t.) administration of antisense oligodeoxynucleotides (ODNs) targeting Cav3.2 T-channels in rats or mice (Maeda et al. 2009; Okubo et al. 2012). Interestingly, i.t. administration of NaHS also rapidly decreases nociceptive threshold in rats, as determined by the paw pressure method. The hyperalgesia caused by i.t. NaHS is also abolished by co-administration of mibefradil and pretreatment with i.t. zinc chloride and by silencing of Cav3.2 protein in the DRG (Maeda et al. 2009). These findings are consistent with the evidence that presynaptic Cav3.2 T-channel regulates spontaneous excitatory synaptic neurotransmitter release from the central terminal of nociceptors in the spinal dorsal horn, in addition to neuronal excitability in the peripheral endings of nociceptors (Jacus et al. 2012). Thus, positive regulation of Cav3.2 T-channel by H2S is considered to have a great impact on nociceptive processing at both peripheral and central endings of the primary afferent neurons (Fig. 1). We have also demonstrated that the NaHS-induced hyperalgesia/allodynia in mice is significantly suppressed by AP18, a TRPA1 blocker, and by silencing of TRPA1 in the sensory neurons (Okubo et al. 2012), suggesting that TRPA1 and Cav3.2 mediate the pronociceptive effect of H2S (Fig. 1). The involvement of TRPA1 in H2S-induced hyperalgesia has been confirmed by independent studies (Andersson et al. 2012; Ogawa et al. 2012). It is likely that H2S causes activation of TRPA1 followed by elevation of membrane potentials that activates Cav3.2 and then enhances the evoked Cav3.2 T-channel currents, leading to increased nociceptor excitability and hyperalgesia. Thus, both TRPA1 and Cav3.2 are considered to participate in the H2S-induced hyperalgesia (Fig. 1).
We have shown that PPG and BCA, CSE inhibitors, partially block the hyperalgesia induced by i.pl. lipopolysaccharide (LPS), an effect being reversed by i.pl. NaHS (Kawabata et al. 2007). The suppression of LPS-induced hyperalgesia by CSE inhibitors might be associated with the prevention of neutrophil recruitment to the plantar tissue (Cunha et al. 2008). H2S is also pronociceptive in the formalin model of persistent inflammatory pain in rats. Injection of formalin into the hindpaw evokes a dose-dependent increase in the concentration of H2S in the paw tissue. Both nociceptive flinching and paw edema induced by formalin are attenuated by pretreatment with PPG. Furthermore, PPG pretreatment attenuates the induction of c-Fos in spinal laminae I–II following injection of formalin (Lee et al. 2008). It has also been reported that pretreatment of mice with PPG reduces zymosan-induced articular hyperalgesia (Cunha et al. 2008). Recent evidence has shown that the inflammatory pain in temporomandibular joint by injection of complete Freund’s adjuvant in rats is attenuated by subcutaneous administration of aminooxyacetic acid (AOAA), known as a CBS inhibitor (Miao et al. 2014), although the selectivity of AOAA for CBS is now questioned (Asimakopoulou et al. 2013). Thus, there is plenty of evidence that H2S participates in inflammatory pain processing. Nevertheless, it is noteworthy that exogenously applied H2S reveals antinociceptive activity in certain experimental conditions through activation of KATP channels or unknown mechanisms (Cunha et al. 2008).
