Abstract
Persons suffering from schizophrenia present cognitive impairments that have a major functional impact on their lives. Particularly, executive functions and episodic memory are consistently found to be impaired. Neuroimaging allows the investigation of affected areas of the brain associated with these impairments and, moreover, the detection of brain functioning improvements after cognitive remediation interventions. For instance, executive function impairments have been associated with prefrontal cortex volume and thickness; cognitive control impairments are correlated with an increased activation in the anterior cingulate cortex, and episodic memory impairments are linked to hippocampal reduction. Some findings suggest the presence of brain compensatory mechanisms in schizophrenia, e.g. recruiting broader cortical areas to perform identical tasks. Similarly, neuroimaging studies of cognitive remediation in schizophrenia focus differentially on structural, functional and connectivity changes. Cognitive remediation improvements have been reported in two main areas: the prefrontal and thalamic regions. It has been suggested that those changes imply a functional reorganisation of neural networks, and cognitive remediation interventions might have a neuroprotective effect. Future studies should use multimodal neuroimaging procedures and more complex theoretical models to identify, confirm and clarify these and newer outcomes. This chapter highlights neuroimaging findings in anatomical and functional brain correlates of schizophrenia, as well as its application and potential use for identifying brain changes after cognitive remediation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
It has been widely emphasised that people suffering from schizophrenia show cognitive impairments in multiple areas [1,2,3] although those impairments might, according to some authors, be overestimated [4]. More precisely, executive functions, episodic memory and social cognition are consistently found to be impaired and are the favoured target for cognitive remediation [5, 6].
Interestingly, these impairments are found in all disease stages, including the schizophrenia prodromal phase [7] and first episodes [8]. They are even found in children or adolescents who later will develop schizophrenia [9]. These impairments also are present to a certain extent in patient’s relatives, and some of them are thought to constitute an endophenotype of the disorder [10, 11]. However, they usually do not increase with disease duration [7, 12].
Cognitive impairments have an important functional impact on the daily life of patients, and antipsychotics drugs show little effect on them [13]. Consequently, a substantial body of literature has been developed on the neural correlates of these impairments, both from an anatomical and a functional point of view.
Furthermore, schizophrenia is characterised by multiple brain anomalies at many levels, structural and functional, and in terms of both activity and connectivity [14,15,16]. The majority of studies are based on differences in activation patterns although an increasing number of studies presenting data of cerebral connectivity are being published (see Canu et al. [17] for a review on connectivity).
The first part of this chapter is organised around cognitive functions frequently found to be impaired in patients suffering from schizophrenia, i.e. executive functions (working memory and cognitive control) and episodic memory. The latest neuroimaging studies about the anatomical and functional correlates of these impairments are presented. The second part of the chapter reviews the neuroimaging evidence of structural, functional and connectivity changes found in patients with schizophrenia after cognitive remediation psychotherapies.
6.2 Executive Functions
Executive functions are an umbrella expression that designate a group of abilities aiming at organising and controlling cognitive functions, behaviours and emotions. The cognitive part of executive functions refers to an ensemble of top-down processing recruited to perform efficiently a demanding and/or new task. Executive functions are mostly developed in human beings and enable us to efficiently face new situations [18]. They are composed of a large number of cognitive functions, such as working memory, planning, inhibition, flexibility and reasoning [19, 20]. These functions are difficult to disentangle as high-level executive functions involve many other lower-level executive functions, e.g. planning involves working memory, inhibition and flexibility.
Despite this clinical description, working memory is often studied apart from other executive functions, as it is also strongly linked to episodic memory [21].
6.2.1 Anatomical Data
Executive functions are known to be dependent on the prefrontal area [18, 22], and prefrontal volume and thickness are associated to executive performances in healthy participants [22].
In schizophrenia, performances at executive functioning tasks were found to be related to the volume of some part of the prefrontal cortex. Indeed, Bonilha et al. [23] found a significant correlation between flexibility measured by tests and volume of left dorsolateral prefrontal cortex (DLPFC). The relationship between volume and cognitive control abilities seems to be limited, although a study conducted by Frascarelli et al. [24] evidenced a decrease of volume with duration of illness in medial frontal gyrus but failed to link it to performance of flexibility tasks. Another frontal area, the left orbital inferior cortex, has been found to be linked to performances on the Stroop task [25]. Links between cognitive control and prefrontal cortex volume are limited to several regions. Working memory performances have also been linked to smaller hippocampal grey matter volume [25].
6.2.2 Functional Data
6.2.2.1 Working Memory
Working memory is one of the core cognitive impairments in schizophrenia. It frequently is found to be associated with inefficient engagement of the DLPFC [26]. This hypoactivation is correlated with performance, with a greater hypoactivation leading to poorer performances. However, some studies did not replicate these results and found no differences of activation or even hyperactivation of DLPFC [27]. This apparent lack of consistency could be explained by the variation of task difficulty. Indeed, it has been hypothesised that the activation follows an inverted U-shape function. Therefore, a small activation is needed for an easy task, but it increases with a high task demand. Nonetheless, when the task is too difficult, activation decreases. It is argued that patients suffering from schizophrenia show a shift of this function to the left. Therefore, when the task is relatively easy, they show a greater activation than healthy controls, whereas when the task is difficult, they show a hypoactivation as they have already reached their limit [21, 27, 28]. Kraguljac et al. [21], in a review of the literature, suggested that these findings could reflect a frontal-based, top-down, cognitive control impairment. This impairment would lead to compensatory strategies, and patients suffering from schizophrenia would show a wider pattern of activation, particularly in regions accounting for attention.
