Abstract
With ever improving survival rates and the success of modern medicine in fine tuning the treatment of Wilms’ tumor (WT), there is a decreasing trend of a recurrent or a relapsed WT. Infrequent though a recurrence is in today’s day-to-day practice, it is still an unfortunate part of treatment of WT. In this chapter, we attempt to understand the incidence and the required surveillance for detecting a relapse. We need to also understand the factors influencing the occurrence site and the timing of a relapse, the basics of patient risk stratification, and how it influences the strategy for further management of a recurrence along with the newer therapies that may become available in the future.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
31.1 Introduction
The management of Wilms’ tumor (WT) has undergone a sea change with the introduction and refinement of multimodal therapy, which includes surgery, chemotherapy (ChT), and radiotherapy (XRT). With these advancements, children with these tumors can expect an overall survival (OS) rates approaching 90% [1].
However, relapse/recurrence of WT is not uncommon. About 15% of patients with favorable-histology (FH) WT experience a recurrence, whereas half the patients with an anaplastic WT (AWT) have a recurrence [2]. The incidence of recurrences in low and middle income countries (LMIC) have been high, with even the latest rates being reported up to 30% [3]. Most recurrences in WT occur within 2 years from the time of diagnosis. Late recurrences are rare and can occur up to 25 years from the initial diagnosis [4,5,6,7]. In a retrospective study in more than 13,000 children across various WT trials, the rate of late recurrence were only 0.5% [8]. Lung and pleura account for 50–60% of recurrences, whereas the abdominal recurrences contribute toward 30% of relapses. Other sites like the brain and bone are involved in 10–15% [9,10,11].
In contrast to the primary WT, the recurrent Wilms’ tumors (RWT) carry poor prognosis, with only 3-year OS of only 24–40%, while a subset of patients with FH have an OS of 77% [3, 12].
The surveillance protocol for a patient treated for WT is discussed in another chapter and is not repeated here.
31.2 Site(s) of Relapse and Presentation
The recurrence can occur in the lungs and abdomen (with or without involvement of the lungs) and rarely in the brain and bones. Most common recurrence is seen within the lungs (58–63%), followed by the abdomen, with or without involvement of other sites (29–49%) [8, 12]. RWT in the brain or bones is a rare event (13%). Abdominal RWT can involve the previous site, liver, and opposite kidney and, sometimes extremely rare, unusual sites like the uterus and cervical lymph nodes (LN) [5, 13]. The distribution of the site of recurrence was similar, irrespective of whether the patients had received XRT or not.
Recurrences, in cases with FH in initial diagnosis, confined to the lungs only tend to have better prognosis compared to abdominal or other site recurrence, with 3-year OS of 44% vs. 28% vs. 11% [12]. Unfavorable histology (UH) has poor prognosis irrespective of the site of relapse. Though recurrence in the liver carries poorer prognosis, with 4-year OS of 14%, successful surgical excision of these tumors can have good prognosis.
The RWT may or may not cause symptoms in these patients. The prognosis of patients who present with asymptomatic relapses, which are detected during the surveillance imaging, is better compared to those that present with symptoms (nearly twice the mortality) [14]. Abdominal recurrences may present with lump in the abdomen due to recurrence at previous site or liver or gross distension due to ascites, contralateral kidney mass, or pelvic mass. Pulmonary recurrences manifest as difficulty in breathing due to parenchymal masses or pleural effusion, cough, and very rarely pneumothorax [15]. For those with intracranial recurrences, presentation features include seizures, headache, vomiting, paresis/paralysis, and impaired consciousness [11].
31.3 Time of Recurrence
RWT are more prevalent within 2 years after treatment. Recurrences occurring beyond 5 years of treatment are termed as late recurrences. In the largest study that observed late recurrences, the distribution of recurrences in both alive and dead cases had no correlation with gender (equal incidence in both the genders), initial tumor stage, or type of previous treatment received. However, most of these cases had FH in the previous tumor [8]. Late recurrences can be either true recurrence or a metachronous WT in the contralateral kidney (attributed to persistence of nephrogenic rests). The survival in such case is better (87% vs. 45%) compared to recurrences elsewhere. The exact etiopathogenesis of late recurrences is not known. Quiescent tumor stem cells in such sites might escape the immune vigilance and may get activated by unknown stimuli (e.g., hormones in adolescents).
