Abstract
Pediatric anxiety disorders are common and associated with impairment in academic, social, familial, and personal domains of functioning. The negative effects of excessive anxiety can be ameliorated with effective treatments, which also have been found to improve academic functioning. Unfortunately, most afflicted youth are unidentified and never receive needed interventions. School-based intervention for anxiety can result in improved detection and better generalization of skills and thus represents a promising option for addressing excessive anxiety and disparities in care. A growing literature documents the effectiveness of school-based interventions for students with anxiety. This chapter summarizes and critiques extant literature on school-based interventions for anxiety, with a review organized by categories within a prevention science framework that also align with the multi-tiered system of supports (MTSS) and Response to Intervention (RtI) models (i.e., primary prevention or Tier 1 interventions, secondary prevention or Tier 2 interventions, and tertiary or Tier 3 interventions). Findings reveal mixed support for the effectiveness of school-based interventions for anxiety and highlight a need for enhanced methodological rigor for future studies. In addition to improving the effectiveness of school-based interventions, one important task is to ensure the adoption and sustained use of interventions by school staff. Additional suggestions for future directions are also provided.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pediatric anxiety
- School-based intervention
- Cognitive–behavioral therapy for anxiety
- Universal prevention
- Secondary prevention
Introduction
In a classroom of 30 students, approximately three will meet full criteria for an anxiety disorder and an additional three will experience excessive anxiety that causes impairment in daily functioning (Kessler et al., 2012; Polanczyk et al., 2015; Rapee et al., 2012). The high prevalence of excessive anxiety in youth makes it the most common psychiatric disorder and, according to the Centers for Disease Control, rates of pediatric anxiety disorders are on the rise (Bitsko et al., 2019). Decades of careful research demonstrate that excessive anxiety confers significant impairment across key domains of development such as academic, social, familial, and personal functioning (Swan & Kendall, 2016). Within the academic domain, excessive anxiety has been associated with school absenteeism and school refusal (Kearney & Albano, 2004); deficits in academic performance (Mazzone et al., 2007); grade retention (Stein & Kean, 2000); and early school dropout (Breslau et al., 2008). Importantly, the link between excessive anxiety and poor academic outcomes is both concurrent and prospective (Woodward & Fergusson, 2001).
Fortunately, the negative effects of anxiety can be ameliorated with effective treatment. Evidence from meta-analyses and systematic reviews indicates that cognitive–behavioral therapy (CBT) and medication are two effective treatments for pediatric anxiety (Ipser et al., 2009; James et al., 2018). Importantly, these treatments have also been found to improve academic functioning including higher academic motivation and performance on standardized tests, increases in grade point average (GPA), and improved classroom behavior such as test taking, reading in class, and homework completion (Nail et al., 2015; Sanchez et al., 2019; Weems et al., 2009).
Rationale for School-Based Interventions for Anxiety
Despite the high prevalence, documented impairment, and effective treatment of pediatric anxiety disorders, most afflicted youth are unidentified and never receive needed interventions (Merikangas et al., 2011). Reasons for under-identification and low service utilization in outpatient settings are numerous and include pragmatic barriers (e.g., costs, transportation, limited time, lack of access to providers) as well as psychological barriers such as stigma and concerns about confidentiality (Gulliver et al., 2010).
To address these barriers, efforts at the national and state levels have advocated providing psychosocial interventions to youth in the school setting. The advantages of providing interventions in schools are numerous and include early and improved detection and better generalization of therapy skills. For instance, school-based clinicians can facilitate the application of coping skills in anxiety-provoking situations in real time and in ways that are not accessible to outpatient community therapists. Finally, school-based interventions improve access to care, do not require out-of-pocket payments, and reduce barriers associated with transportation. Elimination of these barriers is particularly relevant for historically underserved student groups, as a substantial body of evidence indicates that racial/ethnic minorities and lesbian, gay, bisexual, transgender, and queer/questioning (LGBTQ) youth are significantly less likely to seek or receive mental health services than their non-minority peers (Cummings & Druss, 2011; Garland et al., 2005; Su et al., 2016). Accessing mental health services in school therefore presents a promising option for addressing these disparities.
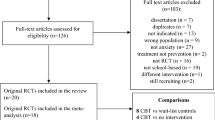
Recognizing these advantages, a growing literature now documents the effectiveness of school-based interventions for students with anxiety. In the following sections, we summarize this literature by first presenting data from recent reviews and meta-analyses on school-based interventions. Subsequently, we review a selected set of randomized controlled trials (RCTs) of school-based interventions for anxiety organized by categories within a prevention science framework that also align with the multi-tiered system of supports (MTSS) and Response to Intervention (RtI) models (Gamm et al., 2012; Sugai & Horner, 2009). Specifically, primary prevention models (also referred to as universal or Tier 1 interventions) represent those interventions that are delivered to all students in a classroom or an entire school. Secondary prevention models (which include selective and indicated or Tier 2 interventions) are delivered to students who are at risk for disorder onset or show elevated anxiety symptoms. Finally, tertiary models (similar to Tier 3 interventions) are treatments for students meeting criteria for an anxiety disorder.
