Abstract
Although quite overlooked, increasing evidence points to a significant association between attention-deficit/hyperactivity disorder (ADHD) and obesity. Here, we present an updated systematic review and a critical discussion of studies on the relationship between ADHD and obesity, with a particular emphasis on the possible behavioral, neurobiological, and genetics underlying mechanisms. Available empirically based studies indicate that the prevalence of ADHD in clinical samples of patients seeking treatment for their obesity is higher than that in the general population. Moreover, although still limited, current evidence shows that individuals with ADHD have higher-than-average body mass index z-scores and/or significantly higher obesity rates compared with subjects without ADHD. Three mechanisms underlying the association between ADHD and obesity have been proposed: (1) obesity and/or factors associated with it (such as sleep-disordered breathing and deficits in arousal/alertness) manifest as ADHD-like symptoms; (2) ADHD and obesity share common genetics and neurobiological dysfunctions, involving the dopaminergic and, possibly, other systems (e.g., brain-derived neurotropic factor, melanocortin-4-receptor); and (3) impulsivity and inattention of ADHD contribute to weight gain via dysregulated eating patterns. With regards to the possible clinical implications, we suggest that it is noteworthy to screen for ADHD in patients with obesity and to look for abnormal eating behaviors as possible contributing factors of obesity in patients with ADHD. If further studies confirm a causal relationship between ADHD and obesity, appropriate treatment of ADHD may improve eating patterns and, as a consequence, weight status of individuals with both obesity and ADHD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Recent evidence suggests strong links between attention-deficit/hyperactivity disorder (ADHD) and obesity, although findings are not always consistent. A better insight into this association is of relevance for two reasons. First, it may contribute to the understanding of possible psychopathological and pathophysiological mechanisms underlying both ADHD and obesity, at least in a subset of patients. Second, it might have important implications for the management of patients with both obesity and ADHD, suggesting common therapeutic strategies when these two conditions coexist. This seems particularly noteworthy because of the high prevalence and the enormous personal, family, and social burden associated with both obesity and ADHD.
Therefore, the aims of this chapter are to: (1) review the evidence for an association between ADHD and obesity; (2) examine the behavioral and pathophysiological mechanisms that have been proposed to underlie this potential association; and (3) discuss the implications of this newly described potential comorbidity on the clinical management of patients who present with both ADHD and obesity.
Before examining the relationship between ADHD and obesity, we introduce in the following paragraph the definition of obesity and overweight that will be used throughout this chapter. We refer to the definitions available in the World Health Organization (WHO) website: http://www.who.int/en/. Overweight and obesity are characterized by abnormal or excessive fat accumulation that may impair health. Body mass index (BMI) is a simple index of weight-for-height that is commonly used in classifying overweight and obesity in adult populations and individuals. It is defined as the weight in kilograms divided by the square of the height in meters (kg/m2). BMI provides the most useful population-level measure of overweight and obesity, as it is the same for both sexes and for adults of all ages. However, it should be considered as a rough guide because it may not correspond to the same degree of fatness in different individuals. The WHO defines “overweight” as a BMI greater than or equal to 25 kg/m2, and “obesity” as a BMI greater than or equal to 30. The new WHO Child Growth Standards, launched in April 2006, include BMI charts for infants and young children up to the age of 5. However, measuring overweight and obesity in children aged 5–14 years is challenging because there is not a standard definition of childhood obesity applied worldwide. WHO is currently developing an international growth reference for school-age children and adolescents. Since BMI does not adequately describe central adiposity, other indices of body fatness are being explored. A recent study showed a significant correlation between BMI and neck circumference in children; the best cutoff that identified high BMI in boys ranged from 28.5 to 39.0 cm; corresponding values in girls ranged to 27.0–34.6 cm (Nafiu et al. 2010). However, since this a recent proposal, no study assessing the relationship between ADHD and obesity has used this index, which, therefore, will not be taken into consideration in this chapter.
2 Studies Assessing the Relationship Between ADHD and Obesity
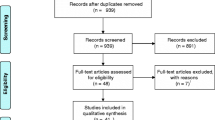
Our group published in 2008 a systematic review (Cortese et al. 2008a) of the studies exploring the relationship between ADHD and obesity. We searched both for studies assessing the prevalence of ADHD in obese subjects and for those evaluating the weight status of subjects with ADHD. We included methodologically sound studies, published up to January 2007, conducted in children and in adults with ADHD diagnosed according to formal criteria. Since drugs used for the treatment of ADHD may have anorexigenic effects, we did not consider studies examining weight status in treated patients with ADHD or studies which did not control for the effect of ADHD medications. Since that review, an additional three methodologically sound studies (where the diagnosis of ADHD was based on formal criteria) have been published (Braet et al. 2007; Pagoto et al. 2009; Ptacek et al. 2009). In the following section, we present and critically discuss the key results from the studies included in our initial systematic review plus those from the three new additional studies published after January 2007. We also present additional studies that, although do not meet the criteria for inclusion in the systematic review, provide interesting insights on the relationship between ADHD symptoms and obesity.
