Abstract
Serum amyloid A (SAA) is an acute-phase reactant protein predominantly bound to high-density lipoprotein in serum and presumed to play various biological and pathological roles. Upon tissue trauma or infection, hepatic expression of SAA increases up to 1,000 times the basal levels. Prolonged increased levels of SAA may lead to amyloid A (AA) amyloidosis, a usually fatal systemic disease in which the amyloid deposits are mostly comprised of the N-terminal 1–76 fragment of SAA. SAA isoforms may differ across species in their ability to cause AA amyloidosis, and the mechanism of pathogenicity remains poorly understood. In vitro studies have shown that SAA is a marginally stable protein that folds into various oligomeric species at 4 °C. However, SAA is largely disordered at 37 °C, reminiscent of intrinsically disordered proteins. Non-pathogenic murine (m)SAA2.2 spontaneously forms amyloid fibrils in vitro at 37 °C whereas pathogenic mSAA1.1 has a long lag (nucleation) phase, and eventually forms fibrils of different morphology than mSAA2.2. Remarkably, human SAA1.1 does not form mature fibrils in vitro. Thus, it appears that the intrinsic amyloidogenicity of SAA is not a key determinant of pathogenicity, and that other factors, including fibrillation kinetics, ligand binding effects, fibril stability, nucleation efficiency, and SAA degradation may play key roles. This chapter will focus on the known structural and biophysical properties of SAA and discuss how these properties may help better understand the molecular mechanism of AA amyloidosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Inflammation
- Amyloidosis
- Intrinsically disordered protein
- Prion-like infectivity
- Acute phase
- High-density lipoprotein
5.1 Introduction
5.1.1 Serum Amyloid A and AA Amyloidosis
Serum amyloid A (SAA, ~12 kDa) belongs to a highly conserved family of proteins that appears to play very important roles, including cholesterol transport (Kisilevsky and Manley 2012; van der Westhuyzen et al. 2007) and various immunological functions (Eklund et al. 2012). Acute phase SAA is predominantly synthesized by the liver and is secreted into plasma where it binds to high-density lipoprotein (HDL) (Benditt and Eriksen 1977). SAA is also expressed in normal tissue (Urieli-Shoval et al. 1998), as well as in cells in atherosclerotic plaques (Meek et al. 1994), tumor tissue (Malle et al. 2009), and the brains of individuals with Alzheimer’s disease (Chung et al. 2000; Liang et al. 1997). Considering the wide expression profile of SAA in normal tissue and in disease, it appears that this protein may not just be important during inflammation, but may also play an active role in many disease processes (for reviews see (Urieli-Shoval et al. 2000; Cunnane 2001).
Although the functions of SAA remain poorly understood, the protein appears to play a seminal role in cholesterol metabolism and transport (Kisilevsky and Subrahmanyan 1992; Liang et al. 1996; Steinmetz et al. 1989; Tam et al. 2002). Specifically, SAA binds to HDL and directs it toward cholesterol-loaded macrophages near damaged tissue to allow cholesterol recycling for tissue repair (Kisilevsky and Manley 2012). The normal level of SAA in serum is 1–3 μg/mL (Gabay and Kushner 1999). However, during acute inflammation such as infection, injury, or trauma, the levels of SAA may increase up to 1,000-fold (Gabay and Kushner 1999; McAdam and Sipe 1976). Due to this dramatic increase in SAA concentration, combined with approximately twofold decline in plasma level of HDL during the acute phase response, it is likely that not all SAA is bound to HDL (Webb et al. 1997). However, due to SAA’s intrinsic tendency to aggregate, it seems unlikely that SAA would circulate in the plasma unbound to any ligand.
The prolonged high levels of SAA associated with chronic inflammatory conditions sometimes lead to amyloid A (AA) amyloidosis, which is a secondary amyloidosis characterized by the deposition of SAA-derived amyloid fibrils in organs like liver, spleen, and kidney (Pepys 2006; Sipe 1992). AA is one of the most common systemic amyloid diseases worldwide, but is much less prevalent in western nations, ranging from 0.50 to 0.86 % (Simms et al. 1994). The prevalence is higher for particular chronic diseases, such as rheumatoid arthritis. For example, one study showed that 9 % of Finnish individuals with rheumatoid arthritis died of AA amyloidosis (Mutru et al. 1985). Another study reported that 5 % of individuals with rheumatoid arthritis develop AA amyloidosis (Husby 1998). There is no cure for AA amyloidosis, but an effective treatment involves reducing the high levels of SAA circulating in serum via administration of anti-inflammatory drugs (Hazenberg and van Rijswijk 2000; Immonen et al. 2011). It has been shown that the outcome in AA amyloidosis is favorable when the concentration of SAA is maintained below 0.01 mg/mL, but those with SAA concentration of 0.05 mg/mL had poor prognosis (Gillmore et al. 2001).
AA amyloidosis usually involves fibrillar deposits comprising the N-terminal 76-residue fragment of SAA (Sletten and Husby 1974). However, because full-length SAA and other N-terminal SAA fragments have been found in human amyloid deposits (Husebekk et al. 1985; Rocken and Shakespeare 2002; Westermark et al. 1989), and amyloid deposits in duck comprise full-length SAA (Ericsson et al. 1987), the specific role of SAA proteolysis in amyloid formation and the etiology of AA amyloidosis remains unclear. Nevertheless, the absence of the C-terminus of SAA in most AA deposits suggests that the main determinants of fibril formation are found within the N-terminal 3/4 of SAA. This hypothesis is supported by in vitro studies involving synthetic peptides representing different region of human and mouse SAA (Egashira et al. 2011; Lu et al. 2014; Westermark et al. 1992), site-directed mutations at the N-terminus of human SAA (Patel et al. 1996), proteolytic degradation of the N-terminus (Yamada et al. 1995), as well as by the amino acid sequence analysis (see Chap. 8 by Das and Gursky in this volume).
5.1.2 Pathogenic and Nonpathogenic Isoforms of SAA: Mouse Model of AA Amyloidosis
Humans and mice have two acute-phase SAA isoforms that differ in their pathogenicity, presumably due to their different ability to form amyloid deposits in vivo. Human acute phase SAAs include SAA1 and SAA2 that differ at eight residues (SAA1#SAA2: V52A, A57V, D60N, F68L, F69T, H71R, E84K, K90R). SAA1 is mostly found in amyloid deposits associated with AA amyloidosis (Liepnieks et al. 1995), and is known to exist in three different isotypes that differ from each other at residues 52 and/or 57, resulting in SAA1.1 (V52/A57), SAA1.3 (A52/A57), and SAA1.5 (A52/V57). It has been shown that Japanese individuals homozygous for SAA1.3 have a greater chance of developing AA amyloidosis, and the disease course is more likely to be aggressive with a poorer outcome (Nakamura et al. 2006). Furthermore, individuals with SAA1.1/1.1 genotype are three to seven times more likely to develop AA amyloidosis (van der Hilst 2011). In mice, most strains have SAA1.1 and SAA2.1 isoforms (formerly known as SAA2 and SAA1, respectively (Sipe 1999)) that differ at nine residues (SAA1.1#SAA2.1: I6V, G7H, G27N, D30N, G31S, A60G, S63A, M76I, A101D). AA amyloidosis can be induced in mice by injection of inflammatory reagents (Ishihara 1973; Skinner et al. 1977). Most studies have been performed in type A mice (Ishihara 1973), which produce equal amounts of SAA2.1 and SAA1.1 isoforms. Only SAA1.1 in mouse is found in amyloid deposits (Hoffman et al. 1984; Meek et al. 1986; Shiroo et al. 1987). In addition, other animal species differ in their SAA sequence and consequently, are either highly susceptible to AA amyloidosis or resistant to the disease (Sipe et al. 1993; Woldemeskel 2012; Zhang et al. 2008). Interestingly, the CE/J strain of mice expressing just one isoform, SAA2.2, was discovered to be resistant to AA amyloidosis (de Beer et al. 1993; Sipe et al. 1993). Thus, even though the sequence of SAA is highly conserved in vertebrates, differences in primary structure appear to account for the divergent pathogenicity of SAA in various species. The mechanism for this structure-pathogenic function relationship remains poorly understood.