6.2.2.2 Cognitive Control
As cognitive control comprises several cognitive functions, it can be studied using different tasks. We first will focus on studies using the Wisconsin Card Sorting Test (WCST), one of the most used tasks to evaluate cognitive control. Patients must classify cards according to a criterion that they have to find by themselves. After a certain amount of correct trials, the criterion changes, and patients must find the new one. Using event-related, functional magnetic resonance imaging (fMRI), authors can compare cortical response after a positive feedback and a negative feedback, therefore aiming to study the effort of changing strategy (i.e. set-shifting). In healthy participants, the paradigm reveals a cortical-subcortical loop comprising the prefrontal and parietal cortices and basal ganglia [29]. When comparing healthy participants to patients with schizophrenia, Wilmsmeier et al. [30] found a more extensive activation network in patients compared to controls, although in their study, both groups performed equally. More specifically, they evidenced an increased response in both dorsal and rostral anterior cingulate cortex (ACC) in patients. According to the authors, the increased activation in dorsal ACC reflects a stronger cognitive effort to shift, whereas rostral ACC overactivation reflects a stronger emotional response to negative feedback. Other studies, however, evidenced that rostral overactivation in patients with schizophrenia in these conditions was associated with better performances and learning abilities, suggesting that rostral ACC might be involved in cognitive control [31].
Wilmsmeier et al. [30] found an overactivation in the insula, known to be related to unsuccessful inhibition of negative state. In addition, the inferior frontal gyrus (IFG), associated with set-shifting, and the bilateral caudate nucleus, which has been shown to play an important role in executive processing [29], were both overactivated in patients. Therefore, a negative feedback would generate a stronger and more distributed activation network in patients, reflecting enhanced cognitive effort to change strategy and obtain the same performances as healthy participants. In addition, it can also be speculated that disappointment might be more difficult to handle for patients.
Interestingly, no overactivation was found in healthy controls when compared to patients. These results suggest that patients show more activation both in terms of intensity and number of activated areas. That could suggest compensatory mechanisms at work, recruiting a broader cortical area to perform the same task.
As explained earlier, executive functioning is recruited by many tasks, and, although they all refer to the same concept, they might rely on slightly different processing and therefore different secondary neuronal correlates [32, 33]. To avoid this pitfall, Minzenberg et al. [34] performed a meta-analysis, comprising 41 studies, to investigate neural correlates of executive functions in schizophrenia using different paradigms (including go/no-go, mental arithmetic, n-back, Stroop test, WCST). Within-group results showed that healthy controls and patients with schizophrenia activated a similarly distributed cortical subcortical network. That network comprises DLPFC, ACC, ventrolateral prefrontal cortex (VLPFC), premotor cortex, lateral temporal cortical areas, parietal areas, cerebellum and thalamus. Significant co-occurrence of activation across studies was found among the DLPFC, ACC and mediodorsal thalamus. When comparing both groups, hypoactivation in patients was found in the DLPFC, VLPFC, dorsal ACC, occipital and parietal cortices and thalamus.
These results are interpreted in the context of models of cognitive control [18], suggesting that lateral PFC provides top-down control on other brain areas. ACC is known to monitor performance [32] and would modulate the engagement of DLPFC. Therefore, dysfunction of DLPFC in schizophrenia would lead to poor engagement of other brain regions related to a given task and explain poor executive performances. The results are in line with the Wilmsmeier et al. [30] study specifying that overactivation of the ACC could reflect a compensatory mechanism to increase the engagement of the DLPFC. That mechanism of compensation would help to control functioning in other brain regions and eventually to obtain similar performances as healthy controls.
6.3 Episodic Memory
Memory relies on three basic processes: encoding, storage and retrieval. Verbal memory evaluations therefore usually comprise an immediate recall accounting for encoding and a delayed recall accounting for storage and retrieval abilities. Verbal memory is frequently found to be impaired in schizophrenia, and the encoding phase is particularly difficult for patients. As this verbal declarative memory impairment is consistently found in patients and their relatives, it is sometimes considered as an endophenotype of schizophrenia [11].
6.3.1 Anatomical Data
In healthy populations, episodic memory is known to be highly dependent on hippocampus integrity [35]. Studies consistently find a reduction of hippocampus volume in patients suffering from schizophrenia [36, 37] and in their unaffected healthy relatives [25], compared to healthy controls. This reduction does not worsen during illness [36], and a large sample study investigating subcortical brain volumes in 15 centres across the world found that hippocampal atrophy was more important in a sample scaled with a proportion of unmedicated patients [37].