Grundy et al. measured the time to relapse and divided the period into early (0–5 months), intermediate (6–11 months), and late relapse (12+ months). The early relapse cases were mostly UH types at initial diagnosis and had the poorest 3-year-OS among the above strata (18%) [9].
31.4 Factors Influencing Occurrence of Relapse
Stage and histology are two of the most important factors that dictate the course of the disease. With respect to relapse, though no specific identifiable factors causing relapse are identified, the risk of relapse can be predicted in certain subgroups.
Stage III–IV WT, which have gained access to the lympho-vascular structures, can lead to seeding of tumor cells at local and distant sites, potentially causing more recurrences than the stage I–II tumors. The patients with initial stage I FH WT had better post-relapse survival compared to stage IV FH (57% vs. 17%) [12].
AWT and pretreated tumors with blastemal-type histology, which are considered as high-risk types, are again resistant to treatment and cause early relapses.
Biological markers have been much discussed in recent times. Especially the loss of heterozygosity (LOH) at 1p and 16q, which, in even the FH WT, have caused more relapses [16].
The initial treatment received also holds significance with respect to post-relapse prognosis. Patients who received two-drug therapy, vincristine (VCR) and actinomycin-D (AMD), had better survival rates compared to patients who received three-drug therapy (VCR, AMD, and doxorubicin) (42% vs. 26%), in an analysis done for stage II–III (FH) cases. Perhaps patients who received only two drugs had better sensitivity of RWT for the third drug during post-relapse treatment.
XRT to the abdomen doesn’t predict the future risk of relapse. But previously unirradiated abdominal RWT are better salvageable compared to RWT in previously irradiated cases. RWT in the lungs occurred more frequently in unirradiated sites.
Percutaneous biopsy of renal tumor at initial presentation has been considered a risk for recurrence for a long time. But a study from UK found the initial biopsy increased the risk of local relapse (abdomen, other than liver) while having no effect on distant relapse [17]. But the significance was less when histology and size were considered in the multivariate analysis for local relapse.
Another factor to be considered here is the size of the tumor at initial diagnosis. Tumors >12 cm in size are significantly large and have high risk of rupture. This is more significant for those above 15 cm in size. Rupture of tumor is associated with increased risk of local recurrence [18].
Males fare slightly worse than females [19].
In a multivariate analysis of adverse prognostic factor in children with RWT who had been enrolled under the SIOP-6 or SIOP-9 treatment strategies, SIOP identified various adverse factors for RWT [20]:
-
1.
Stage IV disease.
-
2.
UH.
-
3.
Time to recurrence of 6 months or less after initial diagnosis.
-
4.
Multiple sites of recurrence.
-
5.
Previous history of XRT.
Other studies have analyzed 95 patients and demonstrated an association of LN involvement and anaplasia as an adverse prognostic factor correlated with an increased probability of relapse [21]. A European group analyzed 170 patients with relapse and found the following adverse risk factors for a relapse [22]:
-
1.
Initial stage III or IV.
-
2.
High-risk histology.
-
3.
Time to recurrence of 6 months or less after initial diagnosis.
-
4.
Site of relapse.
The precise effect of site of relapse in a RWT is vitiated by the fact that many abdominal recurrences may occur in irradiated fields and many published reports may include contralateral kidney as a recurrence along with tumor bed, liver, or LN. Similarly, many lung recurrences may occur in previously unirradiated areas but may also include mediastinal recurrences. There is a definite need to further evaluate the site of relapse as a prognostic factor for a recurrence.
31.5 Therapy for RWT
There is a limited experience available for the optimal rescue therapy for RWT. Most patients receive VCR and AMD, with or without doxorubicin (DOX), as part of the initial therapy for the primary lesion. Before the 1990s, the same ChT agents were used for the treatment of both primary and recurrent disease. However, the salvage rates with the same ChT agents in recurrent disease were as low as 25–40% [2]. With the introduction of alternate treatment combinations, the outcomes started improving up to 60% in the last 20 years [23]. As a general principle, it is preferable to avoid the agents that have been previously used as part of the initial therapy and to tailor the therapy using a risk-stratified approach. It is common to use ifosfamide, carboplatin (CARB), and etoposide (ETOP), either as a single agent or in combination (ICE regimen) (Fig. 31.1) [24].
