Abstract
β-d-glucan (Fungitell) and polymerase chain reaction-based (T2Candida) assays of blood samples are FDA-approved adjuncts to cultures for diagnosing candidemia and other types of invasive candidiasis, but their clinical roles are unclear. In this chapter, we describe laboratory protocols for performing Fungitell and T2Candida assays. We then discuss step-by-step methods for interpreting test results at the bedside using a Bayesian framework, and for incorporating assays into rational patient management strategies. Prior to interpreting results, clinicians must recognize that test performance varies based on the type of invasive candidiasis being diagnosed. In general, the type of invasive candidiasis that is most likely in a given patient can be identified, and the pretest likelihood of disease estimated. From there, positive and negative predictive values (PPV, NPV) for an assay can be calculated. At a population level, tests can be incorporated into screening strategies for antifungal treatment. NPV and PPV thresholds can be defined for discontinuing antifungal prophylaxis or initiating preemptive treatment, respectively. Using the thresholds, it is possible to assign windows of pretest likelihood for invasive candidiasis (and corresponding patient populations) in which tests are most likely to valuable. At the individual patient level, tests may be useful outside of the windows proposed for screening populations. The interpretive and clinical decision-making processes we discuss will be applicable to other diagnostic assays as they enter the clinic, and to existing assays as more data emerge from various populations.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
- Candidemia
- Invasive candidiasis
- Intra-abdominal candidiasis
- β-d-glucan
- Fungitell
- Polymerase chain reaction (PCR)
- T2Candida
- Diagnosis
- Bayesian
1 Introduction
The development of new diagnostic tests for candidemia and other forms of invasive candidiasis is among the top priorities in infectious diseases [1, 2]. Blood and deep tissue cultures, the gold standard tests, have sensitivity of only 50 %, turnaround times of several days, and turn positive late in the course of disease [1]. Tissue cultures are further limited by need for invasive sampling procedures, which are often dangerous and infeasible in patients at-risk for candidiasis. Non-culture diagnostics like β-d-glucan and polymerase chain reaction (PCR ) assays are directed against constituents of Candida cells rather than viable organisms [1]. At present, two assays of blood samples are approved by the U.S. Food and Drug Administration as adjuncts to cultures for the diagnosis of invasive candidiasis. The older and more widely employed test is the Fungitell serum β-d-glucan assay (Associates of Cape Cod, East Falmouth, MA), which is cleared for diagnosing a variety of invasive fungal infections. The assay does not provide Candida speciation nor distinguish between Candida, Aspergillus and certain other fungi. The more recently approved T2Candida assay (T2 Biosystems, Lexington, MA) uses a self-contained instrument to amplify detect Candida DNA within whole blood by PCR and T2 magnetic resonance, respectively. Used thoughtfully as adjuncts to cultures, these tests may identify more patients with invasive candidiasis, at earlier stages of disease. Despite growing literature on β-d-glucan and PCR-based assays, there is much confusion about test performance in the clinic, and how to interpret and best utilize results when caring for patients [3].
In this chapter, we describe methods for using Fungitell β-d-glucan and T2Candida assays in the laboratory and clinic. First, we provide detailed protocols for performing the assays (Subheadings 3.1 and 3.2). Then, we describe step-by-step methods for interpreting results at the bedside using a Bayesian framework (Subheadings 3.3 and 3.4), and for incorporating tests into rational patient management strategies (Subheadings 3.5 and 3.6). The interpretive and clinical decision-making processes that we describe will be applicable to other diagnostic assays as they enter clinical practice, and to existing assays as more data emerge from various patient populations. Our discussion focuses on candidemia and intra-abdominal candidiasis, the most common types of invasive candidiasis.
2 Materials
2.1 Fungitell Assay (See Note 1 )
2.1.1 Materials Supplied with the Kit (See Note 2 )
-
1.
Fungitell Reagent, a lyophilized (1,3)-β-d-Glucan specific Limiulus Amebocyte Lysate (LAL; two vials).
-
2.
Pyrosol Reconstitution Buffer, Tris–HCl 0.2 M pH 7.4 (two vials).
-
3.
Glucan standard (two vials).
-
4.
Reagent grade water (RGW) (two bottles).
-
5.
Flat-bottom, 96-well, uncoated microplates, with lids (two).
-
6.
KCl 1.2 M and KOH 0.25 M (one vial each).
2.1.2 Materials Not Supplied with the Kit (See Note 3 )
-
1.
Pipette tips* (250 μL) (see Note 4 ).
-
2.
Pipettors capable of delivering 5–25 μL and 100–1000 μL volumes.
-
3.
Stepper pipettor, with syringe tips, capable of delivering 100 μL.
-
4.
Test tubes* (13 × 100 mm borosilicate glass).
-
5.
Incubating (37 °C) plate reader capable of dual wavelength monitoring at 405 and 490 nm, with a dynamic range up to ≥2.0 Absorbance Units, coupled with appropriate computer-based kinetic assay software.
-
6.
Sterile, glucan-free, screw-cap storage tubes for aliquotting samples (most tubes that are certified to be RNAse, DNAse, and pyrogen-free are free of interfering levels of (1,3)-β-d-Glucan).
-
7.
Parafilm.
2.2 T2Candida Assay (See Note 5 )
2.2.1 Materials Supplied with the Kit
-
1.
T2Candida Panel, comprised of the T2Candida Cartridge and T2Candida Reagent Pack (see Note 6 ).
-
2.
T2Candida Cartridge includes T2Candida Base (calcium hypochlorite and lysis reagent comprised of a detergent mix and 0.09 % sodium azide in an aqueous buffer solution) and T2Candida Sample Inlets (12 single-use bases and inlets per box).
-
3.
T2Candida Reagent Pack includes internal control (aqueous buffered solution containing internal control DNA, carrier DNA and 0.09 % sodium azide preservative), reagent A (aqueous buffered solution containing dNTPs, Candida primers, and 0.09 % sodium azide preservative), enzyme solution (polymerase), Candida albicans / C. tropicalis particles, C. parapsilosis particles, C. krusei/C. glabrata particles, and Candida internal control particles (probe-coupled superparamagnetic particles that hybridize to amplicons of given spp. or internal control sequence, in an aqueous buffered solution containing 0.09 % sodium azide preservative).
2.2.2 Materials Not Supplied with the Kit
-
1.
T2Dx Instrument and Barcode Scanner (see Note 7 ).
-
2.
Bleach (household bleach at 5 % sodium hypochlorite, such as Clorox diluted 1:10), Bleach-Rite Disinfecting Spray or equivalent.
-
3.
70 % Isopropyl Alcohol.
