Abstract
The impact acceleration (I/A) model of traumatic brain injury (TBI) was developed to reliably induce diffuse traumatic axonal injury in rats in the absence of skull fractures and parenchymal focal lesions. This model replicates a pathophysiology that is commonly observed in humans with diffuse axonal injury (DAI) caused by acceleration–deceleration forces. Such injuries are typical consequences of motor vehicle accidents and falls, which do not necessarily require a direct impact to the closed skull. There are several desirable characteristics of the I/A model, including the extensive axonal injury produced in the absence of a focal contusion, the suitability for secondary insult modeling, and the adaptability for mild/moderate injury through alteration of height and/or weight. Furthermore, the trauma device is inexpensive and readily manufactured in any laboratory, and the induction of injury is rapid (~45 min per animal from weighing to post-injury recovery) allowing multiple animal experiments per day. In this chapter, we describe in detail the methodology and materials required to produce the rat model of I/A in the laboratory. We also review current adaptations to the model to alter injury severity, discuss frequent complications and technical issues encountered using this model, and provide recommendations to ensure technically sound injury induction.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
1 Introduction
The rodent I/A model was designed by Marmarou and co-workers in 1994 to replicate the characteristics of DAI, a pathology commonly observed in humans following diffuse brain trauma [1]. The I/A model (also commonly known as the Marmarou model) has been adopted by laboratories around the world, generating more than 150 publications in just over 20 years. Together with the midline fluid percussion injury model, it remains one of the most validated experimental paradigms to study the diffuse traumatic axonal pathology (TAI, the experimental counterpart of human DAI ) intrinsic to diffuse brain trauma. The I/A model is also one of the few models of TBI resulting in post-traumatic apnea in rodents, thus faithfully reproducing an immediate post-traumatic loss of consciousness of TBI. The model is scalable to produce multiple injury severities; it is suited to the addition of secondary insults (e.g. hypoxia ); and compatible with a number of quantifiable behavioral tests ranging from motor, sensorimotor, and cognitive/memory function to determine the extent of initial neurological deficits, ongoing recovery post-trauma, and therapeutic efficacy on functional outcome.
The I/A model is produced using a weight-drop device consisting of a cylindrical brass weight of 250–450 g that falls through a Plexiglas tube from 1 to 2 m in height. The falling weight impacts a stainless steel disk that is fixed to the rat skull prior to trauma with dental acrylic, while the animal lies prone on a foam cushion of known density (14 kg/m3). The steel disk prevents the skull from fracturing by distributing the impact force uniformly across the skull and into the brain. Following the impact of the weight, the head of the animal is accelerated into the foam pad, and then decelerated, mimicking the forces transferred to TBI patients during motor vehicle accidents (e.g. whiplash injury). When using the highest severity combination of a 450 g weight from 2 m, a velocity of 6.06 m/s is achieved, resulting in a brain acceleration of 900 G and a brain compression gradient of 0.28 mm [1]. This force translates into an immediate suppression of neurological reflexes and apnea [2], as well as widespread axonal injury with a specific target on the corpus callosum and brain stem. The severity of injury can be reduced by varying the falling weight (<450 g, commonly 250 g) or the fall height (1, 1.5 m).
The I/A model has been particularly useful in elucidating the pathology underlying DAI [3], and to characterize other cellular and molecular mechanisms leading to secondary brain damage, including BBB dysfunction, edema, inflammation, glial activation, blood leukocyte infiltration, and neuronal degeneration [4–9]. Furthermore, this model is useful to study the impact of secondary post-traumatic hypoxia in exacerbating neurological deficits caused by TAI [4, 10]. This combined insult model is of particular relevance in the clinical setting since post-traumatic hypoxia is known to double mortality and worsen outcomes after severe TBI [11].
Behavioral impairment has been widely reported after TAI in the rat, specifically in relation to neurological reflexes, beam walk, beam balance, inclined plane, forelimb placement, and the Rotarod [4, 12, 13]. These deficits have been shown to persist for at least 4 weeks post-trauma [4, 14], with the Rotarod being the most sensitive amongst the multiple motor assessments. Long-lasting cognitive changes and memory loss have also been reported, primarily using the Morris Water Maze [14].
2 Materials
2.1 Animals
This model was established using adult male Sprague–Dawley rats, with a weight range of 350–400 g. Rats of this strain and weight have provided consistent replication of outcome measures (see Note 1 ).
