Abstract
The question of the financial balance of the health system is crucial for every country. The digitalization of health impacts strongly this issue and offers a new way to reconfigure the financial regulation. In the first section, we introduce the idea of cycle of care borrowed from Porter and his colleagues to escape from the traditional cost object, that is, the episode of care. In the second section, we explore new kinds of regulation applying the responsibilities of the actors inspired by the concept of commons (Ostrom, Governing the Commons—The Evolution of Institutions for Collective Action, Cambridge University Press, 1990). In the last section, we present examples where digitalization in health should promote this new way of regulation. Finally, we claim for a vision that articulates individualization of the health and collective empowerment of the actors.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
Digital health brings a disruptive advantage to patients by empowering them in a value co-creation process with health providers. This is reached by a Business to Consumer model. By doing so, digital health raises a main ethical issue that can be stated as follows: the patient should afford to be a digital health consumer; otherwise he/she cannot get access to it. This chapter contributes to address this issue by exploring digital health and identifying business models that may reconcile patient empowerment and equity. This leads us to propose a new typology of digital health business models.
The question of the financial balance of the health system is crucial for every country due to the on-going rise of expenses. The financial sustainability of Western health systems in the configuration allowing health services access for as many as possible is an increasingly debated issue. The Prospective Payment System (PPS)-driven regulation based on diagnosis-related group (DRG) fees has proved to fail both in containing health-care expenditures and in guaranteeing high-quality services as highlighted by Angelé-Halgand and Garrot (2014, 2015) for the French case. Researchers from various backgrounds try to address this issue by searching for disruptive innovation business models (Hwang and Christensen 2008) that would match the Anthropocene new deal characterized by increasing pressures put both on budgets and demand for care. In such a difficult context, Information Technologies (ITs) seem to bring a fruitful contribution as they promise to facilitate the development of better coordinated care models (Hunt 2013). Nevertheless, the issue is so complex than solutions that are based only on technology are likely not to be wholly satisfying: the resort to expertise in human and social sciences is required. Pointing out policies that pursue digitalization as a self-evident “solution” to problems in health care (Garrety et al. 2014) highlights the disruptive effects of national electronic health record systems on the production, ownership use and responsibility for health records. We aim at contributing to this debate by analysing a series of business models induced by digital health innovations and discussing their contribution to sustainable health accessible for as many as possible.
To do this, we first present a series of digital health innovations and propose to characterize them into those that relate to personalized health (1), those targeting community-based care providers (2) and those contributing to the performance management of healthcare delivery within a defined territory (3). We then analyse the business models associated to these digital health innovations to propose a typology of business models for digitalized health with a special attention granted to the financial impacts of each type (4).
2 Digital Innovations and Personalized Health Care
In line with patient-centred care, personalized medicine or mass customization in health institutions (Minvielle et al. 2014), some digital start-ups promise you to become manager of your health. This proposes to the patient to play the role of a general practitioner (GP) at home.
Ignilife is a Luxembourger start-up implicated in connected “health coaching”. They propose digital solutions to coach people all day long to promote a healthy life. The software available on digital multi-support gives the opportunity to identify the patient’s risk factors, for him/her to receive alarm for recommended exams or to follow a personalized program in nutrition, backache, sleep disorder, tobacco or stress. The company pretends to “help people become actors of their health”. “Get your health under control” is its disclosed target. Digital software provides advices to the customer with a personalized information link to his/her needs. Ignilife grants special attention to prevention by safe living practices and healthy behaviours in accordance to the patient’s risk factors. The underlying logic is that such a behaviour will reduce the demand for both cure and care, along with the number of unworked days leading to significant savings and positive returns on investment at the global level.