-
4.
Powderless disposable gloves, lint-free wipes, absorbent pads.
-
5.
Distilled or deionized water.
-
6.
Biohazard waste bags.
-
7.
APG External Positive Control, TPK External Positive Control, Negative External Control (see Note 8 ).
3 Methods
3.1 Performing the Fungitell Assay
3.1.1 Sample Collection (See Note 9 )
-
1.
Collect serum samples in sterile vacuum tubes (red tops) or serum separator tubes (SST), and allow them to clot. Separate serum from clot and decant to a suitable container that is free of interfering levels of (1,3)-β-d-Glucan.
-
2.
Store serum samples at 2–8 °C before assay, or freeze at ≤−20 °C. Conduct testing promptly to minimize the possibility of sample degradation (see Note 10 ).
3.1.2 Testing Procedure (See Note 11 )
-
1.
Set plate reader software to collect data in the Vmean mode. Ensure proper settings such that the value calculated is the mean rate of optical density change for all data points gathered (see Note 12 ). The curve fit setting should be “linear/linear” or equivalent.
-
2.
Set the interval between reads to the minimum allowed over the 40 min test period.
-
3.
Set software wavelength as 405 nm minus the background at 490 nm. If dual wavelength reading is not available, read at 405 nm.
-
4.
Set incubation temperature at 37 °C.
-
5.
Shake the plate for 5–10 s prior to the start of reading. Perform reading without lag time.
-
6.
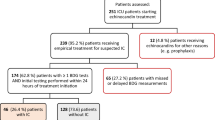
Plan the microtiter plate lay-out to include (in duplicate) standards (St; 25 μL/well), negative controls (Neg) and unknowns (Uk) (Fig. 1). Outside wells may be used if it has been demonstrated that performance is comparable to that of internal wells.
-
7.
Dissolve one vial of the Glucan standard with the volume of RGW stated on the vial, to make a 100 pg/mL solution. Vortex for at least 30 s to resuspend (creating solution 1). Store the glucan solution at 2–8 °C, and use within 3 days.
-
8.
Prepare a standard curve by first mixing 500 μL RGW and 500 μL of solution 1 in a glucan-free tube (solution 2; 50 pg/mL). Repeat dilution scheme through solution 5 (6.25 pg/mL). Vortex for at least 10 s between each step (see Note 13 ).
-
9.
Prepare the alkaline serum pretreatment reagent by combining equal volumes of 0.25 M KOH and 1.2 M KCl, and vortexing well. Recommended volumes are up to 900 μL of each reagent, permitting two preparations. Cover the vials with Parafilm for use with the second plate. Cover the vial with Parafilm using the side of the Parafilm that faced the paper backing.
-
10.
Add serum and pretreatment reagent to plates, after thawing and vortexing frozen serum samples at room temperature (see Note 14 ). Transfer 5 μL of each serum sample to the designated wells (labeled as Uk), and add 20 μL of the serum pretreatment reagent to each well containing serum (see Note 15 ). Agitate the plate for 5–10 s to mix well contents, and incubate for 10 min at 37 °C.
-
11.
While pretreatment incubation is in progress, reconstitute one vial of Fungitell reagent by adding 2.8 mL of RGW and 2.8 mL of Pyrosol Reconstitution buffer using the 1000 μL pipettor. Cover the vial with Parafilm using the side of Parafilm that faced the paper backing. Swirl the vial gently to dissolve completely—do not vortex.
-
12.
At the end of serum pretreatment incubation, remove the plate and add standards and negative controls to wells (25 μL).
-
13.
Use the stepper pipettor to add 100 μL of Fungitell reagent to each well containing negative controls, standards and samples, insert the plate into the microplate reader (equilibrated to 37 °C) with the lid on, and shake for 5–10 s.
-
14.
Read the plate without the lid at 405 nm minus 490 nm, for 40 min at 37 °C. If background subtraction (at 490 nm) is unavailable, read at 405 nm. If a plate shaking function is unavailable with the microplate reader, use an external microplate shaker.
-
15.
Collect data and analyze by examining optical density plots of test samples and checking for kinetic trace patterns other than a smooth increase comparable to those of standards. Invalidate plots indicating optical interference.
-
16.
Calculate the mean rate of optical density change (milli-absorbance units per minute) for all points between 0 and 40 min.
-
17.
Results (expressed in pg/mL of serum) range from non-detectable (<31 pg/mL) to >500 pg/mL, and are printed out by the software or read from the standard curve. Accurate values >500 pg/mL require that the sample be diluted in RGW and retested. Results are interpreted as follows: <60 pg/mL—negative; 60–79 pg/mL—possible infection, for which additional sampling and testing are recommended; ≥80 pg/mL—positive (see Note 16 ).
3.2 Performing the T2 Assay (See Note 17 )
3.2.1 Sample Collection
-
1.
Collect blood (≥3 mL) in 4 mL plastic Vacutainer plastic K2EDTA Venous Blood Collection Tubes 13 mm (lavender top), and invert eight to ten times to thoroughly mix with the anticoagulant (see Note 18 ).
-
2.
Store whole blood in the K2EDTA collection tube at 15–25 °C for no longer than 12 h before analysis. Specimens should be tested as soon as possible after collection. Specimens held for longer than 3 days at 2–8 °C may result in a decrease of viable organisms in the specimen. If stored at 2–8 °C, ensure that the sample has equilibrated to room temperature before analysis.
3.2.2 Work Area Preparation
-
1.
Wearing fresh gloves, spray Bleach-Rite (or equivalent) onto a new lint-free wipe. Wipe the prep area bench top in a unidirectional motion and discard the wipe.
-
2.
Using a new wipe for each, repeat the same procedure to clean the T2Dx Instrument touch screen, Barcode Scanner, drawer panel, and the bench top surrounding the T2Dx Instrument. Allow the bleach solution to sit for at least 3 min.
-
3.
Wearing fresh gloves, repeat cleaning procedure using 70 % isopropyl alcohol to wipe all surfaces. Should gloves become soiled during any of the steps of this procedure, remove and replace with a clean pair of gloves following standard lab procedures.
3.2.3 Testing Procedure (See Note 19 )
-
1.
Wearing fresh gloves, place a disposable absorbent pad on the work surface. Remove specimens or controls from storage and ensure that there is sufficient sample volume (≥3 mL) in the K2EDTA Vacutainer and that the specimen or control barcode is legible and undamaged. If there is any blood or fluid present on the exterior of the sample tube, clean the Vacutainer using standard lab practices.
-
2.