Links between cortical thickness and memory impairment were evaluated by Guimond et al. [38]. They investigated cortical thickness in regions known to be involved in episodic memory like the parahippocampal gyrus, frontal cortex and hippocampus in a group of patients showing low to mild memory impairment and in a group of patients showing moderate to severe memory impairment. The results showed a greater cortical thickness in the latter group of patients. Particularly, they were found to show a thinning in the left inferior frontal gyrus, left middle frontal gyrus and orbitofrontal cortex (OFC). The left parahippocampal gyrus was also thinner than in healthy control participants. They failed, however, to find any hippocampal atrophy.
A recent meta-analysis by Antoniades et al. [39] investigated the links between hippocampal volume reduction and functionality. Interestingly, verbal memory performances were found to be correlated with hippocampal volume. The authors showed that verbal learning and performances at delayed recall were associated with both right and left hippocampal volume in patients suffering from schizophrenia, whereas this correlation was not found in healthy controls. The volume of other subcortical structures, such as the amygdala and putamen, also was found to be linked to verbal memory performances although they were less systematically investigated.
6.3.2 Functional Data
Episodic memory functioning is considered to rely mainly on the medial temporal lobe (MTL) with contribution of the prefrontal cortex. In the prefrontal cortex, three regions are principally recruited: ACC, which is thought to support adjustment in cognitive controls; DLPFC, which is considered to process links between items; and VLPFC, supposed to be responsible for semantic processing of the item [40].
6.3.2.1 Prefrontal Implications
In patients suffering from schizophrenia, episodic memory impairment is usually accompanied by a lesser activation of the prefrontal cortex. Indeed, in a meta-analysis, Ragland et al. [40] evidenced that during encoding, patients suffering from schizophrenia showed a hypoactivation of the left frontopolar cortex, VLPFC and DLPFC. This suggests that the observed differences in performance between patients and healthy controls rely more on information monitoring than on pure memory processes. Indeed, these regions are involved in working memory processes, particularly for linking information with its context and with each other [41].
A second analysis was performed including only studies in which patients were given explicit strategies to improve encoding. The authors found a similar pattern of results, except for VLPFC hypoactivation which was not found. This suggests that when strategies are given to patients, the activation of the ventrolateral prefrontal cortex reaches the level of healthy controls, suggesting that patients are able, when initiated, to semantically process and link stimulus with context.
Ragland et al. [40] also performed an analysis accounting for performance differences in the retrieval phase. As for encoding, the differences in the pattern of activation in patients compared to control participants reflected more difficulty in task managing than in memory per se. It revealed hypoactivation in the DLPFC, right ACC, thalamus and cerebellum. The authors hypothesised—given that hypoactivation was found in structures involved in error monitoring, working memory, attention and mental flexibility—that people suffering from schizophrenia show difficulties in monitoring their responses, detecting their errors and adjusting their behaviour. Other evidences in favour of this hypothesis were found recently, suggesting that the VLPFC can be recruited by participants suffering from schizophrenia when explicit encoding strategies are recommended to them [42].
Surprisingly, Ragland et al. [40] found many differences in the prefrontal cortex and not in the MTL, as one could have hypothesised. That has one exception: the hyperactivation found in the right parahippocampal gyrus that might reflect a compensation mechanism. Differences in MTL activation are not systematic in the literature, and it seems that they can be determined by the method of data analysis used in each study. Indeed, studies using region of interest (ROI) analysis seem to find more often significant differences in activation between patients and control groups in the MTL [40, 43].
6.3.2.2 Medial Temporal Implications
Using this type of analysis, several studies found different significant patterns of activation of the hippocampal and parahippocampal areas in patients with schizophrenia during declarative memory tasks as compared to healthy controls [43, 44]. Indeed, when comparing successful encoding with fixation condition, it seems that the successful encoding of an item is characterised by a hyperactivation of the anterior hippocampus in patients as compared to healthy controls and unaffected relatives [44]. This overactivation might reflect an improved effort for patients to successfully encode a stimulus. This hypothesis was supported by the finding that the parietal superior areas also were overactivated. These regions are known to be linked to the hippocampus and involved in integrated perception processing and conscious organisation during encoding. Therefore, this activation pattern suggests that successful encoding of information is more effortful in patients and/or that information processing is longer.
As declarative memory impairment in schizophrenia might be an endophenotype of the disorder, the pattern of activation in the memory task in unaffected relatives was also investigated. Interestingly some anterior left hippocampal hypoactivation was found in both patients and relatives, when comparing successful encoding to unsuccessful encoding, suggesting that some part of irregular cerebral activity might be linked to genetic liability factors [44].
To conclude this section, it seems that verbal episodic memory impairment in schizophrenia relies on abnormal hippocampal volume and prefrontal hypoactivation. Prefrontal hypoactivation suggests that impairment of patients in monitoring information generates difficulties in encoding and retrieval. These difficulties might also be enhanced by a more effortful processing of stimuli.