This chapter will review the biophysical properties of HDL-free (apo) SAA and discuss the potential implications in AA amyloidosis. Despite the wealth of cellular and clinical studies involving SAA and AA amyloidosis (Obici and Merlini 2012; Westermark et al. 2015), fundamental questions remain. For example, how the biophysical properties of SAA isoforms influence their potential pathogenicity, as well as the disease onset and progression, is poorly understood. Although the biological relevance of in vitro experiments is limited and is often difficult to assess, much of our understanding about the molecular basis of amyloid diseases have benefited from such studies. Similarly, a better understanding of the structural and biophysical properties of SAA isoforms may reveal the basis for their diverse pathogenicity, and provide novel insight leading to a better understanding of the molecular mechanism of AA amyloidosis and developing novel therapeutic strategies.
5.2 AA Amyloidosis: What Is the Pathogenic Mechanism?
5.2.1 Molecular Mechanism of SAA Fibril Formation In Vivo
Amyloid formation occurs by a nucleation-dependent or seeding mechanism, where the rate-limiting step is the formation of a nucleus/seed building block that propagates fibril growth. Here, we are referring to nuclei as any oligomeric to short fibrillar species that can seed fibril formation. The time required for the nuclei to form is known as the lag phase, and it usually takes from hours to days in in vitro experiments, depending on the protein concentration and the solvent conditions. In AA amyloidosis, the disease onset in mice can be accelerated when an inflammatory stimulus is accompanied by an injection of protein extracted from AA amyloid-laden mouse (Axelrad et al. 1982; Kisilevsky and Boudreau 1983). This elusive “amyloid enhancing factor” (AEF) in AA amyloidosis was found to comprise SAA fibrils (Lundmark et al. 2002). However, the molecular entity responsible for AEF activity has not been defined, and may comprise one or more degradation-resistant species, including amyloid nuclei or small fibrils readily generated from the breakup of larger SAA fibrils. Remarkably, AEF was shown to be effective when administered orally, indicating that AA amyloidosis may be transmissible via a prion-like mechanism (Lundmark et al. 2002). A hallmark of prion transmissibility is the high stability of the prion species, which enables it to resist denaturation and proteolytic degradation in the digestive tract, thereby allowing oral transmissibility. Thus, the stability of the SAA-based amyloid nuclei or protofibrils, which are the putative prion-genic species, is likely critical for the onset and transmissibility of AA amyloidosis.
The persistently high level of SAA during chronic inflammation is an essential prerequisite for AA amyloidosis. However, the relationship between inflammation – unrelated to the high levels of SAA – and amyloid deposition is not easily decoupled. A recent transgenic mouse model study in which the concentration of SAA was increased by doxycycline-inducible expression showed that high expression (>1.0 mg/mL) of SAA is sufficient for the onset of AA amyloidosis independently of inflammation (Simons et al. 2013). In addition, this dose-dependent transgenic model showed that when the concentration of SAA was raised modestly to ~0.12 mg/mL for a few weeks, the still healthy mice were primed for very fast amyloid deposition when the concentration of SAA was subsequently increased to the pathological concentration of >1.0 mg/mL. Furthermore, when the concentration of SAA was decreased after the onset of AA amyloidosis, there was evidence of amyloid clearance, even though the mice remained primed for disease. These remarkable results demonstrate that the structure and biophysical properties of SAA and its fibrils, along with time of exposure to high SAA concentration, are critical factors in the etiology of AA amyloidosis. The apparent competition between AA accumulation and clearance suggests that, unlike other amyloid diseases where a putative toxic species is responsible for pathology (Guerrero-Munoz et al. 2014; Stefani 2012), the pathology in AA amyloidosis arises from the progressive accumulation of amyloid fibrils that interfere with normal organ function.
5.2.2 Intrinsic Factors Affecting the Pathological Accumulation of SAA Fibrils
Although biophysical properties of SAA isoforms, such as nucleation/fibrillation kinetics and nucleus/fibril stability, likely play a major role in the etiology of AA amyloidosis, the relative contributions of these and other endogenous factors remain unclear. In particular, two inherent SAA properties stand out. One is the kinetics of amyloid nucleation and fibril growth; the other is the kinetic stability, i.e. degradation-resistance, of amyloid nuclei and fibrils. The kinetics of amyloid formation depends strongly on the SAA concentration that must exceed a required threshold for nuclei formation and fibril growth. Below a certain concentration, SAA may not fibrillate fast enough to overcome its clearance. In individuals with AA amyloidosis, keeping their SAA levels below 0.01 mg/mL via aggressive treatment of inflammation has been shown to result in beneficial outcome, including regression of amyloid deposits (Gillmore et al. 2001; Lachmann et al. 2007). In contrast, the disease progressed in patients whose SAA levels were persistently above 0.05 mg/mL (Gillmore et al. 2001). Thus, administration of anti-inflammatory medication to keep the SAA concentration at low levels has been effective in reducing the incidence and mortality of AA amyloidosis in developed countries (Gillmore et al. 2001). The persistence of amyloid deposition also depends on nuclei and fibril stability. The inherent ability of SAA to form highly stable amyloid nuclei is also likely a main factor in AA amyloidosis. The persistence of SAA nuclei in mice primed for SAA deposition (Simons et al. 2013) suggests that these precursor aggregates (i.e. seeds) are kinetically stable and, therefore, resistant to proteolysis (Manning and Colon 2004). The stability of SAA seeds would explain the AEF effect observed in mice in vivo, as well as the observation that cheetah exhibits prion-like infectivity of AA amyloidosis (Lundmark et al. 2002; Zhang et al. 2008). Thus, the kinetics of SAA amyloid nucleation and growth, as well as the stability of the precursor aggregates and fibrils are likely the main contributors to the diverse pathogenicity of SAA isoforms.
5.2.3 Endogenous Factors Affecting the Pathological Accumulation of SAA Fibrils
The low incidence of AA amyloidosis indicates that endogenous genetic or environmental factors play an important pathological role. The most important endogenous factor is the expression level of SAA during inflammation. The concentration of SAA may increase up to 1,000-fold during episodes of acute inflammation, but the exact level, as well as the frequency and the duration of the acute episodes, vary for different individuals. Another endogenous factor involves the availability and effect of SAA ligands. Although SAA is an apolipoprotein-related protein that binds HDL, as well as heparin/heparan sulfate (HS) and other ligands, e.g. laminin and various peripheral membrane proteins (Urieli-Shoval et al. 2000), it remains unclear how the endogenous amounts of these ligands impact the etiology of AA amyloidosis. Most SAA that circulates in plasma in HDL-bound form is presumably safe from fibrillation. Therefore, SAA and its fragments seem at the greatest risk for deposition at sites of inflammation, where SAA is released and internalized by macrophages. However, one possibility is that not all SAA may be HDL-bound during acute inflammation and, therefore, it is plausible that free SAA (or SAA bound to some other ligand) may build up in certain tissues and be at risk of aggregating. This is supported by reports of extra-hepatic SAA leading to amyloid deposition in mice brain and chicken joint (Guo et al. 2002; Landman 1999). Therefore, the significance of localized HDL-free SAA may be more pathologically relevant than commonly assumed. Since HDL-free SAA is at risk of aggregation, the endogenous level of HDL may affect the levels of HDL-free SAA in vivo and thereby influence AA amyloidosis.
