Abstract
As normal constituents of blood serum, the Serum Amyloid A (SAA) proteins are small (104 amino acids in humans) and remarkably well-conserved in mammalian evolution. They are synthesized prominently, but not exclusively, in the liver. Fragments of SAA can associate into insoluble fibrils (called “amyloid”) characteristic of “secondary” amyloid disease in which they can interrupt normal physiology and lead to organ failure. SAA proteins comprise a family of molecules, two members of which (SAA1 and SAA2) are (along with C-reactive protein, CRP) the most prominent members of the acute phase response (APR) during which their serum levels rise dramatically after trauma, infection and other stimuli. Biologic function (s) of SAA are unresolved but features are consistent with a prominent role in primordial host defense (including the APR ). SAA proteins are lipophilic and contribute to high density lipoproteins (HDL) and cholesterol transport. SAA proteins interact with specific receptors and have been implicated in tissue remodeling through metalloproteinases, local tissue changes in atherosclerosis, cancer metastasis, lung inflammation, maternal–fetal health and intestinal physiology. Molecular details of some of these are emerging.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Serum amyloid A
- SAA
- Acute phase reaction
- Lipoproteins
- Inflammation
- Cytokine
- Atherosclerosis
- Metastasis
- Arthritis
- Amyloidosis
- APR
- HDL
Introduction
Serum amyloid A (SAA) proteins constitute a family of very closely-related, highly conserved serum molecules whose pathophysiology has been studied for nearly 70 years. As their name implies, molecules in this category originally were identified as constituents of so-called “amyloid” deposits in both clinical and laboratory studies. “Amyloid” (from Greek, meaning “starch-like”) is a well-recognized pathologic finding in which regions appearing amorphous by light microscopy stain characteristically with dyes like Congo Red or Thioflavin T (see Fig. 17.1). When viewed by electron microscopy, however, amyloid deposits are seen to be composed of fibrils (see Fig. 17.2) (Cohen and Calkins 1959). SAA proteins are related to so-called “reactive” or “secondary” amyloid—where deposits develop in response to chronic or recurrent infections and/or inflammation. Such amyloid deposits often were found in histopathologic studies in the preantibiotic era when chronic infections were particularly common. In “secondary” amyloid, the unique fibrillary proteins (usually ≈76 aa long) were called “Amyloid A” or AA (historically designating the first amyloid protein identified). AA proteins were later shown to be derived from partial proteolysis of a larger (104 aa) serum protein—hence the name of this latter species was proposed as “Serum Amyloid A” (SAA). (Thus meaning “the serum protein precursor of the first [hence, “A”] well-characterized protein [“AA”] found in amyloid deposits.) Subsequent analysis has identified other types of “amyloid” and with protein constituents related to their pathophysiologic context(s) (Sack 2009, 2019).
Photomicrographs of serial sections of human tissue showing amyloid deposits in blood vessel walls. a Hematoxylin and eosin staining viewed with regular illumination. Note loss of normally visible details. b Congo red staining viewed with regular illumination. Note that the amyloid deposits appear pink but without details. c Congo red staining viewed with polarized light showing characteristic birefringence of the amyloid deposits (collection of author)
Electron microscopic image of amyloid fibrils (Alzheimer amyloid-β(1–42)) (Lührs et al. 2005)
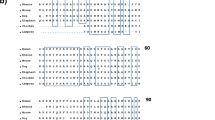
The unique sequence(s) of SAA proteins were identified relatively early. These have served as basic identifying data in many studies. Particularly notable is the remarkable aa sequence conservation throughout evolution in mammals as well as other vertebrates (for examples, see Fig. 17.3). Although human SAA proteins have 104 aa small length variations are found in other species (Fig. 17.3). Amino acid polymorphisms have been identified in large human population studies and a classification has been proposed (see Fig. 17.4 for a consensus) (Sipe 1999; Sun and Ye 2016; Benson 2019). However, most of these variants represent conservative aa changes.