6.4 Cognitive Remediation Therapies
Cognitive remediation is an evidence-based psychotherapy for schizophrenia aiming to remediate cognitive impairments. There are different programmes and formats, but all of them have in common some principles and methods. The Cognitive Remediation Expert Working group has proposed a definition of cognitive remediation, considering those principles common to all cognitive remediation approaches: a behavioural training intervention targeting cognitive impairment, including attention, memory, executive functions or metacognition, using scientific principles of learning with the ultimate goal of improving functional outcomes. Several studies have tested the outcomes of cognitive remediation in schizophrenia, and two meta-analyses have established its efficacy [45, 46]. Cognitive remediation is helpful for improving cognition as well as daily functioning, but the underlying neural mechanisms of this treatment are not fully understood.
To demonstrate the existence of brain functional changes, researchers have followed the simple strategy of scanning participants before and after the cognitive intervention. In both moments, the participants should be performing a cognitive task that facilitates the activation of the targeted brain areas. Initially, different studies followed a single-case or case-series methodology [47,48,49]. Those studies helped to demonstrate the possibility of detecting changes in brain functioning after cognitive remediation. The design of the studies was theoretically driven and based on the selection of a few regions of interest, mainly prefrontal areas. All of the studies showed positive effects after cognitive remediation in terms of frontal activation improvement, but some studies showed that some patients could not present any improvement [50]. Despite the obvious limitations of the single-case methodology, these sorts of studies could still be helpful in understanding intersubject variability. There are an important number of studies focusing on the effects of cognitive remediation with neuroimaging procedures (Table 6.1), and the majority of these are randomised and controlled trials.
6.4.1 Findings in Frontal Lobe
Mostly, the main preference of researchers has been testing the activation of the prefrontal areas. Consequently, these have relied on cognitive paradigms that are dependent on the activation of those areas such as the n-back, verbal fluency or relational learning tasks [51,52,53,54,55,56,57,58,59].
Thus, with the n-back task, some interesting results have been described. Wykes et al. [53] were the first authors to demonstrate the potentiality of cognitive remediation to improve brain functioning in a randomised and controlled trial. The improvements found in different areas of cognition were significantly related with an increase of activation of the inferior frontal gyrus. A number of researchers then conducted similar studies to replicate those findings. Haut et al. [54] found increases in the activation of the left DLPFC and the ACC. Edwards et al. [55] implicated more areas of improved activation, including the frontal, parietal, inferior frontal junction and visual cortex. Similar results were found by Bor et al. [56] involving the frontal gyrus, cingulate gyrus and inferior parietal cortex. Recently, Ramsay et al. [57] also found increases in left lateral prefrontal activation during an n-back task. Subramanian et al. [58] used a different cognitive paradigm for scanning. They used a word generation and recognition task. After cognitive remediation, patients showed a significant improvement of the medial prefrontal activation pattern. It is interesting to highlight a tendency toward the normalisation of the prefrontal activation pattern although patients still showed poorer activation than healthy controls. Finally, Vianin et al. [59] reported increased activation after treatment in different areas including the parietal lobule, precentral gyrus, occipital cortex, middle cingulate cortex and superior parietal lobule, using a verbal fluency paradigm. Strikingly, the authors reported increased activation in Broca’s area, claiming that verbalisation might be the main factor underlying these brain changes.
In general, it seems to be proven that patients showed some increases in the activity of some parts of the frontal lobe after the cognitive remediation. These areas were mainly the left DLPFC, left DLPFC, anterior cingulate and right and left prefrontal cortex.
6.4.2 Findings in Connectivity and Brain Functioning
It has been suggested, however, that high levels of activation should not necessarily be considered an indicator of better brain functioning. A decrease in activation in some brain areas could be correlated with better cognitive performance in healthy people [27]. Penadés et al. [60] used the nback task and showed that two different networks, the central executive network and the default mode network, were overactive when compared to the healthy participants despite the finding that their task performances are similar. Interestingly, decreased activation was found in both networks after treatment. In healthy people, the default-mode network has been proven to be anti-correlated with the other networks, but in schizophrenia, this always remains overactive. Particularly interesting is the decreased activity in the default mode network after treatment. This could mean a better synchronisation in the activation of one network, the central executive network, and deactivation of the other, the default mode network. On the whole, the activation patterns after treatment were more similar to the patterns observed in healthy controls. Those findings could be interpreted as an improvement in the efficiency of both networks.
Recently, a number of researchers have begun focusing on new targets that come from new theoretical frameworks like brain networks theory. The use of the whole-brain approach has allowed focusing on the totality of brain regions and not only on the frontal lobes. Connectivity between different regions of the brain also is becoming the focus of new research [60,61,62]. Additionally, new methods of analysis of neuroimaging data enable us to test changes not only on taskrelated performance but also on restrelated brain functioning. Those innovative aspects are potentially constructing a more accurate picture of the effects that cognitive remediation may produce on brain functioning.
In this context, Penadés et al. [60] conducted a trial using a wholebrain approach that combined fMRI and diffusion tensor imaging (DTI). They investigated the effect of cognitive remediation on brain functioning, trying to test the potential changes on white matter fibres. The analysis of white matter on DTI showed an increase in the fractional anisotropy index after treatment for participants who received cognitive remediation. That increment was found in the anterior part of the genu of the corpus callosum, and it was correlated with cognitive gains. Although these findings need to be replicated, the authors speculated about the possibility that cognitive remediation could be improving connectivity between the two prefrontal hemispheres. The prefrontal cortex in both hemispheres is connected via the anterior part of the corpus callosum, and the whole system is an important element of the working memory system.