Interestingly, it has been shown that HS and heparin (Hep) can displace SAA from HDL (Noborn et al. 2012). This observation is significant because of substantial evidence that HS and, perhaps, Hep are important in AA amyloidosis, presumably by accelerating amyloid formation (Elimova et al. 2009; Li et al. 2005; Snow et al. 1991). Thus, it is plausible that the SAA displacement from HDL may occur in the Hep-rich macrophages or in HS-rich extracellular matrix environment, where SAA is then internalized by macrophages. The binding of SAA to HS may also serve as a way to increase the concentration of SAA in amyloidogenic focal points in tissues. In vitro studies have found that HS and Hep accelerate the fibrillation of many amyloidogenic proteins, including SAA (Elimova et al. 2009; van Horssen et al. 2003; Zhang and Li 2010). Thus, the displacement of SAA from HDL at sites of tissue damage and the consequent conformational changes in SAA are dynamic processes likely modulated by the levels of glycosaminoglycans (GAGs) and other factors.
Another fundamental endogenous factor in SAA amyloid deposition is the efficiency of the protein quality control system, including the degradation of SAA and its amyloid deposits. The term “proteostasis” describes the overall homeostasis of proteins in an organism, and compromised proteostasis may lead to amyloid diseases (Cuanalo-Contreras et al. 2013; Kim et al. 2013). The persistently high concentration of SAA in chronic inflammatory diseases is likely to place a stress on proteostasis, which in some individuals may have pathological consequences. For example, the incomplete proteolysis of SAA may accelerate its fibrillation kinetics or enhance the stability of the resulting AA fibrils. This may explain why AA deposits comprise N-terminal fragments of SAA, although the etiological role of SAA degradation in AA amyloidosis still remains unclear. Compromised proteostasis would also slow down the clearance of amyloid, which is stabilized by its interaction with serum amyloid P and GAGs, in particular HS. Therefore, the endogenous amounts of these “amyloid stabilizers” are also expected to impact the rate of amyloid clearance. In support of this idea, AA amyloidosis was shown to slow down in a transgenic knockout mouse of serum amyloid P (Inoue et al. 2005), further highlighting the precarious balance between amyloid deposition and degradation.
5.3 Structural Properties of SAA
5.3.1 SAA May Form Different Oligomers Upon Refolding In Vitro
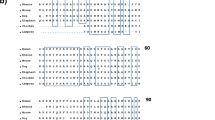
SAA expressed in E. coli must be purified under denaturing conditions due to its tendency to aggregate. Previous studies have shown that mSAA2.2, mSAA1.1, and hSAA1.1 fold into various oligomeric species in vitro, including hexamer, octamer, tetramer, and dodecamer (Lu et al. 2014; Patke et al. 2013; Srinivasan et al. 2013; Wang et al. 2002, 2011). Interestingly, mSAA2.2 first refolds into a kinetically accessible octamer that at 4 °C converts into a more stable hexamer within 3–4 weeks (Fig. 5.1) (Wang et al. 2011). In contrast, mSAA1.1 refolds into a mixture of dodecamer, tetramer, and monomers that does not change much over time at 4 °C (Srinivasan et al. 2013). In the case of hSAA1.1, size-exclusion chromatography data showed a single peak with a variable elution time consistent with a mixture of octamers and hexamers (Patke et al. 2013).
Refolding of murine SAA2.2 monitored by size-exclusion chromatography. Purified and urea-denatured mSAA2.2 was dialyzed against Tris buffer at 4 °C, and protein oligomerization was analyzed by size-exclusion chromatography over time. mSAA2.2 first refolded into an octamer that, over several weeks, converted to a hexamer (Reprinted from (Wang et al. 2011), Copyright (2011), with permission from Elsevier)
The biological relevance of the oligomeric structures of SAA observed in vitro at 4 °C is poorly understood. However, it seems unlikely that proteins would evolve to fold and assemble into specific oligomers without selective pressure to do so. Therefore, although SAA oligomers are marginally stable, it is plausible that the very high concentration of SAA during acute inflammation together with ligand binding may modulate the oligomeric structure of HDL-free SAA in vivo. The ability of certain proteins to oligomerize upon ligand binding or to interconvert among oligomeric species is well established. Many proteins exhibit such oligomeric plasticity, including human porphobilinogen synthase (Breinig et al. 2003), geranylgeranyl diphosphate synthase (Miyagi et al. 2007), protective antigen protein of the anthrax toxin (Kintzer et al. 2009), and LIM domain binding proteins (Cross et al. 2010). Thus, the possibility that SAA may form different functional oligomers is intriguing, and further studies are warranted to explore this idea (see Sect. 5.3.3).
5.3.2 SAA Is an Intrinsically Disordered Protein
Although SAA folds into α-helical oligomeric structures at 4 °C, previous studies have shown that mSAA2.2, mSAA1.1, and hSAA1.1 are marginally stable proteins with thermal denaturation mid-points circa 32, 22, and 20 °C, respectively (Patke et al. 2013; Srinivasan et al. 2013; Wang and Colon 2005; Wang et al. 2005). At 37 °C, SAA is largely disordered prior to aggregation, and hence, HDL-free SAA is an intrinsically disordered protein (IDP). IDPs are characterized by their lack of stable secondary and/or tertiary structure in vitro under physiologically-relevant conditions, and by their ability to acquire one or more functional states upon binding to small ligands or macromolecules (Uversky 2013; also see Chap. 2 by Uversky in this volume). Remarkably, many aggregation-prone proteins associated with human neurodegenerative diseases are intrinsically disordered (Uversky 2009). Viewing the structure and function of SAA from the perspective of an IDP, one could explain how SAA may have multiple functions, depending on the environment and its interactions with ligands. Therefore, in addition to SAA’s key function in cholesterol recycling (Kisilevsky and Manley 2012), other putative functions related to lipid metabolism and immune regulation, as well as SAA functions not yet discovered, likely exist within the framework of an IDP. For example, the structure of SAA may be modulated via an induced fit model, in which binding with high specificity – low affinity to various ligands, ranging from small molecules to peripheral membrane proteins, induces the formation of different functionally relevant conformations (Uversky 2013).
The mechanism by which SAA is released from HDL, which is a likely prerequisite for SAA fibrillation, appears to involve HS and Hep (Noborn et al. 2012). Recent studies have shown that heparin is able to displace SAA from HDL in vitro (Noborn et al. 2012). Since Hep is usually released from mast cells into the blood at sites of tissue injury, one of its physiological roles may involve the release of SAA from HDL at sites of tissue damage. It remains unknown whether turnover of SAA occurs immediately upon release from HDL, or whether Hep/HS binding may modulate the structure of SAA to carry out other functions. In summary, the intrinsic capability of SAA to adopt diverse structures ranging from an intrinsically disordered monomer to HDL-bound form to specific oligomers and higher-order species that are substantially α-helical, is intriguing and may help explain the many putative functions of SAA.
