Abstract
Retinopathy of prematurity (ROP) is a leading cause of childhood blindness worldwide. Proper eye screening and interventions, such as laser ablation and/or anti-vascular endothelial growth factor therapy, are useful in reducing disease activity and preventing blindness. Some eyes are refractory to these treatments and develop tractional retinal detachment, which requires vitrectomy. Vitrectomy for stage 5 ROP is beneficial in preventing total blindness in some eyes; however, its anatomical and functional results are unsatisfactory.
The author has no proprietary interest in any of the products described in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
With the introduction of laser ablation therapy, the prognosis of retinopathy of prematurity (ROP) has significantly improved. Since more than a decade ago, the indication for laser ablation has been changed from threshold retinopathy to prethreshold retinopathy, leading to a decrease in the rate of unfavorable functional outcomes from 19.5% to 14.5% and structural outcomes from 15.6% to 9.1% [1]. However, using laser ablation alone, approximately 10% of patients still present with severe vision loss due to the development of retinal folds, retinal detachment, or retrolental fibroplasia [1].
More recently, anti-vascular endothelial growth factor (VEGF) therapy, which comprises intravitreal injection of an anti-VEGF agent as an off-label treatment, has been introduced [2,3,4] because VEGF may play a major role in the pathogenesis of ROP [5,6,7]. Anti-VEGF therapy is effective in reducing disease activity and is likely to lead to better ROP treatment outcomes particularly in severe ROP cases, such as zone 1 plus ROP or aggressive posterior ROP [4]. The number of eyes with ROP that progresses from stage 4 to 5 seems to be decreasing using anti-VEGF therapy. In addition, recent improvements in neonatal care have helped decrease ROP in patients, particularly in advanced countries. However, some patients still require vitrectomy for tractional retinal detachment (TRD) even after laser ablation and/or anti-VEGF therapy; the reasons may include improper screening or treatment. Sometimes, despite proper treatment, the patients’ condition progresses to TRD due to excessive prematurity. Therefore, surgical treatment for ROP is still required, particularly in developing countries.
2 Stage 5 ROP
Fibrovascular membranes develop along the ridge and grow into various directions, including the ridge to the lens, the ridge to the ciliary body, the ridge to the peripheral retina, the ridge to the ridge (circumferential), and the ridge to the posterior retina. In eyes with stage 5 ROP, the retina is totally detached in a complex manner due to these traction forces. The surgical treatment releases these tractions as much as possible, most likely not completely, without creating an iatrogenic retinal break. Because surgery for stage 5 ROP remains extremely challenging and the anatomical and functional results are generally disappointing, surgical treatment should be considered not for stage 5 but for stage 4A ROP (partial retinal detachment without involvement of the macula).
3 Surgical Technique
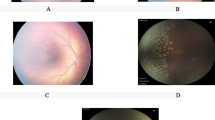
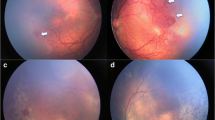
Scleral buckling alone has been attempted for stage 5 ROP as it is safer than vitrectomy. However, complex retinal detachment caused by various traction forces cannot be effectively alleviated enough to reattach the retina in several cases [8, 9]. Meanwhile, vitrectomy can help effectively relieve the forces by directly cutting the fibrous membranes. In most eyes with stage 5 ROP, lensectomy is required to approach the retrolental fibrous membranes. The locations where surgical entry would be made should be carefully determined preoperatively. If the retrolental fibrous membranes are located adjacent to the ciliary body, the surgical entry should be made at the limbus to avoid an iatrogenic retinal break or ora dialysis. If there is a space between the ciliary body and the membranes, sclerotomies may be made 0.5–1 mm from the limbus, which allows for better visibility and easier manipulation during vitrectomy. In addition, a mixture of limbal (for infusion) and pars plicata (for other two ports) incisions can be used depending on the space between the ciliary body and the membranes. Lensectomy should be meticulously performed and should include the entire lens capsule because its remnants can adhere to the iris and/or remaining retrolental membrane after surgery. If the anterior chamber is shallow and the iris cannot be dilated due to posterior synechiae (Fig. 14.1), which is caused by the anterior displacement of the lens due to contraction of the retrolental fibrous membrane, viscoelastic material can be injected through the limbal wound to provide some space for an infusion cannula and a vitreous cutter. Then, a vitreous cutter is used to remove the lens and the iris of the pupillary margin (Figs. 14.2 and 14.3). Alternatively, instruments that can dilate the iris, such as an iris retractor, can be used.