a Consensus sequence for human SAA1. Variants recognized in Fig. 17.4. b Comparison of SAA sequences in multiple organisms. Preserved amino acids are enclosed. Note length variation(s) (USCS Genome Browser [GRCh38/hg38] Assembly)
Monomer and Fibril Structure
The 3-dimensional structure of the SAA monomer is notable for having 4 α-helices and a relatively unstructured C-terminal domain (Fig. 17.5) (Lu et al. 2014). As predicted from earlier circular dichroism (CD) studies (Meeker and Sack 1998), no β-sheet regions have been identified in the monomer. Because, as noted above, fibrils in tissue amyloid deposits generally do not contain isolated monomers, particular interest has been directed to determining structural features of the fibrils themselves. To date, many details of AA fibril structure remain unknown. However, studies of AA-derived as well as other types of amyloid fibrils have shown at least some common features. The most prominent fibril features are arrays of β-pleated sheets (usually antiparallel but in some cases parallel) stacked above and below one another and stabilized by extensive hydrogen bonding and van der Waals interactions. The general dimensions of amyloid fibrils include a 20 nm diameter with 10 Å between the stacked sheets. As predicted by earlier sequencing, SAA fibrils do not contain the entire 104 aa parent protein. Most fibrils comprise ≈76 N-terminal aa residues although there are reports of both shorter and longer forms. Reference to the monomer model (Fig. 17.5) shows an unstructured region at aa 69–73 that may make nearby regions more susceptible to proteolysis. Given the absence of β-sheet domains in the parent monomer structure (Meeker and Sack 1998; Lu et al. 2014), substantial reorganization of the primary chain must occur prior to fibril assembly.
Three-dimensional structure of monomeric SAA1.1. Note 4 α-helices (1—aa 1–27; 2—aa 32–47; 3—aa 50–69; 4—aa 73–88). C-terminal tail—aa 89–104. (Lu et al. 2014)
Cytologic data indicate that at least initial AA amyloid fibril formation occurs intracellularly, in lysosomal compartments where low pH likely contributes to structural changes (Claus et al. 2017; Sack 2018). Once formed, small fibril “nuclei” likely interact with other N-terminal monomer fragments as “seeds” to extend the longitudinal dimensions of the fibrils into largely insoluble and relatively chemically insert macromolecular arrays. These become the fibrils seen by electron microscopy and are the site(s) of specific planar dye interaction(s) that are responsible for birefringence.
A characteristic feature of AA and other types of amyloid fibrils is very slow spontaneous dissociation and this, among other features, contributes to their cytopathology by interrupting cell–cell communication, nutrient and ion transport and visible organ microstructure. Fibril stability (and the macroscopic fibril deposits) reflects at least several factors. First, formation of individual fibrils involves considerable negative free energy (–ΔG). Second, individual fibril microarchitecture with tightly packed polypeptide chains makes the structure(s) relatively inaccessible to proteases. Third, the fibrils themselves are generally packed together tightly. These features help explain the association of amyloid fibrils (generally of all types) with chronic, often progressive, organ dysfunction and disease and slow (if any) spontaneous resolution.
Molecular Biology
SAA-related proteins and genes constitute a closely-related family. In all organisms studied to date, genes for all members of the SAA “family” are clustered on a single chromosome. Human SAA genes are on chromosome 11p; those of the mouse are on murine chromosome 7. Figure 17.6 shows the human SAA gene family. A low level of aa polymorphism is recognized among family members (corresponding to the variations noted in Fig. 17.4), much of which has been cataloged. In mice there are 4 functional SAA genes and one pseudogene. These correspond to SAA1 and 2 (virtually identical APR proteins) and SAA3. The latter differs from SAA1 and 2 by aa changes in the N-terminal region. Human SAA1 and 2 genes similarly encode nearly identical proteins. The human SAA3 gene closely resembles its murine counterpart. However, although capable of being transcribed, the human SAA3 gene contains a single nucleotide insertion leading to an altered reading frame with early termination of transcription and likely loss of the corresponding mRNA through nonsense-mediated decay (Sack et al. 2018). No protein corresponding to SAA3 has been found in human serum. In mice, most anti SAA antibodies detect all species (SAA1, 2, and 3) but similar use of antibodies in humans reveals only SAA1 and 2. The SAA4 gene is constitutively transcribed in humans and mice and contains an insertion of 8 aa leading to a serum protein of 112 aa (De Buck et al. 2016b). Glycosylation may occur within the octapeptide and both glycosylated and unglycosylated forms have been detected in humans.
The remarkable evolutionary conservation of SAA protein sequences also is reflected in structural features of their corresponding genes (Fig. 17.6). SAA genes have been characterized in many organisms and all, to date, share a structure of 4 exons (Fig. 17.7). The aa of the mature protein(s) are encoded in exons 2–4. Consistent with SAA’s status as a secreted or “serum” protein, the primary translated aa sequence also encodes an 18 aa N-terminal leader. The leader also is well-conserved and is removed from the primary translation product prior to secretion of the 104 aa species (or 112 aa species for SAA4). Consistent with features of some other proteins and their genes, exon/intron junctions correspond reasonably well to turns or unstructured loops in the mature, folded monomer. At least some SAA in the serum associates into hexamers, but these likely are in equilibrium with monomers, particularly in lipid environments (e.g. HDL).