5.3.3 The 3D Structures of Human SAA1.1 and Mouse SAA3 Have Been Solved
Although SAA was discovered over 40 years ago (Levin et al. 1972), the 3D structures of two different SAA proteins were solved only in 2014, providing an unprecedented opportunity to understand how small differences in SAA sequence affect the biochemical and biophysical properties of the protein. The 2.2 Å resolution crystal structure of hSAA1.1 revealed a hexamer comprised of two trimers, with each monomer folding into a cone-shaped four-helix bundle stabilized by the C-terminal tail wrapped around it (Fig. 5.2) (Lu et al. 2014). The structure also showed two clusters of positively charged residues, one around the central pore of the hexamer (involving residues Arg15, Arg19, and Arg47) and another at the trimer apex (involving residues Arg1, Arg62, and His71) (Fig. 5.2). Experiments involving mutations of the relevant Arg residues showed that both charged regions bind to Hep. Subsequent experiments showed that HDL could not bind to hSAA1.1 when Hep was bound to the apex region, indicating that the HDL binding site involves the apex region and can be inhibited by Hep and, presumably, HS (Lu et al. 2014). These results are consistent with the recent observation that HS and Hep can dissociate SAA from HDL (Noborn et al. 2012). The crystal structure of hSAA1.1 also showed that helices 1 and 3, which are the most amyloidogenic regions of SAA, are sequestered within the hexameric structure, in agreement with prior in vitro studies showing that dissociation of the hexameric structure is required for aggregation and formation of fibrils (Patke et al. 2013; Srinivasan et al. 2013; Wang et al. 2005). The 3D structure of hSAA1.1 supports many previous in vitro findings and conclusions regarding the biophysical properties of SAA. These include the hexameric assembly of hSAA1.1 (Patke et al. 2013), the finding that different SAAs are likely to assemble into different oligomers (Srinivasan et al. 2013; Wang et al. 2002, 2011), and the observation that the C-terminal part of SAA is important for α-helical stability and oligomer formation (Patke et al. 2012).
Three-dimensional x-ray crystal structure of hSAA1.1 (a) hexamer and (b) monomer determined to 2.2 Å resolution (PDB 4IP9) (Lu et al. 2014). hSAA1.1 folds into an up-down-up-down cone-shaped four-helix bundle with a C-terminal tail that stabilizes the fold by wrapping around the bundle. Each helix is labeled in a different color. The hexamer (viewed down the threefold axis) is comprised of two trimers. Three copies of the N-terminal GAG/HDL binding site located at the trimer apex are indicated
The second crystal structure was that of mouse (m)SAA3, determined to 2.0 Å resolution (Derebe et al. 2014). Comparison of the two atomic structures revealed remarkable similarity in the conformations of hSAA1.1 and mSAA3 molecules. However, unlike hSAA1.1, which was crystallized as a dimer or a hexamer, mSAA3 was crystallized as a tetramer with a central hydrophobic pocket that binds retinol with nanomolar affinity. Retinol, a small lipid-soluble compound plays crucial roles in protecting against bacterial infection, and must be transported by a protein carrier. The remarkable discovery that mSAA3 is a retinol binding protein provides the first direct evidence of a functional oligomeric SAA structure, and more such functions may exist. Interestingly, even though mSAA2.2 forms a hexamer in vitro, electron microscopic images revealed a ring-like assembly where the mSAA2.2 monomers interact side-by-side (Wang et al. 2002), suggesting that more oligomeric architectures of SAA will likely be forthcoming. Thus, the atomic structures of hSAA1.1 and mSAA3 will be major assets in future efforts to understand the breadth of SAA structure-function relationship, including the promising prospect of gaining a structural-level understanding for the diverse pathogenicity of SAA isoforms.
5.4 In Vitro Studies Provide Insights into the Diverse Pathogenicity of SAA Isoforms
5.4.1 Inherent Amyloidogenicity of SAA Does Not Correlate with the Pathogenicity of Different Isoforms
Although many factors likely contribute to the development of AA amyloidosis, the existence of pathogenic and nonpathogenic SAA isoforms suggests that their pathogenic potential correlates with their amyloidogenicity, i.e. with the rate of fibril formation at near-physiologic conditions. However, this is not the case. In fact, nonpathogenic SAA2.2, which is the only isoform present in AA amyloidosis-resistant CE/J mouse, quickly self-assembles into fibrils upon incubation at 37 °C (Wang et al. 2005). In contrast, pathogenic mSAA1.1 exhibits a longer (3–4 days at 0.3 mg/mL SAA1.1) oligomer-rich fibrillation lag phase before forming fibrils (Fig. 5.3).
Kinetics of mSAA1.1 and mSAA2.2 fibrillation at 37 °C probed by (a) Thioflavin-T fluorescence and (b) atomic force microscopy (AFM). Error bars correspond to normalized standard deviation from three independent experiments. AFM images show mSAA2.2 and mSAA1.1 samples incubated at 37 °C for 24 h and 48 h, respectively. The images are shown as height traces, and the scale bar corresponds to 1 μm (The panels in this figure were originally published in The Journal of Biological Chemistry (Srinivasan et al. 2013) © the American Society for Biochemistry and Molecular Biology)
The lack of correlation between the in vitro rate of SAA fibril formation and pathogenicity is further supported by studies showing that pathogenic hSAA1.1 forms aggregates and protofibril-like species, but does not form mature amyloid fibrils in vitro upon incubation at 37 °C (Fig. 5.4) (Lu et al. 2014; Patke et al. 2013). In contrast, recombinant Met-hSAA1.1 protein expressed in E. coli, which contains an additional methionine at position 1, does form fibrils in vitro (Fig. 5.4), suggesting that fibril formation is importantly modulated by the N-terminal methionine (Patke et al. 2013). It is possible the pathologically relevant property is the relative amyloidogenicity of the N-terminal fragments and not of the full-length protein. This would explain the lack of correlation between the in vitro amyloid formation of full-length SAA isoforms and their pathogenicity. Alternatively, it may be that the timescale of in vitro experiments is biologically irrelevant because in vivo formation of the hSAA1.1 amyloid nucleus is probably a much slower process. Here, we are using the kinetics of fibril formation to define amyloidogenicity. However, in the years-long timescale of individuals with chronic inflammatory conditions, the biologically relevant definition of amyloidogenicity may not be “how fast”, but rather “how persistent/stable”. In summary, it may not be the rate of full-length SAA fiber formation in vitro, but perhaps other properties of SAA and other in vivo factors that determine the fibril accumulation in AA amyloidosis.
Atomic force microscopy images of fibrils and aggregates formed by MetSAA1.1 and hSAA1.1, respectively. MetSAA1.1 is recombinant hSAA1.1 with an additional methionine at position 1. The samples (0.24 mg/mL) were incubated at 37 °C for the designated amount of time. AFM images correspond to (a) MetSAA1.1, 3 h; (b) MetSAA1.1, 72 h; (c) hSAA1.1, 3 h; (d) hSAA1.1, 200 h. The insets show expanded regions, and the three black arrows in (c) outside the inset point to assemblies of spherical aggregates. The images are shown as height traces, and the scale bar corresponds to 1 μm (This figure was originally published in PLOS One Patke et al. 2013)
5.4.2 Stability of SAA Amyloid
The accumulation of SAA deposits is the main histopathological feature in AA amyloidosis. Therefore, the dynamic equilibrium between the accumulation of amyloid and its clearance is of paramount importance. It is clear from mouse model studies that if the fibrillation of SAA is decreased or inhibited, amyloid deposits can be cleared, and AA amyloidosis can be averted (Simons et al. 2013). However, the rate of amyloid clearance depends not only on the robustness of the protein degradation system, but also on the stability of the amyloid fibrils. At one end of the spectrum, marginally stable amyloid fibrils may never accumulate enough to cause the disease, even if they form during acute inflammation. At the other extreme, the formation of kinetically stable, degradation-resistant fibrils will stress the protein degradation system, thereby increasing the risk of disease.
Although most amyloid fibrils formed by different proteins and peptides are known to be very stable, recent studies have shown that amyloid fibrils formed in vitro by non-pathogenic mSAA2.2 are marginally stable (Ye et al. 2011). Although at inflammation-relevant concentration (≥0.3 mg/mL), mSAA2.2 quickly fibrillates upon incubation at 37 °C, the resulting fibrils dissociate upon modest increase in temperature (over 45 °C) and urea concentration (>1.0 M) (Ye et al. 2011). Fibrils formed by pathogenic mSAA1.1 appear to be similarly unstable (unpublished results). Thus, the mSAA1.1 fibrils formed in vitro may not be the same as the pathogenic fibrils formed in vivo.