The digital service includes three phases. First, the evaluation phase identifies the healthy profile for the patient in a holistic approach with a dynamic and interactive questionnaire trying to define his/her risks at present and in the future. At the end of this stage, the patient receives a personal health score with a detailed report that he/she should share with his/her relatives and GP. The software programme processes the answers given by the patient through the questionnaire to suggest targets and prioritize actions to improve his/her experience with Ignilife. Second is the definition of a personalized rhythm and program taking into account all the aspects of the health profile of the customer/patient. It reviews four mains domains: clinical risks, nutrition, physical activity and emotional health. As a target, the patient can choose to lose weight, control stress, eat healthy or improve sleep, and the digital application guides him/her, day after day, with simple and small actions that trigger significant and lasting change at last. The commercial flyer argues that motivation is maintained by defining well-calibrated targets, that is, not too easy to reach but still reachable, daily implication and progressive learning. The role of small wins in the progression is underlined and the promise of easy activities to follow the program is put forward. Third, an evaluation is made with a visual and interactive scorecard to assess the progression. Each progress is rewarded to keep patient’s motivation high. This leads the patient to receive gratifications like free products, or commercial services on health and welfare.… Ignilife provides to the patient’s digital environment the possibility to directly collect data from connected objects, to store all Electronic Health Records in a unique personal database that can be shared with clearly identified persons for free. Messages alert him/her in case of deviant behaviours. Ignilife also propose to connect patients with similar conditions by a social network called Ignilife users.
Visiomed Group is one of Ignilife’s competitors. It is a small enterprise that develops “BewellConnect”, that is, a product that provides a personal health assistant service. It has also launched several health-oriented innovations developed on smart and connected objects. Visiomed Group’s expertise in reliable and precise medical connected measurement tools has led to propose a new concept targeting patients suffering from chronic diseases (diabetes, hypertension, cardiac pathologies, asthma…), pregnant women, seniors, people living in remote areas with problems of access to medical resources, travellers and hypochondriacs who wish to be reassured 24 hours a day and 7 days a week. As an innovation leader the group promises to enable its clients to monitor their health in an autonomous way by empowering them to make a diagnosis, thanks to the distant support provided by medical doctors and allied professionals.
This group has a physiological approach trying to collect data through connected objects. The data is contextualized, precise, reliable and secure. It is useful to assess the severity of a series of signs and enables to guide medical interpretation. From this background, the company has launched a range of services with a choice between three levels. At the first level, BewellCheck-up collects a set of data about the patient’s body including medical data (measure of temperature, blood pressure, pulse, saturation in oxygen, glycaemia, heart rhythm), localization of the pain, an assessment of the patient’s risks by asking the right questions to define his/her symptoms (fever, headache), taking into account his/her profile and histories (diabetes, high blood pressure, cardiac insufficiency) and geographical situation in terms of offers of care around him/her (remote place, duration of transport to get access to a doctor) and give a first diagnosis (list the most likely causes of your ill-being or pain) with an estimation of the medical emergency degree and guide him/her in the health system. The software guides the patient with ergonomic and intuitive approach, slightly the same situation as if the patient faced a physician in emergency conditions. In a few minutes, it can review the most likely roots of the patient’s problem. The service is supported by a revolutionary artificial intelligence system that supports medical decision developed with the help of a team of emergency physicians. The software allows sending a report with the patient’s data, answers, histories, to his/her regular medical doctor and proposes to the patient to get in touch with a medical advising platform reachable by phone 24 hours a day and 7 days a week via MyDoc. This advising phone platform is operated by physicians and offers a full time access from several points of the app on a smartphone. This enables the patient to directly get in touch with a regulating doctor of the medical platform on the phone, who assesses the situation, recommends the patient, guides him/her to an emergency service or sends assistance to him/her (ambulance, emergency medical service). This service is fully accessible in France and from foreign countries. The medical team is based in France and answers in French. The extra service combines the two offers in one BewellCheck-up plus MyDoc called BewellConnect.
The set of services is channelled through a mobile application on a smartphone/tablet/computer with a payment that depends on both the uses and how frequently the provider is called. As an example, Visiomed proposes nine packs of services with two dimensions: the nature of the service (BewellCheck-up or MyDoc or BewellConnect the both) and the intensity of uses (free usages called “Discover”, with commitment of 12 months called “Privilege”, and with commitment of 24 months called “Serenity”). For an aged chronicle patient with cardiac pathology and hypertension who accepts a commitment of 24 months, he/she has to pay 31.90 € a month to access with no time limitation restricting the access to the whole digital environment (follow-up and medical advices by phone). Digital connected objects have to be added to the registration fee: a thermometer (99 €), a tensiometer (109 €) and ECG (349 €), easily amounting to 557 €. The patient can test the service before committing him/herself. Going for intensive use, that corresponds to 3 calls per month and full usage of surveillance medical, requires a monthly increase of 69.7 €, that is, 836.4 € per year.