Wearing fresh gloves, obtain the required number of T2Candida Reagent Packs and T2Candida Cartridges from storage. Open the packaging without touching the inner contents. Since the outer packaging is considered potentially contaminated, do not remove from the package at this time (see Note 20 ).
-
3.
Wearing fresh gloves, take out one T2Candida Sample Inlet, one T2Candida Base and one T2Candida Reagent Pack and place them on the clean absorbent pad. Do not touch the outside of the packaging or the foil on top of the T2Candida Reagent Pack. Check the labels and barcodes for integrity.
-
4.
Holding the Reagent Pack on the sides and being careful not to touch the foil on top, briefly mix by agitating in a horizontal motion for 3–5 s. Visually inspect the contents to ensure all solutions are homogeneous. Gently tap on the bench top to displace any trapped air bubbles, and visually confirm that air bubbles are removed.
-
5.
Insert the T2Candida Reagent Pack onto the T2Candida Base using the orientation notch of the T2Candida Reagent Pack to assist in properly aligning the two components. While taking care to avoid the seal over the wells, push down on the T2Candida Reagent Pack at the site of the barcode until an audible snap-in sound is heard, indicating that the T2Candida Reagent Pack is fixed onto the T2Candida Base.
-
6.
Assure that the specimen is at room temperature (~20 min for refrigerated samples). Resuspend the patient sample in a capped blood collection tube by inverting the blood collection tube a minimum of eight to ten times. A blood specimen rocker may also be used to ensure sample homogeneity. Do not use the blood sample if the mixture is not homogenous after resuspension.
-
7.
Uncap the blood collection tube following standard laboratory procedures. Exercise care to not spill or aerosolize the sample. Dispose of cap as biohazard waste.
-
8.
Invert the T2Candida Sample Inlet and use it to re-cap the blood collection tube, using a push and twist motion to secure the blood collection tube. It is critical to ensure that a good seal has formed between the tube and the Sample Inlet blood collection tube seal (the soft portion of the inlet). Ensure that the blood collection tube is seated firmly in the Sample Inlet before proceeding to the next step.
-
9.
Invert the Sample Inlet assembly and blood collection tube and assure that the sample level in the blood collection tube drops as the blood transfers from the collection tube to the T2Candida Sample Inlet. If the blood collection tube’s liquid level does not drop after 1 min, invert back to the original position; ensure that there is at least 3 mL of specimen remaining in the blood collection tube and repeat step 8.
-
10.
Once it is verified that sample is flowing into the Sample Inlet, place the T2Candida Base on a flat surface and snap the T2Candida Sample Inlet onto it. Taking care to avoid contact with the foil seal, push the T2Candida Sample Inlet down until an audible snap-in sound is heard, indicating that the T2Candida Sample Inlet is correctly attached to the T2Candida Base. Do not place the assembled cartridge in front of the instrument to avoid accidental drops due to automated drawers.
-
11.
Wearing fresh gloves, press “Load” on the touch screen of the T2Dx Instrument.
-
12.
Using the Barcode Scanner on the T2Dx Instrument, scan the patient sample barcode, the T2Candida Reagent Tray barcode and the T2Candida Base barcode, according to the instrument prompts. When necessary, enter a unique sample identifier using the touch screen keyboard instead of scanning the blood collection tube barcode.
-
13.
The system will open an available drawer and prompt loading of the fully assembled T2Candida Cartridge with specimen into the T2Dx Instrument drawer. Ensure that the T2Candida Cartridge is level when seated in the drawer and fully in contact with the metal rails and the Location Pins.
-
14.
Once the cartridge is properly positioned in the T2Dx Instrument drawer, press “Next”. When prompted by the instrument to “Tear Off Label”, gently remove the top seal from the cartridge by pulling on the tab while holding down the cartridge assembly (see Note 21 ).
-
15.
Press “Confirm” on the T2Dx Instrument touch screen. The locking mechanism will engage to hold the T2Candida Cartridge in place and the drawer will close (see Note 22 ).
-
16.
The T2Dx Instrument automatically selects the next available drawer for use (1 through 7). Drawer 7 (orange STAT drawer) may be used at any time to process priority samples.
-
17.
After changing gloves, repeat steps 3–16 for each additional sample if there are available drawers in the T2Dx Instrument. The T2Dx touch screen “Drawer Status” display will indicate whether drawers are available.
-
18.
Once the sample is finished, the “Run Complete” indicator will appear on the display screen. All the used and unused disposables along with reagents, sample and liquid waste are contained in the T2Candida Cartridge.
-
19.
To remove the used T2Candida Cartridge from the T2Dx Instrument, put on a fresh pair of gloves and press “Unload” on the T2Dx Instrument touch screen. Follow the T2Dx Instrument prompts to open the drawer.
-
20.
With one hand inside a biohazard bag, remove the used T2Candida Cartridge from the T2Dx Instrument and pull the biohazard bag over the cartridge, as an additional precaution to limit the risk of inadvertent cross-contamination (see Note 23 ).
-
21.
Seal or tie up the bag, and then discard in a biohazardous waste receptacle. Dispose of gloves immediately into biohazard waste.
-
22.
Wearing fresh gloves, press “Next” twice more in the T2Dx Instrument touch screen and the drawer will close. Repeat for all other drawers that display a “Run Complete” indication, using a fresh pair of gloves for each cartridge.
-
23.
Each valid T2Candida Panel will yield three total results (Positive or Negative) for (1) C. albicans / C. tropicalis (A/T), (2) C. parapsilosis (P) and (3) C. glabrata/C. krusei (K/G) (Table 1). In addition, an Internal Control (IC) result (Valid or Invalid) will be reported (see Note 24 ).
Table 1 Interpretation of results as reported by T2Dx instrument
3.3 Prior to Interpreting Test Results: Understanding Invasive Candidiasis, Test Performance Characteristics, and Pretest Likelihoods of Invasive Candidiasis
-
1.
Recognize that invasive candidiasis comprises the distinct, but overlapping diseases of candidemia and deep-seated candidiasis (see Note 25 ).
-
2.
Understand the sensitivity and specificity of tests for diagnosing different types of invasive candidiasis (see Note 26 ).
-
3.
Assess the most likely type of invasive candidiasis in the patient being tested (Table 2) (see Note 27 ).
Table 2 Incidence of the most common types of invasive candidiasis in various populations -
4.
Estimate the pretest likelihood of invasive candidiasis in the patient being tested (Table 2) (see Note 28 ).
3.4 Interpreting Test Results at the Bedside: A Bayesian Framework
-
1.
Understand positive and negative predictive values (PPV, NPV) in various clinical settings (Table 3) (see Note 29 ).
