Abstract
Optimal healthcare policies require assessment of cancer risk at the individual level, especially for more common diseases like breast cancer. As outlined in a chapter titled “hereditary breast cancer and pathogenic germline variants” in this book, there are a complex array of environment and genetic risk factors with uncertain interactions between these. Therefore assessment of cancer risk must be approached and evaluated in a systematic and structured manner that is based on various risk assessment tools that have been developed, validated, and applied in the clinical setting [1–8].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Optimal healthcare policies require assessment of cancer risk at the individual level, especially for more common diseases like breast cancer. As outlined in a chapter titled “hereditary breast cancer and pathogenic germline variants” in this book, there are a complex array of environment and genetic risk factors with uncertain interactions between these. Therefore assessment of cancer risk must be approached and evaluated in a systematic and structured manner that is based on various risk assessment tools that have been developed, validated, and applied in the clinical setting [1,2,3,4,5,6,7,8].
Risk Assessment Tools (RATs)
The Breast Cancer Risk Assessment Tool (BCRAT) represents the most widely used RAT in routine clinical practice [1]. This model calculates a woman’s risk of developing invasive breast cancer over the next 5 years and up to age 90 years using minimal information relating to personal and reproductive history and the frequency of breast cancer among first-degree relatives. This tool has been validated among different racial groups in the United States including women of white, black/African American, Hispanic Asian, and Pacific Islander ethnicity [4, 5, 7, 8]. The Tyrer-Cuzick (TC) International Breast Cancer Intervention Study model (IBIS) risk assessment tool was developed among cohorts of women in the UK, but is used worldwide for evaluation of breast cancer risk [9,10,11,12,13,14]. Currently, the v8.0 (IBIS) assessment tool calculates an individual’s 10-year risk, lifetime risk, and likelihood of carrying BRCA1/BRCA2 pathogenic gene variants (PGVs). Genetic counseling is advised if the predicted chance of a woman carrying a mutation in BRCA1 or BRCA2 PGV or both is 10% or greater. The Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA)/CanRisk Tool is a comprehensive platform that can be used to accurately estimate individual risk of developing breast or ovarian cancer and incorporates personal details, lifestyle factors such as alcohol consumption, reproductive factors such as the age of first menarche, menopause, contraceptive pill usage and hormone replacement therapy history together with family history, breast cancer screening history, and mammographic density [15,16,17]. In addition to these environmental factors, PGVs for hereditary breast cancer along with polygenic risk scores (PRS) for both breast and ovarian cancer can be included. This tool provides risk estimates for the next 5 and 10 year periods as well as remaining lifetime risk up to the age of 80 years. It can also calculate the likelihood of carrying mutations in moderate to high-risk genes (namely BRCA1, BRCA2, PALB2, ATM, CHEK2, BARD1, RAD51C, and RAD51D). The risk assessment tool is readily available for clinical usage for populations in the UK, United States, Canada, and Australia. However, some other countries, including Asian ones, have started using the tool with appropriate calibrations. The Breast Cancer Surveillance Consortium (BCSC) model is another tool that has been widely used for calculation of breast cancer risk [18,19,20]. Information required by these various tools to calculate breast cancer risk is summarized in Table 1.
These risk assessment tools (RATs) are used for decisions on screening strategies at the individual level [21,22,23,24,25,26] and can also provide data for exploring the indications for chemoprevention with agents such as selective estrogen modulators (SERMs) and aromatase inhibitors. Current guidelines include these RATs in their screening algorithms and recommend more widespread use of chemoprevention within the at-risk population [21, 22]. It is also possible to employ these methods to calculate breast cancer risk for the purpose of coordinating screening activity within clinical trials [24, 25]. Screening programs can be stratified based on age, breast cancer history, and RAT; age is closely related to breast cancer incidence and the risk of a false-negative screening mammography (MMG) relating to dense breast tissue. The level of individual risk calculated by RATs provides guidance on the most cost-effective screening schedule in addition to the most appropriate diagnostic modality where sensitivity is often age-dependent.
Nowadays, the population tends to be divided into three groups based on breast cancer risk: high risk (>20% lifetime), medium risk (15–20% lifetime; 1.67% to 2.49% 5 years), average (<15% lifetime, <1.66% 5 years). Testing for pathogenic variants in the high-risk genes BRCA1/2 is a pervasive trend in society and other PGVs such as PALB2, CHEK2, BARD1, ATM, BRIP1, RAD51C, and RAD51D can now also be tested for within a reasonable timeframe and cost. Many of these latter genes confer a lifetime risk of over 30% and are therefore classified as high-risk groups. On the other hand, those women with a lifetime risk of less than 10% can be classified as low-risk [21,22,23,24].
At the present time, RATS cannot be used to perform breast cancer risk assessment in conjunction with additional information on tumor proliferative characteristics, but polygenic risk scores (PRSs) may be used in the future to predict breast cancer risk. Potential application of PRSs for risk prediction is being evaluated in several studies, but these are highly dependent on local resources relating to costs, equipment, and manpower. Therefore, for average-risk women, current practice involves estimation of the number of cases of breast cancer that would be detected at each screening round and during the screening interval. These estimates are based on age and breast cancer risk and will guide recommendations for the “optimal” screening schedule. An important aspect of contemporary screening programmes is overdiagnosis and this is also factored into screening schedules that will involve multiple modalities including magnetic resonance imaging (MRI), mammography, and breast ultrasound examination [25, 26]. The role of the whole breast ultrasound in breast screening programmes remains controversial but may have a role in screening high risk women with dense breasts.
