Abstract
The novel coronavirus outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was recognized in late 2019 in Wuhan, China. Subsequently, the World Health Organization declared coronavirus disease 2019 (COVID-19) as a pandemic on 11 March 2020. The proportion of potentially fatal coronavirus infections may vary by location, age, and underlying risk factors. However, acute respiratory distress syndrome (ARDS) is the most frequent complication and leading cause of death in critically ill patients. Immunomodulatory and anti-inflammatory agents have received great attention as therapeutic strategies against COVID-19. Here, we review potential mechanisms and special clinical considerations of supplementation with curcumin as an anti-inflammatory and antioxidant compound in the setting of COVID-19 clinical research.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
11.1 Introduction
The novel coronavirus outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was recognized in late 2019, following announcement of a cluster of pneumonia cases in Wuhan, China [1]. World Health Organization declare coronavirus disease 2019 (COVID-19) as a pandemic on 11 March 2020 [2]. According to published reports, the proportion of potentially fatal infections may vary by location, age, and underlying risk factors [3]. Acute respiratory distress syndrome (ARDS) is the most frequent complication and leading cause of death in severely ill patients. Cytokine release syndrome characterized by elevated serum levels of proinflammatory cytokines including interleukin (IL)-6, IL-1β, IL-2, IL-8, IL-17, granulocyte colony-stimulating factor (G-CSF), granulocyte-macrophage colony-stimulating factor (GM-CSF), interferon-inducible protein 10 (IP-10), monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein 1α (MIP-1α), and tumor necrosis factor α (TNF-α) was detected in severe cases of COVID-19 [1, 4, 5]. Unrestrained immune activation and subsequent systemic inflammation result in diffuse alveolar damage and pulmonary capillary endothelial injury that recognized as ARDS [6]. As a consequence, immunomodulatory and anti-inflammatory agents have received great attention in therapeutic strategies for COVID-19[5].
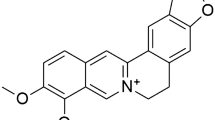
Turmeric, as a precious spice obtained from Curcuma longa rhizomes, has a remarkable history in traditional herbal medicine. Curcumin (diferuloylmethane) is a bioactive polyphenolic ingredient of turmeric with manifold pharmacological effects including potent anti-inflammatory and antioxidant properties [7,8,9,10,11,12,13,–14]. Studies demonstrated that curcumin shows anti-inflammatory, antioxidant and antineoplastic properties through regulation of cytokines, transcription factors, adhesion molecules and enzymes. Due to such properties, some studies are being conducted to evaluate the probable clinical profit of curcumin for the treatment of COVID-19. In the current study, we focused on probable mechanisms of curcumin against ARDS and acute lung inflammation (ALI) and discussed the special clinical considerations of curcumin supplementation in patients with COVID-19.
11.2 COVID-19-Associated ARDS and Related Cytokines
ARDS is a serious lung inflammatory disorder which mortality rate is estimated to be 30–50% [15]. It was described as a syndrome accompanied by inflammation and enhanced permeability of pulmonary capillary endothelial cells followed by fluid leakage into lung parenchyma and activation of inflammatory responses leading to ALI [16]. It was demonstrated that the severity of ARDS directly depends on the magnitude of induced inflammatory responses [17].
Recent studies reported that the cytokine profile of COVID-19 is similar to ARDS and sepsis. Besides, studies confirmed the relevance of elevated levels of inflammatory cytokines with poor prognosis of COVID-19 patients [18]. The inflammatory cytokines that playing key roles in development and progression of ARDS, are introduced here to better understand the relying mechanisms of curcumin in Table 11.1.
TNF-α and IL-1β are among the first proinflammatory cytokines released into the systemic circulation in response to an infectious stimulus. It was demonstrated that TNF-α and IL-1β both activate neutrophils and in sepsis, they are released within 30–90 min from exposure to lipopolysaccharides (LPS) which stimulate the release of the second inflammatory cascade including cytokines, reactive oxygen species (ROS), and upregulation of cell adhesion molecules. Thereupon, inflammatory cells adhere to vascular endothelial cells and migrate into tissues [19]. Moreover, it was shown that TNF-α caused multi-organ damage through the recruitment of neutrophils [20].