4 Visceral Pain
4.1 Pancreatic Pain
Clinically, pancreatic pain is a serious problem for patients with pancreatitis or pancreatic cancer. In humans, pain elicited from the pancreas is often referred to the upper abdominal area and radiates to the back, and these skin areas are usually tender to touch. In pancreatic acinar cells isolated from mice, treatment with cerulein increases the levels of H2S and CSE mRNA expression (Tamizhselvi et al. 2007). Furthermore, the activity and protein expression of CSE in the pancreatic tissues increase after the development of cerulein-induced pancreatitis in mice (Nishimura et al. 2009). Given the prevention by PPG, a CSE inhibitor, of cerulein-induced pancreatitis and referred hyperalgesia/allodynia (Bhatia et al. 2005; Nishimura et al. 2009), H2S is considered to play a critical role in the development of acute pancreatitis and related pain. NaHS infused into the pancreatic duct causes the expression of Fos protein (Nishimura et al. 2009) and ERK phosphorylation (Fukushima et al. 2010), delayed and rapid markers for neuronal activation, respectively, in the superficial layers of spinal cord in anesthetized mice or rats, which are attenuated by i.p. administration of mibefradil, a T-channel blocker. Mibefradil also suppresses the referred hyperalgesia/allodynia in mice with cerulein-induced pancreatitis (Nishimura et al. 2009). Together, H2S produced by upregulated CSE during the development of pancreatitis augments the function of T-channels, contributing to pancreatitis-related pain. As described above for somatic pain processing, TRPA1 in addition to T-channels appears to mediate H2S-induced pancreatic nociception in naïve animals, because the TRPA1 inhibitor AP18 or the T-channel inhibitor NNC 55-0396 prevents spinal Fos expression following injection of NaHS into the pancreatic duct in mice without pancreatitis. In contrast, in mice with cerulein-induced pancreatitis, NNC 55-0396 or genetic silencing of Cav3.2 abolishes the referred hyperalgesia accompanying cerulein-induced pancreatitis, while AP18 or genetic TRPA1 silencing just facilitates the effect of NNC 55-0396, but had no significant effect on the pancreatitis-related pain by itself (Terada et al. 2014). Given the downregulation of TRPA1, but not Cav3.2, in the pancreatic tissue following cerulein treatment (Terada et al. 2014), Cav3.2 is considered to primarily participate in the pancreatitis-related pain, while TRPA1 appears to play a secondary role in nociceptive signaling during pancreatitis.
4.2 Colonic Pain
In the colonic lumen, H2S is also produced by sulfate-reducing bacteria and may be associated with the pathogenesis of inflammatory bowel disease (IBD) and colorectal cancer (Roediger et al. 1997; Ohge et al. 2003; Taniguchi et al. 2009). Nonetheless, there is evidence for a protective role of H2S against IBD (Wallace et al. 2009). H2S regulates the secretion of HCO3 − in the duodenum (Ise et al. 2011) and Cl− in the colon (Schicho et al. 2006), predicting possible involvement of H2S in visceral nociception. Distrutti et al. (Distrutti et al. 2006) have described that i.p. injection of H2S donors suppressed responses to colorectal distention by activating KATP channels. However, it has been reported that CBS in colonic sensory neurons is upregulated and contributes to visceral hypersensitivity in a rat model of irritable bowel syndrome (IBS) (Xu et al. 2009) and that upregulation of CBS expression by NF-κB contributes to visceral hypersensitivity in rats (Li et al. 2012). We have demonstrated that intracolonic (i.col.) administration of NaHS induces visceral nociceptive behavior accompanied by referred hyperalgesia/allodynia and phosphorylation of ERK in the spinal cord in mice (Matsunami et al. 2009). The behavioral effects of i.col. NaHS are abolished by mibefradil and NNC 55-0396; T-channel blockers; and zinc chloride, known to selectively inhibit Cav3.2 among three isoforms of T-channels by genetic knockdown of Cav3.2 and also to be attenuated by AP18, a TRPA1 blocker, but not verapamil, an L-type Ca2+ channel blocker, or glibenclamide, a KATP channel blocker (Matsunami et al. 2009; Matsunami et al. 2011). Interestingly, Cav3.2 is constantly exposed to Zn2+ inhibition under physiological conditions, and zinc chelators applied exogenously enhance Cav3.2 functions by cancelling the Zn2+ inhibition (Nelson et al. 2007a). We have shown that two distinct Zn2+ chelators, N,N,N′,N′-tetrakis (2-pyridylmethyl)-ethylenediamine (TPEN) and dipicolinic acid, when administered intracolonically, mimics the NaHS-evoked visceral nociceptive behavior, referred abdominal hyperalgesia/allodynia, and phosphorylation of ERK in the spinal dorsal horn, which are inhibited by T-channel blockers (Matsunami et al. 2011). The contribution of Cav3.2 T-channels to colonic hypersensitivity has been confirmed by an independent group (Marger et al. 2011). Collectively, H2S plays critical roles in colonic pain signaling through facilitation of Cav3.2 T-channel functions by cancelling the Zn2+ inhibition and also activation of TRPA1 channels. Our recent study has also shown that Cav3.2-dependent excitation of capsaicin-sensitive sensory neurons by H2S contributes to colonic mucosal cytoprotection in rats with 2,4,6-trinitrobenzenesulfonic acid (TNBS)-induced colitis (Matsunami et al. 2012a).