2.1 Studies Examining the Prevalence of ADHD in Obese Subjects (Table 1)
We located five methodologically sound studies (Agranat-Meged et al. 2005; Altfas 2002; Braet et al. 2007; Erermis et al. 2004; Fleming et al. 2005) conducted in clinical settings, and one survey (Mustillo et al. 2003) in the general population. The five clinical studies were conducted, respectively, in a clinical sample of: 215 obese adults receiving obesity treatment in a clinic specialized in the prevention and treatment of obesity (Altfas 2002); 30 obese adolescents (aged 12–16 years) seeking treatment from a pediatric endocrinology outpatient clinic (Erermis et al. 2004); 26 children (aged 8–17 years) hospitalized in an eating disorder unit for the treatment of their refractory morbid obesity (Agranat-Meged et al. 2005); 75 obese women (mean age: 40.4 years) consecutively referred to a medical obesity clinic (Fleming et al. 2005); and in a clinical sample of 56 overweight children versus 53 normal weight children (10–18 years) (Braet et al. 2007). All these studies, except one (Braet et al. 2007), reported a significantly higher prevalence of ADHD (diagnosed according to formal criteria) in obese patients than in comparable controls or age-adapted reference values. As for the negative study (Braet et al. 2007), we believe that its results cannot lead to a firm conclusion since neither the details of the interview nor the medication status of the patients was reported.
However, the four positive studies also present some methodological limitations that hamper a firm conclusion from their results, such as: the relatively small sample sizes; the lack of a control group in some of them (Altfas 2002; Fleming et al. 2005); and possible selection biases (e.g., the study by Fleming et al. was conducted in a female sample (Fleming et al. 2005)). However, despite these limitations, they all suggest that obese patients referred to obesity clinics may present with higher than expected prevalence of ADHD.
By contrast, the only epidemiological study reported no association between ADHD and obesity. This study (Mustillo et al. 2003) was conducted in a large sample (991 youths aged 9–16 years) and was based on the state-of-the-art assessment for psychiatric disorder in childhood (Child and Adolescent Psychiatric Assessment, CAPA). However, given the epidemiological nature of the study and the large sample size, it was difficult to obtain information from multiple sources, as required for an appropriate diagnosis of ADHD. The discordance of the results between the four clinical studies and the epidemiological survey may be due to methodological issues. Indeed, clinical settings may favor a higher case-finding rate because the opportunity to observe and assess behavior is greater than the methods of epidemiological surveys.
In summary, current evidence points to higher than expected prevalence of ADHD in clinical samples of obese patients seeking for treatment, while there are no data supporting significantly higher prevalence of ADHD in the general population of obese individuals.
2.2 Studies Assessing the Weight Status of Subjects with ADHD
In our systematic review, we located 12 studies (Anderson et al. 2006; Biederman et al. 2003; Curtin et al. 2005; Faraone et al. 2005; Holtkamp et al. 2004; Hubel et al. 2006; Lam and Yang 2007; Pagoto et al. 2009; Ptacek et al. 2009; Spencer et al. 1996, 2006; Swanson et al. 2006) that examined the weight status of children with ADHD. Eight of these studies (Biederman et al. 2003; Curtin et al. 2005; Faraone et al. 2005; Holtkamp et al. 2004; Ptacek et al. 2009; Spencer et al. 1996, 2006; Swanson et al. 2006) were conducted in clinical settings, while four (Anderson et al. 2006; Hubel et al. 2006; Lam and Yang 2007; Pagoto et al. 2009) examined the general population. These studies showed that children with ADHD presented with higher-than-average body mass index standard deviations scores (BMI-SDS). Interestingly, one of these studies (Ptacek et al. 2009), besides BMI, used also other indices of body mass (percentage of body fat and abdominal circumference): the authors found that these were significantly higher in ADHD compared to controls.
Limitations of these 12 studies included a lack of control group (Curtin et al. 2005; Faraone et al. 2005; Holtkamp et al. 2004; Spencer et al. 2006; Swanson et al. 2006), selection biases (e.g., inclusion of males, but not females (Holtkamp et al. 2004)), lack of control for the effect of comorbid psychiatric disorders, which may have an impact on subjects’ BMI (Anderson et al. 2006; Lam and Yang 2007), or retrospective diagnosis of adult ADHD (Pagoto et al. 2009). However, this last study (Pagoto et al. 2009) is the only one that we were able to locate in adults. Interestingly, in this study, adult ADHD remained associated with overweight (OR = 1.57; 95% CI = 0.99, 2.70) and obesity (OR = 1.69; 95% CI = 1.01, 2.82) when controlling for major depressive disorder. However, the association was no longer statistically significant when controlling for binge-eating disorder in the past 12 months (1.41, 95% CI = 0.76–2.53).
Although they did not rely on formal criteria for the diagnosis of ADHD (and, therefore, they are not mentioned in Table 2), we believe it is interesting to mention two additional studies that we located in our search. In the first, a large cohort of 46,707 subjects, aged 10–17 years, collected by the National Survey of Children’s Health (NSCH-2003), the authors (Chen et al. 2010) reported that the prevalence of obesity was 18.9% (95% CI: 18.7–19.0) in children with ADHD compared to 12.2% (95% CI: 11.5–13.0) in children without chronic diseases. Differences in the prevalence of obesity in children with and without ADHD remained significant after adjustment for age, sex, race/ethnicity, family income, family structure, parental education, and region. Similarly, in the second study, another large cross-sectional analysis of 62,887 children and adolescents, aged 5–17 years from the 2003–2004 National Survey of Children’s Health, the authors (Waring and Lapane 2008) found that children with ADHD, who were not currently using medication, had about 1.5 times the odds of being overweight compared to non-ADHD children. However, as we stated, the major limitation of both these studies was the lack of a formal diagnosis of ADHD, since the assessment of the presence of ADHD was based on the question: “Has a doctor or health professional ever told you [you suffer from ADHD]?” Moreover, the authors did not control for the effect of medication status and psychiatric comorbidity.