Acute Phase Response
An important feature of SAA proteins, recognized early in their study, is their prominence among the serum constituents of the “acute phase response” (APR). This stereotyped process is well-characterized as a response to experimental as well as clinical conditions—endotoxin, trauma, infections, etc. (Kushner 1982). Among the serum protein changes during the APR are rapid elevations in the levels of SAA and C-reactive protein (CRP, q.v.); these can rise 1000-fold in 24–36 h following the initiating stimulus. These impressive changes as recognized in humans and experimental animals reflect new synthesis and secretion of both SAA and CRP largely, although not exclusively, by the liver. In the absence of persistent stimulus (i) the entire APR resolves, usually beginning 48–72 h after induction. Interestingly, prolonged inflammation or other stimuli can cause long-term elevation of SAA and CRP levels. Chronically, or repeatedly, elevated SAA levels set the stage for their cleavage and deposition as pathologic amyloid fibrils as noted above. This helps explain “secondary” (i.e. “AA”) amyloid deposition in individuals with chronic or recurrent inflammation.
Note that the C-reactive protein (CRP) (see Chap. 20) also is a well-conserved serum protein and specifically binds to the C-polypeptide of S. pneumoniae (hence its name). CRP has historically been considered to be a contributor to primordial host defense, generally in the context of the APR.
SAA gene transcription responds to various APR “inducers.” Some of these are well-characterized at the molecular level (including IL-1β, IL-6, TNFα and participants in MAPK activation including pERK1/2, pJNK, p38) while other less well-defined agents include sepsis, intraperitoneal casein, and lipopolysaccharides (LPS, bacterial endotoxin). At the onset of the APR levels of SAA mRNA can rise dramatically (in mouse liver SAA mRNA can comprise 5% of mRNA 24 h after APR induction) (Morrow et al. 1981). In most systems studied, elevated SAA and CRP serum levels resolve completely. Viewed phenomenologically this is a circuit with stereotyped “feedback” attenuation. The multiple pathways to APR induction involve different factors that interact with different cells in different organs in different ways, making generalizations difficult. An important, currently unresolved, question relates to details of how the APR process is resolved once the initiating stimulus is withdrawn.
An established protocol in mice—CLP (cecal ligation and puncture)—provides an APR model by producing acute polymicrobial sepsis (in which LPS is prominent). About 75% of normal mice survive at day 5 after CLP. By contrast, mice unable to synthesize characteristic APR SAA due to homozygosity for liver-specific deletion of gp130 (gp130Δhepa) showed ≈90% lethality using the same protocol. Treating these mice with exogenous SAA restored normal survival levels. In addition, using this model in normal mice treated with a monoclonal antibody against aa 33–43 region of SAA (helix 2 in model, see Fig. 17.5) also led to ≈90% lethality. These studies are all consistent with a critical “survival” function for SAA (and, possibly specifically the helix 2 region containing the epitope(s) recognized by the monoclonal antibody) (Linke et al. 2017).
Another CLP-APR study in mice transgenic for constitutive SAA production evaluated protection against lung injury (Cheng et al. 2018). Using intratracheal TNFα to induce the APR in the lung of the transgenic mice led to tissue damage and a prominent cytokine response that was unaffected by the constitutive presence of SAA. This is consistent with a protective effect of SAA against LPS that did not generalize to TNFα as a stimulus. Further study showed direct molecular interaction between SAA and LPS leading to macrophage uptake (via the SR-B1 receptor—see below) of the product and attenuation of serologic APR changes (reduced IL-6 and TNFα, and increased IL-10). The protective effect of SAA (and the cytokine responses) was largely blocked by treating the mice with an aa 32–47 polypeptide (also overlapping the helix 2 domain of SAA), consistent with competitive displacement of full length SAA from LPS and thus reducing macrophage uptake of LPS that would have attenuated the APR.
As further evidence for changes in other study systems, treating HeLa cells transgenic for receptor TLR-2 with SAA induced pERK1/2 and pJNK—a response different from treating with an aa 11–58 SAA polypeptide (overlapping helices 1 and 2) which increased pERK1/2 and p38 but not pJNK, indicating that presumably other domains of SAA could affect the response (Zhou et al. 2017). Attempts to assign specific function(s) to specific parts of the SAA monomer (recall Fig. 17.5) have been complicated by not knowing whether these exist as specific domains and/or can function independently in the parent protein. None has been identified as an independent species in vivo.