The nuclear factor kappa B (NF-κß) plays a critical modulatory role in the transcription of adhesion molecules, cytokines and other mediators involved in the function of immune system, inflammatory and acute responses, recruitment of leucocytes to extravascular tissues [21]. The NF-κß is mainly composed of two subunits which are sequestered in the cytoplasm through integration with I-κß [22]. When activation mediators such as TNF-α or IL-1β are bound to their receptors, I-κß becomes phosphorylated resulting in activation of NF-κß. Afterwards, the complex translocate to the nucleus where enhancing the transcription of its target genes. Rather than TNF-α and IL1 β, viral and bacterial products such as double stranded RNA, LPS, and free radicals are potent inducers of NF-κß [23]. Studies demonstrated that enhanced activation of NF-κß pathway results in increased cell viability and decreased apoptosis. In fact, enhanced viability of activated neutrophils in the lung tissue of patients with ARDS, leads to more production of ROS and proinflammatory cytokines which might preserve and prolong pulmonary inflammatory process [24]. Actually, neutrophils play a fundamental role in the development and progression of ARDS. Previous studies confirmed that accumulation of alveolar neutrophils correlated with enhanced lung permeability, hypoxemia, and low survival rates. Increased amount of neutrophils in airspaces led to microvascular and lung tissue damage. IL-8 is also a potent neutrophil attractant which plays a significant role in ALI/ARDS [25]. Reactive oxygen and nitrogen species (ROS and RNS, respectively) are produced by lung endothelial cells, alveolar cells and airway epithelial cells, neutrophils, and macrophages which lead to increased endothelial permeability promoting the migration of polymorphonuclear leukocytes (PMNs) and fluid into the alveolar lumen. This process finally stimulates the release of proinflammatory agents, expression of adhesion molecules needed for leukocyte recruitment and neutrophil migration promoting the lung injury [17, 26].
IL-6 is secreted by almost all stromal cells and immune cells such as macrophages, monocytes and T/B lymphocytes [27]. The presence of IL-6 and other inflammatory agents is essential for host defense against infections. However, elevated levels of IL-6 can lead to severe acute systemic inflammatory responses named cytokine release syndrome (CRS) [28]. Studies indicated that sustained release of IL-6 is correlated with serum viral RNA load in COVID-19 patients which is correlated to disease severity [29]. Additionally, high serum levels of IL-6 in acute phase of disease were associated with lung lesions in coronavirus infected patients [30]. As a result, ongoing clinical trials of tocilizumab (a humanized monoclonal antibody against IL-6 receptor) in severe COVID-19 cases are being conducted worldwide. In contrast, IL-10 is an anti-inflammatory cytokine which suppresses the release of proinflammatory cytokines such as TNF-α, IL-1β and IL-6, thereby limiting the damage to the host tissues [31].
Macrophages play a dual role in ALI and ARDS. In the acute phase, resident alveolar macrophages’ main phenotype is M2 which shift into M1 phenotype and release potent proinflammatory cytokines such as interferon gamma (IFN-γ), TNF-α, and IL-1β that demonstrate inflammatory effects in the early stage of disease. Besides, blood monocytes are also recruited which finally differentiate to M1 macrophages. In the later stage of ALI/ARDS, macrophages differentiate into M2 phenotype which is regulated through the release of IL-4, IL-10, IL-13, signal transducer and activator of transcription 6 (STAT6), and interferon regulatory factor 4 (IRF4). This process finally leads to elimination of debris, pathogens and apoptotic cells exhibiting an anti-inflammatory effect [32].
The results of a clinical trial in critically ill patients with ALI/ARDS demonstrated that the levels of inflammatory biomarkers including inflammatory cytokines (IL-6 and IL-8), protein C, surfactant protein D (SP-D), intercellular adhesion molecule 1 (ICAM-1), plasminogen activator inhibitor (PAI), tumor necrosis factor receptor (TNFR), and von Willebrand factor (VWF) were significantly lower in surviving patients when compared to non-survivors. However, among all these, the best prognostic biomarkers were IL-8 which is a potent neutrophil attractant and SP-D [33].
Immune system possesses a complex structure and describing all the details of known mechanisms involved in ARDS pathophysiology is so intricate. The main purpose of this part was to classify inflammatory and anti-inflammatory biomarkers and to briefly describe the role of each cytokine in the process to better understanding the potential pathways that curcumin involves and modulates the immune system responses.
11.3 Potential Anti-Inflammatory Mechanisms of curcumin Against ARDS
Studies have indicated that curcumin shows anti-inflammatory, antioxidant and anti-neoplastic activities [34, 35] which are regulated through several molecular targets such as cytokines (e.g. TNF-α, IL-10, IL-6), transcription factors (e.g. NF-κß), enzymes (e.g. matrix metalloproteinases [MMPs]) and adhesion molecules (e.g. ICAM-1) playing key roles in inflammation and carcinogenesis [36]. In this part we are going to study the effects and anti-inflammatory mechanisms of curcumin in the setting of ALI/ARDS resulted by different underlying causes.