In summary, studies both in clinical and epidemiological samples showed that individuals with ADHD have higher than average BMI-SDS and a higher prevalence of obesity compared to non-ADHD subjects. We note that, besides ADHD, other psychological disorders such as depression, low-self esteem, and anxiety have also been found to relate to obesity in children and adolescents (Zametkin et al. 2004).
3 Behavioral and Neurobiological Mechanisms Underlying the Association Between ADHD and Obesity
Since all the studies reviewed above (with the exception of one study, Mustillo et al. (2003)) are cross-sectional, they do not enable an understanding of the causality between ADHD and obesity.
From a theoretical point of view, it is possible that: (1) obesity and/or factors associated with obesity (such as sleep-disordered breathing (SDB)) lead to, or manifest as, ADHD/ADHD symptoms; (2) ADHD and obesity are the expression of a common biological dysfunction that manifests itself as both obesity and ADHD in a subset of patients; (3) ADHD contributes to obesity. We discuss these hypotheses in the following sections.
3.1 Obesity or Related Factors Manifest as ADHD
Two factors, potentially associated with obesity, have been proposed that might manifest as ADHD or its symptoms: these are binge eating and excessive daytime sleepiness.
3.1.1 Binge Eating
It is known that a subgroup of patients with obesity, especially those with severe obesity (Hudson et al. 2006), presents with binge eating. One can hypothesize that impulsivity associated with abnormal eating behavior in these patients contributes to, or manifests itself as, impulsivity of ADHD. It is also possible that impulsivity associated with abnormal eating behaviors fosters symptoms of inattention and hyperactivity. It has been reported that patients with bulimic or abnormal eating behaviors may present with repeated and impulsive interruptions of their activities to get food; this behavior results in ADHD symptoms, such as disorganization, inattention, and restlessness (Cortese et al. 2007a). Of note, a research group (Rosval et al. 2006) reported higher rates of motor impulsiveness in patients with bulimia nervosa and anorexia nervosa binge/purge subtype, in comparison to anorexia nervosa, restricting subtype and normal eater control group. This finding further confirms previous studies that linked binge-eating behaviors and behavioral impulsivity (Engel et al. 2005; Nasser et al. 2004). However, other authors (Davis et al. 2009) found evidence against the role of binge eating in explaining the association between ADHD and obesity. After predicting that ADHD symptoms would be more severe in the binge eaters compared to obese controls, using a case–control design (binge eaters, n = 60, versus non-binge eaters with normal weight, n = 61, and obese subjects, n = 60) these authors, contrary to their prediction, reported that symptoms of ADHD were elevated in obese adults, with and without binge eating, but there was no difference between these two groups.
3.1.2 Excessive Daytime Sleepiness
Another hypothesis is based on the link between obesity, hypoarousal (manifested as excessive daytime sleepiness, EDS), and ADHD symptoms. According to this theory, obesity may contribute to excessive daytime sleepiness which, in turn, could lead to ADHD symptoms.
As for the link between EDS and ADHD, EDS, either due to SDB or independent from it, may contribute to ADHD symptoms. According to the “hypoarousal theory” of ADHD (Weinberg and Brumback 1990), subjects with ADHD behaviors (or at least a subgroup of them) might be sleepier than controls and might use motor hyperactivity and impulsivity as a strategy to stay awake and alert. In a recent meta-analysis, we found evidence supporting this proposal: a higher prevalence of excessive daytime sleepiness in children with ADHD versus controls (Cortese et al. 2009). As for the link between obesity and EDS, several studies have reported an association between obesity and SDB or other sleep disorders (Cortese et al. 2008b). These disorders may cause sleep fragmentation, leading to excessive daytime sleepiness. Moreover, as reported in the review of the literature (Vgontzas et al. 2006), recent evidence, based on subjective as well as objective measures, indicates that obesity may be associated with EDS independently of SDB or any other sleep disturbances. It has been suggested (Vgontzas et al. 2006) that, at least in some obese patients, EDS may be related to a metabolic and/or circadian abnormality associated with obesity rather than being a consequence of SDB or other sleep disturbances. Interestingly, in a study by our group (Cortese et al. 2007b) using a subjective measure of sleepiness (a subscale of the Sleep Disturbance Scale for Children, SDSC) in a sample of 70 obese children (age range: 10–16 years), scores of excessive daytime sleepiness on the SDSC were associated with symptoms of inattention, hyperactivity, and impulsivity on both the Conners Parent Rating Scale-R:S and the ADHD-Rating Scale. Clearly, this finding needs to be replicated in studies using objective (i.e., polysomnographic) measures of EDS (hypoarousal).
3.2 ADHD and Obesity Share Common Biological Mechanisms
Another possibility is that obesity and ADHD are different expressions of common underlying biological mechanisms or share common biological underpinnings, at least in a subset of patients with both these conditions. Several biological processes have been proposed, including: altered reinforcement mechanisms, brain-derived neurotropic disorder, and melanocortin-4-receptor (MC4-R) deficiency.
3.2.1 Altered Reinforcement Mechanisms
The “reward deficiency syndrome” may play a significant role. This syndrome is characterized by an insufficient dopamine-related natural reinforcement that leads to the use of “unnatural” immediate rewards, such as: substance use, gambling, risk-taking, and inappropriate eating. Several lines of evidence suggest that patients with ADHD may present with behaviors consistent with the “reward deficiency syndrome” (e.g., Blum et al. 1995; Heiligenstein and Keeling 1995). This syndrome has been reported also in obese patients with abnormal eating behaviors (Comings and Blum 2000).