Validation of RATs
Risk assessment tools are used for a range of purposes, and robust processes for validation are an essential prerequisite to more widespread application within screened populations. The ratio of the observed number of breast cancers based on the model (O) to the expected number of breast cancers (E) is often used to assess model performance calibration (O/E ratio). The area under the receiver operating characteristic curve (AUC) is commonly used to assess the discriminatory accuracy of a particular tool. An AUC near 0.5 indicates relatively low discriminatory accuracy while an AUC closer to 1 reflects a high level of discriminatory accuracy [14, 27,28,29].
The Breast Cancer Prospective Family Study Cohort (ProF-SC) group validated four independent models of risk prediction (BCART, IBIS, BRACAPRO, and BOADICEA). The initial cohort involved almost 19,000 women age between 20 and 70 years, mainly from Australia and Canada, with the United States recruiting between 1992 and 2011. There was follow up available for 10-years on this observational data [14]. BOADICEA and IBIS were well calibrated in the overall cohort, whereas BRCAPRO and BCRAT tended to under-predict risk with O/E ratios as follows BOADICEA (1.05), IBIS (1.03), BRCAPRO (0.59), and BRCAT (0.79). The estimated AUC values for BOADICEA, IBIS, BRCAPRO, and BCRAT were 0.7, 0.71, 0.68, and 0.60, respectively. The authors conclude from these results that models involving multigenerational family history perform better at predicting breast cancer risk, even for those women with average- or below-average levels of risk. The Newton-Wellesley Mammography Cohort, BCRAT, BCSC, and BRCAPRO were considered to be well-calibrated models. However, IBIS slightly overestimated risk and this was most apparent when mammographic density was used (O/E 0.84) [28]. The corresponding AUC values were 0.64, 0.61, 0.64, and 0.62 for BCRAT, BRACAPRO, BCSC, and IBIS (v 8.0), respectively, with each model showing only moderate performance in terms of discriminatory accuracy. Nonetheless, Gail himself has stated that RATs with modest discriminatory accuracy could be helpful when counseling women and providing a general perspective on risk and making shared decisions on preventive interventions [27].
Nickson and colleagues have also confirmed impressive performance of the BCRAT tool for breast cancer risk prediction among a cohort of more than 40,000 women aged 50–69 years within the Australian breast screening programme. They reported excellent agreement across a broad range of decile groups for Gail scores, albeit with an element of over-estimation in the top decile group and an AUC of 0.59 [30].
Calibrations for the Asian American population have been undertaken in the BCART system. Approximately 20 studies have reported performance of BCART among Asian groups, but variable study outcomes are reported [31]. Some studies have shown similar performance characteristics to validation studies in Europe and the United States but this is not a universal finding with only a proportion using the adjusted or modified system for the Asian population. The latter have differences in both the incidence and patterns of breast cancer as well as intrinsic risk factors and lifestyles compared with their Western counterparts [32]. Moreover, there is probably less heterogeneity of risk factors within Asian relative to Western populations. It is reasonable to conclude that the performance of BCRAT in Asian populations is promising, but there remains uncertainty about the accuracy of these particular risk assessment tools for this group of women.
Our group recently conducted a study to verify the prediction accuracy of the Tyrer-Cuzik model for carrying BRCA1/2 mutations in female Japanese breast cancer patients [33]. This revealed that the performance of the model was only moderately predictable and that further calibration is needed. It has been suggested that the type of cancer caused by PGVs in the BRCA1/2 genes may vary from one ethnic group to another and racial factors are also likely to influence the chance of developing a particular cancer. Recent epidemiological studies on PGVs have also highlighted the importance of race and ethnicity in any discussions on interpretation of the role of known pathogenic mutations [34,35,36,37,38]. Increasing amounts of data will be generated in the next few years from ongoing studies around the world that will provide a global perspective on this issue of racial differences in the phenotypic manifestations of PGVs.
Polygenic Risk Score in Breast Cancer Risk Assessment
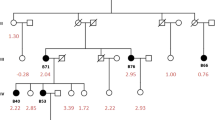
Multiple polygenic risk score panels have been investigated and tested in the clinical setting. Some of these studies have involved a direct comparison of polygenic risk scores with RATs while others have attempted to define whether polygenic risk scores add to the discriminatory accuracy of RATs [39,40,41]. One of the most validated polygenic risk scores for breast cancer is PRS313, which was found to have a positive association with breast cancer incidence in more than 20 clinical investigations. A large case-cohort study from the Breast Cancer Association Consortium analyzed PRS313 in combination with clinical breast cancer risk factors for women of European ancestry. This study reported that RS313 is a good risk discriminator for breast cancer, and the combined use of a polygenic risk score with details of family history and other risk factors provides better predictive performance (Fig. 1) [41]. Hence this predictive platform might be helpful for planning individualized breast cancer screening and strategies for chemoprevention. In a related study, Arthur and colleagues investigated the interaction between polygenic risk scores (304 of 313) and a healthy lifestyle index (HLI). The latter was developed using data from the UK Biobank and includes details of diet, physical activity, smoking, alcohol consumption, and BMI with assignment of scores in three groups [42]. There was a linear association between the PRS304 score and breast cancer risk for both pre- and postmenopausal women. Moreover, there was a significant reduction in estimated breast cancer risk attributed to a healthy lifestyle among premenopausal women who were otherwise in a high genetic risk group. For postmenopausal women, the reductions in risk associated with a favorable HLI likewise occurred across all polygenic risk score groups. These results indicate the importance of combined usage of polygenic risk scores with other tools for risk assessment that include lifestyle factors for more accurate prediction of breast cancer risk. Moreover, menopausal status modulates risk prediction with differences between pre- and postmenopausal women that may be independent of age. A recent report further suggested the possible emergence of ER-specific risk prediction models [43]. Another study from the Breast Cancer Association Consortium showed an independent predictive value for the polygenic risk score RS313 in terms of contralateral breast cancer risk [44]. There is now a trend for inclusion of polygenic risk scores into more recent risk assessment tools and indeed CanRisk includes PRS313 in their risk prediction platform.