Effectiveness of School-Based Interventions for Anxiety
Several meta-analyses and qualitative reviews have been published describing the effectiveness of school-based psychosocial interventions for internalizing problems including anxiety (Caldwell et al., 2019; Gee et al., 2020; Hugh-Jones et al., 2021; Sanchez et al., 2018; Werner-Seidler et al., 2017). Sanchez et al. (2018) reviewed school-based mental health interventions exclusively in elementary-aged children across symptom domains of internalizing, externalizing, and attention problems. With respect to interventions for internalizing problems (including anxiety), a small effect size was found (Hedge’s g = 0.30; SE = 0.07; 95% CI = 0.16–0.43) across all interventions. Gee and colleagues reviewed 45 studies of school-based interventions for adolescents with elevated depression or anxiety symptoms across all intervention models (primary, secondary, and tertiary), and found the standardized mean difference of interventions versus control groups at post-intervention was modest (0.52; 95% CI = −0.85 to −0.18; p = 0.003; k = 13). Subgroup analyses generally did not yield significant differences in effect size based on study characteristics. In the most recent review, Hugh-Jones et al. (2021) conducted a meta-analysis of 18 studies focused exclusively on indicated interventions for youth with elevated anxiety. Small but significant positive intervention effects compared to control groups were found at post-test (g = −0.28; 95% CI = −0.50 to −0.05), with maintenance of benefit identified at 6- and 12-month follow-ups. Subgroup analyses based on theoretical orientation (i.e., CBT or other), child age, and delivery agent (e.g., teacher or research personnel) were not possible due to small sample sizes, but type of control group (i.e., waitlist vs. attention control vs. no intervention) was not found to significantly impact treatment effects (Hugh-Jones et al., 2021).
Across studies in these reviews, the magnitude of intervention effects varied widely—likely attributable to differences in the provider of the intervention (i.e., research staff vs. school personnel), extent of provider training and ongoing coaching, level of adherence/fidelity to intervention protocols, length and duration of intervention, inclusion of parental involvement, inclusion criteria (e.g., initial severity of anxiety symptoms, comorbid disorders), assessment strategies (assessor, specific measures, and timepoints), and other key study design characteristics (control group, primary outcome). One important conclusion was that the methodological quality of studies was uniformly low, suggesting a significant need for improvement with respect to trial design and intervention implementation.
Compared to studies conducted in outpatient research settings, school-based interventions show smaller effect sizes. For instance, a meta-analysis of outpatient treatment trials indicates effect sizes ranging from 0.65 to 0.94 (James et al., 2018). Reasons for these larger effects likely reflect differences in efficacy versus effectiveness RCTs (and similar to reasons for variations within school-based treatment trials), where efficacy studies use highly trained mental health specialists who receive ongoing supervision, deliver a higher dosage of treatment, have stricter inclusion/exclusion criteria (e.g., limited comorbidity), and incorporate greater parental involvement in treatment.
Below we highlight a representative sample of school-based interventions for anxietyFootnote 1 across each of the three levels of intervention models (primary, secondary, and tertiary); readers are referred to the meta-analyses referenced above for a more comprehensive analysis. Key features of selected studies focused on anxiety are highlighted in Tables 3.1, 3.2, and 3.3. In light of the number of interventions based on CBT, Table 3.4 outlines the core therapeutic ingredients of this model used in school-based interventions.
Primary Prevention (Universal Interventions)
Several randomized controlled trials (RCTs) have evaluated the impact of universal interventions delivered to entire classrooms or schools. The 11 universal interventions in Table 3.1 span from preschool-aged children to adolescents in high school, with a majority (7 studies) focusing on middle childhood. Given that interventions were delivered universally, sample sizes were generally large, ranging from 100 to over 900 (Miller et al., 2010; Rooney et al., 2013). In terms of structure, most, but not all, universal interventions were provided in 1-h sessions administered on a weekly basis for a total number of sessions ranging from 3 to 30. Some universal interventions were quite brief, including one program administered in three 45-min classroom sessions (Aune & Stiles, 2009), whereas another intervention was delivered in a much smaller dosage (less than 15 min) daily for 6 weeks (Britton et al., 2014).
With regard to theoretical orientation, cognitive–behavioral approaches were the most common (core strategies described in Table 3.4); however, 3 of the 11 universal studies utilized mindfulness-based or positive psychology approaches (Britton et al., 2014; Burckhardt et al., 2015; van de Weijer-Bergsma et al., 2014) that were delivered with greater frequency for shorter duration, ranging from daily to biweekly.
Because universal interventions are delivered to all students in a school or classroom, many of these protocols were delivered at least in part by regular classroom teachers rather than research staff (e.g., licensed psychologists, graduate students). One computer-based study was evaluated that involved students logging time on a website delivering intervention content, with teachers observing and facilitating (Burckhardt et al., 2015). In cases where mainstream classroom teachers administered interventions, training most often took the form of one-day workshops led by research staff (Anticich et al., 2013; Barrett & Turner, 2001; Miller et al., 2010; Rooney et al., 2013).
Intervention effects reported in these universal interventions were variable. Five of the 11 studies reported statistically significant improvement in anxiety symptoms from baseline to post or follow-up evaluations for intervention groups as compared to waitlist, no treatment, or active control groups (Anticich et al., 2013; Aune & Stiles, 2009; Barrett & Turner, 2001; Essau et al., 2012; Keogh et al., 2006). Four of these five studies used manualized CBT-based protocols delivered by research staff (e.g., graduate students or licensed clinical psychologists) as opposed to classroom teachers. Despite the setting for these studies, few evaluated the impact of interventions on academic performance. In one notable exception, Keogh et al. (2006) evaluated a universal stress management intervention among adolescents in the United Kingdom preparing for a nationally administered standardized exam, finding that participants receiving the intervention performed, on average, one letter grade better than their peers in a no-intervention control group.