It is instructive to consider two possible scenarios in which the stability of SAA fibrils may or may not contribute to AA amyloidosis. First, one can envision two distinct types of SAA fibrils differing in stability and morphology. Fibrils of one type may be intrinsically unstable in vivo and be easily degraded, thereby explaining the poorly understood low incidence of AA amyloidosis in humans with chronic inflammatory conditions. Fibrils of the other type, which are more stable and pathogenic, may not be kinetically favored, requiring a long time to form. The latter fibrils may have similar morphology to AEF, thereby explaining the persistence of the AEF and its ability to catalyze the formation of stable pathologically relevant SAA fibrils. Second, the development of AA amyloidosis may require other ligands or factors to either accelerate the formation of stable SAA fibrils or to stabilize the already formed fibrils. Either effect could potentially overwhelm the degradation of SAA fibrils and result in increased amyloid deposition. Thus, understanding the intrinsic stability of amyloid fibrils accessible to different SAA isoforms, and the effect of ligand binding and the cellular environment, will be critical for better understanding the AEF effect, SAA isoform pathogenicity, and species susceptibility in AA amyloidosis.
5.4.3 SAA Can Form Fibrils of Different Morphology: Effects of GAGs
Over the past 15 years there has been an increased appreciation for the morphological differences among amyloid fibrils, including the ability of certain peptides and proteins to form fibrils of different morphologies depending on the solution conditions (Jahn and Radford 2008; Kodali and Wetzel 2007). These morphological disparities may result in (or reflect) different biochemical and biophysical properties of fibrils that may determine the preference for amyloid deposition in certain tissue, its resistance to degradation, and prion-like transmissibility (Meyer-Luehmann et al. 2006; Seilheimer et al. 1997; Tanaka et al. 2006).
Recent studies showed that lipid-free nonpathogenic mSAA2.2 and pathogenic mSAA1.1 form amyloid fibrils with different morphologies (Fig. 5.5). Longitudinal atomic force microscopy (AFM) experiments showed that the morphological differences arose from formation of different pre-fibrillar oligomers and amyloid seeds resulting in different fibrillation pathways (Fig. 5.6) (Srinivasan et al. 2013). This is consistent with earlier studies revealing morphological diversity in ex vivo SAA amyloid deposits (Jimenez et al. 2001). Due to the marginal stability of SAA at 37 °C and its high tendency to quickly aggregate, kinetic factors are likely to play an important role in determining the morphologic outcome of fibril formation (Pellarin et al. 2010). The ability of SAA to form fibrils of different morphologies is consistent with the observation that different amyloid-forming peptides/proteins can serve as an AEF in mouse models of AA amyloidosis (Westermark et al. 2009).
AFM data showing that mSAA1.1 and mSAA2.2 form amyloid fibrils of different morphologies. (a) AFM images of mSAA1.1 and mSAA2.2 aggregates after incubation at 37 °C for 70 h and 10 h, respectively. (b) Plot of early fibril (i.e. protofibril) cross-section was obtained from the corresponding height traces in (a). (c) AFM images of mSAA1.1 and mSAA2.2 full-length fibrils formed after incubation at 37 °C for 150 h and 50 h, respectively. (d) Plot of the fibril cross-section was obtained from the corresponding height traces in (c) (This figure was originally published in The Journal of Biological Chemistry (Srinivasan et al. 2013) © the American Society for Biochemistry and Molecular Biology)
Model of mSAA1.1 and mSAA2.2 fibril formation in vitro. At 37 °C mSAA2.2 misfolds and forms oligomers that self-assemble into curvilinear fibrils. They further grow and intertwine into mature fibrils that may self-assemble into braided bundles. mSAA1.1 quickly forms spherical oligomers larger than those formed by mSAA2.2, which slowly give rise to rod-like protofibrils or short fibrils that assemble into straight fibrils. Mature mSAA1.1 fibrils seem more rigid than those formed by mSAA2.2, and appear to interact laterally with each other rather than intertwine (This figure was originally published in The Journal of Biological Chemistry (Srinivasan et al. 2013) © the American Society for Biochemistry and Molecular Biology)
In addition to the amino acid sequence of SAA, in vivo factors, including the concentration of SAA and binding to ligands, may affect the morphology of SAA fibrils. Of the potential ligands, GAGs are of particular importance because of their role in the etiology of AA amyloidosis (Ancsin and Kisilevsky 1999; Elimova et al. 2004; Li et al. 2005; Snow et al. 1991; Wang et al. 2012). The importance of GAGs, in particular HS, in amyloid diseases is not limited to AA amyloidosis, as it is well known that HS are ubiquitously present in nearly all amyloid deposits (Zhang and Li 2010). In addition, in vitro studies with many proteins have shown that HS can accelerate amyloid formation (see Bourgault et al. 2011; Martin and Ramirez-Alvarado 2011; Solomon et al. 2011). Concerning SAA, it has been shown that GAGs affect the biophysical properties of SAA, including its aggregation kinetics and aggregate morphology (Aguilera et al. 2014; Elimova et al. 2009). Interestingly, the aggregation of mSAA1.1 in vitro may be modulated by the presence of GAGs (Fig. 5.7) (Aguilera et al. 2014). When HS, hyaluronic acid, and heparosan (these sugars have similar backbone moeities) were individually incubated with refolded mSAA1.1 at 37 °C, SAA1.1 fibril morphology was largely unaffected. In contrast, mono-sulfated chondroitin sulfate A (CSA) blocked SAA fibril formation and enabled the formation of spherical aggregates of various sizes. Heparin – the most sulfated GAG – was not only the most effective GAG in accelerating the aggregation of mSAA1.1, but also resulted in the formation of vast amounts of thin protofibrils that were latent in converting to mature fibrils (Fig. 5.7). Thus, Hep catalyzes the in vitro aggregation of mSAA1.1 along a different pathway (Aguilera et al. 2014).
Effect of different GAGs on the aggregation and fibrillation of mSAA1.1 at 37 °C. The central pathways (green arrows) show prototypical mSAA1.1-like fibril formation indicating minimal effect of HS on fibril morphology. Hep (red curve) caused formation of abundant mSAA1.1 protofibrils that appear to be capped and unable to grow into mature fibrils. mSAA1.1 fibril formation was completely inhibited by interactions with chondroitin sulfate (blue curve), which mostly produced spherical species of various size (Reprinted from Aguilera et al. 2014, Copyright (2014), with permission from Elsevier)
Numerous studies have probed the effect of GAGs on SAA fibrillation (Elimova et al. 2004, 2009; Kisilevsky and Fraser 1996; Li et al. 2005; Noborn et al. 2012). The results are not in consistent agreement with each other, which is likely a result of differences in experimental design, including in vitro versus in vivo experiments, various SAA isoforms or peptides, differences in the solvent pH, SAA concentrations, etc. Nevertheless, overall these studies suggest that HS and Hep exert a major influence on the aggregation and fibrillation pathway of SAA in vivo.
