Abstract
Biological markers have served for diagnosis, risk stratification and guided therapy of heart failure (HF). Our knowledge regarding abilities of biomarkers to relate to several pathways of HF pathogenesis and reflect clinical worsening or improvement in the disease is steadily expanding. Although there are numerous clinical guidelines, which clearly diagnosis, prevention and evidence-based treatment of HF, a strategy regarding exclusion of HF, as well as risk stratification of HF, nature evolution of disease is not well established and requires more development. The aim of the chapter is to discuss a role of biomarker-based approaches for more accurate diagnosis, in-depth risk stratification and individual targeting in treatment of patients with HF.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Heart failure (HF) is a leading cause of premature cardiovascular (CV) death in patients with established CV disease (Ponikowski et al. 2016). Prevalence of HF has been exhibiting a tendency to worldwide, despite the scientific progress in the field of the two past decades. HF is also characterized by an elevated rate of primary and secondary hospitalization and increased economic burden for patients and their families. Although there are numerous clinical guidelines, which clearly indicated diagnosis, prevention and evidence-based treatment of HF, a strategy regarding exclusion of HF diagnosis, as well as risk stratification of HF, nature evolution of disease is not well established and requires more development (Wettersten and Maisel 2016). In this context, biological markers reflected several pathophysiological stages of HF have become a powerful and convenient noninvasive tool for diagnosis of HF, a stratification of HF patients at risk of progression, HF severity, and biomarker-guided therapy (Ledwidge et al. 2013). The aim of the chapter is to discuss a role of biomarker-based approaches for more accurate diagnosis, in-depth risk stratification and individual targeting in treatment patients with HF.
2 Conventionally Used Biomarkers of Heart Failure
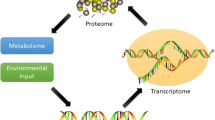
According to The Biomarkers Definitions Working Group Biomarkers are defined as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention (Biomarkers Definitions Working Group (National Institutes of Health) 2001).There are numerous of biomarkers, which reflect several pathophysiological stages of HF and allow stratifying individuals at risk (Fig. 1). Currently updated clinical recommendations have been reported that the natriuretic peptides (NPs), including brain NP (BNP), mid-regional pro-atrial NP (MR-proANP), NT-pro-brain NP (NT-proBNP), mid-regional pro-brain NP (MR-proBNP), are the most frequently used biomarkers in clinical practice to stratify patients at risk of cardiac dysfunction, a risk of admission/readmission to the hospital due to HF-related reasons, and a risk of death (Pouleur 2015), while galectin-3, high-sensitivity cardiac troponins and soluble suppressor of tumorigenicity-2 (sST2) receptor are thought to be promising biomarkers in this respect (Table 1). Most data on cardiac biomarkers have been derived from chronic HF individuals. In contrast, risk prediction in patients admitted to hospital with acute HF remains a challenge.
2.1 Natriuretic Peptides
First NPs were recommended by the European Society of Cardiology and American Heart Association for exclusion HF, and then they were discussed as a tool for risk stratification, and NPs-guided therapy (Ponikowski et al. 2016; Wettersten and Maisel 2016). The majority of NPs’ family members (Atrial NP [ANP] and brain [BNP] apart from C-type of NP [CNP]) are mechanical stress-related markers. They are actively released by cardiomyocytes as a result in fluid overload, cardiac stretching, as well as due to exposure to other causes, e.g. ischemia/ necrosis, metabolic and toxic damage, membrane stability loss, and inflammation (Berezin 2017a). ANP is released from atrial granules upon acute volume overload, whereas BNP is stressed-related peptide that does not accumulate before stimulation. In contrast, CNP is secreted from activated endothelial cells and renal cells in response to cytokine activation and through endothelium-dependent agonists, e.g. acetylcholine (Berezin 2017a). The biological effects of ANP and BNP are mediated by binding with appropriate NP receptor type A (NPRA). NPRA are expressed at the surfaces of the target cells and are linked with cGMP mediating water/electrolyte homeostatic effects, i.e. diuresis/natriuresis, increasing glomerular filtration rate, volume of circulating plasma, suppressing systemic sympathetic activities, maintenance of cardiac output and regulation of blood pressure. NPs may demonstrate anti-proliferative activity and anti-mutagenic effect, mediate vascular dilatation and prevent vascular wall hypertrophy (Berezin 2017a). Additionally, NPs show modest anti-aldosterone and endothelin-1 effects.
In patients with HF the plasma levels of BNP and NT-proBNP are typically >100 pg/ml and >250 pg/mL, respectively, while there is high individual biological variability of both biomarkers irrespective of presentation of HFrEF or HFpEF (Felker et al. 2017). Elevated levels of NPs are well correlated with clinical status and severity of HFrEF/HFpEF patients, a risk of developing acute HF regardless etiology of the disease, risk of hospital admission/re-admission, as well as all-cause mortality, CV and HF death in individuals with established HF including at discharge from the hospital after treating HF decompensation (Feng et al. 2017). More recent evidence suggests that NPs along with the next generation of CV biomarkers could provide added predictive value to drug therapy of HF, which could potentially lower HF-related risk of outcomes (Fonarow 2017; Chow et al. 2017).
2.2 Biomarkers of Myocardial Fibrosis
2.2.1 Galectin-3
Galectin-3 is a soluble β-galactoside-binding protein, which is actively secreted by activated mononuclears and macrophages due to inflammatory stimulation. The main biological function of galectin-3 is to activate the fibroblasts for further collagen synthesis (Yancy et al. 2017). Recent pre-clinical and clinical studies have revealed the pivotal role of galectin-3 in progressive accumulation of extracellular matrix leading to cardiac fibrosis, cardiac remodeling, and worsening cardiac performances associated with impaired cardiac systolic and diastolic function, dilation of cardiac cavities, and induction of cardiac arrhythmias (Boulogne et al. 2017a; Souza et al. 2017). Galectin-3 in elevated concentrations was measured in a serum of the patients at risk of HF and CV disease (Lala et al. 2017). In patients with acute HF galectin-3 associated with NT-proBNP levels and the estimated glomerular filtration rate but not with age and serum cardiac troponins (Imran et al. 2017). Galectin-3 was not superior to NT-proBNP, sST2 receptor, Growth Differentiation Factor (GDF)-15 or high-sensitive C-reactive protein (hsCRP) in prediction of CV mortality and HF death, while the combination of galectin-3 and NPs was more accurate in predicting HF death compared to either of the biomarkers alone (Besler et al. 2017a).
2.2.2 Soluble Suppressor of Tumorigenicity-2 Receptor
Soluble suppressor of tumorigenicity-2 receptor (sST2) belongs to the interleukin (IL)-1 receptor family members, which has two isoforms, i.e. membrane-bound (ST2L) and soluble (sST2) isoforms. sST2 interacts with its ligand IL-33 and through myocardial mRNA expressions of Th1-related cytokines (tumor necrosis factor-alpha) may directly enhance cardiac hypertrophy, fibrosis, cavity dilation with impaired cardiac function (Berezin 2017a).
The serum levels of sST2 in acute HF were dramatically increased on admission and appeared to be decreased rapidly depending on clinical improvement. Therefore, sST2 in HF has well correlated with BNP and GDF15 levels (Srivatsan et al. 2015). sST2 levels at discharge were better predictor of HF re-admission than ones at admission (Boulogne et al. 2017b). Although both biomarkers of myocardial fibrosis (sST2 receptor and galectin-3) are predictive of HF-related admission to the hospital and CV death (Billebeau et al. 2017), direct head-to-head comparison of sST2 and galectin-3 revealed superiority of sST2 over galectin-3 in HF risk stratification (Bayes-Genis et al. 2014).
