Abstract
3D printers are small-scale manufacturing facilities in a box. With minimal resources, they enable rapid on-demand production. Cost-effective complex products are made when needed with decreased transportation, storage, and customs costs. The immediate access to medical devices created by 3D printing reduces uncertainty and delivery delays. This paper introduces a pilot project to collaborate with local clinicians and design medical devices with a 3D printer in Haiti. The pilot aimed to empirically ascertain whether locally engaged staff could implement 3D printing of medical devices. This process may be replicated globally and brought to other areas of need. On multiple occasions, we visited three healthcare delivery sites in Haiti. By observing and interviewing medical staff, we identified high-demand supplies with the potential for 3D printed fabrication. We also identified equipments not used due to broken parts that could be easily fabricated. In collaboration with local clinicians, we developed a list of 16 3D printable objects to meet the localized demand in real time. 3DPforHealth launched a 3D printing lab in Haiti and trained local people in design using the Makerbot Rep 1 printers. To demonstrate 3D printing medical application, we collaboratively designed an umbilical cord clamp prototype. Variants of the clamp design were iteratively tested to assure durability and efficacy of grip on multiple materials. The process identified initial concerns of printing medical devices including sanitation, product longevity, reuse of retired materials for new product development, and parameters for responsible human trials. Initial trials demonstrate proof of concept for identification and 3D printed production of much-needed medical devices by collaborating with local clinicians. Further, we were able to train local people in 3D printing design. In recent months, 3DPforHealth has been absorbed into a larger initiative for disaster response manufacturing known as Field Ready (http://www.fieldready.org). We envision Field Ready as a replicable model for countries struggling with similar challenges. Field Ready is now a program that designs solutions that are shared with other resource-constrained environments, bypassing infrastructure and distribution limitations globally.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Medical Device
- International Space Station
- Acrylonitrile Butadiene Styrene
- Local Clinician
- Acrylonitrile Butadiene Styrene
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction and Purpose
The catastrophic Haitian earthquake of 2010 resulted in a death toll estimated to be between 200,000 and 500,000 (Sloand et al. 2013). Providing critical medical care in the desperately short window of time proved to be one of the greatest challenges during the disaster. Injuries and casualties continued even after the initial quake due to the rubble and unsafe terrain (Smith et al. 2012).
Local medical staff shared stories of what they deemed in-humane treatment in moments of crisis. In order to save lives from gangrene and other infection, they were forced to perform amputations using only a bread knife and vodka to disinfect the wound when they ran out of appropriate medical supplies. It is in these critical moments that clean sanitary medical devices are most needed.
During a disaster, there is a crucial 48-h period after a wound is inflicted where proper medical supplies are needed to stop the spread of infections and preventable deaths. Though some supplies were air dropped, much of it could not reach the people who needed it most. Between January 12 and May 31, 2010, Médecins Sans Frontières (MSF), one of the many humanitarian organizations on-the-ground, provided emergency medical care to more than 173,000 patients (MSF 2014). The earthquake destroyed 60 % of the existing health facilities and 10 % of medical staff were either killed or left the country (MSF 2011).
Conflicting reports of death tolls mean that no one knows the true-life cost of the devastation. The country as a whole is still reeling from its effects. Regardless of the numbers, the same question rings: What could be done to prevent this?
Aid to Haiti was overwhelming following the earthquake in January 2010. Since 2010, funding has been greatly reduced and lasting change for the better has not been achieved (Rupar et al. 2013). Poverty, the lack of resources and adequate infrastructure are the greatest challenges facing Haiti. The persisting need for healthcare resources, lack of access, and limitations of the distribution systems in this disaster-stricken country contributes to a steadily increasing toll of preventable deaths.
The current state of Haiti illustrates that while the doors are wide open for collaboration between North and South partners, they are yet to be explored fully. This presents an opportunity for collaborative design initiatives and exponential growth technologies. With the majority of its people living on less than US$2 per day (Buss 2008), very few Haitians can afford healthcare, making it difficult to support small local economies specializing in specialty medical equipment and services.