These two examples show that digital devices take part to the emergence of a new relationship between the patient and his/her health. He/she will become the self-organizer of his/her health condition helped by medical professionals depending on the severity of his/her illness. The company highlights the potential of digitalization to redesign care in a more connected way with the patient as proposed by Porter and Olmsted Teisberg (2006, p. 167 and following) in care cycles.
3 Digital Innovations and Community-Based Patients Health-Care Providers
Another start-up in Monaco called IMSPro provides an interesting model coordinating by a software solution named “Askamon” the various health professionals around a group of patients. Askamon solution allows, they argue, to centralize, consult and enrich medical data for a better follow-up and rationalization of health costs. Based on community work in predefined environments it centralizes and allows exchanges of medical information between health professionals. So, every professional selects the information that he/she needs, whenever his/her status: medical doctor, physiotherapist and paramedic. This sharing of information allows to improve significantly care coordination and to optimize the coverage and the patient’s follow-up. Askamon simply and exhaustively meets all users’ needs, they argue. Built on intuitiveness, clarity and simplicity of uses, it is user-friendly whatever the level of the user at using computers. This is a tool induced from the ground field that evolves with daily practice. It is reachable by all electronic devices and software environment.
Firstly developed for the high-level sport world, the start-up now targets companies, health industries, insurers, health institutions and primary care centres. The company provides a personal health record (PHR) that is only used under the agreement of the patient condition, and the agreement shall be given for each caregiver. The system compiles consultations, prescriptions, pathologies, medical histories and reports on the same electronic record. It gives the opportunity to edit all administrative documents, to establish assessments of general health status of patients at any time and finally it contributes to the care organization management. In case of statutory medical follow-up, the software plans, organizes, controls and reports at any time on medical obligations. This part is especially relevant for the firm with a medical department, in the context of dangerous activities, for expatriated staff or for all medical statutory follow-up contexts. The patient has a complete access and a full management of his PHR. He/she can add information, discuss with physicians and find oriented advices on sport activity, nutrition, well-being via multimedia supports.
From the database built on a specific group, with the standardization and in the respect of the legacy, the PHR allows epidemiologic studies to evaluate treatment and therapy or prevent diseases or wounds accidentally.
It also makes it possible to interface Askamon with medical digital equipment or administrative systems. For example, the billing system of the National Health System can be reached; some medical connected devices can also carry out medical tests on the person.
The last step is a performance management tool, which is of special interest to the clients, that is, the health-care providers who would like to manage their group of patients with a same pathology on the long term, or who have to deal with a large population as the pension funds, or mutual insurance companies. The software allows relevant tools for medical prevention, used by companies to improve human resource management and hence global performance.
IMSPro would like to implement this software solution with an unlimited access 24 hours a day and 7 days a week. This could ideally be done with full access for the final user from as many digital devices as required. The data storage is also unlimited. IMSPro proposes a global solution covering all medical needs of the client company employees connecting them to all required health professionals.
We can notice, at this stage, that Askamon solution first targeted clients with strongly homogeneous beneficiaries’ medical profiles, for example high-level sports organizations, and the company has now diversified its market mix with by company clients who have more disparate medical profiles, with insurance companies. At last, this case represents an interesting mix of individual and organizational approach focusing a specific community. It should be viewed as an original situation, in which political aspects are centred on the patient’s interests, decision-makers define general aims, and the organization of care is completely carried out by/with health professionals. Such an experience could well be considered as a bottom-up approach laboratory. If IMSPro has clearly identified clients dealing with a defined community of care, it is not the case of all start-ups, which propose to take care of a patient community.