4.3 Bladder Pain
The most common visceral pain in the field of urology is bladder pain, a symptom of lower urinary tract diseases such as cystitis, cystolithiasis, and bladder cancer, which impairs the quality of life in patients. Interstitial cystitis or painful bladder syndrome is an idiopathic disease, presenting with bladder pain and urinary frequency or urgency (Kelada and Jones 2007). The bladder pain accompanying interstitial cystitis is regional and chronic and spreads over the lower pelvic and suprapubic area and mimics neuropathic pain (Theoharides et al. 2008). In isolated rat urinary bladder, H2S stimulates capsaicin-sensitive primary afferent neurons and produces contractile responses (Patacchini et al. 2004). There is also evidence that intravesical NaHS produces changes in urodynamic parameters after chemical disruption of the urothelial barrier in rats (Streng et al. 2008). Intraperitoneal administration of cyclophosphamide induces cystitis in mice, accompanied by bladder pain-like nociceptive behavior and referred hyperalgesia in the region between the anus and urethral opening, which is now recognized as an animal model of human interstitial cystitis (Wantuch et al. 2007).
We have shown that inhibition of CSE by pre-administration of PPG prevents cyclophosphamide-induced bladder nociception, i.e., bladder pain-like nociceptive behavior and referred hyperalgesia, and that expression of CSE protein is markedly increased in the bladder tissue of mice with cyclophosphamide-induced cystitis (Matsunami et al. 2012b), as observed in the pancreatic tissue of mice with cerulein-induced pancreatitis (Nishimura et al. 2009). Post-administration of T-channel blockers, mibefradil and NNC 55-0396, and the knockdown of Cav3.2 T-channels by the antisense method suppress the cyclophosphamide-induced bladder nociception, while neither an L-type Ca2+ channel blocker, verapamil, nor TRPA1 blockers, AP18 and HC-030031, exert such effect (Matsunami et al. 2012b). The T-channel-dependent pronociceptive role of H2S in bladder nociceptive processing is also supported by our evidence that intravesical administration of NaHS causes phosphorylation of ERK in the spinal cord, an effect prevented by pretreatment with the T-channel blocker NNC 55-0396 (Matsunami et al. 2012b).
5 Neuropathic Pain
Neuropathic pain is the consequence of damage to peripheral nerves or to the CNS and common in clinical practice and greatly impairs the quality of life of patients. The neuropathic syndromes include painful diabetic neuropathy, postherpetic neuralgia, phantom limb pain, complex regional pain syndrome (CRPS), etc. The molecular mechanisms underlying neuropathic pain involve abnormal functions and/or altered expression of voltage-gated ion channels such as sodium (McGowan et al. 2009), calcium (Boroujerdi et al. 2011), and potassium channels (Cao et al. 2010) in sensory neurons. There is evidence for upregulation of T-current density in small DRG cells isolated from rats with neuropathic pain due to chronic constrictive injury (CCI) of the sciatic nerve (Jagodic et al. 2008) and that genetic silencing of Cav3.2 T-channels reverses CCI-induced neuropathic pain (Bourinet et al. 2005). We have shown that neuropathic hyperalgesia/allodynia caused by L5 spinal nerve cutting (L5SNC) is strongly suppressed by i.p. administration of CSE inhibitors and by i.pl. administration of T-channel blockers or genetic silencing of Cav3.2 T-channels (Takahashi et al. 2010). Given that the protein levels of Cav3.2 T-channels, but not CSE, are dramatically upregulated in the DRG of rats with L5SNC (Takahashi et al. 2010), our data suggest that the upregulated Cav3.2 T-channels in sensory neurons after spinal nerve injury are exposed to positive regulation by CSE-derived endogenous H2S, contributing to the maintenance of neuropathic pain. H2S is also considered to be involved in diabetes-associated peripheral neuropathy, since systemic administration of inhibitors of CSE or CBS and silencing of Cav3.2 T-channels in DRG reverse mechanical allodynia/hyperalgesia in streptozotocin (STZ)-induced diabetic neuropathy rats (Todorovic et al. 2001; Velasco-Xolalpa et al. 2013). It is also to be noted that T-channels, particularly of the Cav3.2 isoform, are upregulated and involved in the hyperalgesia/allodynia in the laboratory animals with the diabetic neuropathy (Messinger et al. 2009). Upregulation of T-channel current density has also been shown in DRG cells isolated from diabetic Bio-Bred/Worchester (BB/W) rats and from rats with STZ-induced diabetic neuropathy (Todorovic and Jevtovic-Todorovic 2011). Thus, the upregulation of Cav3.2 T-channels in the sensory neurons appears to cause diabetes-induced hyperexcitability of the nociceptors, contributing to the pathogenesis of diabetic neuropathy.