Table 3 Performance of non-culture tests for invasive candidiasis in various populations -
2.
Understand the impact of blood culture results on the interpretation of non-culture test results (Table 3) (see Note 30 ).
-
3.
Calculate PPV and NPV of the result in the patient being tested (see Note 31 ).
3.5 Making Treatment Decisions: Using Non-culture Diagnostics as Screening Tools for Antifungal Treatment (See Note 32 )
-
1.
Understand a paradigm that uses non-culture diagnostics and blood cultures to guide prophylactic or preemptive antifungal treatment (Fig. 2) (see Note 33 ).
Fig. 2 Paradigm for incorporating non-culture tests into prophylactic or preemptive antifungal strategies against invasive candidiasis. Treatment decisions are made at two stages, in response to non-culture test results and non-culture results combined with blood cultures, respectively. The viability of the paradigm depends upon NPVs and PPVs at each stage. By applying data from Table 3, clinical settings in which non-culture test-driven strategies are likely to be useful can be identified (Table 4). Strategies such as these that use non-culture diagnostics to direct antifungal treatment require validation in clinical trials
-
2.
Define NPV and PPV thresholds to discontinue prophylaxis or initiate preemptive treatment (see Note 34 ).
-
3.
Assign windows of pretest likelihoods in which non-culture tests are most likely to be valuable in guiding antifungal therapy (Table 4) (see Note 35 ).
Table 4 Windows of pretest likelihoods in which non-culture tests are predicted to be useful in guiding antifungal treatment
3.6 Making Treatment Decisions: Using Non-culture Diagnostics in the Management of Individual Patients
-
1.
Understand that non-culture tests may be useful in the management of individual patients, even if performed outside of the windows proposed for screening populations (see Note 36 ).
4 Notes
-
1.
The reader is referred to highly detailed instructions provided with the Fungitell kit. Note that the assay detects fungi in addition to Candida spp. A positive result does not distinguish between fungi. Common medically relevant fungi that are not detected include Cryptococcus spp., Zygomycetes such as Rhizopus, Mucor and Absidia, and (in most instances) the yeast morphology of Blastomyces dermatitidis.
-
2.
Materials supplied with each kit are sufficient to assay 110 wells on two microtiter plates (55 wells on each). Store all reagents at 2–8 °C in the dark. Use reconstituted Fungitell within 2 h, or freeze at −20 °C for up to 20 days, thaw once and use.
-
3.
Glassware must be dry-heat depyrogenated at ≥235 °C for 7 h (or a validated equivalent) to be considered suitable for use. Glass pipettes with cotton plugs are a potential source of glucan contamination.
-
4.
Materials marked by asterisks are certified free of interfering glucans and available from Associates of Cape Cod, Inc.
-
5.
The reader is referred to highly detailed instructions provided with the T2Candida panel and T2Dx Instrument. Note that T2Candida results are reported for three spp. groups: (1) C. albicans / C. tropicalis ; (2) C. parapsilosis; and (3) C. glabrata/C. krusei. The assay is not quantitative, nor does it detect other Candida spp. or fungi.
-
6.
Store T2Candida Cartridge at 15–30 °C. Store T2Candida Reagent Packs at 2–8 °C.
-
7.
Assays can only be run with the T2Dx Instrument.
-
8.
Available from T2 Biosystems.
-
9.
Use powder-free gloves when handling patient specimens.
-
10.
Off-color or turbid samples such as those that are grossly hemolyzed, lipemic, or contain excessive bilirubin may cause interference. If such samples are tested, results should be examined for evidence of optical interference and/or unusual kinetic trace patterns.
-
11.
The Fungitell assay requires rigorous attention to technique and testing environment. The assay should be performed by personnel who are thoroughly trained in the methods and in the avoidance of contamination.
-
12.
Settings may vary with different instruments and software.
-
13.
When plotting the standard curve, multiply the concentration of the standards by five so that the range is from 500 to 31 pg/mL. Enter the standards into the software settings as 500, 250, 125, 62.5, and 31 pg/mL, respectively.
-
14.
To avoid accidental contamination when manipulating the plate, replace the cover after adding samples and reagents to the wells. Remove the cover before reading to avoid optical interference from condensation.
-
15.
The steps in this sentence can be conducted in reverse order.
-
16.
There are several quality control measures that should be assessed. (1) The correlation coefficient (r) of the standard curve should be >0.980. (2) Negative control wells (25 μL of RGW only) should have actual optical density rate (Vmean) values <50 % of the lowest standard. If values are not in this range, the assay should be repeated using all new reagents. (3) If optical density kinetics are unusual in testing a sample that is cloudy, off-color, or turbid, the sample must be diluted in RGW and retested. The dilution must be accounted for in the reporting of results by multiplying the result by the dilution factor. Typically, the dilution factor is entered in the software setup for the sample and the correction is automatically applied. (4) Control samples at cut-off and highly positive levels may be run to verify that reagents and the assay are performing properly. Each user of the test should establish a quality control program to assure proficiency in the performance of the test.
-
17.
The assay should only be processed by technicians who have been trained on use of the T2Candida Panel and the T2Dx Instrument.
-
18.
Blood should be collected using aseptic technique, similar to blood culture sample acquisition. A minimum blood specimen volume of 3 mL is required to assure optimal T2Candida Panel performance. Specimens should not be drawn from a central line or port through which antifungal therapy has been administered.
-
19.
As for any nucleic acid amplification technology, avoidance of contamination is crucial. Pay scrupulous attention to maintaining a clean environment, changing gloves as specified, etc.
-
20.
Excellent figures for steps throughout the procedure are provided in the T2Candida manual.
-
21.
Ensure that all tray components are present before proceeding.
-
22.
Watch the locking mechanism to ensure that it engages the T2Candida Cartridge as the drawer closes.
-
23.
Be careful when removing the used T2Candida Cartridge to avoid spillage of reagents, samples and disposables. Do not tip or invert the used T2Candida Cartridge. Ensure that the T2Candida Cartridge remains upright while unloading.
-
24.
If the Internal Control is invalid and the specimen result is reported as negative, “Invalid” will be displayed as the Internal Control result. In this case, repeat the T2Candida Panel from a different sample from the patient. T2 Biosystems provides positive and negative T2Candida External Controls separately, formulated in whole blood, to be used for periodic quality control checks with the T2Candida Panel reagents and the T2Dx Instrument. It is recommended that a single Positive (APG or TPK) Control Tube and a single Negative Control Tube from the respective External Controls kits are run at least once every 30 days. Users should alternate the multiplex blend between APG and TPK Positive Control Tubes with each QC check. Positive APG, Positive TPK and Negative Control Tubes should be run when a new reagent lot is received into the laboratory, or significant maintenance (including software upgrades) is performed on the T2Dx Instrument.
