Abstract
Delivering evidence-based treatments in schools is considered a promising avenue for addressing the high rates of anxious youth who do not receive treatment. This chapter reviews recent literature documenting progress toward evaluating the transportability and dissemination of anxiety interventions to school settings. Although training school professionals, such as guidance counselors, to deliver these treatments is an important step toward dissemination, additional study is needed. Critical issues for the future of this growing field are explored, namely the need to establish standardized methods of monitoring treatment fidelity and to develop feasible and effective training and supervision models. Such advances in implementation science will be essential for promoting the feasibility and sustainability of evidence-based treatments in school settings.
This work was supported by an NIMH grant awarded to Dr. Masia Warner, Grant No. R01MH081881.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Anxiety disorders are the most common psychopathology in children and adolescents, affecting over 30% before adulthood (Merikangas et al., 2010). With median age of onset ranging from 6 to 14 years, anxiety disorders are among the earliest classes of psychopathology to develop (Costello, Egger, & Angold, 2005; Merikangas et al., 2010). Youth with anxiety disorders experience significant subjective distress and disability that negatively affects friendships, family relationships, and academic achievement (Grover, Ginsburg, & Ialongo, 2007; Langley, Bergman, McCracken, & Piacentini, 2004). Without intervention, anxiety disorders often run a chronic course and persist into adulthood (Costello et al., 2005), placing youth at risk for later mood and substance use disorders (Bittner et al., 2007; Costello, Mustillo, Erkanli, Keeler, & Angold, 2003). Thus, it is not surprising that anxiety disorders are among the most costly classes of mental health disorders (Rice & Miller, 1998), with direct and indirect costs estimated at over 42 billion dollars per year in the United States (Greenberg et al., 1999). The psychosocial and financial consequences of untreated anxiety disorders underscore the importance of effective and available treatments.
Several cognitive-behavioral treatments (CBT) for childhood anxiety disorders have been systematically evaluated and received empirical support (e.g., Beidel, Turner, & Morris, 2000; Kendall, 1994; Silverman et al., 1999). Despite these efforts, many anxious youth remain unidentified (Masia Warner, Fisher, Shrout, Rathor, & Klein, 2007), and more than 80% remain untreated (Merikangas et al., 2011). Even when anxious youth do come into contact with various health sectors, they may not receive mental health services. One recent study found that students identified as anxious based on a school-wide screening were significantly less likely than students with other mental health problems to have received follow-up care from a provider (Husky, Sheridan, McGuire, & Olfson, 2011). It has been shown that anxious youth seen by pediatricians are less likely to be referred for treatment than children with externalizing problems (Wren, Scholle, Heo, & Comer, 2005). Additionally, logistical barriers can prevent families from accessing community mental health services (e.g., long waitlists, high costs; Owens et al., 2002), and only a small percentage of these are evidence-based treatments (EBTs), such as CBT (Collins, Westra, Dozois, & Burns, 2004; Labellarte, Ginsburg, Walkup, & Riddle, 1999).
Because many anxious youth are not identified or referred, it follows that traditional mental health service delivery models (e.g., community mental health centers, independent practitioner offices) may not be sufficient to meet their treatment needs. Given the impairment and cost associated with anxiety disorders, it is imperative that researchers, clinicians, and policy makers explore alternate methods and venues for providing anxious youth with effective treatment (Weist, 1999).
Rationale for School-Based Anxiety Treatment
Schools have been increasingly recognized as a critical avenue for helping address the unmet mental health needs of youth with anxiety disorders (Masia Warner, Nangle, & Hansen, 2006). Implementing EBTs for anxiety in the school setting has several potential advantages. For example, partnering with schools to educate school personnel in identifying anxiety or implementing school-wide screenings may facilitate early detection and intervention (Fox, Halpern, & Forsyth, 2008; Weist, Myers, Hastings, Ghuman, & Han, 1999). Beyond increasing recognition, conducting treatments within the school setting minimizes barriers to accessing community services (Husky et al., 2011).
Moreover, the school environment is an ecologically valid setting for treating anxiety disorders. Common triggers of anxiety for youth are often found at school, ranging from worries about tests and class presentations to separating from caregivers and talking with new peers. Therefore, implementing treatment for anxiety disorders in schools provides opportunities to practice new skills and engage in exposure exercises in a real-world setting that may promote generalization (Evans, 1999; Evans, Langberg, & Williams, 2003). For example, children with class participation fears have a multitude of opportunities to work their way up a fear hierarchy in school, from answering a question in their favorite class to eventually volunteering in the class in which they are most nervous. Peers and teachers can also be enlisted to assist in exposure activities (e.g., requesting a teacher to call on the child to ensure repeated practice), while school-based treatment providers can be on hand to offer coaching and process the experience. In this way, treatment delivered in schools can reduce the divide between the clinical setting and the “real world.”
Movement Toward Transportability and Dissemination to Schools
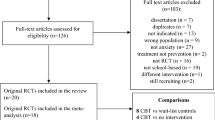
Inspired by the potential benefits of implementing anxiety treatments in schools, researchers have begun to develop, evaluate, and demonstrate support for several school-based CBT programs. Studies of these anxiety treatments can be classified along a continuum according to the degree to which researchers are involved in implementing the intervention (Chorpita, 2008). Efficacy studies conducted in the 1980s and 1990s showed that CBT was highly successful in treating child anxiety disorders in clinic and laboratory settings under controlled conditions (e.g., using highly trained and supervised therapists). This past decade witnessed an increase in transportability studies, which evaluate CBT programs delivered in school settings by research-based providers (e.g., doctoral-level psychologists or graduate students), under more real-world conditions, and with fewer exclusionary criteria placed on participation. In the past few years, dissemination studies have begun to emerge, representing an exciting advance in school-based anxiety treatment research. The aim of dissemination studies is to evaluate whether school-based providers, including specialized school mental health professionals (e.g., school social workers and school psychologists) and other school personnel (e.g., school guidance counselors and teachers), can be trained to effectively implement CBT programs.