Cumulative and 10-year absolute risk of developing breast cancer for (a) overall breast cancer, (b) ER-positive disease, and (c) ER-negative disease by percentiles of the 313 SNP polygenic risk scores (PRSs) [41]
As risk prediction is crucially dependent on ethnicity and lifestyles, polygenic risk scores need to be modified and adapted for each ethnic group [45]. Several approaches are being explored at the present time and include the use of polygenic risk scores alongside multigene panel tests for PGVs. These amalgamated tools potentially allow more precise prediction of the chance of developing breast and other cancer types among individuals carrying PGVs. This may also include prediction of tumor subtypes, which could assist with planning of screening schedules [46,47,48,49,50]. Likewise, various approaches are underway for evaluating the predictive value of polygenic risk scores not only for breast cancer risk estimation, but also other cancer types as well as lifestyle-related diseases and drug metabolism. These approaches might collectively lead to development of polygenic risk scores as a comprehensive platform for a broad range of individual risk assessments for both cancer and non-cancerous conditions [51, 52].
Tumor Growth and Early Detection
Tumor volume doubling time (TVDT) for breast cancer has been measured using serial mammograms and ultrasound. Factors such as high grade, high Ki-67 index, ER negativity, triple-negative subtype, and younger age are significantly correlated with shorter TVDT and related to rates of proliferation. For example, the average TVDT for a grade 3 cancer is approximately 150–170 days, while this figure is notably lower for grade 1 and 2 cancers (205–220 days) [53, 54]. Studies investigating TVDTs using preoperative measurements with ultrasound examination have shown dependence upon tumor receptor profile: ER positive/HER2 negative 185 days; ER positive/HER2 positive 165 days; ER negative/HER2 positive 85 days; triple-negative breast cancer (TNBC) 124 days [55]. Limitation of these studies includes relatively sample sizes and use of different measurement modalities, but there are some apparent trends. If the detection limit for a particular screening modality is 4–5 mm and a 2 cm size tumor is detected 2 years later during a subsequent screen, the estimated TVDT is calculated to be about 120 days. Comparing tumors of 5 mm and 2 cm in size, the associated rates of axillary lymph node metastasis are increased for the larger tumor.
Triple-negative breast cancers are relatively aggressive lesions, have increased risk of recurrence within 5 years, and are more likely to present as interval cancers within a screening programme. By contrast, luminal type cancers (A and B) are relatively slow-growing and are more likely to be detected by regular breast screening (every 2–3 years) in women with non-dense breasts. Moreover, these less-aggressive luminal cancers have a relatively constant annual risk of recurrence for up to 20 years [56]. Although the benefits of early cancer detection through screening remain controversial, there is a sound clinico-biological rationale supporting the premise that detection of tumors with a more aggressive phenotype at an earlier stage before micrometastatic dissemination to distant sites can improve breast cancer mortality. On the other hand, early detection is arguably less likely to improve the long-term prognosis of slow-growing cancers that do not form distant micrometastatic disease in the sojourn period between screen-detection and presentation symptomatically. Early detection of faster-growing cancers is complicated and in particular the screening interval has to be appropriate to minimize the numbers of interval cancers. In attempts to overcome this paradox, annual screening for women starting from age 40 years has been considered. At the same time, supplemental ultrasound or MRI might be employed for women with dense breasts to increase overall sensitivity of breast imaging. However, much controversy surrounds these supplemental imaging modalities from a screening perspective and in particular within a managed healthcare system where any screening programme has to be cost-effective. Interestingly, engagement of artificial intelligence for reading and interpretation of screening data is currently being tested (e.g., digital breast tomosynthesis) and may improve diagnostic accuracy as well as reducing harms of overdiagnosis and the workload burden for diagnosticians.
RATs and Clinical Trials
Modern prospective clinical trials are designed to incorporate multiple aspects and include not only a woman’s age and breast density, but also individual risk assessment based on RATS and polygenic risk scores [25, 57,58,59,60,61,62]. These trials have a variety of endpoints and aim to address breast cancer screening issues from a bidirectional approach that maximizes benefits and minimizes harms of screening for individual women. These trials are designed to compare a standard screening schedule in the observation arm with an intervention arm that involves a risk-stratified schedule with or without an option for a supplemental screening examination (for example, ultrasound for women with dense breasts). Many of these trials will incorporate RATs, and polygenic risk scores are also being included in more recent trials for optimal risk assessment. With a risk-stratified approach, higher risk women will tend to have more intensive screening programs while those women deemed to be at low- or average-risk will be considered for de-escalation with a less intense screening schedule. Therefore, accurate risk assessment is the key issues for a successful risk-stratified approach to breast screening.