Six of the studies in Table 3.1 evaluating universal interventions failed to find evidence of efficacy of the intervention over comparison conditions. Two studies evaluating the effects of the Aussie Optimism Program-Positive Thinking Skills (AOP-PTS) as delivered by classroom teachers failed to outperform no-intervention control groups (Johnstone et al., 2014; Rooney et al., 2013), and a third CBT-based, teacher-delivered intervention produced similar results when compared to a waitlist (Miller et al., 2010). Mindfulness and positive psychology-based interventions also demonstrated non-significant effects when compared to active controls (Britton et al., 2014), attention controls (Burckhardt et al., 2015), and waitlist controls (van de Weijer-Bergsma et al., 2014). Four of these six interventions were delivered by teachers, while one was a computer-based intervention. Notably, one study directly compared differences in intervention effects (using the FRIENDS intervention) when delivered by psychologists versus teachers (Barrett & Turner, 2001). Results indicated significant reductions in children’s self-reported anxiety scores from pre- to post-intervention relative to a monitoring-only control group for both teacher-delivered and psychologist-delivered CBT, which did not differ from each other. Notably, teachers delivering the intervention were supervised by postgraduate psychologists for 25% of their sessions, which may account in part for the positive findings.
Taken together, evidence reviewed on primary prevention/universal interventions is mixed. Reporting of effect sizes was rare, but the magnitude of change on anxiety symptoms (based also on meta-analyses) suggests a small but significant positive effect size in at least half of the studies. Studies failing to find a significant impact on student anxiety were more likely to be delivered by teachers (rather than researchers or mental health specialists) and relied on mindfulness/positive psychology approaches (rather than CBT).
Secondary Prevention (Selective and Indicated) Interventions
Interventions reviewed in this section reflect those targeting youth who are at risk for developing a disorder and/or have elevated symptoms of anxiety. Though some studies required that participants simply experience above-average levels of anxiety (e.g., Cooley-Strickland et al., 2011), other studies stipulated that participants demonstrate anxiety symptom scores at or above the 75th–90th percentiles as compared to their same-age peers (e.g., Balle & Tortella-Feliu, 2010; McLoone & Rapee, 2012; Mifsud & Rapee, 2005; Sportel et al., 2013). Anxiety symptoms were typically measured by widely used standardized questionnaires with well-established psychometrics, such as the Screen for Child Anxiety Related Disorders (SCARED; Birmaher et al., 1997), the Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1979), or the Multidimensional Anxiety Scale for Children (MASC; March et al., 1997).
Of the 11 studies highlighted in Table 3.2, 10 evaluated manualized CBT interventions. Studies evaluating the FRIENDS program (total of four; delivered by research staff, school clinicians, and teachers) failed to find an intervention effect over waitlist or attention control conditions. In contrast, all four studies that evaluated the Cool Kids intervention demonstrated superior intervention effects compared to waitlist and/or active intervention controls. No clear trends were evident to separate the two interventions with regard to content, number of sessions, intervention training, or intervention fidelity/integrity. In fact, a recent study using data from a Cool Kids RCT found that intervention adherence and competence did not predict improvement in anxiety, although adherence and competence were greater for brief (as compared to full-length) intervention protocols (Husabo et al., 2022). One potential explanation for the superiority of Cool Kids over FRIENDS may be the variation in inclusion criteria. The majority of Cool Kids studies represented in Table 3.2 included youth with anxiety scores above the 75th–90th percentiles, or with “elevated anxiety and interference” (Haugland et al., 2020; McLoone & Rapee, 2012; Misfud & Rapee, 2005), whereas FRIENDS studies often included youth with milder elevations, such as T-scores that are simply above average (e.g., Cooley-Strickland et al., 2011; Miller et al., 2011). The inclusion of more severely affected youth in Cool Kids may increase the likelihood of improvement, either via treatment effects or spontaneous remission. As with universal interventions, collection of data on academic outcomes was rare, with no studies explicitly reporting on academic performance or other school outcomes.
In an attempt to broaden the network of school-based providers who can assist students with anxiety, Ginsburg and colleagues have developed brief teacher and school-nurse CBT-based interventions (Piselli et al., 2021; Ginsburg et al., 2019). The school nurse intervention called Child Anxiety Learning Modules (CALM; Drake et al., 2015) includes similar CBT principles to those used in FRIENDS and Cool Kids, but with the crucial distinction that CALM is designed to be delivered by school nurses, who may be particularly well-suited to this task given that students with anxiety frequently visit the school nurse with somatic symptoms. A pilot RCT (summarized in Table 3.2) compared the CALM intervention to a relaxation skills-only curriculum (CALM-R). Results indicated that both CALM and CALM-R participants demonstrated significant clinical improvements as measured by interviews conducted by masked independent evaluators (IEs). Within-group effect sizes for key outcomes for CALM were moderate to large, ranging from Cohen’s d = 0.55–1.74 (Ginsburg et al., 2019).
Two non-CBT interventions explored the effects of cognitive bias modification training (CBM; Fitzgerald et al., 2016; Sportel et al., 2013). CBM aims to address anxiety symptoms by using computer-based tasks to modify negative or threatening attention biases that are often present in individuals with elevated anxiety (Notebaert et al., 2015). Both studies failed to demonstrate significant intervention effects for CBM compared to both a placebo computer task (Fitzgerald et al., 2016) and a traditional CBT protocol (Sportel et al., 2013). The latter of these studies indicated no significant difference between CBM and a no-intervention control condition. Thus, although CBM-based interventions are time-efficient and obviate challenges associated with training teachers, school nurses, or counselors, there is currently limited evidence to support their use in school settings. The use of technology as an intervention aid has shown more promising evidence when used to adapt or support implementation of CBT protocols (Storch et al., 2015).