In a sample of women with seasonal affective disorder (SAD), the 7R allele of DRD4 was associated with higher scores of childhood inattention on the WURS-25 and with higher maximal lifetime BMI. SAD is characterized by marked craving for high-carbohydrate/high-fat foods, resulting in significant weight gain during depressive episodes in the winter. A potential implication of the reward system in the pathophysiology of the disorder has been suggested. It has been hypothesized (Levitan et al. 2004) that childhood attention deficit and adult obesity could be the expression of a common biological dysfunction of the 7R allele of DRD4 associated with a dopamine dysfunction in prefrontal attentional areas and brain circuits involved in the reward pathways. Alterations in the dopamine D2 receptor (DRD2) (Bazar et al. 2006) and, to a lesser extent, DRD4 (Mitsuyasu et al. 2001; Tsai et al. 2004) have been associated with the above-mentioned “reward deficiency syndrome.” Dysfunctions of DRD2 and DRD4 have been found in obese patients (Poston et al. 1998). Several studies suggest a role of altered DRD4 and DRD2 in ADHD as well (although the alteration in DRD2 has not been replicated in all studies) (Noble 2003). Therefore, obese patients with abnormal eating behaviors and ADHD may present with common genetically determined dysfunctions in the dopaminergic system, in particular the dopaminergic circuits underlying reward mechanisms and executive functions necessary for appropriate eating behaviors. However, these hypotheses need to be tested in empirically based, methodologically sound studies.
3.2.2 Brain-Derived Neurotropic Factor
Another potential common biological mechanism involves alterations in the brain-derived neurotropic factor (BDNF), a protein member of the family of growth factors. It supports the survival of existing neurons and encourages the growth and differentiation of new neurons and synapses. Preliminary evidence from animal models points to a potential dysfunction of BDNF underlying both ADHD and obesity (Kernie et al. 2000; Lyons et al. 1999). Although one research group (Friedel et al. 2005) failed to find a large role of genetic variation of BDNF in ADHD and obesity, another group (Gray et al. 2006) reported a functional loss of one copy of the BDNF gene in an 8-year old with hyperphagia, severe obesity, impaired cognitive function, and hyperactivity. Moreover, a recent study has reported a significant association among 11p14.1 microdeletions (encompassing the BDNF gene), ADHD, and obesity (Shinawi et al. 2011).
3.2.3 Melanocortin-4-Receptor Deficiency
MC4-R is a 332-amino acid protein encoded by a single exon gene localized on chromosome 18q22 and is a key element in the hypothalamic control of food intake. MC4-R deficiency has been proposed recently (Agranat-Meged et al. 2008) and has been reported to disrupt neuronal pathways that regulate hunger/satiety and results in abnormal eating behaviors. The authors analyzed 29 subjects (19 males and 10 females) from 5 “proband nuclear families” with morbid obese children (BMI percentile >97%), and found that the prevalence of ADHD was higher than expected only in the groups carrying the homozygous or heterozygous mutation. Recently, Albayrak et al. (2011) reported the case of a 2-year-old child heterozygous for a non-conservative functionally relevant MC4-R mutation (Glu308Lys) and who also showed severe ADHD.
Given the limited and, at least in part, inconsistent findings, the role of common genetic mutations underlying shared neurobiological dysfunctions in ADHD and obesity deserves further investigation.
3.3 ADHD Contributes to Obesity
Finally, behavioral and cognitive features of ADHD may play a significant role in abnormal eating behaviors, which in turn lead to obesity. A study of 110 adult healthy women (age range: 25–46 years) using structural equation modeling (Davis et al. 2006) found that ADHD symptoms and impulsivity correlated with abnormal eating behaviors, including binge eating and emotionally induced eating, which were, in turn, positively associated with BMI. These results have been recently replicated in males (Strimas et al. 2008). In our study, conducted in a clinical sample of 99 severely obese adolescents (aged 12–17 years), we found that, after controlling for potentially confounding depressive and anxiety symptoms, ADHD symptoms were associated with bulimic behaviors (Cortese et al. 2007a). Bearing in mind that loss of control and excessive food intake are important determiners of weight gain, children and adolescents who report binge-eating symptoms gain more weight over time than children and adolescents without such history (Lourenco et al. 2008).
At present, it is not clear which dimension of ADHD (inattention, hyperactivity, or impulsivity) is associated with abnormal eating behaviors. We speculated that both impulsivity and inattention, but not hyperactivity, might lead or contribute to abnormal eating behaviors (Cortese et al. 2007a). We detail this hypothesis in the following sections.
3.3.1 Role of Impulsivity
It has been suggested (Davis et al. 2006) that both deficient inhibitory control and delay aversion, which are an expression of the impulsivity component of ADHD, may foster abnormal eating behaviors and, as a consequence, obesity. Deficient inhibitory control manifests as poor planning and difficulty in monitoring one’s behavior effectively. This could lead to over-consumption when not hungry, associated with a relative absence of concern for daily caloric intake. A strong delay aversion could favor the tendency to eat high caloric, but readily available “fast food,” in preference to less caloric content home-cooked meals, which take longer to prepare. This may contribute to maintenance of a chronic positive energy balance that culminates in obesity.