2.2 Trauma device
The components of the I/A device are described briefly below. For full description of parts and construction, refer to the original manuscript describing the model [1]. The I/A device consists of:
-
1.
Wood/metal base (77 × 60 × 2, width × length × height in cm).
-
2.
Wood/metal stand to support the tube (4.5 × 4.5 × 200, W × L × H in cm).
-
3.
Plexiglas tube (height of 220 cm, diameter of 2.5 cm) (see Note 2 ).
-
4.
Small U-shaped metal brace to provide external stability for the tube (2 × 2.5 × 230 cm).
-
5.
Roll of 100 % cotton twill tape, 12 mm wide (Medline, Mountainside Medical Equipment, Marcy, NY; see Note 3 ).
-
6.
Cylindrical brass column of desired weight (for 450 g: height of 25 cm, diameter of 1.59 cm; see Note 4 ).
2.3 Equipment
2.3.1 Anesthesia
Endotracheal intubation and mechanical ventilation are required to adequately anesthetize the rat. Control of ventilation is also advantageous where investigators wish to superimpose a secondary insult such as hypoxia (see Notes 5 – 7 ). For this setup, you will require:
-
1.
Small animal ventilator with pressure and volume control (Inspira ASVV, Harvard Apparatus, Holliston, MA).
-
2.
Isoflurane Anesthesia Machine with oxygen and nitrogen inputs capable of gas mixture (e.g. CDS 9000 small animal anesthesia machine, Smiths Medical, Dublin, OH).
-
3.
Oxygen (piped, or in a cylinder).
-
4.
Nitrogen (piped, or in a cylinder).
-
5.
Gas regulators (if using cylinders).
-
6.
4× lots of corrugated heavy-duty plastic tubing with collared ends, cut into lengths of: 64 cm, 2 × 58 cm, and 15 cm (222 mm diameter, Implox Healthcare, Adelaide, SA, Australia).
-
7.
1 large “Y” piece connector, plastic or metal (Implox Healthcare).
-
8.
1 small barbed “Y” piece connector, plastic (Implox Healthcare).
-
9.
1 male luer lock adapter (B. Braun, Bethlehem, PA).
-
10.
4× lots of clear PVC tubing cut into lengths of 60 cm and 3 × 40 cm (4 mm internal diameter, ANPROS, Bayswater, VIC, Australia).
-
11.
Surgical tape, to secure tubing in place.
-
12.
Induction chamber.
-
13.
Laryngoscope handle and blade (e.g. Harvard Apparatus, #586592, #596774).
-
14.
Intubation rack.
-
15.
16 G IV catheter for intubation, needle cut down approximately 2 cm and blunted (Introcan Safety® catheter, B. Braun, Bethlehem, PA).
-
16.
Yarn or suture, cut into 20 cm lengths to secure endotracheal catheter to snout.
2.3.2 Surgical Supplies and Instruments
-
1.
Clinical record sheets and surgery data sheets.
-
2.
Two heat pads (one for placement under the animal during surgery, the other for the recovery box) (e.g. Harvard Apparatus, #340925).
-
3.
Bench pads.
-
4.
Acetone (for glue removal).
-
5.
70 % alcohol.
-
6.
Local anesthetic (e.g. Lignocaine or Lidocaine).
-
7.
Povidone-iodine solution.
-
8.
Dental cement or Superglue.
-
9.
Cotton-tipped applicators.
-
10.
Gauze.
-
11.
Small animal clippers (e.g. Wahl cordless pocket pro, #9961-2801, Sterling, IL).
-
12.
Scalpel blade and holder.
-
13.
Hemostats (e.g. Aesculap, #MB893R, Center Valley, PA).
-
14.
Forceps (e.g. Aesculap #MB780R).
-
15.
Surgical scissors (e.g. Aesculap, #MB925R).
-
16.
Staples and stapler applicator or suture.
-
17.
Helmet: stainless steel disk, 10 mm in diameter and 2 mm in thickness (scored on one side if adhering using superglue; see Notes 8 and 9 ).
-
18.
Tape/hook and loop fastener.
-
19.
Foam (type E bed foam, density of 14 kg/m3 and stiffness of 2500 N/m, measuring 13 × 43 × 11.5 cm, Foam to Size, Ashland, VA; see Notes 10 and 11 ).