ICE regimen IFO Ifosfamide [24]
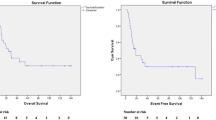
ETOP has demonstrated an efficacy of 42% in clinical trials [25], whereas ifosfamide and CARB have shown a 52% objective response [25, 26]. Recent studies have documented the activity of topotecan in FH RWT but have not demonstrated any efficacy in AWT [27]. The introduction of these drugs led to event-free survival (EFS) rates ranging from 50 to 70% [23]. However, the best combinations, dose intensity, and the duration of therapy still remain to be fleshed out. Moreover, the prognosis of the patients with RWT depends upon many other factors including the initial tumor stage, histology, previous modalities of therapies, site of relapse, and the time from the initial diagnosis to relapse. It also becomes difficult to standardize the various other modalities for treatment, viz., local surgical excision and XRT, especially for already irradiated relapses. High-dose ChT with stem cell rescue (SCR) is being increasingly utilized for the treatment of RWT with improving survival rates [28].
31.6 Management: Patient Risk Stratification Approach
A number of potential prognostic features influence the outcomes post a relapse. However, it is often difficult to determine the effect of each factor independently, as the numbers are low, and it is difficult to compare the subgroups of these patients. Also, the prognostic factors seem to be changing over time as the understanding and the therapy of primary and RWT evolve [21, 22].
Based on the current state of science, the following risk categories for RWT can be identified (Table 31.1) [29, 30]:
-
1.
Standard risk [30].
-
(a)
FH RWT with initial therapy with therapy with VCR and/or AMD.
-
(b)
Account for 30% of all recurrences.
-
(c)
Event-free survival (EFS) of 70–80%.
-
(a)
-
2.
High risk (HR) [31].
-
(a)
FH RWT with initial therapy with three or more ChT agents.
-
(b)
Account for 45–50% of all recurrences.
-
(c)
EFS of 40–50%.
-
(a)
-
3.
Very high risk (VHR) [32].
-
(a)
Anaplastic, or blastemal-predominant RWT.
-
(b)
Account for 10–15% of all recurrences.
-
(c)
EFS of 10–15% only.
-
(a)
However, it is expected that with changes in treatment and further refinement in treating WT, the factors identified for risk stratification may lose their significance. More aggressive regimens which are more effective in dealing with RWT along with a judicious use of radiotherapy may also affect the significance of factors identified.
31.6.1 Management of Standard Risk RWT
The data on the management of standard risk RWT is limited due to a limited cohort of patients. However, the management of the standard risk RWT has revolved around two main protocols- one from National Wilms Tumor Study (NWTS) Group and the other from United Kingdom’s Children’s Cancer and Leukaemia Group (UKCCLG):
31.6.1.1 Stratum B of the NWTS-5 Relapse Protocol [33]
NWTS-5 relapse treatment consisted mainly of alternating courses of VCR-DOX- CTX and ETOP, which is similar to the Regimen I used as standard treatment for WT (Fig. 31.2). Surgical excision is employed only in locations which are amenable to surgical excision. XRT may also be used in selected cases. Four-year overall survival (OS) was 81.8% for all patients with a slightly lower EFS rates for children who had lung relapses.
Stratum B of the NWTS-5 Relapse Protocol [33]
31.6.1.2 UKW-R Protocol of UKCCLG [34]
Here, patients with recurrences were managed by either a pulse intensive regimen of VCR, AMD, and DOX or an alternating course of DOX-CYCLO and CYCLO-ETOPO (Fig. 31.3).
UKW-R Protocol [34]
31.6.2 Management of High-Risk RWT
The management of these difficult cases has revolved around either a conventional-dose ChT or a high-dose ChT with an autologous SCR.
31.6.2.1 Conventional-Dose Chemotherapy
A study published on the treatment of 60 children with relapse reported the management of these children by alternate courses of CTX and CARB with CARB and ETOP over a period of 90 weeks as part of the Stratum C of the NWTS relapse protocol [35]. They reported a 4-year EFS and OS of 42.3% and 48%, respectively. Abu-Ghosh et al. reported 63.6% EFS and OS with high-risk (HR) RWT treated with ICE ChT along with other therapies like surgical excision and XRT [36].