Thus, SAA1 (and, particularly aa 32–44/47 domain of helix 2) appears to specifically interact with LPS to attenuate lethality. Since SAA production is stimulated in macrophages (as well as liver) during the APR this adds a potential source for direct interaction with, at least, LPS species in a polymicrobial situation. SAA’s response to the initiating APR stimulus could thus help to eliminate LPS as a stimulus and reduce the magnitude of the APR.
SAA “Receptors”
SAA interacts with specific cells and, possibly, macromolecules such as LPS. Recalling that CRP was defined (and named) by bacterial binding, it is notable that SAA binds to the outer membrane protein A (ompA) of E. coli., acting as an opsonin and enhancing bacterial uptake by polymorphonuclear leukocytes. E. coli not producing ompA were unaffected (Hari-Dass et al. 2005; Shah et al. 2006). E. coli growth in culture can be reduced by SAA.
The notion of cellular “receptors” for SAA has proved complicated and, not surprisingly, studies of this problem have led to complicated answers. Association of SAA with various “receptors” has been studied using different systems. The array of reported interactions (see Table 17.1) implies that at least some of them likely are primary; others may be incidental. Nevertheless, considering them together illustrates possibilities for multiple physiologic roles for SAA. A particularly well-characterized example is the “scavenger receptor” SR-B1. As discussed above, this is likely involved with SAA/LPS uptake by macrophages. SR-B1 also is involved with cholesterol transport (see below). Toll-like receptors likely help mediate inflammatory processes. Others likely are involved both with advancing and, finally, resolving, inflammation.
SAA Physiology
Many anecdotal reports have implicated SAA in (patho)physiology. Not all observations have been studied in rigorous detail but several important processes clearly involve SAA. Molecular details of SAA participation in some of these have been defined. Important overlaps between the categories indicate that a more inclusive view of SAA biology is needed. Prominent aspects of SAA biology will be considered below. Several features are notable: (1) no enzymatic activity has been identified for SAA (the protein is likely too small). (2) participation in APR and inflammation is compatible with a primordial signaling/communication/defense function (this would be consistent with its impressive evolutionary preservation as well as its clinical/laboratory association with chronic disorders). (3) lipophilicity of the SAA monomer (consistent with its exposed aa residues—see Fig. 17.5) makes it likely to be partitioned into lipid environments and also to associate with host and bacterial lipoproteins. (4) participation in aspect(s) of inflammation is likely (based both on the APR as well as clinical /laboratory association with chronic infections). (5) formation of the AA amyloid fibril itself likely represents a biologic “dead end” (since such deposits are long-lived and at least relatively inert).
It is likely important to distinguish acute, short-term activities of SAA from those associated with chronic, high-level, or localized longer-term effect(s). Interpreting different reports involves consideration of the source of SAA studied. Early concern about recombinant SAA produced in E. coli was that the material might contain endotoxin and that this could explain some results. This problem was recognized and, although contaminating endotoxin could largely be removed, Burgess et al. (2018) recently examined such preparations and found multiple bacterial proteins, at least some of which were lipoproteins. They emphasized that recombinant SAA proteins should be derived from eukaryotic cells to avoid this important contamination (this was not the case with many previous reports). De Buck (2016a) summarized data showing that SAA derived from blood serum or plasma lacks much of the proinflammatory effect of recombinants derived from bacteria. After nearly 70 years of study no single role can be assigned to SAA; participation in multiple pathways is likely. Unless otherwise noted below, most studies have been done using the nearly-identical SAA1/2 proteins.
Lipophilicity and Lipid Interactions
As already noted, SAA1/2 proteins are remarkably lipophilic and this has led to their characterization as apolipoproteins of high density lipoprotein (HDL). In serum, most SAA is associated with HDL and the concentration of free SAA monomer is quite low. Measuring SAA concentration in serum generally involves dissociating it from HDL particles. In addition to its being partitioned into the HDL fraction in the serum, SAA has been related to cholesterol transport and recycling. Many study systems have been used and despite some controversy [likely reflecting, at least in part, bacterial protein contamination of recombinant SAA used (see above)] several consistent features are recognized. As summarized elsewhere (Sack 2018): (1) SAA promotes an increase in cholesterol ester hydrolase (hence increased intracellular free cholesterol). (2) Macrophage acyl-CoA:cholesterol acyl transferase (ACAT) activity is reduced by SAA. (3) HDL containing SAA is targeted to the macrophage within which it can be loaded with free cholesterol for transport (usually back to the liver). (4) Multiple receptors including SR-B1 are involved in recognition and uptake of SAA. (5) Different SAA isoforms may affect this process (but all are not fully characterized).