This chapter will present five school-based treatments for anxiety that have been evaluated in controlled trials. School-based trials implemented by research-based providers have demonstrated support for transportability to schools for most of these programs. More recently, a limited number of school-based trials implemented by school-based providers have examined whether these programs can be delivered by school personnel with limited background in CBT. In reviewing both types of school-based studies, we will describe the treatment programs, present clinical outcome data, and include available information on treatment fidelity or the degree to which an intervention is implemented as intended (Perepletchikova, Hilt, Chereji, & Kazdin, 2009). The order in which the programs are described reflects the types of anxiety they address; programs treating a range of anxiety problems are presented first, followed by programs treating specific anxiety disorders (e.g., social phobia). We will conclude by highlighting critical next steps the field must address to successfully disseminate school-based interventions.
FRIENDS
Program Overview
FRIENDS is a group-based cognitive-behavioral anxiety prevention program for school-age youth (Barrett & Turner, 2001). Adapted from Coping Koala (Barrett, Dadds, & Rapee, 1996), an Australian adaptation of Coping Cat (Kendall, 1994), FRIENDS has been shown to be efficacious in the treatment of clinically anxious youth (Shortt, Barrett, & Fox, 2001). In a group format, children are taught skills and techniques for coping with anxiety, including emotion recognition and regulation, relaxation, cognitive restructuring, problem solving, and in vivo exposure. The acronym “FRIENDS” assists children in remembering the program’s core skills: F (“Feeling worried”), R (“Relax and feel good”), I (“Inner thoughts”), E (“Explore plans of action”), N (“Nice work, reward yourself”), D (“Don’t forget to practice”), and S (“Stay cool!”). FRIENDS consists of 10 weekly group sessions (approximately 1-hour long), as well as two booster sessions conducted 1 month and 3 months after the final group. Four sessions conducted at regular intervals during the program give parents an opportunity to learn about the program and parenting strategies to promote anxiety management. The FRIENDS program manual and other materials are available for purchase at www.australianacademicpress.com.au/friends.
School-Based Trial of FRIENDS with Research-Based Providers
Although most often evaluated in a curriculum-based format applied universally to entire classes of schoolchildren, FRIENDS has also been investigated within an indicated prevention framework for children deemed “at risk” for anxiety disorders based on the presence of mild to moderate anxiety symptoms. Dadds and colleagues (Dadds et al., 1999; Dadds, Spence, Holland, Barrett, & Laurens, 1997), for example, compared Coping Koala (n = 61), the precursor to FRIENDS, to a no-treatment control group (n = 67) in a sample of 128 children between the ages of 7 and 14. Parents of children who received elevated scores on an anxiety self-report measure as part of a school-wide screening, or who were nominated by their teachers, were invited to complete an in-person diagnostic interview. Children were eligible to participate if they received a diagnosis of an anxiety disorder at a mild to moderate severity level or if they had features of an anxiety disorder that did not meet criteria for a disorder (e.g., subthreshold). The Coping Koala intervention was delivered over 1–2-h weekly sessions in groups of five to twelve students. Program leaders were trained clinical psychologists assisted by one to two clinical psychology graduate students, who completed a 1-day training session and received weekly supervision by program leaders.
Overall, findings were mixed. No group differences in anxiety diagnoses were found immediately following intervention, with both groups showing improvement. However, differences emerged over time, with fewer children in the intervention group (~25%) meeting criteria for anxiety diagnoses relative to controls (~60%) at 6-month follow-up. In addition, children with anxious features, but without baseline diagnoses, progressed to clinical diagnoses by 6-month follow-up at differing rates (16% of intervention and 54% of controls). At 12-month follow-up, rates of anxiety diagnoses were equivalent across study groups (37% for intervention and 42% for control), though group differences were again observed at 24 months (20% for intervention and 39% for controls).
An extension of the work by Dadds and colleagues, Bernstein, Layne, Egan, and Tennison (2005) evaluated a modified version of FRIENDS that added nine weekly group parent training sessions, also conducted in school. Discussion centered on the bidirectional relationship between the child’s anxiety and the family system. In addition to learning behavioral strategies to encourage their children to face their fears, parents were taught how to manage their own anxiety in order to become a more effective coach and model. The child group portion was shortened by one session, though no content was lost. In the RCT, 61 children between ages 7 and 11 with mild to moderate symptoms of separation, generalized, or social anxiety disorder (either meeting the criteria or subthreshold) were randomized to FRIENDS (n = 17), FRIENDS plus parent training (n = 20), or a no-treatment control (n = 24). Both FRIENDS groups were delivered by experienced CBT therapists who were part of the research team. Overall, results demonstrated superiority of both active treatments compared to no treatment based on clinician-, child-, and parent-report measures at post-treatment (Bernstein, Layne, Egan, & Tennison, 2005) and at 3-, 6-, and 12-month follow-ups (Bernstein, Bernat, Victor, & Layne, 2009). However, because few significant differences were found between the two FRIENDS conditions, it is unclear whether there is added benefit of parent training.
School-Based Trials of FRIENDS with School-Based Providers
Recent years have been marked by initial attempts to disseminate FRIENDS via two controlled studies that examined the effectiveness of FRIENDS when delivered by school-based personnel for children reporting elevated anxiety symptoms (Hunt, Andrews, Crino, Erksine, & Sakashita, 2009; Miller et al., 2011). Hunt and colleagues, 2009 compared a nine-session version of FRIENDS (n = 136), led by a school counselor assisted by a support teacher, to a no-treatment control (n = 124) in a sample of children ages 11–13. Miller and colleagues (2011) compared a ten-session version of FRIENDS (n = 64), led by a teacher and either a school counselor or psychology graduate student, to an attention-control group (n = 125) in a sample of fourth through sixth graders (mean age = 10.1). Approaches to training and supervision differed. Hunt and colleagues provided a 2-day training workshop without ongoing supervision, while Miller and colleagues provided 6 h of in-school training followed by weekly meetings with the research team to review session goals. With respect to treatment fidelity, research staff in Hunt et al. listened to session recordings (obtained at 4 of 10 schools where FRIENDS was delivered) and rated 55% of selected sessions as having met the stated aims either moderately or extremely well. In sharp contrast to research staff ratings, FRIENDS program leaders self-rated about 94% of selected sessions as having met that same standard. In Miller et al., two trained graduate students blind to study conditions rated adherence of 25% of group sessions. Adherence to program objectives was reported to be nearly 80%.