Eack et al. [62] conducted a pioneering research, testing the potential effects of cognitive remediation over brain connectivity. A longitudinal, randomised and controlled trial was carried out with 45 participants. These individuals were treated for 2 years with cognitive enhancement therapy (CET), which combines cognitive computer exercises on an individual basis and social cognitive exercises in group format. Functional MRI data was collected annually, and a resting-state functional analysis was performed. To test potential effects of cognitive remediation on frontotemporal connectivity, they used a seed-to-voxel general linear model. Statistical analyses showed that only participants who underwent CET showed two sorts of changes in connectivity. Firstly, connectivity loss between the resting network and the DLPFC was inferior for patients who followed the cognitive intervention. Secondly, connectivity with the insular cortex extending to the superior temporal gyrus significantly increased. Both networks seem to be related with problem-solving and emotional processing. The authors concluded that CET may improve brain connectivity, particularly between frontal and temporal regions.
To sum up, the findings of these studies suggest that cognitive remediation could be acting in different areas of the brain and not only in the areas of the frontal lobe. In any case, more brain activation is not always a suggestion of better brain functioning. Networks theory suggests that some brain areas, like the default mode network, are impaired in schizophrenia because they are overactive. For these reasons, not only activation of networks but also connectivity and synchronisation between them may become the focus of future studies.
6.4.3 Structural Findings
Eack et al. [63] published the first study trying to identify the effects of cognitive remediation in brain morphology. Using a voxel-based, morphometry methodology, they performed volumetric analysis in different regions of interest involving frontal and temporal regions. Participants were treated with the CET for 2 years, and the control group followed a supportive therapy for the same period. Noticeably, the analyses revealed some remarkable changes. Patients following cognitive intervention showed significant preservation of the grey matter in relation with the control group. The group with cognitive intervention showed less grey matter loss in fusiform gyrus and in the left parahippocampal region. Moreover, significant increases of grey matter were found in the left amygdala. All of these findings were statistically related with cognitive improvement after the cognitive intervention. The authors defended the possibility that cognitive remediation might have a protective effect on the brain in persons affected by schizophrenia.
Morimoto et al. [64] recently performed a randomised controlled study using a computer-assisted, cognitive remediation programme. They used a whole-brain, voxel-based, morphometric analysis to detect significant volume changes in cortical grey matter. Interestingly, patients who received the cognitive intervention showed statistically significant increases in right hippocampal volume. Changes in hippocampal volumes were positively correlated with verbal fluency improvements. The results suggest that cognitive remediation might be able to facilitate, hippocampal plasticity to some degree.
Finally, despite the incipient evidence for structural changes in the context of cognitive remediation, little is known about whether neuroimaging data can be used as a predictor of treatment response. This question was tested by Penadés et al. [65], who used baseline cortical thickness as a potential predictor of outcomes. The results suggested that baseline measures of cortical thickness in the frontal and temporal lobes are associated with responsiveness to cognitive remediation. In particular, improvement in non-verbal and verbal memory was associated with greater thickness in some areas of the frontal and temporal lobes at baseline. Significant differences were found in the left superior frontal, left caudal middle frontal, left precuneus and paracentral, superior frontal, right caudal middle frontal gyrus and pars opercularis. The results of this study need to be replicated, but they suggest that responsiveness to cognitive remediation may be dependent on the integrity of some brain structures located mainly in frontal and temporal lobes.
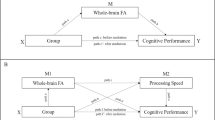
On the whole, structural studies suggest some detectable changes in the context of cognitive remediation. Some putative protective effects in the grey matter of the frontal and temporal lobes have been suggested. In addition, some sort of plasticity has been detected in the form of an increase of volume in the hippocampal region and in augmentation of white matter fibres at the corpus callosum. Finally, responsiveness to cognitive remediation may be related to the integrity of some brain areas in frontal and temporal lobes (Fig. 6.1).
Areas of the brain associated with cognitive remediation improvements in schizophrenia. For more detailed regions, direction of change and related studies, see Table 6.1. (a) Functional findings: areas that have shown activation changes. Bilateral and sagittal views of the brain. (b) Connectivity findings. Sagittal and superior coronal view of the brain. Arrows symbolise connectivity. (c) Structural findings: areas that have shown changes in terms of volume (grey and white matter). Inferior transverse views of the brain. All the figures are qualitative representations. ACC anterior cingulate cortex, DLPFC dorsolateral prefrontal cortex, B bilateral, L left, R right
6.5 Conclusion
Neuroimaging studies in recent years have shed some light on the topic of the neurobiological basis of cognitive function in schizophrenia. Thus, prefrontal cortex engagement appears to be a core characteristic in schizophrenia, although the results of studies investigating the neural correlates of cognition are far from consensus. Some authors suggest that some neurocognitive dysfunction could be seen as a consequence of prefrontal cortex dysfunction [40, 42]. Interestingly, cues for compensatory mechanisms are found in all the cognitive domains reviewed, suggesting that schizophrenic brains adapt their functioning to improve performance, although it is not fully efficient.