Kisilevsky and coworkers proposed that SAA is central to mobilizing cholesterol from macrophages and other constituents of sites of tissue injury, trauma, breakdown, etc. (Kisilevsky and Manley 2012). Such injury or tissue damage could, for example, accompany APR induction during which SAA levels would be high as described above. According to this hypothesis, the APR and its role in cholesterol recycling through salvage and transport could be an evolutionarily favored process, helping explain SAA biology and conservation as important for survival.
By contrast to acute lipid mobilization changes due to injury, chronic inflammation also changes local tissue architecture and cellular as well as extracellular contents. Especially when prolonged, this changes endothelial transport leading to extravascular accumulation of monocytes and macrophages and an altered local tissue proteoglycan milieu. SAA is known to induce metalloproteinases (see below) and can extend local tissue damage and release more lipid. Macrophages can take up the released LDL and then persist as “foam cells.” The entire process can become self-perpetuating with chronic reorganization of the site—as large-scale juxtavascular change(s) accumulate this can become recognized as atherosclerosis (King et al. 2011). Evidence connecting all parts of this process has been gathered from multiple systems. In addition to the proposed (and detected) involvement of SAA, many more studies have been devoted to CRP, possibly because it has been simpler to measure and large data collections are available. As an inflammatory marker, CRP has been used as a “proxy” or biomarker for the inflammation that is central to atherosclerosis. The CANTOS trial in humans provided convincing evidence that reducing chronic inflammation —and CRP levels (e.g. reducing IL-1β with the monoclonal antibody Canakinumab)—was associated with reduced vascular complications (Ridker et al. 2017). Presumably, SAA participation is similarly affected (although not yet studied in detail).
Tissue Remodeling
SAA’s relation to extracellular metalloproteinase release and function was shown many years ago. Treating rabbit synovial fibroblasts with phorbolmyristate not only released collagenase but also small molecules including β2-microglobulin and an “SAA-like” protein (later designated SAA3 and featuring a unique TFLK sequence near the N-terminus). Significantly, adding this SAA3 to otherwise untreated, quiescent cells also stimulated collagenase release—consistent with a paracrine circuit capable of prolonging tissue destruction and remodeling (Brinckerhoff et al. 1989). SAA transcripts also were found by in situ hybridization in synovial tissue from caprine retroviral arthritis (Sack and Zink 1992). More recent studies also detected SAA expression in arthritic synovium and related it to metalloproteinase induction (Connolly et al. 2010, 2012).
Cancer
Serum SAA levels have been studied as potential biomarkers for cancer and clinical associations have been described for many tumor types (Table 17.2). This has not uniformly led to utility as a biomarker, however, but chronic inflammation and cytokine participation has been recognized (Landskron et al. 2014). Of more mechanistic interest has been dissecting direct relationships. SAA production within the tumor tissue has been found in colorectal, ovarian, uterine and glioblastoma cancers (Moshkovskii 2012).
SAA also has been implicated in tumor growth. Melanoma cells with SAA expression correlated with finding immunosuppressive neutrophils within the tumor. SAA in humans and mice has been considered an effector for metastasis promotion by S100A4. In mice, cells surrounding pancreatic ductal adenocarcinoma were found to secrete IL-6. This cytokine led to SAA synthesis by the liver (via STAT3). After the IL-6/SAA stimulation, metastatic “niches” were formed within the liver that were followed by tumor metastases. This process did not occur in SAA knock-out mice (although metastasis to lung and other areas was unaffected) (Lee et al. 2019). Consistent with the observations relating SAA to metalloproteinases and paracrine effects (see above) this is consistent with a central role for SAA in local tissue remodeling that could affect metastasis (i.e. “niche”) formation.