31.6.2.2 High-Dose ChT with Autologous SCR
High-dose myeloablative ChT is utilized along with bone marrow transplantation (BMT) and autologous SCR in an effort to treat the HR RWT. However, most of these treatments are outside the realm of controlled clinical trials. The aim is to obtain a better outcome than historical controls and various centers reporting higher 4-year OS rates (60–73%) [36, 37]. The French Society for Paediatric Oncology reported on 28 HR RWT treated with high-dose ChT with SCR and achieved an OS of 60.9% [37]. The regimen used in these studies utilized either a high dose ICE Regimen or a therapy using elphalan, ETOP, and CARB (MEC regimen) [35]. The German Cooperative Wilms Tumor Study Group reported on patients with HR RWT with ChT utilizing alternating regimen of CTX-ETOP with CARB-ETOP. Children who achieved complete response (CR) were continued on the same therapy, whereas who had partial response (PR) or and no response received ablative ChT with autologous SCR [38]. Campbell et al. reported on 13 children with relapsed WT treated with high-dose ChT with SCR and reported a 4-year OS of 73% [39].
Topotecan has been variably incorporated in the treatment of patients with RWT who failed initial treatment with three or more effective drugs. Topotecan is a camptothecin analog that has demonstrated antitumor activity in various childhood cancers including WT. A retrospective review of 16 children who received topotecan as part of their salvage regimens for HR RWT demonstrated no effectiveness in the treatment of HR histology RWT patients. However, its role is still equivocal in standard risk histology [39].
Thus, the current state of literature suggests that high-dose ChT with SCR might be an effective treatment for patients with HR RWT.
31.6.3 Management of Very-High-Risk RWT
Patients with AWT or advanced tumors on initial therapy who present with a recurrence have generally demonstrated abysmal survival rates to the currently employed treatment strategies [23, 40, 41]. Overall, in these patients, a very poor response to any drug combination due to intrinsic drug resistance has been reported and only a handful of survivors. Other ChT agents and novel strategies may be required to improve the outcomes in this group of patients.
31.7 Other Strategies
Most patients with RWT can be rescued with salvage therapy especially in the standard risk group. However, the HR and the VHR groups demonstrate poorer survival rates with almost very poor survival rates in the VHR. There is a need to identify newer novel agent and targeted therapies for the treatment of these children. A systematic review of literature for published phase I and II clinical trials that registered patients with WT had identified 62 trials. Fifty of these were phase I and 12 were phase II trials, and these enrolled a total of 214 patients with RWT [42]. Overall, only 33 WTs demonstrated any degree of tumor control with these strategies with only 5 patients (2%) demonstrating CR and only 15 patients (7%) demonstrating a PR. This highlights the currently dismal outlook with newer strategies. Various agents that have been attempted in the management have been oxaliplatin, thiotepa, VEGF, bevacizumab, and all-trans-retinoic acid among other agents [43].
31.8 Role of Surgery and XRT in the Management of RWT
Logically, surgical removal of operable tumors should be helpful, but the evidence for the same is lacking in literature. The NWTS group suggests that a surgical removal of all pulmonary metastasis is unlikely to improve survival rate when compared to ChT [43]. Fuchs et al. reported on children with liver metastasis and the outcome of surgical excision in those group [44]. They reported that the patients who could be managed by a complete surgical excision survived. Similarly, an excision of solitary lung metastasis might avoid the toxicity of lung XRT. There have been no clear guidelines for administering XRT in this select group of patients. However, reports of administration of whole abdominal irradiation (WAI) for abdominal or hepatic recurrence and whole lung irradiation (WLI) for pulmonary recurrence(s) do exist [43].
