Effective treatment is now available for retinopathy of prematurity (ROP) using peripheral laser ablation and cryotherapy, as well as scleral buckling and/or vitrectomy for severe ROP with retinal detachment. However, with the continued improvement in survival of low birth weight and early gestational age infants, ROP remains a significant cause of childhood blindness.1 While ROP is well known for damaging the posterior eye structures such as the retina and vitreous, ROP and its treatment can also predispose patients to develop anterior segment conditions, including cataract 2 and glaucoma 3
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Effective treatment is now available for retinopathy of prematurity (ROP) using peripheral laser ablation and cryotherapy, as well as scleral buckling and/or vitrectomy for severe ROP with retinal detachment. However, with the continued improvement in survival of low birth weight and early gestational age infants, ROP remains a significant cause of childhood blindness.1 While ROP is well known for damaging the posterior eye structures such as the retina and vitreous, ROP and its treatment can also predispose patients to develop anterior segment conditions, including cataract2 and glaucoma3 (Table 22.1 4). In fact, patients with stage V ROP have been reported to have a 30% risk of developing secondary angle-closure glaucoma5–7 and a 50% risk of developing cataracts.8
Glaucoma
As traditionally described in the literature, angle-closure glaucoma associated with ROP occurs in infants and young children, corresponding with the cicatricial phase of ROP, which usually has its onset at the age of 3–6 months9,10 (Table 22.2). Kushner suggested another possible and rare etiology when he described three cases of ciliary block glaucoma.11 Rubeosis iridis or neovascularization of the iris commonly occurs with chronic retinal detachment due to ROP and can also lead to angle-closure glaucoma.12 Angle-closure glaucoma has been reported after scleral buckling and after laser treatment for ROP.13–15 Finally, angle-closure glaucoma related to pupillary block may occur later in childhood and even into adulthood in patients born with ROP.16–19
Hittner postulated that angle-closure glaucoma is becoming a more significant aspect of the ROP sequelae in his older ROP population. This is not only due to the increased survival of patients now reaching ages where progressive anterior segment complications may occur more frequently but also because advances in surgical technique have led to improved vision, despite initial severe retinal pathology. Thus glaucoma can be a vision-limiting factor in this population.3
Smith and Tasman reviewed 86 adult eyes with a history of ROP and found that 16% had glaucoma; 7% had narrow angle treated with iridotomy, open angle was diagnosed in nearly 6%, and the remaining 3.5% had neovascular.20
Smith and Shivitz presented three cases of adults with a history of ROP who presented with pupillary block glaucoma17 and Michael presented ten eyes aged 12–45 years with a history of ROP who presented with angle-closure glaucoma.21 In the series by Michael, two had neovascularization and the other eight had pupillary block. Ueda and Ogino reported a case of pupillary block glaucoma in a 22-year-old with a history of ROP who responded to iridotomy.18
Mechanism of Glaucoma
The angle-closure glaucoma in ROP patients has multiple proposed mechanisms. In infants and children with stage V ROP, the mechanism considered most likely to cause secondary angle-closure glaucoma is contraction of the retrolental membrane, during the cicatricial or scarring phase of ROP, causing anterior displacement of the lens-iris diaphragm and subsequent closure of the chamber angle3,5,21. Suzuki demonstrated this mechanism with high resolution ultrasonography in three cases.19 Inflammation causing posterior synechiae formation and the subsequent development of pupillary block glaucoma can lead to angle closure in ROP eyes.7,11 A thickened lens and shallow anterior chamber are malformations commonly noted in ROP and could also lead to pupillary block as well as account for the high degree of myopia often seen in children with ROP.7,22–24 (Table 22.3). In a small cohort of children, McLoone used biometry with the IOL Master (Zeiss Meditec, Dublin, CA) to verify that eyes with a history of prior ROP had myopia associated with steeper corneas and shallower anterior chambers compared to control eyes with no history of ROP.25
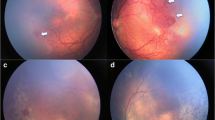
Whatever the exact mechanism, there often is a reduced passage of aqueous humor from the posterior chamber to the anterior chamber, as iridectomy/iridotomy has frequently been successful in curing the glaucoma episode16,17,19–21,26 (Fig. 22.1a, b).