Outcomes were disappointing in both studies. Compared to their respective controls, no differences were observed on self-report measures of anxiety symptoms immediately following intervention. Additionally, Miller et al. found no post-intervention group differences on parent or teacher reports. Hunt et al. found no differences at a 2-year follow-up, though greater reduction in self-reported anxiety symptoms for FRIENDS was obtained on one measure at a 4-year follow-up. It is possible that inadequate treatment fidelity contributed to the lack of significant effects. In fact, Hunt and colleagues suggest that their use of training workshops alone may have been insufficient for achieving high-quality program implementation, an assertion consistent with the literature on training community clinicians (e.g., Beidas, Barmish, & Kendall, 2009; DeViva, 2006). However, given the limited nature of treatment integrity data in both studies (adherence ratings only on a small sample of treatment sessions), it is difficult to draw conclusions regarding the relationship between therapist competence and clinical outcomes. In summary, while FRIENDS may have potential as a universal prevention program, it remains unclear whether it is an effective option for treating anxious youth in schools, particularly when delivered by school personnel.
Cool Kids
Program Overview
Cool Kids is a cognitive-behavioral group intervention for children between ages seven and 12 with anxiety symptoms (Mifsud & Rapee, 2005). Unlike FRIENDS, Cool Kids was specifically designed as an indicated intervention. Adapted from a previous treatment program for youth with clinical anxiety disorders (Rapee, 2000), Cool Kids is comprised of eight weekly sessions (60 min long) conducted during school hours in small groups of approximately eight to ten children. Initial sessions emphasize psychoeducation and cognitive restructuring, while later sessions focus on graduated exposure to feared situations. Children are also taught skills for problem solving, social interaction, handling bullying or teasing, and increasing assertiveness. Two additional sessions for parents offer information about the program and behavior management skills. The Cool Kids therapist manual is available for purchase at www.emotionalhealthclinic.com.au.
School-Based Trial of Cool Kids with Research-Based and School-Based Providers
Mifsud and Rapee (2005) examined Cool Kids in a sample of 91 children (ages 8–11) recruited from nine schools in socioeconomically disadvantaged communities in Australia. Children with elevated self-reported anxiety scores on school-wide screenings were included. Nine schools were randomly assigned to Cool Kids (n = 51) or a waitlist control (n = 40). Each Cool Kids group was delivered by a school counselor paired with a community mental health therapist hired by the research team. All group leaders received a full day of training but did not receive ongoing supervision. Data on treatment fidelity was not reported. The Cool Kids group exhibited greater reductions in self-reported and teacher-reported anxiety symptoms at post-treatment and at 4-month follow-up, when compared to the control. These findings are promising, though further research is needed to evaluate the effectiveness of Cool Kids when delivered exclusively by school personnel.
Baltimore Child Anxiety Treatment Study in the Schools (BCATSS)
Program Overview
BCATSS was designed to evaluate the feasibility and utility of school-based CBT tailored for anxious youth in inner-city, low-income, and predominantly African American communities, a population with typically unmet mental health service needs (Ginsburg, Becker, Kingery, & Nichols, 2008). Utilizing an individual format, the 10-session treatment in BCATSS features modifications for this population, such as providing culturally relevant examples and making traditional CBT techniques more interactive. Each session is approximately 35 min in length and designed to be delivered by school-based mental health clinicians. BCATSS utilizes a manualized treatment with a modular protocol, such that therapists have flexibility in choosing which core CBT skills (“modules”) to implement in a given session based on the needs of the child. Modules include psychoeducation, contingency management, relaxation, exposure, cognitive restructuring, problem solving, and relapse prevention.
School-Based Trial of BCATSS with Research-Based Providers
In an initial controlled study preceding BCATSS, Ginsburg and Drake (2002) randomly assigned 12 clinically anxious African American adolescents (ages 14–17) from inner-city Baltimore to either a school-based CBT (n = 6) or attention-support (AS; n = 6) condition. In contrast to the newer modular/individual approach of BCATSS, Ginsburg and Drake utilized a group format. Two advanced psychology graduate students trained in CBT served as program leaders. Both the CBT and AS conditions met for 10 group sessions during regular class periods (45–50 min in length) at the same school. Results supported the efficacy of school-based CBT for this population, with 75% of the CBT participants no longer meeting criteria for their primary anxiety diagnosis at post-treatment, compared to 20% of the AS participants. Clinician-rated impairment and self-rated anxiety levels were lower in the CBT condition at post-treatment.
School-Based Trial of BCATSSwith School-Based Providers
Building on this initial pilot study, BCATSS was developed to test the effectiveness of CBT for inner-city African American youth when delivered by school-based mental health clinicians with limited prior background in CBT. BCATSS therapists are social workers and doctoral-level psychologists who each serve as the full-time clinician at their respective schools. In the ongoing RCT designed for BCATSS, children (ages 7–12) are referred by school personnel or parents and invited to enroll if they have a primary diagnosis of social anxiety disorder (SAD), separation anxiety disorder, generalized anxiety disorder, or specific phobia. Children are assigned to either the 12-session individual CBT program described earlier or treatment as usual (TAU). In addition to attending a 2-day training covering anxiety symptoms and the CBT modules, clinicians receive weekly supervision. The TAU condition is conducted individually by the same clinician administering the CBT condition in his or her school, with careful monitoring of treatment contamination integrated in study procedures. Although outcome data has not yet been published, positive findings from BCATSS may aid in efforts to integrate anxiety treatment into schools and meet the mental health needs of anxious youth from diverse backgrounds.