5.5 Conclusions
A better understanding of the biological functions and pathogenicity of SAA across different species will require a better understanding of the biochemical and biophysical properties of SAA isoforms. In particular, questions related to different pathogenicity of SAA isoforms, the low disease incidence in individuals at risk, the role of ligands (such as HDL and GAGs) in SAA function and in AA disease, and the prion-like transmission potential of SAA are directly related to the biophysical properties of SAA. The current picture emerging from biophysical studies is that, depending on the environmental conditions, SAA proteins have many structural options with distinct functional and pathological implications. At low temperature, SAAs are marginally stable proteins that can fold into various oligomeric structures, whereas at 37 °C SAA behaves like an IDP that is highly prone to aggregation into higher-order species, including fibrils of different morphologies. These morphological differences could be relevant to disease onset and transmissibility and deserve further investigation. In addition, due to the marginal stability of SAA and its inherent oligomeric and aggregate plasticity, the fibrillation of SAA seems particularly susceptible to modulation by extrinsic factors, in particular HDL and GAGs. Further biophysical studies are needed to explore whether the development of AA amyloidosis is mostly determined by the competition between SAA fibril formation and its degradation. The recently determined atomic structures of SAA have provided much needed biophysical insight, and future structural studies will be essential to understand the biophysical properties of SAA that determine the diverse pathogenicity of SAA isoforms.
Abbreviations
- AA:
-
Amyloid A
- AEF:
-
Amyloid enhancing factor
- AFM:
-
Atomic force microscopy
- GAGs:
-
Glycosaminoglycans
- HDL:
-
High-density lipoprotein
- Hep:
-
Heparin
- HS:
-
Heparan sulfate
- hSAA:
-
Human serum amyloid A
- IDP:
-
Intrinsically disordered proteins
- mSAA:
-
Mouse serum amyloid A
- SAA:
-
Serum amyloid A
- SEC:
-
Size-exclusion chromatography
References
Aguilera JJ, Zhang F, Beaudet JM, Linhardt RJ, Colon W (2014) Divergent effect of glycosaminoglycans on the in vitro aggregation of serum amyloid A. Biochimie 104:70–80
Ancsin JB, Kisilevsky R (1999) The heparin/heparan sulfate-binding site on apo-serum amyloid A. Implications for the therapeutic intervention of amyloidosis. J Biol Chem 274:7172–7181
Axelrad MA, Kisilevsky R, Willmer J, Chen SJ, Skinner M (1982) Further characterization of amyloid-enhancing factor. Lab Invest 47:139–146
Benditt EP, Eriksen N (1977) Amyloid protein SAA is associated with high density lipoprotein from human serum. Proc Natl Acad Sci U S A 74:4025–4028
Bourgault S, Solomon JP, Reixach N, Kelly JW (2011) Sulfated glycosaminoglycans accelerate transthyretin amyloidogenesis by quaternary structural conversion. Biochemistry 50:1001–1015
Breinig S, Kervinen J, Stith L, Wasson AS, Fairman R, Wlodawer A, Zdanov A, Jaffe EK (2003) Control of tetrapyrrole biosynthesis by alternate quaternary forms of porphobilinogen synthase. Nat Struct Biol 10:757–763
Chung TF, Sipe JD, McKee A, Fine RE, Schreiber BM, Liang JS, Johnson RJ (2000) Serum amyloid A in Alzheimer’s disease brain is predominantly localized to myelin sheaths and axonal membrane. Amyloid 7:105–110
Cross AJ, Jeffries CM, Trewhella J, Matthews JM (2010) LIM domain binding proteins 1 and 2 have different oligomeric states. J Mol Biol 399:133–144
Cuanalo-Contreras K, Mukherjee A, Soto C (2013) Role of protein misfolding and proteostasis deficiency in protein misfolding diseases and aging. Int J Cell Biol 2013:1–10
Cunnane G (2001) Amyloid precursors and amyloidosis in inflammatory arthritis. Curr Opin Rheumatol 13:67–73
de Beer MC, de Beer FC, McCubbin WD, Kay CM, Kindy MS (1993) Structural prerequisites for serum amyloid A fibril formation. J Biol Chem 268:20606–20612
Derebe MG, Zlatkov CM, Gattu S, Ruhn KA, Vaishnava S, Diehl GE, MacMillan JB, Williams NS, Hooper LV (2014) Serum amyloid A is a retinol binding protein that transports retinol during bacterial infection. Elife 3:e03206
Egashira M, Takase H, Yamamoto I, Tanaka M, Saito H (2011) Identification of regions responsible for heparin-induced amyloidogenesis of human serum amyloid A using its fragment peptides. Arch Biochem Biophys 511:101–106
Eklund KK, Niemi K, Kovanen PT (2012) Immune functions of serum amyloid A. Crit Rev Immunol 32:335–348
Elimova E, Kisilevsky R, Szarek WA, Ancsin JB (2004) Amyloidogenesis recapitulated in cell culture: a peptide inhibitor provides direct evidence for the role of heparan sulfate and suggests a new treatment strategy. FASEB J 18:1749–1751
Elimova E, Kisilevsky R, Ancsin JB (2009) Heparan sulfate promotes the aggregation of HDL-associated serum amyloid A: evidence for a proamyloidogenic histidine molecular switch. FASEB J 23:3436–3448
Ericsson LH, Eriksen N, Walsh KA, Benditt EP (1987) Primary structure of duck amyloid protein A. The form deposited in tissues may be identical to its serum precursor. FEBS Lett 218:11–16
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Gillmore JD, Lovat LB, Persey MR, Pepys MB, Hawkins PN (2001) Amyloid load and clinical outcome in AA amyloidosis in relation to circulating concentration of serum amyloid A protein. Lancet 358:24–29
Guerrero-Munoz MJ, Castillo-Carranza DL, Kayed R (2014) Therapeutic approaches against common structural features of toxic oligomers shared by multiple amyloidogenic proteins. Biochem Pharmacol 88:468–478
Guo JT, Yu J, Grass D, de Beer FC, Kindy MS (2002) Inflammation-dependent cerebral deposition of serum amyloid a protein in a mouse model of amyloidosis. J Neurosci 22:5900–5909
Hazenberg BP, van Rijswijk MH (2000) Where has secondary amyloid gone? Ann Rheum Dis 59:577–579
Hoffman JS, Ericsson LH, Eriksen N, Walsh KA, Benditt EP (1984) Murine tissue amyloid protein AA. NH2-terminal sequence identity with only one of two serum amyloid protein (ApoSAA) gene products. J Exp Med 159:641–646
Husby G (1998) Treatment of amyloidosis and the rheumatologist. State of the art and perspectives for the future. Scand J Rheumatol 27:161–165
Husebekk A, Skogen B, Husby G, Marhaug G (1985) Transformation of amyloid precursor SAA to protein AA and incorporation in amyloid fibrils in vivo. Scand J Immunol 21:283–287
Immonen K, Finne P, Gronhagen-Riska C, Pettersson T, Klaukka T, Kautiainen H, Hakala M (2011) A marked decline in the incidence of renal replacement therapy for amyloidosis associated with inflammatory rheumatic diseases – data from nationwide registries in Finland. Amyloid 18:25–28
Inoue S, Kawano H, Ishihara T, Maeda S, Ohno S (2005) Formation of experimental murine AA amyloid fibrils in SAP-deficient mice: high resolution ultrastructural study. Amyloid 12:157–163