(a) Eye of an 8-year-old adopted child followed for suspected ROP with retinopathy with macular dragging, high myopia in this eye, and angle-closure glaucoma following a dilated exam. A peripheral iridectomy was done, due to her age and nystagmus with good control of the IOP. Cataract surgery will be done when her angle further narrows, PAS develops, or elevated IOP ensues. (b) Note her shallow anterior chamber, despite iridectomy thought secondary to a large lens secondary to ROP. Photographs courtesy of Tom Monego, ophthalmic photographer, Dartmouth Hitchcock Medical Center, Lebanon, NH
Initial Management
As mentioned previously, pupillary block is commonly the cause of glaucoma in ROP patients, and therefore iridectomy/iridotomy should be considered an initial treatment. In the three cases of babies, who had had prior treatment for ROP as infants, reported by Suzuki, the ultrasound was able to show opening of the angle following the iridectomy.19 Additionally, Walton recommended prophylactic iridectomy when signs of cicatrization and shallowing of the anterior chamber are seen and are progressing, even when no signs of glaucoma are present.1,12 Walton found that in some patients, following peripheral iridectomy, continued shallowing of the anterior chamber produced apposition of the coloboma in the iris against the peripheral cornea leading to ineffectiveness of the iridectomy. To avoid this complication, he therefore recommended a sector iridectomy.
However, iridotomy/iridectomy has not been universally beneficial, suggesting that pupillary block is not the sole form of glaucoma in ROP.16,27
Corticosteroids and cycloplegics have had some degree of success in treating glaucoma in ROP eyes11,27 (Table 22.4). Corticosteroids were shown often to be successful at controlling IOP and eliminating ocular discomfort. However, patients often experienced a rebound effect when attempting to discontinue corticosteroids, leading Pollard to conclude that they cannot be considered a definitive treatment16 and cycloplegics are sometimes unsuccessful in treating pupillary block, due to posterior synechiae formation, during the cicatricial phase of ROP, which inhibits pupil dilation.16
After reporting ciliary block glaucoma in ROP eyes, Kushner made two recommendations: (1) If after dilation of ROP eyes there is noticeable deepening of the anterior chamber, suspect ciliary block glaucoma, and (2) if ROP eyes in acute angle glaucoma are unresponsive to miotic therapy, consider treating with a cycloplegic.27 So while medical treatments such as steroids and cycloplegics may not always provide the definitive treatment, they should be explored prior to surgery. Kushner argues that medical treatment as opposed to surgery may be less costly, and provide less risk to the patient, as well as less emotional trauma to the parents, especially where there may be very limited visual potential.