31.9 Treatment of RWT in SIOP-RTSG Umbrella protocol
In the UMBRELLA protocol, patients with relapsed tumours are classified into three groups AA, group BB, and group CC, based on these factors [45]. Treatment of group AA relapsed WT, defined as patients with initial stage I−II low-risk or intermediate-risk tumours, who received only VCR and/or AMD (no XRT) in their first-line treatment, will include four drugs (combinations of DOX and/or CTX and CARB and/or ETOP). The combination of these drugs are same used in NWTS-5 relapse protocol and UKW-R protocol and the, but drug combinations and doses vary. Treatment of group BB relapsed WT without initial diffuse anaplasia or blastemal-type histology, who have already received DOX in their initial treatment receive an intensive reinduction drug regimen (including the combination of ETOP and CARB with either IFO or CTX), followed by either high-dose melphalan and autologous stem cell rescue (ASCR) or two further reinduction courses [29]. Relapsed group CC includes patients with initial diffuse anaplasia or blastemal-type tumours. For patients in this category, and for the other relapsing patients showing no response to salvage treatment, the UMBRELLA protocol advises trying camptothecins (irinotecan or topotecan) or novel compounds, as these patients will have already received most conventional active agents in their first-line therapy and are likely to develop ChT-resistant disease [46]. UMBRELLA protocol also provides structured guide-lines for administering XRT and surgery at relapse [45].
31.10 Surveillance Schedule After a Complete Response (CR) Following Relapse
There is scarce evidence about optimal surveillance schedules and methods for detection of tumor relapse after a CR following a relapse. Since there are no optimal guidelines for surveillance schedules available in literature, a surveillance schedule detailed for WT with high risk of recurrence might be suitable. In view of the late effects of highly intensive and toxic ChT and XRT, a long-term surveillance protocol may be required to capture recurrent relapse, second malignancies, and/or other effects [43].
References
de Kraker J, Graf N, van Tinteren H, Pein F, Sandstedt B, Godzinski J, et al. SIOP. Reduction of postoperative chemotherapy in children with stage I intermediate-risk and anaplastic Wilms’ tumour (SIOP 93-01 trial): a randomised controlled trial. Lancet. 2004;364(9441):1229–35. https://doi.org/10.1016/S0140-6736(04)17139-0.
Kalapurakal JA, Dome JS, Perlman EJ, Malogolowkin M, Haase GM, Grundy P, et al. Management of Wilms’ tumour: current practice and future goals. Lancet Oncol. 2004;5:37–46. https://doi.org/10.1016/s1470-2045(03)01322-6.
Zekri W, Yacoub DM, Ibrahim A, Madney Y. Relapsed Wilms’ tumor in pediatric patients: challenges in low- to middle-income countries- a single-center experience. J Egypt Natl Canc Inst. 2020;32:21. https://doi.org/10.1186/s43046-020-00032-6.
Radhakrishnan V, Mishra S, Raja A, Sundersingh S. Relapse of Wilms tumor after 20 years: a rare presentation and review of literature. Ped Hemat Oncol J. 2017;1:86–8. https://doi.org/10.1016/j.phoj.2017.02.001.
Sudour-Bonnange H, Lervat C, Renaud F, Gauthier H, Rocourt N. An unusual late recurrence of Wilms tumor. J Pediatr Hematol Oncol. 2016;38:e151–3. https://doi.org/10.1097/MPH.0000000000000522.
Park WY, Hong KT, Ahn HY, Choi JY, Kang HJ, Park SH, et al. Late recurrence of Wilms tumor after 17 years: a case report. J Pediatr Hematol Oncol. 2020;42:e488–90. https://doi.org/10.1097/MPH.0000000000001473.
Lee SY, Kim KR, Park JY, Ro JY. Wilms’ tumor with long-delayed recurrence: 25 years after initial treatment. Korean J Urol. 2012;53:288–92. https://doi.org/10.4111/kju.2012.53.4.288.
Malogolowkin M, Spreafico F, Dome JS, van Tinteren H, Pritchard-Jones K, van den Heuvel-Eibrink MM, et al. COG renal tumors committee and the SIOP renal tumor study group. Incidence and outcomes of patients with late recurrence of Wilms’ tumor. Pediatr Blood Cancer. 2013;60:1612–5. https://doi.org/10.1002/pbc.24604.
Grundy P, Breslow N, Green DM, Sharples K, Evans A, D'Angio GJ. Prognostic factors for children with recurrent Wilms’ tumor: results from the second and third National Wilms’ tumor study. J Clin Oncol. 1989;7:638–47. https://doi.org/10.1200/JCO.1989.7.5.638.