Other start-ups target the providers of services at home rather than the patient and his/her family carers. It is the case of DVSanté, which is a silver economy start-up in Nice. It proposes a dematerialized global platform dedicated to better meet the needs of persons suffering of loss of autonomy, who live at home (Bottero 2016). This is achieved by a group of partners having a relevant expertise in various domains related to the needs of the person. The existing institutions in charge of home care waste much time in coordination by phone. Thanks to the professional platform, DVSanté uses a user-friendly and rapid tool, which allows the care coordinators and the actors to gain in efficiency and in productivity. It is the first private platform for health-care professionals that is accessible for free. It allows in a few clicks to organize for the patient to remain at home by putting him/her in contact with the health professionals who can bring the most complete answers to his/her needs. This includes nurses, physiotherapists, speech therapists, chiropodists, health aid and helping staff at home. It also required medical equipment, leading to adapt accommodation, transport, general services, catering, assistance, leisure activities, holidays, and putting in touch with relevant specialized structures (day care hospital, care services at home, nursing home…). This young start-up claims to make the current system of care more fluid in organizing continuous care to the patients from hospital to home, including the intermediate structures (long-term care, convalescent homes, nursing homes…). This is reached thanks to an effective coordination between the various stakeholders. What is at stake is to fully cover all patients’ needs at home. This is carried out by tracing health professionals’ contributions to a patient real time. This saves critical time, it is argued. The business is presented as a solution intermediating patients and medical professionals: searching for and connecting allied health professionals and home service providers with a guarantee of quality, follow-ups through several tools (a quality charter, an app for home services and an interface hospital/home). Resorting to specialized partners they also offer organizational consultancy (pharmaceutical or logistics platform, operating room organization, patient flow) and app development services. According to the start-up CEO, the digital devices proposed allow to reduce the patient’s hospital length of stay while guaranteeing a better communication between the hospital and home professionals, by bringing comfort and safety. Those solutions give the opportunity to the caregivers at home to become relevant intermediaries between the service providers generally unknown by the patient and their future customers. The company provides a unique digital service of intermediation and sharing of medical data within a territory. The large majority of health institutions buy this services offer as some big health institutions like teaching hospitals or cancer institutes. Not surprisingly, health professionals like the digital services designed by DVSanté because they improve coordination between themselves. This issue of coordination is indeed critical when the patient lives at home. The territorial aspect is more acute in this business, which is not completely stabilized yet. DVSanté tools are completely free of charge for health professionals, that is, nursing consultants at home, and give them the opportunity to put in contact their patients with home service providers. These providers have to give back a percentage of the revenues that they generate through the platform. Another source of revenues comes from hospitals. The software hence enables to optimize the part of the care path, which is outside the hospital, and this generates subsequent savings in term of internal organization and length of stay at the benefit of the hospital. According to DVSanté CEO (Sierra 2016), the return on investment for the hospital of the annual fees to DVSanté is around four months. He declares to prospect mutual insurance companies with an interest for covering the risk of hospitalization of their beneficiaries.
This second type of digital health innovation is striking because it was originally designed to help caregivers to deal with the needs of a patient at home. These patients may be less medically homogeneous than sport champions, and the contribution of the innovator moves step by step towards a service of intermediation of health professionals for a population on a defined territory.
4 Digital Innovations and Territorial Performance Management of Health-Care Delivery
IMS Health should be qualified as an “international digital company”. Founded in 1954, it is the leading global information and technology services company (operating in more than 100 countries) providing more than 5,000 clients in the health-care industry with tailored solutions to measure and improve performance. It employs around 7,000 experts in data management and saves on cloud platform huge volume of information from health systems. They consider themselves as the Unique Foundation for Driving Healthcare Performance operating at the heart of what is shaping the future of health care: information and technology services. They connect their assets and expertise across all questions raised by their clients. The company collects big data in health, develops strong expertise on data mining to exploit information and identifies ways to improve their offer.