Intestinal Immunology
Adhesion of segmented filamentous bacteria (sfb) to intestinal epithelial cells leads to specific, IL-17 secreting Th17 cell accumulation in the lamina propria. Within these cells SAA transcripts are the most upregulated species. Actin reorganization within the cells led to C/EBPδ expression which is proposed to interact with two DNase hypersensitive sites 3′ to the SAA1 gene (Ivanov et al. 2009). Further study of this system showed that ILC3 cells in the ileum secreted IL-22 after sfb adhesion and that this then led to SAA production via a STAT-independent mechanism (Atarashi et al. 2015). In another murine system, colonic bacteria (and possibly other bacterial products) led to SAA1/2 expression to modulate Th17 cell differentiation and cytokine production (Sano et al. 2015).
Lung Disease and Sarcoidosis
Exacerbations of symptoms in individuals with chronic obstructive pulmonary disease (COPD) showed better correlation with blood SAA levels than with those of CRP. SAA levels in bronchoalveolar lavage fluid correlated well with IL-8 and neutrophil elastase levels; both related to the pathophysiologic changes (Bozinovski et al. 2008, 2012). Detailed study of noncaseating granulomata, macrophages and multinucleated giant cells from sarcoidosis patients showed prominent SAA. Noting that TLR2 and RAGE receptor polymorphisms are related to disease progression in sarcoidosis, it has been proposed that SAA is a central participant in the characteristic “granulomatous inflammation” seen in these patients (Chen et al. 2010).
Maternal/Fetal Health
Pregnancy and Delivery
Measuring SAA levels during pregnancy has led to important associations. In mice, SAA levels rose with preterm delivery (Yang et al. 2009). In humans, SAA levels correlate with the severity of neonatal encephalopathy and mortality (Aly et al. 2011). Ibrahim et al. (2017) found that SAA levels provided an independent indicator of early pregnancy loss. Elevated cord blood levels of SAA , CRP and haptoglobin (all members of the APR) were associated with early onset neonatal sepsis in preterm infants (Mithal et al. 2017).
Mammary-Derived SAA
Bovine colostrum (early milk) contains an SAA protein with a characteristic TFLK sequence near its N-terminus (in mouse this would be classified as SAA3) (McDonald et al. 2001). Exposing intestinal epithelial cells to this protein led to prominent MUC3 mucin production as well as a corresponding decrease in adherence of enteropathogenic E. coli (Mack et al. 2003). Both LPS and prolactin can stimulate transcription of this “SAA3” protein in vitro using human breast epithelial cell cultures (Larson et al. 2005). This process is consistent with a pro-survival transmission of this “SAA3” molecule to the newborn by nursing and, particularly, by early exposure to colostrum, hence reducing the risk of infection for the neonate. In humans, as noted above, the SAA3 protein is not translated, likely due to nonsense-mediated mRNA decay; instead SAA1 is present in colostrum (Sack et al. 2018). Its protective effect(s) have not yet been confirmed.
Perspective
Despite many years of study, all biologic interactions and functions of SAA proteins remain unresolved. Initially discovered due to prominent participation in the acute phase response as well as its contribution to pathologic fibril formation in chronic inflammation , SAA has been implicated in many processes. The hypothesis that SAA proteins have an evolutionarily preserved role in survival appears correct; their widespread distribution across species as well as striking amino acid sequence conservation are consistent with this. The APR itself is recognized as a “primordial” defensive response, serving as a generic front-line for maintaining organismal integrity. With a perspective based on evolution, it is likely that SAA and the APR have served their survival functions well. Over the course of longer organismal lifespans, however, the pathophysiologic roles have had broader implications. As shown, a wide array of “receptors” (some established, others implicated) can serve multiple pathways. In at least some instances, high blood levels of SAA can simply be “biomarkers” that reflect underlying inflammation (infection, trauma, cancer, etc). (CRP can be viewed similarly.) Gathering reports, however, implicate SAA participation in multiple basic processes and disorders. For example, paracrine stimulation of metalloproteinase(s) can be central to arthritic joint destruction as well as remodeling niches for tumor metastasis. Stimulating mucin secretion in the neonatal gut may have been essential for survival, particularly in human evolution and animal communities. Lipid transfer between site(s) for recycling, storage or modification (e.g. atherosclerosis) is consistent with basic chemical features of the SAA monomer as well as its many serum interactions. As noted, there is some irony in having the name of this family of molecules derived from what likely is a “terminal” state of their biology—the AA fibril appears chemically inert, but biologically quite stable.