Many anticancer agents, such as vincristine, paclitaxel, and oxaliplatin, often cause painful peripheral neuropathies that limit their use in cancer therapy. It has been demonstrated that ethosuximide, a T-channel blocker, reverses paclitaxel- and vincristine-induced painful peripheral neuropathy in laboratory animals (Flatters and Bennett 2004). We have reported that paclitaxel-induced neuropathic hyperalgesia is reversed by i.pl. administration of NNC 55-0396 or mibefradil, systemic administration of PPG or BCA, CSE inhibitors, and genetic silencing of Cav3.2. Unlike L5SNC rats, neither Cav3.2 nor CSE are upregulated at protein levels in the DRG, spinal cord, or peripheral tissues including the hindpaws, whereas H2S content in hindpaw tissues is elevated (Okubo et al. 2011). Together, Cav3.2, a target for H2S formed by CSE, is a key molecule in the maintenance of distinct types of neuropathic pain.
6 Conclusion
H2S plays important roles in processing of somatic, visceral, and neuropathic pain signals by targeting Cav3.2 T-channels and TRPA1. In this context, H2S-generating enzymes, Cav3.2, and TRPA1 could be molecular targets for treatment of inflammatory and neuropathic pain including visceral pain. However, endogenous H2S plays important protective roles in the cardiovascular and gastrointestinal systems, CNS, and so on. Therefore, we must consider the risk of side effects of CSE and CBS inhibitors, especially in the case of their long-term use. Thus, blockade of Cav3.2 T-channels and/or TRPA1 would have greater advantage than inhibition of H2S formation. In particular, the development of selective Cav3.2 inhibitors should impact on improvement of therapeutic strategy for neuropathic pain, although no isoform selective T-channel inhibitors are available at present.
References
Abe K, Kimura H (1996) The possible role of hydrogen sulfide as an endogenous neuromodulator. J Neurosci 16:1066–1071
Andersson DA, Gentry C, Bevan S (2012) TRPA1 has a key role in the somatic pro-nociceptive actions of hydrogen sulfide. PLoS One 7, e46917
Asimakopoulou A, Panopoulos P, Chasapis CT, Coletta C, Zhou Z, Cirino G et al (2013) Selectivity of commonly used pharmacological inhibitors for cystathionine beta synthase (CBS) and cystathionine gamma lyase (CSE). Br J Pharmacol 169:922–932
Bhatia M, Wong FL, Fu D, Lau HY, Moochhala SM, Moore PK (2005) Role of hydrogen sulfide in acute pancreatitis and associated lung injury. FASEB J 19:623–625
Boroujerdi A, Zeng J, Sharp K, Kim D, Steward O, Luo ZD (2011) Calcium channel alpha-2-delta-1 protein upregulation in dorsal spinal cord mediates spinal cord injury-induced neuropathic pain states. Pain 152:649–655
Bourinet E, Alloui A, Monteil A, Barrere C, Couette B, Poirot O et al (2005) Silencing of the Cav3.2 T-type calcium channel gene in sensory neurons demonstrates its major role in nociception. EMBO J 24:315–324
Cao XH, Byun HS, Chen SR, Cai YQ, Pan HL (2010) Reduction in voltage-gated K+ channel activity in primary sensory neurons in painful diabetic neuropathy: role of brain-derived neurotrophic factor. J Neurochem 114:1460–1475
Cheung NS, Peng ZF, Chen MJ, Moore PK, Whiteman M (2007) Hydrogen sulfide induced neuronal death occurs via glutamate receptor and is associated with calpain activation and lysosomal rupture in mouse primary cortical neurons. Neuropharmacology 53:505–514