Sepsis, severe pneumonia, aspiration, toxic inhalation and trauma are the major underlying conditions leading to ARDS [17]. Xiao et al. prepared rat models of sepsis-induced ALI using cecal ligation puncture (CLP) model. Then, they studied the effect of different doses of curcumin on various cytokines’ concentrations and the final survival rate. The results revealed that the use of curcumin downregulated the pro-inflammatory cytokines such as TNF-α and IL-8. Besides, the results showed that the treatment with curcumin led to improvement of the survival rate by 40–50% in CLP induced ALI model [37]. Additionally, it reduced the oxidative stress in the lung tissue through reduction of myeloperoxidase (MPO), malondialdehyde (MDA) and enhancement of superoxide dismutase (SOD) activity. As demonstrated above, ROS react with macromolecules, produce lipid peroxidases and mutate DNA leading to host tissues toxicity. SOD is an anti-oxidant enzyme which scavenges superoxide substrate and studies demonstrated that its concentration is decreased in sepsis induced ARDS.
In a rat model of intestinal ischemia and reperfusion induced ALI, oral treatment with curcumin further confirmed the antioxidant activity of curcumin. The results indicated the reduction of elevated tissue MDA levels, enhancement of SOD and glutathione peroxidase. Also there was a significant reduction in inducible nitric oxide synthase activity and enhanced the expression of SP-D in lung tissue [38]. SP-D plays vital roles in innate host defense of the lung tissue and regulates surfactant homeostasis [39].
Another interesting mechanism was highlighted in a study by chai et al. They showed that curcumin promoted T regulatory (Treg) cells differentiation and enhanced Treg-derived IL-10 in serum and broncho-alveolar lavage fluid (BALF). Enhancement of Treg-derived IL-10 is the main factor affecting macrophage polarization and conversion of M1 macrophages to M2 [40].
Madathilparambil et al. demonstrated that the administration of cyclodextrin-curcumin complex in LPS induced ALI in mice led to reduced pulmonary edema and neutrophil accumulation in BALF and lung tissue. Besides, the proinflammatory transcription factor, NF-κß was decreased causing the reduction of severe inflammation and lung injury [41]. Qingquan et al. showed that the levels of cytokine-induced neutrophil chemoattractant-1 (CINC-1) in rat model of LPS induced ALI was remarkably increased. They demonstrated that curcumin pretreatment resulted in inhibition of lung CINC-1 expression leading to suppression of neutrophil recruitment and activity in the lung tissue [42].
High-mobility group box 1 (HMGB1) is one of the important inflammatory inducers which is produced by activated monocytes and macrophages. Binding of HMGB1 to receptor for advanced glycation end products (RAGE) stimulates NF-κß signaling pathway, promoting the expression of pro-inflammatory cytokines. Studies indicated that the administration of curcumin to the rat model of LPS-induced ALI led to upregulation of peroxisome proliferator-activated receptor γ (PPAR γ) pathway, further inhibiting the HMGB/RAGE pro-inflammatory pathway [43].
Avasarala and collogues also demonstrated that the use of curcumin affects both pro-inflammatory and anti-inflammatory biomarkers causing a remarkable decrease in development of ARDS and lung injury [44]. They showed that the mechanism was regulated through downregulation of NF-κß and reduction of transforming growth factor beta (TGF-ß) receptor II in virus-induced ARDS resulting in inhibition of inflammatory responses and further lung fibrosis.
Taken together, the precise modulatory mechanisms of curcumin in ARDS has not been defined yet. However, in the current section, we pointed out some of the prominent pathways by which curcumin affects the inflammatory cascade in ARDS.
11.4 Curcumin Formulations
Multiple drug delivery systems such as micelles, liposomes, phospholipid complexes, emulsions, micro-emulsions, nano-emulsions, solid lipid nanoparticles, nanostructured lipid carriers, biopolymer nanoparticles, and micro-gels have been formulated to enhance oral absorption, bioavailability, and therapeutic outcomes of curcumin. Compared with unformulated curcumin, significant enhancement of absorption and bioavailability have been obtained with the micellar and micronized formulations (>100-fold) [45,46,–47].
11.5 Curcumin Dosage
Although the results from both in-vivo and in-vitro studies on curcumin have been promising, clinical trials in patients with viral pneumonia and/or ARDS have not yet been reported. Therefore, in case of curcumin supplementation in COVID-19 patients with or without ARDS, it should be used in typical doses for other medical conditions ranging from 500–4000 mg per day [7, 48]. However, dose adjustment should be made with respect to bioavailability-enhanced preparations as these formulae may cause systemic concentrations in the order of hundreds to thousands of times higher those obtained with unformulated curcumin.
