Abstract
In recent years, many nanotechnology platforms in the area of medical biology, including cancer therapy, have attracted remarkable attention. In particular, research in targeted, polymeric nanoparticles for cancer therapy has increased dramatically in the past 5–10 years. However, the potential success of nanoparticles in the clinic relies on consideration of important parameters such as nanoparticle fabrication strategies, their physical properties, drug loading efficiencies, drug release potential, and, most importantly, minimum toxicity of the carrier itself. Recent work has suggested that chitosan materials hold much promise in advancing nanoparticle-based therapeutics. The field of oncology could soon be revolutionized by novel strategies for therapy employing chitosan-based nanotherapeutics. Several aspects of cancer therapy would be involved. Chitosans can also be applied to a variety of cancer therapies to improve their safety and efficacy. Further applications of chitosans in cancer therapy are being examined. This review focuses on providing brief updates on chitosan nanoparticles for cancer therapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Recently, interdisciplinary research in cancer diagnosis and therapy has evolved to the point where nanoscale particles can be monitored in real-time and noninvasively at a molecular level in live animals by using imaging modalities, such as optical imaging, magnetic resonance imaging, and nuclear imaging [1]. Nanoparticle size allows for interactions with biomolecules on the cell surfaces and within the cells in ways that do not necessarily alter the behavior and biochemical properties of those molecules [2]. With the advances in polymer science, the field of polymeric nanoparticles has been expanding and has attracted significant interest in recent years, with most focus on biodegradable nanoparticles for drug delivery. In addition, noninvasive live animal imaging technology is providing new research opportunities in the preclinical and clinical development of nanosized drug carriers in cancer therapy [3]. Biodegradable nanoparticles are frequently used to improve the therapeutic value of various water-soluble and insoluble medicinal drugs and bioactive molecules by improving bioavailability, solubility, and retention time [4]. These nanoparticle–drug formulations reduce the patient expenses and risks of toxicity [5]. Nanoencapsulation of medicinal drugs (nanomedicines) increases drug efficacy, specificity, tolerability, and therapeutic index of corresponding drugs [6–11]. Several disease-related drugs and bioactive molecules have been successfully encapsulated to improve bioavailability, bioactivity, and controlled delivery [12–14]. Nanomedicines are being developed for dreadful diseases like cancer [15], AIDS [16], diabetes [17], malaria [18], prion disease [19] and tuberculosis [20].
2 Chitosan-Based Nanotechnology
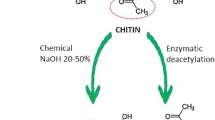
Polysaccharides, lipids, surfactants, and dendrimers have received increasing attention because of their outstanding physical and biological properties [21]. Natural cationic polysaccharides from crab and shrimp have drawn increasing attention for pharmaceutical and biomedical applications, due to their abundant availability, unique mucoadhesivity, inherent pharmacological properties, and other beneficial biological properties such as biocompatibility, biodegradability, nontoxicity, and low-immunogenicity [22, 23]. Chitosan (deacetylated chitin) is a nontoxic biodegradable, cationic polysaccharide with randomly distributed b(1,4)-linked N-actyl-d-glucosamines and d-glucosamines. Chitosan was introduced as a potential gene carrier in 1995 and various nanosystems based on chitosans and chitosan derivatives have been investigated, including unmodified chitosans with different molecular weights and degrees of deacetylation, quaternized chitosans, bile acid-modified chitosan, PEGylated chitosan, and chitosans bearing specific ligands [24]. Chitosan-based nanodelivery systems have been extensively studied for organ-specific applications (e.g., for colon, kidney, lung, and liver) [25].
3 Chitosan Nanoparticles in Cancer Therapy
There are a variety of nanoparticle systems currently being explored for cancer therapeutics [26]. The types of nanoparticles currently used in research for cancer therapeutic applications include dendrimers [27], liposomes [28], polymeric nanoparticles [29], micelles [30], protein nanoparticles [31], ceramic nanoparticles [32], viral nanoparticles [33], metallic nanoparticles [34], and carbon nanotubes [35]. These nanoparticles have been investigated in order to minimize the side effects of anticancer drugs and enhance the antitumoral drug efficacy in cancer therapy since they have shown a high tumor targeting ability, leading to high antitumoral therapeutic efficacies [36–43].
To elevate the local concentrations of anticancer drugs at tumor sites, various drug delivery systems involving intratumoral administration of anticancer drugs have been investigated [44–46]. For example, glycol chitosan (GC) nanoparticles that had been modified with hydrophobic bile acid analogs were shown to self-assemble into polymeric nanoparticles with hydrophilic shells of GC and hydrophobic cores of bile acid derivatives [47–54]. These self-assembling hydrophobically modified GC–5β cholanic acid conjugates were shown to encapsulate water-insoluble anticancer drugs and to have enhanced tumor-targeting properties in tumor-bearing mice [53, 55–57]. It was concluded that these amphiphilic chitosan-based nanoparticles (CNPs) can efficiently take up various hydrophobic anticancer drugs into their hydrophobic inner cores, which are covered with biocompatible and biodegradable GC shells. Compared to a free drug formulation, the biodegradable and biocompatible anticancer drug-encapsulating CNPs showed prolonged blood circulation time in vivo, enhanced tumor specificity, and improved therapeutic efficacy [58, 59].
Recent years have witnessed the development of new nanoscale drug carriers such as CNPs that can be used for photodynamic therapy [60]. In the context of nanomedicine-based therapeutics, effective cancer therapy requires drug delivery to cancer tissues, meaning that a drug delivery system should hold the anticancer drug in the blood and then allow a burst or continuous drug release at the cancer site.
3.1 Breast Cancer
It was estimated by the American Cancer Society that 15% of cancer-related deaths in women were due to breast cancer, making breast cancer the most common type of cancer among women. This mortality rate is due, in part, to the high rate of tumor metastasis to bone and lymph nodes that develops during the progression of the disease in patients. Thus, early diagnosis is crucial to improve the survival rates of breast cancer patients. To this end, there has been much research on the design of nanosized and tumor-targeting polymeric drug carriers, focusing on improving drug solubility, prolonging drug circulation time, and reducing drug toxicity. A number of studies have developed hydrophobically modified glycol chitosan (HGC) nanoparticles composed of a hydrophilic shell of GC and hydrophobic multicores of bile acid analogs [47, 48, 50, 51, 61–64]. It has been reported that anticancer drug-encapsulated HGC nanoparticles present a promising therapeutic drug delivery system for cancer therapy [63, 64]. HGC nanoparticles protect the active camptothecin (CPT) lactone drug from hydrolysis and target solid tumors with high specificity. Hence, HGC nanoparticles preferentially localized in tumor tissues can supply active CPT molecules for extended times through a sustained release (the so-called metronomic effect) pattern, thereby exerting an antitumor effect in the MDA-MB231 human breast cancer xenograft model [65]. Because of their hydrophobic inner cores, HGC nanoparticles can efficiently imbibe various hydrophobic anticancer drugs, and show a sustained drug release profile. Also, near infrared fluorescence-labeled HGC nanoparticles were shown by noninvasive and in real-time imaging system in tumor-bearing mice to have reasonably prolonged blood circulation time and tumor targeting ability, compared to control nanoparticles [65]. Examination of a nanosized drug delivery system for encapsulating CPT into prolonged circulating and tumor-homing HGC nanoparticles were addressed [66]. The in vivo tissue distribution, tumor targeting ability, and time-dependent excretion profile were also confirmed by noninvasive and live animal imaging systems, suggesting the anticancer efficacy of CPT-HGC nanoparticles in a human breast cancer xenograft model, compared to free CPT-treated mice [66].
Targeted delivery of small interfering (siRNA) against HER2 to HER2-overexpressing SKBR3 breast cancer cells was shown to be specific, with chitosan/quantum dot (QD) nanoparticles labeled on their surface with HER2 antibody targeting the HER2 receptors on SKBR3 breast cancer cells [67]. These experiments demonstrated that the chitosan/QD nanoparticles labeled with suitable surface ligands can be specifically targeted to cells with a high degree of precision. In vitro confocal microscopy and flow cytometry studies using MCF-7 and SKBR3 cells also showed that chitosan/QD nanoparticles may be readily internalized into cells [67]. A recent insight into overexpression of RhoA in cancer suggests that this indicates a poor prognosis, because of increased tumor cell proliferation and invasion and tumor angiogenesis. Researchers reported that anti-RhoA siRNA inhibited aggressive breast cancer more effectively than conventional blockers of Rho-mediated signaling pathways [68]. The study reports the efficacy and lack of toxicity of intravenously administered anti-RhoA siRNA encapsulated in chitosan-coated poly(isohexylcyanoacrylate) (PIHCA) nanoparticles in xenografted aggressive breast cancers (MDA-MB-231) [68]. A recent study reported that a system incorporating methotrexate (MTX) covalently conjugated to chitosan nanoparticles has potential as a delivery system for MTX [69]. By conjugating MTX to chitosan using glutaraldehyde as crosslinking agent, in vitro release tests showed that the stable covalent bonding of chitosan and MTX was beneficial for providing slow release of MTX. In vitro studies using MCF-7 cancer cells further demonstrated the effective anticancer efficacy of this new type of delivery for MTX [69].
As an alternative approach, investigators tried the use of an in situ implant incorporating superparamagnetic iron oxide nanoparticles (SPIONs) as a form of minimally invasive treatment of cancer lesions by magnetically induced local hyperthermia [70]. Studies showed that injectable formulations that form gels are capable of entrapping magnetic particles when injected into a tumor [70]. Using SPIONs embedded in silica microparticles to favor injectability, a chitosan gel incorporated the highest proportion possible to allow large heating capacities. The hydrogel (a single-solvent organogel and low-toxicity hydrophilic cosolvent organogel) formulation was injected into human cancer tumors xenografted in mice. Unfortunately, the thermoreversible hydrogels (poloxamer, chitosan), which accommodated 20% w/v of the magnetic microparticles, proved to be inadequate at reducing tumors [70].
Using “click chemistry,” the selective introduction of a trimethylammonium cationic group into the C-6 position of chitosan was successfully performed for the first time and the 6-N,N,N-trimethyltriazole–chitosans (TCs) showed good solubility in water. The introduction of a trimethyltriazole group led to significantly increased cellular uptake compared with unmodified chitosan, which resulted in higher transfection efficiency in HEK 293 and MDA-MB-468 cells [71]. Further studies also showed that chitosan colloidal carriers, which consist of an oily core and a chitosan coating, facilitated a controlled intracellular delivery of docetaxel (DTX) [72]. Fluorescence was observed in more than 80% of MCF7 (human breast adenocarcinoma) cells after only 2 h of treatment with fluorescent chitosan carriers. As a result, the DTX-loaded chitosan carriers had an effect on cell proliferation that was significantly greater than that of free DTX. These results suggest that DTX remains fully active upon its encapsulation into the colloidal carriers and that these systems actively transport DTX into cancer cells and, thus, result in a significant increase in its antiproliferative effect [72].
To achieve a therapeutic effect at lower doses of paclitaxel (PTX), to minimizing the adverse side effects, chitosan/glyceryl monooleate (GMO) nanoparticles loaded with PTX were characterized and their safety and efficacy evaluated by MTT cytotoxicity assay in human breast cancer cells (MDA-MB-231) [73]. This nanoparticle formulation showed evidence of mucoadhesive properties, a fourfold increased cellular uptake, and a 1,000-fold reduction in the half-inhibitory concentration (IC50) of PTX [73].
Two polymers, chitosan and poly(lactide-co-glycolide) (PLGA) copolymer, were developed in the form of nanoparticles for delivery of protein drug substances into tumor cells [74]. Cystatin was selected as a model protein drug due to its high potential to inhibit cysteine proteases, known to trigger the invasive process. As a result, the cellular uptake of the nanoparticles was tested on a transformed human breast epithelial cell line, MCF-10A neoT, a cell line characterized by an increased expression of cysteine proteases and a highly invasive cell phenotype. The results suggested that cystatin delivery by nanoparticles effectively inhibits intracellular proteolytic activity of cathepsin B [74]. Another strategy to develop biodegradable nanoparticles suitable for cellular delivery of chemotherapeutic drugs has been to modify the surface of PLGA nanoparticles with chitosan [75]. Chitosan-modified PLGA nanoparticles showed significant uptake by neoplastic 4 T1 cells, and were distributed to several major organs that are frequently seen as sites of cancer metastasis in mice [75]. Poly(methyl methacrylate) nanoparticles coated with chitosan–glutathione conjugate were studied for anticancer drugs encapsulation [76]. Nanoparticles were synthesized through radical polymerization of methyl methacrylate initiated by cerium (IV) ammonium nitrate and then PTX, a model anticancer drug, was encapsulated in the nanoparticles with a maximal encapsulation efficiency of 98.27%. The PTX-loaded nanoparticles showed cytotoxicity for NIH 3 T3 and T47D breast carcinoma cells [76].
3.2 Prostate Cancer
According to the American Cancer Society, prostate cancer is the most common cancer in men, and the second most deadly. As a result of slow tumor growth, the disease is usually not detected early, which results in spreading of the disease via metastasis in 30–50% of patients diagnosed with prostate cancer. Thus, improved techniques are urgently needed for detection of the disease in its early stages in order to improve the survival rates of patients. Downregulation of Relaxin (RLN) family peptide receptor 1 (RXFP1) expression using siRNA reduces cancer growth and metastasis in a xenograft model of prostate cancer. One group has shown that intratumoral injections of siRNAs loaded on biodegradable chitosan nanoparticles led to a downregulation of RXFP1 receptor expression and a dramatic reduction in tumor growth [77]. In the xenograft models treated with siRNA against RXFP1, the smaller tumor size was associated with decreased cell proliferation and increased apoptosis suggesting that the suppression of RLN/RXFP1 might have potential therapeutic benefits in prostate cancer [77]. Magnetofluorescent polymeric nanoparticles for prostate cancer imaging in vivo have been extensively studied using GC chemically modified with N-acetyl histidine (NAHis) as a hydrophobic moiety. Bombesin (BBN) was conjugated to the hydrophobically modified GC for use in targeting gastric-releasing peptide receptors (GRPR) overexpressed in prostate cancer cells [78]. BBN-conjugated chitosan-NAHis-GC nanoparticles (BC-NAHis-GC nanoparticles) showed significantly higher binding to the PC3 cell surface than nanoparticles without BBN, and the cellular binding was clearly inhibited by BBN [78]. Further, iron oxide nanoparticles (IO) were loaded into BC-NAHis-GC nanoparticles to investigate the possibility of their use as a probe for Magentic resonance imaging (MRI). IO-BC-NAHis-GC nanoparticles were well observed in the PC3 cells, and the blocking with BBN significantly reduced the cellular binding of the nanoparticles. Altogether the results show that BBN conjugation to NAHis-GC nanoparticles improves their tumor accumulation in PC3-bearing mice in comparison to nanoparticles without BBN, suggesting that BC-NAHis-GC nanoparticles may be useful for prostate cancer imaging [78]. Springate et al. reported an injectable, intratumoral, controlled release delivery system for clusterin antisense oligonucleotide (clusterin ASO) [79]. They showed that when clusterin ASO complexed with chitosan microparticles (CC complexes) and then blended with a biodegradable polymeric paste (CC in paste), there was a 52–62% inhibition of the expression of clusterin protein in PC-3 cells in vitro as compared to clusterin ASO alone [79]. The authors concluded that the amount of clusterin ASO loaded into microparticulate chitosan was dependent on the amount of chitosan present and the pH of the environment, and that clusterin ASO was released from the various formulations in a controlled manner and in a bioactive form [79]. Other researchers studied an injectable, controlled release delivery system for a phosphorothioate ASO for intratumoral treatment of solid tumors that was based on complexed ASO–chitosan dispersed in a biodegradable polymeric paste [80]. Results were similar to those for the clusterin ASO complexed with a chitosan particle system. When injected intratumorally with or without PTX or DTX, the tumor volumes and serum prostate specific antigen (PSA) levels in tumor-bearing mice decreased over the 4 week period. Complexation of clusterin ASO with chitosan and incorporation into polymeric paste with PTX or DTX produced in vitro controlled release of the ASO [80].