Cunha TM, Dal-Secco D, Verri WA Jr, Guerrero AT, Souza GR, Vieira SM et al (2008) Dual role of hydrogen sulfide in mechanical inflammatory hypernociception. Eur J Pharmacol 590:127–135
Dai Y, Wang S, Tominaga M, Yamamoto S, Fukuoka T, Higashi T et al (2007) Sensitization of TRPA1 by PAR2 contributes to the sensation of inflammatory pain. J Clin Invest 117:1979–1987
Distrutti E, Sediari L, Mencarelli A, Renga B, Orlandi S, Antonelli E et al (2006) Evidence that hydrogen sulfide exerts antinociceptive effects in the gastrointestinal tract by activating KATP channels. J Pharmacol Exp Ther 316:325–335
Donatti AF, Araujo RM, Soriano RN, Azevedo LU, Leite-Panissi CA, Branco LG (2014) Role of hydrogen sulfide in the formalin-induced orofacial pain in rats. Eur J Pharmacol 738:49–56
Elies J, Scragg JL, Huang S, Dallas ML, Huang D, MacDougall D et al (2014) Hydrogen sulfide inhibits Cav3.2 T-type Ca2+ channels. FASEB J 28(12):5376–5387
Eto K, Ogasawara M, Umemura K, Nagai Y, Kimura H (2002) Hydrogen sulfide is produced in response to neuronal excitation. J Neurosci 22:3386–3391
Flatters SJ, Bennett GJ (2004) Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain 109:150–161
Francois A, Laffray S, Pizzoccaro A, Eschalier A, Bourinet E (2014) T-type calcium channels in chronic pain: mouse models and specific blockers. Pflugers Arch 466:707–717
Fukushima O, Nishimura S, Matsunami M, Aoki Y, Nishikawa H, Ishikura H et al (2010) Phosphorylation of ERK in the spinal dorsal horn following pancreatic pronociceptive stimuli with proteinase-activated receptor-2 agonists and hydrogen sulfide in rats: evidence for involvement of distinct mechanisms. J Neurosci Res 88:3198–3205
Geng B, Yang J, Qi Y, Zhao J, Pang Y, Du J et al (2004) H2S generated by heart in rat and its effects on cardiac function. Biochem Biophys Res Commun 313:362–368
Iftinca MC, Zamponi GW (2009) Regulation of neuronal T-type calcium channels. Trends Pharmacol Sci 30:32–40
Ise F, Takasuka H, Hayashi S, Takahashi K, Koyama M, Aihara E et al (2011) Stimulation of duodenal HCO3 − secretion by hydrogen sulphide in rats: relation to prostaglandins, nitric oxide and sensory neurones. Acta Physiol (Oxf) 201:117–126
Jacus MO, Uebele VN, Renger JJ, Todorovic SM (2012) Presynaptic Cav3.2 channels regulate excitatory neurotransmission in nociceptive dorsal horn neurons. J Neurosci 32:9374–9382
Jagodic MM, Pathirathna S, Joksovic PM, Lee W, Nelson MT, Naik AK et al (2008) Upregulation of the T-type calcium current in small rat sensory neurons after chronic constrictive injury of the sciatic nerve. J Neurophysiol 99:3151–3156
Kawabata A, Ishiki T, Nagasawa K, Yoshida S, Maeda Y, Takahashi T et al (2007) Hydrogen sulfide as a novel nociceptive messenger. Pain 132:74–81
Kelada E, Jones A (2007) Interstitial cystitis. Arch Gynecol Obstet 275:223–229
Kimura H (2000) Hydrogen sulfide induces cyclic AMP and modulates the NMDA receptor. Biochem Biophys Res Commun 267:129–133
Kimura H (2010) Hydrogen sulfide: from brain to gut. Antioxid Redox Signal 12:1111–1123
Kimura Y, Kimura H (2004) Hydrogen sulfide protects neurons from oxidative stress. FASEB J 18:1165–1167
Kimura Y, Dargusch R, Schubert D, Kimura H (2006) Hydrogen sulfide protects HT22 neuronal cells from oxidative stress. Antioxid Redox Signal 8:661–670
Kimura Y, Mikami Y, Osumi K, Tsugane M, Oka J, Kimura H (2013) Polysulfides are possible H2S-derived signaling molecules in rat brain. FASEB J 27:2451–2457