In summary, the majority of secondary interventions are based on CBT, and of those that led to significant reductions in student anxiety (e.g., Cool Kids, CALM), effect sizes ranged from moderate to large (Cohen’s d = 0.34–2.7). Future research is needed to clarify why similar CBT protocols fail to have a similar impact on anxiety and the impact of these interventions on academic outcomes should be prioritized.
Tertiary Interventions
A summary of ten school-based RCTs of treatments for youth with anxiety disorders appears in Table 3.3. Interventions were delivered in elementary through high schools and targeted youth with social anxiety disorder exclusively (Masia-Warner et al., 2016) or with a broad range of primary anxiety disorders (e.g., Ginsburg et al., 2020). Study sample sizes ranged from small (N < 50) to moderate (N = 216; Ginsburg et al., 2020). Treatments evaluated in these studies were based on cognitive and/or behavioral interventions and were delivered using both group and individual formats. The length of treatments ranged from 10 to 12 student meetings (and some included parent and teacher meetings; see Table 3.3). In the majority of studies, research staff delivered the treatments, though there are three notable exceptions (Ginsburg et al., 2012, 2020; Masia-Warner et al., 2016) where treatments were delivered by school counselors. Only half of the studies used an active comparison condition (vs. a no-treatment control condition).
Among the smaller RCTs, CBT was generally compared to a waitlist control condition and results indicate that youth receiving CBT experienced a more positive response relative to those in the waitlist control condition (e.g., Bernstein et al., 2005; Chiu et al., 2013; Masia-Warner et al., 2005). Among studies that compared school-based CBT to an active control condition, and/or used non-CBT experts to administer the interventions (Ginsburg et al., 2020; Masia-Warner et al., 2016), findings were mixed. Masia-Warner et al. (2016) evaluated a 12-week group-based intervention (i.e., Skills for Academic and Social Success; SASS) for adolescents with social anxiety disorder (SOP). In this study, 138 adolescents were randomized to: (a) SASS delivered by school counselors (C-SASS), (b) SASS delivered by doctoral-level psychologists (P-SASS), or (c) a control condition, Skills for Life (SFL), a non-specific counseling program. School clinicians received didactic training, co-led their first therapy group with a study expert, and received 40 min of weekly supervision for all future groups. Independent evaluators (IEs) completed post-intervention assessments. At post-treatment and follow-up, respectively, between 21% and 39% of youth in C-/P-SASS no longer met diagnostic criteria for SOP compared to 7% and 11% in the control condition, a statistically significant difference. There were no significant differences between SASS delivered by school counselors and research staff psychologists. The authors concluded that with extensive training and ongoing supervision, school counselors can deliver evidence-based treatments with equal success as trained mental health specialists.
In contrast, two studies by Ginsburg and colleagues (2012, 2020) found similar outcomes for students receiving CBT and treatment as usual (TAU). For instance, in a large school-based study, a modular CBT was compared to treatment as usual (TAU) delivered by school-based clinicians in youth (N = 216) aged 6–18 years meeting Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for a broad range of primary anxiety disorders. Clinicians received one day of training in anxiety disorders, the CBT model and intervention modules, and study procedures, and were provided with treatment materials (e.g., treatment manual, handouts). Supervision was offered but not mandatory. Based on intent-to-treat analyses, youth in both treatment groups improved; however, no treatment group differences were found on most of the clinical outcomes measured at post-treatment or follow-up.
In summary, school-based treatments for students with anxiety disorders were based on cognitive–behavioral strategies. In most studies, the treatments were delivered by research staff and led to significant reductions in anxiety when compared to waitlist (i.e., no-treatment control conditions). However, in the three studies where treatment was delivered by school staff and compared to an active comparison condition (TAU, SFL), only one revealed that the experimental treatment was superior to the comparison condition, likely due to extensive training and continuous supervision provided by the research team, which possibly enhanced adherence and quality of treatment delivery. The feasibility and costs associated with training and ongoing supervision pose important practical barriers to large-scale adoption of school-based treatments. Studies demonstrating cost-effectiveness and impact on academic outcomes are needed.
Future Directions
Providing school-based interventions for students with impairing anxiety holds the promise of broadening access to services for a population that is under-identified and under-treated. As reviewed in this chapter, growing numbers of anxiety reduction interventions have been evaluated in elementary, middle, and high school settings and several have been shown to be effective in lowering anxiety severity, though the magnitude of effects is modest and inconsistent.
Despite the rise in the number of school-based interventions for students with anxiety, numerous gaps in this literature remain. Most importantly, research is needed to identify ways of enhancing intervention effectiveness. Related, sustainable methods of intervention delivery (i.e., researchers vs. school staff) and the examination of treatment durability are needed. Research methods must increase in rigor as the majority of studies are described in extant meta-analyses as “low in quality,” failing to use gold standard designs and methods, which are barriers to drawing clear conclusions from published studies. Future work should also include analysis of academic outcomes. Finally, as schools operate within changing fiscal contexts, data are needed to evaluate the cost-effectiveness and cost benefits of school-based interventions.