-
20.
Wooden or Plexiglass box, with the dimensions 14 × 44 × 11.5 cm (W × L × H).
-
21.
Step ladder (If unable to reach 2 m).
-
22.
Injury device (as described above).
-
23.
Warmed clean cage for animals to recover from surgery (recovery box).
-
24.
Sodium pentobarbital-based anesthetic (e.g. Lethabarb or Euthosolv) for animal euthanasia in the event of skull fracture.
3 Methods
Firstly, the rat should be weighed and inspected for any signs of sickness. If healthy and within the weight range, the rat can be included in the study.
3.1 Experimental Set Up
-
1.
Place the trauma device on a level floor close to where the surgical procedures will be undertaken, and put a stepladder on the side closest to the weight.
-
2.
Position anesthesia machine at the end of the surgical table (Fig. 1a). Connect oxygen and nitrogen sources to anesthetic device.
Fig. 1 Experimental set-up for impact acceleration traumatic axonal injury. (a) Set up anesthetic machine close to the surgical table, with tubing arranged as described to provide anesthesia to the induction chamber and ventilator. (b) Arrange the ventilator tubes so that anesthesia and gas are both passing through the ventilator to the rat. (c) The helmet should sit flat on the skull, and the rat should be placed prone on the foam mattress. Keep the male luer lock adapter hub from the ventilator (d) attached to the female endotracheal tube port until ready to induce trauma. (e) One researcher releases the weight after climbing the stepladder to reach it, while the other positions the rat beneath the device. (f) Surgical equipment should be kept close at hand
-
3.
Prepare tubing: One 64 cm corrugated tube with collared ends is required to deliver the anesthesia/gas mixture between the intubation chamber and the rat. Connect one end to the anesthesia machine, and attach the y-connector to the other (see Fig. 1a). Attach one of the 58 cm corrugated tubes and the 15 cm corrugated tube to each of the “y” arms of the y-connector.
-
(a)
Connect the 58 cm tube to the anesthetic induction chamber. To the smaller 15 cm tube, attach one 60 cm clear PVC tube using surgical tape, and connect this PVC tube to the ventilator “gas input” (Fig. 1d). Attach the remaining corrugated tube to the opposite end of the induction chamber to the input tube. This last corrugated tube is required for waste gas removal.
-
(a)
-
4.
Turn on gas inputs, and balance O2 and N2 to 22 %/78 % respectively, to achieve a “room-air” ventilation .
-
5.
Ensure the lid is closed on the induction chamber. Turn isoflurane to 5 % and allow anesthetic gas to mix and fill the chamber.
-
(a)
Check for leaks in tubing, which will be evident by strong odor and whistling noises. Turn isoflurane off until ready to commence anesthesia.
-
(a)
-
6.
Attach two of the 40 cm clear PVC tubes to the rodent ventilator to maintain anesthesia and gas delivery. These tubes are required for gas input and exhaust—connect them to the ventilator’s input/output attachments (Fig. 1b, d). Join the end of each PVC tube not attached to the ventilator to the “y” arms of the small barbed y connector. Attach the opposite end of the y connector to the luer lock adapter, with the male hub facing outwards. This will connect to the female catheter port once the rat is intubated.
-
7.
Adjust the settings on the ventilator to 80 breaths/min and 2.5 ml/breath.
-
8.
Place one heatpad near the ventilator and cover with a bench pad. Place all surgical equipment, saline, Betadine, lignocaine, superglue, etc. close at hand (Fig. 1f).
-
9.
Cut yarn into lengths of approximately 25 cm and tie tightly around catheter. These will be used to secure the catheter around the snout.
3.2 Anesthesia Induction
-
1.
Place rat in the anesthesia induction chamber and leave animal for 5–7 min, or until deep anesthesia is achieved. This is observed by slow, regular breathing, decreased muscle tone (“floppy” posture), and absence of a pedal withdrawal reflex.
-
2.