11.6 Common Adverse Effects Between COVID-19 and Curcumin
Previous studies have been investigated the safety and clinical benefits of curcumin in a broad range of diseases including gastrointestinal diseases, rheumatic diseases, pulmonary diseases, diabetes, cardiovascular diseases, liver diseases, pancreatic diseases, neurologic and neurodegenerative diseases, infectious disease and malignancies [7, 8, 49,50,51,52]. In accordance with the results of clinical trials, curcumin has a long-established record of tolerability and safety in human studies. An acceptable daily intake (ADI) of 0–3 mg/kg of body weight per day for curcumin was established by JECFA (The Joint United Nations and World Health Organization Expert Committee on Food Additives) and EFSA (European Food Safety Authority) [7, 53]. Although generally well tolerated, curcumin may cause mild nausea, dyspepsia, diarrhea, yellow stool, headache, and rash in some patients [54,55,56]. Nausea, diarrhea, rash, and headache occur in patients with COVID-19 as well. Therefore, initiation of curcumin supplementation in patients with COVID-19 may increase the risk or intensity of mentioned side effects. Furthermore, curcumin supplementation causes increased bile formation and demonstrates cholekinetic effects [57, 58]. Moreover, curcumin presents antiplatelet, anticoagulation, and fibrinolysis activities [59, 60]. In addition, curcumin supplementation increases insulin sensitivity and subsequently leads to lower blood glucose levels among diabetic patients who were taking diabetes medications [61, 62]. As a result, curcumin supplementation should be avoided in COVID-19 patients with gallbladder diseases, bleeding disorders, and diabetes.
11.7 Clinically Significant Drug Interaction Between Curcumin and Conventional Medications
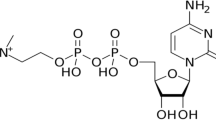
Natural products including herbal medications and dietary supplements can interact with co-administered conventional medications, potentially lead to unexpected side effects, toxicity, and/or suboptimal therapeutic responses [63, 64]. Also curcumin is a safe natural product, clinically significant drug interactions must be avoided in the setting of clinical trials especially in critically ill patients with polypharmacy. Curcumin supplementation can lead to reduced activities of cytochrome p450 monooxygenase (CYP1A1, 2A6, 1B1, 2B6, 2C9, 2C19, 2D6, 2E1, and 3A4), P-glycoprotein (P-gp), organic anion-transporting polypeptide (OATP), glutathione-S-transferase (GST), and uridine dinucleotide phosphate glucuronosyltransferases (UDPG) [65,66,67,68]. Clinically important drug interactions of curcumin are summarized in Table 11.2. Although, limited trials have investigated the pharmacokinetic and/or pharmacodynamic interactions between curcumin and conventional medications. We recommend to exclude the COVID-19 patients who take listed medications from curcumin supplementation trials. However, included patients must be investigated and monitored closely due to the lack of adequate and well-designed clinical trials that investigate the pharmacokinetic and pharmacodynamic drug interactions between curcumin and other conventional medications. Furthermore, there is possible drug interactions between curcumin and antiviral agents for the treatment of COVID-19. For example, remdesivir is an adenosine nucleotide prodrug that converted to the pharmacologically active nucleoside triphosphate form (GS-443902) into cells and subsequently intervene in the viral RNA-dependent RNA polymerase action. Remdesivir is metabolized by CYP (2C8, 2D6, and 3A4), OATP1B1/1B3, and P-glycoprotein/ABCB1 enzyme systems [69,70,71]. So, pharmacokinetic drug interactions are possible in patients who administrated curcumin and COVID-19 specific therapies. Although, clinical data are not available in this area.
11.8 Conclusion
Ongoing COVID-19 pandemic is the pressing global health challenge of our time and our information about COVID-19 is being updated almost on a daily basis. Immunomodulatory and anti-inflammatory agents have received great attention during this period of time based on the inflammatory nature of disease. However, one should minimize any unnecessary co-medication in the setting of COVID-19 due to the lack of clinical and/or experimental information and potential risk of toxicity. We suggest not using curcumin supplementation outside of the setting of clinical trials given the lack of clear clinical evidences on the benefit of curcumin in COVID-19 patients. Further clinical investigations should be performed to clarify the role of curcumin supplementation in the setting of COVID-19. It is also unknown if curcumin can help the patients during the initial phase of the disease or might be more effective in later phases to ameliorate complications.