Kurokawa Y, Sekiguchi F, Kubo S, Yamasaki Y, Matsuda S, Okamoto Y et al (2011) Involvement of ERK in NMDA receptor-independent cortical neurotoxicity of hydrogen sulfide. Biochem Biophys Res Commun 414:727–732
Lee AT, Shah JJ, Li L, Cheng Y, Moore PK, Khanna S (2008) A nociceptive-intensity-dependent role for hydrogen sulphide in the formalin model of persistent inflammatory pain. Neuroscience 152:89–96
Li L, Xie R, Hu S, Wang Y, Yu T, Xiao Y et al (2012) Upregulation of cystathionine beta-synthetase expression by nuclear factor-kappa B activation contributes to visceral hypersensitivity in adult rats with neonatal maternal deprivation. Mol Pain 8:89
Maeda Y, Aoki Y, Sekiguchi F, Matsunami M, Takahashi T, Nishikawa H et al (2009) Hyperalgesia induced by spinal and peripheral hydrogen sulfide: evidence for involvement of Cav3.2 T-type calcium channels. Pain 142:127–132
Marger F, Gelot A, Alloui A, Matricon J, Ferrer JF, Barrere C et al (2011) T-type calcium channels contribute to colonic hypersensitivity in a rat model of irritable bowel syndrome. Proc Natl Acad Sci U S A 108:11268–11273
Matsunami M, Tarui T, Mitani K, Nagasawa K, Fukushima O, Okubo K et al (2009) Luminal hydrogen sulfide plays a pronociceptive role in mouse colon. Gut 58:751–761
Matsunami M, Kirishi S, Okui T, Kawabata A (2011) Chelating luminal zinc mimics hydrogen sulfide-evoked colonic pain in mice: possible involvement of T-type calcium channels. Neuroscience 181:257–264
Matsunami M, Kirishi S, Okui T, Kawabata A (2012a) Hydrogen sulfide-induced colonic mucosal cytoprotection involves T-type calcium channel-dependent neuronal excitation in rats. J Physiol Pharmacol 63:61–68
Matsunami M, Miki T, Nishiura K, Hayashi Y, Okawa Y, Nishikawa H et al (2012b) Involvement of the endogenous hydrogen sulfide/Cav3.2 T-type Ca2+ channel pathway in cystitis-related bladder pain in mice. Br J Pharmacol 167:917–928
McGowan E, Hoyt SB, Li X, Lyons KA, Abbadie C (2009) A peripherally acting Nav1.7 sodium channel blocker reverses hyperalgesia and allodynia on rat models of inflammatory and neuropathic pain. Anesth Analg 109:951–958
Messinger RB, Naik AK, Jagodic MM, Nelson MT, Lee WY, Choe WJ et al (2009) In vivo silencing of the Ca(V)3.2 T-type calcium channels in sensory neurons alleviates hyperalgesia in rats with streptozocin-induced diabetic neuropathy. Pain 145:184–195
Miao X, Meng X, Wu G, Ju Z, Zhang HH, Hu S et al (2014) Upregulation of cystathionine-beta-synthetase expression contributes to inflammatory pain in rat temporomandibular joint. Mol Pain 10:9
Miyamoto R, Otsuguro K, Ito S (2011) Time- and concentration-dependent activation of TRPA1 by hydrogen sulfide in rat DRG neurons. Neurosci Lett 499:137–142
Munchberg U, Anwar A, Mecklenburg S, Jacob C (2007) Polysulfides as biologically active ingredients of garlic. Org Biomol Chem 5:1505–1518
Nagasawa K, Tarui T, Yoshida S, Sekiguchi F, Matsunami M, Ohi A et al (2009) Hydrogen sulfide evokes neurite outgrowth and expression of high-voltage-activated Ca2+ currents in NG108-15 cells: involvement of T-type Ca2+ channels. J Neurochem 108:676–684
Nelson MT, Joksovic PM, Perez-Reyes E, Todorovic SM (2005) The endogenous redox agent L-cysteine induces T-type Ca2+ channel-dependent sensitization of a novel subpopulation of rat peripheral nociceptors. J Neurosci 25:8766–8775
Nelson MT, Woo J, Kang HW, Vitko I, Barrett PQ, Perez-Reyes E et al (2007a) Reducing agents sensitize C-type nociceptors by relieving high-affinity zinc inhibition of T-type calcium channels. J Neurosci 27:8250–8260