3.3.2 Role of Inattention
It is also possible that ADHD-related inattention and associated deficits in executive functions cause difficulties in adhering to a regular eating pattern and so favor abnormal eating behaviors. It has been pointed out that patients with ADHD may be relatively inattentive to internal signs of hunger and satiety (Davis et al. 2006). Therefore, they may forget about eating when they are engaged in interesting activities but are more likely to eat when less stimulated.
Another hypothesis is that compulsive eating may be a compensatory mechanism to cope frustration associated with attentional and organizational difficulties (Schweickert et al. 1997). It is also possible that difficulties in initiating activities linked to attentional and organizational problems contribute to decreased caloric expenditure, leading to progressive weight gain (Levitan et al. 2004). Moreover, it has been hypothesized that, since patients with ADHD are susceptible to committing more cognitive effort to take charge of standard mental tasks, it is likely that this cognitive effort accentuates a proneness to an abnormally increased appetite, and the consequent long-term weight gain (Riverin and Tremblay 2009). Finally, other researchers (Waring and Lapane 2008) evoked the role of television, also. Since children with ADHD claim to spend more time watching television, or playing computer or video games to the detriment of exercising, this would contribute to weight gain. However, one cannot exclude the possibility that all the preceding hypotheses hold true, and that the effects on eating behavior may be additive or interactive, at least in certain subjects.
4 Clinical Management of Patients with ADHD and Obesity
4.1 Screening for Both ADHD and Problematic Eating Behavior
From a clinical standpoint, the putative association between ADHD and obesity suggests that it may be useful to screen for ADHD in patients with obesity and also to look for abnormal eating behaviors, as possible contributing factors of obesity. It has been pointed out that clinicians may overlook the need to screen for ADHD in obese patients since “obese individuals are less mobile” and, as a consequence, obesity may mask hyperactivity (Agranat-Meged et al. 2005). However, screening for ADHD in patients with obesity may be relevant since treatment of ADHD might prevent this disorder from exacerbating the personal and social burden of obesity. Conversely, binge eating and other abnormal eating behaviors, which are generally poorly investigated in patients with ADHD, should be screened as well. These abnormal eating behaviors could further compromise the quality of life of ADHD patients and exacerbate their weight gain.
4.2 Therapeutic Strategies
If ADHD contributes to obesity, as hypothesized, then the treatment of ADHD might be expected to prevent obesity. Several reports (Schweickert et al. 1997; Sokol et al. 1999) have suggested that stimulants improve ADHD and restore normal eating behaviors in patients with both conditions. According to some authors (Surman et al. 2006), the treatment of ADHD-related impulsivity could improve abnormal eating behaviors as well. Improvement in attention, leading to more regular eating patterns, may also play a role.
A group of Canadian researchers (Levy et al. 2009) conducted an interesting study in 78 obese patients with a lengthy history of failure to lose weight. After an average of 466 days of continuous ADHD pharmacotherapy, weight loss in treated patients was 15.05 kg, whereas nontreated patients gained weight (3.26 kg). The authors noted the low attrition rate in pharmacologically treated patients and observed that “with the advent of the salutary effects of medication on ADHD symptoms, subjects spoke enthusiastically and in optimistic terms regarding their future plans in life.” Moreover, “improvements in daytime energy, restlessness, distractibility, working memory, impulsivity and mood were instrumental in their successful execution of weight loss plans.” Of note, appetite suppression almost vanished within 2 months. Therefore, it is unlikely that appetite suppression explains the positive outcome in terms of weight control. Finally, subjects reported feeling more alert and energized with treatment. As a consequence, it is likely that this greater physical movement contributed to successful weight control. These interesting clinical observations should be investigated systematically and thoroughly in the future studies.
Indeed, all the above-mentioned studies on pharmacological treatments support the hypothesis that ADHD and abnormal eating behaviors share common underlying biological mechanisms. These could be the common target of ADHD medications. Alternatively, ADHD medications could act on both the brain pathways involved in ADHD and those that mediate abnormal eating behaviors. Interestingly, a trial reported the efficacy of atomoxetine in weight reduction in obese women (Gadde et al. 2006). The positive results of the trial suggested that this ADHD treatment may act on the noradrenergic synapses in the medial and paraventricular hypothalamus that are thought to play a major role in modulating satiety and feeding behavior.
These preliminary observations suggest that in patients with ADHD and abnormal eating behaviors (associated with obesity), both conditions might improve using the same class of agents.
5 Conclusions and Future Perspectives
Converging empirical evidence from recent literature points to a bidirectional association between ADHD and obesity. Both clinical and nonclinical samples indicate that subjects with ADHD have a higher BMI than average, as well as a higher prevalence of obesity/overweight, compared to non-ADHD controls. On the other hand, obese patients present with a higher prevalence of ADHD. To date, there are no data supporting a higher prevalence of ADHD in obese persons, seeking treatment in specialized clinics, from the general population. Evidently, further epidemiological studies exploring the prevalence of ADHD in obese subjects are needed.
Even if the association between ADHD and obesity holds true only in obese patients who seek treatment in specialized clinics, it would still be noteworthy because this is the group of patients with the highest mortality and morbidity risk and the greatest need for effective treatment.