References
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223):497–506
Acuti Martellucci C, Flacco ME, Cappadona R, Bravi F, Mantovani L, Manzoli L (2020) SARS-CoV-2 pandemic: an overview. Adv Biol Reg 77100736
Clark A,Jit M,Warren-Gash C,Guthrie B,Wang HHX,Mercer SW et al. (2020) Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health
Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R (2020) The COVID-19 cytokine storm; what we know so far. 11(1446)
Zhong J, Tang J, Ye C, Dong L (2020) The immunology of COVID-19: is immune modulation an option for treatment? Lancet Rheumatol 2(7):e428–e436
Ware LB, Matthay MA (2000) The acute respiratory distress syndrome. N Engl J Med 342(18):1334–1349
Hewlings SJ, Kalman DS (2017) Curcumin: a review of Its’ effects on human health. Foods 6(10)
Hassanzadeh S, Read MI, Bland AR, Majeed M, Jamialahmadi T, Sahebkar, A (2020) Curcumin: an inflammasome silencer. Pharmacol Res 159:104921. https://doi.org/10.1016/j.phrs.2020.104921
Panahi Y, Ahmadi Y, Teymouri M, Johnston TP, Sahebkar A (2018) Curcumin as a potential candidate for treating hyperlipidemia: A review of cellular and metabolic mechanisms. J Cell Physiol 233(1):141–152
Mollazadeh H, Cicero AFG, Blesso CN, Pirro M, Majeed M, Sahebkar A (2019) Immune modulation by curcumin: the role of interleukin-10. Crit Rev Food Sci Nutr 59(1):89–101
Momtazi AA, Derosa G, Maffioli P, Banach M, Sahebkar A (2016) Role of microRNAs in the therapeutic effects of Curcumin in non-Cancer diseases. Mol Diagnosis Therapy 20(4):335–345
Iranshahi M, Sahebkar A, Hosseini ST, Takasaki M, Konoshima T, Tokuda H (2010) Cancer chemopreventive activity of diversin from Ferula diversivittata in vitro and in vivo. Phytomedicine 17(3-4):269–273
Ghandadi M, Sahebkar, A (2017) Curcumin: An effective inhibitor of interleukin-6. Curr Pharm Des 23(6):921–931
Teymouri M, Pirro M, Johnston TP, Sahebkar A (2017) Curcumin as a multifaceted compound against human papilloma virus infection and cervical cancers: a review of chemistry, cellular, molecular, and preclinical features. Biofactors 43(3):331–346
Rodríguez-González R, Ramos-Nuez Á, Martín-Barrasa JL, López-Aguilar J, Baluja A, Álvarez J et al (2015) Endotoxin-induced lung alveolar cell injury causes brain cell damage. Exp Biol Med (Maywood) 240(1):135–142
Gonzales JN, Lucas R, Verin AD (2015) The acute respiratory distress syndrome: mechanisms and perspective therapeutic approaches. Austin J Vasc Med 2(1)
Bhatia M, Moochhala S (2004) Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. J Pathol 202(2):145–156
Wilson JG,Simpson LJ,Ferreira A-M,Rustagi A,Roque J,Asuni A et al. (2020) Cytokine profile in plasma of severe COVID-19 does not differ from ARDS and sepsis. 2020.2005.2015.20103549
Wrigge H, Stüber F, Putensen C (2001) Ventilator-associated systemic inflammation. Springer, Berlin Heidelberg, pp 35–43
Johnson BL 3rd, Goetzman HS, Prakash PS, Caldwell CC (2013) Mechanisms underlying mouse TNF-α stimulated neutrophil derived microparticle generation. Biochem Biophys Res Commun 437(4):591–596
Tran K, Merika M, Thanos D (1997) Distinct functional properties of IkappaB alpha and IkappaB beta. Mol Cell Biol 17(9):5386–5399
May MJ, Ghosh S (1998) Signal transduction through NF-κB. Immunol Today 19(2):80–88
Sun Z, Andersson R (2002) NF-kappaB activation and inhibition: a review. Shock 18(2):99–106
Parsey MV, Kaneko D, Shenkar R, Abraham E (1999) Neutrophil apoptosis in the lung after hemorrhage or endotoxemia: apoptosis and migration are independent of IL-1beta. Clin Immunol 91(2):219–225
Miller EJ, Cohen AB, Nagao S, Griffith D, Maunder RJ, Martin TR et al (1992) Elevated levels of NAP-1/interleukin-8 are present in the airspaces of patients with the adult respiratory distress syndrome and are associated with increased mortality. Am Rev Respir Dis 146(2):427–432
Kellner M, Noonepalle S, Lu Q, Srivastava A, Zemskov E, Black SM (2017) ROS signaling in the pathogenesis of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). Adv Exp Med Biol 967:105–137
Magro G (2020) SARS-CoV-2 and COVID-19: is interleukin-6 (IL-6) the ‘culprit lesion’ of ARDS onset? What is there besides Tocilizumab? SGP130Fc. Cytokine: X 2(2):100029