Surgical Management
When iridectomy and medical management fail, surgical management including lensectomy, tube shunt implantation, cyclo-destructive procedures, or trabeculectomy is the next step in management8 (Fig. 22.2a, b). In cases of rubeotic glaucoma, management is often difficult, but includes shunt implantation in eyes with vision and cyclodestructive procedures in blind eyes.8
Indications for Surgery
Lensectomy, which can effectively treat both pupillary and ciliary block glaucoma by lessening the anterior displacement of the iris and reducing angle closure, remains an effective means of controlling acute angle glaucoma in ROP.8 Pollard reported that lensectomy was universally successful in controlling pain and lowering IOP in eyes with a history of ROP, although visual outcome was poor, due to retinal detachment and cicatricial changes1,16,24,28 Because lensectomy can keep the eye in a pain-free state, it is a preferred alternative to enucleation in a young infant, as early enucleation can lead to decreased growth of the bony orbit and facial asymmetry.29 This disfiguring asymmetry, as well as the possible problems and fitting of a prosthesis are thus avoided According to Hittner, the most successful treatment in stage V ROP is lens aspiration.2 Intraocular surgery on a blind eye was deemed indicated in these cases to avoid enucleation. However, efforts to reattach the retina are resulting in improved vision in some cases.1,9,30–32 Rarely, only one eye develops severe cicatricial changes with angle closure, while the other eye is relatively free of ROP malformations. In this situation, Pollard recommends considering the alternatives to lensectomy – including enucleation, retrobulbar alcohol, or cyclocryotherapy – in order to avoid the rare development of sympathetic ophthalmia in the good eye.16
Cataract
Cataracts occur more commonly in ROP patients as compared to general population. Low birth weight and prematurity are risk factors for both ROP and cataracts.33,34Like glaucoma, cataracts also occur at a greater frequency over time, now that treatment modalities have preserved vision in eyes that would have otherwise been lost. Transpupillary laser photocoagulation is now the standard treatment for threshold ROP. Compared to cryotherapy, laser photocoagulation results in better structural and functional outcomes. However, laser-treated eyes have a higher incidence of secondary cataracts than cryo-treated eyes.35–37 In 1997, Gold reported 68 cataracts in association with ROP treatment.38 Sixty-two percent were associated with argon laser, 31% with diode laser, and 7% with cryotherapy.
Lens opacities associated with ROP comes in three types. First, focal punctuate or vacuolated opacities may occur at the subcapsular level. These are usually transient and visually insignificant.39,40 Second, progressive lens opacities may occur in patients without retinal detachment. Most of these eyes have had transpupillary laser treatment or “lens-sparing” vitrectomy. These cataracts may progress rapidly or much more slowly, but they almost always eventually obstruct the entire visual axis and require surgery (Fig. 22.3). One study reported a median interval of 3 weeks for diagnosis of cataract after laser photocoagulation.41 These patients may also develop glaucoma. The third type of cataract is one that develops as a result of cicatricial ROP with retinal detachment, which is also associated with glaucoma as discussed previously. In one series,8 54.6% (17/31) of eyes treated for advanced ROP had cataracts. In the series reported by Smith and Tasman, 83.7% of the 86 adult eyes aged 45–56 years with a history of ROP had cataract or cataract surgery.20
Operative Techniques
The two approaches to lensectomy in grade V ROP are pars plana lensectomy versus lensectomy via the limbal approach. A pars plana lensectomy can be combined with an attempt at retinal repair. Pars plan lensectomy with anterior vitrectomy was used successfully by Pollard for five eyes reported with angle closure, after the age of 2.28 The limbal approach is easier and more consistent, as the pars plana entry may be difficult in these immature eyes with retinal detachment. Even when the anterior chamber is extremely shallow, an anterior corneal entry can usually be made with the assistance of a viscous ophthalmic viscosurgical device (OVD).
A visually significant cataract after laser treatment or vitrectomy for ROP is approached much like childhood cataracts in children without ROP.2 At times the anterior capsule can be fibrotic, but a vitrectorhexis can still be easily performed.2 IOL (intraocular lens) calculations can be performed using an immersion A-scan ultrasound unit and a portable keratometer in the operating room, after the child is under general anesthesia for cataract surgery. IOLs are implanted routinely, unless the child is in the early months of life and has microphthalmia. Most commonly, a single-piece hydrophobic acrylic IOL is implanted in children. In anticipation of myopic shift of refraction, the IOL power for a child undergoing cataract surgery should be customized based on many characteristics – especially age, laterality (one eye or both), amblyopia status (dense or mild), likely compliance with glasses, and family history of myopia. For a child with ROP and cataract, slightly higher hypermetropia may be considered in anticipation of developing more myopia, especially if treated with cryotherapy.42
A primary posterior capsulectomy and anterior vitrectomy is performed for children who are younger than 6 years of age. If previous vitrectomy has been performed as part of the ROP treatment, the surgeon must be aware that the posterior capsule may have been violated during the previous surgery. Lens surgery and glaucoma surgery can be done together when necessary in eyes with previous treatment for ROP. The vitrector handpiece is often used to create a peripheral iridectomy, since in young children it is also used to perform the capsulotomy, lens aspiration, posterior capsulotomy, and anterior vitrectomy.