Studies using a 166Ho–chitosan complex (DW-166HC) in rats showed its absorption, distribution, and excretion after administration into the prostate [81]. DW-166HC administered into the prostate of male rats resulted in three- to fourfold higher levels of radioactivity in the main tissues, including liver, spleen, kidney cortex, and bone, 24 h after administration as compared to controls administered 166Ho nitrate alone. It was concluded that the chitosan complex may be used to retain 166Ho within a limited area in cancer of the prostate [81]. Studies on the treatment of metastatic prostate tumors using GC as immunoadjuvant and indocyanine green (ICG) showed that this treatment significantly reduced the growth of primary tumors and lung metastases. Long-term survival of the rats bearing the prostate tumors was observed after the laser immunotherapy treatment [82].
3.3 Lung Cancer
Lung cancer is the leading cause of cancer death among both men and women, with 5-year survival rates of only 50–80% after pathologically complete resection of stage I or II disease, in particular. Nanotechnology is an exciting and rapidly progressing field that offers potential solutions to multiple challenges in the diagnosis and treatment of lung cancer, with the potential for improving imaging and mapping techniques, drug delivery, and ablative therapy. In studies performed to overcome drug delivery limitations inhibiting the optimization of deep lung therapy, isolated rat Sertoli cells were preloaded with chitosan nanoparticles to obtain a high density distribution and concentration (92%) of the nanoparticles in the lungs of mice [83]. In a similar study, Sertoli cells loaded with chitosan nanoparticles coupled with the anti-inflammatory compound curcumin, were injected intravenously into control or experimental mice with deep lung inflammation [83]. Mice model studies showed the therapeutic effect achieved 24 h following curcumin treatment delivered by this Sertoli cell nanoparticle protocol (SNAP), suggesting an efficient protocol for targeted delivery of drugs to the deep lung mediated by extra-testicular Sertoli cells [83].
Zhang et al. devised a process for forming self-assembled oleoyl-chitosan (OCH) nanoparticles based on chitosan with different molecular weights (5, 38, and 300 kDa) [84]. They loaded their OCH nanoparticles with doxorubicin hydrochloride (DOX) and showed that the drug had a sustained release in phosphate-buffered saline (PBS), and that loading efficiency and the DOX release rate increased as the molecular weight of chitosan decreased [84]. Zhang et al. proposed the utilization of DOX-loaded OCH nanoparticles for treatment of human lung cancer, since DOX-loaded OCH nanoparticles exhibited significant inhibitory effects on A549 cells as compared to DOX solution. They concluded that low molecular weight OCH nanoparticles have potential as carriers for antitumor agents. The blank OCH nanoparticles showed no cytotoxicity to mouse embryo fibroblasts or human lung cancer cell line A549 [84]. Beisner et al. developed chitosan-coated PLGA nanoparticles to mediate efficient delivery of 2′-O-methyl-RNA into human lung cancer cells [85]. Cellular uptake of the inhibitor mediated by chitosan-coated PLGA nanoparticles was greatly enhanced compared to the uptake of ASO alone, as shown by flow cytometry analysis. Results clearly showed that the chitosan-coated PLGA nanoparticles were suitable for delivery of 2′-O-methyl-RNA and induced effective telomerase inhibition and telomere shortening in human lung cancer cells [85]. Also, complexes such as chitosan-modified PLGA Nanospheres (CS-PLGA NS) were designed to be preferentially taken up by human lung adenocarcinoma cells (A549) [86]. Cellular uptake of CS-PLGA NS by lung cells (A549) was energy-dependent, suggesting a clathrin-mediated endocytic process. It was also observed that CS-PLGA NS showed low cytotoxicity, similar to non-PLGA NS [86]. In a further exploration of the usefulness of chitosan nanoparticles, Yang et al. developed a method of encapsulating PTX-loaded CNPs (PTX-CNPs) to understand the mechanism of the preferential accumulation of PTX in lung tumors [87]. Parameters such as ζ-potential and in vitro cellular cytotoxicity (A549 cells and CT-26 cells) of PTX-CNPs, and in vitro uptake of coumarin 6 to lung cells from chitosan-modified PLGA nanoparticles containing coumarin 6 (coumarin 6-CNPs) were examined. However, the in vitro uptake of coumarin 6 by A549 cells and CT-26 cells was enhanced at lower pH for coumarin-6-CNPs. Analyses showed that PTX-CNPs showed enhanced cytotoxicity as the pH became more acidic. Therefore, enhanced electrostatic interaction between chitosan-modified PLGA nanoparticles and the acidic microenvironment of tumor cells appears to be an underlying mechanism of lung tumor-specific accumulation of PTX from PTX-CNPs [87].
Methods for preparing polymeric amphiphilic nanoparticles based on oleoyl-chitosan (OCH) loaded with DOX were developed by Zhang et al. and involved envelopment of the OCH nanoparticles efficiently loaded with DOX and provided a sustained released after a burst release in PBS [88]. Nanoparticles alone showed no cytotoxicity to mouse embryonic fibroblasts (MEF) and low hemolysis rates (<5%). Human lung carcinoma cells (A549) and mouse macrophages (RAW264.7) were used to determine the time and concentration dependence of cellular uptake by incubating with fluorescently labeled OCH nanoparticles. Their findings revealed that the activity of OCH nanoparticles increases cancer cell uptake of DOX, resulting in significant improvement for therapeutic efficiency [88]. Novel Pluronic/chitosan nanocapsules encapsulating iron oxide nanoparticles were produced by Bae et al., resulting shell crosslinked nanocapsules with a unique core–shell nanoreservoir architecture: an inner core encapsulating magnetic nanoparticles and a hydrophilic Pluronic/chitosan polymer shell layer [89]. Confocal laser scanning microscopy of rhodamine-labeled nanocapsules clearly showed efficient internalization of the nanocapsules by human lung carcinoma cells upon exposure to an external magnetic field. These novel Pluronic/chitosan nanocapsules encapsulating iron oxide nanoparticles were suitable for the magnetically triggered delivery of various anticancer agents and for successful cancer diagnosis using magnetic resonance imaging [89].
Taetz et al. developed a method utilizing tailorable cationic chitosan–PLGA nanoparticles for the delivery of an antisense 2′-O-methyl-RNA (2OMR) directed against the RNA template of human telomerase [90]. The efficacy of the nanoplex system was determined by measurements of binding efficiency, complex stability, and uptake in different human lung cell types. Results of flow cytometry analysis clearly showed that the uptake of 2OMR into A549 lung cancer cells was considerably higher in combination with nanoparticles than alone, and was dependent on the amount of chitosan. Furthermore, the uptake into A549 cells was confirmed by confocal laser scanning microscopy and suggested that uptake is mediated via complexes of 2OMR and chitosan–PLGA nanoparticles [90]. To produce nanoparticles as vehicles for anticancer compounds to lung, Yang et al. developed a method of preparing chitosan-modified PTX-loaded PLGA nanoparticles [91]. Their findings revealed that the loading of drug-encapsulating nanoparticles was significantly high. Data also demonstrated that a lung-specific increase in the distribution index of PTX [i.e., AUC (lung)/AUC (plasma)] was observed for chitosan-modified nanoparticles (e.g., 99.9 for nanoparticles versus 5.4 for Taxol) when nanoparticles were administered to lung-metastasized mice via the tail vein at a PTX dose of 10 mg/kg. These findings revealed the transient formation of aggregates in the blood stream followed by enhanced trapping in the lung capillaries. An electrically mediated interaction appeared to be responsible for the lung-tumor-specific distribution of the chitosan-modified nanoparticles via an enhanced uptake across the endothelial cells of the lung tumor capillary [91].
Another chitosan colloidal, consisting of oily core and a chitosan coating, was utilized for targeting human lung carcinoma cells for anticancer drug delivery. Lozano et al. developed a method of preparing biodegradable colloidal carrier loaded with DTX to facilitate a controlled intracellular delivery of the drug [72]. Flow cytometry analysis in a human lung cells showed that the fluorescent chitosan carriers were rapidly internalized and that almost 100% of A549 cells were fluorescent. Data revealed that for 24 h after treatment, DTX-loaded chitosan carriers had a greater effect on cell proliferation than free DTX. With this delivery system, the DTX anticancer agent remains fully active upon its encapsulation into the colloidal chitosan carrier and resulted in active delivery of drug into cancer cells and increasing treatment specificity [72]. Hydrophobically modified GC (HGC) nanoparticles, a new nanosized drug carrier, were prepared by Hwang et al. by introducing a hydrophobic molecule, cholanic acid, to water-soluble GC [92]. The HGC nanoparticles were formulated comprising DTX-loaded self-assembled aggregates with a mean diameter of 350 nm in aqueous condition using a dialysis method. The DTX–HGC nanoparticles were well dispersed and stable for 2 weeks under physiological conditions (pH 7.4 and 37°C) and showed a sustained drug release profile in vitro. In addition, the DTX–HGC nanoparticles were found to be stable in the presence of excess bovine serum albumin, which suggests that the DTX–HGC nanoparticles might also be stable in the blood stream. Furthermore, noninvasive live animal imaging technology showed the time-dependent excretion profile, in vivo biodistribution, prolonged circulation time, and tumor targeting ability of the DTX–HGC nanoparticles. Finally, under optimal conditions for cancer therapy, the DTX–HGC nanoparticles clearly showed a higher antitumor efficacy (e.g., reduced tumor volume and increased survival rate) in mice bearing A549 lung cancer cells, and strongly reduced the anticancer drug toxicity compared to free DTX in tumor-bearing mice. The studies on encapsulating DTX illustrated the efficacy of nanosized drug carriers and demonstrated a promising nanosized drug formulation for cancer therapy [92].
Nafee et al. studied chitosan-coated PLGA nanoparticles utilizing AOS to lung cancer cells [93]. Biodegradable nanoparticles of 130 nm were formed and the adjustable surface charge tailored by controlling the process parameters. As a proof of concept, the overall potential of these particulate carriers to bind the AOS 2′-O-methyl-RNA and improve its cellular uptake was demonstrated. The study proved the efficacy of chitosan-coated PLGA nanoparticles as a flexible and efficient delivery system for AOS to lung cancer cells [93].
Cafaggi et al. developed a technique utilizing an anionic cisplatin–alginate complex with a cationic polyelectrolyte, i.e., chitosan or N-trimethyl chitosan nanoparticles were prepared through electrostatic interaction [94]. Particles of 180–350 nm mean diameter were formed, and cisplatin–alginate complex release studies showed that almost all the drug was released in saline-buffered solution at pH 7.4, i.e., approximately 40% w/w of total cisplatin was released from negative nanoparticles and roughly 50% w/w from positive nanoparticles. Furthermore, the drug loading of nanoparticles with a positive ζ-potential (43 mV–60 mV) ranged from 13 to 21% w/w and particle yield (referred to total polymers) was about 15% w/w (50% w/w if referred to the cisplatin–alginate complex). On A549 human cells, the nanoparticles with the smallest size and the lowest positive ζ-potential were more active than cisplatin and showed a similar capability to induce apoptosis in other human cancer cells (A2780). These results indicate that cisplatin complexes with polycarboxylate polymers can be transformed into cisplatin particulate carriers for anticancer therapy [94]. Another interesting study demonstrates that use of biomaterial chitosan to form chitosan–siRNA nanoparticles for gene silencing protocols. Liu et al. directed much effort towards the application of chitosan as a nonviral carrier for siRNA and the importance of polymeric properties for the optimization of gene silencing using chitosan–siRNA nanoparticles [95]. The studies showed that the physicochemical properties (size, ζ-potential, morphology, and complex stability) and in vitro gene silencing of chitosan–siRNA nanoparticles are strongly dependent on chitosan molecular weight (Mw) and degree of deacetylation (DD). High Mw and DD of chitosan resulted in the formation of discrete stable nanoparticles of approximately 200 nm in size. Data revealed that chitosan–siRNA formulations (N:P 50) prepared with low Mw (approximately 10 kDa) chitosan showed almost no knockdown of endogenous enhanced green fluorescent protein (EGFP) in H1299 human lung carcinoma cells, whereas those prepared from chitosan of higher Mw (64.8–170 kDa) and DD (approximately 80%) showed greater gene silencing that ranged between 45 and 65%. Interesting, the study achieved the highest gene silencing efficiency (80%) using chitosan–siRNA nanoparticles at an N: P ratio of 150 using higher Mw (114 and 170 kDa) and DD (84%) that correlated with formation of stable nanoparticles of approximately 200 nm [95].