Buonaguro FM, Puzanov I, Ascierto PA (2020) Anti-IL6R role in treatment of COVID-19-related ARDS. J Transl Med 18(1):165
Chen W, Lan Y, Yuan X, Deng X, Li Y, Cai X et al (2020) Detectable 2019-nCoV viral RNA in blood is a strong indicator for the further clinical severity. Emerg Microbes Infect 9(1):469–473
Hsueh PR, Chen PJ, Hsiao CH, Yeh SH, Cheng WC, Wang JL et al (2004) Patient data, early SARS epidemic, Taiwan. Emerg Infect Dis 10(3):489–493
Saraiva M, O’Garra A (2010) The regulation of IL-10 production by immune cells. Nat Rev Immunol 10(3):170–181
Huang X, Xiu H, Zhang S, Zhang G (2018) The role of macrophages in the pathogenesis of ALI/ARDS. Mediat Inflamm 20181264913
Ware LB, Koyama T, Billheimer DD, Wu W, Bernard GR, Thompson BT et al (2010) Prognostic and pathogenetic value of combining clinical and biochemical indices in patients with acute lung injury. Chest 137(2):288–296
Alibolandi M, Mohammadi M, Taghdisi SM, Abnous K, Ramezani M (2017) Synthesis and preparation of biodegradable hybrid dextran hydrogel incorporated with biodegradable curcumin nanomicelles for full thickness wound healing. Int J Pharm 532(1):466–477
Alibolandi M, Hoseini F, Mohammadi M, Ramezani P, Einafshar E, Taghdisi SM et al (2018) Curcumin-entrapped MUC-1 aptamer targeted dendrimer-gold hybrid nanostructure as a theranostic system for colon adenocarcinoma. Int J Pharm 549(1–2):67–75
Lelli D, Sahebkar A, Johnston TP, Pedone C (2017) Curcumin use in pulmonary diseases: state of the art and future perspectives. Pharmacol Res:115133–115148
Xiao X, Yang M, Sun D, Sun S (2012) Curcumin protects against sepsis-induced acute lung injury in rats. J Surg Res 176(1):e31–e39
Guzel A, Kanter M, Guzel A, Yucel AF, Erboga M (2013) Protective effect of curcumin on acute lung injury induced by intestinal ischaemia/reperfusion. Toxicol Ind Health 29(7):633–642
Leth-Larsen R, Nordenbaek C, Tornoe I, Moeller V, Schlosser A, Koch C et al (2003) Surfactant protein D (SP-D) serum levels in patients with community-acquired pneumonia. Clin Immunol 108(1):29–37
Chai YS, Chen YQ, Lin SH, Xie K, Wang CJ, Yang YZ et al (2020) Curcumin regulates the differentiation of naïve CD4+T cells and activates IL-10 immune modulation against acute lung injury in mice. Biomed Pharmacother 125109946
Suresh MV, Wagner MC, Rosania GR, Stringer KA, Min KA, Risler L et al (2012) Pulmonary administration of a water-soluble curcumin complex reduces severity of acute lung injury. Am J Respir Cell Mol Biol 47(3):280–287
Lian Q, Li X, Shang Y, Yao S, Ma L, Jin SJ et al (2006) Protective effect of curcumin on endotoxin-induced acute lung injury in rats. 26(6):678–681
Cheng K, Yang A, Hu X, Zhu D, Liu K (2018) Curcumin attenuates pulmonary inflammation in lipopolysaccharide induced acute lung injury in neonatal rat model by activating peroxisome proliferator-activated receptor γ (PPARγ) pathway. Med Sci Monitor Int Med J Exp Clin Res 24:1178–1184
Avasarala S, Zhang F, Liu G, Wang R, London SD, London L (2013) Curcumin modulates the inflammatory response and inhibits subsequent fibrosis in a mouse model of viral-induced acute respiratory distress syndrome. PLoS One 8(2):e57285
Dei Cas M, Ghidoni R (2019) Dietary Curcumin: correlation between bioavailability and health potential. Nutrients 11(9)
Stanić Z (2017) Curcumin, a compound from natural sources, a true scientific challenge - a review. Plant Foods Hum Nutr 72(1):1–12
Stohs SJ, Chen O, Ray SD, Ji J, Bucci LR, Preuss HG (2020) Highly bioavailable forms of Curcumin and promising avenues for Curcumin-based research and application: a review. Molecules 25(6)
Gupta SC, Patchva S, Aggarwal BB (2013) Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J 15(1):195–218
Aggarwal BB, Harikumar KB (2009) Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int J Biochem Cell Biol 41(1):40–59
Saberi-Karimian M, Keshvari M, Ghayour-Mobarhan M, Salehizadeh L, Rahmani S, Behnam B, et al (2020) Effects of curcuminoids on inflammatory status in patients with non-alcoholic fatty liver disease: A randomized controlled trial (2020) Complement Ther Med 49:102322. https://doi.org/10.1016/j.phrs.2020.104921