2.3 Biomarkers of Myocardial Injury
Development and progression of HF strongly relates to direct and indirect damages of cardiac cells by effect of etiological factors of cardiac dysfunction (i.e. ischemia/necrosis, inflammation, hypoxia, hypertrophy, fibrosis) as well as by other factors contributing to the pathogenesis of HF (i.e., biomechanical stress due to cardiac remodeling, iron deficiency, oxidative stress/mitochondrial dysfunction). Biomarkers of myocardial injury may be detected in peripheral blood in elevated concentration as a result of leakage through cardiac cell membranes and due to injury of cells. However, regardless of the main cause of cell dysfunction, biomarkers of cardiac cell injury reflect a wide range of pathophysiological process: from instability of lipid layers of membrane due to lipid peroxidation to destroying cell due to necrosis/apoptosis (Berezin 2017a).
There are some biomarkers of myocardial injury and necrosis (cardiac troponins T and I, myoglobin, heart type of fatty acid binding protein, glutathione transferase P1), which are investigated in details as potential predictors of HF onset and HF-related outcomes (Anguita 2017). Since last two decades high-sensitivity cardiac troponins had been suggested to be prognosticators of high risk of CV mortality and combined adverse CV outcomes in HF (Nagarajan et al. 2012; Masson et al. 2010).
3 Biomarker-Guided Therapy of HF
It had been found that NP guided HF therapy improved titration of medications (Feng et al. 2017; Fonarow 2017), but did not lead to better HF clinical outcomes (Wettersten and Maisel 2016; Berezin 2017a). Meanwhile, serial measurements of NPs could be useful for determining the severity of HF for decision about ambulatory and in-hospital medical care. Additionally, NT-proBNP, but not BNP, is better suited during HF therapy based on the new angiotensin-receptor-neprilysin-inhibitor (ARNI) (Malek and Gaikwad 2017). The clinical trials have shown that neprilysin inhibition together with chronic renin-angiotensin system blockage with Sacubitril/Valsartan may increase the bioavailability of NPs and promotes additional cardio-renal benefits and thereby reduce all-cause mortality, CV mortality and HF death (Wong et al. 2017). Because biologically active BNP is degraded by neprilysin, in HF patients treated with ARNI circulating level of BNP sufficiently increases, whereas NT-proBNP concentration declines dramatically. In such situations the principles of NPs-based HF guided therapy are become complicated. Apparently, monitoring of BNP levels is not suitable for risk stratification and HF adjusted medical care, when ARNIs are used, however, NT-proBNP remains useful for risk assessment and HF stratification regardless drug prescriptions (Luchner et al. 2017; Aspromonte et al. 2016; Skaf et al. 2017; Nakanishi et al. 2017). Finally, majority of experts believe that a combination of biomarkers may ultimately prove to be more informative in their predictive ability than single biomarker (Nymo et al. 2017).
4 Limitations in Use of Conventional Biomarkers in HF
Confusingly, the role of NPs in modification of treatment considerably relates to aging, CV disease, metabolic co-morbidities, kidney clearance, metabolism (neprilysin for BNP, glycosylation, methylation, oxidation for other NPs), toxic effect (cardiotoxicity) (Berezin 2016a). Therefore, higher individual biological variability of these biomarkers may impair interpretation of the measured results (Favresse and Gruson 2017). There is a big list of diseases associated with increased level of NPs beyond HF development (Table 2).
Although galectin-3 is an independent predictor of all-cause mortality, CV death and occurrence of HF, there is an inverse relationship between serum galectin-3 level and estimated glomerular filtration rate (Besler et al. 2017b). Accordingly, lowered kidney clearance should be taken into consideration, when data of galectin-3 measurement are interpreted. Therefore, older patients contributed to higher galectin-3 concentrations than younger individuals (Krintus et al. 2017). Amongst other biomarkers (NPs, GDF-15, high-sensitivity troponin T, sST2, aldosterone, phosphate, parathyroid hormone, plasma renin, and creatinine), galectin-3 had the lowest individual biological variability, whereas NPs and GDF-15 had the highest ones (Meijers et al. 2017). In contrast to NPs serum galectin-3 levels did not appear to be significantly related to circulating level of cardiac troponins, left ventricular (LV) ejection fraction and LV mass index (Agnello et al. 2017). However, there was a positive correlation between galectin-3 levels and NT-proBNP in HF individuals. Thus, galectin3 and NPs might be considered as the best markers for both short- and long term death prediction in HF regardless kidney function and age. Unfortunately, no biomarker predicted the short-term composite HF endpoints in acute HF (Miró et al. 2017). Additionally, there are controversial findings related to the lack of association of galectin-3 concentration with adverse outcomes in chronic HF (Wojciechowska et al. 2017).
Even sST2 was not associated with age, female sex, LV structure or LV systolic or diastolic function (Maisel and Di Somma 2016; Berezin 2016b; AbouEzzeddine et al. 2017). Thus, these findings confirmed that the sST2 is a marker of systemic inflammation and fibrosis with predictive ability regarding all-cause and CV death in HF (AbouEzzeddine et al. 2017; Aimo et al. 2017).
5 Novel Biomarkers for HF Management
The discovery of new biomarkers is promising, but rarely novel molecules prove to be significantly better in diagnostic and predictive value than the established biomarkers. In addition to the various types of NPs, galectin-3, sST2, high-sensitive cardiac troponins, several other biomarkers have been investigated to be better predictors in HF (Table 3).
5.1 Procalcitonin
Procalcitonin is propeptide of calcitonin, which is normaly produced and actively secreted by the parafollicular C cells of the thyroid gland (Ryu et al. 2015). Procalcitonin/calcitonin axis is essential for regulation of calcium homeostasis and immunity (Berezin 2017a). The preclinical and clinical studies have shown that extra-thyroidal production of procalcitonin markedly increases in cases of systemic inflammatory reaction, severe infections (viral, bacterial, fungal and parasitic), and shock (Reiner et al. 2017; Hayashida et al. 2017; Simon et al. 2004). Although serial measurements of procalcitonin are recommended to discriminate of in-hospital mortality in various diseases associated with pro-inflammatory activation (pneumonia, chronic obstructive pulmonary disease, acute respiratory tract infections, sepsis, etc.), there is evidence that the serum procalcitotin levels might be a predictive biomarker for chronic HF (Simon et al. 2004). Large clinical trials are required to obtain evidence for a predictive role of procalcitonin in exacerbated HF individuals.
5.2 Copeptin
Copeptin is C-terminal derivative of the arginine vasopressin that normally acts as regulator of water and electrolyte homeostasis (Morgenthaler 2006). Although plasma levels of copeptin are very variable and tightly relate to blood/urine osmolality, copeptin appears to be in higher concentrations in sever hypertension, stroke, acute and chronic HF, myocardial infarction, diabetes mellitus, advanced kidney diseases, and in critical conditions. As quantitative biomarker of endogenous biomechanical stress elevated level of copeptin was found in close positive association with increased CV mortality and CV disease in out-patients and all-cause mortality in critical states (Remde et al. 2016). There is a large body of evidence that the serial measurements of copeptin level may be provide an important information for discrimination of a risk of all-cause mortality, HF-related outcomes and CV events and diseases (Moayedi and Ross 2017; Krane et al. 2017; Yan et al. 2017a; Berezin 2015a). Although both increased NT-proBNP levels and copeptin levels were recognized significant independent predictors of adverse clinical outcomes in HF, the role of dual marker contribution in HF risk stratification remains to be clarified (Savic-Radojevic et al. 2017; Smaradottir et al. 2017; Sahin et al. 2017; Herrero-Puente et al. 2017).
5.3 Heart Type of Fatty Acid Binding Protein
The heart type of fatty acid binding protein (hFABP) is normally essential for the long-chain fatty acids re-uptake, regulation of calcium homeostasis in cardiomyocytes and mediating inflammatory reaction (Chmurzynska 2006). Because hFABP is tissue-specific biomarker of myocardial injury and necrosis, it is reserved as predictor of myocardial infarction at the early hours of development of the disease. Recent studies have shown that circulating levels of hFABP are elevated in cardiac dysfunction and closely predicted CV outcomes and HF-related events in in-patients especially in those who had fluid retention and lung congestion (Savic-Radojevic et al. 2017; Chmurzynska 2006; Qian et al. 2016; Kitai et al. 2017). Although elevated serum level of hFABP yielded better prognostic information on survival in individuals with acute and advanced HF when compared to NPs, cardiac troponins and even galectin-3 taken alone, there is confusion about the improved precision of entire predictive model after incorporating hFABP to NPs and/or galectin-3 (Savic-Radojevic et al. 2017; Qian et al. 2016; Kitai et al. 2017).