References
Aly H, Hamed Z, Mohsen L et al (2011) Serum amyloid A protein and hypoxic ischemic encephalopathy in the newborn. J Perinatol 31:263–268. https://doi.org/10.1038/jp.2010.130
Atarashi K, Tanoue T, Ando M et al (2015) Th17 cell induction by adhesion of microbes to intestinal epithelial cells. Cell 163:367–380
Benson MD, Buxbaum JN, Eisenberg DS et al (2019) Amyloid nomenclature 2018: recommendations by the International Society of Amyloidosis (ISA) nomenclature committee. Amyloid 5pp. https://doi.org/10.1080/13506129.2018.1549825
Bozinovski S, Hutchinson A, Thompson M et al (2008) Serum amyloid A is a biomarker of acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 177:269–278
Bozinovski S, Uddin M, Thompson M et al (2012) Serum amyloid A opposes lipoxin A4 to mediate glucocorticoid refractory lung inflammation in chronic obstructive pulmonary disease. Proc Natl Acad Sci 109:935–940
Brinckerhoff CE, Mitchell TI, Karmilowicz MJ et al (1989) Autocrine induction of collagenase by serum amyloid A-like and B2-microglobulin-like proteins. Science 243:655–657
Burgess EJ, Hoyt LR, Randall MJ et al (2018) Bacterial lipoproteins constitute the TLR-stimulating activity of serum amyloid A. J Immunol 201:2377–2384
Chen ES, Song Z, Willett MH et al (2010) Serum Amyloid A regulates granulomatous inflammation in sarcoidosis through toll-like receptor-2. Am J Respir Crit Care Med 181:360–373
Cheng N, Liang Y, Du X et al (2018) Serum amyloid A promotes LPS clearance and suppresses LPS-induced inflammation and tissue injury. EMBO Rep (e45517):14pp. https://doi.org/10.15252/embr.201745517
Claus S, Meinhardt K, Aumuller T et al (2017) Cellular mechanism of fibrila formation from serum amyloid A1 protein. EMBO Rep 18(8):1352–1366
Cohen AS, Calkins E (1959) Electron microscopic observations on a fibrous component in amyloid of diverse origins. Nature 183:1202–1203
Connolly M, Marelli A, Blades M et al (2010) Acute serum amyloid A induces migration, angiogenesis, and inflammation in synovial cells in vitro and in a human rheumatoid arthritis/SCID mouse chimera model. J Immunol 184:6427–6437
Connolly M, Mullan RH, McCormick J et al (2012) Acute=phase serum amyloid A regulates tumor necrosis factor alpha and matric turnover and preficts disease progression in pastients with inflammatory arthritis before and after biologic therapy. Arthritis Rheum 64(4):1035–1045
De Buck M, Gouwy M, Wang JM et al (2016a) The cytokine-serum amyloid A-Chemokine network. Cytokine Growth Factor Rev 30:55–69
De Buck M, Gouwy M, Wang JM et al (2016b) Structure and expression of different serum amyloid A (SAA) variants and their concentration-dependent functions during host insults. Curr Med Chem 23:1725–1755
Hari-Dass R, Shah C, Meyer DJ et al (2005) Serum amyloid A proteins binds to outer membrane protein A of gram-negative bacteria. J Biol Chem 280(19):18562–18567
Ibrahim M, Ramy AR, Abdelhamid A et al (2017) Maternal serum amyloid A level as a novel marker of primary unexplained recurrent early pregnancy loss. Int J Gynecol Obstet 136:298–303
Ivanov II, Atarashi K, Manel N et al (2009) Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell 139:485–498
King VL, Thompson J, Tannock LR (2011) Serum amyloid A in atherosclerosis. Curr Opin Lipidol 22:302–307
Kisilevsky R, Manley PN (2012) Acute-phase serum amyloid A: perspectives on its physiological and pathological roles. Amyloid 19(1):5–14
Knebel FH, Uno M, Galatro TF, Bellé LP, Oba-Shinjo SM, Marie SKN, Campa A (2017) Serum amyloid A1 is upregulated in human glioblastoma. J Neuro-Oncol 132(3):383–391
Kushner I (1982) The phenomenon of the acute phase response. Ann N Y Acad Sci 39–48
Landskron G, De La Fuente M, Thuwajit P et al (2014) Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res 2014:149185. https://doi.org/10.1155/2014/149185
Larson MA, Weber A, Weber AT et al (2005) Differential expression and secretion of bovine serum amyloid A3 (SAA3) by mammary epithelial cells stimulated with prolactin or lipopolysaccharide. Vet Immunol Immunopathol 107:255–264