There are other areas of research that deserve further and deeper investigation. First, the potential role of psychiatric comorbidities in explaining the higher prevalence of obesity in ADHD patients should be better addressed in the future. Second, all available studies are cross-sectional prospective and, therefore, they cannot contribute to an understanding of causality: prospective, longitudinal studies, at present, are lacking but could lead to a better understanding of the causal relationship between ADHD and obesity and shed light on the psychopathological pathways linking the two conditions. Third, the exact neurobiological and psychopathological mechanisms underlying the association deserve further exploration. In particular, both family studies, examining the occurrence of ADHD and obesity, and specific animal model studies (which, at present time, are lacking) could advance our knowledge of any common genetic underpinnings. Fourth, only one study (Levy et al. 2009) has assessed the effects of pharmacological treatment of ADHD on weight control in obese patients: further research in this area is warranted. Moreover, non-pharmacological treatment studies and multimodal (pharmacological plus non-pharmacological) ADHD treatment strategies for these patients are greatly needed to help us find more appropriate and effective therapeutic strategies for their weight control.
In summary, clinical empirically based studies, epidemiological surveys (both cross-sectional and prospective), genetic studies, animal model studies, non-pharmacological treatment studies, and pharmacological trials should all be encouraged since they would advance our knowledge in this field, allowing for better management and quality of life for patients with both obesity and ADHD.
Abbreviations
- ADD:
-
Attention-deficit disorder
- BDNF:
-
Brain-derived neurotropic factor
- BMI-SDS:
-
Body mass index standard deviations scores
- CAPA:
-
Child and Adolescent Psychiatric Assessment
- CI:
-
Confidence interval
- CPRS-R:S:
-
Conners Parent Rating Scale-Revised:Short version
- DRD2:
-
Dopamine D2 receptor
- DRD4:
-
Dopamine D4 receptor
- EDS:
-
Excessive daytime sleepiness
- MC4-R:
-
Melanocortin-4-receptor
- NSCH:
-
National Survey of Children’s Health
- OR:
-
Odds ratio
- SAD:
-
Seasonal affective disorder
- SDSC:
-
Sleep Disturbance Scale for Children
- WURS-25:
-
Wender Utah Rating Scale-25
References
Agranat-Meged AN, Deitcher C, Goldzweig G, Leibenson L, Stein M, Galili-Weisstub E (2005) Childhood obesity and attention deficit/hyperactivity disorder: a newly described comorbidity in obese hospitalized children. Int J Eat Disord 37:357–359
Agranat-Meged A, Ghanadri Y, Eisenberg I, Ben NZ, Kieselstein-Gross E, Mitrani-Rosenbaum S (2008) Attention deficit hyperactivity disorder in obese melanocortin-4-receptor (MC4R) deficient subjects: a newly described expression of MC4R deficiency. Am J Med Genet B Neuropsychiatr Genet 147B:1547–1553
Albayrak O, Albrecht B, Scherag S, Barth N, Hinney A, Hebebrand J (2011) Eur J Pharmacol 660(1):165–70
Altfas JR (2002) Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry 2:9
Anderson SE, Cohen P, Naumova EN, Must A (2006) Relationship of childhood behavior disorders to weight gain from childhood into adulthood. Ambul Pediatr 6:297–301
Bazar KA, Yun AJ, Lee PY, Daniel SM, Doux JD (2006) Obesity and ADHD may represent different manifestations of a common environmental oversampling syndrome: a model for revealing mechanistic overlap among cognitive, metabolic, and inflammatory disorders. Med Hypotheses 66:263–269
Biederman J, Faraone SV, Monuteaux MC, Plunkett EA, Gifford J, Spencer T (2003) Growth deficits and attention-deficit/hyperactivity disorder revisited: impact of gender, development, and treatment. Pediatrics 111:1010–1016
Blum K, Sheridan PJ, Wood RC, Braverman ER, Chen TJ, Comings DE (1995) Dopamine D2 receptor gene variants: association and linkage studies in impulsive-addictive-compulsive behaviour. Pharmacogenetics 5:121–141
Braet C, Claus L, Verbeken S, Van VL (2007) Impulsivity in overweight children. Eur Child Adolesc Psychiatry 16:473–483
Chen AY, Kim SE, Houtrow AJ, Newacheck PW (2010) Prevalence of obesity among children with chronic conditions. Obesity (Silver Spring) 18:210–213
Comings DE, Blum K (2000) Reward deficiency syndrome: genetic aspects of behavioral disorders. Prog Brain Res 126:325–341
Cortese S, Isnard P, Frelut ML, Michel G, Quantin L, Guedeney A, Falissard B, Acquaviva E, Dalla BB, Mouren MC (2007a) Association between symptoms of attention-deficit/hyperactivity disorder and bulimic behaviors in a clinical sample of severely obese adolescents. Int J Obes (Lond) 31:340–346
Cortese S, Maffeis C, Konofal E, Lecendreux M, Comencini E, Angriman M, Vincenzi B, Pajno-Ferrara F, Mouren MC, Dalla Bernardina B (2007b) Parent reports of sleep/alertness problems and ADHD symptoms in a sample of obese adolescents. J Psychosom Res 63:587–590