Outcomes
In all 15 patients in a report by Pollard,16 lensectomy cured the glaucoma. Eight patients presented with acute angle-closure glaucoma and the other seven had a chronic glaucoma. All vision remained extremely poor in the range of light perception to hand motion due to the prior ROP, but all eyes remained pain-free and had resolution of their glaucoma. This was a similar outcome to his cohort of five patients with a history of ROP who presented with glaucoma and were treated with pars plana lensectomy with anterior vitrectomy.28 Thus, Pollard suggested lensectomy via the limbal/corneal approach be considered in infants with grade V ROP and secondary angle-closure glaucoma. Blodi warned of potentially disastrous complications in opening an eye in such patients.5 At times, the lensectomy is merely a precursor to the inevitable enucleation. Lambert and coauthors41 reported a high rate of progression to total retinal detachment and phthisis after cataract surgery in patients with a history of transpupillary laser photocoagulation, even when the retina is attached at the time of cataract surgery.
Other reports show a more encouraging surgical outcome for cataract surgery with posterior chamber IOL implantation in children and adults with a past history of ROP.43–45 Yu reported on eight eyes with a history of ROP with cataract treated with lensectomy, posterior capsulectomy, and anterior vitrectomy with posterior chamber IOL.43 All the patients were under the age of 2. Two eyes of the same patient required cryotherapy and scleral buckle at the time of the lensectomy. Two eyes were able to have vision measured at 20/60 at the last follow-up and the others were central steady maintained fixation at the last recorded follow-up. These eyes did not have glaucoma. Krolicki reported on cataract surgery in ten adults with a history of ROP.44 Eight eyes had improved vision. Six of the eyes had coexisting glaucoma and the control improved following cataract surgery. One eye developed a retinal detachment. Farr reported on 21 adult eyes with a history of ROP who underwent cataract surgery.45 Eight eyes had narrow angle glaucoma and five with open angle. Two eyes had angle closure treated with iridectomy and one eye had phacomorphic glaucoma that resolved with the cataract extraction, otherwise in their series, the glaucoma control did not improve. No patient lost vision with the surgery and 18 had improved vision.
Summary
In summary, ROP remains a leading cause of vision impairment in children. Glaucoma and cataract can result from the ROP or from the treatment needed to control the ROP. Stage V ROP has a very high association with glaucoma and cataract. However, glaucoma and cataract can also occur in infants, children, and young adults after successful treatment for ROP with preservation of vision. General principles of pediatric anterior segment surgery should be followed for cataract surgery in children. A history of prematurity should be sought in patients with angle closure and other findings of ROP, such as high myopia and evidence of prior retinopathy. Cataract surgery should be considered in the treatment of the angle-closure glaucoma in these eyes. Based on the report by Farr, open angle glaucoma associated with a history or ROP and concurrent cataract are unlikely to experience improved glaucoma control with cataract surgery.45 The risk of retinal detachment needs to be discussed with the patients and the posterior segments monitored.
References
Ritch R, Shields MB, Krupin T, eds. The Glaucomas. 2nd ed., St. Louis: Mosby; 1996:941–3.
Wilson ME, Trivedi RH, Pandey SK, eds. Pediatric Cataract Surgery: Techniques, Complications, and Management. Philadelphia, PA: Lippincott Williams and Wilkins 2005:179–83.