In the Wisdom trial, women aged between 40 and 74 years are categorized into four groups based on level of risk as follows: (1) highest-risk, (2) elevated-risk, (3) average-risk, and (4) lowest-risk [57, 58]. The highest-risk group relates mainly to women carrying pathogenic mutations in high-risk predisposition genes (BRCA1/2, TP53, PTEN, STK11, CDH1, ATM, PALB2, or CHEK2). However, this group also contains women with an estimated 5-year risk of at least 5% or women with a history of mantle nodal irradiation for Hodgkin’s lymphoma. Annual screening with both mammography and MRI is recommended for high-risk group of women. Women at elevated but slightly lower risk include those aged 40–49 years with very dense breast tissue or with a 5-year risk of at least 1% based on susceptibility from single nucleotide polymorphisms (SNPs) in the top 2.5th percentile of risk by 1-year age category. Annual mammography only is recommended for this group. The average-risk group consists of women aged 50–70 years or women aged 40–49 years with a 5-year risk of less than 1.3%. Biennial mammography is recommended for these average-risk women. The lowest-risk group includes women aged 40–49 years with a 5-year estimated risk for developing breast cancer of less than 1.3%. These low-risk women do not require any form of screening until they reach the age of 50 years. The expected annual hazard for mammographically detected breast cancer for low-risk, average-risk, elevated-risk, and high-risk is 0.0198, 0.0414, 0.0774, and 0.2808, respectively. The median time from mammography to clinically detectable cancer is expected to be 18 months. Primary endpoints within the Wisdom Trial are the proportion of breast cancers diagnosed with Stage IIB disease or higher and the rate of breast biopsy (needle or open) over a 5 year period. Secondary outcome measures are multiple and include (1) the interval cancer rate, (2) number of women requiring systemic therapy, (3) mammography recall rate, (4) rate of detection of in situ carcinoma, (5) chemoprevention uptake rate, (6) choice of risk-based versus an annual screening in a self-assigned cohort, (7) adherence to assigned screening schedule, (8) breast cancer anxiety measured by the patient-reported outcomes measurement information system (PROMIS) anxiety scale, (9) decisional regret and finally, (10) ultra-low-risk cancer rate (time frame 5 years).
My Personalized Breast Screening (MyPeBS) is another multi-cohort randomized prospective clinical trial that includes 85,000 women aged between 40 and 74 years of age and has a risk-stratified approach in the experimental arm [25, 60]. Estimates of risk are based on age, family history, previous history of benign breast biopsy, personal hormone and reproductive history, breast mammographic density, and polygenic risk score. Risk assessment was undertaken using Mammorisk™ for those women with at most one first-degree relative with breast or ovarian cancer and the Tyrer-Cuzik risk score for those women with more than one first-line first-degree relative with breast or ovarian cancer. The trial population is divided into 4 groups according to the 5-year risk for development of invasive breast cancer; low-risk <1%, average-risk 1–1.66%, high-risk 1.67–6%, and very high-risk ≥6%. For low-risk women, just an end-of-study screening mammogram is carried out while for average-risk mammography is recommended every 2 years. Annual MMG screening is undertaken for high- or very high-risk women. Supplemental imaging with ultrasound is recommended for average-risk or high-risk women with especially high breast density and for very high-risk women annual MRI is recommended until age 60 years. A preliminary report from this study was presented at the European Society of Medical Oncology conference in 2022. The proportion of risk-stratified patients in low-, average-, high-, and very high-risk groups were 36%, 29%, 34%, and 1.2%, respectively [60]. The primary endpoint of the MyPeBS study is the incidence rate of stage 2 breast cancer with a non-inferiority analysis over a time frame of 4 years.
The BREAst screening Tailored for HEr (BREATHE) trial aims to assess the acceptability of a comprehensive risk-based individualized breast screening program in Singapore. This study integrates genetic and non-genetic breast cancer risk prediction tools that include BCRAT, mammographic density, BOADICEA, and polygenic risk scores [62].
Blood Tests and Multi-Cancer Early Detection
Amidst the ongoing debate on the relative merits or otherwise of breast cancer screening based on conventional imaging modalities, there is increasing interest in use of blood tests as a method for screening for cancer and other diseases. Blood tests may permit more accurate screening with detection at an earlier stage with less expenditure on equipment and personnel. Imaged-based screening for breast cancer not only incurs a high-cost burden, but can generate anxiety from false positive events and other stress-related side effects. Over the past decade, multiple studies have established the value of circulating tumor and/or cell-free DNA (ctDNA/cfDNA)—liquid biopsies—in primary cancer diagnosis, detection of relapse, assessment of treatment response, and development of disease resistance [63,64,65,66,67]. New age blood tests have been developed to screen for multiple cancers early on in otherwise healthy individuals with a family history of cancer. They have particular relevance to those cancers for which there is no other screening methods readily available. These multi-cancer early detection (MCED) tests use a liquid biopsy to detect multiple cancers, which otherwise might go undetected. Early detection can provide patients with better treatment alternatives, responses to therapy and may ultimately improve rates of survival. An estimation of the impact of MCED screening in the United States and UK concluded that inclusion of a MCED blood test can potentially benefit and complement existing screening tools by further reducing false positive results [68].