Once deep anesthesia has been achieved, remove rat and hang by teeth on intubation rack. Using forceps, move tongue to one side and insert laryngoscope. Visualize the vocal cords and gently insert the 16 G catheter between vocal cords and into the trachea. If placed correctly, the catheter should feel like passing over small corrugations. Place the rat in a supine position and attach the male hub from the ventilator to the female port of the catheter to check whether endotracheal intubation has been achieved. This is confirmed with the rib cage moving in slow rhythmic breaths synchronized to the ventilator movement. If expansion and contraction are seen in the abdomen, or breathing is out of time with the ventilator, it is likely that the tube has been placed in the esophagus. If this has occurred, remove the catheter and place the rat back in the intubation chamber before attempting re-catheterization (see Notes 12 and 13 ).
-
3.
Once endotracheal intubation has been achieved, tie the catheter firmly in place with the yarn, looping around the snout to ensure the catheter does not come loose or slip out.
-
4.
Turn the isoflurane concentration down to 2–3 % to maintain the rat under anesthesia, and turn the rat carefully into a prone position, adjusting the endotracheal catheter as you do so to prevent twisting.
3.3 Surgical Preparation
-
1.
Using clippers, shave the rat’s head.
-
2.
Place Betadine onto gauze and wipe shaved scalp.
-
3.
Inject a small amount of local anesthetic into scalp, wait 3–5 min.
-
4.
Check once again that pedal withdrawal reflex is absent. Using a scalpel, make a 1.5–2 cm incision in the scalp from a rostral to a caudal direction, starting above the level of the ears.
-
5.
Expose the skull by finely cutting the overlying periosteum with the scalpel in a crosshatch pattern out to the most lateral edges of the incision.
-
6.
Using gauze, apply gentle pressure to absorb any blood and dry the skull thoroughly.
-
7.
If using dental acrylic: mix the powder with the liquid and work into a wet paste. Apply about half a teaspoon evenly to the skull, and then place the steel disk (“helmet”) over the parietal bone midway between bregma and lambda, directly over the midline suture (see Note 14 ).
-
8.
If using superglue: Apply the superglue to the underside of the helmet, and then place the disk on the skull midway between bregma and lambda, directly over the midline suture (Fig. 1c; see Note 9 ).
-
9.
Allow the acrylic/glue to dry completely. Superglue will take approximately 3–5 min, while acrylic may take up to 10 min.
-
10.
While waiting, prepare the foam mattress. It should be placed snugly inside the wooden or Plexiglas box, so that the head support portion sits level with the top of the box, and the body support portion sits approximately 1 cm below the box. Have it close to the surgical bench so you are able to swiftly move the rat from bench to mattress (see Note 11 ).
-
11.
One person should monitor the mattress, whilst another transports the rat, supporting the head and neck as well as the body to ensure the endotracheal catheter stays in place. Put the rat onto the mattress and place it prone on the foam bed, ensuring the head is positioned straight so the disk is flat (Fig. 1c).
-
12.
Disconnect the rat from the ventilator and secure to the box using surgical or masking tape over the dorsal surface below the armpit, attaching it to either side of the box (Fig. 1c).
-
13.
Rapidly move the rat and the mattress underneath the trauma device, and align the rat so the weight will hit directly onto the middle of the steel helmet. While one person maintains the animal in position, the other should be ready to release the weight, climbing the stepladder if necessary (Fig. 1e).
-
14.
Induce injury by releasing the weight from the desired height through the Plexiglas tube. Ensure the rat is rapidly moved away from the device to avoid a “second-hit” of the rebounding weight.
-
15.
Rapidly reconnect the rat to mechanical ventilation and turn off anesthesia, so that rat is ventilated only with supporting room air.
-
16.
Remove helmet using hemostats and inspect for skull fracture, cleaning off any remaining blood with gauze (see Note 15 ).
-
17.
Suture or staple the scalp incision closed.
-
18.
Once showing signs of wakefulness (independent breathing, recovery of righting reflex ), wean the rat from mechanical ventilation . The time may be variable, though most rats should be awake 10–20 min after the impact. Place the rat in a warmed recovery box on a heatpad for 60 min and monitor for recovery.
4 Discussion
The I/A model originally described by Marmarou and colleagues in 1994 [1, 2] reliably recreates the pathophysiology of human DAI , including diffuse white matter damage , neurological and cognitive deficits , neuroinflammation, and neuronal damage and dysfunction [3, 5, 7, 10, 15, 16].