Ishihara T (1973) Experimental amyloidosis using silver nitrate – electron microscopic study on the relationship between silver granules, amyloid fibrils and reticuloendothelial system. Acta Pathol Jpn 23:439–464
Jahn TR, Radford SE (2008) Folding versus aggregation: polypeptide conformations on competing pathways. Arch Biochem Biophys 469:100–117
Jimenez JL, Tennent G, Pepys M, Saibil HR (2001) Structural diversity of ex vivo amyloid fibrils studied by cryo-electron microscopy. J Mol Biol 311:241–247
Kim YE, Hipp MS, Bracher A, Hayer-Hartl M, Hartl FU (2013) Molecular chaperone functions in protein folding and proteostasis. Annu Rev Biochem 82:323–355
Kintzer AF, Thoren KL, Sterling HJ, Dong KC, Feld GK, Tang II, Zhang TT, Williams ER, Berger JM, Krantz BA (2009) The protective antigen component of anthrax toxin forms functional octameric complexes. J Mol Biol 392:614–629
Kisilevsky R, Boudreau L (1983) Kinetics of amyloid deposition. I. The effects of amyloid-enhancing factor and splenectomy. Lab Invest 48:53–59
Kisilevsky R, Fraser P (1996) Proteoglycans and amyloid fibrillogenesis. Ciba Found Symp 199:58–67 (discussion 68-72, 90-103)
Kisilevsky R, Manley PN (2012) Acute-phase serum amyloid A: perspectives on its physiological and pathological roles. Amyloid 19:5–14
Kisilevsky R, Subrahmanyan L (1992) Serum amyloid A changes high density lipoprotein’s cellular affinity. A clue to serum amyloid A’s principal function. Lab Invest 66:778–785
Kodali R, Wetzel R (2007) Polymorphism in the intermediates and products of amyloid assembly. Curr Opin Struct Biol 17:48–57
Lachmann HJ, Goodman HJ, Gilbertson JA, Gallimore JR, Sabin CA, Gillmore JD, Hawkins PN (2007) Natural history and outcome in systemic AA amyloidosis. N Engl J Med 356:2361–2371
Landman WJ (1999) Amyloid arthropathy in chickens. Vet Q 21:78–82
Levin M, Franklin EC, Frangione B, Pras M (1972) The amino acid sequence of a major nonimmunoglobulin component of some amyloid fibrils. J Clin Invest 51:2773–2776
Li JP, Galvis ML, Gong F, Zhang X, Zcharia E, Metzger S, Vlodavsky I, Kisilevsky R, Lindahl U (2005) In vivo fragmentation of heparan sulfate by heparanase overexpression renders mice resistant to amyloid protein A amyloidosis. Proc Natl Acad Sci U S A 102:6473–6477
Liang JS, Schreiber BM, Salmona M, Phillip G, Gonnerman WA, de Beer FC, Sipe JD (1996) Amino terminal region of acute phase, but not constitutive, serum amyloid A (apoSAA) specifically binds and transports cholesterol into aortic smooth muscle and HepG2 cells. J Lipid Res 37:2109–2116
Liang JS, Sloane JA, Wells JM, Abraham CR, Fine RE, Sipe JD (1997) Evidence for local production of acute phase response apolipoprotein serum amyloid A in Alzheimer’s disease brain. Neurosci Lett 225:73–76
Liepnieks JJ, Kluve-Beckerman B, Benson MD (1995) Characterization of amyloid A protein in human secondary amyloidosis: the predominant deposition of serum amyloid A1. Biochim Biophys Acta 1270:81–86
Lu J, Yu Y, Zhu I, Cheng Y, Sun PD (2014) Structural mechanism of serum amyloid A-mediated inflammatory amyloidosis. Proc Natl Acad Sci U S A 111:5189–5194
Lundmark K, Westermark GT, Nystrom S, Murphy CL, Solomon A, Westermark P (2002) Transmissibility of systemic amyloidosis by a prion-like mechanism. Proc Natl Acad Sci U S A 99:6979–6984
Malle E, Sodin-Semrl S, Kovacevic A (2009) Serum amyloid A: an acute-phase protein involved in tumour pathogenesis. Cell Mol Life Sci 66:9–26
Manning M, Colon W (2004) Structural basis of protein kinetic stability: resistance to sodium dodecyl sulfate suggests a central role for rigidity and a bias toward beta-sheet structure. Biochemistry 43:11248–11254
Martin DJ, Ramirez-Alvarado M (2011) Glycosaminoglycans promote fibril formation by amyloidogenic immunoglobulin light chains through a transient interaction. Biophys Chem 158:81–89
McAdam KP, Sipe JD (1976) Murine model for human secondary amyloidosis: genetic variability of the acute-phase serum protein SAA response to endotoxins and casein. J Exp Med 144:1121–1127
Meek RL, Hoffman JS, Benditt EP (1986) Amyloidogenesis. One serum amyloid A isotype is selectively removed from the circulation. J Exp Med 163:499–510
Meek RL, Urieli-Shoval S, Benditt EP (1994) Expression of apolipoprotein serum amyloid A mRNA in human atherosclerotic lesions and cultured vascular cells: implications for serum amyloid A function. Proc Natl Acad Sci U S A 91:3186–3190
Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E, Neuenschwander A, Abramowski D, Frey P, Jaton AL, Vigouret J-M, Paganetti P, Walsh DM, Mathews PM, Ghiso J, Staufenbiel M, Walker LC, Jucker M (2006) Exogenous induction of cerebral beta-amyloidogenesis is governed by agent and host. Science 313:1781–1784
Miyagi Y, Matsumura Y, Sagami H (2007) Human geranylgeranyl diphosphate synthase is an octamer in solution. J Biochem 142:377–381
Mutru O, Laakso M, Isomaki H, Koota K (1985) Ten year mortality and causes of death in patients with rheumatoid arthritis. Br Med J (Clin Res Ed) 290:1797–1799
Nakamura T, Higashi S, Tomoda K, Tsukano M, Baba S, Shono M (2006) Significance of SAA1.3 allele genotype in Japanese patients with amyloidosis secondary to rheumatoid arthritis. Rheumatology (Oxford) 45:43–49
Noborn F, Ancsin JB, Ubhayasekera W, Kisilevsky R, Li JP (2012) Heparan sulfate dissociates serum amyloid A (SAA) from acute-phase high-density lipoprotein, promoting SAA aggregation. J Biol Chem 287:25669–25677
Obici L, Merlini G (2012) AA amyloidosis: basic knowledge, unmet needs and future treatments. Swiss Med Wkly 142:w13580
Patel H, Bramall J, Waters H, De Beer MC, Woo P (1996) Expression of recombinant human serum amyloid A in mammalian cells and demonstration of the region necessary for high-density lipoprotein binding and amyloid fibril formation by site-directed mutagenesis. Biochem J 318(Pt 3):1041–1049
Patke S, Maheshwari R, Litt J, Srinivasan S, Aguilera JJ, Colon W, Kane RS (2012) Influence of the carboxy terminus of serum amyloid A on protein oligomerization, misfolding, and fibril formation. Biochemistry 51:3092–3099
Patke S, Srinivasan S, Maheshwari R, Srivastava SK, Aguilera JJ, Colon W, Kane RS (2013) Characterization of the oligomerization and aggregation of human serum amyloid a. PLoS One 8:e64974
Pellarin R, Schuetz P, Guarnera E, Caflisch A (2010) Amyloid fibril polymorphism is under kinetic control. J Am Chem Soc 132:14960–14970
Pepys MB (2006) Amyloidosis. Annu Rev Med 57:223–241
Rocken C, Shakespeare A (2002) Pathology, diagnosis and pathogenesis of AA amyloidosis. Virchows Arch 440:111–122
Seilheimer B, Bohrmann B, Bondolfi L, Muller F, Stuber D, Dobeli H (1997) The toxicity of the Alzheimer’s beta-amyloid peptide correlates with a distinct fiber morphology. J Struct Biol 119:59–71
Shiroo M, Kawahara E, Nakanishi I, Migita S (1987) Specific deposition of serum amyloid A protein 2 in the mouse. Scand J Immunol 26:709–716