Also, neuroimaging studies of cognitive remediation in patients with schizophrenia have led to a better understanding of cognitive processes in schizophrenia. Cognitive remediation therapies have proven their proficiency to induce significant improvements on brain functioning. In particular, changes involving the prefrontal and thalamic regions are the most commonly reported results. These changes are being interpreted in terms of functional reorganisation of the neural networks. Moreover, structural changes in grey and white matter have also been described. These could be understood as the effects of neuroplasticity induced by the cognitive intervention. At the same time, these findings suggest a neuroprotective effect in response to cognitive remediation as they could be preventing, to some degree, grey matter loss. Obviously, more studies are required to confirm and clarify these results. As already suggested [5, 6], future studies should incorporate multimodal neuroimaging procedures, whole-brain analyses, brain networks theories, studies of connectivity, tractography and more complex theoretical models like graph theory.
References
Green MF, Nuechterlein KH, Gold JM, Barch DM, Cohen J, Essock S et al (2004) Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-MATRICS conference to select cognitive domains and test criteria. Biol Psychiatry 56(5):301–307
Heinrichs RW (2005) The primacy of cognition in schizophrenia. Am Psychol 60(3):229–242
Reichenberg A (2010) The assessment of neuropsychological functioning in schizophrenia. Dialogues Clin Neurosci 12:383–392
Moritz S, Klein JP, Desler T, Lill H, Gallinat J, Schneider BC (2017) Neurocognitive deficits in schizophrenia. Are we making mountains out of molehills? Psychol Med 47(15):2602–2612
Bon L, Franck N (2018) The impact of cognitive remediation on cerebral activity in schizophrenia: systematic review of the literature. Brain Behav 8(3):e00908. https://doi.org/10.1002/brb3.908
Penadés R, González-Rodríguez A, Catalán R, Segura B, Bernardo M, Junqué C (2017) Neuroimaging studies of cognitive remediation in schizophrenia: a systematic and critical review. World J Psychiatry 7(1):34–43
Bora E, Murray RM (2014) Meta-analysis of cognitive deficits in ultra-high risk to psychosis and first-episode psychosis: do the cognitive deficits progress over, or after, the onset of psychosis? Schizophr Bull 40(4):744–755
Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ (2009) Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology 23(3):315–336
Bilder RM, Reiter G, Bates J, Lencz T, Szeszko P, Goldman RS et al (2006) Cognitive development in schizophrenia: follow-back from the first episode. J Clin Exp Neuropsychol 28(2):270–282
Goghari VM (2011) Executive functioning-related brain abnormalities associated with the genetic liability for schizophrenia: an activation likelihood estimation meta-analysis. Psychol Med 41(6):1239–1252
Stone WS, Giuliano AJ, Tsuang MT, Braff DL, Cadenhead KS, Calkins ME et al (2011) Group and site differences on the California Verbal Learning Test in persons with schizophrenia and their first-degree relatives: findings from the Consortium on the Genetics of Schizophrenia (COGS). Schizophr Res 128(1–3):102–110
Ekerholm M, Firus Waltersson S, Fagerberg T, Söderman E, Terenius L, Agartz I et al (2012) Neurocognitive function in long-term treated schizophrenia: a five-year follow-up study. Psychiatry Res 200(2–3):144–152
Fett A-KJ, Viechtbauer W, Dominguez M-G, Penn DL, van Os J, Krabbendam L (2011) The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev 35(3):573–588
Howes OD, Kapur S (2009) The dopamine hypothesis of schizophrenia: Version III--The final common pathway. Schizophr Bull 35(3):549–562
Sugranyes G, Kyriakopoulos M, Dima D, O’Muircheartaigh J, Corrigall R, Pendelbury G et al (2012) Multimodal analyses identify linked functional and white matter abnormalities within the working memory network in schizophrenia. Schizophr Res 138(2–3):136–142
Unschuld PG, Buchholz AS, Varvaris M, van Zijl PCM, Ross CA, Pekar JJ et al (2014) Prefrontal brain network connectivity indicates degree of both schizophrenia risk and cognitive dysfunctions. Schizophr Bull 40(3):653–664
Canu E, Agosta F, Filippi M (2015) A selective review of structural connectivity abnormalities of schizophrenic patients at different stages of the disease. Schizophr Res 161(1):19–28
Miller EK, Cohen JD (2001) An integrative theory of prefrontal cortex functions. Annu Rev Neurosci 24:167–202
Diamond A (2013) Executive functions. Annu Rev Psychol 64:135–168
Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD (2000) The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn Psychol 41(1):49–100
Kraguljac N, Srivastava A, Lahti A (2013) Memory deficits in schizophrenia: a selective review of functional magnetic resonance imaging (fMRI) studies. Behav Sci (Basel) 3(3):330–347