To make clear how big the business is, here are some examples. More than 500 pharmaceutical wholesalers and distributors report on their shipment of products to every distribution channel—including hospitals, clinics, retail and mail-order pharmacies, pharmaceutical chains, mass merchandisers and food stores. Health plans principally in North America send anonymous medical claims data for a record of patient care. Tens of thousands of pharmacies send information on the prescriptions from US Government, Medicare and Medicaid databases and the health records of military forces and their families. Physicians report on consultations worldwide on Electronic Medical Reports (EMR) that include diagnoses, patient types and therapies. Thousands of hospitals report on the products they purchase, the treatment and discharge records worldwide. Laboratory and imaging companies report on their results like medical imaging. Data also come from a panel of healthcare stakeholder groups, including physicians, worldwide who regularly participate in quantitative and qualitative research studies. Thanks to a mix of automation and human intelligence IMS Health tries to collect structured and unstructured social media data related to drugs, treatments and health-care companies, while respecting patient privacy. The company also exploits its cloud-based listening platform; customers can hence gain insights from the Web real time. The company works also with patient anonymous information with specific conditions or those receiving a particular treatment about their quality of life, reasons for treatment changes, structured measures of disease severity and treatment and care information. Promotional expenditures for individual products are assessed, with both qualitative and quantitative feedback on all the commercial activity. IMS Health has also invested in Genomic sequence data for the opportunities it gives to improve health, patient by patient. The company collects data on the sales of ethical pharmaceutical products, capturing more than 95% of the value of the global market. The company conducts qualitative research with physicians, dentists, pharmacists, nurses, payers and patients by face-to-face interviews, focus groups and questionnaires trying to understand attitudes, motivations and intentions. All these data are useful for a Global Customer Base—including government agencies, payers, providers and nearly every major pharmaceutical and biotech company worldwide—to rely on the information collected, services and technologies to guide strategic and tactical planning and drive more effective marketplace interactions. All these customers are segmented as follows: consumer health, medical device and diagnostics, pharmaceutical manufacturers, specialty/oncology, generics manufacturers, payer/provider/government and pharmacies and wholesalers.
But even if this health big brother seems to be on track, few elements show some failures and points out some avenues for improvement. The company recognizes that “available information is very fragmented and difficult to bring together in a meaningful way”. What is required is to have “partnering with high-value physicians, engaging proactively with physicians and populations and acquiring clearer insights into care dynamics.” This shows that information needs to be more focused on care processes or on a clearly identified health condition. Also, the company has many expectations in what is called “Real-World” Evidence (RWE) or Data (RWD) and proposes to create a specific RWE ecosystem with its customers focused on anonymous patient-level data. Moreover, the so-called Better Together by Design proposes to move “from big data by collectively leveraging our best-in-breed capabilities”. This shows that the complexity of health, even if digital information is centralized in Big Data, needs to be addressed by a large, collective and engaged group of actors suggesting the value of empowering the actors.
Another fascinating experience is of HealthPartners (Isham George et al. 2013). HealthPartners is a Minnesota-based, consumer-governed, non-profit organization, founded in the 1950s. It provides health insurance through a large integrated system (from prevention to hospitals, five at least, more than 75 medical and dental clinics, and a network of contracted providers). HealthPartners’ mission is to “improve the health of our members, our patients and the community.” In 2010, the leaders heard a presentation from the University of Wisconsin for the Robert Wood Johnson Foundation’s County Health Rankings program. The result was: “contribute to health outcomes, the model estimates that clinical care contributes 20 percent, health behaviours contribute 30 percent, social and economic factors 40 percent, and the physical environment 10 percent. In other words, the three nonclinical care factors are responsible for an estimated 80 percent of health outcomes” (Isham George et al. 2013, pp. 1446–1447). It was hence decided to implement what is called a “community business model—a type of multisectoral partnership that involves actors that are seldom accustomed to work together and not always aware of how their actions affect population health” (Isham George et al. 2013, p. 1447). To do so, the company strategy integrated aims and performance measurement system “secondary” influence on health outcomes, such as health behaviours, social and economic factors and the physical environment. To better understand how this partnership works, the example of “yumPower School Challenge” can help. A number of school districts and a children’s media outlet, Radio Disney became partners of the challenge. The challenge of each participating school was one part of the “healthy eating” campaign. It included advertising, cooking classes and a website with expert advices and resources. The main purpose was “the promotion of the consumption of five fruits and vegetables a day for people of all ages”. Schools volunteered to compete for cash prizes that could be used to promote health and well-being. The whole budget invested by HealthPartners was around $300,000 after integrating creative components of the campaign, staff time to support schools, and evaluation services. This action was tightly accompanied by HealthPartners leaders even if it was not the case of twenty others initiatives, in which HealthPartners was involved.
Even if digital devices are not the main purpose of this kind of collective partnership, we understand how digital solutions play a central role in terms of communication, evaluation and following-up for each school. Another point that deserves attention is the notion of community in that example: as HealthPartners is a Minnesota-based organization which deals with a huge objective towards the population of this territory, which is to improve health of their members, that is, patients and beyond all people living in the geographic zone.
5 Towards a Business Model Typology for Digital Health
A series of models have been drawn from other sectors like e-commerce or disruptive innovations in general business companies to be applied to health care. We will first review these models and what can be learnt from then. We will then propose a new typology the distinctive feature of which is that it is drawn directly from digital health cases.