5.4 Growth Differentiation Factor-15
Growth differentiation factor (GDF)-15 is multifunctional cytokine that belongs to the transforming growth factor-β superfamily (Kempf and Wollert 2009). GDF-15 is normally expressed in various cells including immune cells, fibroblasts, myocardial cells, endothelial cells, and mononuclears. Additionally, GDF-15 is actively secreted into circulation by cardiac myocytes due to stretching and biochemical stress (Berezin 2015a; Kempf and Wollert 2009; Chan et al. 2016).
Serum levels of GDF-15 are associated with increased risk of all-cause death independent of age, clinical signs and symptoms of cardiac dysfunction, LVEF, renal function and NPs in HF (Hage et al. 2017). Interestingly, in in-patients with acute HF the serum levels of GDF-15 were not better to NPs and galectin-3 taken alone in accuracy to predict HF-related outcomes including death and re-admission to the hospital after discharge (Demissei et al. 2017). In contrast, out-patients with chronic HFrHF/HFpEF may be candidates to multiple predictive biomarker strategy based on collective measurement of NPs, GDF-15, and galectin-3 (Berezin et al. 2015a; Berezin 2015b).
5.5 Endothelial Cell-Derived Micro Particles and Endothelial Progenitor Cells
Impaired endothelial function plays a pivotal role in HF development and HF-related complications and also associates with an appearance in the peripheral blood of specific circulating biomarkers, i.e. endothelial microparticles (EMPs) and endothelial progenitor cells (EPCs) (Berezin et al. 2015a; Berezin 2015b; Berezin at al. 2016). Recent clinical studies have shown that an ability of mature endothelial cells and their precursors to release of secretom progressively worse depended on HF stage and severity (Berezin 2015b, c; Berezin et al. 2014a, 2015b, 2016c). There is novel HF risk prediction score created by means of biomarkers, e.g. NPs, galectin-3, high sensitive CRP and estimated ratio between both numbers of apoptotic EMPs and EPCs (Berezin et al. 2015b; Berezin 2015d). However, it is not clear whether new predictive models would be effective in HF treatment. More clinical trials are required to improve our understanding in the field of individualized therapy of HF under biomarker control.
5.6 Biomarkers of Collagen Metabolism
Recent studies have shown that impaired collagen metabolism may alter the myocardial collagen network, enable cardiovascular remodeling, and mediates HF complications, i.e. atrial fibrillation/flutter, sudden death, and decline in LV pump function (Löfsjögård et al. 2014). Interestingly, there is evidence regarding causative role of BNP in alterations in collagen type I metabolism in HFrEF (Berezin 2016c). The OPTIMAL (The Optimizing Congestive Heart Failure Outpatient Clinic trial) revealed that disturbances of collagen type I metabolism are independent predictors of long-term, all-cause mortality and CV mortality in HFrEF individuals (Löfsjögård et al. 2017). Therefore, circulating CITP is probably an independent predictor of survival in patients with HFrEF (Tziakas et al. 2012).
5.7 Matrix Metalloproteinases
Development of HF strongly associates with CV remodeling, biomechanical and oxidative myocardial stress, neurohormonal and inflammatory activation that are modulated by matrix metalloproteinases (MMPs). It has demonstrated that MMPs determine extracellular accumulation of collagen and mediate pro-fibrotic processes (Berezin and Samura 2013). Recent pre-clinical and clinical studies have shown that an impairment of cardiac function may relate to the collagen accumulation due to an imbalance between expression of MMPs, predominantly MMP-1, MMP-3, MMP-6, MMP-9, and suppression of their tissue inhibitors (Collier et al. 2011; Hutchinson et al. 2010; Berezin et al. 2015c). However, the predictive value of these biomarkers was not confirmed and requires more future investigations.
5.8 Biomarkers of Oxidative Stress
5.8.1 Serum Uric Acid
Observational and clinical studies have shown that the elevated level of serum uric acid (SUA) is a common feature in patients with HF, hypertension, atherosclerosis, obesity, diabetes mellitus and chronic renal disease (Grassi et al. 2013; Borghi et al. 2015). The role of SUA in pathogenesis of CV disease is controversial. On the one hand, SUA induces an oxidative stress through over-production of reactive oxygen species. SUA often impairs vascular function via enhancement of inflammatory damage, inducing vascular calcification and directly via cell membranes deterioration effect (Grassi et al. 2013). On the other hand, low-grading inflammation that is frequently found in HF may cause xanthine oxidase over-activity and leads to increased tissue SUA accumulation, which acts as scavenger of free radicals and protects against an damaging effect of oxidative stress (Berezin and Kremzer 2013; Berezin 2014). Additionally, an increase of SUA may be an attribute of lowered kidney clearance in a progress of HF. Therefore, there is evidence regarding the regulatory role of SUA in EPC differentiation that allow discussing uric acid as a mediator of reparation of tissues in HF (Berezin et al. 2014b).
Numerous clinical studies have emphasized the predictive role of baseline SUA for early post-discharge HF outcomes (Amin et al. 2017; Okazaki et al. 2016, 2017). Interestingly, the activity of xanthine oxidoreductase that is a key rate-limiting enzyme of purine degradation may be more accurate predictor of HFrEF severity and HF clinical outcomes than SUA (Otaki et al. 2017; Huerta et al. 2016; Kim et al. 2013). Consequently, SUA remains an established risk factor of clinical outcomes in acute HF (Berezin 2017b), while poor prognosis in patients with chronic HF is not elucidated (Berezin 2017c).
5.8.2 Other Biomarkers of Oxidative Stress
Serum levels of myeloperoxidase, vitamin D3, ceruloplasmin and 8-hydroxy-2′-deoxyguanosine correlate with staging of chronic HF regardless of LVEF and predict a development of HFrEF, while the role of these biomarkers of oxidative stress remains under discussion (Chan et al. 2016; Mozos et al. 2017). Although there is evidence regarding the close link between vascular remodeling (Berezin 2017d; Mozos and Marginean 2015), endothelial dysfunction and CV disease the predictive role of vitamin signature in serum (i.e., vitamin A, B12, D, K, C and E) in HF individuals is not still clear and requires to be investigated (Berezin 2017c).
5.9 Biomarkers of Renal Dysfunction in HF
5.9.1 Cystatin C
Cystatin C is an endogenous inhibitor of cysteine proteases and this biomarker is discussed as an alternative predictor of CV events in acute and chronic HF patients with any types of cardiorenal syndrome (Kim et al. 2013). The patients with HFrEF demonstrated elevated serum cystatin C, especially in cases with serious risk of CV complications (Kim et al. 2013). Additionally, increased cystatin C level in hypertensive patients with HFpEF was found (Berezin 2017d). It appears to be associated with LV diastolic dysfunction and alterations in collagen metabolism regardless of estimated GFR (Berezin 2017d). Although cystatin C has now validated a powerful predictor of CV outcomes and kidney injury, its sensitivity in patients with chronic HF is inferior to that of hs-CRP and NPs (Berezin 2017c). In contrast, in acute HF Cystatin C provided an incremental value for prognosis more than NT-proBNP and uric acid (Kim et al. 2015; Taub et al. 2012).
5.9.2 Other Biomarkers of Kidney Injury in HF
There are many perspective biomarkers of kidney injury that could be useful for stratification of HF at risk, i.g. stromal cell-derived factor-1, exosomes, MPs, neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1, interleukin-18 and miRNAs (Berezin 2017d; Taub et al. 2012). Although they are at the early stages of renal dysfunction prior to any elevations in serum creatinine, the prognostication of clinical outcomes in acute HF and chronic HF require more investigations.