Hittner HM, Rhodes LM, McPherson AR. Anterior segment abnormalities in cicatricial retinopathy of prematurity. Ophthalmology. 1979;86(5):803–16.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Blodi FC. Symposium: retrolental fibroplasia (retinopathy of prematurity). Management. Trans Am Acad Ophthalmol Otolaryngol. 1955;59:35–8.
Kwitko M. Secondary glaucoma in infancy and childhood. In Kwitko M, ed. Glaucoma in Infants and Children, New York: Appleton-Century-Crofts; 1973
Hartnett ME, Gilbert MM, Richardson TM, Krug JH, Jr, Hirose T, Anterior segment evaluation of infants with retinopathy of prematurity. Ophthalmology. 1990;97(1):122–30.
Knight-Nanan DM, Algawi K, Bowell R, O’Keefe M. Advanced cicatricial retinopathy of prematurity – outcome and complications. Br J Ophthalmol. 1996;80:343–45.
Shields MB. Textbook of Glaucoma. 2nd ed. Baltimore: Williams and Wilkins, 1987:272.
McCormick AQ, Pratt-Johnson JA. Angle closure glaucoma in infancy. Ophthalmic Surg. 1971:2:91–3.
Kushner BJ, Sondheimer S. Medical treatment of glaucoma associated with retinopathy of prematurity. Am J Ophthalmol. 1982;94:313–7.
Walton DS. Retrolental ibroplasia with glaucoma. In Chandler DA, Grant WM, eds. Glaocoma. 2nd ed. Philadelphia: Lea and Febiger; 1979:361–2.
Lee GA, Lee LR, Gole GA. Angle-closure glaucoma after laser treatment for retinopathy of prematurity. J AAPOS. 1998;2:383–4.
Halperin LS, Schoch LH. Angle closure glaucoma after scleral buckling for retinopathy of prematurity. Case report. Arch Ophthalmol. 1988;106:453
Trigler L, Weaver G, O’Neil JW, Barondes MJ, Freedman SF. Case series of angle-closure glaucoma after laser treatment for retinopathy of prematurity. J AASPO. 2005;9:17–21.
Pollard ZF. Lensectomy for secondary angle-closure glaucoma in advanced cicatricial retrolental fibroplasia. Ophthalmology. 1984; 91(4):395–8.
Smith J, Shivitz I. Angle-closure glaucoma in adults with cicatricial retinopathy of prematurity. Arch Ophthalmol. 1984;102: 371–2.
Ueda N, Ogino N. Angle-closure glaucoma with papillary block mechanism in cicatricial retinopathy of prematurity. Ophthalmologica. 1988;196:15–8.
Suzuki A, Kondo N, Terasaki H. High resolution ultrasonography in eyes with angle closure glaucoma associated with the cicatricial stage of retinopathy of prematurity. Jpn J Ophthalmol. 2005;49:312–4.
Smith BT, Tasman WS. Retinopathy of prematurity: late complications in the baby boomer generation (1946–64). Trans Am Ophthalmol Soc. 2005;103:225–36.
Michael AJ, Pesin SR, Katz LJ, Tasman WS. Management of late-onset angle-closure glaucoma associated with retinopathy of prematurity. Ophthalmology. 1991;98(7):1093–8.
Gordon RA, Donzis PB. Myopia associated with retinopathy of prematurity. Ophthalmology. 1986;93:1593–8.
Ritch R, Chang BM, Liebmann JM. Angle closure in younger patients. Ophthalmology. 2003;110(10):1880–9.
Choi MY, Park IK, Yu YS. Long term refractive outcome in eyes of preterm infants with and without retinopathy of prematurity: comparison of keratometric value, axial length, anterior chamber depth, and lens thickness. Br J Ophthalmol. 2000;84:138–43.
McLoone EM, O’Keefe M, McLoone SF, Lanigan BM. Long-term refractive and biometric outcomes following diode laser therapy for retinopathy or prematurity. J AAPOS, 2006;5:454–9.
Johnson DR, Swan KC. Retrolental fibroplasia – a continuing problem. Trans Pac Coast Otoophthalmol Soc Annu Meet. 1966;47:129–33.