Lowis SP, Foot A, Gerrard MP, Charles A, Imeson J, Middleton H, et al. Central nervous system metastasis in Wilms’ tumor: a review of three consecutive United Kingdom trials. Cancer. 1998;83:2023–9. https://doi.org/10.1002/(sici)1097-0142(19981101)83:9<2023::aid-cncr20>3.0.co;2-l.
van den Heuvel-Eibrink MM, Graf N, Pein F, Sandstedt B, van Tinteren H, van der Vaart KE, et al. Intracranial relapse in Wilms tumor patients. Pediatr Blood Cancer. 2004;43:737–41. https://doi.org/10.1002/pbc.20150.
Phelps HM, Kaviany S, Borinstein SC, Lovvorn HN 3rd. Biological drivers of Wilms tumor, prognosis and treatment. Children (Basel). 2018;5:145. https://doi.org/10.3390/children5110145.
Alldredge J, Mercurio C, Berman M. Very late recurrence of Wilms’ tumor at the uterus and concurrent BRCA2 risk reduction: a case report. Pediatr Hematol Oncol J. 2019;4:89–93. https://doi.org/10.1016/j.phoj.2019.12.002.
Brok J, Lopez-Yurda M, Tinteren HV, Treger TD, Furtwangler R, Graf N, et al. Relapse of Wilms’ tumor detection methods: a retrospective analysis of 2001 Renal Tumour Study Group-International Society of Paediatric Oncology Wilms’ tumor protocol database. Lancet Oncol. 2018;19:1072–81.
Gordon J, Akhtar S, Thorpe A. Recurrent Wilms tumour presenting as bilateral pneumothoraces. Eur J Cardiothorac Surg. 2003;23:645–6. https://doi.org/10.1016/S1010-7940(03)00028-9.
Grundy PE, Breslow NE, Li S, Perlman E, Beckwith JB, Ritchey ML, et al. National Wilms Tumor Study Group. Loss of heterozygosity for chromosomes 1p and 16q is an adverse prognostic factor in favorable-histology Wilms tumor: a report from the National Wilms Tumor Study Group. J Clin Oncol. 2005;23:7312–21. https://doi.org/10.1200/JCO.2005.01.2799.
Irtan S, Jitlal M, Bate J, Powis M, Vujanic G, Kelsey A, et al. Renal Tumours Committee of the Children’s Cancer and Leukaemia Group (CCLG). Risk factors for local recurrence in Wilms tumour and the potential influence of biopsy—the United Kingdom experience. Eur J Cancer. 2015;51:225–32. https://doi.org/10.1016/j.ejca.2014.10.026.
Gow KW, Barnhart DC, Hamilton TE, Kandel JJ, Chen MK, Ferrer FA, et al. Primary nephrectomy and intraoperative tumor spill: report from the Children’s oncology group (COG) renal tumors committee. J Pediatr Surg. 2013;48:34–8. https://doi.org/10.1016/j.jpedsurg.2012.10.015.
Faranoush M, Bahoush G, Meharvar A, Hejazi S, Vossough P, Asl AAH, et al. Wilm’s tumor: epidemiology and survival. Res J Biol Sci. 2009;4:86–9.
Pein F, Rey A, de Kraker J. Multivariate analysis of adverse prognostic factors (APF) in children with recurrent Wilms’ tumor (WT) after initial treatment according to SIOP-6 or SIOP-9 strategies. Med Pediatr Oncol. 1999;33:170.
Honeyman JN, Rich BS, McEvoy MP, Knowles MA, Heller G, Riachy E, et al. Factors associated with relapse and survival in Wilms tumor: a multivariate analysis. J Pediatr Surg. 2012;47:1228–33. https://doi.org/10.1016/j.jpedsurg.2012.03.030.
Reinhard H, Schmidt A, Furtwängler R, Leuschner I, Rübe C, Von Schweinitz D, et al. Outcome of relapses of nephroblastoma in patients registered in the SIOP/GPOH trials and studies. Oncol Rep. 2008;20:463–7.