3.4 Ovarian Cancer
Ovarian carcinoma is the leading cause of death from gynecologic malignancy, which is due to its late initial diagnosis in addition to recurrence of ovarian cancer associated with resistance to therapy. To date, several depot systems have been designed for local delivery for ovarian cancer therapy. Nanotechnology has great promise in addressing existing problems and could improve diagnosis and therapy of ovarian cancer. As an example, Han et al. developed an Arg-Gly-Asp (RGD) peptide-labeled chitosan nanoparticle (RGD-CNP) by thiolation reaction [96]. In vitro studies examined the binding of RGD-CNP with αvβ3 integrin by flow cytometry and fluorescence microscopy. A human ovarian cancer-bearing orthotopic animal model utilizing RGD-CNPs loaded with siRNA showed significant increased selective intratumoral delivery. In addition, the same group showed targeted silencing of multiple growth-promoting genes (POSTN, FAK, and PLXDC1) along with therapeutic efficacy in the SKOV3ip1, HeyA8, and A2780 models using siRNA incorporated into RGD-CNP (siRNA/RGD-CNP) [96]. Furthermore, the in vivo tumor vascular targets using RGD-CNP by delivering PLXDC1-targeted siRNA into the αvβ3 integrin-positive tumor endothelial cells in A2780 tumor-bearing mice [96]. These studies showed that RGD-CNP is a novel and highly selective delivery system for siRNA, with the potential for broad applications in human disease and especially ovarian cancer [96]. Liu et al. developed a method of target diagnosis of ovarian cancer using magnetic resonance imaging and used prepared anti-Sperm protein 17 (Sp17) immunomagnetic nanoparticles (IMNPs) [97]. To assess the anti-Sp17 IMNPs for study of ovarian cancer target therapy, the group developed a method involving complex formation between the anti-human Sp17 IMNPs by grafting anti-Sp17 antibodies on the surface of chitosan-coated magnetic nanoparticles (MNPs) using the linker EDC/NHS [1-ethyl-3-(3-dimethylaminopropyl)carbodiimide/N-hydroxysuccinimide]. In addition, the immunologic activity of IMNPs was evaluated by enzyme-linked immunosorbent assay (ELISA). The efficacy was determined using ovarian cancer HO-8910 cells by transfecting IMNPs with human Sp17 gene. Results clearly showed that the MNPs grafted with anti-Sp17 antibody and the IMNPs kept good bioactivity and a significant targeting of cells was observed [97]. Yang et al. developed a method of targeting Multi drug resistant 1 genes (MDR1) that can effectively reverse the PTX resistance in A2780/TS cells in a time-dependent manner using PTX-loaded chitosan/pshRNA plasmid nanoparticle preparations [98]. Nanoparticles were synthesized by means of a complex coacervation technique and A2780/TS cells transfected with MDR1-targeted chitosan/pshRNA plasmid nanoparticles were examined. Cells transfected with chitosan/pGPU6/GFP/Neo no-load plasmid nanoparticles served as negative control cells. Furthermore, the MDR1 mRNA in the transfected cells was significantly decreased by 17.6, 27.8, and 52.6% on post-transfection days 2, 4, and 7, respectively, when compared with that in A2780/TS control cells (P < 0.05). Data clearly suggest that the IC50 of PTX for A2780/TS cells, as determined by the MTT method, revealed that the relative reversal efficiency increased over time and was 29.6, 51.2, and 61.3% in the transfected cells at 2, 4, and 7 days after transfection, respectively, and that IC50 values (0.197 ± 0.003, 0.144 ± 0.001, and 0.120 ± 0.004) decreased, with the difference being significant (P < 0.05) as compared to A2780/TS control cells (0.269 ± 0.003) [98].
Localized and sustained delivery of anticancer agents to the tumor site has great potential for the treatment of solid tumors. Lim Soo et al. proposed the utilization of PLA-b-PEG/PLA nanoparticles containing a chitosan–egg phosphatidylcholine (chitosan-ePC) implant system for the delivery of PTX to treat ovarian cancer [99]. Overproduction of ascites fluid in the peritoneal cavity is a physical manifestation of ovarian cancer. The efficacy of PTX was determined by in vitro release studies from the implant system and were conducted in various fluids including human ascites fluid. The experimental data showed a strong correlation (r 2 = 0.977) between the release of PTX in ascites fluid and in PBS containing lysozyme (pH 7.4) at 37°C. In addition, the swelling, degradation, and morphology data suggested that the drug release mechanism. Furthermore, healthy Balb/C mice were used to confirm that the in vitro release of PTX was a good indicator of the in vivo release profile (correlation between release rates: r 2 = 0.965). Healthy Balb/C mice were also used to determine the efficiency of the release of PTX over a 4-week period following implantation of the chitosan-ePC system into the peritoneal cavity of mice. Further results indicated that there was constant level of PTX concentration in both plasma and tissues (e.g., liver, kidney, and small intestine) [99].
Nanoparticle carriers of encapsulated anionic cisplatin–alginate complex with a cationic polyelectrolyte (known as chitosan or N-trimethyl chitosan) may also be modified to provide efficient drug release in the human ovarian carcinoma cell lines [94]. Cafaggi et al. developed a technique utilizing anionic cisplatin–alginate complex with chitosan or N-trimethyl chitosan nanoparticles for efficient drug release [94]. Mean particle diameter ranged from 180 to 350 nm and cisplatin–alginate complex release studies showed almost all the drug in saline-buffered solution at pH 7.4: approximately 40% w/w of total cisplatin was released from negative nanoparticles and roughly 50% w/w from positive ones. Furthermore, the drug loading of nanoparticles with a positive ζ-potential (43–60 mV) ranged from 13 to 21% w/w, and the particle yield (referred to total polymers) was about 15% w/w (50% w/w if referred to cisplatin–alginate complex). Human and murine model studies showed that the cytotoxic activity of the positive nanoparticles was similar to or lower than that of cisplatin, probably depending on the combination of size and ζ-potential values, in P388 murine and A2780 human cells. These results indicate that cisplatin complexes with polycarboxylate polymers can be transformed into cisplatin particulate carriers for anticancer therapy [94].
Grant et al. developed a method of reducing therapeutic difficulties associated with PTX preparation and use by encapsulating PTX into chitosan and ePC [100]. The method involved preparation of composite films for localized drug delivery using chitosan and ePC. Therapeutic efficacy was determined using chitosan-ePC film as a matrix for the localized delivery of PTX. Nanoparticles containing PTX were dispersed throughout the chitosan-ePC film to result in a drug:material ratio of 1:8 (wt/wt). Results clearly showed that the composite film provided a sustained release of PTX over a 4-month period in biologically relevant media. It was proposed that utilization of PTX loaded in the chitosan-ePC film could provide sustained release of the drug in SKOV-3 human ovarian cancer cells [100].
Therapeutic efficiency of the delivery of camptothecin is limited by the low aqueous solubility and high toxicity of the drug. Zhou et al. developed a method of preparing camptothecin encapsulation in N-trimethyl chitosan (CPT-TMC) to increase its water-solubility and lower its side effects, and tested it on a high potential lymphogenous metastatic model of human ovarian cancer [101]. In that study, SKOV3 cells were transfected with VEGF-D recombinant plasmid DNA (pcDNA3.1(±)/VEGF-D) and stable SKOV3/VEGF-D cell lines were established to study the lymphogenous metastatic model. In vivo nude mice model studies looked at the antitumor and antimetastatic activities of CPT-TMC after subcutaneous injection with SKOV3/VEGF-D cells. In contrast to controls, the results clearly showed that the administration of CPT-TMC achieved effective inhibition of primary tumor volume and lymphogenous metastasis, yet without apparent systemic toxic effects. These effects were associated with simultaneously downregulated VEGF-D and MMP-9 expression, significantly decreased tumor-associated lymphatic and blood sprouts, tremendously reduced systemic toxic effects, and dramatically increased tumor apoptotic index. The investigator proposed that CPT-TMC is superior to CPT because of maximizing its anticancer and antimetastatic activities with minimal toxicity on hosts, suggesting that treatment with CPT-TMC can be a highly efficient and effective therapeutic strategy against advanced human ovarian cancer [101].
In a further exploration of the usefulness of nanocarriers, Li et al. developed a method of encapsulating tCPT to overcome the problem of low water solubility and severe toxicity of CPT after intravenous administration [102]. The method of preparation is based on using chitosan and dibasic sodium phosphate (DSP) to encapsulate CPT intended for local administration. Encapsulation of CPT nanocolloids had a large effect on the gelling time as well as the micro-structure of the hydrogel. Data from both in vitro and in vivo degradation studies revealed that the chitosan/DSP hydrogel was biodegradable and biocompatible. In vitro release studies revealed that CPT was released from chitosan/DSP hydrogel over an extended period, with about 70% of total CPT released from hydrogel after 18 days. Furthermore, nearly 90% of CPT in the chitosan hydrogels could be preserved in the lactone form (active form) even after 7 days of storage at 37°C. Furthermore, in vitro cytotoxicity of CPT nanocolloids on SKOV3 human ovarian cancer cells suggested that good antitumor cell efficiency could be gained at a lower concentration [102]. A series of chitosan derivatives (mPEGOSC) with hydrophobic moieties of octyl and hydrophilic moieties of sulfate and polyethylene glycol monomethyl ether (mPEG) groups were synthesized by the group of Qu et al. [103]. The method involved preparation of PTX-loaded micelles into a chitosan complex. The in vivo–in vitro correlations of PTX-loaded micelles was studied, including interaction of the drug-loaded micelles with protein and the kinetics of PTX-loaded micelles with O-carboxymethylated chitosan (CMC). Data from tissue distribution studies in mice showed that PTX-mPEGOSC2000M micelles were phagocytozed less than PTX-OSC micelles by the reticulo-endothelial system (RES). Furthermore, a higher targeting efficiency of PTX-mPEGOSC2000M to the uterus (including ovary) was estimated. Together, the results of Qu et al. suggested that PTX-encapsulated formulations could be used for the chemotherapy of ovarian cancer [103]. Anticancer agents known to have a high effect in anticancer treatment, such as PTX, are either unable to be formulated safely or do not have a well-tolerated method of administration [104].
Vassileva et al. developed a method of preparing a novel chitosan-ePC implantable drug delivery system that is safe, less toxic, biocompatibile, and with antitumor efficacy [104]. The novel PTX-loaded ePC formulation was used in their experiment for providing controlled and sustained release of PTX (ePC) compared with commercial PTX formulated in Cremophor EL, PTX (CrEL). Therapeutic efficacy of PTX-loaded ePC was determined utilizing a human ovarian carcinoma SKOV-3-bearing xenograft model. Results clearly showed that the enhanced antitumor efficacy was achieved with PTX (ePC) in contrast to PTX (CrEL) with the same total dose of 60 mg/kg PTX. Furthermore, to determine the safety and toleration, toxicity studies were conducted using healthy CD-1 female mice. Data showed that the drug-free or PTX (ePC) formulations did not exhibit observable toxicity, local inflammation, or fibrous encapsulation of the implant. In contrast, mice receiving PTX (CrEL) or CrEL encountered significant toxicity, lethality, abnormal peritoneal organ morphology, and hepatic inflammation. The maximum tolerable dose (MTD) of PTX (CrEL) was 20 mg/kg/week, whereas PTX doses of up to 280 mg/kg/week were well tolerated when administered as PTX (ePC) [104].
Gene therapy is a method used to stimulate the body’s immune response so that it attacks cancer cells by introducing genetic material (DNA or RNA) to activate cellular processes [105]. Chitosan-mediated gene delivery has gained increasing interest due to its ability to treat cancers and genetic diseases [105]. Lee et al. developed a method utilizing folic acid covalently conjugated to chitosan (FACN) as a targeting ligand in an attempt to specifically deliver DNA to folate receptor-overexpressing ovarian and breast cancer cells. Cells from human epithelial ovarian cancer OV2008 and human breast cancer MCF-7 were used to determine the in vitro gene transfer potential of FACN. The FACN formed nanoparticles that, at a weight ratio of 10:1, exhibited significantly (P<0.01) enhanced gene transfer potential in folate receptor-overexpressing cancer cells as compared to unmodified chitosan. Transfection efficiency of FACN/pDNA nanocomplexes was shown to be competitively inhibited by free folic acid, suggesting that the specific gene delivery of FACN/pDNA nanocomplexes was achieved through folate receptor-mediated endocytosis. These results showed that the formed nanocomplex of FACN had a high gene delivery efficiency and is a promising carrier for cancer gene therapy [105].
3.5 Pancreatic Cancer
Pancreatic cancer is sometimes called a “silent killer” because early pancreatic cancer often does not cause symptoms, and the later symptoms are usually nonspecific and varied. Therefore, pancreatic cancer is often not diagnosed until it is advanced. Therefore, new treatment strategies are urgently required to combat this deadly disease. In cancer therapeutics, nanoparticle-mediated targeted delivery systems might significantly reduce the low toxicities and improve bioavailability. Zaharoff et al. developed techniques for investigating biodegradable polysaccharide chitosan co-formulated with intratumoral (i.t.) administration of interleukin (IL)-12 to enhance the antitumor activity of IL-12 while limiting its systemic toxicity [106]. IL-12 is a potent antitumor cytokine that exhibits significant clinical toxicities after systemic administration. Noninvasive imaging studies monitored local retention of IL-12, with and without chitosan co-formulation, after i.t. injection. Antitumor efficacy of IL-12 alone and of IL-12 co-formulated with chitosan (chitosan/IL-12) was assessed in mice bearing established colorectal (MC32a) and pancreatic (Panc02) tumors. Additional studies involving depletion of immune cell subsets, tumor rechallenge, and CTL activity were designed to elucidate mechanisms of regression and tumor-specific immunity. Data clearly indicated that co-formulation with chitosan increased local IL-12 retention from 1–2 days to 5–6 days. Weekly i.t. injections of IL-12 alone eradicated ≤10% of established MC32a and Panc02 tumors, while i.t. chitosan/IL-12 immunotherapy caused complete tumor regression in 80–100% of mice. Depletion of CD4(±) or Gr-1(±) cells had no impact on chitosan/IL-12-mediated tumor regression. However, CD8(±) or natural killer cell depletion completely abrogated antitumor activity. chitosan/IL-12 immunotherapy generated systemic tumor-specific immunity, as >80% of mice cured with i.t. chitosan/IL-12 immunotherapy were at least partially protected from tumor rechallenge. Furthermore, CTLs from spleens of cured mice lysed MC32a and gp70 peptide-loaded targets. Chitosan/IL-12 immunotherapy increased local retention of IL-12 in the tumor microenvironment, eradicated established aggressive murine tumors, and generated systemic tumor-specific protective immunity. Chitosan/IL-12 administration is a well-tolerated, effective immunotherapy with considerable potential for clinical translation [106]. Trickler et al. studied whether the drug gemcitabine loaded into chitosan/GMO nanostructures was able to enhance cellular accumulation and provide significant increase in cell death of human pancreatic cancer cells in vitro [107]. The delivery system was prepared by a multiple emulsion solvent evaporation method. The cellular accumulation, cellular internalization, and cytotoxicity of the nanostructures were evaluated by HPLC, confocal microscopy, or MTT assay in Mia PaCa-2 and BxPC-3 cells. The MTT cytotoxicity dose–response studies revealed that placebo at/or below 1 mg/mL has no effect on MIA PaCa-2 or BxPC-3 cells. The delivery system demonstrated a significant decrease in the IC50 (3–4 log unit shift) for gemcitabine nanostructures at 72 and 96 h post-treatment compared with treatment with a solution of gemcitabine alone. The nanostructure reported here can be resuspended in an aqueous medium, and demonstrated increased effective treatment compared with gemcitabine treatment alone in an in vitro model of human pancreatic cancer. The drug delivery system demonstrates the capability to entrap both hydrophilic and hydrophobic compounds to potentially provide an effective treatment option for human pancreatic cancer [107]. Chitosan/gelatin hydrogels were utilized for the functional longevity of microencapsulated islet cells during xenotransplantation [108]. Yang et al. demonstrated that the hydrogel acts as an immunoisolative matrix to provide additional protection to the microencapsulated islet cells [108]. This study assessed whether chitosan/gelatin hydrogels provide protection for the microencapsulated islet cells during xenotransplantation. Their data demonstrated the biocompatibility of the chitosan/gelatin hydrogel with the mouse insulinoma cell line, NIT-1. Insulinoma/agarose microspheres macroencapsulated in hydrogel revealed functional activity and secreted insulin continually for 60 days in vitro. Data clearly indicated that chitosan/gelatin hydrogel was not cytotoxic to islet cells, and in contrast, the hydrogel showed cytoprotective effects against cytokine-mediated cytotoxicity. In vivo, an insulinoma/agarose microsphere with chitosan/gelatin solution was applied as an injectable bioartificial pancreas (BAPs). As an experimental approach, an insulinoma/agarose microspheres suspended in phosphate-buffered saline or in chitosan/gelatin solution were injected into the subcutaneous layer of diabetic rats. Data clearly showed that the non-fasting blood glucose (NFBG) of diabetic rats transplanted with free insulinoma/agarose microspheres was decreased to euglycemia but restored to hyperglycemia in 15 days. By contrast, the NFBG of rats transplanted with insulinoma/agarose microspheres with hydrogel remained euglycemic for 42 days. After predetermined intervals, the histologic sections revealed that the fibrous tissue envelopment and the infiltrated immune-related cells contributed to the dysfunction of BAPs [108]. Similarly, the group of Yang et al. demonstrated again that chitosan/gelatin hydrogel can be used as a cell carrier for an injectable bioartificial pancreas; the hydrogel prolonged the function of cells encapsulated in agarose microspheres during xenogenic transplantation for protections [109]. The NFBG of diabetic rats injected with chitosan/gelatin hydrogel, which contained insulinoma/agarose microspheres, was maintained at less than 200 mg/dL for 25 days. The histological section revealed immune cell infiltration and accumulation within the hydrogel and around the insulinoma/agarose microspheres that may have contributed to the slowly increasing NFBG after day 25. Together, the data suggest that chitosan/gelatin hydrogel can provide an injectable bioartificial pancreas and achieve prolonged function of cells encapsulated in agarose microspheres during xenogenic transplantation [109].