Nelson MT, Joksovic PM, Su P, Kang HW, Van Deusen A, Baumgart JP et al (2007b) Molecular mechanisms of subtype-specific inhibition of neuronal T-type calcium channels by ascorbate. J Neurosci 27:12577–12583
Nishimura S, Fukushima O, Ishikura H, Takahashi T, Matsunami M, Tsujiuchi T et al (2009) Hydrogen sulfide as a novel mediator for pancreatic pain in rodents. Gut 58:762–770
Ogawa H, Takahashi K, Miura S, Imagawa T, Saito S, Tominaga M et al (2012) H2S functions as a nociceptive messenger through transient receptor potential ankyrin 1 (TRPA1) activation. Neuroscience 218:335–343
Ohge H, Furne JK, Springfield J, Sueda T, Madoff RD, Levitt MD (2003) The effect of antibiotics and bismuth on fecal hydrogen sulfide and sulfate-reducing bacteria in the rat. FEMS Microbiol Lett 228:137–142
Okubo K, Takahashi T, Sekiguchi F, Kanaoka D, Matsunami M, Ohkubo T et al (2011) Inhibition of T-type calcium channels and hydrogen sulfide-forming enzyme reverses paclitaxel-evoked neuropathic hyperalgesia in rats. Neuroscience 188:148–156
Okubo K, Matsumura M, Kawaishi Y, Aoki Y, Matsunami M, Okawa Y et al (2012) Hydrogen sulfide-induced mechanical hyperalgesia and allodynia require activation of both Cav3.2 and TRPA1 channels in mice. Br J Pharmacol 166:1738–1743
Patacchini R, Santicioli P, Giuliani S, Maggi CA (2004) Hydrogen sulfide (H2S) stimulates capsaicin-sensitive primary afferent neurons in the rat urinary bladder. Br J Pharmacol 142:31–34
Perez-Reyes E (2003) Molecular physiology of low-voltage-activated t-type calcium channels. Physiol Rev 83:117–161
Pozsgai G, Hajna Z, Bagoly T, Boros M, Kemeny A, Materazzi S et al (2012) The role of transient receptor potential ankyrin 1 (TRPA1) receptor activation in hydrogen-sulphide-induced CGRP-release and vasodilation. Eur J Pharmacol 689:56–64
Roediger WE, Moore J, Babidge W (1997) Colonic sulfide in pathogenesis and treatment of ulcerative colitis. Dig Dis Sci 42:1571–1579
Rose KE, Lunardi N, Boscolo A, Dong X, Erisir A, Jevtovic-Todorovic V et al (2013) Immunohistological demonstration of Cav3.2 T-type voltage-gated calcium channel expression in soma of dorsal root ganglion neurons and peripheral axons of rat and mouse. Neuroscience 250:263–274
Schicho R, Krueger D, Zeller F, Von Weyhern CW, Frieling T, Kimura H et al (2006) Hydrogen sulfide is a novel prosecretory neuromodulator in the Guinea-pig and human colon. Gastroenterology 131:1542–1552
Sekiguchi F, Kawabata A (2013) T-type calcium channels: functional regulation and implication in pain signaling. J Pharmacol Sci 122:244–250
Sekiguchi F, Miyamoto Y, Kanaoka D, Ide H, Yoshida S, Ohkubo T et al (2014) Endogenous and exogenous hydrogen sulfide facilitates T-type calcium channel currents in Cav3.2-expressing HEK293 cells. Biochem Biophys Res Commun 445:225–229
Streng T, Axelsson HE, Hedlund P, Andersson DA, Jordt SE, Bevan S et al (2008) Distribution and function of the hydrogen sulfide-sensitive TRPA1 ion channel in rat urinary bladder. Eur Urol 53:391–399
Stucky CL, Dubin AE, Jeske NA, Malin SA, McKemy DD, Story GM (2009) Roles of transient receptor potential channels in pain. Brain Res Rev 60:2–23
Takahashi T, Aoki Y, Okubo K, Maeda Y, Sekiguchi F, Mitani K et al (2010) Upregulation of Cav3.2 T-type calcium channels targeted by endogenous hydrogen sulfide contributes to maintenance of neuropathic pain. Pain 150:183–191