5.10 Genetic Biomarkers
By now, genetic testing has incorporated as a part of patient evaluation for suspected inherited cardiomyopathies (Teekakirikul et al. 2013; Teo et al. 2015). It turns out the epigenetic modifications through DNA methylation, ATP-dependent chromatin remodeling, histone modifications with an involvement of microRNA-related mechanisms might be sufficient pathophysiological factors contributing to adverse cardiac remodeling and altered cardiac function (Hershberger and Siegfried 2011). In this context, the novel risk scores reflecting variabilities in genetic and epigenetic features in HF development appear to be promising (Berezin 2016d; Yang et al. 2015; Lopes and Elliott 2013). Indeed, some early studies have reported interesting results with respect to genetic precursors of HFpEF and HFrEF (Berezin 2016e; Fazakas et al. 2016; McNamara et al. 2014; Friedrich et al. 2013; Hofman et al. 2010; Sutter et al. 2013; Kolder et al. 2012). There are numerous studies depicted the role of single nucleotide polymorphisms (SNPs) of genes encoding enzymes related to oxidative stress (Berezin 2016e), genotype of guanine nucleotide-binding proteins (G-proteins) beta-3 subunit (GNB3) (Fazakas et al. 2016), transcription factor Islet-1 gene (McNamara et al. 2014), troponin T (Friedrich et al. 2013), CYP2D6 polymorphism (Hofman et al. 2010), cardiac myosin binding protein-C mutations (Sutter et al. 2013), renin-angiotensin-aldosterone system polymorphism (Kolder et al. 2012) etc. in HF development and progression. It is well known that angiotensin-converting enzyme (ACE) I/D gene D allele was associated with higher overall mortality as compared with the I allele in HF patients and that the effect could be modified by ACE inhibitors’ given (Wu et al. 2010). Additionally, ACE DD and angiotensin-1-receptor 1166 CC genotypes may synergistically increase the predisposition to HFpEF (Kolder et al. 2012; Wu et al. 2009, 2010).
The ARIC (Atherosclerosis Risk in Communities) study reported that none of the metabolite SNPs including pyroglutamine, dihydroxy docosatrienoic acid were individually associated with incident HF, whereas a genetic risk score created by summing the most significant risk alleles from each metabolite determined 11% greater risk of HF per allele (Yu et al. 2013). (Ganna et al. 2013) have reported that amongst 707 common SNPs associated with 125 diseases including HF it would not be easy to obtain explainable results by common genetic variants related to HF development. Consequently, a close gene-gene interaction may determine an individual’s risk of HF through different pathways including epigenetic modifications. All these findings lead to the assumption that genes score might be a powerful tool for prediction of HF development.
More successful genome-wide linkage studies toward genes-related contribution in HF have been done by incorporating SNPs of several genes (i.g. the bradykinin type 1 receptor gene, angiotensin-II type I receptor gene, the β1-adrenoceptor gene and CYP2D6 polymorphism) in predictive score to benefit and suffer harm from HF therapy. Although these pharmacogenetic studies have focused on promised topics, the obtained results have not been absolutely consistent (Ganna et al. 2013; Yip and Pirmohamed 2013; Nelveg-Kristensen et al. 2015). In contrast, there is evidence that the gene expression profiles might be useful rather for risk prediction in HF than for choosing HF treatment regime (Bondar et al. 2014; Berezin 2016f). Thus, the clinical implementation of the HF therapy based on genes scoring remains uncertain and requires more evaluation in the future (Poller et al. 2017).
5.11 Micro-RNAs
It has been established that microRNAs (miRNA) are involved in the development and progression of HF across all pathophysiological stages of the disease (Berezin 2016d). miRNA are epigenetic regulators of myocardial response and fibrosis, growth of cardiac myocytes, cardiac and vasculature reparation, immunity, angiogenesis, and inflammation (Berezin 2016e). The altered miRNA’ signature was found in patients with asymptomatic and symptomatic HF (Jin et al. 2017; Vegter et al. 2017; Yan et al. 2017b). It has suggested the signatures of non-coding RNAs would be candidate to improve diagnosis and prognostication of HF (Wong et al. 2014).
5.12 Mid-Regional pro-Adrenomedullin
Mid-regional pro-adrenomedullin (MR-proADM) is the prohormone of the CV protein adrenomedullin and it is well-established neurohumoral marker of cardiac biochemical stress that is raised in patients with infections, acute dyspnea, acute HF, severe chronic HFrEF/HFpEF, unstable angina pectoris/myocardial infarction, and throughout the first week after stroke (Bustamante et al. 2017). There is evidence that the MR-proADM is an early predictor of in-hospital mortality due to various reasons, i.e. respiratory infections, surgical procedure and CV diseases (Odermatt et al. 2017; Dres et al. 2017; Lopes and Menezes Falcão 2017). MR-proADM as a marker of biomechanical stress and fibrosis was not better than NPs and did not exhibit equal predictive value to sST2r and galectin-3 in HFrEF/HFpEF (Lopes and Menezes Falcão 2017). Interestingly, sST2 was better to MR-proADM, because it is more closely related to left ventricular remodeling and cardiac fibrosis. Moreover, MR-proADM did not improve a risk stratification based on NPs in patients with chronic HFrEF and moderate anaemia (Welsh et al. 2017). Thus, the role of MR-proADM as a component of biomarker-based stratification is discussable, may contribute to determine the short-term outcomes of critical ill patients with acute severe dyspnea, respiratory infection and acute HF.
6 Validation of Multiple Biomarker Predictive Scores
Despite several predictive scores based on biomarkers’ measurement and approved for chronic HF, predictive scores for acute HF have not been validated (Bayes-Genis and Ordonez-Llanos 2015; Cohen-Solal et al. 2015). Current multiple biomarker scores for prognostication, risk stratification and diagnosis of HF (Fig. 2) are based on NPs in combination with biomarkers of myocardial injury and fibrosis (galectin-3 and sST2 receptor). A new score was validated by the American Heart Association/American College of Cardiology (2017), suitable for patients at risk of HF, with established chronic HF (for both HFrEF and HFpEF), with suspected and documented acute HF (at admission), as well as patients with HF at discharge from the hospital.
Practical use of various biomarkers in HF development and progression
Abbreviations: ADHF actually decompensated heart failure, pts patients, Gal-3 galectin-3, NT – proBNP NT-pro-brain natriuretic peptide, BNP brain natriuretic peptide, TrT troponin T, TrI troponin I, sST2 soluble suppressor of tumorigenicity-2 receptor
Interestingly, there are several attempts regarding use of biomarkers to stratify at risk patients with HFrEF and HFpEF. Whether add-on biomarkers are needed to improve cumulative predictive value for wide spectrum of HF individuals with different HF phenotypes, co-morbidities, ages and sex-related peculiarities is not fully clear. There is no clarity and consistent evidence for multiple biomarker strategy in improvement in CV mortality and CV outcomes. It has been suggested that sST2 and galectin-3 could improve prognosis in HF-related hospitalization and CV death, when added to NPs. This strategy is confirmed by experts of various medical associations and is the only one that is validated now (Chow et al. 2017).
7 Conclusions
There are many controversies regarding the importance of biomarkers as predictors of survival and in diagnosis of HF. Improvement of clinical guideline recommendations for optimizing HF therapy in routine clinical practice under biomarkers’ control is required. Obviously, galectin-3 or sST2r would be optimal for improving NPs- based biomarker strategy in HF individuals, while there is evidence regarding other biomarkers that could individualize stratification of risk and treatment. There is need of larger clinical trials in order to head-to-head compare different biomarkers and clarify their role in diagnosis and guided therapy of HF.