Skills for Academic and Social Success (SASS)
Program Overview
Skills for Academic and Social Success (SASS; Masia et al., 1999) is a cognitive-behavioral group treatment for adolescents with SAD designed for delivery in school settings. Adapted from Social Effectiveness Therapy for Children, an efficacious group treatment for children with SAD (Beidel et al., 2000; Beidel, Turner, Young, & Paulson, 2005), SASS similarly emphasizes exposure and social skills training but includes modifications for an adolescent population (e.g., age-appropriate social skills, addition of cognitive restructuring) and the school environment (e.g., fewer/shorter sessions, involvement of teachers, parents, and school peers). SASS consists of 12 weekly group school sessions, two individual meetings, two parent meetings, two teacher meetings, four social events, and two booster sessions (Ryan & Masia Warner, 2012). Group sessions, each lasting a roughly 40-min class period, focus on three core components: (1) cognitive restructuring (realistic thinking); (2) social skills training, including initiating and maintaining conversations; and (3) in vivo exposure to feared social situations, which are often integrated in the school environment (e.g., talking with teachers or classmates in the lunchroom). Individual meetings provide group members the opportunity for problem solving around obstacles to treatment and conducting additional exposure exercises. Social events bring group members and outgoing peers together in natural community “hangouts” (e.g., bowling) to facilitate real-world exposure and skills generalization. Parent meetings educate parents about the cognitive, physiological, and behavioral markers of social anxiety, along with strategies for managing their child’s social anxiety, including preventing avoidance and rewarding non-anxious behavior. Teacher meetings educate teachers about social anxiety and the goals of SASS, obtain information about areas of difficulty for participating students, and enlist their help with potential classroom exposures (e.g., answering questions in class).
School-Based Trials of SASS with Research-Based Providers
To date, SASS has been evaluated in two randomized controlled trials. First, Masia Warner et al. (2005) compared SASS (n = 18) to a waiting-list control group (n = 17) in a sample of 35 adolescents (ages 13–17) with SAD recruited from two urban parochial high schools. SASS groups were co-led by a clinical psychologist and a psychology graduate student. Findings supported the SASS intervention, with 94% of SASS participants classified as responders based on their improved functioning at post-treatment versus only 12% of the control group. Furthermore, 67% of SASS participants, compared to only 6% of controls, no longer met criteria for a diagnosis of SAD at post-intervention. Significantly lower scores were observed for the SASS group at post-treatment and 9-month follow-up with respect to clinician-rated diagnostic severity and adolescent self-reported social anxiety and social avoidance.
In a second controlled trial designed to test the specific efficacy of SASS, Masia Warner et al. (2007) randomly assigned 36 adolescents (ages 14–16) with SAD to either SASS (n = 19) or a credible attention control (n = 17). A group program identical in time and professional attention, the attention control excluded elements related to the core components of SASS (e.g., exposure, social skills), instead focusing on relaxation training and four social events without outgoing peers. Results demonstrated superiority of the SASS condition. Over 82% of SASS participants were responders, compared to 7% of attention-control participants. While all controls still qualified for SAD diagnoses at post-treatment, this was only true for 41% of SASS participants. Students receiving SASS also exhibited significantly lower clinician-rated social anxiety severity and greater overall improvement at posttreatment and 6-month follow-up.
School-Based Trials of SASS with School-Based Providers
With SASS showing efficacy as a school-based treatment for adolescent SAD, attention has turned to examining whether SASS can be delivered effectively by frontline school personnel. In a preliminary study by Miller et al. (2011), teachers implemented a modified version of SASS, which consisted of only two social events and no parent or teacher meetings. Participants included 27 students (ages 13–17) nominated by a variety of sources (teachers, counselors, parents, etc.) due to anxiety-related concerns. SASS groups were co-led by a teacher and a student peer counselor selected by school staff. Program leaders received 6 h of training in the intervention, followed by weekly supervision while delivering the program (e.g., telephone contact with the research team). Results showed initial promise, as participants reported significantly reduced social anxiety symptoms and behavioral avoidance from pre- to post-treatment. Participants also reported satisfaction with the SASS program. Teachers and peer counselors who led the intervention likewise reported a positive experience, though some felt overwhelmed by the amount of information they had to learn.
To provide a robust test of its effectiveness and disseminability to school settings, Masia Warner and colleagues are currently conducting a large, federally-funded randomized controlled trial (RCT) of SASS as led by school guidance counselors (Masia Warner, Ryan, Colognori, Fox, & Herzig, 2011). This study will examine whether school personnel without specialized training in CBT can deliver a cognitive-behavioral intervention with treatment fidelity. Positive findings would underscore the disseminability of SASS and point to a model for promoting evidence-based care for underserved youth with SAD, as well as other mental health disorders.
Cognitive-Behavioral Intervention for Trauma in Schools (CBITS)
Program Overview
Cognitive-Behavioral Intervention for Trauma in Schools (CBITS; Stein et al., 2003) is a school-based group treatment for children and adolescents with previous trauma exposure (excluding sexual abuse) and clinically significant symptoms of PTSD and depression. Treatment components of CBITS include psychoeducation, relaxation skills, adaptive coping skills, cognitive restructuring techniques, graduated imaginal exposure to traumatic memories, processing of traumatic memories, and social problem-solving skills. The program typically consists of 10 one-hour weekly group treatment sessions (five to eight students per group), one to three individual sessions, two optional parent education meetings, and one teacher education meeting (Jaycox, Morse, Tanielian, & Stein, 2006; Stein et al., 2003). Imaginal exposure through writing and drawing is initially conducted in individual sessions and subsequently in the group. The CBITS therapist manual is available for purchase at store.cambiumlearning.com.
School-Based Trials of CBITS with School-Based Providers
As CBITS was designed specifically to be delivered by school-based mental health professionals, no studies have been reported evaluating the treatment as delivered by research-based providers. Two controlled trials, however, have demonstrated the effectiveness of CBITS when implemented by school psychiatric social workers (Kataoka et al., 2003; Stein et al., 2003). Both studies compared CBITS to a waitlist condition in youth with clinically significant PTSD symptoms secondary to exposure to community violence. First, Kataoka and colleagues (2003) examined CBITS in third through eighth graders recently emigrated from Spanish-speaking countries. CBITS was adapted slightly by reducing group sessions from ten to eight and increasing parent sessions, which focused on themes of loss and separation common to immigration, from two to four. Among youth with clinical levels of PTSD symptoms, findings indicated greater reductions at post-treatment for the intervention group (n = 152) compared to the waitlist control (n = 47). Second, Stein and colleagues (2003) found similar results in their evaluation of CBITS in a sample of sixth grade students. At post-treatment and 6-month follow-up, the CBITS group (n = 61) reported significantly lower PTSD symptoms than the waitlist control (n = 65). Treatment fidelity was evaluated by an independent rater on a subset of randomly selected audiotapes for an unknown percentage of group sessions. The mean rating of completion of session-specific intervention components was 96%, and the quality of implementation was classified as “moderate to high.” Taken together, these studies support the effectiveness of CBITS for PTSD symptoms in an urban multicultural population.