-
25.
It is impossible to interpret non-culture test results without considering the type of invasive candidiasis that is being diagnosed. Candidemia and deep-seated candidiasis (submucosal tissue and organ infections) may occur concurrently or independently. Approximately 50 % of primary candidemia causes secondary deep-seated candidiasis due to hematogenous seeding [1]. Primary deep-seated candidiasis results from non-hematogenous introduction of Candida into sterile sites, most commonly the abdominal cavity following disruption of the gastrointestinal (GI) tract or via an infected peritoneal catheter or drain. Studies suggest that 5–20 % of primary deep-seated candidiasis is associated with secondary candidemia [4–6]. Therefore, to be most useful, diagnostic tests must identify three clinical entities: (1) candidemia without deep-seated candidiasis; (2) candidemia with deep-seated candidiasis; (3) deep-seated candidiasis without candidemia. Studies suggest that roughly one-third of patients with invasive candidiasis fall into each group [7]. Best estimates are that blood cultures will identify the majority of patients in group 1 during active candidemia, approximately 50 % of patients in group 2, and none of the patients in group 3. The power of non-culture tests lies in their potential for identifying the so-called “missing 50 %”—patients in the latter two groups who are currently not diagnosed by blood cultures. The identification of these patients is possible through detection of Candida cellular components that persist in the bloodstream after elimination of viable cells or that are released from deep tissue sites.
-
26.
In well-performed meta-analyses of β-d-glucan studies, pooled sensitivity and specificity for invasive candidiasis (the vast majority of which was candidemia) were 75–80 % and 80 %, respectively [8, 9]. T2Candida was approved by the FDA based on data from 1500 control patients with Candida -negative blood cultures, and 250 contrived blood specimens spiked with C. albicans , C. glabrata, C. parapsilosis, C. tropicalis , or C. krusei at concentrations ranging from 1 to 100 CFU/mL [10]. The overall sensitivity and specificity of T2Candida were 91 % and 98 %, respectively. The performance of the assay (in particular, its sensitivity) needs to be corroborated, as there are limited published data on whole blood specimens from patients with invasive candidiasis [11, 10]. Nevertheless, the preliminary findings are in keeping with data from a meta-analysis of Candida PCR studies, in which pooled sensitivity and specificity for invasive candidiasis (vast majority candidemia) were 95 % and 92 %, respectively [12].
In two recent studies, Fungitell β-d-glucan was 53–65 % sensitive and 73–78 % specific for diagnosing deep-seated Candida infections, almost all of which was intra-abdominal candidiasis [4, 5]. Blood cultures were only 7–21 % sensitive. Sensitivity and specificity of Candida PCR for deep-seated candidiasis were 89 % and 70 %, respectively, in one of the studies [4]; PCR was significantly more sensitive than β-d-glucan. For purposes of this chapter, sensitivities and specificities of Fungitell and PCR-based assays for diagnosing candidemia are assumed to be 80 %/80 % and 90 %/90 %, respectively. The respective values for intra-abdominal candidiasis are assumed to be 60 %/75 % and 80 %/75 %, respectively. Since clinical data are much less extensive for T2Candida than Fungitell β-d-glucan, we assume that performance characteristics for the former assay are comparable to published data for PCR assays.
-
27.
Candidemia and intra-abdominal candidiasis are believed to occur with equal frequency [1, 7]. The predominant type of invasive candidiasis is dictated by the clinical setting. When clinicians order a diagnostic test in a given patient, the most likely type of invasive candidiasis should be apparent. For the most part, candidemia is a low-incidence disease among relatively large at-risk populations. Risk factors are nonspecific and common in hospitalized patients, including broad-spectrum antibiotics, intravenous access devices, total parenteral nutrition, mechanical ventilation, renal insufficiency and replacement therapy, diabetes mellitus, corticosteroids, neutropenia or neutrophil dysfunction, and Candida colonization [13]. In contrast, intra-abdominal candidiasis is a relatively high-incidence disease among more narrowly defined populations. While patients often have some of the risks above, the disease does not occur in the absence of predisposing intra-abdominal factors such as liver transplantation, severe pancreatitis, or disruption of GI tract or peritoneal cavity integrity by disease or medical intervention.
-
28.
In most instances, it should be possible to estimate the pretest likelihood of invasive candidiasis in the patient being tested. Based on published data, the incidence of candidemia increases from <1 to ~10 % as one moves from any hospitalized patient in whom blood cultures are collected, low-risk intensive care unit (ICU) patients or patients undergoing non-gastrointestinal (GI) surgery [14, 15], to more moderate-risk patients who are ICU residents for ≥4 days or who are in septic shock [16, 17], to higher-risk ICU patients identified by clinical prediction rules [16, 18, 19] (Table 2). The incidence of intra-abdominal candidiasis increases from ~3 to ≥30 % as one moves from low-to-moderate risk liver transplant recipients or peritoneal dialysis patients with peritonitis [20, 21], to moderate-risk liver transplant recipients, to high-risk patients with severe acute or necrotizing pancreatitis, recurrent leaks of the GI tract, or bile leaks following liver transplantation [6, 13, 22] (Table 2). Using data such as those in Table 2 as a starting point, the estimated pretest likelihood of invasive candidiasis can be adjusted based on the context of a particular case. “Context” encompasses factors such as presenting complaints, underlying conditions, medications, physical findings, imaging studies and laboratory data, and the likelihood or exclusion of alternative etiologies. Each factor can be considered a “result” in its own right, which adjusts the probability of invasive candidiasis [23]. As an example, moderate-risk ICU patients who fulfill clinical predictive criteria may have different pretest likelihoods of candidemia at the time of testing, even though criteria by themselves assign comparable risk (~10 % incidence).
-
29.