Abbreviations
- ADM:
-
adrenomedullin
- ANP:
-
atrial natriuretic peptide
- ARNI:
-
angiotensin receptor neprilysin inhibitors
- BNP:
-
brain natriuretic peptide
- BRPs:
-
bone related proteins
- cGMP:
-
cyclic guanylyl monophosphate
- CITP:
-
carboxy-terminal telopeptide
- CNP:
-
C-type natriuretic peptide
- CRP:
-
C-reactive protein
- CT-proET-1:
-
C-terminal-pro-endothelin-1
- CV:
-
cardiovascular
- EMPs:
-
endothelial microparticles
- EPCs:
-
endothelial progenitor cells
- Gal-3:
-
galectin-3
- GDF-15:
-
Growth differentiation factor-15
- HF:
-
heart failure
- hFABP:
-
heart type of fatty acid binding protein
- HFpEF:
-
heart failure with preserved ejection fraction
- HFrEF:
-
heart failure with reduced ejection fraction
- LV:
-
left ventricular
- MMP:
-
matrix metalloproteinase
- MPs:
-
micro particles
- MR-proANP:
-
mid-regional pro-atrial natriuretic peptide
- MR-proADM:
-
mid-regional pro-adrenomedullin
- NPs:
-
natriuretic peptides
- NT-proBNP:
-
NT-pro-brain natriuretic peptide
- PICP:
-
carboxy-terminal propeptide
- sST2:
-
soluble suppressor of tumorigenicity-2 receptor
References
AbouEzzeddine OF, McKie PM, Dunlay SM, Stevens SR, Felker GM, Borlaug BA et al (2017) Suppression of tumorigenicity 2 in heart failure with preserved ejection fraction. J Am Heart Assoc 6(2). https://doi.org/10.1161/JAHA.116.004382
Agnello L, Bivona G, Sasso BL, Scazzone C, Bazan V, Bellia C et al (2017) Galectin-3 in acute coronary syndrome. Clin Biochem. https://doi.org/10.1016/j.clinbiochem.2017.04.018. [Epub ahead of print]
Aimo A, Vergaro G, Ripoli A, Bayes-Genis A, Pascual Figal DA, de Boer RA et al (2017) Meta-analysis of soluble suppression of tumorigenicity-2 and prognosis in acute heart failure. JACC Heart Fail 5(4):287–296
Amin A, Chitsazan M, Shiukhi Ahmad Abad F, Taghavi S, Naderi N (2017) On admission serum sodium and uric acid levels predict 30 day rehospitalization or death in patients with acute decompensated heart failure. ESC Heart Fail 4(2):162–168
Anguita M (2017) High-sensitivity troponins and prognosis of heart failure. Rev Clin Esp 217(2):95–96
Aspromonte N, Gulizia MM, Clerico A, Di Tano G, Emdin M, Feola M et al (2016) ANMCO/ELAS/SIBioC consensus document: recommendations for the use of cardiac biomarkers in heart failure patients. G Ital Cardiol (Rome) 17(9):615–656
Bayes-Genis A, Ordonez-Llanos J (2015) Multiple biomarker strategies for risk stratification in heart failure. Clin Chim Acta 443:120–125
Bayes-Genis A, de Antonio M, Vila J, Peñafiel J, Galán A, Barallat J et al (2014) Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 63(2):158–166
Berezin AE (2014) Serum uric acid as a metabolic regulator of endothelial reparative processes in heart failure patients. Stem Cell Transl Invest 1(1):1–5
Berezin AE (2015a) Biological markers of cardiovascular diseases. Part 4. Diagnostic and prognostic value of biological markers at risk stratification among patients with heart failure. LAMBERT Academic Publishing GmbH, Moscow. 329 p
Berezin AE (2015b) The risk stratification in heart failure patients: the controversial role of high-sensitive ST2. J Integr Cardiol 1(6):216–217
Berezin A (2015c) Endothelial derived micro particles: biomarkers for heart failure diagnosis and management. J Clin Trial Cardiol 2(3):1–3
Berezin AE (2015d) Impaired pattern of endothelial derived microparticles in heart failure patients. J Mol Genet Med 9:1. https://doi.org/10.4172/1747-0862.1000152
Berezin AE (2016a) Prognostication in different heart failure phenotypes: the role of circulating biomarkers. J Circ Biomark 5:01. https://doi.org/10.5772/62797
Berezin A (2016b) Biomarkers for cardiovascular risk in diabetic patients. Heart 102(24):1939–1941
Berezin AE (2016c) Impaired phenotype of endothelial cell-derived micro particles: the missed link in heart failure development? Biom J 2(2):14–19
Berezin A (2016d) Epigenetics in heart failure phenotypes. BBA Clinical 6:31–37
Berezin AE (2016e) Epigenetically modified endothelial progenitor cells in heart failure. J Clin Epigenet 2(2):21–23
Berezin AE (2016f) Genetic predictive scores in heart failure: possibilities and expectations. J Data Mining Genomics Proteomics 7(5):e127–e128
Berezin AE (2017a) Contemporary approaches of biological markers in heart failure. Scholars’ Press, Omni Scriptum Management GmbH, Saarbrücken
Berezin A (2017b) Does serum uric acid play a protective role against tissue damage in cardiovascular and metabolic diseases? Ann Clin Hypertens 1:39–41
Berezin A (2017c) Biomarkers in heart failure. J Blood Lymph 7(3):172–179
Berezin A (2017d) Up-to-date clinical approaches of biomarkers’ use in heart failure. Biomed Res Ther 4(6):1341–1370
Berezin AE, Kremzer AA (2013) Serum uric acid as a marker of coronary calcification in patients with asymptomatic coronary artery disease with preserved left ventricular pump function. Cardiol Res Pract, Article ID 129369. https://doi.org/10.1155/2013/129369
Berezin AE, Samura TA (2013) Prognostic value of biological markers in myocardial infarction patients. Asian Cardiovasc Thorac Ann 21(2):142–150
Berezin AE, Kremzer AA, Samura TA, Martovitskaya YV (2014a) Apoptotic microparticles to progenitor mononuclear cells ratio in heart failure: relevance of clinical status and outcomes. JCvD 2(2):50–57
Berezin AE, Kremzer AA, Martovitskaya YV, Samura TA, Berezina TA (2014b) Serum uric acid predicts declining of circulating proangiogenic mononuclear progenitor cells in chronic heart failure patients. J Cardiovasc Thorac Res 6(3):153–162. https://doi.org/10.5681/jcvtr.2014.0XX
Berezin AE, Kremzer AA, Martovitskaya YV, Samura TA, Berezina TA, Zulli A et al (2015a) The utility of biomarker risk prediction score in patients with chronic heart failure. Int J Clin Exp Med 8(10):18255–18264
Berezin AE, Kremzer AA, Berezina TA, Martovitskaya YV (2015b) Pattern of circulating microparticles in chronic heart failure patients with metabolic syndrome: relevance to neurohumoral and inflammatory activation. BBA Clinical 4:69–75
Berezin AE, Kremzer AA, Samura TA (2015c) Circulating thrombospondine-2 in patients with moderate-to-severe chronic heart failure due to coronary artery disease. J Biomed Res 30. https://doi.org/10.7555/JBR.29.20140025. [Epub ahead of print]
Berezin A, Kremzer A, Martovitskaya Y, Samura T, Berezina T (2016) The novel biomarker risk prediction score in patients with chronic heart failure. Clin Hypertens 22(3). https://doi.org/10.1186/s40885-016-0041-1.