Two MCED tests have generated much promise for early cancer screening potential in the past 5 years. CancerSEEK was developed in 2018 and is based on mutations in 16 genes and eight proteins. This MCED can detect eight different cancer types (including breast cancer) from blood samples yielding ctDNA and/or cfDNA [69]. This test demonstrated 70% sensitivity for detection of cancers in non-metastatic patients. Five of the eight cancer types investigated in this study have no other methods of clinical screening for early cancer detection. A more recent test (the Galleri) was evaluated in a case-control study involving patients with stages I, II, II, and IV disease and showed sensitivity of 39%, 69%, 83%, and 92%, respectively, among 12 known cancers. There was specificity greater than 99% and an extremely low false positive rate [70]. Targeted methylation analysis of cfDNA provided information on the origin of cancerous tissue with greater than 90% accuracy, which could assist in precision oncology. In a validation case-control study, the authors reported 99.5% specificity in detecting cancer and demonstrated improved sensitivity of the test with cancer stage [71]. Both these tests reveal improved cancer detection rates and confirm the clinical utility of MCED screening tests and their potential impact on cancer-related mortality rates. Following the initial CancerSEEK findings, an interventional study evaluated the practical use and safety of CancerSEEK with positron emission tomography-computed tomography (PET-CT) imaging in about 10,000 women with no prior cancers [72]. An initial positive MCED test resulted in patients being further assessed with PET-CT for localized cancer screening.
MCEDs and Clinical Trials
MCED tests provide an alternative to traditional breast screening approaches driven by imaging technologies. In both healthy individuals and subjects with cancer family history, an initial MCED test can establish the cancer type, which is then followed by more localized screening and precision treatment. This permits improved quality-of-life and standard of care. Although the sensitivity of MCED tests is low compared to single/specific cancer tests, this is mainly based on their overall performance and incidence in cohort-based studies. The search for clinical trials using the term “multi-cancer early detection tests” on 3 May 2022 resulted in 14 studies across different cancers and regions [73]. These studies assessed the use of MCED tests as potential biomarkers, implementation in standard care, and early screening among pan-cancer patients and asymptomatic populations. Three prospective studies aim to evaluate the use of the Galleri test in different cohorts; STRIVE (NCT03085888, approximately 100,000 women aged 18 years and over undergoing screening mammography [UK cohort]), SUMMIT (NCT03934866, 25,000 women, 55–77 years of age, high-risk for lung cancer [UK cohort]), PATHFINDER2 (NCT05155605, 20,000 individuals aged 50 years or older [US cohort]). REFLECTION (NCT05205967, 35,000 participants) is an observational study to test the feasibility of the Galleri test in clinical settings and its overall impact on both patients and healthcare providers. Recent interim findings from the PATHFINDER (NCT04241796) study supported the readiness of the Galleri MCED test in clinical settings to predict cancer signal origins (CSO) with high accuracy [74]. A few other prospective clinical trials in Chinese cohorts (NCT04820868, NCT04822792, NCT04835675, NCT04903665, NCT04972201, and NCT05227534) evaluate the use of MCEDs by analyzing cfDNA mutations, cfDNA methylations, and microRNA (miRNA) expression for early cancer detection in subjects with and without cancers (Table 2).
With increased focus on large and inclusive cohort studies across ethnicities and countries, consortia with real-world data sharing could offer an excellent opportunity to cover the randomized clinical trial limitations. MCED tests include pan-cancer analysis, and such consortia can also assess any impact on cancer-specific mortality. Hence, MCED tests can complement conventional screening methods such as mammography for early breast cancer detection and are likely to become more precise and presumably cost-effective.
Multidirectional approaches are necessary to improve on current methods for breast cancer screening with a fundamental requirement for more precise prediction of breast cancer risk. Risk predictions need to be adjusted or modified for different ethnic groups due to varying patterns in the magnitude of risks with a heterogeneous landscape. These risks include genetic and epigenetic factors, overall and age-specific breast cancer incidence. Secondly, MCEDs should be included in screening scheme, not only for detection of breast but also other primary malignancies. Third, we need more diagnostic tools and optimal screening schedules are essential to identify very early-stage cancers. Furthermore, in terms of endpoints, breast cancer-specific modality may be the most appropriate endpoint. Nonetheless, ongoing trials have chosen the proportion of advanced breast cancers as the most suitable endpoint. The proportion of early-stage breast cancers such as node-negative tumors less than 1 cm may also be meaningful in this context and has a very favorable prognosis without the need for intensive systemic therapy. Finally, artificial intelligence (AI) offers the opportunity to potentially enhance accuracy and quantitative assessment of breast composition to improve diagnostic interpretation and keep false positives and false negatives to a minimum in breast cancer screening programs [75, 76]. Recent studies have shown that AI enabled radiomics increases predictive power for both breast cancer risk and tumor subtype [77]. At the same time, liquid biopsy results are being integrated into these risk assessment platforms which can also take account of racial and ethnic specific data to facilitate global application of these advanced risk assessment tools. This will aid collection of real-world data on a large scale to yield clinically meaningful results.
Conclusion
Risk assessment tools have been widely incorporated into breast screening programs, and several of these RATs allow inclusion of polygenic risk scores to refine risk estimation. MCED blood tests are being intensively investigated in ongoing clinical trials and may ultimately replace more conventional screening methodologies. Artificial intelligence offers promise in the screening setting and may allow more accurate risk prediction especially when used to facilitate radiomics. Improved predictive capacity from these newer technologies will underpin risk-stratified approaches to screening with escalation of schedules for high-risk individuals and reduced intensity of interventions for those deemed to be at low risk for development of breast cancer.