Lee JW, Stone ML, Porrett PM et al (2019) Hepatocytes direct the formation of a pro-metastatic niche in the liver. Nature 567:249–252
Linke RP, Meinel A, Chalcroft JP et al (2017) Serum amyloid A (SAA) treatment enhances the recovery of aggravated polymicrobial sepsis in mice, whereas blocking SAA's invariant peptide results in early death. Amyloid 24(S1):149–150
Lu J, Yu Y, Zhu I et al (2014) Structural mechanism of serum amyloid A-mediated inflammatory amyloidosis. Proc Natl Acad Sci 111(14):5189–5194
Luhrs T, Ritter C, Adrian M et al (2005) 3D structure of Alzheimer's amyloid-β(1–42) fibrils. Proc Natl Acad Sci USA 102(48):17341–17347
Mack DR, McDonald TL, Larson MA et al (2003) The conserved TFLK motif of mammary-associated Serum Amyloid A3 is responsible for Up-regulation of intestinal MUC3 mucin expression in vitro. Pediatr Res 53(1):137–142
McDonald TL, Larson MA, Mack DR et al (2001) Elevated extrahepatic expression and secretion of mammary-associated serum amyloid A3 (M-SAA3) into colostrum. Vet Immunol Immunopathol 83:203–211
Meeker AK, Sack GH Jr (1998) A fusion protein between serum amyloid A and staphylococcal nuclease—synthesis, purification, and structural studies. Proteins Struct Funct Genet 30:381–387
Mithal LB, Palac HL, Yogev R et al (2017) Cord blood acute phase reactants predict early onset neonatal sepsis in preterm infants. PLoS ONE 12(1):E0168677. https://doi.org/10.1371/journal.pone.0168677
Morrow JF, Stearman RS, Peltzman CG et al (1981) Induction of hepatic synthesis of serum amyloid A protein and actin. Proc Natl Acad Sci USA 78:4718–4722
Moshkovskii SA (2012) Why do cancer cells produce serum amyloid A acute-phase protein? Biochemistry (Moscow) 77(4):339–341
Ridker PM, Everett BM, Thuren T et al (2017) Antiinflammatory therapy with Canakinumab for atherosclerotic disease. N Engl J Med 377(12):1119–1131
Sack GH Jr (2009) Amyloidosis (Chap. 46). In: Stone JH (ed) A clinician's pearls and myths in rheumatology. Springer, Dordrecht, pp 461–466
Sack GH Jr (2018) Serum amyloid A - a review. Mol Med 24:46. https://doi.org/10.1186/s10020-10018-10047-10020
Sack GH Jr (2019) The pathophysiology of amyloid fibril formation. In: Amyloidosis. IntechOpen, London. https://doi.org/10.5772/intechopen.81965
Sack GH Jr, Zink MC (1992) Serum amyloid A (SAA) gene expression in synovial cells in retroviral arthritis. Am J Pathol 141:525–529
Sack GH Jr, Zachara N, Rosenblum N et al (2018) Serum amyloid A1 (SAA1) protein in human colostrum. FEBS OpenBio 8:435–441. https://doi.org/10.1002/2211-5463.12383
Sano T, Huang W, Hall JA et al (2015) An IL-23/IL-22 circuit regulates epithelial serum amyloid A to promote local effector Th17 responses. Cell 163:381–393
Shah C, Hari-Dass R, Raynes JG (2006) Serum amyloid A is an innate immune opsonin for Gram-negative bacteria. Blood 108:1751–1757
Sipe JD (1999) Revised nomenclature for serum Amyloid A (SAA). Nomenclature committee for the international society of amyloidosis. Part 1. Amyloid 6:67–70
Sun L, Ye RD (2016) Serum amyloid A1: structure, function and gene polymorphism. Gene 583:48–57
Yang Q, Whitin JC, Ling XB et al (2009) Plasma biomarkers in a mouse model of preterm labor. Pediatr Res 66(1):11–16
Ye RD, Sun L (2015) Emerging functions of serum amyloid A in inflammation. J Leukoc Biol 98(6):923–929
Zhou H, Chen M, Zhang G et al (2017) Suppression of lipopolysaccharide-induced inflammatory response by fragments from serum amyloid A. J Immunol 199:1105–1112
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sack, G.H. (2020). Serum Amyloid A (SAA) Proteins. In: Hoeger, U., Harris, J. (eds) Vertebrate and Invertebrate Respiratory Proteins, Lipoproteins and other Body Fluid Proteins. Subcellular Biochemistry, vol 94. Springer, Cham. https://doi.org/10.1007/978-3-030-41769-7_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-41769-7_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-41768-0
Online ISBN: 978-3-030-41769-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)