Besler C, Lang D, Urban D, Rommel KP, von Roeder M, Fengler K et al (2017a) Plasma and cardiac Galectin-3 in patients with heart failure reflects both inflammation and fibrosis: implications for its use as a biomarker. Circ Heart Fail 10(3). https://doi.org/10.1161/CIRCHEARTFAILURE.116.003804
Besler C, Lang D, Urban D, Rommel KP, von Roeder M, Fengler K et al (2017b) Plasma and cardiac galectin-3 in patients with heart failure reflects both inflammation and fibrosis: implications for its use as a biomarker. Circ Heart Fail 10(3). https://doi.org/10.1161/CIRCHEARTFAILURE.116.003804
Billebeau G, Vodovar N, Sadoune M, Launay JM, Beauvais F, Cohen-Solal A (2017) Effects of a cardiac rehabilitation programme on plasma cardiac biomarkers in patients with chronic heart failure. Eur J Prev Cardiol. https://doi.org/10.1177/2047487317705488. [Epub ahead of print]
Biomarkers Definitions Working Group (National Institutes of Health) (2001) Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther 69:89–95
Bondar G, Cadeiras M, Wisniewski N, Maque J, Chittoor J, Chang E et al (2014) Comparison of whole blood and peripheral blood mononuclear cell gene expression for evaluation of the perioperative inflammatory response in patients with advanced heart failure. PLoS One 9(12):e115097
Borghi C, Rosei EA, Bardin T, Dawson J, Dominiczak A, Kielstein JT et al (2015) Serum uric acid and the risk of cardiovascular and renal disease. J Hypertens 33:1729–1741
Boulogne M, Sadoune M, Launay JM, Baudet M, Cohen-Solal A, Logeart D (2017a) Inflammation versus mechanical stretch biomarkers over time in acutely decompensated heart failure with reduced ejection fraction. Int J Cardiol 226:53–59
Boulogne M, Sadoune M, Launay JM, Baudet M, Cohen-Solal A, Logeart D (2017b) Inflammation versus mechanical stretch biomarkers over time in acutely decompensated heart failure with reduced ejection fraction. Int J Cardiol 226:53–59
Bustamante A, García-Berrocoso T, Penalba A, Giralt D, Simats A, Muchada M et al (2017) Sepsis biomarkers reprofiling to predict stroke-associated infections. J Neuroimmunol 312:19–23
Chan MM, Santhanakrishnan R, Chong JP, Chen Z, Tai BC, Liew OW et al (2016) Growth differentiation factor 15 in heart failure with preserved vs. reduced ejection fraction. Eur J Heart Fail 18(1):81–88
Chmurzynska A (2006) The multigene family of fatty acidbinding proteins (FABPs): function, structure, and polymorphism. J Appl Genet 47:39–48
Chow SL, Maisel AS, Anand I, Bozkurt B, de Boer RA, Felker GM, Fonarow GC et al (2017) Role of biomarkers for the prevention, assessment, and management of heart failure: a scientific statement from the American Heart Association. Circulation. https://doi.org/10.1161/CIR.0000000000000490. [Epub ahead of print]
Cohen-Solal A, Laribi S, Ishihara S, Vergaro G, Baudet M, Logeart D et al (2015) Prognostic markers of acute decompensated heart failure: the emerging roles of cardiac biomarkers and prognostic scores. Arch Cardiovasc Dis 108(1):64–74
Collier P, Watson CJ, Voon V, Phelan D, Jan A, Mak G et al (2011) Can emerging biomarkers of myocardial remodeling identify asymptomatic hypertensive patients at risk for diastolic dysfunction and diastolic heart failure? Eur J Heart Fail 13(10):1087–1095
Demissei BG, Cotter G, Prescott MF, Felker GM, Filippatos G, Greenberg BH et al (2017) A multimarker multi-time point-based risk stratification strategy in acute heart failure: results from the RELAX-AHF trial. Eur J Heart Fail. https://doi.org/10.1002/ejhf.749. [Epub ahead of print]
Dres M, Hausfater P, Foissac F, Bernard M, Joly LM, Sebbane M et al (2017) Mid-regional pro-adrenomedullin and copeptin to predict short-term prognosis of COPD exacerbations: a multicenter prospective blinded study. Int J Chron Obstruct Pulmon Dis 12:1047–1056
Favresse J, Gruson D (2017) Natriuretic peptides: degradation, circulating forms, dosages and new therapeutic approaches. Ann Biol Clin (Paris). https://doi.org/10.1684/abc.2017.1235. [Epub ahead of print]
Fazakas Á, Szelényi Z, Szénási G, Nyírő G, Szabó PM, Patócs A et al (2016) Genetic predisposition in patients with hypertension and normal ejection fraction to oxidative stress. J Am Soc Hypertens 10(2):124–132
Felker GM, Anstrom KJ, Adams KF, Ezekowitz JA, Fiuzat M, Houston-Miller N et al (2017) Effect of natriuretic peptide-guided therapy on hospitalization or cardiovascular mortality in high-risk patients with heart failure and reduced ejection fraction: a randomized clinical trial. JAMA 318(8):713–720
Feng SD, Jiang Y, Lin ZH, Lin PH, Lin SM, Liu QC (2017) Diagnostic value of brain natriuretic peptide and β-endorphin plasma concentration changes in patients with acute left heart failure and atrial fibrillation. Medicine (Baltimore) 96(34):e7526. https://doi.org/10.1097/MD.0000000000007526
Fonarow GC (2017) Biomarker-guided vs guideline-directed titration of medical therapy for heart failure. JAMA 318(8):707–708
Friedrich FW, Dilanian G, Khattar P, Juhr D, Gueneau L, Charron P et al (2013) A novel genetic variant in the transcription factor Islet-1 exerts gain of function on myocyte enhancer factor 2C promoter activity. Eur J Heart Fail 15(3):267–276
Ganna A, Rivadeneira F, Hofman A, Uitterlinden AG, Magnusson PK, Pedersen NL et al (2013) Genetic determinants of mortality. Can findings from genome-wide association studies explain variation in human mortality? Hum Genet 132(5):553–561
Grassi D, Ferri L, Desideri G, Di Giosia P, Cheli P, Del Pinto R et al (2013) Chronic hyperuricemia, uric acid deposit and cardiovascular risk. Curr Pharm Des 19:2432–2438
Hage C, Michaëlsson E, Linde C, Donal E, Daubert JC, Gan LM et al (2017) Inflammatory biomarkers predict heart failure severity and prognosis in patients with heart failure with preserved ejection fraction: a holistic proteomic approach. Circ Cardiovasc Genet 10(1). https://doi.org/10.1161/CIRCGENETICS.116.001633
Hayashida K, Kondo Y, Hara Y, Aihara M, Yamakawa K (2017) Head-to-head comparison of procalcitonin and presepsin for the diagnosis of sepsis in critically ill adult patients: a protocol for a systematic review and meta-analysis. BMJ Open 7(3):e014305
Herrero-Puente P, Prieto-García B, García-García M, Jacob J, Martín-Sánchez FJ, Pascual-Figal D et al (2017) Predictive capacity of a multimarker strategy to determine short-term mortality in patients attending a hospital emergency department for acute heart failure. BIO-EAHFE study. Clin Chim Acta 466:22–30
Hershberger RE, Siegfried JD (2011) Update 2011: clinical and genetic issues in familial dilated cardiomyopathy. J Am Coll Cardiol 57(16):1641–1649
Hofman N, van Langen I, Wilde AAM (2010) Genetic testing in cardiovascular diseases. Curr Opin Cardiol 25(3):243–248