Abbreviations
- AI:
-
Artificial intelligence
- AUC:
-
Area under the receiver operating characteristic curve
- BCRAT:
-
Breast Cancer Risk Assessment Tool
- BCSC:
-
Breast Cancer Surveillance Consortium
- BOADICEA:
-
Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm
- BREATHE:
-
BREAst screening Tailored for HEr
- cfDNA:
-
Circulating cell-free DNA
- ctDNA:
-
Circulating tumor DNA
- HLI:
-
Healthy lifestyle index
- IBIS:
-
International Breast Cancer Intervention Study
- MCEDs:
-
Multi-cancer early detection tests
- MMG:
-
Mammography
- MRI:
-
Magnetic resonance imaging
- MyPeBS:
-
My Personalized Breast Screening
- PET-CT:
-
Positron emission tomography-computed tomography
- PGVs:
-
Pathogenic gene variants
- ProF-SC:
-
Prospective Family Study Cohort
- PROMIS:
-
Patient-reported outcomes measurement information system
- PRS:
-
Polygenic risk scores
- RATs:
-
Risk assessment tools
- SERMs:
-
Selective estrogen modulators
- TC:
-
Tyrer-Cuzick
- TVDT:
-
Tumor volume doubling time
References
National Cancer Institute. The breast cancer risk assessment tool. https://bcrisktool.cancer.gov/.
Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81(24):1879–86.
Gail MH, Pfeiffer RM. Breast cancer risk model requirements for counseling, prevention, and screening. J Natl Cancer Inst. 2018;110(9):994–1002.
Schonberg MA, Li VW, Eliassen AH, et al. Performance of the breast cancer risk assessment tool among women age 75 years and older. J Natl Cancer Inst. 2015;108(3):djv348.
Pankratz VS, Degnim AC, Frank RD, et al. Model for individualized prediction of breast cancer risk after a benign breast biopsy. J Clin Oncol. 2015;33(8):923–9.
Carver T, Hartley S, Lee A, Cunningham AP, et al. CanRisk tool-a web Interface for the prediction of breast and ovarian cancer risk and the likelihood of carrying genetic pathogenic variants. Cancer Epidemiol Biomark Prev. 2021;30(3):469–73.
Gail MH, Costantino JP, Pee D, et al. Projecting individualized absolute invasive breast cancer risk in African American women. J Natl Cancer Inst. 2007;99(23):1782–92. Erratum in: J Natl Cancer Inst. 2008;100(15):1118. Erratum in: J Natl Cancer Inst. 2008;100(5):373.
Gail MH, Costantino JP, Bryant J, et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J Natl Cancer Inst. 1999;91(21):1829–46. Erratum in: J Natl Cancer Inst. 2000;92(3):275.
IBIS. IBIS risk assessment tool. https://ibis.ikonopedia.com/.
Cuzick J, International Breast Cancer Intervention Study. A brief review of the international breast cancer intervention Study (IBIS), the other current breast cancer prevention trials, and proposals for future trials. Ann N Y Acad Sci. 2001;949:123–33.
Cuzick J, Forbes J, Edwards R, et al. First results from the international breast cancer intervention Study (IBIS-I): a randomised prevention trial. Lancet. 2002;360(9336):817–24.
Smith SG, Sestak I, Howell A, Forbes J, Cuzick J. Participant-reported symptoms and their effect on long-term adherence in the international breast cancer intervention Study I (IBIS I). J Clin Oncol. 2017;35(23):2666–73. Erratum in: J Clin Oncol. 2018;36(3):304.
Cuzick J, Sestak I, Forbes JF, Dowsett M, et al. Use of anastrozole for breast cancer prevention (IBIS-II): long-term results of a randomised controlled trial. Lancet. 2020;395(10218):117–22. Erratum in: Lancet. 2020;395(10223):496. Erratum in: Lancet. 2021;397(10276):796.
Britt KL, Cuzick J, Phillips KA. Key steps for effective breast cancer prevention. Nat Rev Cancer. 2020;20(8):417–36.
Ming C, Viassolo V, Probst-Hensch N, et al. Machine learning-based lifetime breast cancer risk reclassification compared with the BOADICEA model: impact on screening recommendations. Br J Cancer. 2020;123(5):860–7.
Lee A, Mavaddat N, Wilcox AN, Cunningham AP, et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med. 2019;21(8):1708–18. Erratum in: Genet Med. 2019 Feb 21.
Breast Cancer Surveillance Consortium Risk Calculator. Introduction. https://tools.bcsc-scc.org/BC5yearRisk/intro.htm.
Vachon CM, Pankratz VS, Scott CG, et al. The contributions of breast density and common genetic variation to breast cancer risk. J Natl Cancer Inst. 2015;107(5):dju397.
Tice JA, Bissell MCS, Miglioretti DL, et al. Validation of the breast cancer surveillance consortium model of breast cancer risk. Breast Cancer Res Treat. 2019;175(2):519–23.
National Comprehensive Cancer Network. Breast cancer screening and diagnosis. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1421.
National Comprehensive Cancer Network. Genetic/familial high-risk assessment: breast, ovarian, and pancreatic. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1503.
Yadav S, LaDuca H, Polley EC, Hu C, et al. Racial and ethnic differences in multigene hereditary cancer panel test results for women with breast cancer. J Natl Cancer Inst. 2021;113(10):1429–33.
Pashayan N, Antoniou AC, Ivanus U, et al. Personalized early detection and prevention of breast cancer: ENVISION consensus statement. Nat Rev Clin Oncol. 2020;17(11):687–705. Erratum in: Nat rev Clin Oncol. 2020 Jun 29.
Roux A, Cholerton R, Sicsic J, et al. Study protocol comparing the ethical, psychological and socio-economic impact of personalised breast cancer screening to that of standard screening in the “my personal breast screening” (MyPeBS) randomised clinical trial. BMC Cancer. 2022;22(1):507.