5.1 Reviewing Existing Typologies of Health Business Models
In 2000, the first typology of business models (BM) on health digitalization was proposed inspired by e-commerce (Parente 2000). Eight years later, a new typology of BM was designed borrowing from disruptive innovation theoretical frameworks applied to health delivery (Hwang and Christensen 2008). Several recent papers also address this issue (Davey et al. 2010; Kimble 2015).
Davey (2010, p. 24) puts that a “business model performs two important functions: it creates value and it captures a portion of that value”. According to Hwang and Christensen (2008, pp. 1331–1332) and Kimble (2015, pp.27–29), a business model should present four elements: (1) A value proposition or offer should provide a product or a service done more effectively, conveniently and affordably; (2) a set of resources that may bring together people, supplies, intellectual property, equipment, and cash; (3) a profit or finance formula compares prices, costs, mark-ups, margins, asset turns, and volumes necessary to profitability; (4) a client or a process, that is, the beneficiary of the offer or the process that would transform the health system on the long term.
Parente (2000, p. 94) highlights “Health e-commerce b-to-b models” based on Web sales directly to providers through online auction and services (consulting, strategy or performance measurement…). Several examples presented in the previous section (n° 2) seem to fall into this category. After deep analysis they tried to add (for IMS Health) or to design (for DVSanté) not only a digital business model but a basis aiming at enriching the answer brought to a series of health problems. For example, IMS Health collects information for businesses from their clients but it aims at getting a better understanding of the business model to propose to design with the client the relevant database for analysis and decision-making activities. The “b-to-c model” (Parente 2000, p. 95), which allows customers to purchase health products through Internet, also seems relevant to our cases. The author presents the case of Vivius, which gives the opportunity to build one’s own health plan. Interestingly yet he noticed that this service must be self-funded by the patient or partially financed by an employer contribution. This case is in between a person-based BM aligned with health individualization principles (e.g. Ignilife) and a community-based BM targeting company employees (IMSPro-Askamon).
Hwang and Christensen (2008, pp. 1332–1333) classify BM depending on three types of disruptive innovations: solution shops, value-adding process businesses and facilitated user networks. The “solution shop” can solve unstructured problems with skills and the talent of the people employed as distinctive features. Providing unique combination of services for each customer being their target. IMS Health illustrates the solution shop, as it sells digital information and digital treatment to its clients. As we previously saw, they yet try to move to a more global hand to hand business involving more and more stakeholders in the design of the database, in collecting data and also in the meaningful way to analyse information on a given health condition. This suggests that even if the project is to build a huge data warehouse on health, the need to develop a reflection on how to use it remains critical. “Value-adding process businesses” transform resources in greater value outputs. They generally focus on process excellence providing better quality services at lower cost. It seems to be the case for IMSPro and DVSanté, as far as quality is concerned, their costs being not lower. Services provided are new and increases the fees to be paid by end-users, raising the issues of equity and accessibility to this new health process. “User networks” is probably the most distinctive BM, as it describes situations where “same people buy and sell and deliver and receive things to and from each other”. Digital health is close to this type as each stakeholder must be involved in improving people’s health. HealthPartners is certainly the best illustration of this type of BM.
Jason and Christensen (2008) stress two limits that we consider as a call for proposing a complementary typology of Health Digitalization BM. The first limit refers to the lack of retail market. Authors argued that a disruptive innovation needs to meet a competitive market to increase sales and they denounce the third-party payer system in health that introduces an intermediation between clients and providers. Beyond this limit lies one of the most critical issues in health, leading to identify products and clients understood as the final users. Three levels can be listed, we argue: individual, community and population. The second limit is put as follows: “In health care, most technological enablers have failed to bring about lower costs, higher quality, and greater accessibility.”
5.2 Proposing a New Business Model Typology for Digital Health
In addition to these limits, a new typology for health digitalization is also required, we argue, because previous typologies were all built with no consideration given to the foremost health challenge: how can health digitalization address the most challenging financial issues faced by the health system? Three challenges should be tackled by health digitalization BM, we argue.