Panahi Y, Khalili N, Sahebi E, Namazi S, Simental-Mendía LE, Majeed M, Sahebkar A. Effects of Curcuminoids Plus Piperine on Glycemic, Hepatic and Inflammatory Biomarkers in Patients with Type 2 Diabetes Mellitus: A Randomized Double-Blind Placebo-Controlled Trial. Drug Res (Stuttg). 2018 Jul;68(7):403-409. https://doi.org/10.1055/s-0044-101752
Soleimani V, Sahebkar A, Hosseinzadeh H (2018) Turmeric (Curcuma longa) and its major constituent (curcumin) as nontoxic and safe substances: review. Phytother Res 32(6):985–995
Kocaadam B, Şanlier N (2017) Curcumin, an active component of turmeric (Curcuma longa), and its effects on health. Crit Rev Food Sci Nutr 57(13):2889–2895
Lao CD, Ruffin MT, Normolle D, Heath DD, Murray SI, Bailey JM et al (2006) Dose escalation of a curcuminoid formulation. BMC Complement Altern Med 610
Sharma RA, Euden SA, Platton SL, Cooke DN, Shafayat A, Hewitt HR et al (2004) Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res 10(20):6847–6854
Carroll RE, Benya RV, Turgeon DK, Vareed S, Neuman M, Rodriguez L et al (2011) Phase IIa clinical trial of curcumin for the prevention of colorectal neoplasia. Cancer Prev Res (Phila) 4(3):354–364
Rasyid A, Lelo A (1999) The effect of curcumin and placebo on human gall-bladder function: an ultrasound study. Aliment Pharmacol Ther 13(2):245–249
Rasyid A, Rahman AR, Jaalam K, Lelo A (2002) Effect of different curcumin dosages on human gall bladder. Asia Pac J Clin Nutr 11(4):314–318
Keihanian F, Saeidinia A, Bagheri RK, Johnston TP, Sahebkar A (2018) Curcumin, hemostasis, thrombosis, and coagulation. J Cell Physiol 233(6):4497–4511
Tabeshpour J, Hashemzaei M, Sahebkar A (2018) The regulatory role of curcumin on platelet functions. J Cell Biochem 119(11):8713–8722
Pivari F, Mingione A, Brasacchio C, Soldati L (2019) Curcumin and type 2 diabetes mellitus: prevention and treatment. Nutrients 11(8)
Zhang DW, Fu M, Gao SH, Liu JL (2013) Curcumin and diabetes: a systematic review. Evid Based Complement Alternat Med:2013636053
Gardiner P, Phillips R, Shaughnessy AF (2008) Herbal and dietary supplement--drug interactions in patients with chronic illnesses. Am Fam Physician 77(1):73–78
Graham RE,Gandhi TK,Borus J,Seger AC,Burdick E,Bates DW et al. (2008) Advances in patient safety risk of concurrent use of prescription drugs with herbal and dietary supplements in ambulatory care. In: Henriksen K et al. (eds) Advances in patient safety: new directions and alternative approaches (Vol. 4: Technology and Medication Safety). Agency for Healthcare Research and Quality (US)
Bahramsoltani R, Rahimi R, Farzaei MH (2017) Pharmacokinetic interactions of curcuminoids with conventional drugs: a review. J Ethnopharmacol:2091–2012
Butterweck V, Derendorf H, Gaus W, Nahrstedt A, Schulz V, Unger M (2004) Pharmacokinetic herb-drug interactions: are preventive screenings necessary and appropriate? Planta Med 70(9):784–791
Chearwae W, Anuchapreeda S, Nandigama K, Ambudkar SV, Limtrakul P (2004) Biochemical mechanism of modulation of human P-glycoprotein (ABCB1) by curcumin I, II, and III purified from turmeric powder. Biochem Pharmacol 68(10):2043–2052
Rodríguez Castaño P, Parween S, Pandey AV (2019) Bioactivity of Curcumin on the cytochrome P450 enzymes of the Steroidogenic pathway. Int J Mol Sci 20(18)
Eastman RT, Roth JS, Brimacombe KR, Simeonov A, Shen M, Patnaik S et al (2020) Remdesivir: a review of its discovery and development leading to emergency use authorization for treatment of COVID-19. ACS Cent Sci 6(5):672–683
Humeniuk R, Mathias A, Cao H, Osinusi A, Shen G, Chng E et al (2020) Safety, tolerability, and pharmacokinetics of Remdesivir, an antiviral for treatment of COVID-19, in healthy subjects. Clin Transl Sci
Yang K (2020) What do we know about Remdesivir drug interactions? Clin Transl Sci
Mukhopadhyay S, Hoidal JR, Mukherjee TK (2006) Role of TNFα in pulmonary pathophysiology. Respir Res 7(1):125
Voiriot G, Razazi K, Amsellem V, Tran Van Nhieu J, Abid S, Adnot S et al (2017) Interleukin-6 displays lung anti-inflammatory properties and exerts protective hemodynamic effects in a double-hit murine acute lung injury. Respir Res 18(1):64–64
Calfee CS, Eisner MD, Parsons PE, Thompson BT, Conner ER Jr, Matthay MA et al (2009) Soluble intercellular adhesion molecule-1 and clinical outcomes in patients with acute lung injury. Intensive Care Med 35(2):248–257