Kushner BJ. Ciliary block glaucoma in retinopathy of prematurity. Arch Ophthalmol. 1982 July;100(7):1078–9.
Pollard ZF. Secondary angle-closure glaucoma in cicatricial retrolental fibroplasia. Am J Ophthalmol. 1980;89(5):651–3.
Kennedy RE. The effect of early enucleation on the orbit in animals and humans. Adv Ophthalmic Plast Reconstr Surg. 1992;9: 1–39.
Machemer R. Closed vitrectomy for severe retrolental fibroplasia in the infant. Ophthalmology. 1983;90:436.
Trese MT. Surgical results of Stage V retrolental fibroplasia and timing of surgical repair. Ophthalmology. 1984;91:461.
Ferrone PJ, Trese MT, Williams GA, Cox MS. Good visual acuity in an adult population with marked posterior segment changes secondary to retinopathy of prematurity. Retina. 1998;18: 335–8.
SanGiovanni JP, Chew EY, Reed GF, Remaley NA, Bateman JB, Sugimoto TA, et al. Infantile cataract in the collaborative perinatal project:prevalence and risk factors. Arch Ophthalmol. 2002;120:1559–65.
Repka MX, Summers CG, Palmer EA, Dobson V, Tung B, Davis B. The incidence of ophthalmic interventions in children with birth weights less than 1251 grams. Results through 5 ½ years. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology. 1998;105:1621–7.
Christiansen SP, Bradford JD. Cataract in infants treated with argon laser photocoagulation for threshold retinopathy of prematurity. Am J Ophthalmol. 1995;119:175–80.
Christiansen SP, Bradford JD. Cataracts following diode laser photoablation for retinopathy of prematurity. Arch Ophthamol. 1997;115:275–6.
Kaiser RS, Trese MT. Iris atrophy, cataracts, and hypotony following peripheral ablation for threshold retinopathy of prematurity. Arch Ophthalmol. 1995;119:615–7.
Gold RS. Cataracts associated with treatment for retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 1997;34:123–4.
Alden ER, Kalina RE, Hodson WA. Transient cataracts in low-birthweight infants. J Pediatr. 1973;82:314–8.
Drack AV, Burke JP, Pulido JS, Keech RV. Transient punctuate lenticular opacities as a complication of argon laser photoablation in an infant with retinopathy of prematurity. Am J Ophthalmol. 1992;113:583–4.
Lambert SR, Capone A, Jr, Cingle KA, Drack AV. Cataract and phthisis bulbi after laser photoablation for threshold retinopathy of prematurity. Am J Ophthalmol. 2000;129:585–91.
Trivedi RH, Wilson ME. IOL power calculation for children. In: Garg A, Lin, eds. Mastering Intraocular Lenses. New Delhi: Jaypee Brothers Medical Publishers; Chapter 9, 2007:84–91.
Yu YS, Kim SJ, Chang BL. Cataract surgery in children with and without retinopathy of prematurity. J Cataract Refract Surg. 2004;30:96–101.
Krolicki TJ, Tasman W. Cataract extraction in adults with retinopathy of prematurity. Arch Ophthalmol. 1995;113:173–7.
Farr AK, Stark WJ, Haller JA. Cataract surgery by phacoemulsification in adults with retinopathy of prematurity. Am J Ophthalmol. 2001;132:306–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Anfuso, A.J., Edward Wilson, M. (2009). Cataract and Glaucoma in Retinopathy of Prematurity. In: Johnson, S. (eds) Cataract Surgery in the Glaucoma Patient. Springer, New York, NY. https://doi.org/10.1007/978-0-387-09408-3_22
Download citation
DOI: https://doi.org/10.1007/978-0-387-09408-3_22
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-0-387-09407-6
Online ISBN: 978-0-387-09408-3
eBook Packages: MedicineMedicine (R0)