Before interpreting a test result and making treatment decisions in a patient, it is imperative to understand the Bayesian nature of non-culture diagnostics. No matter how sensitive or specific a non-culture assay for invasive candidiasis may be, clinicians must accept a level of uncertainty when interpreting results. By definition, a positive blood culture or tissue culture obtained in a sterile manner establishes the diagnosis of invasive candidiasis. In contrast, non-culture tests are biomarkers that assign a probability of disease, which is shaped by the pretest likelihood, and sensitivity and specificity of the test. In Table 3, PPVs and NPVs of non-culture tests are calculated for various clinical settings in which candidemia or primary intra-abdominal candidiasis is the predominant disease. At low pretest likelihoods of either disease, PPVs and NPVs are extremely low and extremely high, respectively. As likelihoods increase, PPVs improve at the expense of NPVs. For candidemia, β-d-glucan NPVs remain exceptional (≥97 %) in each of the clinical settings; PPV is 31 % in the high-risk ICU setting. The superior sensitivity and specificity of PCR -based assays improve PPVs for candidemia compared to β-d-glucan, but the impact on NPVs is negligible. PPVs and NPVs are lower for intra-abdominal candidiasis than candidemia at a given pretest likelihood of disease, due to lower sensitivities and specificities. β-d-glucan NPV for intra-abdominal candidiasis is strong (≥97 %) in low-risk settings, but values drop below 90 or 80 % in higher-risk settings (e.g., severe acute or necrotizing pancreatitis, high-risk GI surgery or liver transplantation). β-d-glucan PPV rises to 51 % among the highest-risk patients. The superior performance of a PCR-based assay impacts NPVs in the higher-risk settings, but has lesser impact on PPVs.
-
30.
In clinical practice, non-culture tests will be used in conjunction with cultures. It is important to understand that cultures are very sensitive at recovering viable Candida from the bloodstream, with median limits of detection (~1 CFU/mL) that are at or below those of PCR [24, 25]. For this reason, cultures should be positive during the vast majority of ongoing Candida bloodstream infections. If cultures are negative due to extremely low-level candidemia, Fungitell and PCR assays are unlikely to make the diagnosis reliably. At present, it is unknown whether T2Candida is more sensitive than conventional Candida PCR. Even if non-culture tests are not more sensitive than cultures for diagnosing active candidemia, their shorter turnaround times should facilitate more rapid treatment decisions. Perhaps more importantly, non-culture diagnostics have the potential to identify blood culture-negative, primary or secondary deep-seated candidiasis.
In one study, the combination of either a positive Candida blood culture or Fungitell β-d-glucan was 79 % sensitive for diagnosing all types of invasive candidiasis; a positive blood culture or positive PCR was 98 % sensitive [4]. The interpretation of positive non-culture tests in the setting of negative blood cultures is difficult, since the latter make active candidemia extremely unlikely but do not preclude deep-seated candidiasis. Indeed, the likelihood ratio of primary intra-abdominal candidiasis given negative blood cultures is ~0.8 [4, 5]; in other words, the odds of having the disease are reduced ~20 % if blood cultures are negative. If it is assumed that ~50 % of candidemia results in target organ infection, the likelihood ratio of secondary deep-seated candidiasis despite negative blood cultures may be as high as 0.4. Using these data, PPVs and NPVs of β-d-glucan and PCR for invasive candidiasis can be readjusted for negative blood cultures (Table 3).
-
31.
Clinicians can use the estimated pretest likelihood of invasive candidiasis in the patient being tested to calculate PPV and NPV, along the lines of the examples in Table 3. If blood cultures are drawn concurrently with the non-culture test, PPV and NPV are assessed in two stages (based on the non-culture test alone, and then adjusted for culture results). Of course, positive blood cultures diagnose invasive candidiasis conclusively, regardless of the non-culture result. Just as clinicians may adjust the pretest likelihood of invasive candidiasis in response to the context of a particular case, they may modify PPV and NPV based on the magnitude or number of test results. For example, two highly positive results are more compelling than a single borderline result, and multiple negative results are more compelling than a single negative result. It is infeasible for clinicians to calculate precise running tallies of likelihood ratios as they estimate pretest likelihoods or interpret test results in each patient. Nevertheless, they can conceptualize results qualitatively prior to making treatment decisions [23]. Examples of useful qualitative evaluations include “the patient is reasonably likely to have invasive candidiasis, and a positive result significantly increases that likelihood”, or “in this low-risk patient, a positive result does not help me, but a negative result essentially excludes the disease.”
-
32.
The management strategies presented in this chapter are based largely on data from antifungal prophylaxis studies in various patient populations. These strategies (or others that use non-culture diagnostics to direct antifungal treatment) have not been validated in clinical trials. Therefore, the methods we propose may be a basis for designing future research studies, as well as a guide for clinicians struggling to make use of non-culture tests in their practices. As mentioned earlier, the interpretive and clinical decision-making processes we describe can be applied to other assays as they enter the clinic, and to Fungitell and T2Candida assays as more data emerge.
-
33.
Broadly speaking, non-culture tests may be used to screen populations for invasive candidiasis or to manage individual patients. At the population level, screening may be incorporated into prophylactic or preemptive antifungal strategies. In the former, an antifungal agent is initiated in a population at risk for invasive candidiasis, and a negative test result is used to discontinue treatment. In preemptive strategies, antifungal treatment is initiated in response to a positive test result. Several studies suggest that prophylaxis is beneficial in preventing invasive fungal infections in various settings with baseline rates of disease ≥~15 % [26–32]. Preemptive strategies are attractive conceptually, but they have not been validated conclusively [18, 33]. A paradigm that uses non-culture diagnostics and blood cultures to guide prophylaxis or preemptive treatment is presented in Fig. 2. The feasibility of the strategy in a given setting will depend upon PPVs and NPVs in the particular clinical setting.
-
34.
PPV and NPV thresholds to trigger or discontinue antifungal treatment are not established conclusively. Based on the prophylaxis data cited above, however, PPV ≥ ~15 % and NPV ≥ ~85 % are reasonable thresholds to consider initiating preemptive antifungal treatment and withholding antifungal treatment, respectively. NPVs <85 % are likely to leave too high a posttest probability of invasive candidiasis for antifungals to be deferred comfortably. In order for non-culture screening to be viable, a positive or negative result must provide marginal value beyond simply knowing the pretest likelihood. In other words, clinicians should ask: Do results sufficiently change the probability of invasive candidiasis such that threshold PPV and NPV is now achieved?
In certain low- and high-risk settings, the answer to this question is no, and screening with non-culture tests will not be useful. At very low pretest likelihoods of either candidemia or intra-abdominal candidiasis, the practical value of negative test results is negligible. For example, a negative β-d-glucan in an ICU setting that is low-to-moderate risk for candidemia reduces disease likelihood from ~3 to ~1 % (Table 3). At the same time, a β-d-glucan PPV of ~11 % is likely to be too low to justify preemptive treatment in this population, in the absence of a positive culture or other evidence of disease. At some high-end pretest likelihood, NPVs become too low to be useful clinically. The NPV of β-d-glucan among high-risk GI surgery or liver transplant patients (pretest likelihood ~30 %) is only 78 %, meaning clinicians must be willing to forego treatment despite a >20 % chance that intra-abdominal candidiasis is present. Likewise, it is not clear that the 51 % PPV of β-d-glucan in these settings has greater practical value than simply knowing the pretest likelihood. At some point, the pretest likelihood of invasive candidiasis may be sufficient to justify antifungal treatment regardless of non-culture test results. Indeed, universal prophylaxis is beneficial among groups such as bone marrow transplant recipients, surgical patients with recurrent GI leaks, and high-risk liver transplant recipients with bile leaks (≥30 % incidence of Candida infection) [5, 20].