This model is advantageous in that it requires minimal material and is easily set up, with a low mortality rate provided rats are adequately ventilated after injury. Typically, animal numbers as low as 5 per treatment group are sufficient to reach statistical significance, minimizing the number of animals to be used. The wide range of histological and biochemical outcomes, as well as long-term behavioral and cognitive consequences of the I/A model make it particularly suitable for pharmacological intervention studies. Research thus far has focused largely on attenuation of axonal pathology directly through mitigation of the cysteine protease calpain, which causes axonal proteolysis [17, 18] or attenuation of mitochondrial dysfunction [19, 20], or indirectly via multifunctional therapies such as erythropoietin, which prevents early deleterious signaling cascades and subsequent edema formation and behavioral dysfunction [21–23].
However, the I/A model has several drawbacks, including difficulty in translation to other species such as mice due to variations in skull size and thickness, and a failure of the model to translate to immature rats, where the graded cognitive dysfunction seen in adult rats over differing height/weight combinations is absent. A severe injury of 100 g/2 m is sufficient to cause diffuse edema and early motor deficits in postnatal day 17 rats, lasting 3–4 days in the absence of cognitive deficit [24], which is only observed when this injury is performed with the “ultra severe” combination of 150 g/2 m [25, 26]. Few studies have examined the effect of I/A injury in aged rats, however one important factor that has been reproduced is persistent cognitive dysfunction, with decreased capacity for recovery when compared to young adult rats [27].
To achieve success with this I/A model, researchers must pay careful attention to the fine procedural details, which will largely dictate whether standardized reproducible injuries are achieved. For example, incorrect or multiple attempts at placing the endotracheal catheter will cause airway swelling and mucous buildup, which will compromise airway recovery when animals are extubated. However, careful and correct placement will eliminate this consequence. Placement of the steel disk on the rat’s skull is also of critical importance; if the disk is not adhered flat onto the skull, the impacting weight will strike the highest point, increasing the likelihood of unilateral damage and skull fracture. Cooperation between the researcher releasing the weight and the researcher below with the animal is also needed to reach agreement on the exact moment the weight is released, whereby the rat must be moved directly after the first hit of the weight and prior to the weight rebounding, while ensuring the rat is not moved prior to a full first hit of the weight. This timing of movement of the rat requires keen attention, and is likely the most important factor of success in the I/A model.
5 Notes
-
1.
The body weight of the rat is a strong determinant of outcome, with larger animals having little apnea and high survival rates even when non-ventilated, as opposed to smaller animals that frequently experience long apnea, higher incidence of skull fracture, and greater mortality. Using rats heavier than indicated (400 g) will also reduce the likelihood of significant axonal injury , and increase variability between rats, so it is important to maintain a consistent weight at trauma throughout the study group.
-
2.
The Plexiglas tube ought to be higher than 200 cm to enclose the weight prior to its release. Drill a hole at 1 or 2 m from the bottom of the Plexiglas tube and place a bolt through the hole to support the weight. The weight falls when the bolt is removed.
-
3.
Tie the weight securely using the twill tape or string and attach the opposite end to the supporting arms of the injury stand. Ensure excess tape is present to allow the weight to reach through to the Plexiglas tube without becoming taut. While twill tape could be substituted for another high-strength woven tape, the use of fishing wire is not advisable as it may lead to abrasion of the top of the Plexiglas tube over time.
-
4.
Reducing the height of the falling weight will minimize adverse events, with graded pathological response ranging from most severe at 2 m, to mildest when the weight is released from a height of 1 m [4, 28, 29]. Additionally, the weight may be adjusted rather than the height, with a graded response also produced, in which weights of 250–300 g from 2 m resulted in mild injury [30].
-
5.
Isoflurane is a transient inhalation anesthetic with advantages including rapid induction, titratable dose, and swift recovery. However, isoflurane may have adverse side effects to the researcher. The use of this anesthetic should be conducted in a well-ventilated room, with active scavenging systems. As for the animals, isoflurane anesthesia may also result in respiratory depression, and play a role in neuroprotection [31]. Barbiturates such as sodium pentobarbital and sodium thiopental are occasionally used in acute recording or monitoring studies in which rodents are not planned for recovery. This is due to long-lasting anesthesia without depression of cortical evoked responses. Barbiturates are administered via i.p. injection, eliminating the need for anesthesia machinery. However, barbiturates may cause respiratory depression, hypotension with decreased ICP, and elevated mortality if not administered at the correct dose.