McClintock AH, Golob AL, Laya MB. Breast cancer risk assessment: a step-wise approach for primary care providers on the front lines of shared decision making. Mayo Clin Proc. 2020;95(6):1268–75.
Gail MH. Choosing breast cancer risk models: importance of independent validation. J Natl Cancer Inst. 2020;112(5):433–5.
McCarthy AM, Guan Z, Welch M, et al. Performance of breast cancer risk-assessment models in a large mammography cohort. J Natl Cancer Inst. 2020;112(5):489–97.
Pal Choudhury P, Wilcox AN, Brook MN, et al. Comparative validation of breast cancer risk prediction models and projections for future risk stratification. J Natl Cancer Inst. 2020;112(3):278–85.
Nickson C, Procopio P, Velentzis LS, et al. Prospective validation of the NCI breast cancer risk assessment tool (Gail model) on 40,000 Australian women. Breast Cancer Res. 2018;20(1):155.
Solikhah S, Nurdjannah S. Assessment of the risk of developing breast cancer using the Gail model in Asian females: a systematic review. Heliyon. 2020;6(4):e03794.
Yap YS, Lu YS, Tamura K, et al. Insights into breast cancer in the east vs the west: a review. JAMA Oncol. 2019;5(10):1489–96.
Senda N, Kawaguchi-Sakita N, Kawashima M, et al. Optimization of prediction methods for risk assessment of pathogenic germline variants in the Japanese population. Cancer Sci. 2021;112(8):3338–48.
Momozawa Y, Iwasaki Y, Parsons MT, et al. Germline pathogenic variants of 11 breast cancer genes in 7,051 Japanese patients and 11,241 controls. Nat Commun. 2018;9(1):4083.
Shao D, Cheng S, Guo F, Zhu C, et al. Prevalence of hereditary breast and ovarian cancer (HBOC) predisposition gene mutations among 882 HBOC high-risk Chinese individuals. Cancer Sci. 2020;111(2):647–57.
Hung FH, Wang YA, Jian JW, et al. Evaluating BRCA mutation risk predictive models in a Chinese cohort in Taiwan. Sci Rep. 2019;9(1):10229.
Kwong A, Shin VY, Ho JC, et al. Comprehensive spectrum of BRCA1 and BRCA2 deleterious mutations in breast cancer in Asian countries. J Med Genet. 2016;53(1):15–23.
Li S, Silvestri V, Leslie G, et al. Cancer risks associated with BRCA1 and BRCA2 pathogenic variants. J Clin Oncol. 2022;40(14):1529–41.
Cuzick J, Brentnall AR, Segal C, et al. Impact of a panel of 88 single nucleotide polymorphisms on the risk of breast cancer in high-risk women: results from two randomized Tamoxifen prevention trials. J Clin Oncol. 2017;35(7):743–50.
van Veen EM, Brentnall AR, Byers H, et al. Use of single-nucleotide polymorphisms and mammographic density plus classic risk factors for breast cancer risk prediction. JAMA Oncol. 2018;4(4):476–82.
Mavaddat N, Michailidou K, Dennis J, et al. Polygenic risk scores for prediction of breast cancer and breast cancer subtypes. Am J Hum Genet. 2019;104(1):21–34.
Arthur RS, Wang T, Xue X, Kamensky V, Rohan TE. Genetic factors, adherence to healthy lifestyle behavior, and risk of invasive breast cancer among women in the UK biobank. J Natl Cancer Inst. 2020;112(9):893–901. Erratum in: J Natl cancer Inst. 2020;112(10):1076.
Kapoor PM, Mavaddat N, Choudhury PP, et al. Combined associations of a polygenic risk score and classical risk factors with breast cancer risk. J Natl Cancer Inst. 2021;113(3):329–37.
Kramer I, Hooning MJ, Mavaddat N, et al. Breast cancer polygenic risk score and contralateral breast cancer risk. Am J Hum Genet. 2020;107(5):837–48.
Zene. https://www.zene.co.jp/.
Barnes DR, Silvestri V, Leslie G, et al. Breast and prostate cancer risks for male BRCA1 and BRCA2 pathogenic variant carriers using polygenic risk scores. J Natl Cancer Inst. 2022;114(1):109–22.
Gao C, Polley EC, Hart SN, et al. Risk of breast cancer among carriers of pathogenic variants in breast cancer predisposition genes varies by polygenic risk score. J Clin Oncol. 2021;39(23):2564–73.
Borde J, Ernst C, Wappenschmidt B, et al. Performance of breast cancer polygenic risk scores in 760 female CHEK2 Germline mutation carriers. J Natl Cancer Inst. 2021;113(7):893–9.
Zhang H, Ahearn TU, Lecarpentier J, et al. Genome-wide association study identifies 32 novel breast cancer susceptibility loci from overall and subtype-specific analyses. Nat Genet. 2020;52(6):572–81.
Ahearn TU, Zhang H, Michailidou K, et al. Common variants in breast cancer risk loci predispose to distinct tumor subtypes. Breast Cancer Res. 2022;24(1):2.
Zhang YD, Hurson AN, Zhang H, et al. Assessment of polygenic architecture and risk prediction based on common variants across fourteen cancers. Nat Commun. 2020;11(1):3353.
Mars N, Koskela JT, Ripatti P, et al. Polygenic and clinical risk scores and their impact on age at onset and prediction of cardiometabolic diseases and common cancers. Nat Med. 2020;26(4):549–57.
Ryu EB, Chang JM, Seo M, et al. Tumour volume doubling time of molecular breast cancer subtypes assessed by serial breast ultrasound. Eur Radiol. 2014;24(9):2227–35.