-
35.
By applying data such as those in Table 3 to the paradigm of Fig. 2, it is possible to assign windows of pretest likelihoods in which non-culture tests are most likely to valuable in guiding preemptive treatment (Table 4). If validated, the improved performance of T2Candida (or other PCR -based assay) over β-d-glucan should expand the patient populations for prophylactic or preemptive treatment. T2Candida would have greatest impact among those at risk for candidemia, as antifungal strategies become viable for lower-risk ICU patients (e.g., ICU resident for ≥4 days) and patients in septic shock. Such an assay would also extend prophylactic or preemptive treatment to patients at highest-risk for intra-abdominal candidiasis. An ideal non-culture test would diagnose both candidemia and intra-abdominal candidiasis with sensitivity/specificity of ~90 %/90 %. A test with this performance for intra-abdominal candidiasis, rather than 80 %/70 % sensitivity/specificity suggested by the PCR literature, would expand the window to include lower-risk surgical ICU populations and peritoneal dialysis patients with peritonitis.
-
36.
The use of non-culture tests in caring for individuals is more nuanced than when screening populations as part of prophylactic or preemptive antifungal strategies. Clinicians must make decisions about when to order tests based on the context of the particular case, without strict regard to the windows assigned above. For example, a positive non-culture test result with predictive value that is ≤15 % nevertheless may justify antifungal treatment if a patient is sick and there is no alternative diagnosis. Likewise, there is often clinical value in excluding invasive candidiasis in a patient for whom the cause of illness is not apparent, even if the pretest likelihood of invasive candidiasis is beneath the threshold for screening populations.
References
Clancy CJ, Nguyen MH (2013) Finding the “missing 50%” of invasive candidiasis: how nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin Infect Dis 56(9):1284–1292. doi:10.1093/cid/cit006
Andes DR, Safdar N, Baddley JW, Playford G, Reboli AC, Rex JH, Sobel JD, Pappas PG, Kullberg BJ (2012) Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis 54(8):1110–1122. doi:10.1093/cid/cis021
Wheat LJ (2009) Approach to the diagnosis of invasive aspergillosis and candidiasis. Clin Chest Med 30(2):367–377, viii. doi:10.1016/j.ccm.2009.02.012
Nguyen MH, Wissel MC, Shields RK, Salomoni MA, Hao B, Press EG, Shields RM, Cheng S, Mitsani D, Vadnerkar A, Silveira FP, Kleiboeker SB, Clancy CJ (2012) Performance of Candida real-time polymerase chain reaction, beta-D-glucan assay, and blood cultures in the diagnosis of invasive candidiasis. Clin Infect Dis 54(9):1240–1248. doi:10.1093/cid/cis200
Tissot F, Lamoth F, Hauser PM, Orasch C, Fluckiger U, Siegemund M, Zimmerli S, Calandra T, Bille J, Eggimann P, Marchetti O (2013) Beta-glucan antigenemia anticipates diagnosis of blood culture-negative intraabdominal candidiasis. Am J Respir Crit Care Med 188(9):1100–1109. doi:10.1164/rccm.201211-2069OC
Calandra T, Bille J, Schneider R, Mosimann F, Francioli P (1989) Clinical significance of Candida isolated from peritoneum in surgical patients. Lancet 2(8677):1437–1440, S0140-6736(89)92043-6 [pii]
Leroy O, Gangneux JP, Montravers P, Mira JP, Gouin F, Sollet JP, Carlet J, Reynes J, Rosenheim M, Regnier B, Lortholary O (2009) Epidemiology, management, and risk factors for death of invasive Candida infections in critical care: a multicenter, prospective, observational study in France (2005–2006). Crit Care Med 37(5):1612–1618. doi:10.1097/CCM.0b013e31819efac0
Karageorgopoulos DE, Vouloumanou EK, Ntziora F, Michalopoulos A, Rafailidis PI, Falagas ME (2011) Beta-D-glucan assay for the diagnosis of invasive fungal infections: a meta-analysis. Clin Infect Dis 52(6):750–770. doi:10.1093/cid/ciq206
He S, Hang JP, Zhang L, Wang F, Zhang DC, Gong FH (2014) A systematic review and meta-analysis of diagnostic accuracy of serum 1,3-beta-d-glucan for invasive fungal infection: focus on cutoff levels. J Microbiol Immunol Infect. doi:10.1016/j.jmii.2014.06.009
Mylonakis E, Clancy CJ, Ostrosky-Zeichner L, Garey KW, Alangaden GJ, Vazquez JA, Groeger SJ, Judson MA, Vinagre YM, Heard SO, Zervou FN, Zacharioudakis IM, Kontoyiannis DP, Pappas PG (2015) T2 magnetic resonance assay for the rapid diagnosis of candidemia in whole blood: a clinical trial. Clin Infect Dis 60:892–899
Neely LA, Audeh M, Phung NA, Min M, Suchocki A, Plourde D, Blanco M, Demas V, Skewis LR, Anagnostou T, Coleman JJ, Wellman P, Mylonakis E, Lowery TJ (2013) Magnetic resonance enables nanoparticle-mediated rapid detection of candidemia in whole blood. Sci Transl Med 5(182):182ra154. doi:10.1126/scitranslmed.3005377
Avni T, Leibovici L, Paul M (2011) PCR diagnosis of invasive candidiasis: systematic review and meta-analysis. J Clin Microbiol 49(2):665–670. doi:10.1128/JCM.01602-10
Delaloye J, Calandra T (2014) Invasive candidiasis as a cause of sepsis in the critically ill patient. Virulence 5(1):161–169. doi:10.4161/viru.26187
Michalopoulos AS, Geroulanos S, Mentzelopoulos SD (2003) Determinants of candidemia and candidemia-related death in cardiothoracic ICU patients. Chest 124(6):2244–2255
Kett DH, Azoulay E, Echeverria PM, Vincent JL (2011) Candida bloodstream infections in intensive care units: analysis of the extended prevalence of infection in intensive care unit study. Crit Care Med 39(4):665–670. doi:10.1097/CCM.0b013e318206c1ca