The feasibility of CBITS was further supported by a field trial conducted with fourth to eighth grade students in New Orleans 15 months post-Hurricane Katrina (Jaycox et al., 2010). A total of 118 youth with elevated PTSD symptoms were randomized to the school-based CBITS group intervention (n = 58) or to 12 sessions of Trauma-Focused Cognitive-Behavioral Therapy (TF-CBT) with both parent and child at a local community mental health center (n = 60). Both conditions were delivered by therapists trained in the respective treatment, though no information was provided regarding therapist background or treatment fidelity. Youth in both treatments indicated significantly lower PTSD scores at 10-month follow-up, with no significant difference between treatments. Importantly, this study found that CBITS was more feasible for this population, as 98% of youth randomized to CBITS enrolled in treatment versus only 23% of youth assigned to TF-CBT. This underscores the greater ability of school-based treatments to reach and retain distressed youth compared with interventions delivered in traditional mental health settings.
Support for Students Exposed to Trauma (SSET)
To increase its accessibility, the authors of CBITS created Support for Students Exposed to Trauma (SSET), an adaptation of CBITS designed to be implemented by school counselors and teachers (Jaycox, Langley, & Dean, 2009). SSET delivers the cognitive-behavioral components of CBITS in ten 45-min class periods, differing from CBITS due to its lesson plan format and lack of individual and parent meetings. Although SSET is designed to be delivered by school counselors and teachers, the authors strongly recommend having support from a mental health clinician for identifying students appropriate for SSET and addressing any treatment difficulties. The SSET program manual is available for purchase at www.rand.org.
SSET has been evaluated in one study to date. Jaycox, Langley, Stein, and colleagues (2009) compared SSET (n = 39) to a waitlist control (n = 37) in 76 sixth to eighth grade students with moderate levels of PTSD symptoms related to exposure to violence in the past year. Each SSET group was led by either a teacher or a school counselor, who completed a 2-day training with an expert clinician and received weekly or biweekly supervision during the study. Treatment fidelity was measured based on 16% of audiotaped sessions rated by independent evaluators. Ratings suggested that SSET was delivered with high coverage of session components and high quality, defined as strong ability to convey empathy, motivate students, present agendas, and review lessons. Results indicated that the SSET group showed small decreases in self-reported PTSD and depressive symptoms at 3-month follow-up that appeared to be more substantial than the waitlist control. The small sample size, however, resulted in limited statistical power to detect effects. Satisfaction ratings of parents and students involved in the program were high. Although additional studies are needed, these preliminary findings suggest that SSET is an intervention that can be delivered by school personnel to address the sequelae of exposure to violence in youth.
Summary
Findings from studies of five intervention programs suggest that there is promise for delivering EBTs for anxious youth in school settings. School-based treatment trials implemented by research-based providers have demonstrated support for transportability to schools. The evaluation of programs delivered by school-based providers is in its infancy, and drawing conclusions about potential effectiveness would be premature. Integration of interventions into school-based mental health clinics staffed by trained clinicians appears to be a promising approach; the ongoing trial of BCATSS by Ginsburg and colleagues will inform on its benefits. This model, however, may be limited in scope because school-based mental health clinics are few in districts nationwide. Another important avenue is to evaluate the effectiveness of EBT delivery by school counselors (e.g., guidance or student assistance) who are available in schools nationally but lack specialized mental health training (Ryan & Masia Warner, 2012). The current investigation of SASS delivered by school guidance counselors by Masia Warner will highlight the value of this potentially cost-effective approach. Overall, existing studies have failed to collect adequate data on the quality of intervention implementation or on the efficacy of various training models. To advance the dissemination of EBTs to front line school providers, it will be essential to understand factors that influence the effectiveness and sustainability of this approach.
Critical Future Directions
Although previously neglected, treatment fidelity, or the degree to which treatments are implemented as intended, is central to establishing the effectiveness of school-based treatments delivered by frontline school personnel. Used interchangeably with the term treatment integrity, fidelity consists of two main components: adherence, which refers to the application of treatment procedures, and competence, which refers to the therapist’s skill in delivering treatment (Perepletchikova et al., 2009). It is generally assumed, but inconclusively demonstrated, that therapist adherence and competence are related to therapeutic effect (Hogue et al., 2008; Perepletchikova & Kazdin, 2005). Thus, the diminished treatment effects observed in community-based EBTs have often been attributed to reduced treatment fidelity by frontline providers (Weisz, Donenberg, Han, & Weiss, 1995). Demonstrating that school-based personnel, particularly those with less specialized mental health training, can implement EBTs as intended is critical to establishing effectiveness when delivered in a community setting and has been characterized as part of the “next generation of implementation research” (McLeod & Islam, 2011).
Measuring fidelity presents many complex issues, however. Psychometrically sound measures of fidelity are limited, and there are no standard fidelity measures for treatments implemented by school personnel. In addition, an important question is who should rate fidelity. The current gold standard relies on costly independent evaluators, who must have a certain level of familiarity with the EBT in order to rate fidelity. This approach is clearly not feasible for wide-scale dissemination, yet self-ratings from community providers show poor agreement with independent observers (Carroll et al., 2000). Therefore, the development of reliable and valid measures and procedures for monitoring ongoing fidelity in school settings will be essential.
The lack of standardized, validated assessment instruments in this field is partially due to our limited understanding of the critical treatment features. Given that the “active ingredients” of many EBTs have yet to be identified, it is unclear which treatment-specific techniques (e.g., exposure) and nonspecific characteristics (e.g., warmth, timing) warrant monitoring. Thus, fidelity research represents an opportunity to illuminate the most critical elements of EBT delivery by examining links between treatment ingredients and clinical outcomes (Dobson & Singer, 2005; Kazdin & Nock, 2003). Such investigations also have the potential to identify criterion levels of fidelity sufficient for promoting effective treatment delivery to replace the current practice of applying an arbitrary cutoff of 80% (Perepletchikova & Kazdin, 2005).