The great need for health care resources and lack of access to them highlights the challenges and limitations of the distribution systems in this disaster-stricken country. Sustainable design and innovation along with exponential growth technologies can combine to answer the critical questions of “What could be done to prevent this?” and “Why is this still happening?”
Our efforts are dedicated to the belief that the answers lie in our basic assumptions of how proper access to medical care can be acquired. If we can help clinicians gain access to the proper equipment quicker, cheaper, and easier, we have the potential to, on the whole, save thousands of lives daily in disaster-struck areas. Being able to manufacture simple medical devices on-demand when needed has tremendous value for the treatment of patients. Not only will the immediacy of device production save lives but also storage, contamination, and theft risks can be avoided.
By empowering locals to design and create their own tools (through capacity building), we empower them to have an even stronger impact on the lives of those around them. The goal is to create and distribute or share the model of a 3D printing lab that can print much-needed medical devices on-demand. In this lab, we (North) teach local (South) clinicians how to rapidly prototype and produce tools via hyper local digital manufacturing, in particular, small, simple, medical devices that have tremendous value in the immediacy of need. We also aim to eliminate storage risk by reducing waste and contamination. Eventually, we would like to create a system that can be shared and copied freely with other areas providing a sharing model from South to South, not just the typical North to South model.
2 The Need for Technology
There is no denying the great need for medical devices in resource-limited environments such as Haiti. Current limitations facing this pilot program are funding, material resources, lack of technical training, and lack of sufficient infrastructure to access such materials. Every day 800 women die worldwide due to complications with pregnancy and childbirth. Almost 50 % of all the countries surveyed by the World Health Organization (WHO) have less than half the essential medicines needed for basic healthcare in the public sector (GHO 2013). There is a clear calling for this technology with so many in need.
Currently, the Disaster Aid model is to deploy people with general tool kits, as they do not know what they are going to specifically need on the ground. The kits are also dependent on replenishment of supplies, which depends on donors, infrastructure, transport capabilities, and safety of environment. Further, the traditional method of getting aid is a slow and cumbersome method, which can waste materials, money, and time (Chu et al. 2011). The process may involve risk elements in regards to collection of donations, purchasing parts, international shipping, customs, and storage. The latter two adding much time to the process in terms of delays caused by infrastructure and bureaucratic inefficiency (Lancet 2010).
After the earthquake, airports were clogged often with too much congestion by competing nongovernmental organizations (NGOs) deploying unnecessary items (Krin et al. 2010). No one could get through, literally stopping the aid that was on the ground ready to deploy. By using a general-purpose material like plastic in the form of filament that could be made into a variety of tools and supplies, there is a chance this would alleviate some of the issues outlined above.
The scope of this project is greater than just disaster areas and we would like to apply the project to positively benefit limited resource clinics and environments in general. Clinics such as Ti Kay, a TB/HIV clinic, are a perfect example of a rural clinic that is based in a post-disaster zone with limited resources. Based on the grounds of the general hospital in Port-au-Prince, Ti Kay is extremely resource challenged and miraculously serves the poorest of the poor with dignity and respect. Collecting no money from patients, it survives solely on the donations of others. We are working directly with the Ti Kay clinic and they graciously participated in the pilot project.
We, Field ReadyFootnote 1 (which absorbed 3DPforHealth) are developing a platform that can be replicated globally and brought to other areas of need by sharing the designs of tools, customization, and simple fixes on machinery. The platform will share and address solutions that have environmental similarities (such as humidity) by sharing freely online. Locally engaged staff, from clinics in Haiti, will be able to share their experiences with staff based in other countries; and a platform will be facilitated for them to do so.