Cortese S, Angriman M, Maffeis C, Isnard P, Konofal E, Lecendreux M, Purper-Ouakil D, Vincenzi B, Bernardina BD, Mouren MC (2008a) Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Crit Rev Food Sci Nutr 48:524–537
Cortese S, Konofal E, Bernardina BD, Mouren MC, Lecendreux M (2008b) Does excessive daytime sleepiness contribute to explaining the association between obesity and ADHD symptoms? Med Hypotheses 70(1):12–16
Cortese S, Faraone SV, Konofal E, Lecendreux M (2009) Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry 48:894–908
Curtin C, Bandini LG, Perrin EC, Tybor DJ, Must A (2005) Prevalence of overweight in children and adolescents with attention deficit hyperactivity disorder and autism spectrum disorders: a chart review. BMC Pediatr 5:48
Davis C, Levitan RD, Smith M, Tweed S, Curtis C (2006) Associations among overeating, overweight, and attention deficit/hyperactivity disorder: a structural equation modelling approach. Eat Behav 7:266–274
Davis C, Patte K, Levitan RD, Carter J, Kaplan AS, Zai C, Reid C, Curtis C, Kennedy JL (2009) A psycho-genetic study of associations between the symptoms of binge eating disorder and those of attention deficit (hyperactivity) disorder. J Psychiatr Res 43:687–696
Engel SG, Corneliussen SJ, Wonderlich SA, Crosby RD, le Grange D, Crow S, Klein M, Bardone-Cone A, Peterson C, Joiner T, Mitchell JE, Steiger H (2005) Impulsivity and compulsivity in bulimia nervosa. Int J Eat Disord 38:244–251
Erermis S, Cetin N, Tamar M, Bukusoglu N, Akdeniz F, Goksen D (2004) Is obesity a risk factor for psychopathology among adolescents? Pediatr Int 46:296–301
Faraone SV, Biederman J, Monuteaux M, Spencer T (2005) Long-term effects of extended-release mixed amphetamine salts treatment of attention- deficit/hyperactivity disorder on growth. J Child Adolesc Psychopharmacol 15:191–202
Fleming JP, Levy LD, Levitan RD (2005) Symptoms of attention deficit hyperactivity disorder in severely obese women. Eat Weight Disord 10:e10–e13
Friedel S, Horro FF, Wermter AK, Geller F, Dempfle A, Reichwald K, Smidt J, Bronner G, Konrad K, Herpertz-Dahlmann B, Warnke A, Hemminger U, Linder M, Kiefl H, Goldschmidt HP, Siegfried W, Remschmidt H, Hinney A, Hebebrand J (2005) Mutation screen of the brain derived neurotrophic factor gene (BDNF): identification of several genetic variants and association studies in patients with obesity, eating disorders, and attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 132:96–99
Gadde KM, Yonish GM, Wagner HR, Foust MS, Allison DB (2006) Atomoxetine for weight reduction in obese women: a preliminary randomised controlled trial. Int J Obes (Lond) 30:1138–1142
Gray J, Yeo GS, Cox JJ, Morton J, Adlam AL, Keogh JM, Yanovski JA, El GA, Han JC, Tung YC, Hodges JR, Raymond FL, O'rahilly S, Farooqi IS (2006) Hyperphagia, severe obesity, impaired cognitive function, and hyperactivity associated with functional loss of one copy of the brain-derived neurotrophic factor (BDNF) gene. Diabetes 55:3366–3371
Heiligenstein E, Keeling RP (1995) Presentation of unrecognized attention deficit hyperactivity disorder in college students. J Am Coll Health 43:226–228
Holtkamp K, Konrad K, Muller B, Heussen N, Herpertz S, Herpertz-Dahlmann B, Hebebrand J (2004) Overweight and obesity in children with Attention-Deficit/Hyperactivity Disorder. Int J Obes Relat Metab Disord 28:685–689
Hubel R, Jass J, Marcus A, Laessle RG (2006) Overweight and basal metabolic rate in boys with attention-deficit/hyperactivity disorder. Eat Weight Disord 11:139–146
Hudson JI, Lalonde JK, Berry JM, Pindyck LJ, Bulik CM, Crow SJ, McElroy SL, Laird NM, Tsuang MT, Walsh BT, Rosenthal NR, Pope HG Jr (2006) Binge-eating disorder as a distinct familial phenotype in obese individuals. Arch Gen Psychiatry 63:313–319
Kernie SG, Liebl DJ, Parada LF (2000) BDNF regulates eating behavior and locomotor activity in mice. EMBO J 19:1290–1300
Lam LT, Yang L (2007) Overweight/obesity and attention deficit and hyperactivity disorder tendency among adolescents in China. Int J Obes (Lond) 31:584–590
Levitan RD, Masellis M, Lam RW, Muglia P, Basile VS, Jain U, Kaplan AS, Tharmalingam S, Kennedy SH, Kennedy JL (2004) Childhood inattention and dysphoria and adult obesity associated with the dopamine D4 receptor gene in overeating women with seasonal affective disorder. Neuropsychopharmacology 29:179–186
Levy LD, Fleming JP, Klar D (2009) Treatment of refractory obesity in severely obese adults following management of newly diagnosed attention deficit hyperactivity disorder. Int J Obes (Lond) 33:326–334
Lourenco BH, Arthur T, Rodrigues MD, Guazzelli I, Frazzatto E, Deram S, Nicolau CY, Halpern A, Villares SM (2008) Binge eating symptoms, diet composition and metabolic characteristics of obese children and adolescents. Appetite 50:223–230
Lyons WE, Mamounas LA, Ricaurte GA, Coppola V, Reid SW, Bora SH, Wihler C, Koliatsos VE, Tessarollo L (1999) Brain-derived neurotrophic factor-deficient mice develop aggressiveness and hyperphagia in conjunction with brain serotonergic abnormalities. Proc Natl Acad Sci U S A 96:15239–15244