Bhatia M, Zemans RL, Jeyaseelan S (2012) Role of chemokines in the pathogenesis of acute lung injury. Am J Respir Cell Mol Biol 46(5):566–572
Allen TC, Kurdowska A (2014) Interleukin 8 and acute lung injury. Arch Pathol Lab Med 138(2):266–269
Liu AC, Zhao LX, Xing J, Liu T, Du FY, Lou HX (2012) Pre-treatment with curcumin enhances plasma concentrations of losartan and its metabolite EXP3174 in rats. Biol Pharm Bull 35(2):145–150
Juan H, Terhaag B, Cong Z, Bi-Kui Z, Rong-Hua Z, Feng W et al (2007) Unexpected effect of concomitantly administered curcumin on the pharmacokinetics of talinolol in healthy Chinese volunteers. Eur J Clin Pharmacol 63(7):663–668
Zhang W, Tan TMC, Lim L-Y (2007) Impact of Curcumin-induced changes in P-glycoprotein and CYP3A expression on the pharmacokinetics of Peroral Celiprolol and midazolam in rats. Drug Metab Dispos 35(1):110–115
Zhou X, Zhang F, Chen C, Guo Z, Liu J, Yu J et al (2017) Impact of curcumin on the pharmacokinetics of rosuvastatin in rats and dogs based on the conjugated metabolites. Xenobiotica 47(3):267–275
Liu AC, Zhao LX, Lou HX (2013) Curcumin alters the pharmacokinetics of warfarin and clopidogrel in Wistar rats but has no effect on anticoagulation or antiplatelet aggregation. Planta Med 79(11):971–977
Hu S, Belcaro G, Dugall M, Peterzan P, Hosoi M, Ledda A et al (2018) Interaction study between antiplatelet agents, anticoagulants, thyroid replacement therapy and a bioavailable formulation of curcumin (Meriva®). Eur Rev Med Pharmacol Sci 22(15):5042–5046
Taubert D, von Beckerath N, Grimberg G, Lazar A, Jung N, Goeser T et al (2006) Impact of P-glycoprotein on clopidogrel absorption. Clin Pharmacol Therapeutics 80(5):486–501
Pavithra BH, Prakash N, Jayakumar K (2009) Modification of pharmacokinetics of norfloxacin following oral administration of curcumin in rabbits. J Vet Sci 10(4):293–297
Cheng L et al (2011) Effects of Curcumin on the pharmacokinetics of Loratadine in rats: possible role of CYP3A4 and P-glycoprotein inhibition by Curcumin. Biomol Ther 19(3):364–370
Ganta S, Devalapally H, Amiji M (2010) Curcumin enhances Oral bioavailability and anti-tumor therapeutic efficacy of paclitaxel upon administration in Nanoemulsion formulation. J Pharm Sci 99(11):4630–4641
Yan Y-D, Kim DH, Sung JH, Yong CS, Choi HG (2010) Enhanced oral bioavailability of docetaxel in rats by four consecutive days of pre-treatment with curcumin. Int J Pharm 399(1):116–120
Sun X, Li J, Guo C, Xing H, Xu J, Wen Y et al (2016) Pharmacokinetic effects of curcumin on docetaxel mediated by OATP1B1, OATP1B3 and CYP450s. Drug Metab Pharmacokinet 31(4):269–275
Lee C-K, Ki S-H, Choi J-S (2011) Effects of oral curcumin on the pharmacokinetics of intravenous and oral etoposide in rats: possible role of intestinal CYP3A and P-gp inhibition by curcumin. Biopharm Drug Disposit 32(4):245–251
Cho YA, Lee W, Choi JS (2012) Effects of curcumin on the pharmacokinetics of tamoxifen and its active metabolite, 4-hydroxytamoxifen, in rats: possible role of CYP3A4 and P-glycoprotein inhibition by curcumin. Pharmazie 67(2):124–130
Hsieh Y-W, Huang C-Y, Yang S-Y, Peng Y-H, Yu C-P, Chao P-DL et al (2014) Oral intake of curcumin markedly activated CYP 3A4: in vivo and ex-vivo studies. Sci Rep 4(1):6587
Cheng K-W, Wong CC, Mattheolabakis G, Xie G, Huang L, Rigas B (2013) Curcumin enhances the lung cancer chemopreventive efficacy of phospho-sulindac by improving its pharmacokinetics. Int J Oncol 43(3):895–902
Competing Interests
none.
Funding
none.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Heidari, Z., Mohammadi, M., Sahebkar, A. (2021). Possible Mechanisms and Special Clinical Considerations of Curcumin Supplementation in Patients with COVID-19. In: Barreto, G.E., Sahebkar, A. (eds) Pharmacological Properties of Plant-Derived Natural Products and Implications for Human Health. Advances in Experimental Medicine and Biology, vol 1308. Springer, Cham. https://doi.org/10.1007/978-3-030-64872-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-64872-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-64871-8
Online ISBN: 978-3-030-64872-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)