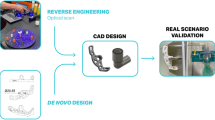
3 Design and Methods
3DPforHealth launched its pilot in Port-au-Prince, Haiti. The location was chosen for its stark healthcare needs, access to medical clinics and professionals, and safe base of operations to operate our machines and design classes. The urban setting promoted a safe environment for teachers, clinicians, and local staff to engage, develop, and learn. The project was based in an established community resource center, Haiti Communitere (North and South), a nongovernmental organization (NGO) focused on response, relief, and renewal. It was established within days of the earthquake.
Partnerships between North and South are critical for the implementation and success of this project. We have done this by piloting in an innovation lab, known as iLab/Haiti, which was founded in a partnership with KIDmob (North). iLab/Haiti is an innovation lab which teaches local Haitian clinicians and unskilled locals (residents of Cité Soleil) creative problem solving skills, design skills, maker skills, and empathy building. While Field Ready focuses on disaster response, KIDmob is dedicated to teaching and developing general curriculum for design.
Over the course of a year, we visited a number of healthcare sites in Haiti. At each site, we observed and interviewed doctors and nurses to identify needs for supplies with the potential to be made with a 3D printer. In addition to basic supplies, we also noticed the number of complex medical devices present but unused because of broken parts. Minor pieces easily produced on a 3D printer are able to restore functionality to this equipment. Some repairs required very simple items in the proper size, like screwdrivers and wrenches. These were easily created during our trials demonstrating that the technology can be used to create any number of useful tools and rehabilitate previously valued devices that had fallen into disrepair.
We worked with a variety of medical stakeholders; local nurses, clinicians, and local residents based in the different areas of Haiti:
-
Ms. Maeve McGoldrick, a disaster response nurse who worked in Haiti juggling clinics in these areas; Ti bois, Williamson and Fond Baptiste in Haiti;
-
Dr. Coffee, Harvard and MIT Infectious Disease specialist at Ti Kay, a TB/HIV clinic;
-
Dr. Julielynn Wong consulting doctor for NASA with experience in 3D printing medical tools for astronauts;
-
Five (formally) uneducated young men from Cité Soleil.
We codeveloped new iterations with local clinicians (South), and tested on a variety of materials and quality with medical professionals (North). We also researched a range of highly effective and more importantly simple medical devices that would have the highest impact.
The advantage of working with clinicians on the ground learning and developing solutions mutually is that we in the North can now provide access and expertise to those in the South so they can codesign or design themselves what is “actually” needed and what is culturally appropriate for their medical needs. We (North) simply do not know, nor can we, the exact needs of the Haitians as they do.
The rural hospitals we worked with identified umbilical cord clamps as a key need. They did so as many births occurred directly after the earthquake, brought on by stress (Blencowe et al. 2010), and clinicians were forced to use shoelaces as umbilical clamps; which presented a contamination risk (UNICEF 2014). After they finished using their shoelaces, they switched to clipping off and using the fingers of their sanitary gloves; which amplified the safety risk for the clinicians as many of the women giving birth were potentially HIV/AIDS positive. The women and children were also at significant risk since umbilical (Ibrahim 2008) cord hemorrhaging (resulting in anemia/death) can also occur if the umbilical cord clamp does not properly occlude one or more of the umbilical vessels (partial clamping of the cord) (Garner et al. 1994).
We designed a prototype of an umbilical cord clamp to demonstrate the concept that 3D printers could be used for localized, on-demand medical device manufacturing. We iteratively designed clamp prototypes to assure their durability and tested the effectiveness of the clamp’s grip on multiple materials. With 58,000 infant deaths in 2010 worldwide due to neonatal tetanus (UNICEF 2014), one can see the tremendous beneficial effect of dissemination and application of this 3D printing lab approach.
4 Results
After establishing partnerships with clinics, 3DPforHealth found that it was possible to design and work side by side with local clinicians to identify and create solutions to address the lack of much-needed medical supplies. 3DPforHealth was then able to work with local clinicians iterating and codesigning medical devices with success. 3DPforHealth has identified a list of 15 medical devices thus far (Table 4.1) which we are confident can be produced with 3D printers. We are focusing on three currently, identified as the most in need by our clinician partners: umbilical cord clamps, oxygen splitters, and IV bag hooks. We found that one of the most important devices needed in the Tuberculosis (Farmer et al. 1991) clinic, Ti Kay, was an oxygen splitter, which we were able to create and test.