After lens removal, dissection of the retrolental fibrous membranes is initiated from the center either using scissors or a sharp knife, such as the V-lance (Fig. 14.4). Separation of the membranes from the detached retina should be cautiously performed taking care to avoid any iatrogenic breaks. It is usually performed using forceps and scissors or a spatula with the bimanual technique (Fig. 14.5). Dissection can be extended peripherally in concentric and/or circumferential manners (Figs 14.6, 14.7, 14.8, 14.9, 14.10, and 14.11). To increase the chance of retinal reattachment (Fig. 14.12), the membranes should be removed as much as possible. Opening of the trough in the peripheral retina is critical; however, it is sometimes challenging and dangerous as a distinction between the thin membrane and avascular retina is often difficult. To avoid dialysis, caution must be taken to avoid pulling of the membranes too far in the peripheral region. The presence of a retinal break is highly associated with surgical failure in stage 5 ROP surgery. If most membranes can be removed, the retina is gradually reattached within several weeks. Otherwise, reoperation to remove residual membranes should be considered. Use of perfluorocarbon liquid as a short-term tamponade may be effective in such cases [9].
4 Surgical Results
Surgical results of vitrectomy for stage 5 ROP are generally unsatisfactory. In a clinical trial conducted in the USA [10], at least a portion of the retina was reattached in 11 (21%) of 52 eyes, and visual acuity was limited to light perception or no light perception in all but one eye after vitrectomy for stage 5 ROP at 5.5 years of age. Cusick et al. [11] have reported that at least partial retinal reattachment was achieved in 33% of 956 eyes from 601 infants, with a visual acuity better than 5/200 in 8 of 183 eyes. In a case series of 48 eyes with stage 5 ROPs evaluated 6 months postoperatively, 20 (42.6%) and 5 (10.6%) eyes exhibited total and partial reattachment of the retina, respectively (unpublished data). Similar results have been reported with retinal reattachment rates of approximately 40%–60% [12,13,14,15,16,17,18,19] and limited functional outcomes 12–16 [20,21,22,23], (Table 14.1). Regarding the factors related to anatomical success, the close shape of the funnel, presence of subretinal hemorrhage and vascularized membranes, and age at vitrectomy are associated with poor surgical outcomes [12, 13, 16].
5 Conclusions
Neonatologists should appropriately care for premature infants, and ophthalmologists must screen at appropriate timings and use proper techniques to reduce severe ROP that requires treatment. Interventions, such as laser ablation or anti-VEGF therapy, are critical in preventing the development of TRD. If tractional detachment occurs, vitrectomy should be performed at stage 4A before the macula is detached to achieve satisfactory outcomes.
References
Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121(12):1684–94.
Quiroz-Mercado H, Martinez-Castellanos MA, Hernandez-Rojas ML, Salazar-Teran N, Chan RV. Antiangiogenic therapy with intravitreal bevacizumab for retinopathy of prematurity. Retina. 2008;28(3 Suppl):S19–25.
Kusaka S, Shima C, Wada K, Arahori H, Shimojyo H, Sato T, Fujikado T. Efficacy of intravitreal injection of bevacizumab for severe retinopathy of prematurity: a pilot study. Br J Ophthalmol. 2008;92(11):1450–5.
Mintz-Hittner HA, Kennedy KA, Chuang AZ, BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage3+ retinopathy of prematurity. N Engl J Med. 2011;364(7):603–15.
Sonmez K, Drenser KA, Capone A Jr, Trese MT. Vitreous levels of stromal cell-derived factor 1 and vascular endothelial growth factor in patients with retinopathy of prematurity. Ophthalmology. 2008;115(6):1065–70.
Sato T, Kusaka S, Shimojyo H, Fujikado T. Vitreous levels of erythropoietin and vascular endothelial growth factor in eyes with retinopathy of prematurity. Ophthalmology. 2009;116(9):1599–603.