The first challenge lies at the individual level and relates to the need for organizing a well-coordinated care/life pathway for the patient or his/her caregiver. Beyond their social, political and economic dimensions’ health issues are personal matters. Hence there is a need for giving to the patient the opportunity to be actor of his/her health coordinating in efficient ways information, behaviours, incentives and social and environmental factors to not only organize acute episodes of care but also to prevent them and decrease risks. The financial model here is the payment individualized upon each final user/client. It puts light on associated questions of equity, accessibility and affordability of health services. Should digital health be considered as medical procedures financed by the National Health Service or is it simply a choice by the patient of better welfare?
The second challenge is situated at a community level, that is, a group of persons with homogeneous health needs. At this level and moving from individuals to the group, the health system should gain in efficiency and effectiveness by optimizing care processes, systemizing epidemiologic studies and associated advices and developing specific preventive actions for the community with homogenous health needs. Even if health is personal matter, its social dimension is obvious because one’s health impacts others and reciprocally. Digital technology offers us both to improve health and dramatically cut costs for standardized care processes through a co-responsibility of patients. This organization is very interesting to better understand how digital technologies could improve quality, efficiency, accessibility and affordability of health. In the case of IMSPro, the situation is unfortunately simplified by the fact that the payer is the employer of the beneficiaries of the digital health services. The question of the generalization of this community approach and the question of the diversity of the communities needs in a general population remain unanswered.
The third challenge is at the level of a territory population. The population includes several communities with different health needs. Social and non-medical health services are then required and need to be organized in an integrated way to get disruptive progresses. IMS Health clearly illustrates the challenge of information digitalization. Specifically, monopolistic positions observed in such contexts raise the issue of knowledge-sharing and information property. Preventive actions should integrate social and economic considerations, health behaviours factors and physical environment ones (County Health Rankings). This population level is completely linked to the smaller one. Health Partners and IMS Health experiences show the necessity of co-building, allowed by a contextual approach with a mutual respect of actors, to tackle these challenges.
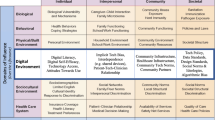
Finally, we can summarize this by crossing the four elements of business models with the three focus levels to improve health with the help of the digital devices (see Table 4.1).
As shown by Table 4.1 most of the digital health innovations that we analysed fall either into individual or community focus types. Nevertheless, two of them are distinctive by their population focus with a business model reconciling finance and ethics.
6 Conclusion
Digital Health disrupts healthcare sector. By providing individualized care it contributes to raise quality of care and reduce the needs for cure. Nevertheless, the new services induced by the revolution may not be accessible to the largest number of people. We first review and characterized DH innovations depending of the level on which they focus. This leads to three types of DH innovations: individualized, community and population. We then propose a typology of business models grounded on this distinction crossed with the BM elements (offer/value, resources, finance/profit formula and clients/process). We identified one BM enabling to empower patient and to preserve access for the largest part of the population reconciling individual and general interests.
The intertwining of business models and ethical issues leads us to call for future work “(the) purpose (of which) is to nurture collective and dynamic re-ordering among actors in a conscious attempt to identify, work through and rethink the rights and responsibilities that are appropriate for supporting the intentions of those who produce and use information to deliver care” (Garrety et al. 2014, p. 75). Isham George et al. (2013, p. 1451) state the same point in a slightly different way: “national bodies such as the Institute of Medicine have called for more robust partnerships as well as a framework to ensure that different actors work together to produce better public health processes and outcomes.” Digital Health technology may support co-production experiments but the critical issue that it raises remains unchanged in an even acuter way: how can institutions provide the conditions favouring such developments to benefit to the large majority of people including the most fragile fringe. In such a search Ostrom’s work on commons (1990) could be usefully applied to health care as we argued previously (Angelé-Halgand and Garrot 2014).
Bibliography
Angelé-Halgand, Nathalie, and Thierry Garrot. “Les biens communs à l’hôpital: De la T2A à la tarification au cycle de soins” Comptabilité, Contrôle, Audit T20, V3 (2014): 15–41.
Angelé-Halgand, Nathalie and Thierry Garrot. “Discipliner par le chiffre: L’hôpital financiarisé au risque de la réification?” Entreprise Et Histoire 79 (2015): 41–58.
BewellConnect (2015). BewellConnect Santé. https://www.bewell-connect.com/fr/sante/. Accessed August 20, 2016.