Improving our understanding of the relationship between fidelity and treatment outcome also has important implications for developing training and supervision approaches that promote high fidelity of EBTs and are still feasible for dissemination (Weisz, Ugueto, Herren, Afienko, & Rutt, 2011). Tailoring training and supervision to emphasize only the most critical treatment components may improve effectiveness while also minimizing costs and resources. Currently, the standard training approach includes a workshop followed by ongoing supervision with an expert. Training workshops alone, while cost-effective, may increase therapist knowledge but do not influence therapist skill or behavior (e.g., Beidas et al., 2009; DeViva, 2006). Ongoing supervision during treatment implementation appears critical to promoting therapist skill acquisition and maintenance (Mannix et al., 2006; Miller, Yahne, Moyers, Martinez, & Pirritano,, 2004; Sholomskas et al., 2005); however, we know little about the parameters of effective supervision. Should training emphasize the conceptual basis of CBT or simply focus on practical teaching of specific treatment techniques? In addition to understanding active ingredients of training and supervision, it will be important to identify the minimum dose necessary for the effective delivery of EBTs (Beidas & Kendall, 2010).
Given that our “gold standard” of weekly supervision of school personnel by experienced clinicians is costly and impractical (Rakovishik & McManus, 2010), finding alternative strategies to maintain skills over time is essential. One option may be pyramid training (e.g., Demchak & Browder, 1990), in which one school personnel would be intensively trained to deliver an EBT for anxious youth and supervise his or her colleagues. However, there is some concern about “watering down” effects with school staff supervised by trained school personnel possibly showing deteriorating implementation fidelity. Another avenue for reducing costs and increasing feasibility may be the utilization of computer software and distance learning. Khanna and Kendall (2008, 2010) have developed a computer-assisted version of Kendall’s Coping Cat program referred to as Camp Cope-A-Lot that has shown feasibility and initial efficacy and may be a practical option for implementation by school personnel. In addition, telemedicine technology (e.g., live teleconferencing) has been initiated for the dissemination of EBTs for other childhood disorders, such as disruptive behavior and autism spectrum disorders (e.g., Funderbunk, Ware, Altshuler, & Chaffin, 2008; Vismara, Young, Stahmer, Griffith, & Rogers, 2009). Additional research will be needed to evaluate these approaches in training frontline school professionals.
Conclusion
School-based programs are considered a promising avenue for addressing the high rates of anxious youth who do not receive treatment. With the efficacy of cognitive-behavioral treatments for anxiety disorders now well documented, recent years have been marked by movement toward enhancing their accessibility through evaluating their transportability and dissemination to school settings. Of the treatments described in this chapter, studies examining their transportability have largely supported their feasibility and effectiveness when delivered in schools by research-based providers, typically specialized psychologists. An increasing number of dissemination studies have begun to test the effectiveness of these treatments when delivered by school-based providers, such as school-based mental health clinicians (e.g., school psychologists and school social workers) and other less specialized school personnel (e.g., school counselors and teachers). However, these studies are fewer in number and have produced mixed evidence, possibly due to the lack of attention to monitoring treatment fidelity. Further research is needed to better understand the link between fidelity and outcome, as well as to evaluate training and supervision models that can promote the effectiveness and sustainability of EBTs in schools. In doing so, these steps will bring us closer to addressing the unmet mental health needs of anxious youth.
References
Barrett, P. M., Dadds, M. R., & Rapee, R. M. (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64, 333–342.
Barrett, P., & Turner, C. (2001). Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. The British Journal of Clinical Psychology, 40, 399–410.
Beidas, R. S., Barmish, A. J., & Kendall, P. C. (2009). Training as usual: Can therapist behavior change after reading a manual and attending a brief workshop on cognitive behavioral therapy for youth anxiety? The Behavior Therapist, 32, 97–101.
Beidas, R. S., & Kendall, P. C. (2010). Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective. Clinical Psychology: Science and Practice, 17, 1–30.
Beidel, D. C., Turner, S. M., & Morris, T. L. (2000). Behavioral treatment of childhood social phobia. Journal of Consulting and Clinical Psychology, 68, 643–650.
Beidel, D. C., Turner, S. M., Young, B., & Paulson, A. (2005). Social effectiveness therapy for children: Three-year follow-up. Journal of Consulting and Clinical Psychology, 73, 721–725.
Bernstein, G. A., Bernat, D. H., Victor, A. M., & Layne, A. E. (2009). School-based interventions for anxious children: 3-, 6-, and 12-month follow-ups. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 1039–1047.
Bernstein, G. A., Layne, A. E., Egan, E. A., & Tennison, D. M. (2005). School-based interventions for anxious children. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 1118–1127.
Bittner, A., Egger, H. L., Erkanli, A., Costello, E. J., Foley, D. L., & Angold, A. (2007). What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry, 48, 1174–1183.
Carroll, K. M., Nich, N., Sifry, R. L., Nuro, K. F., Frankforter, T. L., Ball, S. A., et al. (2000). A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence, 57, 225–238.
Chorpita, B. F. (2008). The frontier of evidence-based practice. In A. Kazdin & J. Weisz (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 42–59). New York: Guilford.
Collins, K. A., Westra, H. A., Dozois, D. J., & Burns, D. D. (2004). Gaps in accessing treatment for anxiety and depression: Challenges for the delivery of care. Clinical Psychology Review, 24, 583–616.
Costello, E. J., Egger, H. L., & Angold, A. (2005). The development epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America, 14, 631–648.
Costello, E., Mustillo, S., Erkanli, A., Keeler, G., & Angold, A. (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60, 837–844.
Dadds, M. R., Holland, D. E., Laurens, K. R., Mullins, M., Barrett, P. M., & Spence, S. H. (1999). Early intervention and prevention of anxiety disorders in children: Results at 2-year follow-up. Journal of Consulting and Clinical Psychology, 67, 145–150.
Dadds, M. R., Spence, S. H., Holland, D. E., Barrett, P. M., & Laurens, K. R. (1997). Prevention and early intervention for anxiety disorders: A controlled trial. Journal of Consulting and Clinical Psychology, 65, 627–635.