Mitsuyasu H, Hirata N, Sakai Y, Shibata H, Takeda Y, Ninomiya H, Kawasaki H, Tashiro N, Fukumaki Y (2001) Association analysis of polymorphisms in the upstream region of the human dopamine D4 receptor gene (DRD4) with schizophrenia and personality traits. J Hum Genet 46:26–31
Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ (2003) Obesity and psychiatric disorder: developmental trajectories. Pediatrics 111:851–859
Nafiu OO, Burke C, Lee J, Voepel-Lewis T, Malviya S, Tremper KK (2010) Neck circumference as a screening measure for identifying children with high body mass index. Pediatrics 126:e306–e310
Nasser JA, Gluck ME, Geliebter A (2004) Impulsivity and test meal intake in obese binge eating women. Appetite 43:303–307
Noble EP (2003) D2 dopamine receptor gene in psychiatric and neurologic disorders and its phenotypes. Am J Med Genet B Neuropsychiatr Genet 116:103–125
Pagoto SL, Curtin C, Lemon SC, Bandini LG, Schneider KL, Bodenlos JS, Ma Y (2009) Association between adult attention deficit/hyperactivity disorder and obesity in the US population. Obesity (Silver Spring) 17:539–544
Poston WS, Ericsson M, Linder J, Haddock CK, Hanis CL, Nilsson T, Astrom M, Foreyt JP (1998) D4 dopamine receptor gene exon III polymorphism and obesity risk. Eat Weight Disord 3:71–77
Ptacek R, Kuzelova H, Paclt I, Zukov I, Fischer S (2009) Anthropometric changes in non-medicated ADHD boys. Neuro Endocrinol Lett 30:377–381
Riverin M, Tremblay A (2009) Obesity and ADHD. Int J Obes (Lond) 33:945
Rosval L, Steiger H, Bruce K, Israel M, Richardson J, Aubut M (2006) Impulsivity in women with eating disorders: problem of response inhibition, planning, or attention? Int J Eat Disord 39:590–593
Schweickert LA, Strober M, Moskowitz A (1997) Efficacy of methylphenidate in bulimia nervosa comorbid with attention-deficit hyperactivity disorder: a case report. Int J Eat Disord 21:299–301
Shinawi M, Sahoo T, Maranda B et al (2011) 11p14.1 microdeletions associated with ADHD, autism, developmental delay, and obesity. Am J Med Genet A 155:1272–1280
Sokol MS, Gray NS, Goldstein A, Kaye WH (1999) Methylphenidate treatment for bulimia nervosa associated with a cluster B personality disorder. Int J Eat Disord 25:233–237
Spencer TJ, Biederman J, Harding M, O'Donnell D, Faraone SV, Wilens TE (1996) Growth deficits in ADHD children revisited: evidence for disorder-associated growth delays? J Am Acad Child Adolesc Psychiatry 35:1460–1469
Spencer TJ, Faraone SV, Biederman J, Lerner M, Cooper KM, Zimmerman B (2006) Does prolonged therapy with a long-acting stimulant suppress growth in children with ADHD? J Am Acad Child Adolesc Psychiatry 45:527–537
Strimas R, Davis C, Patte K, Curtis C, Reid C, McCool C (2008) Symptoms of attention-deficit/hyperactivity disorder, overeating, and body mass index in men. Eat Behav 9:516–518
Surman CB, Randall ET, Biederman J (2006) Association between attention-deficit/hyperactivity disorder and bulimia nervosa: analysis of 4 case-control studies. J Clin Psychiatry 67:351–354
Swanson J, Greenhill L, Wigal T, Kollins S, Stehli A, Davies M, Chuang S, Vitiello B, Skrobala A, Posner K, Abikoff H, Oatis M, McCracken J, McGough J, Riddle M, Ghuman J, Cunningham C, Wigal S (2006) Stimulant-related reductions of growth rates in the PATS. J Am Acad Child Adolesc Psychiatry 45:1304–1313
Tsai SJ, Hong CJ, Yu YW, Chen TJ (2004) Association study of catechol-O-methyltransferase gene and dopamine D4 receptor gene polymorphisms and personality traits in healthy young chinese females. Neuropsychobiology 50:153–156
Vgontzas AN, Bixler EO, Chrousos GP (2006) Obesity-related sleepiness and fatigue: the role of the stress system and cytokines. Ann N Y Acad Sci 1083:329–344
Waring ME, Lapane KL (2008) Overweight in children and adolescents in relation to attention-deficit/hyperactivity disorder: results from a national sample. Pediatrics 122:e1–e6
Weinberg WA, Brumback RA (1990) Primary disorder of vigilance: a novel explanation of inattentiveness, daydreaming, boredom, restlessness, and sleepiness. J Pediatr 116:720–725
Zametkin AJ, Zoon CK, Klein HW, Munson S (2004) Psychiatric aspects of child and adolescent obesity: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 43:134–150
Acknowledgment
Dr. Cortese is supported by a grant from European Union “International outgoing fellowship, Marie Curie actions, FP7 Program, # PIOF-GA-2009-253103.”
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Cortese, S., Vincenzi, B. (2011). Obesity and ADHD: Clinical and Neurobiological Implications. In: Stanford, C., Tannock, R. (eds) Behavioral Neuroscience of Attention Deficit Hyperactivity Disorder and Its Treatment. Current Topics in Behavioral Neurosciences, vol 9. Springer, Berlin, Heidelberg. https://doi.org/10.1007/7854_2011_154
Download citation
DOI: https://doi.org/10.1007/7854_2011_154
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-24611-1
Online ISBN: 978-3-642-24612-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)