Recently, RNase inhibitors, either synthetic or natural, have been intensively sought because they appeared to be promising for therapy of cancer and allergy [110]. However, there are only a limited number of efficient RNase inhibitors. Yakovlev et al. developed a system utilizing the low molecular weight chitosan [M(r) approximately 6 kDa] that inhibits the activity of pancreatic RNase A and some bacterial RNases, with inhibition constants in the range of 30–220 nM at pH 7.0 and ionic strength 0.14 M. The contribution to the chitosan complex formation with RNases is due to establishment of five or six ion pairs. RNase inhibitors are commonly used to block the RNase activity in manipulations with RNA-containing preparations. The results of this work show that polycations may efficiently inhibit ribonuclease activities [110].
3.6 Colon Cancer
Colorectal cancer is one of the leading causes of malignant death because it often remains undetected until later stages of the disease [111]. Kanthamneni et al. produced drug formulations using controlled release polymers chitosan, pectin, and hydroxypropyl methylcellulose (HPMC) for the targeted delivery of combinatorial regimens to the colon for the chemoprevention of colon cancer [111]. Furthermore, the use of aspirin in combination with calcium and folic acid was assessed for synergistic inhibitory responses of a novel chemopreventive combination regimen of drugs on two human colon cancer cell lines, HT-29 and SW-480. Chemopreventive combination regimens demonstrated significant synergistic efficacy in both cell lines using XTT assay studies, when compared to the effects of individual agents. With combinations of aspirin (5 mM) and folic acid (1.5 mM), HT-29 cells demonstrated a 30% decrease in cell viability compared to approximately 38% decrease in the SW-480 cell line. Overall, all drug combinations demonstrated significant synergistic responses in the cell lines tested, with the SW-480 cell line being more significantly affected by the drug regimens than the HT-29 cell line. Drug-encapsulating nanoparticles demonstrated a spherical morphology, <125 nm average particle size (aspirin and folic acid) of nanoparticles, and encapsulation efficiencies in the range of 80–91%. Drug release from nanoparticles was controlled, with approximately 60% of the original amount released over a 96 h period. Overall, the cell line studies demonstrated, for the first time, the ability of novel chemopreventive combinations to inhibit the growth of colon cancer cells, whereas the nanotechnology-based drug delivery system provides valuable evidence for targeted therapy towards colon cancer chemoprevention [111]. Akhlaghi et al. devised a process of forming nanoparticles containing insoluble anticancer drugs [76]. The method of preparation involved a complex formation of poly(methyl methacrylate) nanoparticles coated by chitosan–glutathione conjugate to encapsulate insoluble anticancer drugs. Nanoparticles were synthesized through radical polymerization of methyl methacrylate, initiated by cerium (IV) ammonium nitrate. PTX was encapsulated in nanoparticles with a maximal encapsulation efficiency of 98.27%. These nanoparticles showed sustained in vitro release of the incorporated PTX (75% of the loaded dose was released in 10 days). All nanoparticles had positive charge and were spherical, with a size range of about 130–250 nm. Data revealed that the PTX-loaded nanoparticles showed cytotoxicity for NIH 3 T3 and T47D breast carcinoma cells, and no cytotoxicity for two colon cell lines (HT29, Caco2) [76].
Researchers have also studied a nanoparticle system to deliver oxaliplatin to colorectal tumors. Jain et al. developed methods of preparing hyaluronic acid (HA)-coupled chitosan nanoparticles (HACTNP) bearing oxaliplatin (L-OHP) encapsulated in Eudragit S100-coated pellets for effective delivery to colon tumors [112]. The in vitro drug release was investigated using a United States Pharmacopoeia (USP) dissolution rate test paddle-type apparatus in different simulated gastrointestinal tract fluids. In a murine model, the pellets of free drug, and HA-coupled and uncoupled chitosan nanoparticles bearing L-OHP were administered orally at the dose of 10 mg L-OHP/kg body weight to tumor-bearing Balb/c mice. In vivo data showed that HACTNP delivered 1.99 ± 0.82 and 9.36 ± 1.10 μg of L-OHP/g of tissue in the colon and tumor, respectively, after 12 h, reflecting their targeting potential to the colon and tumor. These drug delivery systems show relatively high local drug concentration in the colonic milieu and colonic tumors with prolonged exposure time, which provides a potential to enhance antitumor efficacy with low systemic toxicity for the treatment of colon cancer [112]. Similarly, the group also investigated the use of HACTNP [113]. The method of preparation of HACTNP nanoparticles encapsulated 5-flurouracil (5FU) drug by an ionotropic gelation method, for the effective delivery of drug to the colon tumors. HACTNP appeared to be spherical in shape and mean size was found to be around 150 ± 3.4 nm, with low polydispersity index. The in vitro drug release was investigated in different simulated gastrointestinal tract fluids. The biocompatibility of nanoparticle formulations were evaluated for in vitro cytotoxicity by MTT assay using HT-29 cell lines, and cell uptake was assessed by fluorescent microscopy. In addition, the data demonstrated cellular uptake of HACTNP by incorporating calcein as a fluorescent marker. The cellular uptake of fluorescent HACTNP was clearly evidenced by fluorescence microscopy. HACTNP nanoparticles showed significant higher uptake by cancer cells as compared to uncoupled nanoparticles, and the uptake of HACTNPs by HT-29 colon cancer cells was observed to be 7.9 times more than uncoupled CTNPs at the end of 4 h. The cytotoxicity of 5FU incorporated in HACTNPs was higher compared to the conventional 5FU solution, even at lower concentrations. 5FU in HACTNP was about 2.60-fold more effective than free 5FU on HT-29 cells [113].
A study by Yang et al. designed an oral form of nanoparticle to encapsulate 5-aminolaevulinic acid (5-ALA) to improve the detection of colorectal cancer cells in vivo [114]. The nanoparticle should escape bacterial uptake in the gastrointestinal tract, which seriously interferes with the results of endoscopic observation. In this study, chitosan was mixed with sodium tripolyphosphate (STPP) and 5-ALA to prepare chitosan nanoparticles and 5-ALA-loaded chitosan nanoparticles (CNA) by adding 5-ALA solutions of different pH values and concentrations. The average particle size and ζ-potential of chitosan nanoparticles and CNA were measured by the Zetasizer-3000. The results revealed that particle size with different ζ-potential could be manipulated just by changing 5-ALA concentrations and pH values. CNA particles prepared at pH 7.4 and pH 9 of 5-ALA solutions with a concentration higher than 0.5 mg/mL showed a promising loading efficiency of up to 75% and an optimum average particle size of 100 nm. Fluorescence microscope examination showed that CNA could be engulfed by Caco-2 colon cancer cells, but showed no evidence of being taken up by Escherichia coli. This result implies that CNA could avoid the influence of normal flora inside the gut and serve as an adequate tool for fluorescent endoscopic detection of colorectal cancer cells in vivo [114].
Park et al. developed all-trans retinoic acid (ATRA)-incorporated nanoparticles of methoxy poly(ethylene glycol) (MPEG)-grafted chitosan through ion-complex formation between ATRA and chitosan preparation [115]. This nanoparticle was around 100 nm in diameter and had favorable reconstitution properties. An ATRA-incorporated nanoparticle has almost similar cytotoxicity against CT-26 tumor cells as free ATRA. But, nanoparticles were more effective at inhibiting invasion of tumor cells than free ATRA in an invasion test using matrigel. Apoptosis analysis revealed that tumor cells treated with free ATRA or ATRA-incorporated nanoparticles shown progressed cell death [115]. Studies also performed on chitosan nanoparticles and copper (II)-loaded chitosan nanoparticles were prepared on the basis of ionic gelation of chitosan with tripolyphosphate anions and copper ion sorption [116]. In their study, the cytotoxic activities of the chitosan nanoparticles and copper (II)-loaded chitosan nanoparticles was investigated and a relationship between physiochemical properties and activity is suggested. Data clearly demonstrates that the chitosan nanoparticles and copper (II)-loaded chitosan nanoparticles elicited dose-dependent inhibitory effects on the proliferation of tumor cell lines [116]. Folic acid can be covalently conjugated to chitosan molecules via its gamma-carboxyl moiety and thus retain a high affinity for colorectal cancer cells bearing folate receptor overexpression [117]. Colorectal cancer is one of the leading causes of malignant death and often goes undetected with current colonoscopy practices. Improved methods of detecting dysplasia and tumors during colonoscopy will improve mortality. Yang et al. studied the effect of folic acid-conjugated chitosan nanoparticles as a suitable vehicle for carrying 5-aminolaevulinic acid (5-ALA) to enhance the detection of colorectal cancer cells in vivo after a short-term uptake period [117]. The method involves preparation of chitosan conjugated with folic acid to produce folic acid-chitosan conjugate, which is then loaded with 5-ALA to create nanoparticles (fCNA). The loading efficiency of 5-ALA in fCNA particles and the z-average diameter were in the range 35–40% and 100 nm, respectively. The ζ-potential for fCNA was 20 mV, enough to keep the nanoparticle stable without aggregation. The fCNA is then incubated with HT29 and Caco-2 colorectal cancer cell lines overexpressing folate receptor on the surface of the cell membrane to determine the rate of accumulation of protoporphyrin IX (PpIX). The results show that fCNA can be taken up more easily by HT29 and Caco-2 cell lines after a short-term uptake period, most likely via receptor-mediated endocytosis, and that the PpIX accumulates in cancer cells as a function of the folate receptor expression and the folic acid modification. The work by Yang et al., suggested that the folic acid–chitosan conjugate could be an ideal vector for colorectal-specific delivery of 5-ALA for fluorescent endoscopic detection [117].
Another interesting approach has been studied by Ji et al. using chitosan nanoparticle-incorporated siRNA to knock down FHL2 gene expression [118]. Furthermore, the knockdown effect of the chitosan/siRNA nanoparticles on gene expression in FHL2 overexpressed human colorectal cancer Lovo cells was investigated. The results showed that FHL2 siRNA formulated within chitosan nanoparticles could knock down about 69.6% of FHL2 gene expression, which is very similar to the 68.8% reduced gene expression when siRNA was transfected with liposome Lipofectamine. Interestingly, protein expression was shown by western blot analysis to be reduced by the chitosan/siRNA nanoparticles. The results also showed that blocking FHL2 expression by siRNA could inhibit the growth and proliferation of human colorectal cancer Lovo cells. Yang et al., proposed that chitosan-based siRNA nanoparticles could be a very efficient delivery system for siRNA in vivo to colon cancer therapy [118]. Guo et al. investigated multifunctional nanocarriers based on chitosan/gold nanorod (CS-AuNR) hybrid nanospheres, which have been successfully fabricated by a simple nonsolvent-aided counterion complexation method [119]. Therapeutic efficiency of the delivery of anticancer drug cisplatin was investigated by loading into the obtained hybrid nanospheres. These CS-AuNR hybrid nanospheres were utilized for real-time cell imaging and as a near-infrared thermotherapy nanodevice to achieve irradiation-induced cancer cell death owing to the unique optical properties endowed by the encapsulated gold nanorods. The efficiency of the loaded anticancer drug cisplatin was studied in the cancer cells. The nanocarriers were an all-in-one system possessing drug delivery, cell imaging, and photothermal therapy functionalities [119]. Yang et al. developed high-performance nanoparticle for photodynamic detection of colorectal cancer, whereby alginate is physically complexed with folic acid-modified chitosan to form nanoparticles with improved drug release in the cellular lysosome [120]. The incorporated alginate molecules could complex stably with chitosan via electrostatic attraction, and the z-average diameter and ζ-potential of the prepared fCAN nanoparticles was 115 nm and 22 mV, respectively, enough to keep the nanoparticles stable in aqueous suspension without aggregation. Using this combined approach, efficiency of 5-ALA loading was assessed and 27% loading efficiency reported. The nanoparticles (fCANA) displayed no differences in particle size or ζ-potential compared to fCAN. Moreover, the fCANA nanoparticles showed uptake of nanoparticles by colorectal cancer cells via folate receptor-mediated endocytosis. Subsequently, the loaded 5-ALA was released in the lysosome, and this was promoted by the reduced intensity of attraction between chitosan and 5-ALA via the deprotonated alginate, resulting in a higher intracellular PpIX accumulation for the photodynamic detection. Together, these studies demonstrate that the alginate incorporated- and folic acid-conjugated chitosan nanoparticles are excellent vectors for colorectal-specific delivery of 5-ALA for fluorescent endoscopic detection [120].