Demchak, M., & Browder, D. M. (1990). An evaluation of the pyramid model of staff training in group homes for adults with severe handicaps. Education and Training in Mental Retardation, 25(2), 150–163.
DeViva, J. (2006). The effects of full-day and half-day workshops for health care providers in techniques for increasing resistant clients’ motivation. Professional Psychology: Research and Practice, 37, 83–90.
Dobson, K. S., & Singer, A. R. (2005). Definitional and practical issues in the assessment of treatment integrity. Clinical Psychology: Science and Practice, 12, 384–387.
Evans, S. W. (1999). Mental health services in schools: Utilization, effectiveness and consent. Clinical Psychology Review, 19, 165–178.
Evans, S. W., Langberg, J., & Williams, J. (2003). Achieving generalization in school-based mental health. In M. Weist, S. Evans, & N. Lever (Eds.), Handbook of school mental health: Advancing practice and research (pp. 335–348). New York: Kluwer Academic/Plenum.
Fox, J. K., Halpern, L. F., & Forsyth, J. P. (2008). Mental health checkups for children and adolescents: A means to identify, prevent, and minimize suffering associated with anxiety and mood disorders. Clinical Psychology: Science and Practice, 14, 182–211.
Funderbunk, B. W., Ware, L. M., Altshuler, E., & Chaffin, M. (2008). Use and feasibility of telemedicine technology in the dissemination of parent–child interaction therapy. Child Maltreatment, 13(377), 382.
Ginsburg, G., Becker, K., Kingery, J., & Nichols, T. (2008). Transporting CBT for childhood and anxiety disorders into inner-city school based mental health clinics. Cognitive and Behavioral Practice, 15, 148–158.
Ginsburg, G. S., & Drake, K. L. (2002). School-based treatment for anxious African-American adolescents: A controlled pilot study. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 768–775.
Greenberg, P. E., Sisitsky, T., Kessler, R. C., Finkelstein, S. N., Berndt, E. R., Davidson, J. R., et al. (1999). The economic burden of anxiety disorders in the 1990s. The Journal of Clinical Psychiatry, 60, 427–435.
Grover, R. L., Ginsburg, G. S., & Ialongo, N. (2007). Psychosocial outcomes of anxious first graders: A seven-year follow-up. Depression and Anxiety, 24, 410–420.
Hogue, A., Henderson, C. E., Dauber, S., Barajas, P. C., Fried, A., & Liddle, H. A. (2008). Treatment adherences, competence, and outcome in individual and family therapy for adolescent behavior problems. Journal of Consulting and Clinical Psychology, 76, 544–555.
Hunt, C., Andrews, G., Crino, R., Erksine, A., & Sakashita, C. (2009). Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Australian and Zealand Journal of Psychiatry, 43, 300–304.
Husky, M. M., Sheridan, M., McGuire, L., & Olfson, M. (2011). Mental health screening and follow-up care in public high schools. Journal of the American Academy of Child and Adolescent Psychiatry, 50(9), 881–891.
Jaycox, L. H., Cohen, J. A., Mannarino, A. P., Walker, D. W., Langley, A. K., Gegenheimer, K., et al. (2010). Children’s mental health care following Hurricane Katrina: A field trial of trauma-focused psychotherapies. Journal of Traumatic Stress, 23, 223–231.
Jaycox, L. H., Langley, A. K., & Dean, K. L. (2009). Support for students exposed to trauma: The SSET program: Group leader training manual, lesson plans, and lesson materials and worksheets [electronic version]. Retrieved from www.rand.org/pubs/technical_reports/2009/RAND_TR675.pdf
Jaycox, L. H., Langley, A. K., Stein, B. D., Wong, M., Sharma, P., Scott, M., et al. (2009). Support for students exposed to trauma: A pilot study. School Mental Health, 1, 49–60.
Jaycox, L. H., Morse, L. K., Tanielian, T., & Stein, B. D. (2006). How schools can help students recover from traumatic experiences: A tool kit for supporting long-term recovery [electronic version]. Retrieved from http://www.rand.org/pubs/technical_reports/TR413.html
Kataoka, S., Stein, B. D., Jaycox, L. H., Wong, M., Escudero, P., Tu, W., et al. (2003). A school-based mental health program for traumatized latino immigrant children. Journal of the American Academy of Child and Adolescent Psychiatry, 42(3), 311–318.
Kazdin, A. E., & Nock, M. K. (2003). Delineating mechanism of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44(8), 1116–1129.
Kendall, P. C. (1994). Treating anxiety disorders in children: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 62, 100–110.
Khanna, M. S., & Kendall, P. C. (2008). Computer-assisted CBT for child anxiety: The Coping Cat CD-ROM. Cognitive and Behavioral Practice, 15, 159–165.
Khanna, M. S., & Kendall, P. C. (2010). Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 78(5), 737–745.
Labellarte, M. J., Ginsburg, G. S., Walkup, J. T., & Riddle, M. A. (1999). The treatment of anxiety disorders in children and adolescents. Biological Psychiatry, 46, 1567–1578.
Langley, A. K., Bergman, L., McCracken, J., & Piacentini, J. (2004). Impairment in childhood anxiety disorders: Preliminary examination of the child anxiety Impact scale–parent version. Journal of Child and Adolescent Psychopharmacology, 14, 105–114.
Mannix, K. A., Blackburn, I. M., Garland, A., Gracie, J., Moorey, S., Reid, B., et al. (2006). Effectiveness of brief training in cognitive behaviour therapy techniques for palliative care practitioners. Palliative Medicine, 20, 579–584.
Masia Warner, C., Fisher, P. H., Shrout, P. E., Rathor, S., & Klein, R. G. (2007). Treating adolescents with social anxiety disorder in school: An attention control trial. Journal of Child Psychology and Psychiatry, 48, 676–686.
Masia Warner, C., Klein, R. G., Dent, H. C., Fisher, P. H., Alvir, J., Albano, A. M., et al. (2005). School-based intervention for adolescents with social anxiety disorder: Results of a controlled study. Journal of Abnormal Child Psychology, 33, 707–722.
Masia Warner, C., Nangle, D. W., & Hansen, D. J. (2006). Bringing evidence-based child mental health services to the schools: General issues and specific populations. Education and Treatment of Children, 29, 165–172.