Dome JS, Liu T, Krasin M, Lott L, Shearer P, Daw NC, et al. Improved survival for patients with recurrent Wilms tumor: the experience at St. Jude Children’s Research Hospital. J Pediatr Hematol Oncol. 2002;24:192–8. https://doi.org/10.1097/00043426-200203000-00007.
Sarin YK, Graf N. Management of recurrent Wilms’ tumor. JIMSA. 2014;27:90–3.
Pein F, Pinkerton R, Tournade MF, Brunat-Mentigny M, Levitt G, Margueritte G, et al. Etoposide in relapsed or refractory Wilms’ tumor: a phase II study by the French Society of Pediatric Oncology and the United Kingdom Children’s Cancer Study Group. J Clin Oncol. 1993;11:1478–81. https://doi.org/10.1200/JCO.1993.11.8.1478.
Pein F, Tournade MF, Zucker JM, Brunat-Mentigny M, Deville A, Boutard P, et al. Etoposide and carboplatin: a highly effective combination in relapsed or refractory Wilms’ tumor—a phase II study by the French Society of Pediatric Oncology. J Clin Oncol. 1994;12:931–6. https://doi.org/10.1200/JCO.1994.12.5.931.
Mavinkurve-Groothuis AM, van den Heuvel-Eibrink MM, Tytgat GA, van Tinteren H, Vujanic G, Pritchard-Jones KL, et al. Treatment of relapsed Wilms tumour (WT) patients: experience with topotecan. A report from the SIOP renal tumour study group (RTSG). Pediatr Blood Cancer. 2015;62:598–602. https://doi.org/10.1002/pbc.25357.
Presson A, Moore TB, Kempert P. Efficacy of high-dose chemotherapy and autologous stem cell transplant for recurrent Wilms’ tumor: a meta-analysis. J Pediatr Hematol Oncol. 2010;32:454–61. https://doi.org/10.1097/MPH.0b013e3181e001c2.
Spreafico F, Pritchard Jones K, Malogolowkin MH, Bergeron C, Hale J, de Kraker J, et al. Treatment of relapsed Wilms tumors: lessons learned. Expert Rev Anticancer Ther. 2009;9:1807–15. https://doi.org/10.1586/era.09.159.
Ha TC, Spreafico F, Graf N, Dallorso S, Dome JS, Malogolowkin M, et al. An international strategy to determine the role of high dose therapy in recurrent Wilms’ tumour. Eur J Cancer. 2013;49:194–210. https://doi.org/10.1016/j.ejca.2012.07.010.
de Camargo B, Melaragno R, Saba e Silva N, Mendonça N, Alvares MN, Morinaka E, et al. Phase II study of carboplatin as a single drug for relapsed Wilms’ tumor: experience of the Brazilian Wilms’ tumor study group. Med Pediatr Oncol. 1994;22:258–60. https://doi.org/10.1002/mpo.2950220409.
Green DM, Cotton CA, Malogolowkin M, Breslow NE, Perlman E, Miser J, et al. Treatment of Wilms tumor relapsing after initial treatment with vincristine and actinomycin D: a report from the National Wilms Tumor Study Group. Pediatr Blood Cancer. 2007;48:493–9. https://doi.org/10.1002/pbc.20822.
NWTS5 Roadmaps. http://www.nwtsg.org/institution/forms/nwts5/NWTS5_Roadmaps.pdf. Accessed 2 Dec 2020.
Hale J, Hobson R, Moroz V, Sartori P. Results of UK Children’s Cancer and Leukaemia Group (CCLG) protocol for relapsed Wilms’ tumour (UKWR): unified relapse strategy improves outcome. Data presented at SIOP 2008, abstract 0.154. http://onlinelibrary.wiley.com/doi/10.1002/pbc.v50:5%2B/issuetoc. Accessed 30 Nov 2020.
Malogolowkin M, Cotton CA, Green DM, Breslow NE, Perlman E, Miser J, et al. National Wilms Tumor Study Group. Treatment of Wilms tumor relapsing after initial treatment with vincristine, actinomycin D, and doxorubicin. A report from the National Wilms Tumor Study Group. Pediatr Blood Cancer. 2008;50:236–41. https://doi.org/10.1002/pbc.21267.