IV bag hooks, oxygen splitters, and umbilical cord clamps have been identified and prototypes have been produced with success utilizing a dual extruder Makerbot Replicator 1 in Port-au-Prince, Haiti. This printer was functional, affordable, and suited to the environment due to its durability and ease of repair. Furthermore, as printers become more common a secondary market of used printers has started to emerge.
Some initial barriers to entry may be that initial projected costs may be high for the local clinician, as in Haiti, it may cost too much for a local Haitian in a small clinic to afford. Over time, we believe the 3D printing lab will become more affordable or can be supplied by external aid organizations in the form of a donation. Much depends on how quickly we can move forward and on how much time or how frequently our team can work onsite in our 3D printing labs.
Costs of small-scale 3D printers are dropping drastically. When printers were first released to the public, the machines cost hundreds of thousands of dollars. A decade later, they are accessible to the layman in the western world for some US$499–8,500 with a printing resolution of up to 100 µ. Not only are prices decreasing for commercially available 3D printers, but also people all over the world are creating their own open-source-based printers in new, innovative, and affordable ways.
Kodjo Afate Gnikou, a resourceful inventor from Togo in West Africa, has made a US$100 3D printer which he constructed from parts he scrounged from broken scanners, computers, printers and other e-waste. The fully functional Do It Yourself (DIY) printer cost a fraction of those currently on the market, and saves environmentally damaging waste from reaching landfill site (Popsci 2014).
The technology is becoming more and more affordable to the developing world. With the costs of a filament recycler recently dropping to US$400, it is possible to utilize all scraps and prints gone wrong allowing for a higher degree of efficiency. It implies a range of simple devices, between 500 and 1000 devices, could be produced from one kilo of Acrylonitrile Butadiene Styrene (ABS) plastic as opposed to the traditional 100–300. Further, it is not unrealistic to assume that if we incorporate recycling of used devices, we could produce 2000 simple devices from one kilo of ABS plastic, without degradation of the material (Kickstarter 2013).
We identified initial limitations of printing medical devices on a 3D printer, including concerns about how to sanitize the clamps, when to retire the product, how to reuse the materials of retired clamps for new product development, and how to responsibly test these devices on humans. This pilot is ongoing and staff has been back and forth to Haiti numerous times since January 2013, exploring the options and capabilities available.
To set up a successful 3D printing lab, community engagement is critical. We learned that our expectations should be flexible, as it took longer than anticipated to set up a functioning lab in a new environment. We imagine that it will be even more challenging without having established relationships and trust built before entering the environment. A significant amount of one-on-one time in the early stages is required to ensure that the local participants understand, as translation can be complicated particularly with complex concepts. It can take up to a month to get someone back in the lab to work if holidays are around, or if danger is prevalent, which is quite common in Haiti. To give an example, a number of our locally engaged staff encountered violence in the area during 2013 that directly arrested their participation in design class. We expect the process will become more streamlined as we apply the project to more areas in need.
As with any learned skill, 3D printing can be taught. It is a technical aptitude and some are quicker to adopt the skill set than others. We believe that with the help of a flexible and translatable curriculum, a good deal can be accomplished. In collaboration with local clinicians, we developed a list of 15 objects that can be made with a 3D printer to meet the localized demand in real time. We also successfully trained local people to design in 3D, using the Makerbot 3D printers. We learned the process of designing a medical device on a 3D printer collaboratively with locally engaged staff.
We believe it is viable to create a self-sustaining design lab based on 3D printing technologies, but it will take time to get it off the ground. In the future, it will be more streamlined. Setting up the labs will be much easier after all research has been completed alongside user experience materials, such as pictorial directions and a premade suggested kit (3D printer and other tools) is established with an initial investment amount. This will also include a recycler so that materials may be reused lowering the cost of production even further, and reducing waste along the way.