Another gap in current knowledge regarding the effectiveness of school-based services for students with anxiety is identifying for whom these services work best—both within and across each model of intervention (primary, secondary, tertiary). Indeed, few published studies examined predictors, moderators, or mediators of intervention response. These analyses are not only needed to enhance student outcomes but can also be used to refine intervention components and delivery methods. In one recent study, youth with the highest level of anxiety did better in CBT compared to TAU (Ginsburg et al., 2020). Additionally, Keogh et al. (2006) conducted a mediation analysis in an attempt to identify mechanisms of change in a cognitive–behavioral stress management program. Results indicated that changes in dysfunctional attitudes fully mediated the effects of the treatment program on academic performance and mental health (Keogh et al., 2006). The mixed outcomes noted in extant work on school-based interventions also speak to a need for future work to build on these initial attempts to identify mediators and moderators of effective treatment. Attention to the components of current interventions (e.g., number of sessions, session content) is also a fruitful area of future research. For instance, most current interventions range from 10 to 15 meetings. However, recent data on shorter (even single session) interventions (Schleider et al., 2020) deserve evaluation. The use of technology-delivered interventions, used as a stand-alone intervention or to augment in-person interventions, has shown promise in outpatient settings (Storch et al., 2015) and is also another productive area of research. Online interventions may also be cost-effective, require less training of school staff, and enhance student outcomes.
Across all areas of future study, improvements in methodological rigor are essential. Specifically, needed improvements include: (1) the use of appropriate control conditions (e.g., active control conditions rather than exclusively using waitlist controls), (2) the inclusion of assessments of adverse events, intervention adherence and acceptability, and school outcomes (e.g., classroom behavior, attendance, engagement), (3) the use of masked evaluators rather than child reports only, and (4) designs that assess the durability of intervention effects by including a long-term follow-up.
Conclusions
Anxiety is a highly prevalent and impairing condition that often goes under-identified and under-treated. Fortunately, a growing literature has emerged evaluating a broad range of school-based anxiety interventions. Findings from extant reviews, meta-analyses, and individual studies reveal mixed support for the effectiveness of school-based interventions for anxiety and highlight a need for enhanced methodological rigor for future studies. In addition to improving the effectiveness of school-based interventions, one important task is to ensure the adoption and sustained use of interventions by school staff. Several studies have begun to address this issue by training teachers, nurses, and counselors to deliver anxiety-reduction interventions. Masia-Warner et al. (2016) showed that with intensive training, school counselors delivered a targeted intervention to students with SOP with fidelity and outcomes of students receiving the intervention from school staff compared to research staff were similar. In another study comparing treatment effects by provider, Barrett and Turner (2001) identified no significant differences in anxiety reduction between psychologist-delivered and teacher-delivered FRIENDS. Finally, Ginsburg et al. (2019) trained school nurses to deliver a brief CBT intervention for students with anxiety with preliminary results showing significant reductions in anxiety. Each of these findings provides support for an ultimate shift toward intervention delivery by school-based providers rather than external research teams. Systematic research on the optimal training model for these school-based providers is viewed as a critical next step to ensuring all students with anxiety receive the interventions they need.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author.
Anticich, S. A. J., Barrett, P. M., Silverman, W., Lacherez, P., & Gillies, R. (2013). The prevention of childhood anxiety and promotion of resilience among preschool-aged children: A universal school based trial. Advances in School Mental Health Promotion, 6(2), 93–121. https://doi.org/10.1080/1754730X.2013.784616
Aune, T., & Stiles, T. C. (2009). Universal-based prevention of syndromal and subsyndromal social anxiety: A randomized controlled study. Journal of Consulting and Clinical Psychology, 77(5), 867–879. https://doi.org/10.1037/a0015813
Balle, M., & Tortella-Feliu, M. (2010). Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety, Stress and Coping, 23(1), 71–85. https://doi.org/10.1080/10615800802590652
Barrett, P., & Turner, C. (2001). Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. The British Journal of Clinical Psychology, 40(4), 399–410. https://doi.org/10.1348/014466501163887
Bernstein, G. A., Layne, A. E., Egan, E. A., & Tennison, D. M. (2005). School-based interventions for anxious children. Journal of the American Academy of Child & Adolescent Psychiatry, 44(11), 1118–1127. https://doi.org/10.1038/jid.2014.371
Berry, K., & Hunt, C. J. (2009). Evaluation of an intervention program for anxious adolescent boys who are bullied at school. Journal of Adolescent Health, 45(4), 376–382. https://doi.org/10.1016/j.jadohealth.2009.04.023
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., & Neer, S. M. (1997). The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 545–553. https://doi.org/10.1097/00004583-199704000-00018
Bitsko, R. H., Holbrook, J. R., Ghandour, R. M., Blumberg, S. J., Visser, S. N., Perou, R., & Walkup, J. T. (2019). Epidemiology and impact of health care provider-diagnosed anxiety and depression among US children. Journal of Developmental and Behavioral Pediatrics, 39(5), 395–403. https://doi.org/10.1097/DBP.0000000000000571
Breslau, J., Lane, M., Sampson, N., & Kessler, R. C. (2008). Mental disorders and subsequent educational attainment in a US national sample. Journal of Psychiatric Research, 42(9), 708–716. https://doi.org/10.1016/j.jpsychires.2008.01.016