Abu-Ghosh AM, Krailo MD, Goldman SC, Slack RS, Davenport V, Morris E, et al. Ifosfamide, carboplatin and etoposide in children with poor-risk relapsed Wilms’ tumor: a Children’s cancer group report. Ann Oncol. 2002;13:460–9. https://doi.org/10.1093/annonc/mdf028.
Pein F, Michon J, Valteau-Couanet D, Quintana E, Frappaz D, Vannier JP, et al. High-dose melphalan, etoposide, and carboplatin followed by autologous stem-cell rescue in pediatric high-risk recurrent Wilms’ tumor: a French Society of Pediatric Oncology study. J Clin Oncol. 1998;16:3295–301. https://doi.org/10.1200/JCO.1998.16.10.3295.
Kremens B, Gruhn B, Klingebiel T, Hasan C, Laws HJ, Koscielniak E, et al. High-dose chemotherapy with autologous stem cell rescue in children with nephroblastoma. Bone Marrow Transplant. 2002;30:893–8. https://doi.org/10.1038/sj.bmt.1703771.
Campbell AD, Cohn SL, Reynolds M, Seshadri R, Morgan E, Geissler G, et al. Treatment of relapsed Wilms’ tumor with high-dose therapy and autologous hematopoietic stem-cell rescue: the experience at Children’s memorial hospital. J Clin Oncol. 2004;22:2885–90. https://doi.org/10.1200/JCO.2004.09.073.
Dome JS, Cotton CA, Perlman EJ, Breslow NE, Kalapurakal JA, Ritchey ML, et al. Treatment of anaplastic histology Wilms’ tumor: results from the fifth National Wilms’ tumor study. J Clin Oncol. 2006;24:2352–8. https://doi.org/10.1200/JCO.2005.04.7852.
Green DM, Beckwith JB, Breslow NE, Faria P, Moksness J, Finklestein JZ, et al. Treatment of children with stages II to IV anaplastic Wilms’ tumor: a report from the National Wilms’ tumor study group. J Clin Oncol. 1994;12:2126–31. https://doi.org/10.1200/JCO.1994.12.10.2126.
Brok J, Kathy Pritchard-Jones K, Geller JI, Spreafico F. Review of phase I and II trials for Wilms’ tumour—can we optimise the search for novel agents? Eur J Cancer. 2017;79:205–13. https://doi.org/10.1016/j.ejca.2017.04.005.
Green DM, Breslow NE, Ii Y, Grundy PE, Shochat SJ, Takashima J, et al. The role of surgical excision in the management of relapsed Wilms’ tumor patients with pulmonary metastases: a report from the National Wilms’ tumor study. J Pediatr Surg. 1991;26:728–33. https://doi.org/10.1016/0022-3468(91)90021-k.
Fuchs J, Szavay P, Luithle T, Furtwängler R, Graf N. Surgical implications for liver metastases in nephroblastoma—data from the SIOP/GPOH study. Surg Oncol. 2008;17:33–40. https://doi.org/10.1016/j.suronc.2007.08.011.
van den Heuvel-Eibrink MM, Hol JA, Pritchard-Jones K, van Tinteren H, Furtwängler R, Verschuur AC, et al. International Society of Paediatric Oncology — Renal Tumour Study Group (SIOP–RTSG). Position paper: Rationale for the treatment of Wilms tumour in the UMBRELLA SIOP-RTSG 2016 protocol. Nat Rev Urol. 2017;14:743–52. https://doi.org/10.1038/nrurol.2017.163.0.
Metzger ML, Stewart CF, Freeman BB 3rd, Billups CA, Hoffer FA, Wu J, et al. Topotecan is active against Wilms’ tumor: results of a multi-institutional phase II study. J Clin Oncol. 2007;25:3130–6. https://doi.org/10.1200/JCO.2007.10.9298.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Sinha, A., Jayakumar, T.K., Sarin, Y.K. (2022). Recurrent/Relapsed Wilms’ Tumor. In: Sarin, Y.K. (eds) Wilms’ Tumor. Springer, Singapore. https://doi.org/10.1007/978-981-19-3428-5_31
Download citation
DOI: https://doi.org/10.1007/978-981-19-3428-5_31
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-3427-8
Online ISBN: 978-981-19-3428-5
eBook Packages: MedicineMedicine (R0)