Yuan P, Raz N (2014) Prefrontal cortex and executive functions in healthy adults: a meta-analysis of structural neuroimaging studies. Neurosci Biobehav Rev 42:180–192
Bonilha L, Molnar C, Horner MD, Anderson B, Forster L, George MS et al (2008) Neurocognitive deficits and prefrontal cortical atrophy in patients with schizophrenia. Schizophr Res 101(1–3):142–151
Frascarelli M, Tognin S, Mirigliani A, Parente F, Buzzanca A, Torti MC et al (2015) Medial frontal gyrus alterations in schizophrenia: relationship with duration of illness and executive dysfunctions. Psychiatry Res Neuroimaging 231(2):103–110
Guo X, Li J, Wang J, Fan X, Hu M, Shen Y et al (2014) Hippocampal and orbital inferior frontal gray matter volume abnormalities and cognitive deficit in treatment-naive, first-episode patients with schizophrenia. Schizophr Res 152(2–3):339–343
Glahn DC, Ragland JD, Abramoff A, Barrett J, Laird AR, Bearden CE et al (2005) Beyond hypofrontality: a quantitative meta-analysis of functional neuroimaging studies of working memory in schizophrenia. Hum Brain Mapp 25(1):60–69
Callicott JH, Mattay VS, Verchinski BA, Marenco S, Egan MF, Weinberger DR (2003) Complexity of prefrontal cortical dysfunction in schizophrenia: more than up or down. Am J Psychiatry 160(12):2209–2215
Barbalat G, Chambon V, Domenech PJD, Ody C, Koechlin E, Franck N et al (2011) Impaired hierarchical control within the lateral prefrontal cortex in schizophrenia. Biol Psychiatry 70(1):73–80
Monchi O, Petrides M, Petre V, Worsley K, Dagher A (2001) Wisconsin card sorting revisited: distinct neural circuits participating in different stages of the task identified by event-related functional magnetic resonance imaging. J Neurosci 21(19):7733–7741
Wilmsmeier A, Ohrmann P, Suslow T, Siegmund A, Koelkebeck K, Rothermundt M et al (2010) Neural correlates of set-shifting: decomposing executive functions in schizophrenia. J Psychiatry Neurosci 35(5):321–329
Pedersen A, Wilmsmeier A, Wiedl KH, Bauer J, Kueppers K, Koelkebeck K et al (2012) Anterior cingulate cortex activation is related to learning potential on the WCST in schizophrenia patients. Brain Cogn 79(3):245–251
Carter CS, MacDonald AW, Ross LL, Stenger VA (2001) Anterior cingulate cortex activity and impaired self-monitoring of performance in patients with schizophrenia: an event-related fMRI study. Am J Psychiatry 158(9):1423–1428
MacDonald AW, Carter CS, Kerns JG, Ursu S, Barch DM, Holmes AJ et al (2005) Specificity of prefrontal dysfunction and context processing deficits to schizophrenia in never-medicated patients with first-episode psychosis. Am J Psychiatry 162(3):475–484
Minzenberg MJ, Laird AR, Thelen S, Carter CS, Glahn DC (2009) Meta-analysis of 41 functional neuroimaging studies of executive function in schizophrenia. Arch Gen Psychiatry 66(8):811–822
Van Petten C (2004) Relationship between hippocampal volume and memory ability in healthy individuals across the lifespan: review and meta-analysis. Neuropsychologia 42(10):1394–1413
Adriano F, Caltagirone C, Spalletta G (2012) Hippocampal volume reduction in first-episode and chronic schizophrenia: a review and meta-analysis. Neuroscientist 18(2):180–200
van Erp TG, Hibar DP, Rasmussen JM, Glahn DC, Pearlson GD, Andreassen OA et al (2016) Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Mol Psychiatry 21(4):547–553
Guimond S, Chakravarty MM, Bergeron-Gagnon L, Patel R, Lepage M (2016) Verbal memory impairments in schizophrenia associated with cortical thinning. NeuroImage Clin 11:20–29
Antoniades M, Schoeler T, Radua J, Valli I, Allen P, Kempton MJ et al (2018) Verbal learning and hippocampal dysfunction in schizophrenia: a meta-analysis. Neurosci Biobehav Rev 86:166–175
Ragland JD, Laird AR, Ranganath C, Blumenfeld RS, Gonzales SM, Glahn DC (2009) Prefrontal activation deficits during episodic memory in schizophrenia. Am J Psychiatry 166(8):863–874
Murray LJ, Ranganath C (2007) The dorsolateral prefrontal cortex contributes to successful relational memory encoding. J Neurosci 27(20):5515–5522
Ragland JD, Ranganath C, Phillips J, Boudewyn MA, Kring AM, Lesh TA et al (2015) Cognitive control of episodic memory in schizophrenia: differential role of dorsolateral and ventrolateral prefrontal cortex. Front Hum Neurosci 9:604. https://doi.org/10.3389/fnhum.2015.00604
Achim AM, Lepage M (2005) Episodic memory-related activation in schizophrenia: meta-analysis. Br J Psychiatry 187:500–509
Pirnia T, Woods RP, Hamilton LS, Lyden H, Joshi SH, Asarnow RF et al (2015) Hippocampal dysfunction during declarative memory encoding in schizophrenia and effects of genetic liability. Schizophr Res 161(2–3):357–366
McGurk SR, Twamley EW, Sitzer DI, McHugo GJ, Mueser KT (2007) A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry 164(12):1791–1802
Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P (2011) A metaanalysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry 168(5):472–485
Wykes T (1998) What are we changing with neurocognitive rehabilitation? Illustrations from two single cases of changes in neuropsychological performance and brain systems as measured by SPECT. Schizophr Res 34(1–2):77–86
Wexler BE, Anderson M, Fulbright RK, Gore JC (2000) Preliminary evidence of improved verbal working memory performance and normalization of task-related frontal lobe activation in schizophrenia following cognitive exercises. Am J Psychiatry 157(10):1694–1697
Penadés R, Boget T, Lomeña F, Mateos JJ, Catalán R, Gastó C et al (2002) Could the hypofrontality pattern in schizophrenia be modified through neuropsychological rehabilitation? Acta Psychiatr Scand 105(3):202–208
Penadés R, Boget T, Lomeña F, Bernardo M, Mateos JJ, Laterza C et al (2000) Brain perfusion and neuropsychological changes in schizophrenic patients after cognitive rehabilitation. Psychiatry Res 98(2):127–132
Rowland LM, Griego JA, Spieker EA, Cortes CR, Holcomb HH (2010) Neural changes associated with relational learning in schizophrenia. Schizophr Bull 36(3):496–503
Subramaniam K, Luks TL, Fisher M, Simpson GV, Nagarajan S, Vinogradov S (2012) Computerized cognitive training restores neural activity within the reality monitoring network in schizophrenia. Neuron 73(4):842–583
Wykes T, Brammer M, Mellers J, Bray P, Reeder C, Williams C et al (2002) Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia. Br J Psychiatry 181:144–152
Haut KM, Lim KO, MacDonald A (2010) Prefrontal cortical changes following cognitive training in patients with chronic schizophrenia: effects of practice, generalization, and specificity. Neuropsychopharmacology 35(9):1850–1859
Edwards BG, Barch DM, Braver TS (2010) Improving prefrontal cortex function in schizophrenia through focused training of cognitive control. Front Hum Neurosci 4:32. https://doi.org/10.3389/fnhum.2010.00032
Bor J, Brunelin J, d’Amato T, Costes N, Suaud-Chagny MF, Saoud M et al (2011) How can cognitive remediation therapy modulate brain activations in schizophrenia? An fMRI study. Psychiatry Res 192(3):160–166
Ramsay IS, Nienow TM, Marggraf MP, MacDonald AW (2017) Neuroplastic changes in patients with schizophrenia undergoing cognitive remediation: triple-blind trial. Br J Psychiatry 210(3):216–222
Subramaniam K, Luks TL, Garrett C, Chung C, Fisher M, Nagarajan S et al (2014) Intensive cognitive training in schizophrenia enhances working memory and associated prefrontal cortical efficiency in a manner that drives long-term functional gains. NeuroImage 99:281–292
Vianin P, Urben S, Magistretti P, Marquet P, Fornari E, Jaugey L (2014) Increased activation in Broca’s area after cognitive remediation in schizophrenia. Psychiatry Res 221(3):204–209
Penadés R, Pujol N, Catalán R, Massana G, Rametti G, García-Rizo C et al (2013) Brain effects of cognitive remediation therapy in schizophrenia: a structural and functional neuroimaging study. Biol Psychiatry 73(10):1015–1023
Keshavan MS, Eack SM, Prasad KM, Haller CS, Cho RY (2016) Longitudinal functional brain imaging study in early course schizophrenia before and after cognitive enhancement therapy. NeuroImage 151:55–64
Eack SM, Newhill CE, Keshavan MS (2016) Cognitive enhancement therapy improves resting-state functional connectivity in early course schizophrenia. J Soc Social Work Res 7(2):211–230
Eack SM, Hogarty GE, Cho RY, Prasad KM, Greenwald DP, Hogarty SS et al (2010) Neuroprotective effects of cognitive enhancement therapy against gray matter loss in early schizophrenia: results from a 2-year randomized controlled trial. Arch Gen Psychiatry 67(7):674–682
Morimoto T, Matsuda Y, Matsuoka K, Yasuno F, Ikebuchi E, Kameda H et al (2018) Computer-assisted cognitive remediation therapy increases hippocampal volume in patients with schizophrenia: a randomized controlled trial. BMC Psychiatry 18(1):83. doi: 10.1186/s12888-018-1667-1
Penadés R, Pujol N, Catalan R, Masana G, Garcia-Rizo C, Bargallo N et al (2016) Cortical thickness in regions of frontal and temporal lobes is associated with responsiveness to cognitive remediation therapy in schizophrenia. Schizophr Res 171(1–3):110–116
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Penadés, R., Franck, N., González-Vallespí, L., Dekerle, M. (2019). Neuroimaging Studies of Cognitive Function in Schizophrenia. In: Guest, P. (eds) Reviews on Biomarker Studies in Psychiatric and Neurodegenerative Disorders. Advances in Experimental Medicine and Biology(), vol 1118. Springer, Cham. https://doi.org/10.1007/978-3-030-05542-4_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-05542-4_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-05541-7
Online ISBN: 978-3-030-05542-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)