Britton, W. B., Lepp, N. E., Niles, H. F., Rocha, T., Fisher, N. E., & Gold, J. S. (2014). A randomized controlled pilot trial of classroom-based mindfulness meditation compared to an active control condition in sixth-grade children. Journal of School Psychology, 52(3), 263–278. https://doi.org/10.1016/j.jsp.2014.03.002
Burckhardt, R., Manicavasagar, V., Batterham, P. J., Miller, L. M., Talbot, E., & Lum, A. (2015). A web-based adolescent positive psychology program in schools: Randomized controlled trial. Journal of Medical Internet Research, 17(7). https://doi.org/10.2196/jmir.4329
Caldwell, D. M., Davies, S. R., Hetrick, S. E., Palmer, J. C., Caro, P., López-López, J. A., Gunnell, D., Kidger, J., Thomas, J., French, C., Stockings, E., Campbell, R., & Welton, N. J. (2019). School-based interventions to prevent anxiety and depression in children and young people: A systematic review and network meta-analysis. The Lancet Psychiatry, 6(12), 1011–1020. https://doi.org/10.1016/S2215-0366(19)30403-1
Chiu, A. W., Lagner, D. A., McLeod, B. D., Har, K., Drahota, A., Galla, B. M., Jacobs, J., Ifekwunigwe, M., & Wood, J. J. (2013). Effectiveness of modular CBT for child anxiety in elementary schools. School Psychology Quarterly, 28(2), 141–153. https://doi.org/10.1037/spq0000017
Chu, B. C., Crocco, S. T., Esseling, P., Areizaga, M. J., Lindner, A. M., & Skriner, L. C. (2016). Transdiagnostic group behavioral activation and exposure therapy for youth anxiety and depression: Initial randomized controlled trial. Behaviour Research and Therapy, 76, 65–75. https://doi.org/10.1016/j.brat.2015.11.005
Cooley-Strickland, M. R., Griffin, R. S., Darney, D., Otte, K., & Ko, J. (2011). Urban African-American youth exposed to community violence: A school-based anxiety preventive intervention efficacy study. Journal of Prevention & Intervention in the Community, 39(2), 149–166. https://doi.org/10.1080/10852352.2011.556573
Cummings, J. R., & Druss, B. G. (2011). Racial/ethnic differences in mental health service use among adolescents with major depression. Journal of the American Academy of Child and Adolescent Psychiatry, 50(2), 160–170. https://doi.org/10.1016/j.jaac.2010.11.004
Dadds, R. M., & Spence, S. H. (1997). Prevention and early intervention for anxiety: A controlled trial. Journal of Counseling and Clinical Psychology, 64(4), 627–635. https://doi.org/10.1037/0022-006X.65.4.627
Drake, K. L., Stewart, C. E., Muggeo, M. A., & Ginsburg, G. S. (2015). Enhancing the capacity of school nurses to reduce excessive anxiety in children: Development of the CALM intervention. Journal of Child and Adolescent Psychiatric Nursing, 28(3), 121–130. https://doi.org/10.1111/jcap.12115
Essau, C. A., Conradt, J., Sasagawa, S., & Ollendick, T. H. (2012). Prevention of anxiety symptoms in children: Results from a universal school-based trial. Behavior Therapy, 43(2), 450–464. https://doi.org/10.1016/j.beth.2011.08.003
Fitzgerald, A., Rawdon, C., & Dooley, B. (2016). A randomized controlled trial of attention bias modification training for socially anxious adolescents. Behaviour Research and Therapy, 84, 1–8. https://doi.org/10.1016/j.brat.2016.06.003
Gamm, S., Elliott, J., Wright Halbert, J., Price-Baugh, R., Hall, R., Walston, D., et al. (2012). Common core state standards and diverse urban students: Using multi-tiered systems of support. Council of the Great City Schools.
Garland, A. F., Lau, A. S., Yeh, M., McCabe, K. M., Hough, R. L., & Landsverk, J. A. (2005). Racial and ethnic differences in utilization of mental health services among high-risk youths. The American Journal of Psychiatry, 162(7), 1336–1343. https://doi.org/10.1176/appi.ajp.162.7.1336
Gee, B., Reynolds, S., Carroll, B., Orchard, F., Clarke, T., Martin, D., Wilson, J., & Pass, L. (2020). Practitioner review: Effectiveness of indicated school-based interventions for adolescent depression and anxiety—A meta-analytic review. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 61(7), 739–756. https://doi.org/10.1111/jcpp.13209
Ginsburg, G. S., & Drake, K. L. (2002). School-based treatment for anxious African-American adolescents: A controlled pilot study. Journal of the American Academy of Child and Adolescent Psychiatry, 41(7), 768–775. https://doi.org/10.1097/00004583-200207000-00007
Ginsburg, G. S., Becker, K. D., Drazdowski, T. K., & Tein, J.-Y. (2012). Treating anxiety disorders in inner city schools: Results from a pilot randomized controlled trial comparing CBT and usual care. Child & Youth Care Forum, 41(1), 1–19. https://doi.org/10.1007/s10566-011-9156-4.Treating
Ginsburg, G. S., Drake, K. L., Muggeo, M. A., Stewart, C. E., Pikulski, P. J., Zheng, D., & Harel, O. (2019). A pilot RCT of a school nurse delivered intervention to reduce student anxiety. Journal of Clinical Child and Adolescent Psychology, 00(00), 1–10. https://doi.org/10.1080/15374416.2019.1630833
Ginsburg, G. S., Pella, J. E., Pikulski, P. J., Tein, J. Y., & Drake, K. L. (2020). School-based treatment for anxiety research study (STARS): A randomized controlled effectiveness trial. Journal of Abnormal Child Psychology, 48, 407–417. https://doi.org/10.1007/s10802-019-00596-5
Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10(1), 113. https://doi.org/10.1186/1471-244X-10-113
Haugland, B., Haaland, Å. T., Baste, V., Bjaastad, J. F., Hoffart, A., Rapee, R. M., Raknes, S., Himle, J. A., Husabø, E., & Wergeland, G. J. (2020). Effectiveness of brief and standard school-based cognitive-behavioral interventions for adolescents with anxiety: A randomized noninferiority study. Journal of the American Academy of Child and Adolescent Psychiatry, 59(4), 552–564.e2. https://doi.org/10.1016/j.jaac.2019.12.003
Hugh-Jones, S., Beckett, S., Tumelty, E., & Mallikarjun, P. (2021). Indicated prevention interventions for anxiety in children and adolescents: A review and meta-analysis of school-based programs. European Child & Adolescent Psychiatry, 30(6), 849–860. https://doi.org/10.1007/s00787-020-01564-x
Hunt, C., Andrews, G., Crino, R., & Erskine, C. (2009). Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Australian and New Zealand Journal of Psychiatry, 43, 300–304.