As detailed in Table 4.2, one of the most interesting results of this project is the comparable price to traditional methods and in some cases an extreme reduction of cost. To achieve the same economies of scale with traditional clamps (sans shipping/customs/storage) 10,000 pieces must be ordered at one time. This makes 3D printing a much more affordable alternative as a rural clinic is unlikely to need 10,000 clamps in any short horizon of time, nor is it likely to have the space needed to store 10,000 clamps securely.
With the potential of recycling and a dual nozzle extruder, one can further cut down on costs. Recycling is yet to be fully proven out, but if the project can include this technology on the basic 3D printing lab, we will be able to collect used (as well as broken or worn down) medical devices, sterilize them, grind them down to be recycled, and used to create new devices. The advantage of having a dual nozzle extruder on the printer provides the ability to print two different types of plastic simultaneously: external material with raw virgin ABS and the internal core support out of recycled plastic to ensure durability of the device.
For the purposes of this project, it appears that ABS filament is the superior filament option as it is the sturdiest and most dependable material we can easily access. It also has the advantage that it can be recycled. The aim is to further test how many times one can recycle the filament, which would ideally lead to a closed loop system for medical devices.
After one of the umbilical cord clamps have been used, they can be sanitized, ground up, recycled, and be reused and reprinted an unknown amount of times. After two uses, the cost of the 3D printer filament already pays for itself. It is unknown how many times the plastic can be recycled, but it is safe to say that it can be done at least two to three times without any serious degradation of the plastic.
We believe that our 3D printing lab will be easy to transport with volunteers carrying 3D printers and filament in their travel luggage as opposed to shipping them in. Filament packages are so small that as volunteers cycle through an aid project, more can be brought in luggage without having a significant impact on their luggage dimensions and weight. To get materials into Haiti we have tested a system to address low material supply by having volunteers carry a kilo of ABS with them each time they enter the country. In this manner, we have a steady stream of supplies coming in. Boards on 3D printers can fail and replacements are hard to come by; to address this issue, we have volunteers bring extra parts and used back up machines.
Access to electricity is problematic and without a dependable power source, we are not able to guarantee any short-term result for medical devices needed. This is a key concern to consider in the design of this project.
We also need to consider the risks arising from the proper sterilization of tools as we could encounter cross contamination that could then lead to illness. Once we have set the process for sterilization, which we are currently investigating alongside our clinician partners, and created user experience materials to provide a pathway for learning there are still risks with people not following directions or taking shortcuts. This is where legal and quality assurance built into the process is key. We are going to build into the design a method that allows users to know when the tool or device is past its prime as well as ample warning that they must follow all directions explicitly.
One item that is not fully addressed in this paper, and is still under study for is device patents. At this point, we do not consider patent infringement to be an issue as none of these parts are being sold, and further, the majority of designs will be designed independently of existing patents via collaboration of North South partners. Some items will be completely redesigned for more appropriate functionality for the need at hand. This will be an ongoing area of study to ensure that we mitigate legal risk for the project.
We anticipate that designs must be tested and tweaked repeatedly in a variety of environments: social, geographical, and climate. Designs must be quality assessed on the development end and we will need to requality test devices in each location due to a variety of factors: heat, humidity, skill level of clinician, quality of printer, and the final quality of print. We are looking into how to create a sufficient feedback loop now. We have done experimenting on this front that are currently in trials; for example, with the umbilical cord clamps, mothers must return the clamp as payment for a secondary check up on the infant.
Another small hindrance may be the time to manufacture for complicated pieces. This can sometimes take up to an hour and a half and constant power is required for a stable print. Finally, because most 3D printers are deployed in the developed world where access to reliable power is not an issue, there is a stark lack of research in this area. We intend to publish our results to improve the knowledge base of the international aid community.