Sato T, Kusaka S, Hashida N, Saishin Y, Fujikado T, Tano Y. Comprehensive gene-expression profile in murine oxygen-induced retinopathy. Br J Ophthalmol. 2009;93(1):96–103.
Greven C, Tasman W. Scleral buckling in stages 4B and 5 retinopathy of prematurity. Ophthalmology. 1990;97(6):817–20.
Imaizumi A, Kusaka S, Noguchi H, Shimomura Y, Sawaguchi S. Efficacy of short-term postoperative perfluoro-n-octane tamponade for pediatric complex retinal detachment. Am J Ophthalmol. 2014;157(2):384–9.
Quinn GE, Dobson V, Barr CC, Davis BR, Palmer EA, Robertson J, Summers CG, Trese MT, Tung B. Visual acuity of eyes after vitrectomy for retinopathy of prematurity: follow-up at 5 1/2 years. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology. 1996;103(4):595–600.
Cusick M, Charles MK, Agrón E, Sangiovanni JP, Ferris FL 3rd, Charles S. Anatomical and visual results of vitreoretinal surgery for stage 5 retinopathy of prematurity. Retina. 2006;26(7):729–35.
Hirose T, Katsumi O, Mehta MC, Schepens CL. Vision in stage 5 retinopathy of prematurity after retinal reattachment by open-sky vitrectomy. Arch Ophthalmol. 1993;111(3):345–9.
Fuchino Y, Hayashi H, Kono T, Ohshima K. Long-term follow up of visual acuity in eyes with stage 5 retinopathy of prematurity after closed vitrectomy. Am J Ophthalmol. 1995;120(3):308–16.
Trese MT, Droste PJ. Long-term postoperative results of a consecutive series of stages 4 and 5 retinopathy of prematurity. Ophthalmology. 1998;105(6):992–7.
Kono T, Oshima K, Fuchino Y. Surgical results and visual outcomes of vitreous surgery for advanced stages of retinopathy of prematurity. Jpn J Ophthalmol. 2000;44(6):661–7.
Jabbour NM, Eller AE, Hirose T, Schepens CL, Liberfarb R. Stage 5 retinopathy of prematurity. Prognostic value of morphologic findings. Ophthalmology. 1987;94(12):1640–6.
Trese MT. Visual results and prognostic factors for vision following surgery for stage V retinopathy of prematurity. Ophthalmology. 1986;93(5):574–9.
Tasman W, Borrone RN, Bolling J. Open sky vitrectomy for total retinal detachment in retinopathy of prematurity. Ophthalmology. 1987;94(4):449–52.
Zilis JD, de Juan E, Machemer R. Advanced retinopathy of prematurity. The anatomic and visual results of vitreous surgery. Ophthalmology. 1990;97(6):821–6.
Karacorlu M, Hocaoglu M, Sayman Muslubas I, Arf S. Long-term functional results following vitrectomy for advanced retinopathy of prematurity. Br J Ophthalmol. 2017;101(6):730–4.
Mintz-Hittner HA, O'Malley RE, Kretzer FL. Long-term form identification vision after early, closed, lensectomy-vitrectomy for stage 5 retinopathy of prematurity. Ophthalmology. 1997;104(3):454–9.
Hartnett ME, Rodier DW, McColm JR, Thompson HW. Long-term vision results measured with Teller Acuity Cards and a new Light Perception/Projection Scale after management of late stages of retinopathy of prematurity. Arch Ophthalmol. 2003;121(7):991–6.
Seaber JH, Machemer R, Eliott D, Buckley EG, deJuan E, Martin DF. Long-term visual results of children after initially successful vitrectomy for stage V retinopathy of prematurity. Ophthalmology. 1995;102(2):199–204.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kusaka, S. (2021). Surgical Management of Stage 5 Retinopathy of Prematurity. In: Wu, WC., Lam, WC. (eds) A Quick Guide to Pediatric Retina. Springer, Singapore. https://doi.org/10.1007/978-981-15-6552-6_14
Download citation
DOI: https://doi.org/10.1007/978-981-15-6552-6_14
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-6551-9
Online ISBN: 978-981-15-6552-6
eBook Packages: MedicineMedicine (R0)