-
6.
When originally described, the investigators assessed incidence of apnea and mortality in this model using rats with or without ventilation [1]. They found that while all rats experienced a period of apnea, unventilated rats had a mortality rate of 58.6 %, compared to those that were ventilated, having a mortality of 8.7 %. Aside from survival, ventilation has the added advantage of administering secondary post-traumatic insult such as hypoxia or hyperoxia, with gas concentrations readily adjusted.
-
7.
Additional (secondary) insults to TBI are commonplace clinically, where isolated brain injury is a rare occurrence. The most frequent insults are hypoxia and hypotension, which substantially worsen outcomes [11]. While hypoxia may occur inherently in this model due to apnea when rats are not ventilated, depth and duration of the insult cannot be controlled, and so administration of hypoxia can be achieved via exchange of normoxic gas (22 % O2/78 % N2) to a hypoxic state. Decreasing the oxygen to 12 % O2 (balance N2) in this model for 30 min reliably produces a severe hypoxic insult in which PO2 is reduced to approximately 40–50 mmHg [10, 32]. Hypoxia/ischemia may also be induced in this model via bilateral carotid artery occlusion after injury [33]. Additionally, this model produces a substantial hypertensive response, with mean arterial pressure significantly elevated above sham levels at least 45 min post-injury [10].
-
8.
The use of other steel materials for the helmet can lead to variations in the force transferred to the brain. It is not recommended to alter the material of the helmet within a study.
-
9.
Scoring allows for better adherence of the superglue to the helmet and reduces the risk of it moving during the impact. Placing the helmet in acetone between each animal may aide in removing superglue.
-
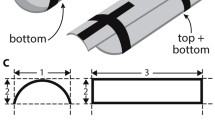
10.
The mattress height should be 11.5 cm in the first 15.5 cm of the mattress’ length to support the rats’ head, and then should be cut down 1 cm to be 10.5 cm for the remainder of the mattress length, to support the body.
-
11.
The density of the foam bed is critical and needs to be checked regularly to ensure consistency of results. From first use, the foam may soften up to 30 %, with a stress reduction of 5 % thereafter [34]. However, any stress reduction after first use is recoverable, with a recommended period of 1 h between uses ensuring proper foam recovery. There will also be a gradual loss with repeated use, so the foam will need regular replacement. As a guideline, the foam should be replaced after every 40–50 weight drops or 3 months.
-
12.
There are several options for rodent intubation, with the main difference being investigator preference. Proper lighting is essential to visualize the vocal cords, which can be achieved by tracheoscope or surgical lights. Rather than hanging the rat from the intubation rack, some prefer to use a bench top and align the animal to the edge of the counter. A string is placed over the front teeth and then attached to hemostats that are allowed to hang toward the floor. This technique opens the mouth and allows visualization of the vocal cords from another angle, with intubation proceeding as per the protocol for an intubation rack. The placement of an endotracheal catheter is multifold, including direct inflation of the lungs if apnea occurs, protection of the airway from fluids or secretions, and direct delivery of anesthetic.
-
13.
This procedure can be repeated a maximum of two times as swelling of the trachea can impair further intubation attempts and injure the animal.
-
14.
Make sure the cement is evenly distributed on the skull and no residues are left on its surface. Ensure that the helmet is placed in flat position. Given the requirement for a relatively flat dorsal skull surface, the model is difficult to use in any species other than rats. The helmet needs to be cleaned well after each experiment to ensure all glue is removed to allow maximal adherence in the next injury.
-
15.
If a skull fracture is noted, immediately euthanize the animal with sodium pentobarbital.
5.1 Conclusion
The I/A rat model of diffuse TBI replicates the unique pathophysiological consequences of human DAI , with a distinct experimental benefit of inducing apnea directly after injury. The I/A model has now been well characterized and utilized in more than 150 publications, with this model proving to be suitable for examination of both short- and long-term histopathological consequences as well as behavior and cognition. These factors, combined with the ease of use of the apparatus, make the I/A model a suitable choice for the experimental study of diffuse TBI, and a strong candidate to examine emerging neuroprotective strategies.