Power access is a big hindrance and we may need access to a high-quality generator to ensure continuous power, as well as a Uninterrupted Power Supply (UPS), to handle momentary lapses of power so as not to disturb the 3D printer as it prints. We are currently in the process of investigating the possibility of using a specialty solar kit and battery to power the 3D printers. Many options will become more available as prices lower and dependability increases. We view durability as the key issue here as we do not want to create a 3D printing lab that will break down easily or require replacement parts frequently.
The ethical and health impact of testing on humans in this area is currently unclear. While patients may require a medical device, we do not intend nor will we, deploy a medical device which has the potential to cause harm. We are also extremely mindful to consider after care. Finding patients to test on (once we ascertain there are no health risks) will be critical to success but we have to be cautious of intentional or unintentional coercion. Currently, the clinician asks the patient for their consent, and the patient may accept or decline; keeping in mind that the patient may fear not receiving health care if they do not go along with the experiment.
We are also working on preventing theft. Our experiences show that by making sure our local team feels valued and important, we can reduce the loss of equipment through theft. We are also sensitive about power dynamics particularly amongst foreigners and locals. Some of these dynamics may not be obvious. We have found that our locally engaged teams provide insights that are invaluable in terms of designing great local solutions, and while they may not realize it, we try to help them understand their capabilities and strengths.
5 Conclusions
Our ongoing pilot project continues to demonstrate that it is possible to collaborate with local clinicians to identify requirements for much-needed medical devices which can be made with a 3D printer. Further, we were able to meet the goal of training local people to design with 3D printers. Field Ready has been founded in part to develop and deploy an easily replicable model for other countries struggling with similar challenges. We will be a site that can design solutions to be shared with other resource-constrained environments, bypassing infrastructure and distribution limitations.
We are also confident that our model will work in other locations in the future; however, this will require much study to see how the model can be applied with partners globally. We are working to illustrate the Haiti use case and further develop our open source “Disaster Tool Kit.” We are working to establish a feedback loop, where devices, Frequently Asked Questions (FAQs), and curriculum can be shared and updated with ease; so that all parties can benefit from the learning achieved. We believe that this method will allow locals on the ground to save lives with medical device production, rather than being limited to dependence on the few formally trained aid workers in the area that have access to traditionally sourced devices and supplies.
We also intend to work with other professionals to gain their expertise and advice. Made in Space is exploring 3D printing capabilities on the International Space Station (ISS); and will be launching as early as summer 2014. Their user case is quite similar to ours given the resource deprived nature of their situation; astronauts are going to use 3D printers to print replacement parts and tools when needed without having to wait for the next rocket launch. If the ISS is in need of a fix that they simply cannot solve themselves, they can now reach out to a network of other experts and engineers on the ground to create a solution who will email them the fix. This is similar to what we are trying to achieve with our project in Haiti.
We intend to study the lifetime of devices and recycling capabilities, other devices that may be useful in clinics, and other printing materials we can use. We are also going to research which medical devices are being produced locally so we do not compete with local industry; to prevent the oft-made mistake of out competing local production and shutting down local industry.
This approach also pushes parts and designs to new limits enabling novel medical capabilities to arise locally. Material innovations will provide new areas of exploration. For example, in the near future, we intend to print O-rings and custom silicone fittings of a variety of different sizes as needed. We also aim to create a downloadable catalogue of devices and parts. When a lab needs a specifically sized tool, part, or device in a disaster scenario, there will be a large variety to choose from as the basis for customization. Taken together, there is also an added benefit where a larger variety of materials, designs, and machines can be used to replace parts and convert or modify previously donated pieces, regardless of manufacturer, into valuable capabilities.
We believe that 3D printers represent a major technological sidestep to traditional manufacturing methods and infrastructure restrictions, similar to that of mobile phones over traditional copper wire networks. When the power of the Internet, computers, and 3D printers are put to use, the North and South can finally share a new healthier and innovative future.