3.7 Melanoma Cancer
Melanoma is the least common but most dangerous and serious type of skin cancer. Melanoma affects people of all ages but the chance of developing it increases with age. Some of the research has focused on tumor therapy and delivery systems using nanotechnology. Examples such as antiangiogenic peptide drugs have received much attention in the fields of tumor therapy and tumor imaging because they show promise in the targeting of integrins such as αvβ3 on angiogenic endothelial cells [121]. However, systemic antiangiogenic peptide drugs have short half-lives in vivo, resulting in fast serum clearance via the kidney, and thus the therapeutic effects of such drugs remain modest. Kim et al. developed techniques of preparation of self-assembled GC nanoparticles and explored whether this construct might function as a prolonged and sustained drug delivery system for RGD peptide, used as an antiangiogenic model drug in cancer therapy [121]. GC hydrophobically modified with 5β-cholanic acid formed nanoparticles with a diameter of 230 nm, and RGD peptide was easily encapsulated into HGC nanoparticles (yielding RGD-HGC nanoparticles) with a high loading efficiency (>85%). Data clearly demonstrated that, in vitro, RGD-HGC have prolonged and sustained release of RGD, lasting for 1 week. RGD-HGC also inhibited HUVEC adhesion to a βig-h3 protein-coated surface, indicating an antiangiogenic effect of the RGD peptide in the HGC nanoparticles. In additional in vivo studies, the antiangiogenic peptide drug formulation of RGD-HGC markedly inhibited bFGF-induced angiogenesis and decreased hemoglobin content in Matrigel plugs. Intratumoral administration of RGD-HGC resulted in significantly decreased tumor growth and microvessel density compared to native RGD peptide injected either intravenously or intratumorally, indicating that the RGD-HGC formulation strongly enhanced the antiangiogenic and antitumoral efficacy of RGD peptide by affording prolonged and sustained RGD peptide delivery locally and regionally in solid tumors [121].
Shikata et al. designed gadolinium loaded as gadopentetic acid (Gd-DTPA) in chitosan nanoparticles (Gd-CNPs), and studied their accumulation in vitro in cultured cells as an evaluation of their use gadolinium neutron-capture therapy (Gd-NCT) for cancer [122]. Using L929 fibroblast cells, the Gd accumulation for 12 h at 37°C was investigated at Gd concentrations lower than 40 ppm. The accumulation leveled above 20 ppm and reached 18.0 ± 2.7 (mean ± S.D.) μg Gd/106 cells at 40 ppm. Furthermore, the corresponding accumulations in B16F10 melanoma cells and SCC-VII squamous cell carcinoma, which were used in the previous Gd-NCT trials in vivo, were 27.1 ± 2.9 and 59.8 ± 9.8 μg Gd/106 cells, respectively, hence explaining the superior growth-suppression in the in vivo trials using SCC-VII cells. The accumulation of Gd-NCPs in these cells was 100–200 times higher than accumulation of Gd from dimeglumine gadopentetate aqueous solution (Magnevist), a magnetic resonance imaging contrast agent. The endocytic uptake of Gd-NCPs, strongly holding Gd-DTPA, was suggested from transmission electron microscopy and comparative studies at 4°C and with the solution system. These findings indicated that Gd-NCPs had a high affinity to the cells, probably contributing to the long retention of Gd in tumor tissue and leading to the significant suppression of tumor growth [122]. Interestingly, new class of chitosan-based hybrid nanogels by in-situ immobilization of CdSe quantum dots (QDs) in the chitosan–poly(methacrylic acid) (chitosan-PMAA) networks were developed by Wu et al. [123]. The method of preparation uses covalently crosslinked hybrid nanogels with chitosan chains semi-interpenetrating in the crosslinked PMAA. The networks exhibit excellent colloidal and structural stability as well as reversible physical property changes in response to a pH variation. In contrast, the hybrid nanogels formed by noncovalent physical association exhibit a significant change in the structure and composition upon exposure to physiological pH [123]. This distinction in the structural stability of hybrid nanogels produces very different outcomes for their biomedical applications. The covalently crosslinked hybrid nanogels have low cytotoxicity and could illuminate the B16F10 cells, sense environmental pH changes, and regulate the release of anticancer drug in the typical abnormal pH range of 5–7.4 found in the pathological zone, thus successfully combining multiple functionality into a single nanoobject. However, the physically associated hybrid nanogels exhibit a nonreversible pH-sensitive PL property and a significant cytotoxicity after 24 h treatment. It is crucial to construct a highly stable biopolymer–QD hybrid nanogel, via a rational design for safe bionanomaterials, to simultaneously combine the biosensing, bioimaging, and effective therapy functions [123].
Delivery nanoparticles system 200–300 nm of apoptin gene with O-carboxymethylated chitosan (CMC) to human melanoma cells A375 in vitro [124]. The ratio of chitosan to apoptin DNA (N:P ratio) was 5.5:1. The apoptin gene in chitosan/apoptin nanoparticles could be protected from DNase degradation and could be used as the model in the process of replication. Data clearly showed that, in human melanoma, A375 cells are transiently transformed by nanoparticles containing the apoptin gene and could induce apoptosis of A375 cells in a dose-dependent manner in vitro at 48 h after transformation. The investigator proposed that the chitosan vector and apoptin gene could be combined to be a safe nanoparticle gene delivery system, which could induce apoptosis in human melanoma A375 cells [124]. The studies from Kim et al. used drug-loaded HGC nanoparticles as a carrier system for PTX [63]. These self-assembled HGC conjugates were prepared by chemically linking 5β-cholanic acid to GC chains using 1-ethyl-3-(3-dimethylaminopropyl)-carbodiimide chemistry. The efficacy of PTX drug loaded into HGC nanoparticles was determined using a dialysis method. The nanoparticles were 400 nm in diameter and were stable in PBS for 10 days. Results clearly demonstrated that PTX-HGC nanoparticles showed sustained release of the incorporated of PTX (80% of the loaded dose was released in 8 days at 37°C in PBS). Owing to sustained release, the PTX-HGC nanoparticles were less cytotoxic to B16F10 melanoma cells than free PTX formulated in Cremophor EL. Injection of PTX-HGC nanoparticles into the tail vein of tumor-bearing mice prevented increases in tumor volume for 8 days. Kim et al. used this proposed system and showed that PTX was less toxic to the tumor-bearing mice when formulated in HGC nanoparticles than when formulated with Cremophor EL [63]. Self-assembled nanoparticles, formed by polymeric amphiphiles, have been demonstrated to accumulate in solid tumors by the enhanced permeability and retention effect, following intravenous administration [125]. Hyung Park et al. prepared hydrophobically modified GCs capable of forming nanosized self-aggregates by chemical conjugation of fluorescein isothiocyanate or DOX to the backbone of GC [125]. The biodistribution of self-aggregates (300 nm in diameter) was evaluated using tissues obtained from tumor-bearing mice, to which self-aggregates were systemically administered via the tail vein. Irrespective of the dose, a negligible quantity of self-aggregates was found in heart and lung, whereas a small amount (3.6–3.8% of dose) was detected in liver for 3 days after intravenous injection of self-aggregates. The distributed amount of self-aggregates gradually increased in tumor as blood circulation time increased. The concentration of self-aggregates in blood was as high as 14% of the dose at 1 day after intravenous injection and was still higher than 8% even at 3 days. Furthermore, the author investigated nanocomplexes loaded with DOX administered into tumor-bearing mice via the tail vein, and found that they exhibited lower toxicity than free DOX but comparable antitumor activity. These results revealed the promising potential of self-aggregates on the basis of GC as a carrier for hydrophobic antitumor agents [125]. Kabbaj et al. developed chitosan-DNA nanoparticles and determined their DNase susceptibility, and its possible influence on their antiproliferative activity [126].
Incorporation of DNA within chitosan nanoparticles significantly decreased degradation by DNase. Mycobacterium phlei DNA inhibits cancer cell division but is susceptible to degradation by DNase. To address the ability of M. phlei DNA-chitosan nanoparticles to inhibit melanoma cell division, the group studied M. phlei DNA and a cationic liposomal M. phlei DNA formulation. M. phlei DNA had antiproliferative activity (MTT reduction, IC50 = 0.9 mg/mL) without intrinsic cytotoxicity (LDH release, ED50 > 50 μg/mL). Cationic polyphosphate chitosan nanoparticles were inert (antiproliferative IC50 > 1 mg/mL, ED50 > 1 mg/mL). As a result, M. phlei DNA-chitosan nanoparticles were 20-fold more potent than M. phlei DNA. Cationic DOTAP/DOPE liposomes were cytostatic (IC50 = 49 μg/mL) and cytotoxic (ED50 = 87 μg/mL), and complexation of M. phlei DNA resulted in a significant reduction of antiproliferative activity. The author proposed that chitosan nanoparticles may therefore be appropriate delivery vehicles for M. phlei DNA [126].
Another interesting potential of gadolinium neutron-capture therapy (Gd-NCT) for cancer was evaluated using chitosan nanoparticles as a novel gadolinium device [127]. Tokumitsu et al. developed nanoparticle synthesis by incorporating 1,200 μg of natural gadolinium and studied the effect of intratumoral administration twice in mice bearing subcutaneous B16F10 melanoma. The thermal neutron irradiation was performed for the tumor site and demonstrated fluorescence of 6. 32 × 1012 neutrons/cm2, 8 h after the second gadolinium administration. The data clearly demonstrate that the tumor growth in the nanoparticle-administered group was significantly suppressed compared to that in the gadopentetate solution-administered group after the irradiation. This study demonstrated the potential usefulness of Gd-NCT using gadolinium-loaded nanoparticles [127]. This same group had also previously reported that Gd-CNPs) may be used for Gd-NCT [128]. Through emulsion-droplet coalescence technique, the group could show in vitro Gd-DTPA release from the Gd-CNPs in plasma over 24 h. In vivo data in mice bearing subcutaneous B16F10 melanoma on the releasing properties of Gd-CNPs and their ability for long-term retention of Gd-DTPA in the tumor indicated that Gd-CNPs might be useful as an i.t. injectable device for Gd-NCT [128]. Wang et al. studied chitosan sulfated derivatives to address the common structural requirement for the sulfate pattern to block P-selectin-mediated tumor cell adhesion [129]. Interestingly, the 6-O-sulfation of chitosan is indispensable for inhibition of P-selectin binding to human melanoma A375 cells and additional N-sulfation or 3-O-sulfation dramatically enhanced the inhibitory activity of 6-O-sulfated chitosan. The author proposed that efficient anti-P-selectin adhesion activity of sulfated saccharides needs the synergy of 6-O-sulfation and N- or 3-O-sulfation in glucosamine units [129].
Camptothecin (CPT) has recently attracted increasing attention as a promising anticancer agent for a variety of tumors. Liu et al. developed a technique to incorporate CPT with N-trimethyl chitosan (CPT-TMC) through microprecipitation and sonication. In this study, Liu et al. were able to demonstrate the inhibition effect on B16-F10 cell proliferation and induction of apoptosis in vitro [130]. Furthermore, the antitumor activity of CPT-TMC in C57BL/6 mice bearing B16-F10 melanoma showed significant inhibition compared with the group treated with free CPT (81.3% vs. 56.9%) in the growth of B16-F10 melanoma xenografts, and prolonged the survival time of the treated mice (P < 0.05). Data clearly showed decreased cell proliferation, increased tumor apoptosis as well as a reduction in angiogenesis. The group proposed that N-trimethyl chitosan-encapsulated camptothecin is superior to free CPT by overcoming its insolubility, and finally raises the potential of its application in melanoma therapy [130].
Antitumor efficacy and systemic toxicity of chitosan-based plumbagin microspheres in comparison to free plumbagin were proposed by Mandala Rayabandla et al. [131]. The optimized formulation had a mean particle size of 106.35 μm with an encapsulation efficiency of 80.12%. Pharmacokinetic studies showed a 22.2-fold increase in elimination half-life, t 1/2, of plumbagin from chitosan microspheres as compared to free plumbagin. In vivo data showed that administration of plumbagin microspheres resulted in a significant tumor growth inhibition and reduced systemic toxicity. Chitosan-based microspheres could be a promising strategy for the systemic delivery of anticancer agents like plumbagin [131]. The study by Kim et al. developed a local chemotherapy device using chitosan as a local drug carrier [132]. The anticancer drug ellagic acid (EA) was complexed with chitosan in the form of chitosan-EA films with concentrations of 0, 0.05, 0.1, 0.5, and 1% (w/v) of EA, and the films characterized. Studying a skin cancer model, the investigator used WM115 human melanoma cell line and demonstrated the cell response to the films with an antiproliferative effect through induction of apoptotic cell death compare to control HS68 human newborn fibroblast cells. In addition, the effect of composites on cell behaviors has been clearly demonstrated for use of local chemotherapy [132].
Nanosized and stable chitosan-g-PEG/heparin polyelectrolyte complexes were developed by Bae et al. [133]. The nanocomplex was utilized to study apoptotic death of cancer cells. The prepared polyelectrolyte complex micelles had a spherical shape with an average diameter of 162.8 ± 18.9 nm. They were highly stable and well dispersed even in the presence of serum due to the presence of a hydrophilic PEG shell layer surrounding the micelles. The polyelectrolyte complex micelles were internalized by cancer cells to a greater extent than free heparin alone, indicating that the dramatic cell death was attributed to the increased cellular uptake of heparin. The internalized heparin was shown to induce apoptotic death of the cancer cells via a caspase-dependent pathway. The proposed chitosan-g-PEG/heparin polyelectrolyte complex micelles facilitated the intracellular delivery of heparin, triggered the caspase activation, and consequently promoted apoptotic death of cancer cells [133].
The crucial event in metastasis is tumor invasion, which in the case of melanoma cells is dependent on matrix metalloprotease 2 (MMP2) [134]. Gorzelanny et al. studied chitosan-based attenuation to the invasive activity of melanoma cells in a cell-based invasion assay and reduced MMP2 activity in the supernatant of melanoma cells [134]. Investigator found that the expression level of MMP2 was not affected. The amount of MMP2 in the cell supernatant was reduced, indicating a post-transcriptional effect of chitosan on MMP2. Data from atomic force microscopy clearly demonstrated a direct molecular interaction between MMP2 and chitosan, forming a complex with a diameter of 349.0 ± 69.06 nm and a height of 26.5 ± 11.50 nm. The high binding specificity of MMP2 to chitosan, shown by affinity chromatography and a colorimetric MMP2 activity assay, suggests a noncompetitive inhibition of MMP2 by chitosan [134]. Laminin, a cell adhesion protein, consists of three peptide chains (α1, β1 and γ1) [135]. The β1 chain contains a Tyr-Ile-Gly-Ser-Arg (YIGSR) sequence that has been found to inhibit experimental metastasis in mice. Hojo et al. developed a method of preparation using a hybrid of a water-soluble chitosan and a laminin-related peptide [135]. A method involving the laminin-related peptide, acetyl-Tyr-Ile-Gly-Ser-Arg-βAla-OH (Ac-YIGSRβA-OH) reacted with a water-soluble chitosan. A small spacer, tert-butyloxycarbonyl-Gly, was intercalated in chitosan, using the TBTU method, to facilitate its coupling with the peptide. After removal of the protecting group, the Gly-chitosan was coupled with Ac-YIGSR βA-OH by the water-soluble carbodiimide method to give Ac-YIGSR βAG-chitosan. Conjugation of the peptide with the larger chitosan molecule did not reduce the inhibitory effect of the peptide on experimental metastasis in mice; it actually potentiated the antimetastatic effect, demonstrating that chitosan may be effective as a drug carrier for peptides [135].