References
Marmarou A, Foda MA, van den Brink W, Campbell J, Kita H, Demetriadou K (1994) A new model of diffuse brain injury in rats. Part I: Pathophysiology and biomechanics. J Neurosurg 80:291–300
Foda MA, Marmarou A (1994) A new model of diffuse brain injury in rats. Part II: Morphological characterization. J Neurosurg 80:301–313
Povlishock JT, Marmarou A, McIntosh T, Trojanowski JQ, Moroi J (1997) Impact acceleration injury in the rat: evidence for focal axolemmal change and related neurofilament sidearm alteration. J Neuropathol Exp Neurol 56:347–359
Beaumont A, Marmarou A, Czigner A, Yamamoto M, Demetriadou K, Shirotani T, Marmarou C, Dunbar J (1999) The impact-acceleration model of head injury: injury severity predicts motor and cognitive performance after trauma. Neurol Res 21:742–754
Csuka E, Hans VH, Ammann E, Trentz O, Kossmann T, Morganti-Kossmann MC (2000) Cell activation and inflammatory response following traumatic axonal injury in the rat. Neuroreport 11:2587–2590
Donkin JJ, Nimmo AJ, Cernak I, Blumbergs PC, Vink R (2009) Substance P is associated with the development of brain edema and functional deficits after traumatic brain injury. J Cereb Blood Flow Metab 29:1388–1398
Hans VH, Kossmann T, Lenzlinger PM, Probstmeier R, Imhof HG, Trentz O, Morganti-Kossmann MC (1999) Experimental axonal injury triggers interleukin-6 mRNA, protein synthesis and release into cerebrospinal fluid. J Cereb Blood Flow Metab 19:184–194
Rancan M, Otto VI, Hans VH, Gerlach I, Jork R, Trentz O, Kossmann T, Morganti-Kossmann MC (2001) Upregulation of ICAM-1 and MCP-1 but not of MIP-2 and sensorimotor deficit in response to traumatic axonal injury in rats. J Neurosci Res 63:438–446
Stahel PF, Kossmann T, Morganti-Kossmann MC, Hans VH, Barnum SR (1997) Experimental diffuse axonal injury induces enhanced neuronal C5a receptor mRNA expression in rats. Brain Res Mol Brain Res 50:205–212
Hellewell SC, Yan EB, Agyapomaa DA, Bye N, Morganti-Kossmann MC (2010) Post-traumatic hypoxia exacerbates brain tissue damage: analysis of axonal injury and glial responses. J Neurotrauma 27:1997–2010
Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, Jane JA, Marmarou A, Foulkes MA (1993) The role of secondary brain injury in determining outcome from severe head injury. J Trauma 34:216–222
Heath DL, Vink R (1995) Impact acceleration-induced severe diffuse axonal injury in rats: characterization of phosphate metabolism and neurologic outcome. J Neurotrauma 12:1027–1034
Stibick DL, Feeney DM (2001) Enduring vulnerability to transient reinstatement of hemiplegia by prazosin after traumatic brain injury. J Neurotrauma 18:303–312
O’Connor C, Heath DL, Cernak I, Nimmo AJ, Vink R (2003) Effects of daily versus weekly testing and pre-training on the assessment of neurologic impairment following diffuse traumatic brain Injury in rats. J Neurotrauma 20:985–993
Nimmo AJ, Cernak I, Heath DL, Hu X, Bennett CJ, Vink R (2004) Neurogenic inflammation is associated with development of edema and functional deficits following traumatic brain injury in rats. Neuropeptides 38:40–47
Yan EB, Hellewell SC, Bellander BM, Agyapomaa DA, Morganti-Kossmann MC (2011) Post-traumatic hypoxia exacerbates neurological deficit, neuroinflammation and cerebral metabolism in rats with diffuse traumatic brain injury. J Neuroinflammation 8:147
Buki A, Farkas O, Doczi T, Povlishock JT (2003) Preinjury administration of the calpain inhibitor MDL-28170 attenuates traumatically induced axonal injury. J Neurotrauma 20:261–268
Saatman KE, Murai H, Bartus RT, Smith DH, Hayward NJ, Perri BR, McIntosh TK (1996) Calpain inhibitor AK295 attenuates motor and cognitive deficits following experimental brain injury in the rat. Proc Natl Acad Sci U S A 93:3428–3433
Buki A, Okonkwo DO, Povlishock JT (1999) Postinjury cyclosporin A administration limits axonal damage and disconnection in traumatic brain injury. J Neurotrauma 16:511–521