Notes
References
Blencowe, H., Lawn, J., Vandelaer, J., Roper, M., & Cousens, S. (2010). Tetanus toxoid immunization to reduce mortality from neonatal tetanus. International Journal of Epidemiology, 39(1): Suppl 1:i102-9). doi: 10.1093/ije/dyq027.
Buss, T. F. (2008). Haiti in the balance: Why foreign aid has failed and what we can do about it. Washington, DC: Brookings Institution Press and the National Academy of Public Administration.
Chu, K., Stokes, C., Trelles, M., & Ford, N. (2011). Improving effective surgical delivery in humanitarian disasters: Lessons from Haiti. PLoS Medicine, 8(4), e1001025. doi:10.1371/journal.pmed.1001025.
Farmer, P., Robin, S., Ramilus, S. L., & Kim, J. Y. (1991). Tuberculosis, poverty, and “compliance”: lessons from rural Haiti. Seminars in Respiratory Infections, 6(4), 254–260.
Garner, P., Lai, D., Baea, M., Edwards, K., & Heywood, P. (1994). Avoiding neonatal death: An intervention study of umbilical cord care. Journal of Tropical Pediatrics, 40(1), 24–28.
Global Health Observatory (GHO). (2013). World health statistics. http://www.who.int/gho/publications/world_health_statistics/2013/en/. Accessed 1 Feb 2014.
Ibrahim, C. P. (2008). Hypotension in preterm infants. Indian Pediatrics, 45(4), 285–294.
Kickstarter. (2013). Filabot: Plastic filament maker. http://www.kickstarter.com/projects/rocknail/filabot-plastic-filament-maker. Accessed 12 Dec 2013.
Krin, C. S., Giannou, C., Seppelt, I. M., Walker, S., Mattox, K. L., et al. (2010). Appropriate response to humanitarian crises. BMJ, 340, c562. doi:10.1136/bmj.c562.
Lancet. (2010). Growth of aid and the decline of humanitarianism. Lancet, 375(9711), 253. doi:10.1016/S0140-6736(10)60110-9.
Médecins Sans Frontières (MSF). (2014). Haiti overview. http://www.doctorswithoutborders.org/country-region/haiti. Accessed 1 Feb 2014.
Médecins Sans Frontières (MSF). (2011). Haiti one year after: Looking ahead—plans and perspectives. http://www.msf.org/article/haiti-one-year-after-looking-ahead-plans-and-perspectives. Accessed 1 Mar 2014.
Popsci. (2014). West African inventor makes a $100 3D printer from e-waste. http://inhabitat.com/west-african-inventor-makes-a-100-3d-printer-from-e-waste/diy-3d-printer/. Accessed 1 Dec 2014.
Rupar, E., Hussain, S., &King, S. (2013). Making poverty history winter 2012: Part 2 where is your money going? Examining post crisis aid relief in Haiti. http://hdl.handle.net/10214/7643. Accessed 1 Dec 2013.
Sloand, E., Ho, G., & Kub, J. (2013). Experiences of nurse volunteers in Haiti after the 2010 earthquake. Research and Theory for Nursing Practice, 27(3), 193–213.
Smith, R. M., Dyer, G. S. M., Antonangeli, K., Arredondo, N., Bedlion, H., Dalal, A., et al. (2012). Disaster triage after the Haitian earthquake. Injury, 43(11), 1811–1815.
UNICEF. (2014). Elimination of maternal and neonatal tetanus. http://www.unicef.org/health/index_43509.html. Accessed 1 Feb 2014.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this paper
Cite this paper
Dotz, A.D. (2015). A Pilot of 3D Printing of Medical Devices in Haiti. In: Hostettler, S., Hazboun, E., Bolay, JC. (eds) Technologies for Development. Springer, Cham. https://doi.org/10.1007/978-3-319-16247-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-16247-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16246-1
Online ISBN: 978-3-319-16247-8
eBook Packages: EnergyEnergy (R0)