Bottero, L., (2016). DV Santé se rapproche de Monali. Resource document. La Tribune Provence-Alpes-Côte d’Azur. http://marseille.latribune.fr/innovation/2016-03-03/dv-sante-se-rapproche-de-la-bordelaise-monali.html. Accessed August 20, 2016.
County Health Rankings (2016). Our Approach. Madison (WI): University of Wisconsin Population Health Institute. http://www.countyhealthrankings.org/our-approach. Accessed August 26, 2016.
Davey Shirley, M. et al. “The Health of Innovation: Why Open Business Models Can Benefit the Healthcare Sector” Irish Journal of Management 30, 1 (2010): 21–40.
DVSanté. DVSanté. http://www.dvsante.com. Accessed August 20, 2016.
Garrety, Karin et al., “National Electronic Health Records and the Digital Disruption of Moral Orders” Social Science & Medicine 101 (2014): 70–77.
Hunt, J., Rt. Hon (2013). Paperless NHS News Story Gov.UK. Resource document. Department of Health. https://www.gov.uk/government/news/paperless-nhs-jeremy-hunt-leads-discussion. Accessed August 25, 2016.
Hwang, Jason and Clayton M. Christensen “Disruptive Innovation in Health Care Delivery: A Framework For Business-Model Innovation” Health Affairs 27, 5 (2008): 1329–1335.
Ignilife (2014). Prenez le contrôle de votre santé. http://ignilife.com/#_=_. Accessed August 20, 2016.
IMS Health (2016a). Imshealth Market Insight. http://www.imshealth.com/en/solution-areas/healthcare-market-insights. Accessed August 18, 2016.
IMS Health (2016b). imshealth Real-World Evidence. http://www.imshealth.com/en/solution-areas/real-world-evidence. Accessed August 18, 2016.
IMSPro. Askamon. http://www.imspro.mc/index.php?option=com_content&view=article&id=54&Itemid=62&lang=fr. Accessed August 20, 2016.
IMSPro. Nos Solutions. http://www.imspro.mc/index.php?option=com_content&view=article&id=48&Itemid=55&lang=fr. Accessed August 20, 2016.
Isham, George J. et al., “HealthPartners Adopts Community Business Model to Deepen Focus on Nonclinical Factors of Health Outcomes” Health Affairs 32, 8 (2013): 1446–1452.
Kimble, Chris “Business Models for E-Health: Evidence from Ten Case Studies” Global Business & Organizational Excellence 34, 4 (2015): 18–30.
Minvielle, Etienne et al., “Managing Customization in Health Care: A Framework Derived from the Services Sector Literature” Health Policy 117 (2014): 216–227.
Ostrom, Elinor. Governing the Commons—The Evolution of Institutions for Collective Action. Cambridge, UK: Cambridge University Press, 1990.
Parente, Stephen T “Beyond the Hype: A Taxonomy of E-Health Business Models” Health Affairs 19, 6 (2000): 89–102.
Porter, Michael and Elizabeth Olmsted Teisberg. Redefining Health Care—Creating Value-Based Competition on Results. New York: Harvard Business School Press, 2006.
Sierra, E., (2016). DV Santé: Un Service Mobile Pour fluidifier le parcours de soins!. Resource Document. Métropole Nice Côte d’Azur. http://www.nicecotedazur.org/developpement-economique/la-maison-de-la-métropole-nca/actualités. Accessed August 19, 2016.
Visiomed GROUP SA (2015). Nos produits. http://visiomed-lab.com/Nos-produits_585.html. Accessed August 18, 2016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Copyright information
© 2017 The Author(s)
About this chapter
Cite this chapter
Garrot, T., Angelé-Halgand, N. (2017). Digital Health Business Models: Reconciling Individual Focus and Equity?. In: Menvielle, L., Audrain-Pontevia, AF., Menvielle, W. (eds) The Digitization of Healthcare. Palgrave Macmillan, London. https://doi.org/10.1057/978-1-349-95173-4_4
Download citation
DOI: https://doi.org/10.1057/978-1-349-95173-4_4
Published:
Publisher Name: Palgrave Macmillan, London
Print ISBN: 978-1-349-95172-7
Online ISBN: 978-1-349-95173-4
eBook Packages: Business and ManagementBusiness and Management (R0)