3.8 Bladder Cancer
Bladder cancer is the fourth leading cause of cancer and it occurs about four times more frequently in men than in women. At the time of diagnosis, approximately 75% of bladder tumors are superficial, 20% are invasive, and up to 5% are metastatic. Superficial bladder cancer is initially managed by transurethral resection (TUR) to allow accurate tumor staging and grading. However, the recurrence rate of superficial bladder transitional cell carcinoma is reported to be between 50 and 80% and has a 15% chance of progression after TUR [136]. Therefore, intravesical chemotherapy or immunotherapy is required. However, intravesical drug delivery is challenged by the difficulty of establishment of a suitable and effective drug concentration because of periodical discharge of the bladder. In this context, researchers looked at different nanosystem deliveries to bladder. In the following examples, the clinical applicability of antibodies and plasmonic nanosensors as topically applied, molecule-specific optical diagnostic agents for noninvasive early detection of cancer and precancer is severely limited by our inability to efficiently deliver macromolecules and nanoparticles through mucosal tissues [137].
Ghosn et al. developed an imidazole-functionalized conjugate of the polysaccharide chitosan (chitosan-IAA) to enhance topical delivery of contrast agents, ranging from small molecules and antibodies to gold nanoparticles up to 44 nm in average diameter [137]. A result shown on contrast agent uptake and localization in freshly resected mucosal tissues was monitored using confocal microscopy. Chitosan-IAA was found to reversibly enhance mucosal permeability in a rapid, reproducible manner, facilitating transepithelial delivery of optical contrast agents. Permeation enhancement occurred through an active process, resulting in the delivery of contrast agents via a paracellular or a combined paracellular/transcellular route depending on size. In addition, co-administration of epidermal growth factor receptor-targeted antibodies with chitosan-IAA facilitated specific labeling and discrimination between paired normal and malignant human oral biopsies. Together, these data suggest that chitosan-IAA is a promising topical permeation enhancer for mucosal delivery of optical contrast agents [137]. Bilensoy et al. prepared cationic nanoparticles of chitosan, poly(ε-caprolactone) coated with chitosan (CS-PCL) and poly(ε-caprolactone) coated with poly-l-lysine (PLL-PCL) to encapsulate the intravesical chemotherapeutic agent Mitomycin C (MMC) for longer residence time, higher local drug concentration, and prevention of drug loss during bladder discharge [136]. Nanoparticle diameters varied between 180 and 340 nm depending on polymer used for preparation and coating. Zeta-potential values demonstrated the positive charge expected from cationic nanoparticles. The determination of MMC encapsulation efficiency was increased twofold for CS-PCL and threefold for PLL-PCL as a consequence of the hydrophilic coating. The cellular interaction was studied in CS-PCL nanoparticles loaded with Rhodamine123, sharing hydrophilic properties with MMC, which were selectively incorporated by the bladder cancer cell line, but not by normal bladder epithelial cells. The author proposed that the CS-PCL nanoparticles seem to be promising for MMC delivery with respect to anticancer efficacy against the MB49 bladder carcinoma cell line [136].
Interleukin-12 (IL-12) is a potent TH1 cytokine with robust antitumor activity and the ability to potentiate immunologic memory [138]. Unfortunately, intravesical IL-12 did not show antitumor efficacy in a recent clinical study of patients with recurrent superficial bladder cancer. Zaharoff et al. developed a co-formulation of IL-12 with chitosan, which demonstrated that 88–100% of mice bearing orthotopic bladder tumors were cured after four intravesical treatments with chitosan/IL-12 [138]. Antitumor responses following chitosan/IL-12 treatments were durable and provided complete protection from intravesical tumor rechallenge. Furthermore, urinary cytokine analysis showed that chitosan/IL-12 induced multiple TH1 cytokines at levels significantly higher than either IL-12 alone or BCG. Immunohistochemistry revealed moderate to intense tumor infiltration by T cells and macrophages following chitosan/IL-12 treatments. Bladder submucosa from cured mice contained residual populations of immune cells that returned to baseline levels after several months. The co-formulation of IL-12 with chitosan was proposed in this study because chitosan is a biocompatible, mucoadhesive polysaccharide that could improve intravesical IL-12 delivery and thus provide an effective and durable alternative for the treatment of superficial bladder cancer [138]. Oztürk et al. proposed pharmaco-therapeutic agent delivery systems for treating bladder cancer in order to supply a suitable dosage of the agent for a certain time period to solve problems due to the recurrency of tumoral tissues after TUR, when further treatment is necessary, usually in the form of intravesical chemotherapy or immunotherapy [139]. Oztürk et al. developed Mitomycin-C-loaded alginate and chitosan carriers to use as an alternative system in postoperative chemotherapy in bladder cancer. The carriers were prepared in the form of cylindrical geometries to facilitate the insertion of the carrier in in vivo studies. The effects of some parameters (i.e., polymer molecular weight, crosslinker concentration, Mitomycin-C to polymer ratio etc.) on the morphology, swelling behavior, bioadhesion, and in vitro drug release rate of the carriers indicated a promising approach for cancer treatment, especially bladder[139]. Similar work was also proposed by Eroğlu et al. for treating bladder cancer by a pharmacotherapeutic agent (i.e., Mytomycin-C) delivery system prepared using a mucoadhesive polymer (i.e., chitosan) in the form of cylindrical geometry to facilitate the insertion of the carrier for in vivo studies [140]. The chitosan carriers were prepared by crosslinking during the solvent evaporation technique. In the preparation of the chitosan carriers, chitosan polymers with different molecular weights, different amounts of crosslinker (i.e., glutaraldehyde), and different amounts of pharmacotherapeutic agent were used to obtain desired attachment onto the bladder wall and optimum release rate of the agent. On the other hand, because of the gelatinous structure of the chitosan, the swelling behavior of the polymer was periodically evaluated by gravimetric determinations in aqueous media [140].
Lekka et al. studied the effect of chitosan on the stiffness of the nonmalignant transitional epithelial cells of ureter (HCV 29) and the transitional cell cancer of urine bladder (T24) [141]. The investigations were performed in culture medium (RPMI 1640) containing 10% fetal calf serum in the presence of the microcrystalline chitosan of the three different deacetylation degrees. In parallel, the effect of chitosan on production of lactate and ATP levels was determined. The results showed a strong correlation between the decrease in energy production and the increase in Young’s modulus values obtained for the cancer cells treated with chitosan in living cells [141].
4 Conclusions
In this review, research has been highlighted on the directions and development of specific tumor targeting gene, protein, and local drug delivery systems using chitosan nanoparticles. These approaches show much promise for improving the therapeutic outcomes of cancer treatments. This review has also presented information on how nanoparticles take advantage of chitosan’s special features to act as effective carriers of agents for delivery to specific tumor sites. Nanotechnology has already advanced cancer detection and treatment. Abraxane is a major success story in the treatment of metastatic breast cancer, and has extended the scope of nanomedicine to other cancers and chemotherapeutic drugs. Nanotechnology has already begun shaping the way disease, particularly cancer, is diagnosed, treated, and monitored [142]. As technologies are perfected, side effects due to healthy cell damage will decrease, enabling patients to have a better quality of life and lengthening survival. A similar approach may be used in the near future to develop chitosan-based nanoparticle delivery for treatment of different human diseases, mainly in the field of cancer.
Abbreviations
- 5-ALA:
-
5-Aminolaevulinic acid
- CNP:
-
Chitosan-based nanoparticle
- CPT:
-
Camptothecin
- CS:
-
Chitosan
- DOX:
-
Doxorubicin hydrochloride
- DTX:
-
Docetaxel
- EA:
-
Ellagic acid
- ePC:
-
Egg phosphatidylcholine
- FACN:
-
Folic acid conjugated chitosan nanoparticle
- GC:
-
Glycol chitosan
- Gd-NCT:
-
Gadolinium neutron capture therapy
- GMO:
-
Glyceryl monooleate
- HACTNP:
-
Hyaluronic acid-coupled chitosan nanoparticles
- HGC:
-
Hydrophobically modified glycol chitosan
- HPMC:
-
Hydroxypropyl methylcellulose
- IL-12:
-
Interleukin 12
- IO:
-
Iron oxide
- MMC:
-
Mitomycin C
- MMP2:
-
Matrix metalloprotease-2
- MTX:
-
Methotrexate
- NFBG:
-
Nonfasting blood glucose
- NP:
-
Nanoparticle
- OCH:
-
Oleoyl chitosan
- PLGA:
-
Poly(lactide-co-glycolide)
- PTX:
-
Paclitaxel
- QD:
-
Quantum dot
- RGD-CNP:
-
Arg-Gly-Asp peptide-labeled chitosan nanoparticle
- siRNA:
-
Small interfering RNA
- SNAP:
-
Sertoli cell nanoparticle protocol
- SPION:
-
Superparamagnetic iron oxide nanoparticle
- TC:
-
6-N,N,N-Trimethyltriazole–chitosan
- TMC:
-
N-Trimethyl chtiosan
References
Brgger I, Dubernet C, Couvreur P (2002) Adv Drug Deliv Rev 54:631
McNeil SE (2005) Nanotechnology for the biologist. J Leukoc Biol 78:1–10
Weissleder R (2001) A clearer vision for in vivo imaging. Nat Biotechnol 19:316–317
Shenoy DB, Amiji MM (2005) Poly(ethylene oxide)-modified poly(epsiloncaprolactone) nanoparticles for targeted delivery of tamoxifen in breast cancer. Int J Pharm 293(1–2):261–270
Glen A (2005) The impact of nanotechnology in drug delivery: global developments, market analysis, and future prospects. Nanomarkets, Sterling, VA. Available at http://www.pharmamanufacturing.com/Media/MediaManager/NanoMarkets_Drug_Delivery_122004.pdf. Accessed 16 May 2011.
Safra T et al (2000) Pegylated liposomal doxorubicin (doxil): reduced clinical cardiotoxicity in patients reaching or exceeding cumulative doses of 500 mg/m2. Ann Oncol 11(8):1029–1033
Schroeder U et al (1998) Nanoparticle technology for delivery of drugs across the blood–brain barrier. J Pharm Sci 87(11):1305–1307
Raghuvanshi RS et al (2002) Improved immune response from biodegradable polymer particles entrapping tetanus toxoid by use of different immunization protocol and adjuvants. Int J Pharm 245(1–2):109–121
Kreutera J et al (1997) Influence of the type of surfactant on the analgesic effects induced by the peptide dalargin after its delivery across the blood–brain barrier using surfactant-coated nanoparticles. J Control Release 49:81
Fassas A et al (2003) Safety of high-dose liposomal daunorubicin (daunoxome) for refractory or relapsed acute myeloblastic leukaemia. Br J Haematol 122(1):161–163
Jean-Christophe L et al (1996) Biodegradable nanoparticles – from sustained release formulations to improved site specific drug delivery. J Control Release 39:339
Budhian A, Siegel SJ, Winey KI (2005) Production of haloperidol-loaded PLGA nanoparticles for extended controlled drug release of haloperidol. J Microencapsul 22(7):773–785
Gomez-Gaete C et al (2007) Encapsulation of dexamethasone into biodegradable polymeric nanoparticles. Int J Pharm 331(2):153–159
Cheng Q et al (2008) Brain transport of neurotoxin-I with PLA nanoparticles through intranasal administration in rats: a microdialysis study. Biopharm Drug Dispos 29:431
Mu L, Feng SS (2003) A novel controlled release formulation for the anticancer drug paclitaxel (taxol): PLGA nanoparticles containing vitamin E TPGS. J Control Release 86(1):33–48
Coester C et al (2000) Preparation of avidin-labelled gelatin nanoparticles as carriers for biotinylated peptide nucleic acid (PNA). Int J Pharm 196(2):147–149
Damge C, Maincent P, Ubrich N (2007) Oral delivery of insulin associated to polymeric nanoparticles in diabetic rats. J Control Release 117(2):163–170
Date AA, Joshi MD, Patravale VB (2007) Parasitic diseases: liposomes and polymeric nanoparticles versus lipid nanoparticles. Adv Drug Deliv Rev 59(6):505–521
Calvo P et al (2001) PEGylated polycyanoacrylate nanoparticles as vector for drug delivery in prion diseases. J Neurosci Methods 111(2):151–155
Ahmad Z et al (2006) Alginate nanoparticles as antituberculosis drug carriers: formulation development, pharmacokinetics and therapeutic potential. Indian J Chest Dis Allied Sci 48(3):171–176
Liu Z, Jiao Y, Wang Y, Zhou C, Zhang Z (2008) Polysaccharides-based nanoparticles as drug delivery systems. Adv Drug Deliv Rev 60:1650–1662
Kumar MN, Muzzarelli RA, Muzzarelli C, Sashiwa H, Domb AJ (2004) Chitosan chemistry and pharmaceutical perspectives. Chem Rev 104:6017–6084