Simms RW, Prout MN, Cohen AS (1994) The epidemiology of AL and AA amyloidosis. Baillieres Clin Rheumatol 8:627–634
Simons JP, Al-Shawi R, Ellmerich S, Speck I, Aslam S, Hutchinson WL, Mangione PP, Disterer P, Gilbertson JA, Hunt T, Millar DJ, Minogue S, Bodin K, Pepys MB, Hawkins PN (2013) Pathogenetic mechanisms of amyloid A amyloidosis. Proc Natl Acad Sci U S A 110:16115–16120
Sipe JD (1992) Amyloidosis. Annu Rev Biochem 61:947–975
Sipe J (1999) Revised nomenclature for serum amyloid A (SAA). Nomenclature committee of the international society of amyloidosis. Part 2. Amyloid 6:67–70
Sipe JD, Carreras I, Gonnerman WA, Cathcart ES, de Beer MC, de Beer FC (1993) Characterization of the inbred CE/J mouse strain as amyloid resistant. Am J Pathol 143:1480–1485
Skinner M, Shirahama T, Benson MD, Cohen AS (1977) Murine amyloid protein AA in casein-induced experimental amyloidosis. Lab Invest 36:420–427
Sletten K, Husby G (1974) The complete amino-acid sequence of non-immunoglobulin amyloid fibril protein AS in rheumatoid arthritis. Eur J Biochem 41:117–125
Snow AD, Bramson R, Mar H, Wight TN, Kisilevsky R (1991) A temporal and ultrastructural relationship between heparan sulfate proteoglycans and AA amyloid in experimental amyloidosis. J Histochem Cytochem 39:1321–1330
Solomon JP, Bourgault S, Powers ET, Kelly JW (2011) Heparin binds 8 kDa gelsolin cross-beta-sheet oligomers and accelerates amyloidogenesis by hastening fibril extension. Biochemistry 50:2486–2498
Srinivasan S, Patke S, Wang Y, Ye Z, Litt J, Srivastava SK, Lopez MM, Kurouski D, Lednev IK, Kane RS, Colon W (2013) Pathogenic serum amyloid A 1.1 shows a long oligomer-rich fibrillation lag phase contrary to the highly amyloidogenic non-pathogenic SAA2.2. J Biol Chem 288:2744–2755
Stefani M (2012) Structural features and cytotoxicity of amyloid oligomers: implications in Alzheimer’s disease and other diseases with amyloid deposits. Prog Neurobiol 99:226–245
Steinmetz A, Hocke G, Saile R, Puchois P, Fruchart JC (1989) Influence of serum amyloid A on cholesterol esterification in human plasma. Biochim Biophys Acta 1006:173–178
Tam SP, Flexman A, Hulme J, Kisilevsky R (2002) Promoting export of macrophage cholesterol: the physiological role of a major acute-phase protein, serum amyloid A 2.1. J Lipid Res 43:1410–1420
Tanaka M, Collins SR, Toyama BH, Weissman JS (2006) The physical basis of how prion conformations determine strain phenotypes. Nature 442:585–589
Urieli-Shoval S, Cohen P, Eisenberg S, Matzner Y (1998) Widespread expression of serum amyloid A in histologically normal human tissues. Predominant localization to the epithelium. J Histochem Cytochem 46:1377–1384
Urieli-Shoval S, Linke RP, Matzner Y (2000) Expression and function of serum amyloid A, a major acute-phase protein, in normal and disease states. Curr Opin Hematol 7:64–69
Uversky VN (2009) Intrinsic disorder in proteins associated with neurodegenerative diseases. Front Biosci 14:5188–5238
Uversky VN (2013) Unusual biophysics of intrinsically disordered proteins. Biochim Biophys Acta 1834:932–951
van der Hilst JC (2011) Recent insights into the pathogenesis of type AA amyloidosis. Sci World J 11:641–650
van der Westhuyzen DR, de Beer FC, Webb NR (2007) HDL cholesterol transport during inflammation. Curr Opin Lipidol 18:147–151
van Horssen J, Wesseling P, van den Heuvel LP, de Waal RM, Verbeek MM (2003) Heparan sulphate proteoglycans in Alzheimer’s disease and amyloid-related disorders. Lancet Neurol 2:482–492
Wang L, Colon W (2005) Urea-induced denaturation of apolipoprotein serum amyloid A reveals marginal stability of hexamer. Protein Sci 14:1811–1817
Wang L, Lashuel HA, Walz T, Colon W (2002) Murine apolipoprotein serum amyloid A in solution forms a hexamer containing a central channel. Proc Natl Acad Sci U S A 99:15947–15952
Wang L, Lashuel HA, Colon W (2005) From hexamer to amyloid: marginal stability of apolipoprotein SAA2.2 leads to in vitro fibril formation at physiological temperature. Amyloid 12:139–148
Wang Y, Srinivasan S, Ye Z, Javier Aguilera J, Lopez MM, Colon W (2011) Serum amyloid A 2.2 refolds into a octameric oligomer that slowly converts to a more stable hexamer. Biochem Biophys Res Commun 407:725–729
Wang B, Tan YX, Jia J, Digre A, Zhang X, Vlodavsky I, Li JP (2012) Accelerated resolution of AA amyloid in heparanase knockout mice is associated with matrix metalloproteases. PLoS One 7:e39899
Webb NR, de Beer MC, van der Westhuyzen DR, Kindy MS, Banka CL, Tsukamoto K, Rader DL, de Beer FC (1997) Adenoviral vector-mediated overexpression of serum amyloid A in apoA-I-deficient mice. J Lipid Res 38:1583–1590
Westermark GT, Sletten K, Westermark P (1989) Massive vascular AA-amyloidosis: a histologically and biochemically distinctive subtype of reactive systemic amyloidosis. Scand J Immunol 30:605–613
Westermark GT, Engstrom U, Westermark P (1992) The N-terminal segment of protein AA determines its fibrillogenic property. Biochem Biophys Res Commun 182:27–33
Westermark P, Lundmark K, Westermark GT (2009) Fibrils from designed non-amyloid-related synthetic peptides induce AA-amyloidosis during inflammation in an animal model. PLoS One 4:e6041
Westermark GT, Fandrich M, Westermark P (2015) AA amyloidosis: pathogenesis and targeted therapy. Annu Rev Pathol 10:321–344
Woldemeskel M (2012) A concise review of amyloidosis in animals. Vet Med Int 2012:427296
Yamada T, Kluve-Beckerman B, Liepnieks JJ, Benson MD (1995) In vitro degradation of serum amyloid A by cathepsin D and other acid proteases: possible protection against amyloid fibril formation. Scand J Immunol 41:570–574
Ye Z, Bayron Poueymiroy D, Aguilera JJ, Srinivasan S, Wang Y, Serpell LC, Colon W (2011) Inflammation protein SAA2.2 spontaneously forms marginally stable amyloid fibrils at physiological temperature. Biochemistry 50:9184–9191
Zhang X, Li JP (2010) Heparan sulfate proteoglycans in amyloidosis. Prog Mol Biol Transl Sci 93:309–334
Zhang B, Une Y, Fu X, Yan J, Ge F, Yao J, Sawashita J, Mori M, Tomozawa H, Kametani F, Higuchi K (2008) Fecal transmission of AA amyloidosis in the cheetah contributes to high incidence of disease. Proc Natl Acad Sci U S A 105:7263–7268
Acknowledgments
Much of the work was supported by a National Institutes of Health Grant (R01 AG028158) to W.C. The authors are grateful to Ms. Jayeeta Sen for creating Fig. 5.2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Colón, W., Aguilera, J.J., Srinivasan, S. (2015). Intrinsic Stability, Oligomerization, and Amyloidogenicity of HDL-Free Serum Amyloid A. In: Gursky, O. (eds) Lipids in Protein Misfolding. Advances in Experimental Medicine and Biology, vol 855. Springer, Cham. https://doi.org/10.1007/978-3-319-17344-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-17344-3_5
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17343-6
Online ISBN: 978-3-319-17344-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)