Husabo, E., Haugland, B. S., McLeod, B. D., Baste, V., Haaland, Å. T., Bjaastad, J. F., ... & Wergeland, G. J.(2022). Treatment fidelity in brief versus standard-length school-based interventions for youth with anxiety. SchoolMental Health, 14(1), 49–62.
Ipser, J. C., Stein, D. J., Hawkridge, S., & Hoppe, L. (2009). Pharmacotherapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews, 2009(3), CD005170. https://doi.org/10.1002/14651858.CD005170.pub2
James, A. C., Reardon, T., Soler, A., James, G., & Creswell, C. (2018). Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews, 2018(10). https://doi.org/10.1002/14651858.CD013162
Johnstone, J., Rooney, R. M., Hassan, S., & Kane, R. T. (2014). Prevention of depression and anxiety symptoms in adolescents: 42 and 54 months follow-up of the Aussie optimism program-positive thinking skills. Frontiers in Psychology, 5(MAY), 1–10. https://doi.org/10.3389/fpsyg.2014.00364
Kearney, C. A., & Albano, A. M. (2004). The functional profiles of school refusal behavior: Diagnostic aspects. Behavior Modification, 28(1), 147–161. https://doi.org/10.1177/0145445503259263
Keogh, E., Bond, F. W., & Flaxman, P. E. (2006). Improving academic performance and mental health through a stress management intervention: Outcomes and mediators of change. Behaviour Research and Therapy, 44(3), 339–357. https://doi.org/10.1016/j.brat.2005.03.002
Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslansky, A. M., & Wittchen, H. U. (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. https://doi.org/10.1002/mpr.1359
March, J. S., Parker, J., Sullivan, K., et al. (1997). The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 554–565. https://doi.org/10.1097/00004583-199704000-00019
Masia-Warner, C., Klein, R. G., Dent, H. C., Fisher, P. H., Alvir, J., Albano, A. M., & Guardino, M. (2005). School-based intervention for adolescents with social anxiety disorder: Results of a controlled study. Journal of Abnormal Child Psychology, 33(6), 707–722. https://doi.org/10.1007/s10802-005-7649-z
Masia-Warner, C., Fisher, P. H., Shrout, P. E., Rathor, S., & Klein, R. G. (2007). Treating adolescents with social anxiety disorder in school: An attention control trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 48(7), 676–686. https://doi.org/10.1111/j.1469-7610.2007.01737.x
Masia-Warner, C., Colognori, D., Brice, C., Herzig, K., Mufson, L., Lynch, C., Reiss, P. T., Petkova, E., Fox, J., Moceri, D. C., Ryan, J., & Klein, R. G. (2016). Can school counselors deliver cognitive-behavioral treatment for social anxiety effectively? A randomized controlled trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 57(11), 1229–1238. https://doi.org/10.1111/jcpp.12550
Mazzone, L., Ducci, F., Scoto, M. C., Passaniti, E., D’Arrigo, V. G., & Vitiello, B. (2007). The role of anxiety symptoms in school performance in a community sample of children and adolescents. BMC Public Health, 7, 1–6. https://doi.org/10.1186/1471-2458-7-347
McLoone, J. K., & Rapee, R. M. (2012). Comparison of an anxiety management program for children implemented at home and school: Lessons learned. School Mental Health, 4(4), 231–242. https://doi.org/10.1007/s12310-012-9088-7
Merikangas, K. R., He, J. P., Burstein, M., Swendsen, J., Avenevoli, S., Case, B., Georgiades, K., Heaton, L., Swanson, S., & Olfson, M. (2011). Service utilization for lifetime mental disorders in U.S. adolescents: Results of the national comorbidity survey. (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 50(1), 32–45. https://doi.org/10.1016/j.jaac.2010.10.006
Mifsud, C., & Rapee, R. M. (2005). Early intervention for childhood anxiety in a school setting: Outcomes for an economically disadvantaged population. Journal of the American Academy of Child and Adolescent Psychiatry, 44(10), 996–1004. https://doi.org/10.1097/01.chi.0000173294.13441.87
Miller, L., Short, C., Garland, E., & Clark, S. (2010). The ABCs of CBT (cognitive behavior therapy): Evidence-based approaches to child anxiety in public school settings. Journal of Counseling and Development, 88(4), 432–439. https://doi.org/10.1002/j.1556-6678.2010.tb00043.x
Miller, L. D., Laye-Gindhu, A., Liu, Y., March, J. S., Thordason, D. S., & Garland, E. J. (2011). Evaluation of a preventive intervention for child anxiety in two randomized attention-control school trials. Behaviour Research and Therapy, 49(5), 315–323. https://doi.org/10.1016/j.brat.2011.02.006
Nail, J. E., Christofferson, J., Ginsburg, G. S., Drake, K., Kendall, P. C., McCracken, J. T., Birmaher, B., Walkup, J. T., Compton, S. N., Keeton, C., & Sakolsky, D. (2015). Academic impairment and impact of treatments among youth with anxiety disorders. Child & Youth Care Forum, 44(3), 327–342. https://doi.org/10.1007/s10566-014-9290-x
Notebaert, L., Clarke, P. J. F., Grafton, B., & Mac Leod, C. (2015). Validation of a novel attentional bias modification task: The future may be in the cards. Behaviour Research and Therapy, 65, 93–100. https://doi.org/10.1016/j.brat.2014.12.007
Piselli, K., Pella, J. E., Chan, G., & Ginsburg, G. S. (2021). The teacher anxiety program for elementary students: Open trial results. Education and Treatment of Children.