Illum L (1998) Chitosan and its use as a pharmaceutical excipient. Pharm Res 15:1326–1331
Mumper RJ, Wang JJ, Claspell JM, Rolland AP (1995) Novel polymeric condensing carriers for gene delivery. In: Proceedings of the international symposium on controlled release bioactive materials, vol 22. Controlled Release Society, Deerfield, IL, pp 178–179
Park JH, Saravanakumar G, Kim K, Kwon IC (2010) Targeted delivery of low molecular drugs using chitosan and its derivatives. Adv Drug Deliv Rev 62(1):28–41
Haley B, Frenkel E (2008) Nanoparticles for drug delivery in cancer treatment. Urol Oncol 26(1):57–64
Kukowska-Latallo JF, Candido KA, Cao Z, Nigavekar SS, Majoros IJ, Thomas TP, Balogh LP, Khan MK, Baker JR Jr (2005) Nanoparticle targeting of anticancer drug improves therapeutic response in animal model of human epithelial cancer. Cancer Res 65(12):5317–5324
Bellocq NC, Pun SH, Jensen GS, Davis ME (2003) Transferrin-containing, cyclodextrin polymer-based particles for tumor-targeted gene delivery. Bioconjug Chem 14(6):1122–1132
Betancourt T, Brown B, Brannon-Peppas L (2007) Doxorubicin-loaded PLGA nanoparticles by nanoprecipitation: preparation, characterization and in vitro evaluation. Nanomedicine 2(2):219–232
Sutton D, Nasongkla N, Blanco E, Gao J (2007) Functionalized micellar systems for cancer targeted drug delivery. Pharm Res 24(6):1029–1046
Veronese FM, Pasut G (2005) PEGylation, successful approach to drug delivery. Drug Discov Today 10(21):1451–1458
Montet X, Montet-Abou K, Reynolds F, Weissleder R, Josephson L (2006) Nanoparticle imaging of integrins on tumor cells. Neoplasia 8(3):214–222
Flenniken ML, Liepold LO, Crowley BE, Willits DA, Young MJ, Douglas T (2005) Selective attachment and release of a chemotherapeutic agent from the interior of a protein cage architecture. Chem Commun (Camb) (4):447–449
Lowery AR, Gobin AM, Day ES, Halas NJ, West JL (2006) Immunonanoshells for targetedphotothermal ablation of tumor cells. Int J Nanomed 1(2):149–154
Kam NW, O’Connell M, Wisdom JA, Dai H (2005) Carbon nanotubes as multifunctional biological transporters and near-infrared agents for selective cancer cell destruction. Proc Natl Acad Sci USA 102(33):11600–11605
Gabizon AA (2001) Stealth liposomes and tumor targeting: one step further in the quest for the magic bullet. Clin Cancer Res 7:223–225
Konishi M, Tabata Y, Kariya M, Suzuki A, Mandai M, Nanbu K, Takakura K, Fujii S (2003) In vivo anti-tumor effect through the controlled release of cisplatin from biodegradable gelatin hydrogel. J Control Release 92:301–313
Kopecek J, Kopeckova P, Minko T, Lu Z (2000) HPMA copolymer-anticancer drug conjugates: design, activity, and mechanism of action. Eur J Pharm Biopharm 50:61–81
Lee ES, Na K, Bae YH (2005) Doxorubicin loaded pH-sensitive polymeric micelles for reversal of resistant MCF-7 tumor. J Control Release 103:405–418
Nishiyama N, Okazaki S, Cabral H, Miyamoto M, Kato Y, Sugiyama Y, Nishio K, Matsumura Y, Kataoka K (2003) Novel cisplatin-incorporated polymeric micelles can eradicate solid tumors in mice. Cancer Res 63:8977–8983
Avgoustakis K, Beletsi A, Panagi Z, Klepetsanis P, Karydas AG, Ithakissios DS (2002) PLGA-mPEG nanoparticles of cisplatin: in vitro nanoparticle degradation, in vitro drug release and in vivo drug residence in blood properties. J Control Release 79:123–135
Chytil P, Etrych T, Konak C, Sirova M, Mrkvan T, Rihova B, Ulbrich K (2006) Properties of HPMA copolymer–doxorubicin conjugates with pH-controlled activation: effect of polymer chain modification. J Control Release 115:26–36
Mitra A, Coleman T, Borgman M, Nan A, Ghandehari H, Line BR (2006) Polymeric conjugates of mono- and bi-cyclic alphaVbeta3 binding peptides for tumor targeting. J Control Release 114:175–183
Duvillard C, Romanet P, Cosmidis A, Beaudouin N, Chauffert B (2004) Phase 2 study of intratumoral cisplatin and epinephrine treatment for locally recurrent head and neck tumors. Ann Otol Rhinol Laryngol 113:229–233
Walter KA, Tamargo RJ, Olivi A, Burger PC, Brem H (1995) Intratumoral chemotherapy. Neurosurgery 37:1128–1145
Lammers T, Peschke P, Kuhnlein R, Subr V, Ulbrich K, Huber P et al (2006) Effect of intratumoral injection on the biodistribution and the therapeutic potential of HPMA copolymer-based drug delivery systems. Neoplasia 8:788–795
Park JH, Cho YW, Chung H, Kwon IC, Jeong SY (2003) Synthesis and characterization of sugar-bearing chitosan derivatives: aqueous solubility and biodegradability. Biomacromolecules 4:1087–1091
Kwon S, Park JH, Chung H, Kwon IC, Jeong SY, Kim IS (2003) Physicochemical characteristics of self-assembled nanoparticles based on glycol chitosan bearing 5b-cholanic acid. Langmuir 19:10188–10193
Son YJ, Jang JS, Cho YW, Chung H, Park RW, Kwon IC et al (2003) Biodistribution and anti-tumor activity of doxorubicin loaded glycol-chitosan nanoaggregates by EPR effect. J Control Release 91:135–145
Kim K, Kwon S, Park JH, Chung H, Jeong SY, Kwon IC (2005) Physicochemical characterizations of self-assembled nanoparticles of glycol chitosanedeoxycholic acid conjugates. Biomacromolecules 6:1154–1158
Yoo HS, Lee JE, Chung H, Kwon IC, Jeong SY (2005) Self-assembled nanoparticles containing hydrophobically modified glycol chitosan for gene delivery. J Control Release 103:235–243
Kim K, Kim JH, Kim S, Chung H, Choi K, Kwon IC et al (2005) Selfassembled nanoparticles of bile acid-modified glycol chitosans and their applications for cancer therapy. Macromol Res 13:167–175
Kim JH, Kim YS, Kim S, Park JH, Kim K, Choi K et al (2006) Hydrophobically modified glycol chitosan nanoparticles as carriers for paclitaxel. J Control Release 111:228–234
Park JH, Kwon S, Nam JO, Park RW, Chung H, Seo SB et al (2004) Selfassembled nanoparticles based on glycol chitosan bearing 5b-cholanic acid for RGD peptide delivery. J Control Release 95:579–588
Kim JH, Kim YS, Park K, Kang E, Lee S, Nam HY et al (2008) Self-assembled glycol chitosan nanoparticles for the sustained and prolonged delivery of antiangiogenic small peptide drugs in cancer therapy. Biomaterials 29:1920–1930
Park JH, Kwon S, Lee M, Chung H, Kim JH, Kim YS et al (2006) Self-assembled nanoparticles based on glycol chitosan bearing hydrophobic moieties as carriers for doxorubisin: in vivo biodistribution and anti-tumor activity. Biomaterials 27:119–126
Cho YW, Park SA, Han TH, Son DH, Park JS, Oh SJ et al (2007) In vivo tumor targeting and radionuclide imaging with self-assembled nanoparticles: mechanisms, key factors, and their implications. Biomaterials 28:1236–1247
Kim JH, Kim YS, Park K, Nam HY, Park JH, Choi K et al (2008) Antitumor efficacy of cisplatin-loaded glycol chitosan nanoparticles in tumor-bearing mice. J Control Release 127:41–49
Min KH, Park K, Kim YS, Bae SM, Lee S, Jo J et al (2008) Hydrophobically modified glycol chitosan nanoparticles-encapsulated camptothecin enhance the drug stability and tumor-targeting in cancer therapy. J Control Release 127:208–218
Lee SJ, Park K, Oh Y-K, Kwon S-H, Her S, Kim I-S, Choi K, Lee SJ, Kim H, Lee SG, Kim K, Kwon IC (2009) Tumor specificity and therapeutic efficacy of photosensitizer-encapsulated glycol chitosan-based nanoparticles in tumor-bearing mice. Biomaterials 30:2929–2939
Son YJ, Jang JS, Cho YW, Chung H, Park RW, Kwon IC, Kim IS, Park JY, Seo SB, Park CR, Jeong SY (2003) Biodistribution and anti-tumor activity of doxorubicin loaded glycol chitosan nanoaggregates by EPR effect. J Control Release 91:135–145
Kim K, Kim JH, Kim S, Chung H, Choi K, Kwon IC, Park JH, Kim YS, Park RW, Kim IS, Jeong SY (2005) Self-assembled nanoparticles of bile acid-modified glycol chitosans and their applications for cancer therapy. Macromol Res 13:167–175
Kim JH, Kim YS, Kim S, Park JH, Kim K, Choi K, Chung H, Jeong SY, Park RW, Kim IS, Kwon IC (2006) Hydrophobically modified glycol chitosan nanoparticles as carriers for paclitaxel. J Control Release 111:228–234
Park JH, Kwon S, Nam JO, Park RW, Chung H, Seo SB, Kim IS, Kwon IC, Jeong SY (2004) Self-assembled nanoparticles based on glycol chitosan bearing 5β-cholanic acid for RGD peptide delivery. J Control Release 95:579–588
Park K, Kim JH, Nam YS, Lee S, Nam HY, Kim K, Park JH, Kim IS, Choi K, Kim SY, Kwon IC (2007) Effect of polymer molecular weight on the tumor targeting characteristics of self-assembled glycol chitosan nanoparticles. J Control Release 122:305–341
Min KH, Park K, Kim YS, Bae SM, Lee S, Jo HG, Park RW, Kim IS, Jeong SY, Kim K, Kwon IC (2008) Hydrophobically modified glycol chitosan nanoparticles-encapsulated camptothecin enhance the drug stability and tumor targeting in cancer therapy. J Control Release 127(3):208–218
Tan WB, Jiang S, Zhang Y (2007) Quantum-dot based nanoparticles for targeted silencing of HER2/neu gene via RNA interference. Biomaterials 28:1565–1571
Pillé JY, Li H, Blot E, Bertrand JR, Pritchard LL, Opolon P, Maksimenko A, Lu H, Vannier JP, Soria J, Malvy C, Soria C (2006) Intravenous delivery of anti-RhoA small interfering RNA loaded in nanoparticles of chitosan in mice: safety and efficacy in xenografted aggressive breast cancer. Hum Gene Ther 17(10):1019–1026
Wu P, He X, Wang K, Tan W, He C, Zheng M (2009) A novel methotrexate delivery system based on chitosan-methotrexate covalently conjugated nanoparticles. J Biomed Nanotechnol 5(5):557–64
Le Renard PE, Jordan O, Faes A, Petri-Fink A, Hofmann H, Rüfenacht D, Bosman F, Buchegger F, Doelker E (2010) The in vivo performance of magnetic particle-loaded injectable, in situ gelling, carriers for the delivery of local hyperthermia. Biomaterials 1(4):691–705
Gao Y, Zhang Z, Chen L, Gu W, Li Y (2009) Synthesis of 6-N, N, N-trimethyltriazole chitosan via “click chemistry” and evaluation for gene delivery. Biomacromolecules 10(8):2175–2182
Lozano MV, Torrecilla D, Torres D, Vidal A, Domínguez F, Alonso MJ (2008) Highly efficient system to deliver taxanes into tumor cells: docetaxel-loaded chitosan oligomer colloidal carriers. Biomacromolecules 9(8):2186–2193
Trickler WJ, Nagvekar AA, Dash AK (2008) A novel nanoparticle formulation for sustained paclitaxel delivery. AAPS PharmSciTech 9(2):486–493
Cegnar M, Kos J, Kristl J (2006) Intracellular delivery of cysteine protease inhibitor cystatin by polymeric nanoparticles. J Nanosci Nanotechnol 6(9–10):3087–3094
Pamujula S, Hazari S, Bolden G, Graves RA, Chinta DM, Dash S, Kishore V, Mandal TK (2010) Preparation and in-vitro/in-vivo evaluation of surface-modified poly (lactide-co-glycolide) fluorescent nanoparticles. Pharm Pharmacol 62(4):422–429
Akhlaghi SP, Saremi S, Ostad SN, Dinarvand R, Atyabi F (2010) Discriminated effects of thiolated chitosan-coated pMMA paclitaxel-loaded nanoparticles on different normal and cancer cell lines. Nanomedicine 6(5):689–697
Feng S, Agoulnik IU, Truong A, Li Z, Creighton CJ, Kaftanovskaya EM, Pereira R, Han HD, Lopez-Berestein G, Klonisch T, Ittmann MM, Sood AK, Agoulnik AI (2010) Suppression of relaxin receptor RXFP1 decreases prostate cancer growth and metastasis. Endocr Relat Cancer 17(4):1021–1033
Lee CM, Jeong HJ, Cheong SJ, Kim EM, Kim DW, Lim ST, Sohn MH (2010) Prostate cancer-targeted imaging using magnetofluorescent polymeric nanoparticles functionalized with bombesin. Pharm Res 27(4):712–721
Springate CM, Jackson JK, Gleave ME, Burt HM (2008) Clusterin antisense complexed with chitosan for controlled intratumoral delivery. Int J Pharm 350(1–2):53–64
Springate CM, Jackson JK, Gleave ME, Burt HM (2005) Efficacy of an intratumoral controlled release formulation of clusterin antisense oligonucleotide complexed with chitosan containing paclitaxel or docetaxel in prostate cancer xenograft models. Cancer Chemother Pharmacol 56(3):239–247
Seong SK, Ryu JM, Shin DH, Bae EJ, Shigematsu A, Hatori Y, Nishigaki J, Kwak C, Lee SE, Park KB (2005) Biodistribution and excretion of radioactivity after the administration of 166Ho-chitosan complex (DW-166HC) into the prostate of rat. Eur J Nucl Med Mol Imaging 32(8):910–917
Chen WR, Liu H, Ritchey JW, Bartels KE, Lucroy MD, Nordquist RE (2002) Effect of different components of laser immunotherapy in treatment of metastatic tumors in rats. Cancer Res 62(15):4295–4299
Kumar A, Glaum M, El-Badri N, Mohapatra S, Haller E, Park S, Patrick L, Nattkemper L, Vo D, Cameron DF (2010) Initial observations of cell mediated drug delivery to the deep lung. Cell Transplant (in press). doi:10.3727/096368910X536491
Zhang J, Chen XG, Sun GZ, Huang L, Cheng XJ (2010) Effect of molecular weight on the oleoyl-chitosan nanoparticles as carriers for doxorubicin. Colloids Surf B Biointerfaces 77(2):125–130
Beisner J, Dong M, Taetz S, Nafee N, Griese EU, Schaefer U, Lehr CM, Klotz U, Mürdter TE (2010) Nanoparticle mediated delivery of 2′-O-methyl-RNA leads to efficient telomerase inhibition and telomere shortening in human lung cancer cells. Lung Cancer 68(3):346–354
Tahara K, Sakai T, Yamamoto H, Takeuchi H, Hirashima N, Kawashima Y (2009) Improved cellular uptake of chitosan-modified PLGA nanospheres by A549 cells. Int J Pharm 382(1–2):198–204