Huerta A, López B, Ravassa S, San José G, Querejeta R, Beloqui Ó et al (2016) Association of cystatin C with heart failure with preserved ejection fraction in elderly hypertensive patients: potential role of altered collagen metabolism. J Hypertens 34(1):130–138
Hutchinson KR, Stewart JA Jr, Lucchesi PA (2010) Extracellular matrix remodeling during the progression of volume overload-induced heart failure. J Mol Cell Cardiol 48(3):564–569
Imran TF, Shin HJ, Mathenge N, Wang F, Kim B, Joseph J et al (2017) Meta-analysis of the usefulness of plasma Galectin-3 to predict the risk of mortality in patients with heart failure and in the general population. Am J Cardiol 119(1):57–64
Jin P, Gu W, Lai Y, Zheng W, Zhou Q, Wu X (2017) The circulating MicroRNA-206 level predicts the severity of pulmonary hypertension in patients with left heart diseases. Cell Physiol Biochem 41(6):2150–2160
Kempf T, Wollert KC (2009) Growth differentiation Factor-15: a new biomarker in cardiovascular disease. Herz 34:594–599
Kim H, Yoon HJ, Park HS, Cho YK, Nam CW, Hur SH et al (2013) Potentials of cystatin C and uric acid for predicting prognosis of heart failure. Congest Heart Fail 19(3):123–129
Kim TH, Kim H, Kim IC (2015) The potential of cystatin-C to evaluate the prognosis of acute heart failure: a comparative study. Acute Card Care 17(4):72–76
Kitai T, Kim YH, Kiefer K, Morales R, Borowski AG, Grodin JL et al (2017) Circulating intestinal fatty acid-binding protein (I-FABP) levels in acute decompensated heart failure. Clin Biochem. https://doi.org/10.1016/j.clinbiochem.2017.02.014. [Epub ahead of print]
Kolder IC, Michels M, Christiaans I, Ten Cate FJ, Majoor-Krakauer D, Danser AH et al (2012) The role of renin-angiotensin-aldosterone system polymorphisms in phenotypic expression of MYBPC3-related hypertrophic cardiomyopathy. Eur J Hum Genet 20(10):1071–1077
Krane V, Genser B, Kleber ME, Drechsler C, März W, Delgado G et al (2017) Copeptin associates with cause-specific mortality in patients with impaired renal function: results from the LURIC and the 4D study. Clin Chem. https://doi.org/10.1373/clinchem.2016.266254. [Epub ahead of print]
Krintus M, Kozinski M, Fabiszak T, Kubica J, Panteghini M, Sypniewska G (2017) Establishing reference intervals for galectin-3 concentrations in serum requires careful consideration of its biological determinants. Clin Biochem. https://doi.org/10.1016/j.clinbiochem.2017.03.015. [Epub ahead of print]
Lala RI, Lungeanu D, Darabantiu D, Pilat L, Puschita M (2017) Galectin-3 as a marker for clinical prognosis and cardiac remodeling in acute heart failure. Herz. https://doi.org/10.1007/s00059-017-4538-5. [Epub ahead of print]
Ledwidge M, Gallagher J, Conlon C, Tallon E, O’Connell E, Dawkins I et al (2013) Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 310:66–74
Löfsjögård J, Persson H, Díez J, López B, González A, Edner M et al (2014) Atrial fibrillation and biomarkers of myocardial fibrosis in heart failure. Scand Cardiovasc J 48(5):299–303
Löfsjögård J, Kahan T, Díez J, López B, González A, Ravassa S et al (2017) Usefulness of collagen Carboxy-terminal propeptide and telopeptide to predict disturbances of long-term mortality in patients ≥60 years with heart failure and reduced ejection fraction. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2017.03.036. [Epub ahead of print]
Lopes LR, Elliott PM (2013) Genetics of heart failure. BBA Mol Basis Dis 1832(12):2451–2461
Lopes D, Menezes Falcão L (2017) Mid-regional pro-adrenomedullin and ST2 in heart failure: contributions to diagnosis and prognosis. Rev Port Cardiol 36(6):465–472
Luchner A, von Haehling S, Holubarsch C, Keller T, Knebel F, Zugck C et al (2017) Indications and clinical implications of the use of the cardiac markers BNP and NT-proBNP. Dtsch Med Wochenschr 142(5):346–355
Maisel AS, Di Somma S (2016) Do we need another heart failure biomarker: focus on soluble suppression of tumorigenicity 2 (sST2). Eur Heart J. https://doi.org/10.1093/eurheartj/ehw462. [Epub ahead of print]
Malek V, Gaikwad AB (2017) Neprilysin inhibitors: a new hope to halt the diabetic cardiovascular and renal complications? Biomed Pharmacother 90:752–759
Masson S, Latini R, Anand IS (2010) An update on cardiac troponins as circulating biomarkers in heart failure. Curr Heart Fail Rep 7(1):15–21
McNamara DM, Taylor AL, Tam SW, Worcel M, Yancy CW, Hanley-Yanez K et al (2014) G-protein beta-3 subunit genotype predicts enhanced benefit of fixed-dose isosorbide dinitrate and hydralazine: results of A-HeFT. JACC Heart Fail 2(6):551–557
Meijers WC, van der Velde AR, Muller Kobold AC, Dijck-Brouwer J, AH W, Jaffe A et al (2017) Variability of biomarkers in patients with chronic heart failure and healthy controls. Eur J Heart Fail 19(3):357–365
Miró Ò, González de la Presa B, Herrero-Puente P, Fernández Bonifacio R, Möckel M, Mueller C et al (2017) The GALA study: relationship between galectin-3 serum levels and short- and long-term outcomes of patients with acute heart failure. Biomarkers 2:1–9. https://doi.org/10.1080/1354750X.2017.1319421.
Moayedi Y, Ross HJ (2017) Advances in heart failure: a review of biomarkers, emerging pharmacological therapies, durable mechanical support and telemonitoring. Clin Sci (Lond) 131(7):553–566
Morgenthaler NG (2006) Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem 52:112–119
Mozos I, Marginean O (2015) Links between vitamin D deficiency and cardiovascular diseases. Biomed Res Int 2015:109275. https://doi.org/10.1155/2015/109275
Mozos I, Stoian D, Luca CT (2017) Crosstalk between vitamin A, B12, D, K, C and E status and arterial stiffness. Dis Markers 2017:8784971. https://doi.org/10.1155/2017/8784971
Nagarajan V, Hernandez AV, Tang WH (2012) Prognostic value of cardiac troponin in chronic stable heart failure: a systematic review. Heart 98(24):1778–1786
Nakanishi M, Nakao K, Kumasaka L, Arakawa T, Fukui S, Ohara T et al (2017) Improvement in exercise capacity by exercise training associated with favorable clinical outcomes in advanced heart failure with high B-type natriuretic peptide level. Circ J. https://doi.org/10.1253/circj.CJ-16-1268. [Epub ahead of print]
Nelveg-Kristensen KE, Busk Madsen M, Torp-Pedersen C, Køber L, Egfjord M, Berg Rasmussen H et al (2015) Pharmacogenetic risk stratification in angiotensin-converting enzyme inhibitor-treated patients with congestive heart failure: a retrospective cohort study. PLoS One 10(12):e0144195
Nymo SH, Aukrust P, Kjekshus J, McMurray JJ, Cleland JG, Wikstrand J et al (2017) CORONA study group. Limited added value of circulating inflammatory biomarkers in chronic heart failure. JACC Heart Fail 5(4):256–264. https://doi.org/10.1016/j.jchf.2017.01.008.