Tamizhselvi R, Moore PK, Bhatia M (2007) Hydrogen sulfide acts as a mediator of inflammation in acute pancreatitis: in vitro studies using isolated mouse pancreatic acinar cells. J Cell Mol Med 11:315–326
Taniguchi E, Matsunami M, Kimura T, Yonezawa D, Ishiki T, Sekiguchi F et al (2009) Rhodanese, but not cystathionine-gamma-lyase, is associated with dextran sulfate sodium-evoked colitis in mice: a sign of impaired colonic sulfide detoxification? Toxicology 264:96–103
Terada Y, Fujimura M, Nishimura S, Tsubota M, Sekiguchi F, Nishikawa H et al (2013) Contribution of TRPA1 as a downstream signal of proteinase-activated receptor-2 to pancreatic pain. J Pharmacol Sci 123:284–287
Terada Y, Fujimura M, Nishimura S, Tsubota M, Sekiguchi F, Kawabata A (2014) Roles of Cav3.2 and TRPA1 channels targeted by hydrogen sulfide in pancreatic nociceptive processing in mice with or without acute pancreatitis. J Neurosci Res 93(2):361–369
Theoharides TC, Whitmore K, Stanford E, Moldwin R, O’Leary MP (2008) Interstitial cystitis: bladder pain and beyond. Expert Opin Pharmacother 9:2979–2994
Todorovic SM, Jevtovic-Todorovic V (2011) T-type voltage-gated calcium channels as targets for the development of novel pain therapies. Br J Pharmacol 163:484–495
Todorovic SM, Jevtovic-Todorovic V, Meyenburg A, Mennerick S, Perez-Reyes E, Romano C et al (2001) Redox modulation of T-type calcium channels in rat peripheral nociceptors. Neuron 31:75–85
Trevisani M, Patacchini R, Nicoletti P, Gatti R, Gazzieri D, Lissi N et al (2005) Hydrogen sulfide causes vanilloid receptor 1-mediated neurogenic inflammation in the airways. Br J Pharmacol 145:1123–1131
Velasco-Xolalpa ME, Barragan-Iglesias P, Roa-Coria JE, Godinez-Chaparro B, Flores-Murrieta FJ, Torres-Lopez JE et al (2013) Role of hydrogen sulfide in the pain processing of non-diabetic and diabetic rats. Neuroscience 250:786–797
Wallace JL, Vong L, McKnight W, Dicay M, Martin GR (2009) Endogenous and exogenous hydrogen sulfide promotes resolution of colitis in rats. Gastroenterology 137:569–578
Wantuch C, Piesla M, Leventhal L (2007) Pharmacological validation of a model of cystitis pain in the mouse. Neurosci Lett 421:250–252
Warenycia MW, Goodwin LR, Benishin CG, Reiffenstein RJ, Francom DM, Taylor JD et al (1989) Acute hydrogen sulfide poisoning. Demonstration of selective uptake of sulfide by the brainstem by measurement of brain sulfide levels. Biochem Pharmacol 38:973–981
Xu GY, Winston JH, Shenoy M, Zhou S, Chen JD, Pasricha PJ (2009) The endogenous hydrogen sulfide producing enzyme cystathionine-beta synthase contributes to visceral hypersensitivity in a rat model of irritable bowel syndrome. Mol Pain 5:44
Zhao W, Zhang J, Lu Y, Wang R (2001) The vasorelaxant effect of H2S as a novel endogenous gaseous KATP channel opener. EMBO J 20:6008–6016
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Terada, Y., Kawabata, A. (2015). H2S and Pain: A Novel Aspect for Processing of Somatic, Visceral and Neuropathic Pain Signals. In: Moore, P., Whiteman, M. (eds) Chemistry, Biochemistry and Pharmacology of Hydrogen Sulfide. Handbook of Experimental Pharmacology, vol 230. Springer, Cham. https://doi.org/10.1007/978-3-319-18144-8_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-18144-8_11
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18143-1
Online ISBN: 978-3-319-18144-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)