Masia Warner, C., Ryan, J. L., Colognori, D., Fox, J. K., & Herzig, K. (2011, November). Adapting treatment of social anxiety disorder for delivery in schools: Training school counselors to deliver a cognitive-behavioral intervention. In R. Gallagher (Chair), How to keep from getting schooled: Dissemination and implementation of empirically-based programs for children and adolescents in educational settingsnn Symposium presented at the 45th Annual Meeting of the Association for Behavioral and Cognitive Therapies, Toronto, ON.
Masia, C., Beidel, D. C., Albano, A. M., Rapee, R. M., Turner, S. M., Morris, T. L., et al. (1999). Skills for academic and social success. Available from C. Masia Warner, Ph.D., New York University School of Medicine, Child Study Center, 215 Lexington Avenue, 13th floor, New York, 10016.
McLeod, B. D., & Islam, N. Y. (2011). Using treatment integrity models to study the implementation process. Clinical Psychology: Science and Practice, 18, 36–40.
Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., et al. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49, 980–989.
Merikangas, K. R., He, J., Burstein, M., Swendsen, J., Avenevoli, S., Case, B., et al. (2011). Service utilization for lifetime mental disorders in U.S. adolescents: Results from the National Comorbidity Survey-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 50, 32–45.
Mifsud, C., & Rapee, R. M. (2005). Early intervention for childhood anxiety in a school setting: Outcomes for an economically disadvantaged population. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 996–1004.
Miller, L. D., Laye-Gindhu, A., Liu, Y., March, J. S., Thondarson, D. S., & Garland, E. J. (2011). Evaluation of a preventive intervention for child anxiety in two randomized attention-control school trials. Behaviour Research and Therapy, 49, 315–323.
Miller, W. R., Yahne, C. E., Moyers, T. B., Martinez, J., & Pirritano, M. (2004). A randomized trial of methods to help clinicians learn motivational interviewing. Journal of Consulting and Clinical Psychology, 72, 1050–1062.
Owens, P. L., Hoagwood, K., Horwitz, S. M., Leaf, P. J., Poduska, J. M., Kellam, S. G., et al. (2002). Barriers to children’s mental health services. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 731–738.
Perepletchikova, F., Hilt, L. M., Chereji, E., & Kazdin, A. E. (2009). Barriers to implementing treatment integrity procedures: Surveys of treatment outcome researchers. Journal of Consulting and Clinical Psychology, 77, 212–218.
Perepletchikova, F., & Kazdin, A. E. (2005). Treatment integrity and therapeutic chance: Issues and research recommendations. Clinical Psychology: Science and Practice, 12, 365–383.
Rakovishik, S. G., & McManus, F. (2010). Establishing evidence-based training in cognitive behavioral therapy: A review of current empirical findings and theoretical guidance. Clinical Psychology Review, 30(5), 496–516.
Rapee, R. M. (2000). Group treatment of children with anxiety disorders: Outcome and predictors of treatment response. Australian Journal of Psychology, 52, 125–129.
Rice, D. P., & Miller, L. S. (1998). Health economics and cost implications of anxiety and other mental health disorders in the United States. The British Journal of Psychiatry, 173, 4–9.
Roeser, R. W., & Midgley, C. M. (1997). Teachers’ views of aspects of student mental health. The Elementary School Journal, 98, 115–133.
Ryan, J. L., & Masia Warner, C. (2012). Treating adolescents with social anxiety disorder in schools. Child and Adolescent Psychiatric Clinics of North America, 21, 105–118.
Sholomskas, D. E., Syracuse-Siewert, G., Rounsaville, B. J., Ball, S. A., Nuro, K. F., & Carroll, K. M. (2005). We don’t train in vain: A dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology, 73, 106–115.
Shortt, A. L., Barrett, P. M., & Fox, T. L. (2001). Evaluating the FRIENDS program: A cognitive-behavioral group treatment for anxious children and their parents. Journal of Clinical Child Psychology, 30, 525–535.
Silverman, W. K., Kurtines, W. M., Ginsberg, G. S., Weems, C. F., Lumpkin, P. W., & Carmichael, D. H. (1999). Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 67(6), 995–1003.
Stein, B. D., Jaycox, L. H., Kataoka, S. H., Wong, M., Tu, W., Elliott, M. N., et al. (2003). A mental health intervention for schoolchildren exposed to violence: A randomized controlled trial. Journal of the American Medical Association, 290, 603–611.
Vismara, L. A., Young, G. S., Stahmer, A. C., Griffith, E. M., & Rogers, S. J. (2009). Dissemination of evidence-based practice: Can we train therapists from a distance? Journal of Autism and Developmental Disorders, 39, 1636–1651.
Weist, M. D. (1999). Challenges and opportunities in expanded school mental health. Clinical Psychology Review, 19, 131–135.
Weist, M. D., Myers, C. P., Hastings, E., Ghuman, H., & Han, Y. L. (1999). Psychosocial functioning of youth receiving mental health services in the schools versus community mental health centers. Community Mental Health Journal, 35, 69–81.
Weisz, J. R., Donenberg, G. R., Han, S. S., & Weiss, B. (1995). Bridging the gap between laboratory and clinic in child and adolescent psychotherapy. Journal of Consulting and Clinical Psychology, 63(5), 688–701.
Weisz, J. R., Ugueto, A. M., Herren, J., Afienko, S. R., & Rutt, C. (2011). Kernels vs. ears, and other questions for a science of treatment dissemination. Clinical Psychology: Science and Practice, 18, 41–46.
Wren, F. J., Scholle, S. H., Heo, J., & Comer, D. M. (2005). How do primary care clinicians manage childhood mood and anxiety syndromes? International Journal of Psychiatry in Medicine, 35, 1–12.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Fox, J.K., Herzig, K., Colognori, D., Stewart, C.E., Warner, C.M. (2014). School-Based Treatment for Anxiety in Children and Adolescents: New Developments in Transportability and Dissemination. In: Weist, M., Lever, N., Bradshaw, C., Owens, J. (eds) Handbook of School Mental Health. Issues in Clinical Child Psychology. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-7624-5_26
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7624-5_26
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-7623-8
Online ISBN: 978-1-4614-7624-5
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)