Polanczyk, G. V., Salum, G. A., Sugaya, L. S., Caye, A., & Rohde, L. A. (2015). Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 56(3), 345–365. https://doi.org/10.1111/jcpp.12381
Rapee, R. M., Bögels, S. M., Van Der Sluis, C. M., Craske, M. G., & Ollendick, T. (2012). Annual research review: Conceptualizing functional impairment in children and adolescents. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 53(5), 454–468. https://doi.org/10.1111/j.1469-7610.2011.02479.x
Reynolds, C. R., & Richmond, O. B. (1979). What I think and feel: A revised measure of children's manifest anxiety. Journal of Personality Assessment, 43, 281–283.
Rooney, R., Hassan, S., Kane, R., Roberts, C. M., & Nesa, M. (2013). Reducing depression in 9-10 year old children in low SES schools: A longitudinal universal randomized controlled trial. Behaviour Research and Therapy, 51(12), 845–854. https://doi.org/10.1016/j.brat.2013.09.005
Sanchez, A. L., Cornacchio, D., Poznanski, B., Golik, A. M., Chou, T., & Comer, J. S. (2018). The effectiveness of school-based mental health services for elementary-aged children: A meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 57(3), 153–165. https://doi.org/10.1016/j.jaac.2017.11.022
Sanchez, A. L., Comer, J. S., Coxe, S., Albano, A. M., Piacentini, J., Compton, S. N., Ginsburg, G. S., Rynn, M. A., Walkup, J. T., Sakolsky, D. J., Birmaher, B., & Kendall, P. C. (2019). The effects of youth anxiety treatment on school impairment: Differential outcomes across CBT, sertraline, and their combination. Child Psychiatry and Human Development, 50(6), 940–949. https://doi.org/10.1007/s10578-019-00896-3
Schleider, J. L., Burnette, J. L., Widman, L., Hoyt, C., & Prinstein, M. J. (2020). Randomized trial of a single-session growth mind-set intervention for rural adolescents’ internalizing and externalizing problems. Journal of Clinical Child and Adolescent Psychology, 49(5), 660–672. https://doi.org/10.1080/15374416.2019.1622123
Sportel, B. E., de Hullu, E., de Jong, P. J., & Nauta, M. H. (2013). Cognitive bias modification versus CBT in reducing adolescent social anxiety: A randomized controlled trial. PLoS One, 8(5). https://doi.org/10.1371/journal.pone.0064355
Stein, M. B., & Kean, Y. M. (2000). Disability and quality of life in social phobia: Epidemiologic findings. American Journal of Psychiatry, 157(10), 1606–1613. https://doi.org/10.1176/appi.ajp.157.10.1606
Storch, E. A., Salloum, A., King, M. A., Crawford, E. A., Andel, R., McBride, N. M., & Lewin, A. B. (2015). A randomized controlled trial in community mental health centers of computer-assisted cognitive behavioral therapy versus treatment as usual for children with anxiety. Depression and Anxiety, 32(11), 843–852.
Su, D., Irwin, J. A., Fisher, C., Ramos, A., Kelley, M., Mendoza, D. A. R., & Coleman, J. D. (2016). Mental health disparities within the LGBT population: A comparison between transgender and nontransgender individuals. Transgender Health, 1(1), 12–20. https://doi.org/10.1089/trgh.2015.0001
Sugai, G., & Horner, R. H. (2009). Responsiveness-to-intervention and school-wide positive behavior supports: Integration of multi-tiered system approaches. Exceptionality, 17(4), 223–237. https://doi.org/10.1080/09362830903235375
Swan, A. J., & Kendall, P. C. (2016). Fear and missing out: Youth anxiety and functional outcomes. Clinical Psychology: Science and Practice, 23(4), 417–435. https://doi.org/10.1111/cpsp.12169
van de Weijer-Bergsma, E., Langenberg, G., Brandsma, R., Oort, F. J., & Bögels, S. M. (2014). The effectiveness of a school-based mindfulness training as a program to prevent stress in elementary school children. Mindfulness, 5(3), 238–248. https://doi.org/10.1007/s12671-012-0171-9
Weems, C. F., Taylor, L. K., Costa, N. M., Marks, A. B., Romano, D. M., Verrett, S. L., & Brown, D. M. (2009). Effect of a school-based test anxiety intervention in ethnic minority youth exposed to hurricane Katrina. Journal of Applied Developmental Psychology, 30(3), 218–226. https://doi.org/10.1016/j.appdev.2008.11.005
Werner-Seidler, A., Perry, Y., Calear, A. L., Newby, J. M., & Christensen, H. (2017). School-based depression and anxiety prevention programs for young people: A systematic review and meta-analysis. Clinical Psychology Review, 51, 30–47. https://doi.org/10.1016/j.cpr.2016.10.005
Woodward, L. J., & Fergusson, D. M. (2001). Life course outcomes of young people with anxiety disorders in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 40(9), 1086–1093. https://doi.org/10.1097/00004583-200109000-00018
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ginsburg, G.S., Smith, I.C. (2023). School-Based Interventions for Students with Anxiety. In: Evans, S.W., Owens, J.S., Bradshaw, C.P., Weist, M.D. (eds) Handbook of School Mental Health. Issues in Clinical Child Psychology. Springer, Cham. https://doi.org/10.1007/978-3-031-20006-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-20006-9_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20005-2
Online ISBN: 978-3-031-20006-9
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)