Ostrosky-Zeichner L, Sable C, Sobel J, Alexander BD, Donowitz G, Kan V, Kauffman CA, Kett D, Larsen RA, Morrison V, Nucci M, Pappas PG, Bradley ME, Major S, Zimmer L, Wallace D, Dismukes WE, Rex JH (2007) Multicenter retrospective development and validation of a clinical prediction rule for nosocomial invasive candidiasis in the intensive care setting. Eur J Clin Microbiol Infect Dis 26(4):271–276. doi:10.1007/s10096-007-0270-z
Hadley S, Lee WW, Ruthazer R, Nasraway SA Jr (2002) Candidemia as a cause of septic shock and multiple organ failure in nonimmunocompromised patients. Crit Care Med 30(8):1808–1814
Ostrosky-Zeichner L, Shoham S, Vazquez J, Reboli A, Betts R, Barron MA, Schuster M, Judson MA, Revankar SG, Caeiro JP, Mangino JE, Mushatt D, Bedimo R, Freifeld A, Nguyen MH, Kauffman CA, Dismukes WE, Westfall AO, Deerman JB, Wood C, Sobel JD, Pappas PG (2014) MSG-01: a randomized, double-blind, placebo-controlled trial of caspofungin prophylaxis followed by preemptive therapy for invasive candidiasis in high-risk adults in the critical care setting. Clin Infect Dis 58:1219–1226. doi:10.1093/cid/ciu074
Paphitou NI, Ostrosky-Zeichner L, Rex JH (2005) Rules for identifying patients at increased risk for candidal infections in the surgical intensive care unit: approach to developing practical criteria for systematic use in antifungal prophylaxis trials. Med Mycol 43(3):235–243
Eschenauer GA, Kwak EJ, Humar A, Potoski BA, Clarke LG, Shields RK, Abdel-Massih R, Silveira FP, Vergidis P, Clancy CJ, Nguyen MH (2015) Targeted versus universal antifungal prophylaxis among liver transplant recipients. Am J Transplant 15:180–189. doi:10.1111/ajt.12993
Matuszkiewicz-Rowinska J (2009) Update on fungal peritonitis and its treatment. Perit Dial Int 29(Suppl 2):S161–S165
Hall AM, Poole LA, Renton B, Wozniak A, Fisher M, Neal T, Halloran CM, Cox T, Hampshire PA (2013) Prediction of invasive candidal infection in critically ill patients with severe acute pancreatitis. Crit Care 17(2):R49. doi:10.1186/cc12569
Gill CJ, Sabin L, Schmid CH (2005) Why clinicians are natural bayesians. BMJ 330(7499):1080–1083. doi:10.1136/bmj.330.7499.1080
Pfeiffer CD, Samsa GP, Schell WA, Reller LB, Perfect JR, Alexander BD (2011) Quantitation of Candida CFU in initial positive blood cultures. J Clin Microbiol 49(8):2879–2883. doi:10.1128/JCM.00609-11
Telenti A, Steckelberg JM, Stockman L, Edson RS, Roberts GD (1991) Quantitative blood cultures in candidemia. Mayo Clin Proc 66(11):1120–1123
Playford EG, Webster AC, Sorrell TC, Craig JC (2006) Antifungal agents for preventing fungal infections in non-neutropenic critically ill and surgical patients: systematic review and meta-analysis of randomized clinical trials. J Antimicrob Chemother 57(4):628–638. doi:10.1093/jac/dki491
Shorr AF, Chung K, Jackson WL, Waterman PE, Kollef MH (2005) Fluconazole prophylaxis in critically ill surgical patients: a meta-analysis. Crit Care Med 33(9):1928–1935, quiz 1936
Eggimann P, Francioli P, Bille J, Schneider R, Wu MM, Chapuis G, Chiolero R, Pannatier A, Schilling J, Geroulanos S, Glauser MP, Calandra T (1999) Fluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgical patients. Crit Care Med 27(6):1066–1072
Garbino J, Lew DP, Romand JA, Hugonnet S, Auckenthaler R, Pittet D (2002) Prevention of severe Candida infections in nonneutropenic, high-risk, critically ill patients: a randomized, double-blind, placebo-controlled trial in patients treated by selective digestive decontamination. Intensive Care Med 28(12):1708–1717. doi:10.1007/s00134-002-1540-y
Pelz RK, Hendrix CW, Swoboda SM, Diener-West M, Merz WG, Hammond J, Lipsett PA (2001) Double-blind placebo-controlled trial of fluconazole to prevent candidal infections in critically ill surgical patients. Ann Surg 233(4):542–548
Goodman JL, Winston DJ, Greenfield RA, Chandrasekar PH, Fox B, Kaizer H, Shadduck RK, Shea TC, Stiff P, Friedman DJ et al (1992) A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med 326(13):845–851. doi:10.1056/NEJM199203263261301
Slavin MA, Osborne B, Adams R, Levenstein MJ, Schoch HG, Feldman AR, Meyers JD, Bowden RA (1995) Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation—a prospective, randomized, double-blind study. J Infect Dis 171(6):1545–1552
Muldoon EG, Denning DW (2014) Editorial commentary: Prophylactic echinocandin: is there a subgroup of intensive care unit patients who benefit? Clin Infect Dis 58(9):1227–1229. doi:10.1093/cid/ciu080
Akamatsu N, Sugawara Y, Kaneko J, Tamura S, Makuuchi M (2007) Preemptive treatment of fungal infection based on plasma (1 → 3)beta-D-glucan levels after liver transplantation. Infection 35(5):346–351. doi:10.1007/s15010-007-6240-7
Jaijakul S, Vazquez JA, Swanson RN, Ostrosky-Zeichner L (2012) (1,3)-Bta-D-glucan as a prognostic marker of treatment response in invasive candidiasis. Clin Infect Dis 55(4):521–526. doi:10.1093/cid/cis456
Financial Disclosures/Acknowledgements
Drs. Clancy and Nguyen have served as site PIs for diagnostic clinical trials funded by T2 Biosystems. Dr. Clancy has received financial support for investigator-initiated research projects from Pfizer, Merck, and CSL Behring. Dr. Nguyen has received financial support for investigator-initiated research projects from Pfizer, Merck, Astellas, and Vira-Cor IBT. The authors received no funding or other assistance for the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Clancy, C.J., Nguyen, M.H. (2016). Diagnostic Methods for Detection of Blood-Borne Candidiasis. In: Calderone, R., Cihlar, R. (eds) Candida Species. Methods in Molecular Biology, vol 1356. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3052-4_16
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3052-4_16
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3051-7
Online ISBN: 978-1-4939-3052-4
eBook Packages: Springer Protocols