Okonkwo DO, Melon DE, Pellicane AJ, Mutlu LK, Rubin DG, Stone JR, Helm GA (2003) Dose-response of cyclosporin A in attenuating traumatic axonal injury in rat. Neuroreport 14:463–466
Bouzat P, Francony G, Thomas S, Valable S, Mauconduit F, Fevre MC, Barbier EL, Bernaudin M, Lahrech H, Payen JF (2011) Reduced brain edema and functional deficits after treatment of diffuse traumatic brain injury by carbamylated erythropoietin derivative. Crit Care Med 39:2099–2105
Valable S, Francony G, Bouzat P, Fevre MC, Mahious N, Bouet V, Farion R, Barbier E, Lahrech H, Remy C, Petit E, Segebarth C, Bernaudin M, Payen JF (2010) The impact of erythropoietin on short-term changes in phosphorylation of brain protein kinases in a rat model of traumatic brain injury. J Cereb Blood Flow Metab 30:361–369
Hellewell SC, Yan EB, Alwis DS, Bye N, Morganti-Kossmann MC (2013) Erythropoietin improves motor and cognitive deficit, axonal pathology, and neuroinflammation in a combined model of diffuse traumatic brain injury and hypoxia, in association with upregulation of the erythropoietin receptor. J Neuroinflammation 10:156
Adelson PD, Robichaud P, Hamilton RL, Kochanek PM (1996) A model of diffuse traumatic brain injury in the immature rat. J Neurosurg 85:877–884
Adelson PD, Dixon CE, Robichaud P, Kochanek PM (1997) Motor and cognitive functional deficits following diffuse traumatic brain injury in the immature rat. J Neurotrauma 14:99–108
Adelson PD, Jenkins LW, Hamilton RL, Robichaud P, Tran MP, Kochanek PM (2001) Histopathologic response of the immature rat to diffuse traumatic brain injury. J Neurotrauma 18:967–976
Maughan PH, Scholten KJ, Schmidt RH (2000) Recovery of water maze performance in aged versus young rats after brain injury with the impact acceleration model. J Neurotrauma 17:1141–1153
Kallakuri S, Cavanaugh JM, Ozaktay AC, Takebayashi T (2003) The effect of varying impact energy on diffuse axonal injury in the rat brain: a preliminary study. Exp Brain Res 148:419–424
Signoretti S, Di Pietro V, Vagnozzi R, Lazzarino G, Amorini AM, Belli A, D’Urso S, Tavazzi B (2010) Transient alterations of creatine, creatine phosphate, N-acetylaspartate and high-energy phosphates after mild traumatic brain injury in the rat. Mol Cell Biochem 333:269–277
Ucar T, Tanriover G, Gurer I, Onal MZ, Kazan S (2006) Modified experimental mild traumatic brain injury model. J Trauma 60:558–565
Statler KD, Alexander H, Vagni V, Holubkov R, Dixon CE, Clark RS, Jenkins L, Kochanek PM (2006) Isoflurane exerts neuroprotective actions at or near the time of severe traumatic brain injury. Brain Res 1076:216–224
Gao G, Oda Y, Wei EP, Povlishock JT (2010) The adverse pial arteriolar and axonal consequences of traumatic brain injury complicated by hypoxia and their therapeutic modulation with hypothermia in rat. J Cereb Blood Flow Metab 30:628–637
Stiefel MF, Tomita Y, Marmarou A (2005) Secondary ischemia impairing the restoration of ion homeostasis following traumatic brain injury. J Neurosurg 103:707–714
Zhang L, Gurao M, Yang KH, King AI (2011) Material characterization and computer model simulation of low density polyurethane foam used in a rodent traumatic brain injury model. J Neurosci Methods 198:93–98
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Hellewell, S.C., Ziebell, J.M., Lifshitz, J., Morganti-Kossmann, M.C. (2016). Impact Acceleration Model of Diffuse Traumatic Brain Injury. In: Kobeissy, F., Dixon, C., Hayes, R., Mondello, S. (eds) Injury Models of the Central Nervous System. Methods in Molecular Biology, vol 1462. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3816-2_15
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3816-2_15
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3814-8
Online ISBN: 978-1-4939-3816-2
eBook Packages: Springer Protocols