Zhang S, Ding Y, Zhou Q, Wang C, Wu P, Dong J. Correlation factors analysis of breast cancer tumor volume doubling time measured by 3D-ultrasound. Med Sci Monit. 2017;23:3147–53.
Nakashima K, Uematsu T, Takahashi K, et al. Does breast cancer growth rate really depend on tumor subtype? Measurement of tumor doubling time using serial ultrasonography between diagnosis and surgery. Breast Cancer. 2019;26(2):206–14.
Plevritis SK, Munoz D, Kurian AW, et al. Association of Screening and Treatment with Breast Cancer Mortality by molecular subtype in US women, 2000–2012. JAMA. 2018;319(2):154–64. Erratum in: JAMA. 2018;319(7):724.
Esserman LJ, WISDOM Study and Athena Investigators. The WISDOM Study: breaking the deadlock in the breast cancer screening debate. NPJ Breast Cancer. 2017;3:34.
Eklund M, Broglio K, Yau C, et al. The WISDOM personalized breast cancer screening trial: simulation Study to assess potential bias and analytic approaches. JNCI Cancer Spectr. 2019;2(4):pky067.
Giordano L, Gallo F, Petracci E, et al. The ANDROMEDA prospective cohort study: predictive value of combined criteria to tailor breast cancer screening and new opportunities from circulating markers: study protocol. BMC Cancer. 2017;17(1):785.
Delaloge S, Giorgi Rossi P, Balleyguier C, et al. 135P Real-time genotyping-based breast cancer risk assessment in MyPeBS, an international randomized trial in the general population comparing risk-stratified to standard breast cancer screening (BCS). Ann Oncol. 2022;33(Suppl. 3):S184. https://doi.org/10.1016/j.annonc.2022.03.152.
French DP, Astley S, Brentnall AR, et al. What are the benefits and harms of risk stratified screening as part of the NHS breast screening Programme? Study protocol for a multi-site non-randomised comparison of BC-predict versus usual screening (NCT04359420). BMC Cancer. 2020;20(1):570.
Liu J, Ho PJ, Tan THL, et al. BREAst screening tailored for HEr (BREATHE)-a study protocol on personalised risk-based breast cancer screening programme. PLoS One. 2022;17(3):e0265965.
Schwarzenbach H, Muller V, Milde-Langosch K, Steinbach B, Pantel K. Evaluation of cell-free tumor DNA and RNA in patients with breast cancer and benign breast disease. Mol BioSyst. 2011;7(10):2848–54.
Dawson SJ, Tsui DW, Murtaza M, et al. Analysis of circulating tumor DNA to monitor metastatic breast cancer. N Engl J Med. 2013;368(13):1199–209.
Bettegowda C, Sausen M, Leary RJ, et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6(224):224ra24.
Takahashi H, Kagara N, Tanei T, et al. Correlation of methylated circulating tumor DNA with response to neoadjuvant chemotherapy in breast cancer patients. Clin Breast Cancer. 2017;17(1):61–69.e3.
Fribbens C, Garcia Murillas I, Beaney M, et al. Tracking evolution of aromatase inhibitor resistance with circulating tumor DNA analysis in metastatic breast cancer. Ann Oncol. 2018;29(1):145–53.
Hackshaw A, Cohen SS, Reichert H, et al. Estimating the population health impact of a multi-cancer early detection genomic blood test to complement existing screening in the US and UK. Br J Cancer. 2021;125(10):1432–42.
Cohen JD, Li L, Wang Y, et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science. 2018;359(6378):926–30.
Liu MC, Oxnard GR, Klein EA, et al. Sensitive and specific multi-cancer detection and localization using methylation signatures in cell-free DNA. Ann Oncol. 2020;31(6):745–59.
Klein EA, Richards D, Cohn A, et al. Clinical validation of a targeted methylation-based multi-cancer early detection test using an independent validation set. Ann Oncol. 2021;32(9):1167–77.
Lennon AM, Buchanan AH, Kinde I, et al. Feasibility of blood testing combined with PET-CT to screen for cancer and guide intervention. Science. 2020;369(6499):eabb9601.
U.S. National Library of Medicine. https://clinicaltrials.gov/.
Nadauld LD, McDonnell CH 3rd, Beer TM, et al. The PATHFINDER Study: assessment of the implementation of an investigational multi-cancer early detection test into clinical practice. Cancers (Basel). 2021;13(14):3501.
Yala A, Mikhael PG, Strand F, et al. Toward robust mammography-based models for breast cancer risk. Sci Transl Med. 2021;13(578):eaba4373.
Yala A, Lehman C, Schuster T, et al. A deep learning mammography-based model for improved breast cancer risk prediction. Radiology. 2019;292(1):60–6.
Eriksson M, Destounis S, Czene K, et al. A risk model for digital breast tomosynthesis to predict breast cancer and guide clinical care. Sci Transl Med. 2022;14(644):eabn3971.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Toi, M., Kataoka, M., Velaga, R., Benson, J.R., Matsumoto, Y. (2023). Breast Cancer Risk Assessment Models and Multi-Cancer Early Detection Tests. In: Toi, M. (eds) Screening and Risk Reduction Strategies for Breast Cancer. Springer, Singapore. https://doi.org/10.1007/978-981-19-7630-8_2
Download citation
DOI: https://doi.org/10.1007/978-981-19-7630-8_2
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-7629-2
Online ISBN: 978-981-19-7630-8
eBook Packages: MedicineMedicine (R0)