Odermatt J, Meili M, Hersberger L, Bolliger R, Christ-Crain M, Briel M et al (2017) Pro-Adrenomedullin predicts 10-year all-cause mortality in community-dwelling patients: a prospective cohort study. BMC Cardiovasc Disord 17(1):178
Okazaki H, Shirakabe A, Kobayashi N, Hata N, Shinada T, Matsushita M et al (2016) The prognostic impact of uric acid in patients with severely decompensated acute heart failure. J Cardiol 68(5):384–391
Okazaki H, Shirakabe A, Kobayashi N, Hata N, Shinada T, Matsushita M et al (2017) Are atherosclerotic risk factors associated with a poor prognosis in patients with hyperuricemic acute heart failure? The evaluation of the causal dependence of acute heart failure and hyperuricemia. Heart Vessel 32(4):436–445
Otaki Y, Watanabe T, Kinoshita D, Yokoyama M, Takahashi T, Toshima T et al (2017) Association of plasma xanthine oxidoreductase activity with severity and clinical outcome in patients with chronic heart failure. Int J Cardiol 228:151–157
Poller W, Dimmeler S, Heymans S, Zeller T, Haas J, Karakas M et al (2017) Non-coding RNAs in cardiovascular diseases: diagnostic and therapeutic perspectives. Eur Heart J. https://doi.org/10.1093/eurheartj/ehx165. [Epub ahead of print]
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Authors/Task Force Members et al (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200
Pouleur AC (2015) Which biomarkers do clinicians need for diagnosis and management of heart failure with reduced ejection fraction? Clin Chim Acta 443:9–16
Qian HY, Huang J, Yang YJ, Yang YM, Li ZZ, Zhang JM (2016) Heart-type fatty acid binding protein in the assessment of acute pulmonary embolism. Am J Med Sci 352(6):557–562
Reiner MM, Khoury WE, Canales MB, Chmielewski RA, Patel K, Razzante MC et al (2017) Procalcitonin as a biomarker for predicting amputation level in lower extremity infections. J Foot Ankle Surg. https://doi.org/10.1053/j.jfas.2017.01.014. [Epub ahead of print]
Remde H, Dietz A, Emeny R, Riester A, Peters A, de Las Heras Gala T et al (2016) The cardiovascular markers copeptin and high-sensitive C-reactive protein decrease following specific therapy for primary aldosteronism. J Hypertens 34:2066–2073
Ryu JA, Yang JH, Lee D, Park CM, Suh GY, Jeon K et al (2015) Clinical usefulness of procalcitonin and C-reactive protein as outcome predictors in critically ill patients with severe sepsis and septic shock. PLoS One 10(9):e0138150
Sahin I, Gungor B, Ozkaynak B, Uzun F, Küçük SH, Avci II et al (2017) Higher copeptin levels are associated with worse outcome in patients with hypertrophic cardiomyopathy. Clin Cardiol 40(1):32–37
Savic-Radojevic A, Pljesa-Ercegovac M, Matic M, Simic D, Radovanovic S, Simic T (2017) Novel biomarkers of heart failure. Adv Clin Chem 79:93–152
Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J (2004) Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis 39:206–217
Skaf S, Thibault B, Khairy P, O’Meara E, Fortier A, Vakulenko HV, EARTH Investigators et al (2017) Impact of left ventricular vs biventricular pacing on reverse remodelling: insights from the evaluation of resynchronization therapy for heart failure (EARTH) trial. Can J Cardiol 33(10):1274–1282
Smaradottir MI, Ritsinger V, Gyberg V, Norhammar A, Näsman P, Mellbin LG (2017) Copeptin in patients with acute myocardial infarction and newly detected glucose abnormalities – a marker of increased stress susceptibility? A report from the glucose in acute myocardial infarction cohort. Diab Vasc Dis Res 14(2):69–76
Souza BSF, Silva DN, Carvalho RH, Sampaio GLA, Paredes BD, Aragão França L et al (2017) Association of cardiac galectin-3 expression, myocarditis, and fibrosis in chronic chagas disease cardiomyopathy. Am J Pathol 187(5):1134–1146
Srivatsan V, George M, Shanmugam E (2015) Utility of galectin-3 as a prognostic biomarker in heart failure: where do we stand? Eur J Prev Cardiol 22(9):1096–1110
Sutter ME, Gaedigk A, Albertson TE, Southard J, Owen KP, Mills LD et al (2013) Polymorphisms in CYP2D6 may predict methamphetamine related heart failure. Clin Toxicol (Phila) 51(7):540–544
Taub PR, Borden KC, Fard A, Maisel A (2012) Role of biomarkers in the diagnosis and prognosis of acute kidney injury in patients with cardiorenal syndrome. Expert Rev Cardiovasc Ther 10(5):657–667
Teekakirikul P, Kelly MA, Rehm HL, Lakdawala NK, Funke BH (2013) Inherited cardiomyopathies: molecular genetics and clinical genetic testing in the postgenomic era. J Mol Diagn 15(2):158–170
Teo LY, Moran RT, Tang WH (2015) Evolving approaches to genetic evaluation of specific cardiomyopathies. Curr Heart Fail Rep 12(6):339–349
Tziakas DN, Chalikias GK, Stakos D, Chatzikyriakou SV, Papazoglou D, Mitrousi K et al (2012) Independent and additive prognostic ability of serum carboxy-terminal telopeptide of collagen type-I in heart failure patients: a multi-marker approach with high-negative predictive value to rule out long-term adverse events. Eur J Prev Cardiol 19(1):62–71
Vegter EL, van der Meer P, Voors AA (2017) Associations between volume status and circulating microRNAs in acute heart failure. Eur J Heart Fail. https://doi.org/10.1002/ejhf.867. [Epub ahead of print]
Welsh P, Kou L, Yu C, Anand I, van Veldhuisen DJ, Maggioni AP et al (2017) Prognostic importance of emerging cardiac, inflammatory, and renal biomarkers in chronic heart failure patients with reduced ejection fraction and anaemia: RED-HF study. Eur J Heart Fail. https://doi.org/10.1002/ejhf.988. [Epub ahead of print]
Wettersten N, Maisel AS (2016) Biomarkers for heart failure: an update for practitioners of internal medicine. Am J Med 129(6):560–567
Wojciechowska C, Romuk E, Nowalany-Kozielska E, Jacheć W (2017) Serum Galectin-3 and ST2 as predictors of unfavorable outcome in stable dilated cardiomyopathy patients. Hell J Cardiol. https://doi.org/10.1016/j.hjc.2017.03.006. [Epub ahead of print]
Wong CM, Hawkins NM, Petrie MC, Jhund PS, Gardner RS, Ariti CA, MAGGIC Investigators et al (2014) Heart failure in younger patients: the meta-analysis global Group in Chronic Heart Failure (MAGGIC). Eur Heart J 35(39):2714–2721
Wong PC, Guo J, Zhang A (2017) The renal and cardiovascular effects of natriuretic peptides. Absence of clear clinical recommendations of biomarker-based HF therapy is the main cause of uncertainty regarding practical use of this approach. Adv Physiol Educ 41(2):179–185. https://doi.org/10.1152/advan.00177.2016
Wu CK, Luo JL, XM W, Tsai CT, Lin JW, Hwang JJ et al (2009) A propensity score-based case-control study of renin-angiotensin system gene polymorphisms and diastolic heart failure. Atherosclerosis 205(2):497–502
Wu CK, Luo JL, Tsai CT, Huang YT, Cheng CL, Lee JK et al (2010) Demonstrating the pharmacogenetic effects of angiotensin-converting enzyme inhibitors on long-term prognosis of diastolic heart failure. Pharmacogenomics J 10(1):46–53
Yan JJ, Lu Y, Kuai ZP, Yong YH (2017a) Predictive value of plasma copeptin level for the risk and mortality of heart failure: a meta-analysis. J Cell Mol Med. https://doi.org/10.1111/jcmm.13102. [Epub ahead of print]
Yan H, Ma F, Zhang Y, Wang C, Qiu D, Zhou K et al (2017b) miRNAs as biomarkers for diagnosis of heart failure: a systematic review and meta-analysis. Medicine (Baltimore) 96(22):e6825. https://doi.org/10.1097/MD.0000000000006825
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM et al (2017) ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Failure Society of America. J Card Fail. https://doi.org/10.1016/j.cardfail.2017.04.014. [Epub ahead of print]
Yang J, Xu WW, Hu SJ (2015) Heart failure: advanced development in genetics and epigenetics. Biomed Res Int 2015:352734
Yip VL, Pirmohamed M (2013) Expanding role of pharmacogenomics in the management of cardiovascular disorders. Am J Cardiovasc Drugs 13(3):151–162
Yu B, Zheng Y, Alexander D, Manolio TA, Alonso A, Nettleton JA et al (2013) Genome-wide association study of a heart failure related metabolomic profile among African Americans in the Atherosclerosis Risk in Communities (ARIC) study. Genet Epidemiol 37(8):840–845
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
Not declared.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Berezin, A.E. (2018). Circulating Biomarkers in Heart Failure. In: Islam, M. (eds) Heart Failure: From Research to Clinical Practice. Advances in Experimental Medicine and Biology(), vol 1067. Springer, Cham. https://doi.org/10.1007/5584_2017_140
Download citation
DOI: https://doi.org/10.1007/5584_2017_140
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-78279-9
Online ISBN: 978-3-319-78280-5
eBook Packages: MedicineMedicine (R0)