Yang R, Shim WS, Cui FD, Cheng G, Han X, Jin QR, Kim DD, Chung SJ, Shim CK (2009) Enhanced electrostatic interaction between chitosan-modified PLGA nanoparticle and tumor. Int J Pharm 371(1–2):142–147
Zhang J, Chen XG, Liu CS, Park HJ (2009) Investigation of polymeric amphiphilic nanoparticles as antitumor drug carriers. J Mater Sci Mater Med 20(4):991–999
Bae KH, Ha YJ, Kim C, Lee KR, Park TG (2008) Pluronic/chitosan shell cross-linked nanocapsules encapsulating magnetic nanoparticles. J Biomater Sci Polym Ed 19(12):1571–1583
Taetz S, Nafee N, Beisner J, Piotrowska K, Baldes C, Mürdter TE, Huwer H, Schneider M, Schaefer UF, Klotz U, Lehr CM (2009) The influence of chitosan content in cationic chitosan/PLGA nanoparticles on the delivery efficiency of antisense 2′-O-methyl-RNA directed against telomerase in lung cancer cells. Eur J Pharm Biopharm 72(2):358–369
Yang R, Yang SG, Shim WS, Cui F, Cheng G, Kim IW, Kim DD, Chung SJ, Shim CK (2009) Lung-specific delivery of paclitaxel by chitosan-modified PLGA nanoparticles via transient formation of microaggregates. J Pharm Sci 98(3):970–984
Hwang HY, Kim IS, Kwon IC, Kim YH (2008) Tumor targetability and antitumor effect of docetaxel-loaded hydrophobically modified glycol chitosan nanoparticles. J Control Release 128(1):23–31
Nafee N, Taetz S, Schneider M, Schaefer UF, Lehr CM (2007) Chitosan-coated PLGA nanoparticles for DNA/RNA delivery: effect of the formulation parameters on complexation and transfection of antisense oligonucleotides. Nanomedicine 3(3):173–183
Cafaggi S, Russo E, Stefani R, Leardi R, Caviglioli G, Parodi B, Bignardi G, De Totero D, Aiello C, Viale M (2007) Preparation and evaluation of nanoparticles made of chitosan or N-trimethyl chitosan and a cisplatin-alginate complex. J Control Release 121(1–2):110–123
Liu X, Howard KA, Dong M, Andersen MØ, Rahbek UL, Johnsen MG, Hansen OC, Besenbacher F, Kjems J (2007) The influence of polymeric properties on chitosan/siRNA nanoparticle formulation and gene silencing. Biomaterials 28(6):1280–1288
Han HD, Mangala LS, Lee JW, Shahzad MM, Kim HS, Shen D, Nam EJ, Mora EM, Stone RL, Lu C, Lee SJ, Roh JW, Nick AM, Lopez-Berestein G, Sood AK (2010) Targeted gene silencing using RGD-labeled chitosan nanoparticles. Clin Cancer Res 16(15):3910–3922
Liu Q, Ge YQ, Li FQ, Zhang SX, Gu N, Wang ZQ, Lu GM (2009) Biological activity assays and cellular imaging of anti-human sperm protein 17 immunomagnetic nanoparticles. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 25(11):987–990
Yang Y, Wang Z, Li M, Lu S (2009) Chitosan/pshRNA plasmid nanoparticles targeting MDR1 gene reverse paclitaxel resistance in ovarian cancer cells. J Huazhong Univ Sci Technol Med Sci 29(2):239–242
Lim Soo P, Cho J, Grant J, Ho E, Piquette-Miller M, Allen C (2008) Drug release mechanism of paclitaxel from a chitosan-lipid implant system: effect of swelling, degradation and morphology. Eur J Pharm Biopharm 69(1):149–57
Grant J, Blicker M, Piquette-Miller M, Allen C (2005) Hybrid films from blends of chitosan and egg phosphatidylcholine for localized delivery of paclitaxel. J Pharm Sci 94(7):1512–1527
Zhou L, Du L, Chen X, Li X, Li Z, Wen Y, Li Z, He X, Wei Y, Zhao X, Qian Z (2010) The antitumor and antimetastatic effects of N-trimethyl chitosan-encapsulated camptothecin on ovarian cancer with minimal side effects. Oncol Rep 24(4):941–948
Li X, Kong X, Zhang J, Wang Y, Wang Y, Shi S, Guo G, Luo F, Zhao X, Wei Y, Qian Z (2011) A novel composite hydrogel based on chitosan and inorganic phosphate for local drug delivery of camptothecin nanocolloids. J Pharm Sci 100(1):232–241
Qu G, Yao Z, Zhang C, Wu X, Ping Q (2009) PEG conjugated N-octyl-O-sulfate chitosan micelles for delivery of paclitaxel: in vitro characterization and in vivo evaluation. Eur J Pharm Sci 37(2):98–105
Vassileva V, Grant J, De Souza R, Allen C, Piquette-Miller M (2007) Novel biocompatible intraperitoneal drug delivery system increases tolerability and therapeutic efficacy of paclitaxel in a human ovarian cancer xenograft model. Cancer Chemother Pharmacol 60(6):907–914
Lee D, Lockey R, Mohapatra S (2006) Folate receptor-mediated cancer cell specific gene delivery using folic acid-conjugated oligochitosans. J Nanosci Nanotechnol 6(9–10):2860–2866
Zaharoff DA, Hance KW, Rogers CJ, Schlom J, Greiner JW (2010) Intratumoral immunotherapy of established solid tumors with chitosan/IL-12. J Immunother 33(7):697–705
Trickler WJ, Khurana J, Nagvekar AA, Dash AK (2010) Chitosan and glyceryl monooleate nanostructures containing gemcitabine: potential delivery system for pancreatic cancer treatment. AAPS PharmSciTech 11(1):392–401
Yang KC, Wu CC, Lin FH, Qi Z, Kuo TF, Cheng YH, Chen MP, Sumi S (2008) Chitosan/gelatin hydrogel as immunoisolative matrix for injectable bioartificial pancreas. Xenotransplantation 15(6):407–416
Yang KC, Wu CC, Cheng YH, Kuo TF, Lin FH (2008) Chitosan/gelatin hydrogel prolonged the function of insulinoma/agarose microspheres in vivo during xenogenic transplantation. Transplant Proc 40(10):3623–3626
Yakovlev GI, Mitkevich VA, Struminskaya NK, Varlamov VP, Makarov AA (2007) Low molecular weight chitosan is an efficient inhibitor of ribonucleases. Biochem Biophys Res Commun 357(3):584–588
Kanthamneni N, Chaudhary A, Wang J, Prabhu S (2010) Nanoparticulate delivery of novel drug combination regimens for the chemoprevention of colon cancer. Int J Oncol 37(1):177–185
Jain A, Jain SK, Ganesh N, Barve J, Beg AM (2010) Design and development of ligand-appended polysaccharidic nanoparticles for the delivery of oxaliplatin in colorectal cancer. Nanomedicine 6(1):179–190
Jain A, Jain SK (2008) In vitro and cell uptake studies for targeting of ligand anchored nanoparticles for colon tumors. Eur J Pharm Sci 35(5):404–416
Yang SJ, Shieh MJ, Lin FH, Lou PJ, Peng CL, Wei MF, Yao CJ, Lai PS, Young TH (2009) Colorectal cancer cell detection by 5-aminolaevulinic acid-loaded chitosan nano-particles. Cancer Lett 273(2):210–220
Park JS, Koh YS, Bang JY, Jeong YI, Lee JJ (2008) Antitumor effect of all-trans retinoic acid-encapsulated nanoparticles of methoxy poly(ethylene glycol)-conjugated chitosan against CT-26 colon carcinoma in vitro. J Pharm Sci 97(9):4011–4019
Qi L, Xu Z, Jiang X, Li Y, Wang M (2005) Cytotoxic activities of chitosan nanoparticles and copper-loaded nanoparticles. Bioorg Med Chem Lett 15(5):1397–1399
Yang SJ, Lin FH, Tsai KC, Wei MF, Tsai HM, Wong JM, Shieh MJ (2010) Folic acid-conjugated chitosan nanoparticles enhanced protoporphyrin IX accumulation in colorectal cancer cells. Bioconjug Chem 21(4):679–689
Ji AM, Su D, Che O, Li WS, Sun L, Zhang ZY, Yang B, Xu F (2009) Functional gene silencing mediated by chitosan/siRNA nanocomplexes. Nanotechnology 20(40):405103
Guo R, Zhang L, Qian H, Li R, Jiang X, Liu B (2010) Multifunctional nanocarriers for cell imaging, drug delivery, and near-IR photothermal therapy. Langmuir 26(8):5428–5434
Yang SJ, Lin FH, Tsai HM, Lin CF, Chin HC, Wong JM, Shieh MJ (2011) Alginate-folic acid-modified chitosan nanoparticles for photodynamic detection of intestinal neoplasms. Biomaterials 32(8):2174–2182
Kim JH, Kim YS, Park K, Kang E, Lee S, Nam HY, Kim K, Park JH, Chi DY, Park RW, Kim IS, Choi K, Kwon IC (2008) Self-assembled glycol chitosan nanoparticles for the sustained and prolonged delivery of antiangiogenic small peptide drugs in cancer therapy. Biomaterials 29(12):1920–1930
Shikata F, Tokumitsu H, Ichikawa H, Fukumori Y (2002) In vitro cellular accumulation of gadolinium incorporated into chitosan nanoparticles designed for neutron-capture therapy of cancer. Eur J Pharm Biopharm 53(1):57–63
Wu W, Shen J, Banerjee P, Zhou S (2010) Chitosan-based responsive hybrid nanogels for integration of optical pH-sensing, tumor cell imaging and controlled drug delivery. Biomaterials 31(32):8371–8381
Liu SS, Ben SB, Zhao HL (2008) Construction of apoptin gene delivery system and its effect on apoptosis of A375 cells. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 24(2):133–135
Hyung Park J, Kwon S, Lee M, Chung H, Kim JH, Kim YS, Park RW, Kim IS, Bong Seo S, Kwon IC, Young Jeong S (2006) Self-assembled nanoparticles based on glycol chitosan bearing hydrophobic moieties as carriers for doxorubicin: in vivo biodistribution and anti-tumor activity. Biomaterials 27(1):119–26
Kabbaj M, Phillips NC (2001) Anticancer activity of mycobacterial DNA: effect of formulation as chitosan nanoparticles. J Drug Target 9(5):317–328
Tokumitsu H, Hiratsuka J, Sakurai Y, Kobayashi T, Ichikawa H, Fukumori Y (2000) Gadolinium neutron-capture therapy using novel gadopentetic acid-chitosan complex nanoparticles: in vivo growth suppression of experimental melanoma solid tumor. Cancer Lett 150(2):177–182
Tokumitsu H, Ichikawa H, Fukumori Y (1999) Chitosan-gadopentetic acid complex nanoparticles for gadolinium neutron-capture therapy of cancer: preparation by novel emulsion-droplet coalescence technique and characterization. Pharm Res 16(12):1830–1835
Wang R, Huang J, Wei M, Zeng X (2010) The synergy of 6-O-sulfation and N- or 3-O-sulfation of chitosan is required for efficient inhibition of P-selectin-mediated human melanoma A375 cell adhesion. Biosci Biotechnol Biochem 74(8):1697–1700
Liu XP, Zhou ST, Li XY, Chen XC, Zhao X, Qian ZY, Zhou LN, Li ZY, Wang YM, Zhong Q, Yi T, Li ZY, He X, Wei YQ (2010) Anti-tumor activity of N-trimethyl chitosan-encapsulated camptothecin in a mouse melanoma model. J Exp Clin Cancer Res 29:76
Mandala Rayabandla SK, Aithal K, Anandam A, Shavi G, Nayanabhirama U, Arumugam K, Musmade P, Bhat K, Bola Sadashiva SR (2010) Preparation, in vitro characterization, pharmacokinetic, and pharmacodynamic evaluation of chitosan-based plumbagin microspheres in mice bearing B16F1 melanoma. Drug Deliv 17(3):103–13
Kim S, Liu Y, Gaber MW, Bumgardner JD, Haggard WO, Yang Y (2009) Development of chitosan-ellagic acid films as a local drug delivery system to induce apoptotic death of human melanoma cells. J Biomed Mater Res B Appl Biomater 90(1):145–155
Bae KH, Moon CW, Lee Y, Park TG (2009) Intracellular delivery of heparin complexed with chitosan-g-poly(ethylene glycol) for inducing apoptosis. Pharm Res 26(1):93–100
Gorzelanny C, Pöppelmann B, Strozyk E, Moerschbacher BM, Schneider SW (2007) Specific interaction between chitosan and matrix metalloprotease 2 decreases the invasive activity of human melanoma cells. Biomacromolecules 8(10):3035–3040
Hojo K, Maeda M, Mu Y, Kamada H, Tsutsumi Y, Nishiyama Y, Yoshikawa T, Kurita K, Block LH, Mayumi T, Kawasaki K (2000) Facile synthesis of a chitosan hybrid of a laminin-related peptide and its antimetastatic effect in mice. J Pharm Pharmacol 52(1):67–73
Bilensoy E, Sarisozen C, Esendağli G, Doğan AL, Aktaş Y, Sen M, Mungan NA (2009) Intravesical cationic nanoparticles of chitosan and polycaprolactone for the delivery of Mitomycin C to bladder tumors. Int J Pharm 371(1–2):170–176
Ghosn B, van de Ven AL, Tam J, Gillenwater A, Sokolov KV, Richards-Kortum R, Roy K (2010) Efficient mucosal delivery of optical contrast agents using imidazole-modified chitosan. J Biomed Opt 15(1):015003
Zaharoff DA, Hoffman BS, Hooper HB, Benjamin CJ Jr, Khurana KK, Hance KW, Rogers CJ, Pinto PA, Schlom J, Greiner JW (2009) Intravesical immunotherapy of superficial bladder cancer with chitosan/interleukin-12. Cancer Res 69(15):6192–6199
Oztürk E, Eroğlu M, Ozdemir N, Denkbaş EB (2004) Bioadhesive drug carriers for postoperative chemotherapy in bladder cancer. Adv Exp Med Biol 553:231–242
Eroğlu M, Irmak S, Acar A, Denkbaş EB (2002) Design and evaluation of a mucoadhesive therapeutic agent delivery system for postoperative chemotherapy in superficial bladder cancer. Int J Pharm 235(1–2):51–59
Lekka M, Laidler P, Ignacak J, Łabedz M, Lekki J, Struszczyk H, Stachura Z, Hrynkiewicz AZ (2001) The effect of chitosan on stiffness and glycolytic activity of human bladder cells. Biochim Biophys Acta 1540(2):127–136
Bharali DJ, Mousa SA (2010) Emerging nanomedicines for early cancer detection and improved treatment: current perspective and future promise. Pharmacol Ther 128(2):324–335
Acknowledgments
The financial support of DST fast track scheme to VKL (Ref No SERC/LS-0558/2009), and to RJ (Ref No SR/FT/CS-005/2008) is gratefully acknowledged. SVN is also grateful to DST, India, which partially supported this work, under a center grant of the Nanoscience and Nanotechnology Initiative program monitored by C. N. R. Rao. The author RJ is also grateful to Department of Biotechnology (DBT), Govt. of India for providing research support.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Lakshmanan, VK., Snima, K.S., Bumgardner, J.D., Nair, S.V., Jayakumar, R. (2011). Chitosan-Based Nanoparticles in Cancer Therapy. In: Jayakumar, R., Prabaharan, M., Muzzarelli, R. (eds) Chitosan for Biomaterials I. Advances in Polymer Science, vol 243. Springer, Berlin, Heidelberg. https://doi.org/10.1007/12_2011_132
Download citation
DOI: https://doi.org/10.1007/12_2011_132
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-23113-1
Online ISBN: 978-3-642-23114-8
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)